Abstract
Three-dimensional printing (3Dp) is being increasingly used in medical education. Although the use of such lifelike models is beneficial, well-powered, randomized studies supporting this statement are scarce. Two spinal fracture simulation models were generated by 3Dp. Altogether, 120 medical students (54.2% females) were randomized into three teaching module groups [two-dimensional computed tomography images (CT), 3D, or 3Dp] and asked to answer 10 key anatomical and 4 evaluative questions. Students in the 3Dp or 3D group performed significantly better than those in the CT group, although males in the 3D group scored higher than females. Students in the 3Dp group were the first to answer all questions and there were no sex-related differences. Pleasure, assistance, effect and confidence were more predominant in students in the 3Dp group than in those in the 3D and CT groups. This randomized study revealed that the 3Dp model markedly improved the identification of complex spinal fracture anatomy by medical students and was equally appreciated and comprehended by both sexes. Therefore, the lifelike fracture model made by 3Dp technology should be used as a means of premedical education.
Similar content being viewed by others
Introduction
Learning and identification of anatomy are a fundamental component for neurosurgery treatments. Practicing dissection of human vertebrae is the best method for improving the understanding of and surgery skills required for spinal fractures1,2. However, because of the scarcity of bones, not all medical students, even those staying in hospitals at all hours, can be provided this opportunity3. Therefore, we believe that if a model reflecting the condition could be used in class, numerous medical students could study and practice using this emulation bone model and benefit from it4,5.
3Dp is a fast and inexpensive technology of rapid prototyping (RP), a technology based on the construction of physical three-dimensional, layer by layer, according to their respective virtual models6,7. The model generated from scanning patients is sliced and its transversal sections are physically reproduced through automated processes of layer-by-layer construction in powdered, solid, or liquid raw materials1,2,6. With the potential of spatial understanding, 3Dp is increasingly used not only in the clinical setting but also in the education of both medical students and patients8,9,10. However, in China, the clinical routine is almost exclusively characterized by two-dimensional (2D) images computed tomography (CT) and magnetic resonance imaging; some medical universities teach through 3D images11. Teaching combined with 3Dp technology is very rare, owing to the theory limitation.
We conducted a randomized controlled study for investigating the impact of 3Dp models on the identification of spinal fracture for medical students as well as for assessing sex-related differences in benefits compared with 2D and 3D presentations.
Material and Methods
Generating simulation fracture models by three-dimensional printing technology
Raw CT data of the spinal vertebrae from two patients were used: one had a fracture in the second cervical vertebra (C2) and another had a fractured ninth thoracic vertebra (T9). CT scans were taken in the horizontal plane using a slice width of 0.5 mm, a helical pitch of 2.5 and an image production interval of 0.1 mm. After scanning, data were exported to a DICOM file. Next, MIMICS 15.0 (Materialise, Belgium) was used for reconstructing a 3D image, which was converted to a **. STL (STereo Lithography) file from the DICOM file. Finally, the **. STL file was sent to the 3D printer (XYZ printing, China) based on fused deposition modeling (FDM) technology, whereas the sintered layers were accumulated using a helical pitch of 0.1 mm12. After assessment by two senior professors, no differences were found compared with the original fracture; therefore, the model was used in the teaching process as the next step.
Medical education
All students completed their basic training by learning anatomy not only through textbooks and dissecting corpses but also through computer simulations in anatomy during their first or second year of enrollment in Binzhou Medical University. First, a lecture was given to the students, describing the spinal anatomy and the definition of normal cervical and thoracic vertebra segments was presented using PowerPoint. Further, a short technical description of the teaching module (TM) was provided for helping the students in successfully completing the teaching process (Fig. 1).
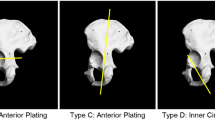
Students were randomized into three groups using a computer program. The TM of the first group (CT group) was based on the CT images of the two patients in sagittal, coronal and axial planes (Fig. 2). The TM of the second group (3D group) was based on the 3D images reconstructed from the DICOM file, original data file from the two patients, each angle freely adjustable in the computer (Fig. 3 and S1,2 Video). In the last group (3Dp group), each student received the two fracture models (Fig. 4 and S3,4 Video). A teacher provided a detailed interpretation of the fracture in each group.
