-
PDF
- Split View
-
Views
-
Cite
Cite
Farhan Bazargani, Anders Magnuson, Björn Ludwig, Effects on nasal airflow and resistance using two different RME appliances: a randomized controlled trial, European Journal of Orthodontics, Volume 40, Issue 3, June 2018, Pages 281–284, https://doi.org/10.1093/ejo/cjx081
Close - Share Icon Share
Summary
To evaluate and compare the effects of tooth-borne (TB) and tooth-bone-borne (TBB) rapid maxillary expansion (RME) on nasal airflow and resistance.
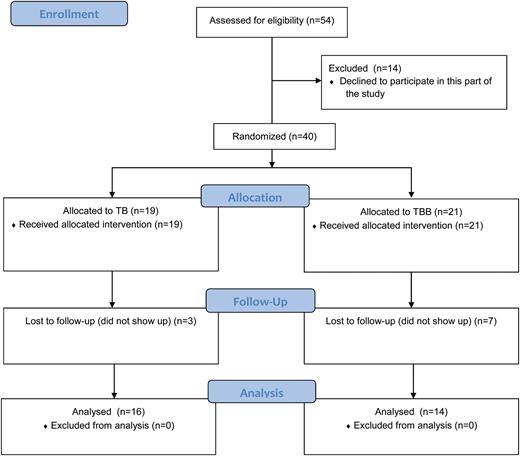
Fifty-four consecutive patients who met the eligibility criteria were recruited from September 2010 to December 2015. Of these 54 subjects, 40 agreed to participate in the part of the study involving evaluation of nasal flow and resistance. The 40 subjects were allocated to either the TB group, mean age 9.7 years (SD 1.5), or the TBB group, mean age 10.2 years (SD 1.4). All subjects performed rhinomanometric registration at baseline (T0), but only 30 attended the post-expansion registration (T1), of whom 16 had been randomized to the TB group and 14 to the TBB group. The study outcomes, nasal airflow and nasal airway resistance, were evaluated with linear regression adjusted for baseline variable of the outcome to compare the study groups with complete cases strategy as well as after multiple imputation (MI).
Participants were randomly allocated in blocks of different sizes, using the concealed allocation principle in a 1:1 ratio. The randomization list was computer generated to ensure homogeneity between groups.
Blinding was done only for outcome assessor due to clinical limitations. The care providers at the ENT unit who conducted all the rhinomanometry examinations were blinded to which group the patients were allocated to.
Complete case analysis showed significantly higher post-expansion nasal airflow values for the TBB group compared with the TB group, mean difference 51.0 cm3/s (P = 0.018). The evaluation after MI showed a similar significant mean difference, 52.7 cm3/s (P = 0.020) in favour of the TBB group when taking into account the missing values from the T1 examination. Even reduction in nasal airway resistance showed similar pattern in favour of the TBB group.
Our results represent the short-term effects. A longer follow-up period would have been preferable.
The TBB RME induced significantly higher nasal airway flow and lower nasal resistance values than TB RME. It might be wiser to use TBB RME in cases with constricted maxilla and upper airway obstruction.
This trial was not registered in any external sites.
The protocol was not published before trial commencement.
Introduction
When a skeletal constricted maxillary arch is diagnosed in adolescents, orthopedic skeletal expansion involving separation of the midpalatal suture is the treatment of choice (1). Various orthodontic appliances and treatment protocols have been developed, and the most common is rapid maxillary expansion (RME).
The maxillary bones form approximately 50 per cent of the nasal cavity’s anatomic structure. Therefore, treatment modalities that alter the morphology of the maxillary dental arch, such as RME, can affect the geometry and function of the nasal cavity (2). It has been reported that RME separates the external walls of the nasal cavity laterally and causes lowering of the palatal vault and straightening of the nasal septum. This remodelling increases nasal volume, decreases nasal resistance, increases nasal airflow, and improves breathing (3–6). However, long-term effects of RME on the nasal cavity and on alleviating breathing are indeterminate.
The original RME design, so-called tooth-borne (TB) RME, is tooth anchored. In recent years, an alternative to TB RME has been introduced. The new hybrid design anchors the RME appliance both to the posterior teeth and also, by means of two mini-implants, directly to the palatal surfaces of the maxilla. Bone-anchored expanders are intended to apply forces directly to the maxilla. In this way, one could possibly reduce the side effects of the original design by means of dental and alveolar bone tipping. The effects of the hybrid, also called tooth-bone-borne (TBB) RME, on the nasal airflow and nasal resistance have not yet been studied.
Thus, the aim of this randomized controlled trial was to assess and compare the influence of the conventional TB RME and TBB RME on nasal airflow and nasal resistance in growing children with constricted maxilla.
