Abstract
The incidence of pan-urothelial cell carcinoma (panUCC), which refers to the presence of both bilateral (UTUC) and bladder tumor (BT), is relatively low. However, the profile of a panUCC cohort of patients remains to be elucidated. We reviewed the data of consecutive UTUC patients who received treatment at our center from 1999 to 2012. Overall, 45 patients were included in this study, with a median age of 64.5 years. Fourteen patients initially presented with unilateral UTUC, 11 initially with BT and the remainder with multiple tumors. Patients with UTUC were more likely to manifest higher rates of muscle invasion and larger-sized tumors. Five patients were treated with complete urinary tract exenteration (CUTE) and most patients (73.3%) received combined management with conservative and radical surgery. After a median follow-up of 77 months, 18 patients (40%) died including 15 (33.3%) due to cancer. Higher tumor stage was the only risk factor predictive of worse survival. Nineteen patients experienced local recurrence after conservative surgery. This study indicated that PanUCC involves either synchronous or metachronous presentation of tumors with a high risk of tumor recurrence, progression and dissemination after conservative surgery.
Similar content being viewed by others
Introduction
Urothelial carcinomas are distinguished by their ability to develop multiple foci in a synchronous or sequential fashion throughout the urinary tract1. Upper tract urothelial carcinoma (UTUC) and bladder tumor (BT) often co-exist2,3 and 1.6% to 6.9% of UTUC patients have been reported to suffer from synchronous or metachronous bilateral disease4,5,6.
Several case reports found patients with both bilateral UTUC and BT7,8,9,10. Nguyen et al. proposed the term pan-urothelial urothelial cell carcinoma (panUCC) to describe cancer in both upper urinary tracts and the bladder11. They analyzed 36 patients treated between 1988 and 2013 in two American centers and found that pan-urothelial involvement indicates poor prognosis11.
Given the rarity of UTUC12, the incidence of panUCC is relatively low and the characteristics of this cohort of patients remain to be elucidated. Whether complete urinary tract exenteration (CUTE), which entails radical removal of both kidneys and bladder, should be the standard surgical option for these patients remains controversial. Further, considering the heterogeneity and differences in incidence of urothelial carcinoma between Asian and Western patients13, profiling the disease in an Asian cohort may facilitate management and elucidation of the underlying mechanisms. In an attempt to address these issues, we performed a descriptive analysis of clinical and pathological features along with surgical outcomes of patients with panUCC in a large Chinese center.
Results
Clinical characteristics, initial presentation and tumor progression
Following approval by the institutional review board, we reviewed the data of consecutive UTUC patients who received treatment in the Department of Urology, Peking University First Hospital from 1999 to 2012. Inclusion criteria entailed diagnosis of urothelial carcinoma in the bilateral upper tracts and in the bladder either synchronously or metachronously. For patients who did not undergo surgical intervention, we defined tumor presence by positive urine cytology in conjunction with direct visualization of the tumors via endoscopy or conclusive imaging studies. A total of 45 patients qualified for our study based on these criteria.
The median age of these urban patients was 64.5 years (IQR 58–70), with 15 male (33.3%) and 30 female patients (66.7%). Four patients (8.9%) had a personal history of another malignancy. Only one patient had a family history of malignant tumors. Twenty-one patients consumed Chinese herbs containing aristolochic acid (AA) for at least six months; 9 patients denied the intake of such herbs and the remaining patients were unable to provide any data regarding their herbal treatment. Six patients reported a history of renal transplantation due to severe chronic kidney disease (CKD), 12 patients suffered from end-stage renal disease (ESRD) and 7 were on dialysis. Patient characteristics are summarized in Table 1.
Fourteen patients initially presented with unilateral UTUC, 11 with BT and the remainder with tumors at multiple synchronous sites: 10 with bilateral UTUC, 6 with unilateral UTUC plus concomitant BT and 4 with synchronous panUCC. The median time from initial presentation to tumor dissemination to a second or a third site was 8 months (range 0–84) and 21 months (range 0–141), respectively. In patients who initially presented with tumor in only one site, the median time for metachronous tumor involvement at second and third sites, was 24 months (range 3–84 and 3–141, respectively).