Photos of the teaching module for three-dimensional printing models.
Two lifelike fracture models were reconstructed by a three-dimensional (3D) printer. The ninth thoracic vertebra (T9): a, b, c and d (dorsal, right, ventral and left views, respectively); the second cervical vertebra (C2): e, f, g and h (dorsal, right, ventral and left views, respectively)
Each group of 40 students was divided into seven subgroups in the teaching progress. Each subgroup was assigned six computers or 12 models. By the end of the class, each student answered 10 questions regarding spinal fractures and 4 evaluation questions (Table 1) about the TM, assessed by an examination paper, which contained many “3D images” (S Figure 1). In the examination paper, each student had to enter sex, school age in medical school and a unique randomization code; an invigilator recorded the assignment time of each student. The answers to each question and the required time were recorded.
Students voluntarily participated through a hospital network post and to protect their rights, no identifying information was recorded. This study was approved by the ethics review committee of Binzhou Medical College (20140108) and all students provided their written informed consent. All methods were performed in accordance with the approved guidelines.
Statistical analysis
Statistical analysis was performed using SPSS (version 19.0 for Windows) and the level of statistical significance was set at the p value of <0.05. The distribution of continuous data was described using mean and standard deviation (SD). The data was analyzed using two-way analysis of variance (ANOVA) after testing for homogeneity. Tukey’s or Sidak’s multiple comparison test was used for post hoc analysis. In categorical data with absolute and relative frequencies (counts and percentages), potential differences between the groups were evaluated using chi-square tests. Box plots were used for visualizing the distribution of continuous data by GraphPad prism (version 6.0 for Windows).
Results
Fracture models were reconstructed by three-dimensional printing technology
Two lifelike fracture models were reconstructed by 3Dp technology, reflecting the situation of two patients with spinal fractures (Fig. 4 and S3,4 Video). Each model was constructed in 6 h at an approximate printing cost of US$ 20.
Characteristics of students
In this randomized controlled study, a total of 120 medical students (54.2% females) participated and no one dropped out. Forty students (22 females) were randomized into the CT group, 40 (21 females) into the 3D group and 40 (22 females) into the 3Dp group, indicating no significant sex-related differences (Table 2). We also counted each student’s school age in medical university and there was no statistically significant difference (Table 2).
Sum scores of correct answers and time spent
We completed the randomized controlled study in three months. Overall, the results of the sum scores of correct answers (Table 3) were significantly different between the three groups affected by the TM and sex [F value of the three TMs (FTM) = 50.65, p < 0.0001 and that of sex (Fsex) = 4.789 p = 0.0307; two-way ANOVA]. Further, post hoc analysis revealed that students in the 3Dp and 3D groups performed better than those in the CT group based on Tukey’s multiple comparison test (3D vs. CT: mean difference (MD) = 2.325, p < 0.0001 and 3Dp vs. CT: MD = 3.075, p < 0.0001), while no significant differences were found between 3D and 3Dp groups (3D vs. CT: MD = 0.7500, p = 0.0508). Males in the 3D group scored higher than females (male vs. female: MD = 0.7500, p = 0.0508) by Sidak’s multiple comparison test; however, this phenomenon did not occur in the CT and 3Dp groups (Fig. 5).
Sum score of correct answers.
Students in the three-dimensional printing (3Dp) or 3D groups performed significantly better than those in the computed tomography (CT) group; males in the 3D group scored higher than females, in contrast to those in the 3Dp (post hoc by Sidak’s test) groups. FTM: F value of the three teaching modules; Fsex: F value of sex; **p < 0.01.