Materials and methods
The regional ethical review board in Uppsala, Sweden, which follows the guidelines of the Declaration of Helsinki, approved the study protocol (Dnr: 2009/334). After receiving oral and written information about the clinical trial, both the patients and their parents/guardians signed informed consents.
Fifty-four consecutive subjects examined at the Postgraduate Dental Education Centre, Department of Orthodontics, Region Örebro County, Sweden, who met the eligibility criteria, were recruited from September 2010 to December 2015. Of these 54 subjects, 40 agreed to participate in the part of the study involving evaluation of nasal flow and resistance, which meant two additional visits to the ENT unit at the Örebro University Hospital.
The following inclusion criteria had to be fulfiled by all participants enroled in the study:
uni- or bilateral crossbite with constricted maxilla and
age at diagnosis of 8–13 years, with dental stage in the early or late mixed dentition
Patients with previous or ongoing orthodontic treatment, craniofacial syndromes, or cleft lip or palate were considered ineligible for the study.
Study casts were taken pre- and post-expansion from all subjects. Almost all subjects had an Angle class I occlusion except one subject in the TB group and two subjects in the TBB group, which had Angle class II molar relationships and slightly larger overjet (range 3 to 4.5 mm).
All 40 subjects were referred to the ENT unit for rhinomanometric measurements (Rhinostream®, Interacoustics, Assens, Denmark) at baseline (T0) and directly post-expansion (T1), 15 min after nasal decongestion (xylomethazoline). Nasal airflow and nasal airway resistance were assessed for each nasal cavity separately, while a reference pressure (150 Pa) was measured for the contralateral nostril.
Participants were randomly allocated in blocks of different sizes, using the concealed allocation principle in a 1:1 ratio, to two groups, a TB group and a TBB group. The randomization procedure was as follows: a computer-generated randomization list was created using SPSS software (version 17.0; SPSS, Chicago, IL, USA) and stored with a research secretary at the Postgraduate Dental Education Centre. Each time a patient gave his/her consent, the secretary was contacted by e-mail to provide the information about which type of expander the patient should receive. After informed consent was obtained from both patients and their parents/guardians, the patients were randomized into two groups: Group A was treated with a TB expander (Figure 1a), and Group B was treated with a TBB expander with two 1.7 × 8 mm mini-screw implants (Orthoeasy®; Forestadent, Pforzheim, Germany) attaching the expander to the palate surface (Figure 1b).
Both expanders were activated two-quarter turns per day (0.5 mm) until the palatal cusps of the maxillary first molars contacted the buccal cusps of the mandibular first molars. Hence, both groups were overexpanded the same amount and had the same endpoint. All patients in both groups were treated by the same orthodontist (F.B.).
The intermolar distances pre- and post-expansion were evaluated on study casts at the shortest intermolar linear distance at the gingival margins and the mesiobuccal cusp tips of the teeth, using a digital caliper (Digital 6, Mauser, Winterhur, Switzerland). The intermolar measurements were blinded; the examiner was unaware of which treatment the patients had received or which models were taken at pre- and post-expansion.
The care providers at the ENT unit who conducted all the rhinomanometry examinations were blinded to which group the patients were allocated to. The ENT examination was performed without any intraoral examination. Thus, the examination protocol was blinded and marked with a consecutive number according to the order in which patients were included in the study.
Statistical analysis
The study outcomes, nasal airflow and nasal airway resistance, were evaluated with linear regression adjusted for baseline variable of the outcome to compare the study groups, TB RME and TBB RME. The evaluation was done with complete cases, but also, due to missing values of post measurements of nasal airflow and resistance, with multiple imputation (MI) technique implemented in STATA (version 14, StataCorp LLC, Texas, USA), which is based on the concept of Rubin (7). Baseline variables of outcome, age, sex, and study group were used as predictors in the imputation model. The normality assumptions were checked with Shapiro-Wilk test on the regressions residuals, and as the outcome resistance showed violation of the normality assumption, it was also evaluated on logarithm scale and presented with mean ratios with 95 per cent confidence intervals (CI) as association measures. A mean ratio of 1 is interpreted as no associations, and a mean ratio of 0.5 is interpreted as a 50 per cent lower mean level in one study group compared with the other. The difference between TB and TBB groups mean expansion was calculated with Independent t-test. P < 0.05 was regarded as statistically significant, and all statistical calculations were performed with SPSS, version 22, or STATA.
Results
The 40 subjects were allocated to either the TB group, mean age 9.7 years (SD 1.5), consisting of 11 boys and 8 girls, or the TBB group, mean age 10.2 years (SD 1.4), consisting of 10 boys and 11 girls.
