Abstract
Lymph node stages (pN stages) are primary contributors to survival heterogeneity of the 7th AJCC staging system for colorectal cancer (CRC), indicating spaces for modifications. To implement the modifications, we selected eligible CRC patients from the Surveillance Epidemiology and End Results (SEER) database as participants in a training (n = 6675) and a test cohort (n = 6760), and verified tumor deposits to be metastatic lymph nodes to derive modified lymph node count (mLNC), lymph node ratio (mLNR), and positive lymph node count (mPLNC). After multivariate Cox regression analyses with forward stepwise elimination of the mLNC and mPLNC for the training cohort, a nomogram was constructed to predict overall survival (OS) via incorporating preoperative carcinoembryonic antigen, pT stages, negative lymph node count, mLNR and metastasis. Internal validations of the nomogram showed concordance indexes (c-index) of 0.750 (95% CI, 0.736–0.764) and 0.749 before and after corrections for overfitting. Serial performance evaluations indicated that the nomogram outperformed the AJCC stages (c-index = 0.725) with increased accuracy, net benefits, risk assessment ability, but comparable complexity and clinical validity. All the results were reproducible in the test cohort. In summary, the proposed nomogram may serve as an alternative to the AJCC stages. However, validations with longer follow-up periods are required.
Similar content being viewed by others
Introduction
Colorectal cancer (CRC) is the third leading cause of cancer morbidity and mortality worldwide1. Despite its increasing complexity, the American Joint Committee on Cancer (AJCC) staging manual, which classifies tumors from the perspective of pathological anatomy, remains the cornerstone for the treatment and prognosis of patients with CRC2. The latest (7th edition) AJCC staging manual for CRC specifies metastases in the lymph nodes and tumor deposits (TDs) as the primary evidence of advanced disease, which results in a significant difference in the selection of subsequent adjuvant therapies and in the prediction of patient outcomes. However, survival heterogeneity is frequently present when patients with the same AJCC stages encounter distinct outcomes3. This is particularly prominent in patients with stage II and stage III CRC3. The current strategy, which determines nodal stages by positive lymph node count (PLNC) and TDs, may constitute the basis of the pN stages (pathological node stages) as a major contributor to the observed survival heterogeneity when the AJCC staging system is used.
The pN stages have several limitations, which indicates that this classification can be modified. First, the pN stages do not consider the effect of TDs on survival when lymph node metastases are present2, although the TDs have a similar prognostic impact as metastatic lymph nodes4,5. Second, the precision of the classification by PLNC depends on adequate assessments of the lymph node count (LNC), yet the LNC tends to be confounded by many operator, patient and tumor factors6,7. Consequently, the prognostic significance of the LNC is inconsistent among published observational studies6,7. No widely accepted minimum requirement of LNC is available to determine whether the identified PLNCs are adequate to maintain the accuracy of node staging7. Third, other node-related parameters such as negative lymph node count8,9 (NLNC) and lymph node ratio6,9,10 (LNR) have been demonstrated to be associated with the survival of patients with CRC, while neither the NLNC or LNR is incorporated into the AJCC staging system. Fourth, the pN stages categorize the positive lymph node count (PLNC) and are unable to incorporate continuous variables, which leads to additional loss of information and predictive accuracy. Lastly, the introduction of biomarkers such as the preoperative expression of carcinoembryonic antigen (CEA) may offer extra precision in the prediction of CRC disease status, which might help to ease increased concerns regarding the anatomical basis of the pN stages11.
In the present study, we anticipated that the expression of CEA, the presence of TDs and node-related parameters including the LNC, NLNC, PLNC and LNR could explain and address to a certain degree the survival heterogeneity caused by the pN stages. Modifications of the pN stages by the addition of CEA expression, TDs and node-related factors to a multivariate nomogram might improve its predictive accuracy for CRC. To test this hypothesis, we retrospectively reviewed relevant clinical-pathological variables and the vital status of CRC patients from the Surveillance Epidemiology and End Results (SEER) database. The first aim of this study was to verify the basis for modifying the pN stages by the above-mentioned parameters and to show whether TDs might be incorporated as metastatic lymph nodes. The second aim was to determine and validate the optimal multivariate model that was used to establish the predictive nomogram after the modifications. This study may help us understand the survival heterogeneity complicated by the pN stages and may offer patients with CRC an improved prognostic tool without increased complexity.
