-
PDF
- Split View
-
Views
-
Cite
Cite
S. Persson, I. Rouvelas, T. Irino, L. Lundell, Outcomes following the main treatment options in patients with a leaking esophagus: a systematic literature review, Diseases of the Esophagus, Volume 30, Issue 12, December 2017, Pages 1–10, https://doi.org/10.1093/dote/dox108
Close - Share Icon Share
Summary
Leakage from the esophagus and gastroesophageal junction can be lethal due to uncontrolled contamination of the mediastinum. The most predominant risk factors for the subsequent clinical outcome are the patients’ delay as well as the delay of diagnosis. Two major therapeutic concepts have been advocated: either prompt closure of the leakage by insertion of a self-expandable metal stent (SEMS) or more traditionally, surgical exploration. The objective of this review is to carefully scrutinize the recent literature and assess the outcomes of these two therapeutic alternatives in the management of iatrogenic perforation—spontaneous esophageal rupture as separated from those with anastomotic leak. A systematic web-based search using PubMed and the Cochrane Library was performed, reviewing literature published between January 2005 and December 2015. Eligible studies included all studies that presented data on the outcome of SEMS or surgical exploration in case of esophageal leak (including >3 patients). Only patients older than 15 years of age by the time of admission were included. Articles in other languages but English were excluded. Treatment failure was defined as a need for change in therapeutic strategy due to uncontrolled sepsis and mediastinitis, which usually meant rescue esophagectomy with end esophagostomy, death occurring as a consequence of the leakage or development of an esophagorespiratory fistula and/or other serious life threatening complications. Accordingly, the corresponding success rate is composed of cases where none of the failures above occurred. Regarding SEMS treatment, 201 articles were found, of which 48 were deemed relevant and of these, 17 articles were further analyzed. As for surgical management, 785 articles were retrieved, of which 82 were considered relevant, and 17 were included in the final analysis. It was not possible to specifically extract detailed clinical outcomes in sufficient numbers, when we tried to separately analyze the data in relation to the cause of the leakage: i.e. iatrogenic perforation—spontaneous esophageal rupture and anastomotic leak. As for SEMS treatment, originally 154 reports focused on iatrogenic perforation, 116 focused on spontaneous ruptures, and only four described the outcome following trauma and foreign body management. Only five studies used a prospective protocol to assess treatment efficacy. Regarding a leaking anastomosis, 80 reports contained information about the outcome after treatment of esophagogastrostomies and 35 reported the clinical course after an esophagojejunostomy. An overall success rate of 88% was reported among the 371 SEMS-treated patients, where adequate data were available, with a reported in hospital mortality amounting to 7.5%. Regarding the surgical exploration strategy, the vast majority of patients had an attempt to repair the defect by direct or enforced suturing. This surgical approach also included procedures such as patching with pleura or with a diaphragmatic flap. The overall reported success rate was 83% (305/368) and the in-hospital mortality was 17% (61/368). The current literature suggests that a SEMS-based therapy can be successfully applied as an alternative therapeutic strategy in esophageal perforation rupture.
INTRODUCTION
Leakage from the esophagus and gastroesophageal junction (GEJ) exposes the patients to lethal threats due to uncontrolled contamination of the mediastinum by gastrointestinal juice, which induces and perpetuates mediastinitis.1,2 It is obvious that this demanding clinical situation can be caused by a variety of different conditions, interventions, and mechanisms, where the most frequent one is complications to therapeutic interventions such as during endoscopy and dilatations.3 In these situations, immediate detection and measures taken to seal the leakage are of vital importance to prevent further damage and to control the ensuing clinical course. The most predominant risk factors for the subsequent outcome are the patients’ delay as well as the delay caused by imprecise diagnostic interventions or even the absence of diagnostic interventions.3–6 The same risk factors are operational in cases with spontaneous rupture of the distal esophagus, where the damage affects an otherwise normal and well-functioning organ. The therapeutic actions advocated in these situations depend on the severity of presenting symptoms and the patient's general condition but also on individual preferences of the physician in charge. In essence, two major therapeutic concepts have been advocated: either to promptly seal the leakage with the insertion of a self-expandable metal stent (SEMS) or more traditionally to undertake a surgical exploration with the dual ambition of cleaning the mediastinum-pleural cavity and covering the defect if possible, or alternatively to resect the damaged-diseased esophagus. Both of these fundamentally different therapeutic strategies harbor the ambition to control the pleural contamination, which by necessity has to incorporate the frequent insertion of drains through the thoracic wall, including when the SEMS-based strategy is followed.
The other and conceptually different situation with a leaking esophagus is represented by a contaminated mediastinum originating from a defect in an esophagogastric or esophagojejunal anastomosis. These situations also entail high postoperative morbidity, mortality, and impaired quality of life at long-term follow-up.7–12 However, the anatomical and physiological preconditions differ between these two clinical situations, given that the anastomotic dehiscence situation harbors special anatomical preconditions complicating the prerequisites for a well-functioning SEMS to control the leakage. In addition, the ongoing posttraumatic response after the elective major surgical intervention may have important consequences for the response to treatment as well as for the subsequent clinical outcomes. Accordingly, there are a number of factors that have to be taken into account when comprehensively assessing the pros and cons of the SEMS- versus surgical exploration-based therapeutic strategies in cases with a leaking esophagus. In addition to these given preconditions, it can also be concluded that the available literature is imprecise and does not offer robust background information for a critical and comprehensive analysis about the benefits and limitations of the various therapeutic alternatives and the risk factors that may be determinant for the respective outcomes. Only exceptionally a standardized assessment of the magnitude of the leakage has been utilized.13
The leakage rates after esophagectomy and total gastrectomy vary between 3% and 25%14–17 and from 3% to 11%,9,11,18,19 respectively. The existing literature, which often comprises only small single institutional series, is also hampered by a multiplicity of confounders. Moreover, irrespective of the therapeutic strategy under scrutiny, the definition of success is either ill-defined or barely specified. Despite these limitations, the experiences of e.g. SEMS therapy, with few exceptions,6,20 report a ‘success rate’ ranging from 50% to 80%.21–24 Added to the significant variation in the reported success rates after both stent treatment and up-front surgical exploration is the diversity in clinical presentations at the time of clinical decision making.
Facing these difficulties, the objective of this study is to carefully review the recent literature trying to assess the outcomes of these two therapeutic alternatives in the management of iatrogenic perforation—spontaneous esophageal rupture as separated from those with leaking esophageal anastomoses. Since the development of care and rehabilitation of patients with mediastinitis, due to leaking esophagus, has developed and improved quite significantly during the last decades we have limited our literature search to the past 10 years.
METHODS
Eligibility criteria
Eligible studies included all clinical studies that presented data on the outcome of SEMS or surgical exploration in case of a leaking esophagus (containing >3 patients each). Only patients who, at the time of admission, were older than 15 years of age were included. Articles for which the full text was not available in English were excluded.
Information sources, search, and study selection
The present review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. A systematic web-based search using PubMed and the Cochrane Library was performed, reviewing medical literature published between January 2005 and December 2015. The last electronic search was carried out on the 2nd of January 2015. The search was performed with a combination of the following Medical Subject Headings (MeSH): esophagus, stents, esophageal perforation, and anastomotic leak and the following keywords: esophagus, stent, perforation and leakage. The following combinations were used: ‘Esophageal Perforation’[Mesh], (‘Esophagus’[Mesh]) AND ‘Anastomotic Leak’[Mesh], ‘Esophagus’[Mesh]) AND ‘Stents’[Mesh]) AND ‘Esophageal Perforation’[Mesh], ‘Esophagus’[Mesh]) AND ‘Stents’[Mesh]) AND ‘Anastomotic Leak’[Mesh], ‘Esophagus’ [Mesh] AND Stent [Mesh] AND ‘Perforation OR Leakage’ [Mesh].
Anastomotic leak included esophagectomy, total gastrectomy, proximal gastrectomy, and esophagogastrectomy. Gastrojejunal or esophagocolonic leakages were not included in this study.
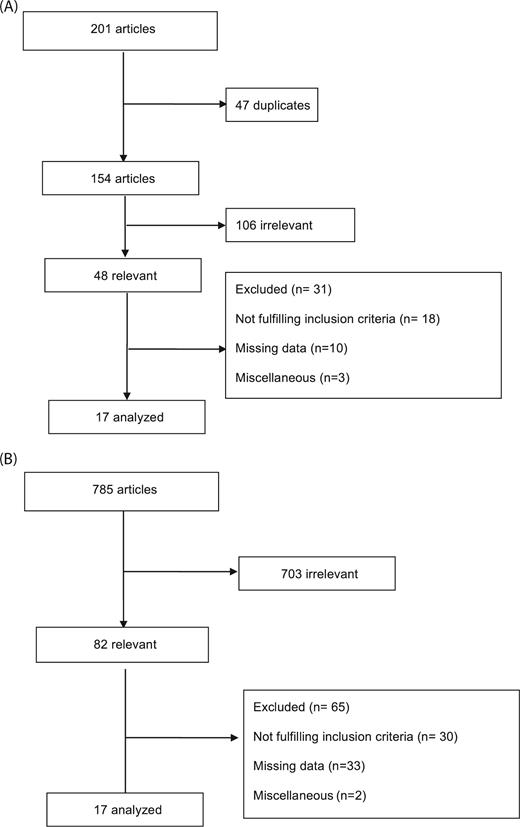
The search identified a total of 785 articles on surgical management of esophageal leakages, out of which only 82 were considered relevant. Regarding SEMS treatment, 201 articles were identified through the search, out of which 48 were deemed relevant. A manual search of the reference lists from the reviewed articles was performed to identify additional relevant publications. Results of the search are shown in Figure 1A, B. Among the articles screened, 34 were selected and included in the final analysis. Owing to the heterogeneity of the patient populations and the wide variations in the definition of a satisfactory functional outcome, only qualitative analyses of the data were considered relevant. Only descriptive statistical analysis was used.