The mean expansion in the TB group was 4.80 mm (SD ± 1.39) and in the TBB group was 5.48 mm (SD ± 0.98). This difference between the groups was not statistically significant (P = 0.061).
All subjects performed rhinomanometric registration at T0, but only 30 showed up at T1 for the post-expansion registration, of whom 16 had been randomized to the TB and 14 to the TBB group (Figure 2).
Complete case analysis showed significantly higher post-expansion nasal airflow values for the TBB group compared with the TB group, mean difference 51.0 cm3/s (P = 0.018). The evaluation after MI showed a similar significant mean difference, 52.7 cm3/s (P = 0.020) in favour of the TBB group when taking into account the missing values from the T1 examination (Table 1).
Comparison of nasal flow and resistance between tooth-bone-borne (TBB) and tooth-borne rapid maxillay expansion (TB RME) groups. Complete case and multiple imputation analysis.
| . | Baseline . | Post . | TBB versus TB . | TBB versus TB . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | All patients . | Complete cases . | Complete cases . | Complete cases . | Multiple imputation . | |||||
| . | n . | Mean (SD) . | n . | Mean (SD) . | n . | Mean (SD) . | Mean difference (95% CI) . | P . | Mean difference (95% CI) . | P . |
| Nasal airflow | ||||||||||
| TBB | 21 | 188.5 (54.7) | 14 | 185.2 (65.7) | 14 | 243.9 (91.4) | 51.0 (9.6 to 92.5) | 0.018 | 52.7 (9.0 to 96.4) | 0.020 |
| TB | 19 | 181.0 (49.6) | 16 | 178.0 (51.6) | 16 | 186.2 (60.3) | ||||
| Nasal resistance | ||||||||||
| TBB | 21 | 0.88 (0.36) | 14 | 0.91 (0.43) | 14 | 0.66 (0.22) | −0.21 (−0.39 to −0.04) 0.77 (0.64 to 0.92) a | 0.016 0.005a | −0.20 (−0.38 to −0.02) 0.78 (0.65 to 0.94) a | 0.028 0.011a |
| TB | 19 | 0.94 (0.38) | 16 | 0.97 (0.40) | 16 | 0.89 (0.32) | ||||
| . | Baseline . | Post . | TBB versus TB . | TBB versus TB . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | All patients . | Complete cases . | Complete cases . | Complete cases . | Multiple imputation . | |||||
| . | n . | Mean (SD) . | n . | Mean (SD) . | n . | Mean (SD) . | Mean difference (95% CI) . | P . | Mean difference (95% CI) . | P . |
| Nasal airflow | ||||||||||
| TBB | 21 | 188.5 (54.7) | 14 | 185.2 (65.7) | 14 | 243.9 (91.4) | 51.0 (9.6 to 92.5) | 0.018 | 52.7 (9.0 to 96.4) | 0.020 |
| TB | 19 | 181.0 (49.6) | 16 | 178.0 (51.6) | 16 | 186.2 (60.3) | ||||
| Nasal resistance | ||||||||||
| TBB | 21 | 0.88 (0.36) | 14 | 0.91 (0.43) | 14 | 0.66 (0.22) | −0.21 (−0.39 to −0.04) 0.77 (0.64 to 0.92) a | 0.016 0.005a | −0.20 (−0.38 to −0.02) 0.78 (0.65 to 0.94) a | 0.028 0.011a |
| TB | 19 | 0.94 (0.38) | 16 | 0.97 (0.40) | 16 | 0.89 (0.32) | ||||
P < 0.05 are considered significant.
aEvaluated on log scale due to violation of normality assumption and the association measure are expressed as mean ratio with 95% CI.
Comparison of nasal flow and resistance between tooth-bone-borne (TBB) and tooth-borne rapid maxillay expansion (TB RME) groups. Complete case and multiple imputation analysis.