Analysis of the time required for answering the 10 questions revealed a significant difference between imaging modalities: students in the CT group required 708.56 ± 212.08 s vs. 896.59 ± 266.08 s (mean ± SD s of male vs. female) for completing the 10 questions, whereas those in the 3D and 3Dp groups required 514.22 ± 177.69 s vs. 593.48 ± 207.36 s and 373.56 ± 206.97 s vs. 376.72 ± 138.95 s, respectively (Table 3). Post hoc analysis revealed that students in the 3Dp group were the first to answer all the questions (3Dp vs. CT: MD = −436.7, p < 0.0001; 3Dp vs. 3D: MD = −177.1, p = 0.0006; Tukey’s test) and there were no differences between males and females (female vs. male: MD = 3.172, p > 0.9999, Sidak’s test, Fig. 6).
Answers to the evaluated questions
All students enjoyed the TM. However, students in the 3Dp (75%) and 3D (62.5%) groups answered the item “pleasure” (question #11) significantly more often with “yes, very much” compared with those in the CT group (37.5%; mean = 15.29, p = 0.004, chi-square test). The modality “assistance” (question #12) was rated “yes” significantly more often by students in the 3D (65%) and 3Dp (75%) groups compared with those in the CT (32.5%; mean = 18.02, p = 0.001, chi-square test) group. When interrogated about the personal learning effect (question #13), students in the CT group (47.5%) significantly more often answered “no,” whereas those in the 3D (60%) and 3Dp (70%) groups significantly more often answered “yes” (mean = 16.2, p = 0.003, chi-square test). Finally, significantly more students in the 3Dp (75%) and 3D (62.5%) groups felt that they could confidently explain the fracture to their fellow students (question #14) compared with those in the CT (25%; mean = 22.24, p = 0.000, chi-square test) group. Pleasure, assistance, effect and confidence were predominant in students in the 3Dp group.
Discussion
3Dp has been extensively used for designing and manufacturing prototypes in the fields of engineering and technology. In recent years, it has also been applied to medicine. There are five types of prototyping methods: those employing a stereolithography apparatus, selective laser sintering and FDM and laminated object manufacturing and inkjet printing13. FDM is popular in hospitals and families in China because the involved printing process is cost-effective and has a high accuracy. In this randomized study, two authentic fracture models were reconstructed by this technology, reflecting the situation of spinal fractures (Fig. 4).
Altogether, 120 medical students (54.2% females) participated and they were randomized into the CT, 3D and 3Dp groups, with no significant sex- and age-related differences. Each student was asked to answer 10 key anatomical questions and 4 evaluative questions. Students in the 3Dp and 3D groups performed significantly better than those in the CT group, although males in the 3D, not 3Dp, group scored higher than females. Meanwhile, students in the 3Dp group were the first to answer all questions and no sex-related differences were found. Students in the 3Dp group answered more positively than those in the CT and 3D groups to the 4 evaluation questions.
Sex-related differences were observed in understanding virtual images, which should not be ignored during teaching14,15. We found that males have an unfair advantage in understanding 3D image reconstructions compared with females. However, this sex-related difference was not present in the 3Dp group because teaching was based on real models.
3Dp is a “clone technology” that enables the generation of realistic models convenient for students to observe from any angle12,16,17,18. We also observed that using 3Dp objects improves the learning efficiency of medical students, helps them acquire expertise and increases their interest and enthusiasm, which are important components in learning.
The application of 3Dp technology in medical education is rapidly developing. However, randomized controlled studies of medical education using 3D printed models remain scarce. Preece et al.19 developed and evaluated the use of a model demonstrating the complex spatial relationships of the equine foot, suggesting that physical models have a significant advantage over alternative learning resources in enhancing visuospatial and 3D understanding of complex anatomical architecture and that 3D computer models have significant limitations with regard to 3D learning. Moreover, many case studies regarding the benefits of 3Dp technology in teaching and training processes have been reported. Mashiko et al.20 developed a method for fabricating a 3D hollow and elastic aneurysm model for surgical simulation and training. They also presented a simulated 3D model of a human temporal bone made by the selective laser sintering method, based on detailed CT data and it was found useful for understanding the 3D aneurysm structure. Cardiovascular anomalies have been presented in a study by Vranicar et al.21, where 3D models of blood vessels were analyzed for a better preoperative planning.