(A) Flow chart illustrating the screening and selection of papers for review regarding the outcome of SEMS treatment of leaking esophagus.6,21,25–39 B) Flow chart illustrating the screening and selection of papers for review of the outcome of surgical exploration and treatment of leaking esophagus.40–56
Definition of treatment failure—success rate
Treatment failure was defined as a need for change in therapeutic strategy due to uncontrolled sepsis and mediastinitis, which usually meant rescue esophagectomy with end esophagostomy, death occurring as a consequence of the leakage or development of an esophagorespiratory fistula and/or other serious life threatening complications. A persistent leakage after stenting, where the leakage and infection could be managed successfully with additional drainage procedures and SEMS reinsertion and antibiotics, was accordingly not considered a treatment failure. The corresponding success rate was accordingly when none of the above was prevailing.
Exclusion criteria
The following conditions were excluded: spontaneous rupture of a previously diagnosed advanced malignant tumor of the esophagus and GE junction. Anastomotic leakage from a gastric bypass operation or sleeve gastrectomy was not included, neither was leakage after a colonic interposition or leakage from a gastrojejunal anastomosis. Moreover, studies with incomplete data on management and follow up regarding in-hospital outcomes were excluded.
Due to the scope of the current review, we had to exclude some patients from the included eligible studies, which did not meet our inclusion criteria, i.e. malignant perforations and leakage from a gastroenteroanastomosis.
RESULTS
As seen in Figure 1A, B, comparatively few studies fulfilled the inclusion criteria for the final analyses concerning both therapeutic strategies under scrutiny. The vast majority of the final included eligible studies were of questionable quality, retrospective single institution series, and consequently hampered by selection and/or information bias.
As for SEMS treatment, originally 154 reports focused on iatrogenic perforation (Table 1), 116 on spontaneous ruptures and four described the outcome following trauma and foreign body management. Only five studies used a prospective protocol over a defined time period, to assess treatment efficacy. Regarding a leaking anastomosis, 80 reports contained information about the outcome after treatment of esophagogastrostomies and 35 reported the clinical course after an esophagojejunostomy. However, only 17 studies were considered relevant and attaining the quality for the final analyses due to the reasons specified in the figure. The numbers of stent migrations were reported in only a few of these reports and it was often unclear how the stent management strategy was pursued, e.g. regarding the necessity to reendoscope the patients and the attitude toward reinsertion of a new stent in case of incomplete sealing of the leakage. It was not possible to specifically extract (in sufficient numbers) detailed clinical outcomes when we tried to separately analyze the data depending on the cause of the leakage i.e. iatrogenic perforation—spontaneous esophageal rupture and the leaking esophageal anastomoses. However, in total a success rate of 88% was reported among the 371 SEMS treated patients, where adequate data were available, with a reported in-hospital mortality amounting to 7.5%.
Eligible studies regarding stent treatment
| Author/ . | Persson/ . | Salminen/ . | Safranek/ . | Radecke/ . | Kroepil/ . | Gubler/ . | Freeman/ . | Freeman/ . | El Hajj/ . | Dai/2011 . | Al-Issa/ . | Zhou/2009 . | Ben-David/ . | Eizaguirre/ . | Tuebergen/ . | Schweigert/ . | Hoeppner/ . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year . | 2014 . | 2009 . | 2014 . | 2006 . | 2013 . | 2014 . | 2007 . | 2009 . | 2014 . | 2011 . | 2014 . | 2009 . | 2014 . | 2016 . | 2008 . | 2013 . | 2014 . |
| Country . | Sweden . | Finland . | Czech Republic . | Germany . | Germany . | Switzerland . | USA . | USA . | USA . | Germany . | Denmark . | China . | USA . | Spain . | Germany . | Germany, UK . | Germany . |
| Study design | Prospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Prospective single center | Prospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Prospective single center | Retrospective multi center | Prospective single center |
| Number of patients receiving stent therapy for leakage† | 40 | 4 | 13 | 4 | 3 | 47 | 17 | 19 | 10 | 32 | 15 | 8 | 68 | 13 | 30 | 13 | 35 |
| Aim of the study | To investigate possible predictors for failed stent therapy in patients with benign esophageal perforation | To evaluate the role of stent therapy for the management of esophageal perforations and anastomotic leaks | To evaluate use of stents for treatment of patients suffering from mediastinitis due to esophageal perforation | Report experience of stent in treatment of nonmalignant esophageal leaks | To review management of patients with esophageal perforation and to create algorithm in the management. | To report experience with stent treatment for benign esophageal leakages | Summarize treatment of iatrogenic perforations with stent | Summarize treatment of spontaneous perforations with stent | Evaluate safety and efficacy of stent treatment in patients with esophageal leaks, fistulae and perforations | Assess efficacy of stent treatment in esophageal leaks | Assess outcome of stent treatment for anastomotic leak after esophagectomy | Review treatment with stent in patients with delayed (> 24 h) intrathoracic esophageal perforation | To establish therapeutic efficacy of minimally invasive therapies in a consecutive series of patients with esophageal perforation | Evaluate results from stent treatment in patients with esophageal intrathoracic and cervical leaks | To evaluate the effects of endoluminal stent treatment in patients with esophageal anastomotic leakages of perforations. | Compare results of primary surgical therapy with endoscopic stenting in patients with spontaneous rupture of the esophagus | Evaluate outcome and clinical effectiveness of CSES in esophageal anastomotic leakage |
| Cause of leakage | |||||||||||||||||
| Iatrogenic | 16 | 2 | 7 | 32 | 17 | 8 | 2 | 7 | 59 | 4 | |||||||
| Spontaneous | 23 | 2 | 2 | 15 | 19 | 2 | 1 | 1 | 9 | 4 | 38 | ||||||
| Trauma | 1 | 1 | |||||||||||||||
| Esophagogastrostomy | 1 | 21 | 15 | 13 | 19 | 11 | |||||||||||
| Esophagojejunostomy | 8 | 3 | 24 | ||||||||||||||
| Foreign body | 2 | ||||||||||||||||
| Success rate stent treatment† (%) | 83 | 50 | 69 | 100 | 67 | 87 | 94 | 89 | 90 | 94 | 87 | 100 | 100 | 92 | 87 | 85 | 71 |
| Success† | 33 | 2 | 9 | 4 | 2 | 41 | 16 | 17 | 9 | 30 | 13 | 8 | 68 | 12 | 26 | 11 | 25 |
| Mortality in stent group | 3 | 2 | 4 | 0 | 1 | 0 | 0 | 0 | 1 | 2 | 1 | 0 | 0 | 1 | 2 | 2 | 9 |
| Conclusion | Stent treatment seems to be a successful concept when applied to an unselected group of benign esophageal perforations. Delayed treatment indicated risk for failed stent therapy. | Traumatic perforations and anastomotic leaks can be treated effectively with stent with adequate drainage even in cases of severely ill patients. | Stent therapy neither increased survival nor decreased length of therapy once mediastinitis had developed. Main advantage is the preservation of native esophagus and reduced extent of surgical mediastinal drainage. | Stents represent a safe method for sealing benign esophageal leaks and should be discussed as first-line therapy in contained perforations without severe mediastinitis of the mid esophagus. | A small subset of patients can be treated conservatively by stenting. In the majority of patients a primary repair can be performed with good prognosis. | Temporary stent placement for benign leakages of the esophagus is safe and seems to improve treatment success. | Stent placement is effective treatment of acute iatrogenic esophageal perforations and may reduce hospital length stay and avoid potential morbidities of operative repair. | Stent placement is effective treatment of most spontaneous esophageal perforations and may reduce hospital length stay and avoid potential morbidities of operative repair. | Stents are safe and effective in treating esophageal leaks, fistulas and perforations. Defect opening size and time from diagnosis to stent placement appear to be candidate predictors for successful closure. | Stenting is a viable option in combination with interventional or surgical drainage | Stents are an effective and safe option in management of post esophagectomy leaks | Esophageal stenting is effective in the management of delayed intrathoracic esophageal perforation | Endoscopically placed removable esophageal stents with minimally invasive repair of the perforation and feeding access is an effective treatment method for patients with esophageal perforation. | Stent treatment can prevent reoperation but does not decrease average hospital stay | Implantation of self-expanding stents after esophageal resection or perforation is a feasible and safe procedure with an acceptable morbidity even if used as last-choice treatment | Authors recommend surgical intervention as primary treatment in patients with spontaneous esophageal rupture | Stents are an effective treatment for leakages in patients with esophagogastrostomies and esophagejejunostomies |
