-
PDF
- Split View
-
Views
-
Cite
Cite
Peter Downey, William Middlesworth, Matthew Bacchetta, Joshua Sonett, Recurrent and congenital tracheoesophageal fistula in adults, European Journal of Cardio-Thoracic Surgery, Volume 52, Issue 6, December 2017, Pages 1218–1222, https://doi.org/10.1093/ejcts/ezx164
Close - Share Icon Share
Abstract
Recurrent congenital tracheoesophageal fistula (TEF) is well documented in infancy but may also present later in life. This study reviews our experience with the clinical presentation, diagnosis and management of 5 recurrent and 2 primary congenital tracheoesophageal fistulas (TEF) in adult patients. There are no literature series of late recurrence of TEF (repaired in childhood and recurring in adulthood) and relatively few reported cases of initial adult presentation of TEF. In this series, we aim to provide the first large series description of late recurrence of congenital TEF following repair in infancy or childhood. We also present management considerations for this unique group of patients.
We performed a computer-based search of the adult thoracic surgery departmental operative database at our institution from 2002 to 2014. Patients with iatrogenic TEF or malignant TEF were excluded.
Seven patients are included in our series. Five patients (71%) had recurrent congenital TEF and 2 (29%) had initial diagnosis of congenital TEF. All presented with severe coughing symptoms, and most (86%) had a history of recurrent aspiration pneumonia. Repair technique was dictated by the location of the TEF and the specific tracheoesophageal pathology. Four patients underwent repair via cervical approach with or without a tracheal resection. Three patients with distal recurrence underwent repair via right thoracotomy with partial oesophagectomy for significant tissue compromise and cervical reconstruction. Patients were followed for at least 1 year. All 7 patients experienced full resolution of symptoms. One patient required postoperative placement of a retrievable tracheal stent for tracheomalacia. There were no mortalities.
Adult presentation of congenital TEF is a rare but recognizable clinical entity. Recurrent TEF in adulthood is a possible late complication of TEF repair performed in childhood that has not previously been described. Adult patients experiencing symptoms of cough and recurrent aspiration pneumonia should be evaluated for congenital TEF. Surgical repair of congenital TEF in the adult is feasible and effective with acceptable morbidity.
INTRODUCTION
Benign congenital tracheoesophageal fistula (TEF) is a common surgical problem that can occur independently or as a combined anomaly with oesophageal atresia. Congenital TEF affects approximately 1 in 4100 individuals [1]. Although most often diagnosed at the time of birth, TEF can also very rarely present in adults, but literature on this topic is limited to case reports and small case series [2–10]. TEF recurrence in the adult population after neonatal repair has not yet been described in the form of a case series.
BACKGROUND
Tracheoesophageal fistula frequently occurs in the setting of other congenital anomalies, most notably oesophageal atresia, as part of the VACTERL/VATER association [11, 12]. Early recurrent congenital TEF after surgical repair is a well-described complication, occurring in approximately 9% of patients who have undergone repair [13]. Recurrence typically occurs in the very early postoperative period but has been reported up to 18 months following initial repair [14]. Late recurrence in the adult population has never been described in the medical literature. This report describes our experience with the management of congenital, benign TEF in the adult population and defines this as a distinct postoperative complication. This population requires unique consideration given the chronicity of their disease and the variable anatomy.
METHODS
We performed a computer-based search of the adult thoracic surgery departmental operative database at our institution from 2002 to 2014. Patients with iatrogenic or malignant TEF were excluded. Over this time, we identified 7 adult patients who were managed for benign initial or recurrent congenital TEF (Table 1). The age of presentation ranged from 15–65 years old (mean age: 38 ± 27 years).