Methods
Patients and eligibility criteria
The SEER program (http://seer.cancer.gov) is maintained by the National Cancer Institute and is a national database of cancer statistics in the United States12. The data on cancer research are freely available to the public upon submission of a signed data-use agreement (http://seer.cancer.gov/data/sample-dua.html) to the SEER administration12. The experimental protocols used in our study were exempt from review by the ethics committee of the Shanghai East hospital since the data were anonymously extracted and analyzed. Informed consents from participants were also waived due to the complete anonymity of the patients. The study was conducted according to the TRIPOD statement13 and adhered to the Declaration of Helsinki for medical research involving human subjects14.
In the present study, any CRC patients from the SEER database who were diagnosed in 2010 and 2011 were considered for inclusion in a training cohort and a test cohort, respectively. However, patients were excluded if they met the following criteria: (1) were not diagnosed with adenocarcinoma, (2) unproven diagnosis by surgical pathology, (3) history of malignancy, (4) multiple primary tumors, (5) preoperative/intraoperative radiation therapy, (6) unknown or borderline CEA status, (7) pTis lesions or inconsistent/insufficient information to specify the tumor-node-metastasis (TNM) stages, (8) unknown number of TDs or unknown LNC or PLNC, (9) follow-ups with incomplete dates or follow-ups of less than one month and (10) inactive follow-ups or unknown outcomes.
Variables and endpoint
The variables that were evaluated were as follows: sex, age, race, tumor location, grade, perineural invasion, CEA expression, TDs, LNC, PLNC, NLNC, LNR, the 7th AJCC/TNM stages, postoperative radiation, survival (in months) and vital status. Among them, the NLNC and the LNR were derived from both the LNC and the PLNC. The endpoint we used was overall survival (OS), which was determined by the vital status.
Statistical analyses
Discontinuous variables were presented as frequencies while continuous variables were presented as medians and ranges due to skewed distributions. Cumulative survival rates among patients with different pN stages with and without stratifications were plotted using the Kaplan-Meier (K-M) curve method and were compared by log-rank test. To modify the pN stages, each TD was quantified as a metastatic lymph node and the node-parameters were recalculated accordingly to yield the modified LNC (mLNC), PLNC (mPLNC), LNR (mLNR) and AJCC (mAJCC) stages. Based on the training cohort, the mLNC, mPLNC, mLNR, NLNC, CEA expression, pT stages and M stages were then incorporated into a multivariate Cox regression analysis with a forward stepwise elimination of relatively unimportant variables. Advantages of the final multivariate model were attested by comparisons with the AJCC and mAJCC stages using goodness of fit (log-likelihood), Akaike information criterion (AIC) and concordance index (c-index). Next, the nomogram was constructed based on the final model of the training cohort. The performance of the nomogram was internally evaluated by c-index, 200-resample bootstrap validation, calibration and the area under the time-dependent receiver operating characteristic (ROC) curve (AUC) at different time points. External validation was achieved by applying the nomogram to the test cohort using similar statistics. Decision curve analysis15 (DCA) was also performed to compare the threshold probabilities and the net benefits associated with the nomogram and the AJCC stages. Lastly, to demonstrate the ability of the nomogram to make risk assessments, each patient in the training cohort was given a total score based on the nomogram. Risk classifications at the overall stage level were illustrated with K-M curves after the patients were divided into different prognostic groups according to percentile scores. Risk stratifications for individual AJCC stages as well as for patients who received postoperative radiation were performed using similar methods. All the analyses were processed by the SPSS 18.0 (SPSS Inc., Chicago, IL, USA) and R 3.2.3 programs. By convention, only a two-sided P value < 0.05 was considered statistically significant.
Results
Characteristics of the study cohorts
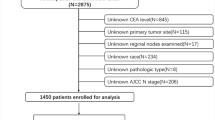
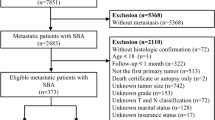
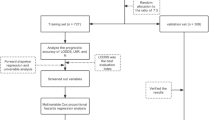
Although 36,792 and 36,369 patients were identified separately, 6675 and 6760 patients met the eligible criteria for the training and test cohorts, respectively (Fig. 1). Descriptive characteristics and the variables assessed in the two cohorts are shown in Tables 1 and 2.