Pathological features of the first tumor site and third (last) metachronous tumor site are listed in Table 2. Patients who initially presented with synchronous tumor in all 3 sites were excluded from this analysis, as were patients with incomplete data. Although no differences in tumor stage or grade were seen between the first and third tumors, the third tumor site more frequently displayed sessile architecture and multiple foci.
Location-based characteristics
Clinicopathologic features stratified by initial site of tumor involvement (i.e., upper tract, bladder, or both) are displayed in Table 3. Initial presentation involved 48 upper tract tumors and 21 bladder tumors. Location of initial tumor had no effect on the time to development of metachronous tumors or on final tumor stage or grade.
We also compared the pathological characteristics of all tumors located in the upper tracts and in the bladder regardless of the sequence of presentation. More muscle-invasive (T ≥ 2) and larger-sized tumors were characteristic of UTUC, while BTs more often featured multiple foci (Table 4). The location of all UTUC and BTs based on available data is shown in Fig. 1. Tumors were ubiquitous in the urothelium, though the posterior wall of the bladder was the most frequent tumor location, while tumors in the upper tract of renal pelvis were more common than ureteral tumors.
Treatment and prognosis
As shown in Table 1, five patients were treated with CUTE, while most patients (73.3%) received combined conservative and radical surgery. Three patients received conservative surgery in all the three sites. Four patients with metachronous UTUC following unilateral treatment refused contralateral radical nephroureterectomy (RNU) despite clinician recommendations. They were treated with unilateral RNU (in 1 case) or nephron-sparing techniques (1 case of pelvic tumor resection and 2 cases of endoscopic ablation) plus synchronous or metachronous transurethral resection (TUR).
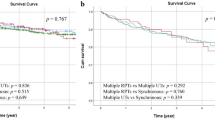
The median follow-up was 77 (16–156) months. Eighteen patients (40%) died, including 15 (33.3%) from urothelial cancer. The 2- and 5-year cancer-specific survival (CSS) rates were 95.6% and 81.2%, respectively. Univariate analysis revealed that higher tumor stage was the only risk factor contributing to worse CSS (Fig. 2), while no parameter had a statistically significant impact on overall survival (Table 5). Neither location of initial tumor nor surgical approach independently predicted survival outcomes.
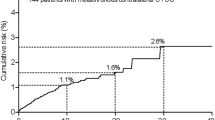
As shown in Table 4, a large proportion of UTUC cases were treated with radical surgery (RNU), while most BT patients underwent conservative surgery (TUR). Nineteen patients (with 22 sites) who received conservative surgery experienced local recurrence. Following surgery for recurrent tumor, 10 patients ultimately underwent CUTE. During follow-up, 19 patients required permanent dialysis (none of whom were renal transplant recipients), including 6 patients with at least one kidney.
Discussion
To the best of our knowledge, this is the first study detailing the clinicopathologic characteristics and treatment outcomes of panUCC in a Chinese cohort, with further substratified analysis based on tumor location. Elucidating the features of this uncommon disease entity, our data may contribute to optimal and personalized risk-based therapy while supporting future investigations into the biological mechanisms underlying multiple urothelial tumors. In our previous study, women tended to more often suffer from synchronous bilateral UTUC5, while patients with CKD had higher risk for synchronous and metachronous bilateral UTUC4,5 as well as concomitant non muscle invasive bladder cancer (NMIBC) with unilateral UTUC2. We have previously found that women also tended to consume more AA-containing herbs2,4,5,14. The current study confirms the elevated risk for panUCC in women and in patients with renal insufficiency. Unlike the cohort of Nguyen et al.11, these patients do not manifest other distinguishing features, such as history of other malignant tumors or tobacco use. Generally, considering the prevalence of CKD and female gender among Chinese patients with UTUC14, it is difficult to recognize a patient who is at risk of pan-urothelial recurrence based on initial presentation alone.