| Author/ . | Persson/ . | Salminen/ . | Safranek/ . | Radecke/ . | Kroepil/ . | Gubler/ . | Freeman/ . | Freeman/ . | El Hajj/ . | Dai/2011 . | Al-Issa/ . | Zhou/2009 . | Ben-David/ . | Eizaguirre/ . | Tuebergen/ . | Schweigert/ . | Hoeppner/ . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year . | 2014 . | 2009 . | 2014 . | 2006 . | 2013 . | 2014 . | 2007 . | 2009 . | 2014 . | 2011 . | 2014 . | 2009 . | 2014 . | 2016 . | 2008 . | 2013 . | 2014 . |
| Country . | Sweden . | Finland . | Czech Republic . | Germany . | Germany . | Switzerland . | USA . | USA . | USA . | Germany . | Denmark . | China . | USA . | Spain . | Germany . | Germany, UK . | Germany . |
| Study design | Prospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Prospective single center | Prospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Prospective single center | Retrospective multi center | Prospective single center |
| Number of patients receiving stent therapy for leakage† | 40 | 4 | 13 | 4 | 3 | 47 | 17 | 19 | 10 | 32 | 15 | 8 | 68 | 13 | 30 | 13 | 35 |
| Aim of the study | To investigate possible predictors for failed stent therapy in patients with benign esophageal perforation | To evaluate the role of stent therapy for the management of esophageal perforations and anastomotic leaks | To evaluate use of stents for treatment of patients suffering from mediastinitis due to esophageal perforation | Report experience of stent in treatment of nonmalignant esophageal leaks | To review management of patients with esophageal perforation and to create algorithm in the management. | To report experience with stent treatment for benign esophageal leakages | Summarize treatment of iatrogenic perforations with stent | Summarize treatment of spontaneous perforations with stent | Evaluate safety and efficacy of stent treatment in patients with esophageal leaks, fistulae and perforations | Assess efficacy of stent treatment in esophageal leaks | Assess outcome of stent treatment for anastomotic leak after esophagectomy | Review treatment with stent in patients with delayed (> 24 h) intrathoracic esophageal perforation | To establish therapeutic efficacy of minimally invasive therapies in a consecutive series of patients with esophageal perforation | Evaluate results from stent treatment in patients with esophageal intrathoracic and cervical leaks | To evaluate the effects of endoluminal stent treatment in patients with esophageal anastomotic leakages of perforations. | Compare results of primary surgical therapy with endoscopic stenting in patients with spontaneous rupture of the esophagus | Evaluate outcome and clinical effectiveness of CSES in esophageal anastomotic leakage |
| Cause of leakage | |||||||||||||||||
| Iatrogenic | 16 | 2 | 7 | 32 | 17 | 8 | 2 | 7 | 59 | 4 | |||||||
| Spontaneous | 23 | 2 | 2 | 15 | 19 | 2 | 1 | 1 | 9 | 4 | 38 | ||||||
| Trauma | 1 | 1 | |||||||||||||||
| Esophagogastrostomy | 1 | 21 | 15 | 13 | 19 | 11 | |||||||||||
| Esophagojejunostomy | 8 | 3 | 24 | ||||||||||||||
| Foreign body | 2 | ||||||||||||||||
| Success rate stent treatment† (%) | 83 | 50 | 69 | 100 | 67 | 87 | 94 | 89 | 90 | 94 | 87 | 100 | 100 | 92 | 87 | 85 | 71 |
| Success† | 33 | 2 | 9 | 4 | 2 | 41 | 16 | 17 | 9 | 30 | 13 | 8 | 68 | 12 | 26 | 11 | 25 |
| Mortality in stent group | 3 | 2 | 4 | 0 | 1 | 0 | 0 | 0 | 1 | 2 | 1 | 0 | 0 | 1 | 2 | 2 | 9 |
| Conclusion | Stent treatment seems to be a successful concept when applied to an unselected group of benign esophageal perforations. Delayed treatment indicated risk for failed stent therapy. | Traumatic perforations and anastomotic leaks can be treated effectively with stent with adequate drainage even in cases of severely ill patients. | Stent therapy neither increased survival nor decreased length of therapy once mediastinitis had developed. Main advantage is the preservation of native esophagus and reduced extent of surgical mediastinal drainage. | Stents represent a safe method for sealing benign esophageal leaks and should be discussed as first-line therapy in contained perforations without severe mediastinitis of the mid esophagus. | A small subset of patients can be treated conservatively by stenting. In the majority of patients a primary repair can be performed with good prognosis. | Temporary stent placement for benign leakages of the esophagus is safe and seems to improve treatment success. | Stent placement is effective treatment of acute iatrogenic esophageal perforations and may reduce hospital length stay and avoid potential morbidities of operative repair. | Stent placement is effective treatment of most spontaneous esophageal perforations and may reduce hospital length stay and avoid potential morbidities of operative repair. | Stents are safe and effective in treating esophageal leaks, fistulas and perforations. Defect opening size and time from diagnosis to stent placement appear to be candidate predictors for successful closure. | Stenting is a viable option in combination with interventional or surgical drainage | Stents are an effective and safe option in management of post esophagectomy leaks | Esophageal stenting is effective in the management of delayed intrathoracic esophageal perforation | Endoscopically placed removable esophageal stents with minimally invasive repair of the perforation and feeding access is an effective treatment method for patients with esophageal perforation. | Stent treatment can prevent reoperation but does not decrease average hospital stay | Implantation of self-expanding stents after esophageal resection or perforation is a feasible and safe procedure with an acceptable morbidity even if used as last-choice treatment | Authors recommend surgical intervention as primary treatment in patients with spontaneous esophageal rupture | Stents are an effective treatment for leakages in patients with esophagogastrostomies and esophagejejunostomies |
†According to the specific study's defined criteria.
Eligible studies regarding stent treatment
| Author/ . | Persson/ . | Salminen/ . | Safranek/ . | Radecke/ . | Kroepil/ . | Gubler/ . | Freeman/ . | Freeman/ . | El Hajj/ . | Dai/2011 . | Al-Issa/ . | Zhou/2009 . | Ben-David/ . | Eizaguirre/ . | Tuebergen/ . | Schweigert/ . | Hoeppner/ . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year . | 2014 . | 2009 . | 2014 . | 2006 . | 2013 . | 2014 . | 2007 . | 2009 . | 2014 . | 2011 . | 2014 . | 2009 . | 2014 . | 2016 . | 2008 . | 2013 . | 2014 . |
| Country . | Sweden . | Finland . | Czech Republic . | Germany . | Germany . | Switzerland . | USA . | USA . | USA . | Germany . | Denmark . | China . | USA . | Spain . | Germany . | Germany, UK . | Germany . |
| Study design | Prospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Prospective single center | Prospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Prospective single center | Retrospective multi center | Prospective single center |
| Number of patients receiving stent therapy for leakage† | 40 | 4 | 13 | 4 | 3 | 47 | 17 | 19 | 10 | 32 | 15 | 8 | 68 | 13 | 30 | 13 | 35 |
| Aim of the study | To investigate possible predictors for failed stent therapy in patients with benign esophageal perforation | To evaluate the role of stent therapy for the management of esophageal perforations and anastomotic leaks | To evaluate use of stents for treatment of patients suffering from mediastinitis due to esophageal perforation | Report experience of stent in treatment of nonmalignant esophageal leaks | To review management of patients with esophageal perforation and to create algorithm in the management. | To report experience with stent treatment for benign esophageal leakages | Summarize treatment of iatrogenic perforations with stent | Summarize treatment of spontaneous perforations with stent | Evaluate safety and efficacy of stent treatment in patients with esophageal leaks, fistulae and perforations | Assess efficacy of stent treatment in esophageal leaks | Assess outcome of stent treatment for anastomotic leak after esophagectomy | Review treatment with stent in patients with delayed (> 24 h) intrathoracic esophageal perforation | To establish therapeutic efficacy of minimally invasive therapies in a consecutive series of patients with esophageal perforation | Evaluate results from stent treatment in patients with esophageal intrathoracic and cervical leaks | To evaluate the effects of endoluminal stent treatment in patients with esophageal anastomotic leakages of perforations. | Compare results of primary surgical therapy with endoscopic stenting in patients with spontaneous rupture of the esophagus | Evaluate outcome and clinical effectiveness of CSES in esophageal anastomotic leakage |
| Cause of leakage | |||||||||||||||||
| Iatrogenic | 16 | 2 | 7 | 32 | 17 | 8 | 2 | 7 | 59 | 4 | |||||||
| Spontaneous | 23 | 2 | 2 | 15 | 19 | 2 | 1 | 1 | 9 | 4 | 38 | ||||||
| Trauma | 1 | 1 | |||||||||||||||
| Esophagogastrostomy | 1 | 21 | 15 | 13 | 19 | 11 | |||||||||||
| Esophagojejunostomy | 8 | 3 | 24 | ||||||||||||||
| Foreign body | 2 | ||||||||||||||||
| Success rate stent treatment† (%) | 83 | 50 | 69 | 100 | 67 | 87 | 94 | 89 | 90 | 94 | 87 | 100 | 100 | 92 | 87 | 85 | 71 |
| Success† | 33 | 2 | 9 | 4 | 2 | 41 | 16 | 17 | 9 | 30 | 13 | 8 | 68 | 12 | 26 | 11 | 25 |
| Mortality in stent group | 3 | 2 | 4 | 0 | 1 | 0 | 0 | 0 | 1 | 2 | 1 | 0 | 0 | 1 | 2 | 2 | 9 |