Evaluation of the pN stages
The results of the K-M curve analyses for the training cohort (Fig. 2) showed that the TDs, LNC, NLNC, LNR and expression of CEA were significantly associated with OS (all Plog-rank < 0.001). All of these could be used to stratify the pN stages (all Plog-rank for trend <0.001), while pairwise comparisons revealed some discrepancies among these parameters. For instance, no apparent survival difference was identified between pN1c stage patients and pN1a stage patients (Plog-rank = 0.318) or between pN1c stage patients and pN1b stage patients (Plog-rank = 0.343) (Fig. 2A). This was also the case for patients who were TD (−) LN (+) (namely, TD-negative and node-positive cases) and patients who were TD (+) LN (−) (Fig. 2D, Plog-rank = 0.164). The results insinuated that metastasis in TDs and lymph nodes might have a comparable impact on OS. Furthermore, the survival of node-positive patients was significantly different depending on the TD status (Fig. 2D, Plog-rank < 0.001), which indicated that the effect of TD could not be ignored when lymph node metastases were present. Moreover, in patients with lymph node metastases (LNR > 0, n = 2796), the OS of pN2 stage patients with a decreased LNR (≤median) was comparable to that of pN1 stage patients with an LNR either above or below the median (0.15) (Fig. 2J, Plog-rank = 0.132 and 0.453). In addition, the expression of CEA exerted a reverse effect on the pN stages (Fig. 2L) as the survival of CEA (−) pN1 patients was better than that of CEA (+) pN0 patients (Plog-rank < 0.001); moreover, a similar relationship was found between CEA (−) pN2 patients and CEA (+) pN1 patients (Plog-rank = 0.021). The results for the LNR and CEA expression implied that advanced pN stages were not necessarily associated with a shortened OS. Modifications of the heterogeneous pN stages might bring improved precision to survival estimations.
Evaluations on the pN stages with Kaplan-Meier curve analyses.
(A) pN stages, (B) broad node stages, (C) TD, (D) stratification by TD status, (E) LNC, (F) stratification by LNC, (G) NLNC, (H) stratification by NLNC, (I) LNR, (J) stratification by LNR, (K) CEA, (L) stratification by CEA. The median LNC and NLNC were 17 and 16, respectively. The analyses for LNR were based on patients with lymph node metastasis (n = 2796) with a median LNR of 0.15. All log-rank P values for trend and pairwise comparisons were <0.05 unless otherwise specified. TD, tumor deposit; LNC, lymph node count; NLNC, negative lymph node count; LNR, lymph node ratio; CEA, carcinoembryonic antigen; Cum OS, cumulative overall survival.
Modifications of the N factor
Considering that TDs had a prognostic effect similar to that of positive lymph nodes, these were combined as the mPLNC, the method of which is described above. The results of multivariate Cox analyses for the training cohort are shown in Table 3. The mLNC and mPLNC were excluded due to lack of significance (both P = 0.675). Comparisons of the models showed that the multivariate model was the optimal model since it yielded the highest log-likelihood (−13,334.16/−13,421.76/−13,422.92), c-index (0.750/0.725/0.725) and the lowest AIC value (26,686.32/26,859.52/26,861.84) compared with the mAJCC and AJCC stages. The mAJCC stages were also improved with higher goodness of fit and lower information loss compared with the AJCC stages.
Predictive nomogram
The nomogram was constructed based on the final multivariate model for the training cohort (Fig. 3A).
Establishment and internal validation of the nomogram.
(A) Nomogram based on the training cohort, (B) calibration for 12-month OS, (C) calibration for 24-month OS, (D) calibration for 36-month OS, (E) calibration for 47-month OS, (F) decision curve analysis for 12-month OS, (G) decision curve analysis for 24-month OS, (H) decision curve analysis for 36-month OS, (I) decision curve analysis for 47-month OS. In the plots of decision curve analysis, the “assume none” lines represented the assumption that no event occurred; while the “assume all” lines represented the assumption that events occurred in all the patients. CEA, carcinoembryonic antigen; pT, pT stages; NLNC, negative lymph node count; mLNR, modified lymph node ratio; OS, overall survival; AJCC, the American Joint Committee on Cancer.