Despite our enthusiasm for this TM, our study has some limitations. First, there is a potential selection bias because the sample size was relatively small. Second, the master knowledge of each student may not have been entirely homogenous, which could have affected the stabilization, validation and generalization of the final results. Third, the printing model and image data did not include analysis of muscles and neurovascular tissue surrounding the fracture, without which the model cannot completely represent a fracture condition. Finally, several technical problems, such as the lengthy printing time, needs to be resolved, which currently limits the applicability of the model.
Future advances in implementing 3Dp in medical education could include the development of printing devices that allow rapid onsite printing in the teaching hospital and development of 3Dp models that mimic the haptic characteristics of specific tissue (i.e., nerves, arteries, muscles).
Conclusion
This randomized study revealed that the 3Dp model markedly improved the identification of complex spinal fracture anatomy by medical students and was equally appreciated and comprehended by both sexes. Therefore, the lifelike fracture model made by 3Dp technology should be used as a means of premedical education.
Additional Information
How to cite this article: Li, Z. et al. Three-dimensional printing models improve understanding of spinal fracture—A randomized controlled study in China. Sci. Rep. 5, 11570; doi: 10.1038/srep11570 (2015).
References
Groth, C., Kravitz, N. D., Jones, P. E., Graham, J. W. & Redmond, W. R. Three-dimensional printing technology. Journal of clinical orthodontics : JCO 48, 475–485 (2014).
Rengier, F. et al. 3D printing based on imaging data: review of medical applications. International journal of computer assisted radiology and surgery 5, 335–341, 10.1007/s11548-010-0476-x (2010).
Peltola, S. M., Melchels, F. P., Grijpma, D. W. & Kellomaki, M. A review of rapid prototyping techniques for tissue engineering purposes. Ann Med 40, 268–280, 10.1080/07853890701881788 (2008).
Wang, F., Ren, X. & Yang, L. Research progress of three-dimensional printing technique in joint surgery. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi = Chinese journal of reparative and reconstructive surgery 28, 272–275 (2014).
Luo, Q., Lau, T. W., Fang, X. & Leung, F. Application of three-dimensional printing technique in orthopaedics. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi = Chinese journal of reparative and reconstructive surgery 28, 268–271 (2014).
Gerstle, T. L., Ibrahim, A. M., Kim, P. S., Lee, B. T. & Lin, S. J. A plastic surgery application in evolution: three-dimensional printing. Plastic and reconstructive surgery 133, 446–451, 10.1097/01.prs.0000436844.92623.d3 (2014).
Schneider, J. et al. A novel 3D integrated platform for the high-resolution study of cell migration plasticity. Macromol Biosci 13, 973–983, 10.1002/mabi.201200416 (2013).
Flugge, T. V., Nelson, K., Schmelzeisen, R. & Metzger, M. C. Three-dimensional plotting and printing of an implant drilling guide: simplifying guided implant surgery. Journal of oral and maxillofacial surgery : official journal of the American Association of Oral and Maxillofacial Surgeons 71, 1340–1346, 10.1016/j.joms.2013.04.010 (2013).
Chien, K. B., Makridakis, E. & Shah, R. N. Three-dimensional printing of soy protein scaffolds for tissue regeneration. Tissue engineering. Part C, Methods 19, 417–426, 10.1089/ten.TEC.2012.0383 (2013).
Akiba, T., Inagaki, T. & Nakada, T. Three-Dimensional Printing Model of Anomalous Bronchi before Surgery. Annals of thoracic and cardiovascular surgery : official journal of the Association of Thoracic and Cardiovascular Surgeons of Asia 20 Suppl, 659–662, 10.5761/atcs.cr.13-00189 (2014).