| Conclusion | Stent treatment seems to be a successful concept when applied to an unselected group of benign esophageal perforations. Delayed treatment indicated risk for failed stent therapy. | Traumatic perforations and anastomotic leaks can be treated effectively with stent with adequate drainage even in cases of severely ill patients. | Stent therapy neither increased survival nor decreased length of therapy once mediastinitis had developed. Main advantage is the preservation of native esophagus and reduced extent of surgical mediastinal drainage. | Stents represent a safe method for sealing benign esophageal leaks and should be discussed as first-line therapy in contained perforations without severe mediastinitis of the mid esophagus. | A small subset of patients can be treated conservatively by stenting. In the majority of patients a primary repair can be performed with good prognosis. | Temporary stent placement for benign leakages of the esophagus is safe and seems to improve treatment success. | Stent placement is effective treatment of acute iatrogenic esophageal perforations and may reduce hospital length stay and avoid potential morbidities of operative repair. | Stent placement is effective treatment of most spontaneous esophageal perforations and may reduce hospital length stay and avoid potential morbidities of operative repair. | Stents are safe and effective in treating esophageal leaks, fistulas and perforations. Defect opening size and time from diagnosis to stent placement appear to be candidate predictors for successful closure. | Stenting is a viable option in combination with interventional or surgical drainage | Stents are an effective and safe option in management of post esophagectomy leaks | Esophageal stenting is effective in the management of delayed intrathoracic esophageal perforation | Endoscopically placed removable esophageal stents with minimally invasive repair of the perforation and feeding access is an effective treatment method for patients with esophageal perforation. | Stent treatment can prevent reoperation but does not decrease average hospital stay | Implantation of self-expanding stents after esophageal resection or perforation is a feasible and safe procedure with an acceptable morbidity even if used as last-choice treatment | Authors recommend surgical intervention as primary treatment in patients with spontaneous esophageal rupture | Stents are an effective treatment for leakages in patients with esophagogastrostomies and esophagejejunostomies |
| Author/ . | Persson/ . | Salminen/ . | Safranek/ . | Radecke/ . | Kroepil/ . | Gubler/ . | Freeman/ . | Freeman/ . | El Hajj/ . | Dai/2011 . | Al-Issa/ . | Zhou/2009 . | Ben-David/ . | Eizaguirre/ . | Tuebergen/ . | Schweigert/ . | Hoeppner/ . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year . | 2014 . | 2009 . | 2014 . | 2006 . | 2013 . | 2014 . | 2007 . | 2009 . | 2014 . | 2011 . | 2014 . | 2009 . | 2014 . | 2016 . | 2008 . | 2013 . | 2014 . |
| Country . | Sweden . | Finland . | Czech Republic . | Germany . | Germany . | Switzerland . | USA . | USA . | USA . | Germany . | Denmark . | China . | USA . | Spain . | Germany . | Germany, UK . | Germany . |
| Study design | Prospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Prospective single center | Prospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Prospective single center | Retrospective multi center | Prospective single center |
| Number of patients receiving stent therapy for leakage† | 40 | 4 | 13 | 4 | 3 | 47 | 17 | 19 | 10 | 32 | 15 | 8 | 68 | 13 | 30 | 13 | 35 |
| Aim of the study | To investigate possible predictors for failed stent therapy in patients with benign esophageal perforation | To evaluate the role of stent therapy for the management of esophageal perforations and anastomotic leaks | To evaluate use of stents for treatment of patients suffering from mediastinitis due to esophageal perforation | Report experience of stent in treatment of nonmalignant esophageal leaks | To review management of patients with esophageal perforation and to create algorithm in the management. | To report experience with stent treatment for benign esophageal leakages | Summarize treatment of iatrogenic perforations with stent | Summarize treatment of spontaneous perforations with stent | Evaluate safety and efficacy of stent treatment in patients with esophageal leaks, fistulae and perforations | Assess efficacy of stent treatment in esophageal leaks | Assess outcome of stent treatment for anastomotic leak after esophagectomy | Review treatment with stent in patients with delayed (> 24 h) intrathoracic esophageal perforation | To establish therapeutic efficacy of minimally invasive therapies in a consecutive series of patients with esophageal perforation | Evaluate results from stent treatment in patients with esophageal intrathoracic and cervical leaks | To evaluate the effects of endoluminal stent treatment in patients with esophageal anastomotic leakages of perforations. | Compare results of primary surgical therapy with endoscopic stenting in patients with spontaneous rupture of the esophagus | Evaluate outcome and clinical effectiveness of CSES in esophageal anastomotic leakage |
| Cause of leakage | |||||||||||||||||
| Iatrogenic | 16 | 2 | 7 | 32 | 17 | 8 | 2 | 7 | 59 | 4 | |||||||
| Spontaneous | 23 | 2 | 2 | 15 | 19 | 2 | 1 | 1 | 9 | 4 | 38 | ||||||
| Trauma | 1 | 1 | |||||||||||||||
| Esophagogastrostomy | 1 | 21 | 15 | 13 | 19 | 11 | |||||||||||
| Esophagojejunostomy | 8 | 3 | 24 | ||||||||||||||
| Foreign body | 2 | ||||||||||||||||
| Success rate stent treatment† (%) | 83 | 50 | 69 | 100 | 67 | 87 | 94 | 89 | 90 | 94 | 87 | 100 | 100 | 92 | 87 | 85 | 71 |
| Success† | 33 | 2 | 9 | 4 | 2 | 41 | 16 | 17 | 9 | 30 | 13 | 8 | 68 | 12 | 26 | 11 | 25 |
| Mortality in stent group | 3 | 2 | 4 | 0 | 1 | 0 | 0 | 0 | 1 | 2 | 1 | 0 | 0 | 1 | 2 | 2 | 9 |
| Conclusion | Stent treatment seems to be a successful concept when applied to an unselected group of benign esophageal perforations. Delayed treatment indicated risk for failed stent therapy. | Traumatic perforations and anastomotic leaks can be treated effectively with stent with adequate drainage even in cases of severely ill patients. | Stent therapy neither increased survival nor decreased length of therapy once mediastinitis had developed. Main advantage is the preservation of native esophagus and reduced extent of surgical mediastinal drainage. | Stents represent a safe method for sealing benign esophageal leaks and should be discussed as first-line therapy in contained perforations without severe mediastinitis of the mid esophagus. | A small subset of patients can be treated conservatively by stenting. In the majority of patients a primary repair can be performed with good prognosis. | Temporary stent placement for benign leakages of the esophagus is safe and seems to improve treatment success. | Stent placement is effective treatment of acute iatrogenic esophageal perforations and may reduce hospital length stay and avoid potential morbidities of operative repair. | Stent placement is effective treatment of most spontaneous esophageal perforations and may reduce hospital length stay and avoid potential morbidities of operative repair. | Stents are safe and effective in treating esophageal leaks, fistulas and perforations. Defect opening size and time from diagnosis to stent placement appear to be candidate predictors for successful closure. | Stenting is a viable option in combination with interventional or surgical drainage | Stents are an effective and safe option in management of post esophagectomy leaks | Esophageal stenting is effective in the management of delayed intrathoracic esophageal perforation | Endoscopically placed removable esophageal stents with minimally invasive repair of the perforation and feeding access is an effective treatment method for patients with esophageal perforation. | Stent treatment can prevent reoperation but does not decrease average hospital stay | Implantation of self-expanding stents after esophageal resection or perforation is a feasible and safe procedure with an acceptable morbidity even if used as last-choice treatment | Authors recommend surgical intervention as primary treatment in patients with spontaneous esophageal rupture | Stents are an effective treatment for leakages in patients with esophagogastrostomies and esophagejejunostomies |
†According to the specific study's defined criteria.
In Figure 1B is given the reasons for selecting the final 17, out of originally 785 articles, covering the surgical exploration strategy. None of these reports had applied a prospective protocol, over a defined time period, to assess treatment efficacy. Likewise, no study had used a strict definition of treatment failure (see above). We were unable to separate the final number of cases representing pure anastomotic dehiscence from other causes behind the leaking organ. Moreover, it was basically impossible to extract information on how often SEMS had been used as an adjunct to the surgical exploration and sealing of the leakage.
The number of patients submitted to the various surgical interventions is depicted in Table 2. The vast majority of these patients had an attempt to repair the defect by direct or enforced suturing. This surgical approach also included procedures such as patching with pleura or with a diaphragmatic flap. It was impossible to separate individual procedures with regard to the final outcome either in terms of success rates or regarding in-hospital mortality, since all series contained a mixture of different surgical repairs and interventions. Nevertheless, the overall reported success rate was 83% (305/368) and the in-hospital mortality was 17% (61/368).