Although both UTUC and BT affect urothelial tissues, there are significant differences in their mechanisms of carcinogenesis, biological behaviors and prognosis15,16. In panUCC, regardless of synchronous or metachronous involvement, tumors in different locations still manifest the biological characteristics of primary UTUC and primary BT. In our cohort, BT demonstrated higher rates of multiple foci, while upper tract tumors were frequently muscle-invasive and larger. TUR is a commonly used bladder-preserving strategy especially for early stage tumors, while the current gold-standard treatment for UTUC remains RNU. Compared with Nguyen et al.’s study11, more patients that initially presented with UTUC than with BT (48 and 21, respectively, vs. 19 and 17, respectively) and 20 patients (44.4%) initially presented synchronously with two or three sites of tumor involvement. Given the higher prevalence of UTUC in China, especially in patients with CKD, endemic differences between the cohorts may potentially account for this discrepancy.
Tumors that metachronously originated at the third site more frequently demonstrated sessile architecture and multiple tumor foci when compared with tumors at the initial site. This finding was consistent with Nguyen et al.’s findings, which showed that six patients who presented with low-grade disease were upgraded at the time of recurrence11. This seems to suggest that recurrent tumors tend to progress and demonstrate more aggressive characteristics, which emphasizes the significance of radical surgery such as CUTE. Although no consensus has been reached on the role of tumor burden in oncologic control3,17, our results suggest that recurrent disease might be lethal, underscoring the poor prognosis of panUCC. Tumor stage was the only predictive factor for worse prognosis in our survival analysis, although limited by small sample size.
Previous studies recommend CUTE for panUCC patients, especially those with ESRD7,8,9,10,18,19. Patients with severe CKD or dialysis have been shown to manifest a higher risk of developing urothelial carcinoma18,20 and of experiencing tumor recurrence4,21,22. Radical surgery decreased the possibility of recurrence and cancer-specific mortality23 and especially for severe CKD patients there’s no worry about the preservation of renal function. Even in unilateral UTUC patients, a prophylactic contralateral nephroureterectomy was recommended for uremic patients or renal transplant recipients24,25. Oncologic control and improved survival should remain the dominant therapeutic goals. Holton et al.19 also proposed that minimizing recurrence and the need for repeat surgery should be the key goals of intervention, rather than concern about the unacceptably high morbidity of CUTE.
Considering the popularity of TUR for NMIBC and the increasing acceptance of NSS in UTUC26,27, carefully selected patients with moderate renal function might be amenable to conservative surgery, which may offer improved quality of life, freedom from dialysis and decreased peri-operative complications, particularly for radical cystectomy versus TUR27,28. In our study, surgical approach and tumor recurrence exhibited no significant impact on survival, but the high recurrence rate should not be neglected and it should be noted of the probable tumor progression after recurrence as is discussed above. Besides, 6 patients ultimately required dialysis despite preservation of at least one kidney, suggesting that the renal function deteriorated after frequent surgery. With increased age, the use of organ-conserving surgeries is decreased. Conservative surgeries should be performed following individual risk-benefit analysis and rigorous post-procedure surveillance, while CUTE should remain the standard treatment.
Field cancerization hypothesis29 and intraluminal seeding30 are currently the two main theories to explain the multifocality of urothelial cancer and recurrence patterns in the urinary tract. In our prior study, we supported the role of field cancerization in explaining this phenomenon4,5, with the presumption that the high prevalence of CKD and consumption of AA-containing herbs might cause nephrotoxicity and carcinogenicity and result in neoplasms of the urothelial tract. Recurrence patterns in our heterogeneous cohort of panUCC patients include BT after UTUC and UTUC following BT. The two theories certainly co-exist and it would be difficult to claim a dominant hypothesis based solely on clinical information. Molecular biomarker profiling of each lesion in multiple urothelial carcinomas may enable the elucidation of the true relationship with AA.
Our study is limited by its retrospective approach, which precluded evaluation of potentially useful variables such as cytology and lymph node status in all patients. Further, our study cohort might be subject to selection and recall bias. Complete pathological results were not available in some patients. Urethral resection was not performed in every radical cystectomy; however, no positive surgical margin was found and no patients exhibited urethral recurrence during later follow-up. Additionally, indications for second surgery were not standardized and were based on the clinical judgment of the treating physician in conjunction with patients’ preferences and expectations.