Patient characteristics
| Patient . | Aetiology . | Age at initial repair . | Age at presentation . | Diagnostic study . | Surgical approach . | Tracheal management . | Fistula outcome . | Complications . |
|---|---|---|---|---|---|---|---|---|
| 1 | Congenital | 15 | – | Oesophagram | Cervical | Primary repair | Closed | – |
| 2 | Congenital | 65 | – | Bronchoscopy | Cervical | 1-ring rsxn | Closed | – |
| 3 | Recurrent | Infant | 22 | Chest CT | Cervical | 3-ring rsxn | Closed | – |
| 4 | Recurrent | Infant | 35 | Bronchoscopy | Cervical | 1-ring rsxn | Closed | Granulation tissue |
| 5 | Recurrent | Infant | 36 | Oesophagram | Thoracotomy | Primary repair | Closed | Thoracic duct leak |
| 6 | Recurrent | Infant | 40 | Oesophagram | Thoracotomy | Primary repair | Closed | – |
| 7 | Recurrent | Infant | 52 | Bronchoscopy | Thoracotomy | Primary repair | Closed | Tracheomalacia |
| Patient . | Aetiology . | Age at initial repair . | Age at presentation . | Diagnostic study . | Surgical approach . | Tracheal management . | Fistula outcome . | Complications . |
|---|---|---|---|---|---|---|---|---|
| 1 | Congenital | 15 | – | Oesophagram | Cervical | Primary repair | Closed | – |
| 2 | Congenital | 65 | – | Bronchoscopy | Cervical | 1-ring rsxn | Closed | – |
| 3 | Recurrent | Infant | 22 | Chest CT | Cervical | 3-ring rsxn | Closed | – |
| 4 | Recurrent | Infant | 35 | Bronchoscopy | Cervical | 1-ring rsxn | Closed | Granulation tissue |
| 5 | Recurrent | Infant | 36 | Oesophagram | Thoracotomy | Primary repair | Closed | Thoracic duct leak |
| 6 | Recurrent | Infant | 40 | Oesophagram | Thoracotomy | Primary repair | Closed | – |
| 7 | Recurrent | Infant | 52 | Bronchoscopy | Thoracotomy | Primary repair | Closed | Tracheomalacia |
Patient characteristics
| Patient . | Aetiology . | Age at initial repair . | Age at presentation . | Diagnostic study . | Surgical approach . | Tracheal management . | Fistula outcome . | Complications . |
|---|---|---|---|---|---|---|---|---|
| 1 | Congenital | 15 | – | Oesophagram | Cervical | Primary repair | Closed | – |
| 2 | Congenital | 65 | – | Bronchoscopy | Cervical | 1-ring rsxn | Closed | – |
| 3 | Recurrent | Infant | 22 | Chest CT | Cervical | 3-ring rsxn | Closed | – |
| 4 | Recurrent | Infant | 35 | Bronchoscopy | Cervical | 1-ring rsxn | Closed | Granulation tissue |
| 5 | Recurrent | Infant | 36 | Oesophagram | Thoracotomy | Primary repair | Closed | Thoracic duct leak |
| 6 | Recurrent | Infant | 40 | Oesophagram | Thoracotomy | Primary repair | Closed | – |
| 7 | Recurrent | Infant | 52 | Bronchoscopy | Thoracotomy | Primary repair | Closed | Tracheomalacia |
| Patient . | Aetiology . | Age at initial repair . | Age at presentation . | Diagnostic study . | Surgical approach . | Tracheal management . | Fistula outcome . | Complications . |
|---|---|---|---|---|---|---|---|---|
| 1 | Congenital | 15 | – | Oesophagram | Cervical | Primary repair | Closed | – |
| 2 | Congenital | 65 | – | Bronchoscopy | Cervical | 1-ring rsxn | Closed | – |
| 3 | Recurrent | Infant | 22 | Chest CT | Cervical | 3-ring rsxn | Closed | – |
| 4 | Recurrent | Infant | 35 | Bronchoscopy | Cervical | 1-ring rsxn | Closed | Granulation tissue |
| 5 | Recurrent | Infant | 36 | Oesophagram | Thoracotomy | Primary repair | Closed | Thoracic duct leak |
| 6 | Recurrent | Infant | 40 | Oesophagram | Thoracotomy | Primary repair | Closed | – |
| 7 | Recurrent | Infant | 52 | Bronchoscopy | Thoracotomy | Primary repair | Closed | Tracheomalacia |
RESULTS
Patient characteristics
Within this series, 2 patients were treated for a new diagnosis of congenital TEF and 5 patients had recurrent TEF following repair at birth. All patients in this series presented with chronic cough and symptoms of aspiration. Six of the 7 patients presented with pneumonia as confirmed by chest X-ray and clinical findings. After obtaining extensive history, none of the patients included in our series showed evidence of malignancy, trauma, intubation or foreign body ingestion that would explain the development of TEF.
To establish diagnosis and characterize the nature of the disease, all patients underwent computed tomography of the chest, oesophagram, oesophagogastroduodenoscopy and bronchoscopy. On exploration, all patients were confirmed to have either initial (2/7) or recurrent (5/7) H-type TEF.
