Abstract
We describe the impact of an antiretroviral therapy program on human resource utilization and service delivery in a rural hospital in Monze, Zambia, using qualitative data. We assess project impact on staff capacity utilization, service delivery, and community perception of care. Increased workload resulted in fatigue, low staff morale, and exacerbated critical manpower shortages, but also an increase in users of antiretroviral therapy, improvement in hospital infrastructure and funding, and an overall community satisfaction with service delivery. Integrating HAART programs within existing hospital units and services may be a good alternative to increase overall efficiency. Commentary JPHP.2011.8, available at www.palgrave-journals.com/jphp/, relates to this article.
Similar content being viewed by others
References
UNAIDS. (2008) Report on the Global AIDS Epidemic, http://www.unaids.org/en/KnowledgeCentre/HIVData/GlobalReport/2008/2008_Global_report.asp.
Ministry of Health/National AIDS Council. (2007) Zambia Country Report – National Monitoring and Evaluation Report to the United Nations General Assembly, 2006–2007. Lusaka, Zambia, http://data.unaids.org/pub/Report/2008/zambia_2008_country_progress_report_en.pdf.
Lewis, S. (2005) Zambia: A constellation of change and commitment in response to AIDS, http://www.africafiles.org/article.asp?ID=7971&ThisURL=./aids.asp&URLName=AIDS.
Van Damme, W., Kober, K. and Kegels, G. (2008) Scaling-up antiretroviral treatment in Southern African countries with human resource shortage. How will health systems adapt? Social Science & Medicine 66 (10): 2108–2121.
Coovadia, H.M. and Hadigham, J. (2005) HIV/AIDS: Global trends, global funds and delivery bottlenecks. Globalization and Health 1 (13), http://www.globalizationandhealth.com/content/1/1/13.
McCoy, D. et al (2004) Expanding access to antiretroviral therapy in Sub-Saharan Africa: Avoiding the pitfalls and dangers, capitalizing on the opportunities. American Journal of Public Health 9 (1): 18–22.
Mills, A. (1983) Vertical versus horizontal programs in Africa: Idealism, pragmatism, resources and efficiency. Social Science & Medicine 26: 1971–1981.
Rifkin, S. and Walt, G. (1986) Why health improves: Defining the issues concerning ‘comprehensive primary health care’ and ‘selective primary health care’. Social Science & Medicine 23: 559–566.
Smith, D.L. and Bryant, J.H. (1988) Building the infrastructure for primary health care: An overview of vertical and integrated approaches. Social Science & Medicine 6: 909–917.
Atun, R.A., Bennett, S. and Duran, A. (2008) When do vertical (stand-alone) programs have a place in health systems? Health Systems and Policy Analysis Policy Brief. World Health Organisation, Regional Office for Europe, Copenhagen, Denmark.
Gonzalez, C.L. (1965) Mass campaigns and general health services. Geneva: World Health Organization. Public Health Papers, no. 29.
Oliveira-Cruz, V., Kurowski, C. and Mills, A. (2003) Delivery of priority health services: Searching for synergies within the vertical versus horizontal debate. Journal of International Development 15: 67–86.
Mills, A. (2005) Mass campaigns versus general health services: What have we learnt in 40 years about vertical versus horizontal approaches? Bulletin of the World Health Organization 83 (4): 315–316.
Msuya, J. (2005) Horizontal and Vertical Delivery of Health Services: What are the Tradeoffs? Washington, DC: World Bank.
Kara, H., Ranson, M.K., Oliveira-Cruz, V. and Mills, A. (2003) Expanding access to priority health interventions: A framework for understanding the constraints to scaling-up. Journal of International Development 15 (1): 1–14.
Central Office of Statistics. (2003) Zambia 2000 Census of Population and Housing. Lusaka, Zambia: Central Office of Statistics.
Ministry of Health. (2006) Health Sector Joint Annual Review Report. Lusaka, Zambia: Government of the Republic of Zambia.
Maykut, P. and Morehouse, R. (1994) Beginning Qualitative Research: A Philosophic and Practical Guide. London: Falmer Press.
Pope, C. and Mays, N. (eds.) (2006) Qualitative Research in Health Care, 3rd edn. Oxford, England: Blackwell Publishing.
Green, J. and Thorogood, N. (2004) Qualitative Methods for Health Research. London: Sage.
Gray, D.E. (2009) Doing Research in the Real World, 2nd edn. London: Sage.
Stringer, J.S.A. et al (2006) Rapid scale-up of antiretroviral therapy at primary care sites in Zambia: Feasibility and early outcomes. Journal of American Medical Association 296 (7): 782–793.