Conclusions
PanUCC presents synchronously or metachronously. It may be difficult to identify patients at risk for metachronous development of PanUCC. We recommend CUTE as the standard surgical intervention for selected PanUCC patients with ESRD. The elevated risk of recurrence, progression and tumor dissemination following conservative surgery reflect potential disadvantages of organ-conserving strategies.
Methods
Patient selection
Ethical approval was obtained from Institutional Review Board of Peking University First Hospital. We reviewed the data of consecutive UTUC patients who received treatment in the Department of Urology, Peking University First Hospital from 1999 to 2012. This research was carried out in accordance with the approved guidelines and informed consent was obtained from all patients. Inclusion criteria entailed diagnosis of urothelial carcinoma in the bilateral upper tracts and in the bladder either synchronously or metachronously. For patients who did not undergo surgery, we defined the presence of tumor as positive urine cytology in conjunction with direct visualization of the tumors by endoscopy or conclusive imaging studies.
Patient evaluation
All patients were diagnosed with UTUC using computed tomography (CT) or magnetic resonance imaging (MRI), cystoscopy, ultrasound, and/or ureteroscopy with or without biopsy. The estimated glomerular filtration rate (eGFR) was calculated using the modified glomerular filtration rate estimating equation for Chinese patients: eGFR(ml/min/1.73m2) = 175 × Scr−1.234 × age−0.179 (×0.79 if female)31. The tumor stage was assessed according to the 2002 Union for International Cancer Control (UICC) TNM classification. Tumor grading was performed according to the World Health Organization (WHO) classification of 1973. The tumor architecture was defined as papillary or sessile after examining the final specimen.
We defined three separate tumor sites including the left upper and right upper tracts and bladder. Tumor multifocality was defined as the synchronous presence of two or more pathologically confirmed tumors in a single site. Ureteral tumors were classified as upper ureter (superior to the upper border of the sacrum), middle ureter (between the upper and lower borders of the sacrum) and lower ureter (inferior to the lower border of the sacrum) tumors.
Treatment
All patients underwent surgery within three months following the development of symptoms. Choice of treatment was left to surgeon’s discretion and performed with patient’s consent. Surgical measures considered in managing UTUC consisted of RNU with resection of bladder cuff and NSS. Treatment for BT included TUR for non-muscle-invasive disease and radical cystectomy for muscle-invasive tumors or superficial disease at high risk for progression. In urethra-sparing radical cystectomy, the surgical margin of the proximal urethra was carefully examined. For patients with synchronous tumor in either 2 or all 3 sites, surgeries for the upper and lower urinary tracts were carried out simultaneously or separately within six months.
A series of post-operative epirubicin or pirarubicin intravesical instillation was administered after TUR showed positive pathologic results, while patients without concomitant BT did not receive post-operative intravesical chemotherapy. None of these patients received neoadjuvant chemotherapy. In some patients, adjuvant chemotherapy or radiotherapy was administered when evidence of distant metastasis or retroperitoneal recurrence was documented.
Follow-up schedule
Post-operative follow-up consisted of cystoscopy every 3 months for the first 2 years, followed by annual cystoscopy surveillance. Chest X-rays, serum creatinine and abdominal ultrasound or CT/MRI were performed at the same intervals.
In patients treated with organ-preserving surgery, we defined recurrence as urothelial cancer in the same operative site on a subsequent setting, e.g. ipsilateral UTUC after endoscopic ablation or recurrent BT after TUR. Treatment measures for recurrent tumor were left to surgeon’s discretion and performed following patient consent. The cause of death was determined by the patients’ treating physicians or by death certificates. Follow-ups were censored until their last visit or death.
Statistical analysis
All statistical tests were performed with SPSS 20.0 (IBM Corp, Armonk, NY, USA). Pearson’s test and Chi-square test were used to assess categorical variables and the Mann-Whitney U test and Kruskal-Wallis H test were used for continuous variables. Univariate and multivariate analyses using the Cox’s proportional hazards regression model were used; only variables that were identified as significant by the univariate analysis were considered for the multivariate analysis. All reported P values were single-sided with statistical significance considered at P < 0.05.
Additional Information
How to cite this article: Fang, D. et al. Characteristics and treatment outcomes of pan-urothelial cell carcinoma: a descriptive analysis of 45 patients. Sci. Rep. 5, 18014; doi: 10.1038/srep18014 (2015).