Recurrent tracheoesophageal fistula patients
The 5 adult patients who were treated for recurrent congenital TEF warrant special consideration. All patients underwent initial congenital repair as infants at separate institutions. Initial repair technique involved concomitant repair or reconstruction of oesophageal atresia. One patient experienced significant anastomotic complications during initial repair. Unfortunately, due to the distant timing of the paediatric repair and lack of electronic medical record at that time, original operative reports are not available for these patients. Based on patients’ personal records and physical exam findings, we are able to conclude that all 5 patients underwent repair via right thoracotomy. None of the patients had undergone repair by our group.
Symptom onset varied among patients. With the exception of 1 patient who was diagnosed 5 days after the onset of recurrent symptoms, there was relative delay in diagnosis of the TEF following the onset of symptoms. The patient who was diagnosed most rapidly had experienced multiple initial complications of his infant repair and there was a high index of suspicion for recurrence. Three of the other 4 patients had effectively lived with significant coughing that had not been identified as a potential complication of the prior intervention.
Multiple diagnostic methods were utilized in these patients. Two patients were diagnosed radiographically with a thinned barium oesophagram. Two other patients with significant lung scarring on preoperative chest radiography failed to demonstrate a fistula on oesophgagram. Due to the severity and persistence of symptoms, oesophagoscopy and bronchoscopy were performed which demonstrated the fistulae. Another patient was diagnosed on computed tomography of the chest after an aspiration event. The anatomical detail of the TEF was confirmed on oesophagoscopy and bronchoscopy.
Characteristics of patients with recurrent tracheoesophageal fistula
Patient 3 (Table 1) was repaired at age 1 via colonic interposition for long-segment oesophageal atresia after creation of a gastrostomy and oesophagostomy at birth. His initial procedure required 2 revisions during the immediate postoperative course for a leak at the proximal anastomosis. He progressed well until the age of 7 when he developed a recurrence requiring a second anastomotic resection and revision. He again improved until age 22 when he developed pneumonia and was diagnosed with recurrence. Additional studies confirmed recurrence secondary to a stricture at his proximal oesophagocolonic anastomosis. He was repaired via a cervical incision with 3-ring tracheal resection and resection and revision of his oesophagocolonic anastomosis.
Patient 4 presented to our practice after 7 years of moderately controlled but steadily worsening asthma. She was diagnosed with recurrent small, proximal TEF via bronchoscopy after persistence of symptoms despite a normal thinned barium oesophagram. She was repaired via a cervical incision with 1-ring tracheal resection. Whereas the full duration of her recurrent TEF is unknown, it is possible that she developed recurrence at a much younger age given the duration of symptoms. The small size of her TEF and otherwise overall excellent health are thought to account for her prolonged compensation.
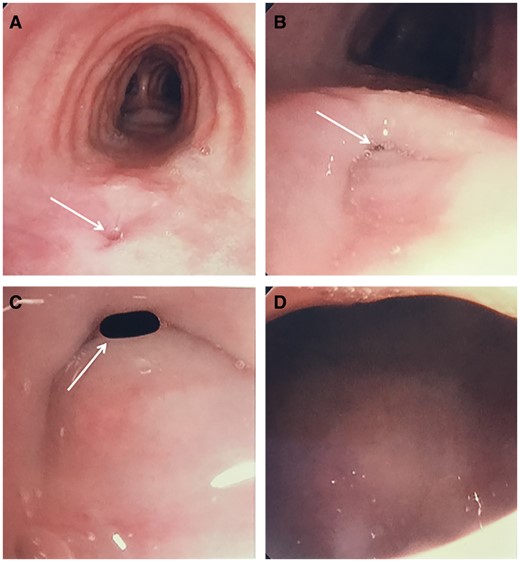
Patient 5 was repaired at birth and had done well until age 36 when she developed severe pneumonia over the course of 1 month. Diagnosis was suggested by thinned barium oesophagram, which demonstrated proximal oesophageal dilation, distal tapering and passage of contrast into the tracheobronchial tree. She underwent bronchoscopy (Fig. 1), which confirmed a recurrent TEF. Following diagnosis, a percutaneous endoscopic gastrostomy tube was placed for enteral feeling while she was treated with a course of intravenous antibiotics for severe pneumonia. Due to distal oesophageal location of her fistula, she was repaired via a thoracic approach. She required an oesophagectomy due to poor quality of the oesophageal tissue following dissection. The nature of her recurrence was thought to be secondary to a relative high-pressure zone within the oesophagus at a point of tapering at the level of her primary repair.