Eligible studies regarding surgical management
| Author/ . | de Aquino/ . | Griffin/ . | Tettey/ . | Sulpice/ . | Sng/ . | Shaker/ . | Pereira-Graterol/ . | Lazar/ . | Lin/ . | Huber-Lang/ . | Fry/ . | Freeman/ . | Breigerion/ . | Bresadola/ . | Cho/ . | Connelly/ . | Dagres/ . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year . | 2014 . | 2008 . | 2011 . | 2013 . | 2008 . | 2010 . | 2006 . | 2011 . | 2014 . | 2006 . | 2007 . | 2015 . | 2008 . | 2008 . | 2011 . | 2013 . | 2006 . |
| Country . | Brazil . | UK . | Ghana . | France . | Singapore . | UK . | Mexico . | Hungary . | China . | Germany . | Germany . | USA . | Brazil . | Italy . | Korea . | UK . | Greece . |
| Study design | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective multi center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective multi center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center |
| Number of patients undergoing surgical treatment for leakage† | 28 | 31 | 16 | 39 | 4 | 23 | 5 | 14 | 36 | 8 | 4 | 30 | 81 | 12 | 15 | 17 | 5 |
| Type of treatment | |||||||||||||||||
| Primary repair | 2 | 5 | 25 | 2 | 21 | 5 | 7 | 33 | 5 | 3 | 30 | 45 | 2 | 15 | 5 | ||
| T-tube | 29 | 14 | 3 | 0 | 11 | ||||||||||||
| Direct reconstruction | 3 | 3 | 1 | 1 | NA | ||||||||||||
| Esophagectomy with end-esophagostomy | 25 | 11 | 1 | 2 | 4 | 2 | 2 | 7 | 3 | ||||||||
| Diversion esophagectomy | 1 | NA | 3 | ||||||||||||||
| Other | Simple drainage, jejunostomy and drainage | Palliative treatment after diagnostic laparotomy due to size of tear and poor clinical condition of the patient | Two patients died before surgery could be performed | ||||||||||||||
| Aim of the study | To demonstrate and analyze the results of urgent esophagectomy in a series of patients with esophageal perforation | To evaluate the diagnosis, management and outcome of patients with spontaneous rupture of the esophagus in a single center. | To evaluate the management options that were employed in the treatment of patients with esophageal perforation and the outcome. | To evaluate outcome of conservative surgery for primary or T-tube repair performed in two tertiary referral centers. | To present a local experience on esophageal perforation secondary to ingested bones. | To present the authors experience in managing patients with esophageal rupture | To describe the technique deployed and the institutions experience with primary laparoscopic repair of distal esophageal perforations produced during laparoscopic esophagomyotomy. | To present the institutions experience in treatment strategy for Boerhaave's syndrome | To characterize an optimal strategy in managing thoracic esophageal perforation focusing on differential diagnosis and treatment of patients with contained vs. noncontained perforations. | To evaluate the management of esophageal perforation. | To assess the incident of perforation, management and outcomes after endoscopic esophageal dilatation. | To compare the outcomes and costs of surgical repair and stent placement in selected patients with acute esophageal perforation. | To identify risk factors for surgical site infections after surgery for esophageal perforation | To review the diagnosis and treatment of patients with perforation in a healthy esophagus | To evaluate the outcomes of thoracoscopic surgery in patients with Boerhaave's syndrome | To analyze outcomes in patients with Boerhaave's syndrome | To identify criteria for rapid recognition and successful treatment of esophageal perforation after radiofrequency ablation for atrial fibrillation |
| Cause of leakage | |||||||||||||||||
| Iatrogenic | 22 | 10 | 2 | NA | 5 | NA | 6 | 4 | 30 | 4 | 7 | 3 | |||||
| Spontaneous | 1 | 31 | 1 | 39 | NA | 14 | NA | 2 | 0 | 5 | 15 | 17 | |||||
| Trauma | 4 | 0 | NA | 32 | |||||||||||||
| Esophagogastrostomy | 0 | 0 | 0 | ||||||||||||||
| Esophagojejunostomy | 1 | 0 | 0 | 0 | |||||||||||||
| Foreign body | 5 | 2 | 0 | NA | 45 | ||||||||||||
| Success rate surgical treatment† (%) | 82 | 65 | 94 | 77 | 75 | 79 | 80 | 100 | 94 | 88 | 75 | 93 | 82 | 75 | 93 | 76 | 100 |
| Success† | 23 | 20 | 15 | 30 | 3 | 19 | 4 | 14 | 34 | 7 | 3 | 28 | 66 | 9 | 14 | 13 | 3 |
| Mortality in surgery group | 5 | 11 | 1 | 9 | 1 | 4 | 1 | 0 | 2 | 1 | 1 | 2 | 15 | 3 | 1 | 4 | 0 |
| Conclusion | Despite the morbidity, emergency esophagectomy has its validity, especially in well-indicated cases of esophageal perforation subsequent to endoscopic dilations for benign strictures. | Spontaneous esophageal rupture represents a spectrum of disease. Accurate radiological and endoscopic evaluation can identify those suitable for radical nonoperative treatment and those who require thoracotomy. | Early diagnosis and the institution of appropriate management is the key to a better outcome. The authors concur with the fact that esophageal perforation is a surgical disease and only a few cases may qualify to be managed non-operatively. | Primary and T-tube repair provide at least equivalent results. Reinforced sutures appear to provide better outcomes by reducing postoperative leakage. | Esophageal perforation requires prompt diagnosis and treatment. Most of the esophageal perforations in the study are secondary to ingested bones and such cases can often be treated conservatively. | Early diagnosis and management (within 24h) are crucial for successful outcome in patients with rupture of the esophagus. | The primary repair of distal esophageal perforations during laparoscopic esophagomyotomy is a valid therapeutic option and does not alter the surgical purpose. If the perforation is not recognized early on, the prognosis can change. | Early diagnosis and carefully selected therapeutic tactics can reduce mortality rate of Boerhaave's syndrome. Methods of organ preservation and minimally invasive techniques can be applied successfully in the treatment. | Contained or non-contained perforation should be rigorously differentiated. For a contained perforation, conservative therapy is reasonable. For a non-contained perforation primary repair can be safely performed within 48h after injury. | Data support the individualized surgical management of esophageal perforation, based on careful evaluation of various patient-related factors, including CT-findings. | Endoscopic esophageal dilatation is a safe procedure. Perforation rate is low. Early recognition of perforation is associated with good outcome. Small perforations can be treated conservatively. | Esophageal stent placement seems to be as effective as surgical repair. Stent placement resulted in a shorter length of stay, lower rates of morbidity and lower costs when compared with traditional surgical repair. | Risk factors for surgical site infection following surgical management of esophageal perforation were age ≥ 50, time delay to treatment > 24 h, associated lesion in other cavity and Injury Severity Score ≥ 15 | The choice of treatment for perforation in a healthy esophagus depends mainly on the site and site of lesion. Esophageal resection and delayed reconstruction seems to be the safest options for thoracic lesions with associated sepsis or major loss of substance. | Thoracoscopic esophageal repair may be a good surgical alternative in patients with Boerhaave's syndrome who have a relatively stable vital sign or mild inflammation regardless of time between perforation and surgery | Aggressive surgical management with direct repair is associated with good survival in patients with Boerhaave's syndrome | Leading symptom of esophageal perforation is high fever or severe chest/epigastric pain. Immediate surgery may prevent neurologic complications and could possible result in a high survival rate without residues. |
| Author/ . | de Aquino/ . | Griffin/ . | Tettey/ . | Sulpice/ . | Sng/ . | Shaker/ . | Pereira-Graterol/ . | Lazar/ . | Lin/ . | Huber-Lang/ . | Fry/ . | Freeman/ . | Breigerion/ . | Bresadola/ . | Cho/ . | Connelly/ . | Dagres/ . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year . | 2014 . | 2008 . | 2011 . | 2013 . | 2008 . | 2010 . | 2006 . | 2011 . | 2014 . | 2006 . | 2007 . | 2015 . | 2008 . | 2008 . | 2011 . | 2013 . | 2006 . |
| Country . | Brazil . | UK . | Ghana . | France . | Singapore . | UK . | Mexico . | Hungary . | China . | Germany . | Germany . | USA . | Brazil . | Italy . | Korea . | UK . | Greece . |
| Study design | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective multi center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective multi center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center |
| Number of patients undergoing surgical treatment for leakage† | 28 | 31 | 16 | 39 | 4 | 23 | 5 | 14 | 36 | 8 | 4 | 30 | 81 | 12 | 15 | 17 | 5 |
| Type of treatment | |||||||||||||||||
| Primary repair | 2 | 5 | 25 | 2 | 21 | 5 | 7 | 33 | 5 | 3 | 30 | 45 | 2 | 15 | 5 | ||
| T-tube | 29 | 14 | 3 | 0 | 11 | ||||||||||||
| Direct reconstruction | 3 | 3 | 1 | 1 | NA | ||||||||||||
| Esophagectomy with end-esophagostomy | 25 | 11 | 1 | 2 | 4 | 2 | 2 | 7 | 3 | ||||||||
| Diversion esophagectomy | 1 | NA | 3 | ||||||||||||||
| Other | Simple drainage, jejunostomy and drainage | Palliative treatment after diagnostic laparotomy due to size of tear and poor clinical condition of the patient | Two patients died before surgery could be performed | ||||||||||||||
| Aim of the study | To demonstrate and analyze the results of urgent esophagectomy in a series of patients with esophageal perforation | To evaluate the diagnosis, management and outcome of patients with spontaneous rupture of the esophagus in a single center. | To evaluate the management options that were employed in the treatment of patients with esophageal perforation and the outcome. | To evaluate outcome of conservative surgery for primary or T-tube repair performed in two tertiary referral centers. | To present a local experience on esophageal perforation secondary to ingested bones. | To present the authors experience in managing patients with esophageal rupture | To describe the technique deployed and the institutions experience with primary laparoscopic repair of distal esophageal perforations produced during laparoscopic esophagomyotomy. | To present the institutions experience in treatment strategy for Boerhaave's syndrome | To characterize an optimal strategy in managing thoracic esophageal perforation focusing on differential diagnosis and treatment of patients with contained vs. noncontained perforations. | To evaluate the management of esophageal perforation. | To assess the incident of perforation, management and outcomes after endoscopic esophageal dilatation. | To compare the outcomes and costs of surgical repair and stent placement in selected patients with acute esophageal perforation. | To identify risk factors for surgical site infections after surgery for esophageal perforation | To review the diagnosis and treatment of patients with perforation in a healthy esophagus | To evaluate the outcomes of thoracoscopic surgery in patients with Boerhaave's syndrome | To analyze outcomes in patients with Boerhaave's syndrome | To identify criteria for rapid recognition and successful treatment of esophageal perforation after radiofrequency ablation for atrial fibrillation |