Internal and external validations
The c-indexes of the nomogram in the training and test cohorts were 0.750 (95% CI, 0.736–0.764) and 0.770 (95% CI, 0.754–0.786), respectively. Similarly, the bias-corrected c-indexes for the training and test cohorts were 0.749 and 0.769, respectively, which indicates no significant changes. Calibration plots displayed a good agreement between the observed and the nomogram-predicted OS at different time points in both the training (Fig. 3B to E) and test cohorts (see Supplementary Fig. S1). The time-dependent AUCs at 12, 24, 36 and 46 months in the training cohort were 0.754 (95% CI, 0.732–0.776), 0.771 (95% CI, 0.755–0.787), 0.781 (95% CI, 0.767–0.795) and 0.771 (95% CI, 0.747–0.796), respectively; the time-dependent AUCs at 12, 24, and 34 months in the test cohort were 0.780 (95% CI, 0.759–0.801), 0.792 (95% CI, 0.776–0.807) and 0.802 (95% CI, 0.777–0.827), respectively. Additional DCA plots (Fig. 3F to I) showed that the nomogram consistently outperformed the AJCC stages, as the nomogram was associated with improved net benefits (higher lines of prediction by the nomogram). However, the nomogram gave comparable threshold probabilities between which a predictive model was clinically valid. The results of the DCA remained stable in the test cohorts (see Supplementary Fig. S2).
Risk classifications and stratifications
After the patients were scored and ranked according to percentiles, risk classifications and stratifications were implemented to illustrate the ability of the nomogram to make risk assessments in the training cohort. In general, the nine AJCC stages were unable to accurately predict the OS of patients with CRC, particularly for those with stage II and stage III disease (Fig. 4A, IIIA vs. I, Plog-rank = 0.766; IIIA vs. IIA, Plog-rank = 0.080; IIIB vs. IIB, Plog-rank = 0.776). Conversely, the nomogram was able to classify patients with stage I-IV disease into nine significant prognostic groups (Fig. 4B, all Plog-rank < 0.016 for pairwise comparisons). Based on the percentile scores of the particular stages, the nomogram could also stratify patients with stage I (Fig. 4C, all Plog-rank < 0.002 for pairwise comparisons), stage II–III (Fig. 4D, all Plog-rank < 0.047 for pairwise comparisons) and stage IV (Fig. 4E, all Plog-rank < 0.001 for pairwise comparisons) disease into a number of significant risk subgroups. Additionally, responses to postoperative radiation therapy (first course therapy) in patients who receive postoperative radiation (n = 325) might also be predicted by the nomogram (Fig. 4F, Plog-rank < 0.001).
Risk assessments using the nomogram.
(A) AJCC stages, (B) nomogram classifications for stage I–IV, (C) nomogram stratifications for stage I, (D) nomogram stratifications for stage II–III with modified sub-stages, (E) nomogram stratifications for stage IV, (F) nomogram stratifications for patients with postoperative radiation (n = 325, median score = 155.9). All log-rank P values for trend and pairwise comparisons were <0.001 unless otherwise specified. Cum OS, cumulative overall survival.
Discussion
In the present study, we evaluated the survival heterogeneity that results from use of the pN stages and proposed a new prognostic nomogram that was able to avoid the limitations associated with the AJCC staging system. The nomogram achieved stable improvements in predictive accuracy, net benefits and reproducibility through the incorporation of the expression of CEA, pT stages, NLNC, mLNR and metastasis without a significant increase in degrees of freedom (df = 9).
As supported by a number of previous studies5,16,17,18,19, there are some reasons that TDs should be considered metastatic lymph nodes irrespective of lymph node status. Most importantly, our study showed that TDs and metastatic lymph nodes had a comparable impact on the survival of patients with CRC and that TDs also imposed risks on node-positive CRC. Consistent with our study, an investigation16 of patients with node-positive CRC reported an increased recurrence rate (49.2% vs. 14.4%, P < 0.001) and decreased OS (P < 0.001) after surgery in those with TDs compared with those without TDs. Other important, supportive reasons include the finding that metastases in the TDs and lymph nodes shared similar recurrence patterns17 and that pathologists experience substantial difficulty in the complete differentiation of these two entities18,19. Actually, our study showed that the mAJCC stages, which were simplified by the combination of TDs and metastatic lymph nodes, achieved a higher log-likelihood and a lower AIC in comparison with conventional AJCC staging. Some studies have also reported that this combination enhanced the diagnostic objectivity19 and predictive accuracy19,20,21 of the pN stages.