Castro, A. and Farmer, P. (2005) Understanding and addressing AIDS-related stigma: From anthropological theory to clinical practice in Haiti. American Journal of Public Health 95: 53–59.
Weiser, S. et al (2003) Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Bostwana. Journal of Acquired Immune Deficiency Syndrome 34: 281–288.
Nachega, J.B. et al (2004) Adherence to antiretroviral therapy in HIV-infected adults in Soweto, South Africa. AIDS Research and Human Retroviruses 20 (10): 1053–1056.
Farmer, P. et al (2001) Community based approaches to HIV treatment in resource-poor settings. The Lancet 358 (9279): 404–409.
Dräger, S., Gedik, G. and Dal Poz, M.R. (2006) Health workforce issues and the Global Fund to fight AIDS, Tuberculosis and Malaria: An analytical review. Human Resources for Health 4 (23): 1–12.
Hirshhorn, L.R., Oguda, L., Fullem, A., Dreesch, N. and Wilson, P. (2006) Estimating health workforce needs for antiretroviral therapy in resource-limited settings. Human Resources for Health 4 (1): 1–16.
Hongoro, C. and McPake, B. (2004) How to bridge the gap in human resources for health. The Lancet 364 (9443): 1451–1456.
Joint Learning Initiative. (2004) Human Resources for Health and Development: Overcoming the Crisis. Boston: Harvard University Press.
Narasimhan, V. et al (2004) Responding to the global human resources crisis. The Lancet 363 (9419): 1469–1472.
Torpey, K.E. et al (2008) Adherence support workers: A way to address human resource constraints in antiretroviral treatment programs in the public health setting in Zambia. PlosOne 3 (5): e2204. doi:10.1371/journal.pone.0002204.
Victoria, C., Hanson, G., Bryce, K. and Vaughan, P.J. (2004) Achieving universal coverage with health interventions. The Lancet 364 (9444): 1541–1548.
Kober, K. and Van Damme, W. (2004) Scaling up access to antiretroviral treatment in southern Africa: Who will do the job? The Lancet 364: 103–107.
Van Damme, W. and Kegles, G. (2004) Health system strengthening and scaling up antiretroviral therapy: The need for context specific delivery models: Comment on Schneider, et al. Reproductive Health Matters 14 (27): 24–26.
Coetzee, D., Boulle, A., Hildebrand, K., Asselman, V., Van Cutsem, G. and Goemaere, E. (2004) Promoting adherence to antiretroviral therapy: The experience from a primary care setting in Khayelitsha, South Africa. AIDS 18 (3): S27–S31.
World Health Organization. (2003) Treating 3 Million By 2005: Making it Happen. The WHO Strategy. Switzerland, Geneva: World Health Organization.
Schneider, H., Blaauw, D., Gilson, L., Chabikuli, N. and Goudge, J. (2004) Health Systems Strengthening and ART Scaling-Up: Challenges and Opportunities. Centre for Health Policy, School of Public Health, University of Witwatersrand, Johannesburg, December.
Physicians for Human Rights. (2005) Statement for Group of 8 meeting in July 2005: Health Workforces Must Be Supported to Achieve the Millennium Development Goals, http://www.healthgap.org/press_releases/05/0705_PHR_INTL_LTR_G8_HCW.pdf.
Yu, D., Souteyrand, Y., Banda, M.A., Kaufman, J. and Perriens, J.H. (2008) Investment in HIV/AIDS programs: Does it help strengthen health systems in developing countries? Globalization and Health 4: 8, doi:10.1186/1744-8603-4-8.
El-Sadr, W.M. and Hoos D . (2008) The president's emergency plan for AIDS relief – Is the emergency over? New England Journal of Medicine 359 (6): 553–555.
Acknowledgements
We are grateful to the District Health Authority, the Board of Monze Mission General Hospital, and the study participants for facilitating and the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
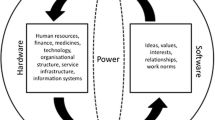
A study of an antiretroviral therapy (ART) program implemented with a stand-alone strategy in a Zambian rural general hospital illustrates some advantages and disadvantages of separating HIV/AIDS care from other services.
Rights and permissions
About this article
Cite this article
Adedimeji, A., Malokota, O. & Manafa, O. Implementing antiretroviral therapy programs in resource-constrained settings: Lessons from Monze, Zambia. J Public Health Pol 32, 198–210 (2011). https://doi.org/10.1057/jphp.2011.4
Published:
Issue Date:
DOI: https://doi.org/10.1057/jphp.2011.4