Li, Q. Application of three-dimensional printing technique in plastic surgery. Zhongguo xiu fu chong jian wai ke za zhi = Zhongguo xiufu chongjian waike zazhi = Chinese journal of reparative and reconstructive surgery 28, 266–267 (2014).
Torres, K., Staskiewicz, G., Sniezynski, M., Drop, A. & Maciejewski, R. Application of rapid prototyping techniques for modelling of anatomical structures in medical training and education. Folia Morphol (Warsz) 70, 1–4 (2011).
Huang, Z., Wang, X. Z. & Hou, Y. Z. Novel method of fabricating individual trays for maxillectomy patients by computer-aided design and rapid prototyping. Journal of prosthodontics : official journal of the American College of Prosthodontists 24, 115–120, 10.1111/jopr.12183 (2015).
Muller-Stich, B. P. et al. Regular three-dimensional presentations improve in the identification of surgical liver anatomy - a randomized study. BMC medical education 13, 131, 10.1186/1472-6920-13-131 (2013).
Beermann, J. et al. Three-dimensional visualisation improves understanding of surgical liver anatomy. Medical education 44, 936–940, 10.1111/j.1365-2923.2010.03742.x (2010).
Rengier, F. et al. 3D printing based on imaging data: review of medical applications. International Journal of Computer Assisted Radiology and Surgery 5, 335–341, 10.1007/s11548-010-0476-x (2010).
Fuller, S. M., Butz, D. R., Vevang, C. B. & Makhlouf, M. V. Application of 3-dimensional printing in hand surgery for production of a novel bone reduction clamp. The Journal of hand surgery 39, 1840–1845, 10.1016/j.jhsa.2014.06.009 (2014).
Anderson, P. J., Yong, R., Surman, T. L., Rajion, Z. A. & Ranjitkar, S. Application of three-dimensional computed tomography in craniofacial clinical practice and research. Aust Dent J 59 Suppl 1, 174–185, 10.1111/adj.12154 (2014).
Preece, D., Williams, S. B., Lam, R. & Weller, R. “Let’s get physical”: advantages of a physical model over 3D computer models and textbooks in learning imaging anatomy. Anatomical sciences education 6, 216–224, 10.1002/ase.1345 (2013).
Chueh, J. Y., Wakhloo, A. K. & Gounis, M. J. Neurovascular modeling: small-batch manufacturing of silicone vascular replicas. AJNR. American journal of neuroradiology 30, 1159–1164, 10.3174/ajnr.A1543 (2009).
Vranicar, M., Gregory, W., Douglas, W. I., Di Sessa, P. & Di Sessa, T. G. The use of stereolithographic hand held models for evaluation of congenital anomalies of the great arteries. Studies in health technology and informatics 132, 538–543 (2008).
Acknowledgements
We would like to thank the colleagues in the affiliated hospital of Binzhou Medical University.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: L.Z.F. L.Z.Z. Performed the experiments: X.R.Y. L.Z.F. L.M. Z.W.S. C.Z. Analyzed the data: X.R.Y. L.Z.Z. L.J.M. L.Y.L. S.D.H. Wrote the paper: L.Z.F. L.Z.Z. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Li, Z., Li, Z., Xu, R. et al. Three-dimensional printing models improve understanding of spinal fracture—A randomized controlled study in China. Sci Rep 5, 11570 (2015). https://doi.org/10.1038/srep11570
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep11570
This article is cited by
-
Development and evaluation of a portable and soft 3D-printed cast for laparoscopic choledochojejunostomy model in surgical training
BMC Medical Education (2023)
-
Full-sized realistic 3D printed models of liver and tumour anatomy: a useful tool for the clinical medicine education of beginning trainees
BMC Medical Education (2023)
-
Research relating to three-dimensional (3D) printing in spine surgery: a bibliometric analysis
European Spine Journal (2023)
-
3D printed skulls in court — a benefit to stakeholders?
International Journal of Legal Medicine (2023)
-
Systematic review of three-dimensional printing for simulation training of interventional radiology trainees
3D Printing in Medicine (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.