Preoperative bronchoscopy for Patient 5. Bronchoscopy demonstrated a mid-tracheal mucosal defect in the membranous trachea (arrow) (A). High magnification bronchoscopy of the membranous trachea further demonstrated the defect (arrow) (B). Bronchoscopic advancement to the area of the defect begins to highlight the TEF (arrow) (C). Further advancement to the area of concern allows direct visualization of the oesophageal lumen from the trachea and confirms the presence of TEF (D).
Patient 6 had required a third rib resection as part of her infant procedure. At age 35, this patient was diagnosed with a recurrence in the chest after 3 months of worsening respiratory symptoms and pneumonia. Oesophagram revealed recurrence of her TEF in the mid-oesophagus with abrupt transition in caliber just proximal to the fistula. She was repaired via thoracotomy, requiring re-entry through the previous operative field. The post-dissection oesophageal tissue quality was deemed unsatisfactory for primary repair and she underwent oesophagectomy. A stricture was identified at the site of the prior repair and was thought to contribute to the recurrence.
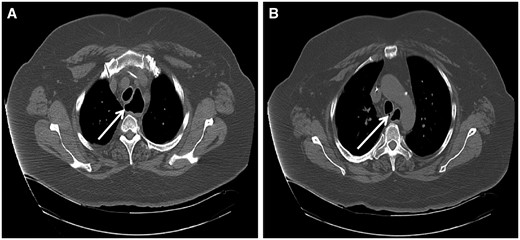
Patient 7 presented with a long-standing smoking history and non-ischaemic cardiomyopathy with left ventricular ejection fraction of 20% and moderately reduced right ventricular function. She developed TEF recurrence at age 52 following infant repair. Due to her comorbidities, she was initially managed with an oesophageal stent at an outside institution. She ultimately required TEF repair with oesophagectomy for persistence of the fistula and worsening respiratory symptoms. On chest CT and in the operating room, she was found to have clear oesophageal dilation proximal to the recurrent TEF (Fig. 2A) with a stricture at the site of prior repair, likely contributing to her recurrence.
Chest computed tomography for Patient 7. Selected images demonstrate proximal oesophageal dilation (arrow) (A) with distal recurrent congenital tracheoesophageal fistula (arrow) (B).
Operative intervention
In our series of 7 total patients, surgical repair was performed via a cervical incision in 4 patients (2 recurrent and 2 primary) and thoracotomy in 3 patients with recurrent TEF. The 4 patients repaired via cervical incision had a proximal fistula with normal oesophageal function as interpreted on barium oesophagram. In this group, the trachea was repaired either primarily or by tracheal ring resection, and the oesophageal defect was repaired primarily. One patient required splitting of the manubrium to achieve adequate exposure for the repair. The tracheal repair or anastomosis was completed using 3–0 Maxon™ absorbable suture. In each patient, a tissue flap of either a strap muscle or the sternocleidomastoid muscle was released and used to protect the repair. All 4 of these patients had a nasoduodenal feeding tube placed prior to leaving the operating room.
The 3 patients who underwent right thoracotomy with primary repair of the trachea required total oesophageal resection. In these 3 patients, pre-operative upper endoscopy demonstrated a patulous proximal oesophageal segment. Pre-operative bronchoscopy also demonstrated relatively distal fistulae. In all patients, the operative procedure was undertaken with the goal of oesophageal preservation and maintenance of present anatomy if tissue quality would allow. In order to isolate the recurrent TEF, all 3 patients required extensive dissection with intense adhesiolysis due to prior surgical intervention in the operative field. Following dissection, intraoperative examination revealed dilated, attenuated oesophageal tissue that had been significantly devitalized. The decision to perform oesophagectomy was then made intraoperatively out of concern for increased risk of recurrence as a result of relative tissue ischaemia.
Surgical technique was total oesophageal resection via either open or laparoscopic-assisted 3-hole approach with a gastric pull-through. In all patients, an intercostal muscle flap was used to protect the repair and a feeding jejunostomy tube was placed.
Postoperative outcomes
One patient remained intubated for 1 night following the procedure out of concern for laryngeal oedema, but she was extubated the following day. All other patients were extubated in the operating room. One patient (Table 1, Patient 5) who underwent oesophagectomy developed a thoracic duct leak and required operative thoracic duct ligation on post-operative Day 2. Additional immediate postoperative management included antibiotics as clinically indicated for preoperative pneumonia and proton pump inhibitor therapy. A thinned-barium oesophagram was performed 1–2 weeks post-operatively, prior to initiation of oral feeding. No patients showed evidence of recurrent TEF or oesophageal leak. All patients were discharged on enteral feeding regimens with 4 patients tolerating oral diets without tube feeding.