Due to the aforementioned limitations, the higher pN stages did not seem to necessarily be associated with shortened survival. The results of the K-M curve analyses revealed that use of the pN stages led to both underestimates (i.e., pN2, LNR ≤ median and pN1, CEA (−)) and overestimates in OS (i.e., pN0, CEA (+) and pN1, CEA (+)) of patients with CRC. We observed that 76.5% (224/293) of the stage IIIA patients and 46.0% (684/1490) of the stage IIIB patients in the training cohort constituted 22.2% and 67.7%, respectively, of the pN1 CEA (−) patients (n = 1010) who were identified to be at risk for underestimation by the pN stages. We also observed that 17.6% (275/1563) of the stage I patients and 34.1% (609/1787) of the stage IIA patients accounted for 24.3% and 53.8%, respectively, of the pN0 CEA (+) patients (n = 1132) whose survival was likely to be overestimated. This explains precisely why some of the stage II patients exhibited a worse survival than stage III patients. In addition, the results indicate that pN1 CEA (−) and pN0 CEA (+) patients may be treated as high-risk stage II patients for whom adjuvant therapies are appropriate, but this requires further validation.
The nomogram successfully avoided the above-mentioned limitations of the pN stages by the inclusion of other node parameters. It was not accidental that the NLNC and mLNR, rather than the mLNC and mPLNC, were prioritized by the multivariate Cox analyses. The mLNR contained additional information about the NLNC, which improved the predictive accuracy of the mPLNC. A recent systematic review confirmed that the prognostic value of the LNR was superior to that of the PLNC22. Moreover, the nomogram allowed the mLNR to be continuously represented. This further avoided the problem of the threshold variability in the LNR, which made studies incomparable and hindered the application of the LNR22. In contrast to the mLNR, the NLNC and LNC were applicable to patients with either early or advanced CRC. Consistent with many other studies3,8,9,23,24, our analyses revealed a positive association among the NLNC, LNC and OS. The mechanisms of this association are increasingly linked to confounders that simultaneously correlate with the LNC and survival of patients with CRC6,7. An emerging role of the adaptive immune response to tumors is also highlighted to characterize the LNC as a patient-specific marker rather than as a quality indicator25. Despite the association, the NLNC showed an advantage over the LNC as a more significant predictor in our study. One reason may be that the favorable effect of the NLNC on OS is more relevant and stable than that of the LNC because the LNC in node-positive patients considers the NLNC and PLNC, while the effect of the LNC may be neutralized since the two components exert opposite effects on prognosis. This is in accord with a recent population-based study, in which the 12-node benchmark proved to be an independent predictor of CRC in patients with stage I-III disease (n = 13,941, HR = 0.67) but not in patients with stage III-IV disease (n = 6810, P = 0.136)24. Another possible reason is that the influence of the LNC on patient survival is more easily diminished by improvements in the quality of external pathology with increasing awareness of the 12-node minimum requirement26. In contrast, the NLNC may be more intrinsically related to enhanced regional lymphocytic reactions that result in an increased NLNC and prolonged survival27. Therefore, the NLNC is a better predictor of survival than the LNC.
Together with previous findings, our study provided one of the first nomograms that incorporates CRC patients with and without metastasis using population-based data. This nomogram is also the first CRC prognostic nomogram that contains a modification of the algorithm for the presence of TDs and the pN stages through the incorporation of both the NLNC and the mLNR. Compared with the published nomograms28 and the AJCC stages for CRC, our nomogram exhibited improved accuracy without a significant increase in model complexity. Nonetheless, our study does have some limitations that deserve attention. Since the analyses were performed retrospectively, selection biases might be underestimated. The duration of the follow-up periods in both cohorts is relatively short because the SEER program did not collect data on TDs until the year 2010. Although we have demonstrated that the performance of the nomogram is reliable and reproducible, this nomogram may still require validation by independent studies with a longer follow-up period. It should also be noted that the SEER research database lacks chemotherapy information albeit the data are irrelevant to the development of the nomogram. Additionally, the inclusion of new biomarkers such as cell-free DNAs29 and circulating tumor cells30 may improve the performance of the nomogram. Lastly, tumor location (i.e., right-sided vs. left-sided location) is associated with site-specific genetic alterations31 that may biologically determine tumor recurrence and outcome32. Thus it may be a simple, reproducible and robust predictor of future modifications of nomograms33 and AJCC stages.