References
Perez-Utrilla, P. M. et al. Simultaneous Cystectomy and Nephroureterectomy due to Synchronous Upper Urinary Tract Tumors and Invasive Bladder Cancer: Open and Laparoscopic Approaches. Curr Urol. 6, 76–81 (2012).
Fang, D. et al. Presence of Concomitant Non-Muscle-Invasive Bladder Cancer in Chinese Patients with Upper Tract Urothelial Carcinoma: Risk Factors, Characteristics and Predictive Value. Ann Surg Oncol. (2015).
Pignot, G. et al. Influence of Previous Or Synchronous Bladder Cancer On Oncologic Outcomes After Radical Nephroureterectomy for Upper Urinary Tract Urothelial Carcinoma. Urol Oncol. 32, 21–23 (2014).
Fang, D. et al. Risk Factors and Treatment Outcomes of New Contralateral Upper Urinary Urothelial Carcinoma After Nephroureterectomy: The Experiences of a Large Chinese Center. J Cancer Res Clin Oncol. 140, 477–485 (2014).
Fang, D. et al. Incidence, Characteristics, Treatment Strategies and Oncologic Outcomes of Synchronous Bilateral Upper Tract Urothelial Carcinoma in the Chinese Population. Urol Oncol. 33, 61–66 (2015).
Holmang, S. & Johansson, S. L. Synchronous Bilateral Ureteral and Renal Pelvic Carcinomas: Incidence, Etiology, Treatment and Outcome. Cancer. 101, 741–747 (2004).
Siqueira, T. J., Falcao, E. & Siqueira, T. M. Complete En Bloc Urinary Exenteration for Synchronous Multicentric Transitional Cell Carcinoma with Sarcomatoid Features in a Hemodialysis Patient. Int Braz J Urol. 32, 560–562 (2006).
Lin, V. C. et al. Single-Session Laparoscopic Total Urinary Tract Exenteration without Repositioning for Multifocal Urothelial Carcinoma in Dialysis-Dependent Patients. Urology. 77, 98–103 (2011).
Juarez-Soto, A. et al. Radical Cystectomy, Hysterectomy with Double Adnexectomy and Bilateral Nephroureterectomy with Transvaginal Extraction. Actas Urol Esp. 38, 694–697 (2014).
Li, C. C. et al. Laparoscopic Complete Urinary Tract Exenteration with the Specimen Withdrawn Transvaginally. Bju Int. 104, 82–86 (2009).
Nguyen, L., Gandhi, N., Sterling, T., Schoenberg, M. & Jarrett, T. Pd35-07 Panurothelial Cell Carcinoma: Lessons Learned. The Journal of Urology. 191, e893 (2014).
Landis, S. H., Murray, T., Bolden, S. & Wingo, P. A. Cancer Statistics, 1998. CA Cancer J Clin. 48, 6–29 (1998).
Nortier, J. L. et al. Urothelial Carcinoma Associated with the Use of a Chinese Herb (Aristolochia Fangchi). N Engl J Med. 342, 1686–1692 (2000).
Chen, X. P. et al. Predictive Factors for Worse Pathological Outcomes of Upper Tract Urothelial Carcinoma: Experience From a Nationwide High-Volume Centre in China. Bju Int. 112, 917–924 (2013).
Catto, J. W. et al. Behavior of Urothelial Carcinoma with Respect to Anatomical Location. J Urol. 177, 1715–1720 (2007).
Roupret, M. Anatomical Location of Urothelial Carcinomas of the Urinary Tract Leads to Perspectives of Specific Treatment. Future Oncol. 3, 595–599 (2007).
Miyake, H., Hara, I., Arakawa, S. & Kamidono, S. A Clinicopathological Study of Bladder Cancer Associated with Upper Urinary Tract Cancer. Bju Int. 85, 37–41 (2000).
Wu, C. F., Shee, J. J., Ho, D. R., Chen, W. C. & Chen, C. S. Different Treatment Strategies for End Stage Renal Disease in Patients with Transitional Cell Carcinoma. J Urol. 171, 126–129 (2004).