| Cause of leakage | |||||||||||||||||
| Iatrogenic | 22 | 10 | 2 | NA | 5 | NA | 6 | 4 | 30 | 4 | 7 | 3 | |||||
| Spontaneous | 1 | 31 | 1 | 39 | NA | 14 | NA | 2 | 0 | 5 | 15 | 17 | |||||
| Trauma | 4 | 0 | NA | 32 | |||||||||||||
| Esophagogastrostomy | 0 | 0 | 0 | ||||||||||||||
| Esophagojejunostomy | 1 | 0 | 0 | 0 | |||||||||||||
| Foreign body | 5 | 2 | 0 | NA | 45 | ||||||||||||
| Success rate surgical treatment† (%) | 82 | 65 | 94 | 77 | 75 | 79 | 80 | 100 | 94 | 88 | 75 | 93 | 82 | 75 | 93 | 76 | 100 |
| Success† | 23 | 20 | 15 | 30 | 3 | 19 | 4 | 14 | 34 | 7 | 3 | 28 | 66 | 9 | 14 | 13 | 3 |
| Mortality in surgery group | 5 | 11 | 1 | 9 | 1 | 4 | 1 | 0 | 2 | 1 | 1 | 2 | 15 | 3 | 1 | 4 | 0 |
| Conclusion | Despite the morbidity, emergency esophagectomy has its validity, especially in well-indicated cases of esophageal perforation subsequent to endoscopic dilations for benign strictures. | Spontaneous esophageal rupture represents a spectrum of disease. Accurate radiological and endoscopic evaluation can identify those suitable for radical nonoperative treatment and those who require thoracotomy. | Early diagnosis and the institution of appropriate management is the key to a better outcome. The authors concur with the fact that esophageal perforation is a surgical disease and only a few cases may qualify to be managed non-operatively. | Primary and T-tube repair provide at least equivalent results. Reinforced sutures appear to provide better outcomes by reducing postoperative leakage. | Esophageal perforation requires prompt diagnosis and treatment. Most of the esophageal perforations in the study are secondary to ingested bones and such cases can often be treated conservatively. | Early diagnosis and management (within 24h) are crucial for successful outcome in patients with rupture of the esophagus. | The primary repair of distal esophageal perforations during laparoscopic esophagomyotomy is a valid therapeutic option and does not alter the surgical purpose. If the perforation is not recognized early on, the prognosis can change. | Early diagnosis and carefully selected therapeutic tactics can reduce mortality rate of Boerhaave's syndrome. Methods of organ preservation and minimally invasive techniques can be applied successfully in the treatment. | Contained or non-contained perforation should be rigorously differentiated. For a contained perforation, conservative therapy is reasonable. For a non-contained perforation primary repair can be safely performed within 48h after injury. | Data support the individualized surgical management of esophageal perforation, based on careful evaluation of various patient-related factors, including CT-findings. | Endoscopic esophageal dilatation is a safe procedure. Perforation rate is low. Early recognition of perforation is associated with good outcome. Small perforations can be treated conservatively. | Esophageal stent placement seems to be as effective as surgical repair. Stent placement resulted in a shorter length of stay, lower rates of morbidity and lower costs when compared with traditional surgical repair. | Risk factors for surgical site infection following surgical management of esophageal perforation were age ≥ 50, time delay to treatment > 24 h, associated lesion in other cavity and Injury Severity Score ≥ 15 | The choice of treatment for perforation in a healthy esophagus depends mainly on the site and site of lesion. Esophageal resection and delayed reconstruction seems to be the safest options for thoracic lesions with associated sepsis or major loss of substance. | Thoracoscopic esophageal repair may be a good surgical alternative in patients with Boerhaave's syndrome who have a relatively stable vital sign or mild inflammation regardless of time between perforation and surgery | Aggressive surgical management with direct repair is associated with good survival in patients with Boerhaave's syndrome | Leading symptom of esophageal perforation is high fever or severe chest/epigastric pain. Immediate surgery may prevent neurologic complications and could possible result in a high survival rate without residues. |
†According to the specific study's defined criteria.
Eligible studies regarding surgical management
| Author/ . | de Aquino/ . | Griffin/ . | Tettey/ . | Sulpice/ . | Sng/ . | Shaker/ . | Pereira-Graterol/ . | Lazar/ . | Lin/ . | Huber-Lang/ . | Fry/ . | Freeman/ . | Breigerion/ . | Bresadola/ . | Cho/ . | Connelly/ . | Dagres/ . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year . | 2014 . | 2008 . | 2011 . | 2013 . | 2008 . | 2010 . | 2006 . | 2011 . | 2014 . | 2006 . | 2007 . | 2015 . | 2008 . | 2008 . | 2011 . | 2013 . | 2006 . |
| Country . | Brazil . | UK . | Ghana . | France . | Singapore . | UK . | Mexico . | Hungary . | China . | Germany . | Germany . | USA . | Brazil . | Italy . | Korea . | UK . | Greece . |
| Study design | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective multi center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective multi center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center |
| Number of patients undergoing surgical treatment for leakage† | 28 | 31 | 16 | 39 | 4 | 23 | 5 | 14 | 36 | 8 | 4 | 30 | 81 | 12 | 15 | 17 | 5 |
| Type of treatment | |||||||||||||||||
| Primary repair | 2 | 5 | 25 | 2 | 21 | 5 | 7 | 33 | 5 | 3 | 30 | 45 | 2 | 15 | 5 | ||
| T-tube | 29 | 14 | 3 | 0 | 11 | ||||||||||||
| Direct reconstruction | 3 | 3 | 1 | 1 | NA | ||||||||||||
| Esophagectomy with end-esophagostomy | 25 | 11 | 1 | 2 | 4 | 2 | 2 | 7 | 3 | ||||||||
| Diversion esophagectomy | 1 | NA | 3 | ||||||||||||||
| Other | Simple drainage, jejunostomy and drainage | Palliative treatment after diagnostic laparotomy due to size of tear and poor clinical condition of the patient | Two patients died before surgery could be performed | ||||||||||||||
| Aim of the study | To demonstrate and analyze the results of urgent esophagectomy in a series of patients with esophageal perforation | To evaluate the diagnosis, management and outcome of patients with spontaneous rupture of the esophagus in a single center. | To evaluate the management options that were employed in the treatment of patients with esophageal perforation and the outcome. | To evaluate outcome of conservative surgery for primary or T-tube repair performed in two tertiary referral centers. | To present a local experience on esophageal perforation secondary to ingested bones. | To present the authors experience in managing patients with esophageal rupture | To describe the technique deployed and the institutions experience with primary laparoscopic repair of distal esophageal perforations produced during laparoscopic esophagomyotomy. | To present the institutions experience in treatment strategy for Boerhaave's syndrome | To characterize an optimal strategy in managing thoracic esophageal perforation focusing on differential diagnosis and treatment of patients with contained vs. noncontained perforations. | To evaluate the management of esophageal perforation. | To assess the incident of perforation, management and outcomes after endoscopic esophageal dilatation. | To compare the outcomes and costs of surgical repair and stent placement in selected patients with acute esophageal perforation. | To identify risk factors for surgical site infections after surgery for esophageal perforation | To review the diagnosis and treatment of patients with perforation in a healthy esophagus | To evaluate the outcomes of thoracoscopic surgery in patients with Boerhaave's syndrome | To analyze outcomes in patients with Boerhaave's syndrome | To identify criteria for rapid recognition and successful treatment of esophageal perforation after radiofrequency ablation for atrial fibrillation |
| Cause of leakage | |||||||||||||||||
| Iatrogenic | 22 | 10 | 2 | NA | 5 | NA | 6 | 4 | 30 | 4 | 7 | 3 | |||||
| Spontaneous | 1 | 31 | 1 | 39 | NA | 14 | NA | 2 | 0 | 5 | 15 | 17 | |||||
| Trauma | 4 | 0 | NA | 32 | |||||||||||||
| Esophagogastrostomy | 0 | 0 | 0 | ||||||||||||||
| Esophagojejunostomy | 1 | 0 | 0 | 0 | |||||||||||||
| Foreign body | 5 | 2 | 0 | NA | 45 | ||||||||||||
| Success rate surgical treatment† (%) | 82 | 65 | 94 | 77 | 75 | 79 | 80 | 100 | 94 | 88 | 75 | 93 | 82 | 75 | 93 | 76 | 100 |
| Success† | 23 | 20 | 15 | 30 | 3 | 19 | 4 | 14 | 34 | 7 | 3 | 28 | 66 | 9 | 14 | 13 | 3 |
| Mortality in surgery group | 5 | 11 | 1 | 9 | 1 | 4 | 1 | 0 | 2 | 1 | 1 | 2 | 15 | 3 | 1 | 4 | 0 |