In summary, our study demonstrates substantial survival heterogeneity among the pN stages, which decreases the performance of the AJCC staging system. The quantification of TDs as metastatic lymph nodes is an effective and practical modification that improves predictive accuracy. Based on that modification, the nomogram that incorporates CEA expression, pT stages, the NLNC, the mLNR and metastasis has been internally and externally validated as a useful tool for risk assessments. This nomogram also outperformed the conventional AJCC staging system in both the training and test cohorts with increased predictive accuracy and net benefits but with comparable complexity and clinical validity. Thus, this nomogram holds promise for future application in clinical practice. However, this nomogram still requires independent validations with longer durations of follow-up.
Additional Information
How to cite this article: Zhang, Z.-y. et al. A nomogram improves AJCC stages for colorectal cancers by introducing CEA, modified lymph node ratio and negative lymph node count. Sci. Rep. 6, 39028; doi: 10.1038/srep39028 (2016).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2016. CA Cancer J Clin 66, 7–30 (2016).
Benson, A. B. 3rd et al. Metastatic colon cancer, version 3.2013: featured updates to the NCCN Guidelines. J Natl Compr Canc Netw 11, 141–152; quiz 152 (2013).
Hari, D. M. et al. AJCC Cancer Staging Manual 7th edition criteria for colon cancer: do the complex modifications improve prognostic assessment? J Am Coll Surg 217, 181–190 (2013).
Jin, M. et al. The impact of tumor deposits on colonic adenocarcinoma AJCC TNM staging and outcome. Am J Surg Pathol 39, 109–115 (2015).
Tong, L. L. et al. Is the seventh edition of the UICC/AJCC TNM staging system reasonable for patients with tumor deposits in colorectal cancer? Ann Surg 255, 208–213 (2012).
Willaert, W. et al. Lymphatic spread, nodal count and the extent of lymphadenectomy in cancer of the colon. Cancer Treat Rev 40, 405–413 (2014).
Li Destri, G., Di Carlo, I., Scilletta, R., Scilletta, B. & Puleo, S. Colorectal cancer and lymph nodes: the obsession with the number 12. World J Gastroenterol 20, 1951–1960 (2014).
Johnson, P. M., Porter, G. A., Ricciardi, R. & Baxter, N. N. Increasing negative lymph node count is independently associated with improved long-term survival in stage IIIB and IIIC colon cancer. J Clin Oncol 24, 3570–3575 (2006).
Ogino, S. et al. Negative lymph node count is associated with survival of colorectal cancer patients, independent of tumoral molecular alterations and lymphocytic reaction. Am J Gastroenterol 105, 420–433 (2010).
Sjo, O. H., Merok, M. A., Svindland, A. & Nesbakken, A. Prognostic impact of lymph node harvest and lymph node ratio in patients with colon cancer. Dis Colon Rectum 55, 307–315 (2012).
Compton, C., Fenoglio-Preiser, C. M., Pettigrew, N. & Fielding, L. P. American Joint Committee on Cancer Prognostic Factors Consensus Conference: Colorectal Working Group. Cancer 88, 1739–1757 (2000).
Kuo, T. M. & Mobley, L. R. How generalizable are the SEER registries to the cancer populations of the USA? Cancer Causes Control (2016).
Collins, G. S., Reitsma, J. B., Altman, D. G. & Moons, K. G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. BMJ 350, g7594 (2015).
World Medical, A. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310, 2191–2194 (2013).
Vickers, A. J., Cronin, A. M., Elkin, E. B. & Gonen, M. Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Med Inform Decis Mak 8, 53 (2008).
Yabata, E., Udagawa, M. & Okamoto, H. Effect of tumor deposits on overall survival in colorectal cancer patients with regional lymph node metastases. J Rural Med 9, 20–26 (2014).
Ueno, H. et al. Actual status of distribution and prognostic impact of extramural discontinuous cancer spread in colorectal cancer. J Clin Oncol 29, 2550–2556 (2011).
Rock, J. B. et al. Debating deposits: an interobserver variability study of lymph nodes and pericolonic tumor deposits in colonic adenocarcinoma. Arch Pathol Lab Med 138, 636–642 (2014).
Ueno, H. et al. Multicenter study for optimal categorization of extramural tumor deposits for colorectal cancer staging. Ann Surg 255, 739–746 (2012).
Song, Y. X. et al. Can the tumor deposits be counted as metastatic lymph nodes in the UICC TNM staging system for colorectal cancer? PLoS One 7, e34087 (2012).