In follow-up at 2–3 weeks, 5 patients were tolerating a regular diet with no symptoms of reflux or recurrent fistula. These patients have had no further complications. One patient required placement of a tracheal stent at 4 months post-operatively for severe tracheomalacia (Table 1, Patient 7). This was thought to be secondary to her initial dissection being significantly challenging and requiring a muscle flap over the posterior trachea at the time of the initial repair. She continues to be monitored every 6 months for stent position adjustment. One other patient underwent bronchoscopy at 3 months postoperatively during which time a small amount of granulation tissue was cauterized at the site of the repair, but she had no evidence of recurrent fistula (Table 1, Patient 4).
DISCUSSION
The vast majority of congenital TEF are diagnosed and repaired at the time of birth. Early recurrence after initial repair in the neonatal period is well documented. In a search of the current literature, no large case series were found of adult recurrent congenital TEF after neonatal repair. Late presentation of congenital TEF in adults is well documented but overall an uncommon disease. We could identify approximately 21 unique cases reported, although early literature and our experience suggest an increased incidence [2–10]. Additionally, late presentation of a second, distinct, congenital H-type TEF after repair of a separate TEF in the same patient has been described [15]. Although not seen in our series, this disease manifestation should also be considered as these patients undergo diagnostic evaluation.
All patients in our series presented with chronic cough, aspiration events, and debilitating recurrent pneumonia requiring hospital admissions. Symptoms of reflux are also common. There were no major identifiable clinical differences in the presentation of recurrent versus initial adult congenital TEF. On detailed history, 1 patient with long-standing symptoms admitted to having developed a compensating swallowing mechanism by which to keep from grossly aspirating. One hypothesis to explain the prolonged duration of symptoms in adult presentation of TEF has been attributed to gradual reduction in tone of the LES allowing for progressive worsening of tracheal contamination over time [4]. We observe that some have long attributed chronic respiratory symptoms in adults who have undergone neonatal repair to increased pulmonary reactivity from soilage during development, but these symptoms may in fact be evidence of recurrent TEF.
Various imaging and diagnostic modalities can be used to document the presence of a TEF in the adult. Computed tomography may be suggestive of a TEF if a dilated proximal oesophagus is identified (Fig. 2A) or it the fistula itself is identified (Fig. 2B). Bronchoscopy is helpful in identifying the location of the fistula for appropriate surgical access (Fig. 1).
For each repair, we used either a cervical or thoracic approach based on fistula anatomy and interpretation of oesophageal function. A cervical incision may be used for patients with a proximal fistula and normal oesophageal function. The thoracic approach is used for a distal TEF and when the oesophageal function is particularly questionable. Additional minimally invasive closure techniques have also been reported with some success. Tracheal or oesophageal stents have been shown to allow fistula closure but are associated with significant morbidity [16–18]. One group has reported successful durable closure of a recurrent TEF with an atrial septal defect occluder device [19]. Full closure of the defect in this case report was observed immediately post-procedure and partial epithelialization was observed as early as 3 months after intervention. One possible explanation for the observed association of significant oesophageal dysfunction with distal TEF requiring thoracic repair is that the initial fistula or repair may have resulted in an area of oesophageal narrowing, thereby creating a proximal high-pressure oesophageal segment which could lead to oesophageal dilation, dysfunction and recurrence or exacerbation of the fistula.
Following repair in our group, 1 patient required multiple bronchoscopic interventions for tracheomalacia, and 1 patient required bronchoscopic cauterization of granulation tissue at the repair site. Our findings highlight the importance of maintaining a high index of suspicion for recurrence in patients who have undergone prior TEF repair, regardless of the duration of time since the initial repair. This condition is highly treatable, and if the diagnosis is established prior to irreversible pulmonary changes, most patients will experience significant functional improvement. Oesophagectomy was well tolerated in the 3 patients in our series with distal recurrent TEF requiring thoracic repair.
REFERENCES
Author notes
Presented at the 24th European Conference on General Thoracic Surgery, Naples, Italy, 29 May – 1 June 2016.
- stents
- aspiration pneumonia
- cough
- adult
- child
- computers
- esophagectomy
- objective (goal)
- infant
- reconstructive surgical procedures
- surgical procedures, operative
- thoracotomy
- tracheoesophageal fistula
- diagnosis
- morbidity
- mortality
- pathology
- thoracic surgery procedures
- trachea
- tracheomalacia
- tracheal resection