Holton, M. R., Van Zijl, P. S., Oberle, W. T., Jacobs, S. C. & Sklar, G. N. Complete Urinary Tract Extirpation: The University of Maryland Experience. Urology. 68, 65–69 (2006).
Wang, S. M., Lai, M. N., Chen, P. C. & Wang, J. D. Increased Risk of Urothelial Cancer in Young and Middle Aged Patients with End-Stage Renal Disease. J Formos Med Assoc. 114, 52–57 (2015).
Li, C. C. et al. Significant Predictive Factors for Prognosis of Primary Upper Urinary Tract Cancer After Radical Nephroureterectomy in Taiwanese Patients. Eur Urol. 54, 1127–1134 (2008).
Chung, S. D. et al. CKD as a Risk Factor for Bladder Recurrence After Nephroureterectomy for Upper Urinary Tract Urothelial Carcinoma. Am J Kidney Dis. 50, 743–753 (2007).
Fajkovic, H. et al. Results and Outcomes After Endoscopic Treatment of Upper Urinary Tract Carcinoma: The Austrian Experience. World J Urol. 31, 37–44 (2013).
Kang, C. H. et al. The Development of Bladder Tumors and Contralateral Upper Urinary Tract Tumors After Primary Transitional Cell Carcinoma of the Upper Urinary Tract. Cancer. 98, 1620–1626 (2003).
Hou, H. J., Xiao, J. & Tian, Y. Contralateral Nephroureterectomy for Renal Transplant Recipients with Unilateral Upper Urinary Tract Transitional Cell Carcinoma: A Report of 12 Cases. Transplant Proc. 45, 2203–2206 (2013).
Yakoubi, R. et al. Radical Nephroureterectomy Versus Endoscopic Procedures for the Treatment of Localised Upper Tract Urothelial Carcinoma: A Meta-Analysis and a Systematic Review of Current Evidence From Comparative Studies. Eur J Surg Oncol. 40, 1629–1634 (2014).
Singla, N. et al. Multi-Institutional Analysis of Renal Function Outcomes Following Radical Nephroureterectomy and Partial Ureterectomy for Upper Tract Urothelial Carcinoma. Urol Oncol. 33, 261–268 (2015).
Raman, J. D. et al. High Rates of Advanced Disease, Complications and Decline of Renal Function After Radical Nephroureterectomy. Urol Oncol. 32, 47–49 (2014).
Miyake, H., Hara, I., Kamidono, S. & Eto, H. Multifocal Transitional Cell Carcinoma of the Bladder and Upper Urinary Tract: Molecular Screening of Clonal Origin by Characterizing CD44 Alternative Splicing Patterns. J Urol. 172, 1127–1129 (2004).
Hafner, C. et al. Evidence for Oligoclonality and Tumor Spread by Intraluminal Seeding in Multifocal Urothelial Carcinomas of the Upper and Lower Urinary Tract. Oncogene. 20, 4910–4915 (2001).
Ma, Y. C. et al. Modified Glomerular Filtration Rate Estimating Equation for Chinese Patients with Chronic Kidney Disease. J Am Soc Nephrol. 17, 2937–2944 (2006).
Acknowledgements
This work was supported by grants from the Collaborative Research Foundation of Peking University Health Science Center and National Taiwan University; the College of Medicine (BMU20120318); the Natural Science Foundation of China (81172419, 81372746); the Natural Science Foundation of Beijing (7122183); the Clinical Features Research of Capital (No. Z151100004015173); and the Research Foundation of Peking University First Hospital. The authors thank the entire staff of the Department of Urology, Peking University First Hospital.
Author information
Authors and Affiliations
Contributions
X.L. and L.Z. contributed to the conception and design of the study. N.S., Q.H., Z.H. and L.Z. contributed to the critical revision of the article. D.F. and P.L. collected and analyzed the data and drafted the article. G.X., L.Z. and G.Z. participated in preparing figures and performing statistical analysis. All authors reviewed the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Fang, D., Liu, P., Li, X. et al. Characteristics and treatment outcomes of pan-urothelial cell carcinoma: a descriptive analysis of 45 patients. Sci Rep 5, 18014 (2016). https://doi.org/10.1038/srep18014
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep18014
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.