Nagtegaal, I. D. et al. Lymph nodes, tumor deposits, and TNM: are we getting better? J Clin Oncol 29, 2487–2492 (2011).
Ceelen, W., Van Nieuwenhove, Y. & Pattyn, P. Prognostic value of the lymph node ratio in stage III colorectal cancer: a systematic review. Ann Surg Oncol 17, 2847–2855 (2010).
Lykke, J., Roikjaer, O., Jess, P. & Danish Colorectal Cancer, G. The relation between lymph node status and survival in Stage I-III colon cancer: results from a prospective nationwide cohort study. Colorectal Dis 15, 559–565 (2013).
Ahmadi, O., Stringer, M. D., Black, M. A. & McCall, J. L. Clinico-pathological factors influencing lymph node yield in colorectal cancer and impact on survival: analysis of New Zealand Cancer Registry data. J Surg Oncol 111, 451–458 (2015).
Markl, B. Stage migration vs immunology: The lymph node count story in colon cancer. World J Gastroenterol 21, 12218–12233 (2015).
Bläker, H. et al. Lymph node count and prognosis in colorectal cancer: the influence of examination quality. Int J Cancer 136, 1957–1966 (2015).
Ogino, S. et al. Lymphocytic reaction to colorectal cancer is associated with longer survival, independent of lymph node count, microsatellite instability, and CpG island methylator phenotype. Clin Cancer Res 15, 6412–6420 (2009).
Kawai, K. et al. Nomograms for colorectal cancer: A systematic review. World J Gastroenterol 21, 11877–11886 (2015).
Basnet, S. et al. The Prognostic Value of Circulating Cell-Free DNA in Colorectal Cancer: A Meta-Analysis. J Cancer 7, 1105–1113 (2016).
Wong, C. S. et al. Isolated tumor cells and circulating CK20 mRNA in pN0 colorectal cancer patients. Int J Surg Pathol 16, 119–126 (2008).
Loupakis, F. et al. Clinico-pathological nomogram for predicting BRAF mutational status of metastatic colorectal cancer. Br J Cancer 114, 30–36 (2016).
Pugh, S. A. et al. Site and Stage of Colorectal Cancer Influence the Likelihood and Distribution of Disease Recurrence and Postrecurrence Survival: Data From the FACS Randomized Controlled Trial. Ann Surg 263, 1143–1147 (2016).
Zhang, Z. Y. et al. Nomograms to predict survival after colorectal cancer resection without preoperative therapy. BMC Cancer 16, 658 (2016).
Acknowledgements
We would like to thank Dr. Cathy Chen for her suggestions about manuscript editing. This study was supported by grants from the Shanghai Science Committee Foundation (no. 34119b0600; no. 16411970800), Shanghai Municipal Health Bureau (no. 20134194), Jiaxing Science Committee Foundation of Zhejiang Province (no. 2015AY23071) and Zhejiang Technology Project of Medicine and Health (no. 2016KYB295).
Author information
Authors and Affiliations
Contributions
Study conception and design: H.Y.G.; acquisition of data: Z.Y.Z., W.G., Q.F.L., X.W.Y., S.B., Z.L.D., H.Y.G.; analysis and interpretation of data: Z.Y.Z., W.G., Q.F.L., X.W.Y., S.B., Z.L.D., H.Y.G.; all authors have drafted and approved the final version of the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhang, Zy., Gao, W., Luo, Qf. et al. A nomogram improves AJCC stages for colorectal cancers by introducing CEA, modified lymph node ratio and negative lymph node count. Sci Rep 6, 39028 (2016). https://doi.org/10.1038/srep39028
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep39028
This article is cited by
-
Prediction models of colorectal cancer prognosis incorporating perioperative longitudinal serum tumor markers: a retrospective longitudinal cohort study
BMC Medicine (2023)
-
Risk factors for long-term survival in patients with ypN+ M0 rectal cancer after radical anterior resection
BMC Gastroenterology (2022)
-
Nomograms for predicting the overall and cause-specific survival in patients with malignant peripheral nerve sheath tumor: a population-based study
Journal of Neuro-Oncology (2019)
-
Carcinoembryonic antigen reduction after medical treatment in patients with metastatic colorectal cancer: a systematic review and meta-analysis
International Journal of Colorectal Disease (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.