| Conclusion | Despite the morbidity, emergency esophagectomy has its validity, especially in well-indicated cases of esophageal perforation subsequent to endoscopic dilations for benign strictures. | Spontaneous esophageal rupture represents a spectrum of disease. Accurate radiological and endoscopic evaluation can identify those suitable for radical nonoperative treatment and those who require thoracotomy. | Early diagnosis and the institution of appropriate management is the key to a better outcome. The authors concur with the fact that esophageal perforation is a surgical disease and only a few cases may qualify to be managed non-operatively. | Primary and T-tube repair provide at least equivalent results. Reinforced sutures appear to provide better outcomes by reducing postoperative leakage. | Esophageal perforation requires prompt diagnosis and treatment. Most of the esophageal perforations in the study are secondary to ingested bones and such cases can often be treated conservatively. | Early diagnosis and management (within 24h) are crucial for successful outcome in patients with rupture of the esophagus. | The primary repair of distal esophageal perforations during laparoscopic esophagomyotomy is a valid therapeutic option and does not alter the surgical purpose. If the perforation is not recognized early on, the prognosis can change. | Early diagnosis and carefully selected therapeutic tactics can reduce mortality rate of Boerhaave's syndrome. Methods of organ preservation and minimally invasive techniques can be applied successfully in the treatment. | Contained or non-contained perforation should be rigorously differentiated. For a contained perforation, conservative therapy is reasonable. For a non-contained perforation primary repair can be safely performed within 48h after injury. | Data support the individualized surgical management of esophageal perforation, based on careful evaluation of various patient-related factors, including CT-findings. | Endoscopic esophageal dilatation is a safe procedure. Perforation rate is low. Early recognition of perforation is associated with good outcome. Small perforations can be treated conservatively. | Esophageal stent placement seems to be as effective as surgical repair. Stent placement resulted in a shorter length of stay, lower rates of morbidity and lower costs when compared with traditional surgical repair. | Risk factors for surgical site infection following surgical management of esophageal perforation were age ≥ 50, time delay to treatment > 24 h, associated lesion in other cavity and Injury Severity Score ≥ 15 | The choice of treatment for perforation in a healthy esophagus depends mainly on the site and site of lesion. Esophageal resection and delayed reconstruction seems to be the safest options for thoracic lesions with associated sepsis or major loss of substance. | Thoracoscopic esophageal repair may be a good surgical alternative in patients with Boerhaave's syndrome who have a relatively stable vital sign or mild inflammation regardless of time between perforation and surgery | Aggressive surgical management with direct repair is associated with good survival in patients with Boerhaave's syndrome | Leading symptom of esophageal perforation is high fever or severe chest/epigastric pain. Immediate surgery may prevent neurologic complications and could possible result in a high survival rate without residues. |
| Author/ . | de Aquino/ . | Griffin/ . | Tettey/ . | Sulpice/ . | Sng/ . | Shaker/ . | Pereira-Graterol/ . | Lazar/ . | Lin/ . | Huber-Lang/ . | Fry/ . | Freeman/ . | Breigerion/ . | Bresadola/ . | Cho/ . | Connelly/ . | Dagres/ . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year . | 2014 . | 2008 . | 2011 . | 2013 . | 2008 . | 2010 . | 2006 . | 2011 . | 2014 . | 2006 . | 2007 . | 2015 . | 2008 . | 2008 . | 2011 . | 2013 . | 2006 . |
| Country . | Brazil . | UK . | Ghana . | France . | Singapore . | UK . | Mexico . | Hungary . | China . | Germany . | Germany . | USA . | Brazil . | Italy . | Korea . | UK . | Greece . |
| Study design | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective multi center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective multi center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center | Retrospective single center |
| Number of patients undergoing surgical treatment for leakage† | 28 | 31 | 16 | 39 | 4 | 23 | 5 | 14 | 36 | 8 | 4 | 30 | 81 | 12 | 15 | 17 | 5 |
| Type of treatment | |||||||||||||||||
| Primary repair | 2 | 5 | 25 | 2 | 21 | 5 | 7 | 33 | 5 | 3 | 30 | 45 | 2 | 15 | 5 | ||
| T-tube | 29 | 14 | 3 | 0 | 11 | ||||||||||||
| Direct reconstruction | 3 | 3 | 1 | 1 | NA | ||||||||||||
| Esophagectomy with end-esophagostomy | 25 | 11 | 1 | 2 | 4 | 2 | 2 | 7 | 3 | ||||||||
| Diversion esophagectomy | 1 | NA | 3 | ||||||||||||||
| Other | Simple drainage, jejunostomy and drainage | Palliative treatment after diagnostic laparotomy due to size of tear and poor clinical condition of the patient | Two patients died before surgery could be performed | ||||||||||||||
| Aim of the study | To demonstrate and analyze the results of urgent esophagectomy in a series of patients with esophageal perforation | To evaluate the diagnosis, management and outcome of patients with spontaneous rupture of the esophagus in a single center. | To evaluate the management options that were employed in the treatment of patients with esophageal perforation and the outcome. | To evaluate outcome of conservative surgery for primary or T-tube repair performed in two tertiary referral centers. | To present a local experience on esophageal perforation secondary to ingested bones. | To present the authors experience in managing patients with esophageal rupture | To describe the technique deployed and the institutions experience with primary laparoscopic repair of distal esophageal perforations produced during laparoscopic esophagomyotomy. | To present the institutions experience in treatment strategy for Boerhaave's syndrome | To characterize an optimal strategy in managing thoracic esophageal perforation focusing on differential diagnosis and treatment of patients with contained vs. noncontained perforations. | To evaluate the management of esophageal perforation. | To assess the incident of perforation, management and outcomes after endoscopic esophageal dilatation. | To compare the outcomes and costs of surgical repair and stent placement in selected patients with acute esophageal perforation. | To identify risk factors for surgical site infections after surgery for esophageal perforation | To review the diagnosis and treatment of patients with perforation in a healthy esophagus | To evaluate the outcomes of thoracoscopic surgery in patients with Boerhaave's syndrome | To analyze outcomes in patients with Boerhaave's syndrome | To identify criteria for rapid recognition and successful treatment of esophageal perforation after radiofrequency ablation for atrial fibrillation |
| Cause of leakage | |||||||||||||||||
| Iatrogenic | 22 | 10 | 2 | NA | 5 | NA | 6 | 4 | 30 | 4 | 7 | 3 | |||||
| Spontaneous | 1 | 31 | 1 | 39 | NA | 14 | NA | 2 | 0 | 5 | 15 | 17 | |||||
| Trauma | 4 | 0 | NA | 32 | |||||||||||||
| Esophagogastrostomy | 0 | 0 | 0 | ||||||||||||||
| Esophagojejunostomy | 1 | 0 | 0 | 0 | |||||||||||||
| Foreign body | 5 | 2 | 0 | NA | 45 | ||||||||||||
| Success rate surgical treatment† (%) | 82 | 65 | 94 | 77 | 75 | 79 | 80 | 100 | 94 | 88 | 75 | 93 | 82 | 75 | 93 | 76 | 100 |
| Success† | 23 | 20 | 15 | 30 | 3 | 19 | 4 | 14 | 34 | 7 | 3 | 28 | 66 | 9 | 14 | 13 | 3 |
| Mortality in surgery group | 5 | 11 | 1 | 9 | 1 | 4 | 1 | 0 | 2 | 1 | 1 | 2 | 15 | 3 | 1 | 4 | 0 |
| Conclusion | Despite the morbidity, emergency esophagectomy has its validity, especially in well-indicated cases of esophageal perforation subsequent to endoscopic dilations for benign strictures. | Spontaneous esophageal rupture represents a spectrum of disease. Accurate radiological and endoscopic evaluation can identify those suitable for radical nonoperative treatment and those who require thoracotomy. | Early diagnosis and the institution of appropriate management is the key to a better outcome. The authors concur with the fact that esophageal perforation is a surgical disease and only a few cases may qualify to be managed non-operatively. | Primary and T-tube repair provide at least equivalent results. Reinforced sutures appear to provide better outcomes by reducing postoperative leakage. | Esophageal perforation requires prompt diagnosis and treatment. Most of the esophageal perforations in the study are secondary to ingested bones and such cases can often be treated conservatively. | Early diagnosis and management (within 24h) are crucial for successful outcome in patients with rupture of the esophagus. | The primary repair of distal esophageal perforations during laparoscopic esophagomyotomy is a valid therapeutic option and does not alter the surgical purpose. If the perforation is not recognized early on, the prognosis can change. | Early diagnosis and carefully selected therapeutic tactics can reduce mortality rate of Boerhaave's syndrome. Methods of organ preservation and minimally invasive techniques can be applied successfully in the treatment. | Contained or non-contained perforation should be rigorously differentiated. For a contained perforation, conservative therapy is reasonable. For a non-contained perforation primary repair can be safely performed within 48h after injury. | Data support the individualized surgical management of esophageal perforation, based on careful evaluation of various patient-related factors, including CT-findings. | Endoscopic esophageal dilatation is a safe procedure. Perforation rate is low. Early recognition of perforation is associated with good outcome. Small perforations can be treated conservatively. | Esophageal stent placement seems to be as effective as surgical repair. Stent placement resulted in a shorter length of stay, lower rates of morbidity and lower costs when compared with traditional surgical repair. | Risk factors for surgical site infection following surgical management of esophageal perforation were age ≥ 50, time delay to treatment > 24 h, associated lesion in other cavity and Injury Severity Score ≥ 15 | The choice of treatment for perforation in a healthy esophagus depends mainly on the site and site of lesion. Esophageal resection and delayed reconstruction seems to be the safest options for thoracic lesions with associated sepsis or major loss of substance. | Thoracoscopic esophageal repair may be a good surgical alternative in patients with Boerhaave's syndrome who have a relatively stable vital sign or mild inflammation regardless of time between perforation and surgery | Aggressive surgical management with direct repair is associated with good survival in patients with Boerhaave's syndrome | Leading symptom of esophageal perforation is high fever or severe chest/epigastric pain. Immediate surgery may prevent neurologic complications and could possible result in a high survival rate without residues. |
†According to the specific study's defined criteria.
DISCUSSION
The current systematic literature review, covering the past 10 years, revealed an astonishingly low level of scientific grading of the evidence behind the efficacy of the two predominant therapeutic management strategies, i.e. primary surgical exploration intervention and SEMS insertion. Although a large number of publications were available for scrutiny, very few fulfilled the inclusion criteria. Without a predefined methodological approach, we would be unable to complete meaningful analyses and make clinically relevant comparison between the available modalities. We had the ambition to carefully review the corresponding literature and to describe the outcomes of the two major therapeutic alternatives in the management of iatrogenic perforation—spontaneous esophageal rupture as separated from those with leaking esophageal anastomoses. Unfortunately, we had to conclude that an upfront comparison was not within reach due to incomplete precision (with few exceptions) in the available clinical information.
Leakages from defects in the native esophagus or in anastomoses engaging the organ represent the most complex and lethal injuries of the gastrointestinal tract.1,57 Overall mortality after esophageal leaks ranges from 10% to 25% even with urgent recognition and vigorous treatment.37–40,58 The mortality is at least two-folded, when the diagnostic and therapeutic delay exceed 24 hours.3–5 Prolonged spillover of digestive enzymes, bacteria, bile, and refluxed gastric contents into the mediastinum, combined with constant mediastinal movement with respiration and negative intrathoracic pressure sucking esophageal contents outward, contributes to these high mortality rates. Nonsurgical treatment strategies range from conservative medical management with antibiotics to endoscopic stenting with or without percutaneous drainage of infected pleural effusions. Surgical options include primary repair of the perforation with decortication and drainage, as well as esophagectomy with either immediate or delayed reconstruction. Prompt treatment of esophageal leak is recognized as a cornerstone for achieving better results in all of these patients, irrespective of which therapeutic strategy that is followed.
Stent grafting of the leakage is expected to reduce the extent and request for subsequent repair procedures and to enable preservation of the esophagus. In a recent study from our institution, we applied an SEMS-based strategy as a first-line treatment of all presenting patients with esophageal perforation-rupture, minimizing the risk of introducing a selection bias.6 Accordingly, the efficacy of SEMS and predictors for failure of this therapeutic concept was analyzed. The major finding in that study was that the time between initiation of symptoms damage and the accuracy of stent positioning were the most predominant risk factors for treatment failure. Two potentially important negative prognostic trends emerged, i.e. a distal esophageal defect (i.e. a defect that straddled the GE junction) and the cardiovascular comorbidity of the patients.6 Given the limitations of the current literature review, we were able to conclude that an overall success rate of close to 90% could be reached by the prompt and vigorous applications of SEMS to control similar leakages. Despite these conclusions, management of acute esophageal perforations ruptures remains variable and lack rigid guidelines, other than early treatment within 24 to 48 h of injury. Obviously, the selection of the treatment option remains to be dictated by the stability and operability of the individual patient and by the surgeon's and the overall team experience and local preferences.1,3,4,59
Likewise, the management strategies for treating leakages from esophageal anastomoses vary as well. The lack of consensus is partly dependent on the rarity of these complications, the substantial variability in clinical severity, lack of a standardized classification of the magnitude and significance of the dehiscence13 and also that the literature is burdened by small single institutional series diluted by a multiplicity of confounders. The clinical decision making has not been simplified by the advent of several minimally invasive endoscopic methods, which include not only esophageal stents but also clips, fibrin glue, and endoluminal vacuum therapy.4,24,60,61 Most publications report the outcome in a limited number of patients, where the focus has been only on clinical characteristics of the anastomotic leakages and the outcome, without analyzing possible predictors for positive or negative clinical courses. When applying the term ‘treatment failure’ to this setting, which was defined as a radical change of the initial treatment strategy due to uncontrolled mediastinitis, it often meant emergency esophagectomy with end esophagostomy or death as a consequence of the uncontrolled mediastinal damage. In one of the few more focused studies on the risk factors behind these treatment failures in leaking esophageal anastomoses, it was found that in those patients in whom the leakage could be controlled, the in-hospital mortality was exceptionally low.62 In the same study, it was demonstrated that several factors predicted a failure of the SEMS-based strategy. A persistent leakage after the first stent placement was identified as such an independent risk factor.62 This strongly suggests that endoscopic reinterventions with adjustment and/or changes of stents shall be considered in a patient who develops signs of continuous leakage, even if there was initial proof of sealed leakage. Routine radiological control after stent placement shall therefore be done. Esophageal stents need to be exchanged or removed because the complications associated with prolonged intubation of the esophagus are well known,63,64 but the exact time course for stent removal has to be better defined. Most studies recommend a period of 10–14 days for small esophageal defects and as long as 8 weeks for extended esophageal wall lesions. We have used fully covered metallic stents to facilitate removal and to minimize tissue in-growth. Future clinical research has to better document the options that can add to the efficacy of SEMS (e.g. vacuum therapy) and also the accurate timing of the switch to second-line treatment.
The detection of esophagotracheal fistula emerged as an independent risk factor for failure of the SEMS-based treatment.62 The reported incidence of airway fistulation amounts to <5%.23,28,62 Our own experience by the treatment of this specific complication with stents, usually applying a dual SEMS strategy, has recently been presented.65 However, in some cases where an esophagotracheal fistula is discovered after placement of a stent to an anastomotic leakage, it cannot be excluded that the airway fistulation may have even been caused by pressure from the esophageal stent on the very frail pars membranacea of the trachea. Future careful assessment of the SEMS-based therapeutic strategy will hopefully finally determine the relevance of these and other potentially lethal complications eventually being inborn with the properties of the device as such.
In patients with anastomotic leakages, there are always cases where the anatomical circumstances are unfit for SEMS insertion or make this strategy upfront redundant.66 It has also to be recognized that the anatomical environment around an esophagogastrostomy is many times unfavorable for SEMS to be effective, why ‘custom made’ stents have been launched in order to address these challenging situations. However, no data have, however, been presented to document the superiority of these sometimes exclusive devices. In our experience, the majority of cases, where the SEMS strategy was not followed, were in patients with a leaking cervical anastomoses, which could be carefully managed by externalization and drainage by a wide opening of the neck incision. Another circumstance, where SEMS cannot be used, is where there are endoscopic signs of conduit necrosis. The complication as well as success rates of endoscopic esophageal stent placement has varied substantially between published series.67–69 Despite the fact that most of these evaluate not only anastomotic leakages but also esophageal leakages of other etiologies, there are reasons (as discussed above) to assume a lower efficacy of SEMSs in the treatment of esophageal anastomotic leaks.
However, many investigators maintain the opinion that open surgical repair of the esophageal defect is the most effective treatment for esophageal perforation as well as anastomotic leakages,45,70,68–70,56 not least when initial aggressive conservative therapy fail.46,68,69 Repairs are also often difficult if the injury is more than 48 hours old. Moreover it has even been claimed that emergency esophagectomy for a perforation can be performed with similar short-term and long-term patient outcomes as an elective esophagectomy for both benign and malignant disease.56,71 In fact, a recent report, of a single institution experience,72 which was not included in the current review due to the timeframe of our literature search, presented unprecedented good results by the appliance of ‘surgical exploration’ based management concept. With zero mortality in patients with anastomotic leakages, this severe complication was associated with even a better short-term survival than in those without such a complication. Obviously, the many strong confounders confined also to the upfront surgical strategy burden the current review. Regarding this management strategy, we again were unable to differentiate the outcomes after iatrogenic perforation—spontaneous esophageal rupture as separated from those with leaking esophageal anastomoses. Given these ambiguities, we can still conclude that the overall post procedural in-hospital mortality is at least double that following the SEMS-based therapeutic concept. This was true despite the fact that the majority of surgical explorations contained attempts to perform minor organ preserving procedure such a repair of the defect or insertion of a T tube. Another point of importance is the reported 85% success rates after surgical approaches, which can be looked upon as incompatible with the high in hospital mortality. A high overall mortality may in these situations be strongly influenced by factors that were not identifiable as related to ‘treatment failure’ rates as such, within the current stringent analysis of the outcomes. Another factor, which always confounds corresponding figures, is the selection of patients for respective procedures. Many of the institutions that present their experiences from the management of iatrogenic perforation—spontaneous esophageal rupture as well as leaking esophageal anastomoses, are high-volume esophageal surgical centers that receive a number of transfers of patients, who have been monitored and treated in peripheral hospitals with drainage, stenting, or even attempted repairs for esophageal injuries, usually without success.
In conclusion, this review of the current literature shows that a SEMS-based therapy, can be successfully applied as a therapeutic strategy in esophageal perforation rupture. However, if more than two days have passed between the injury and the initiation of therapy, there is a high risk of failure. It is possible that cardiovascular comorbidity may be an additional risk factor for failure and defects in the middle-lower third esophagus may have a better chance to heal compared to lesions that straddle the gastroesophageal junction. Regardless of these circumstances, the management of esophageal perforation-rupture defects with stents requires an individualized treatment including vigorous endoscopic reinterventions if the leakage persists and pleural-mediastinal minimal invasive drainage procedures. Another conclusion from this literature review is that SEMS is justified and can be applied upfront in esophagogastric and esophagojejunal anastomotic leakages as part of a carefully processed treatment strategy. Treatment failure has to be vigorously searched for and the main risk factors are continued leakage from the anastomosis, high age, and severe comorbidity and the development of airway fistulation. If these situations are prevailing and/or emerging in a patient with preoperative low physical capacity, then aggressive therapeutic alternatives have to be promptly instituted.
References
Author notes
Specific author contribution: Study conception and design: Person S, Rouvelas I, Irino T, Lundell L; Data acquisition: Person S, Rouvelas I, Irino T, Lundell L; Analysis and data interpretation:
Person S, Rouvelas I, Irino T, Lundell L; Drafting of the manuscript: Person S, Rouvelas I, Irino T, Lundell L; Critical revision: Person S, Rouvelas I, Irino T, Lundell L.