| . | Baseline . | Post . | TBB versus TB . | TBB versus TB . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | All patients . | Complete cases . | Complete cases . | Complete cases . | Multiple imputation . | |||||
| . | n . | Mean (SD) . | n . | Mean (SD) . | n . | Mean (SD) . | Mean difference (95% CI) . | P . | Mean difference (95% CI) . | P . |
| Nasal airflow | ||||||||||
| TBB | 21 | 188.5 (54.7) | 14 | 185.2 (65.7) | 14 | 243.9 (91.4) | 51.0 (9.6 to 92.5) | 0.018 | 52.7 (9.0 to 96.4) | 0.020 |
| TB | 19 | 181.0 (49.6) | 16 | 178.0 (51.6) | 16 | 186.2 (60.3) | ||||
| Nasal resistance | ||||||||||
| TBB | 21 | 0.88 (0.36) | 14 | 0.91 (0.43) | 14 | 0.66 (0.22) | −0.21 (−0.39 to −0.04) 0.77 (0.64 to 0.92) a | 0.016 0.005a | −0.20 (−0.38 to −0.02) 0.78 (0.65 to 0.94) a | 0.028 0.011a |
| TB | 19 | 0.94 (0.38) | 16 | 0.97 (0.40) | 16 | 0.89 (0.32) | ||||
| . | Baseline . | Post . | TBB versus TB . | TBB versus TB . | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| . | All patients . | Complete cases . | Complete cases . | Complete cases . | Multiple imputation . | |||||
| . | n . | Mean (SD) . | n . | Mean (SD) . | n . | Mean (SD) . | Mean difference (95% CI) . | P . | Mean difference (95% CI) . | P . |
| Nasal airflow | ||||||||||
| TBB | 21 | 188.5 (54.7) | 14 | 185.2 (65.7) | 14 | 243.9 (91.4) | 51.0 (9.6 to 92.5) | 0.018 | 52.7 (9.0 to 96.4) | 0.020 |
| TB | 19 | 181.0 (49.6) | 16 | 178.0 (51.6) | 16 | 186.2 (60.3) | ||||
| Nasal resistance | ||||||||||
| TBB | 21 | 0.88 (0.36) | 14 | 0.91 (0.43) | 14 | 0.66 (0.22) | −0.21 (−0.39 to −0.04) 0.77 (0.64 to 0.92) a | 0.016 0.005a | −0.20 (−0.38 to −0.02) 0.78 (0.65 to 0.94) a | 0.028 0.011a |
| TB | 19 | 0.94 (0.38) | 16 | 0.97 (0.40) | 16 | 0.89 (0.32) | ||||
P < 0.05 are considered significant.
aEvaluated on log scale due to violation of normality assumption and the association measure are expressed as mean ratio with 95% CI.
Even reduction in nasal airway resistance showed a similar pattern in favour of the TBB group (Table 1). For the complete case analysis, the TBB group had a significantly lower mean than the TB group, a mean difference of −0.21 Pa s/cm3 (P = 0.016) in favour of the TBB group, and was significantly different (P = 0.005) also after log transformation of the outcome variable. The evaluation after MI showed very similar findings.
Discussion
Findings of this prospective randomized controlled trial show that patients with TBB RME induce significantly higher nasal mean flow and lower nasal mean airway resistance after maxillary expansion compared with patients with TB RME. It has been reported in the literature that the mean total nasal resistance in normal subjects after decongestion ranges between 0.15 and 0.5 Pa s/cm3 (8). A reduction of nasal airway resistance by 0.21 Pa s/cm3 shown in this study in favour of TBB could therefore be considered as close to an equivalent to the decongestant effect of a nose spray, which is surely of clinical significance, for instance, in children suffering from nasal airway obstruction.
When assessing nasal patency, the fact that validated normal values are still lacking is a major problem (8). The wide variability of the nasal mucosa, which is influenced by several internal and external factors, makes it very difficult to compare nasal patency between different subjects before decongestion. After decongestion, however, the situation is different. The congested nasal passage can be evaluated based on the influence of the skeleton (8). For this reason, all the values in our study were presented after decongestion.
Rhinomanometry is the most widely used method for pre- and post-operative evaluation of nasal flow and resistance. Zapletal et al. (9) reported normal values in healthy Caucasians children. They found a significant relation to height and age, but not sex, when it came to resistance values. In our sample, both groups were quite homogeneous in regard to age and sex. Height of the subjects was, unfortunately, not measured.
The different effects on nasal airflow and resistance between the two RME appliances could be a question of design and their efficiency in delivering the force. The appliance design could have an impact on the rate of midpalatal suture opening. If the force induced by expansion screws migrates through the dentition and alveolar bone to reach the midpalatal suture, which is the case in the TB design, it may lose some of its magnitude when it reaches its destination. On the other hand, when an expansion force is directed toward the midpalatal suture directly, which is the case in the TBB design, the whole force is transmitted to the suture. Thus, the rate of the skeletal expansion could be higher in TBB compared with the TB appliances. Gunyuz Toklu et al. (10) conducted a prospective study intended to compare TB RME (n = 13) and TBB RME (n = 12) in a small group of patients. They concluded that both appliances resulted in similar skeletal effects. In their study, the midpalatal suture was not studied. The sample size was calculated on buccal bone loss and not skeletal effects. The spread of the data was rather high, and the subjects were, on average, 4 years older than our sample. So, their conclusion might not be valid when it concerns the skeletal expansion effects in the midpalatal suture.
Strengths and limitations
This study has some limitations. Both groups had attrition. Three subjects in the TB group and seven subjects in the TBB group did not show up for the follow-up rhinomanometry appointments. However, this issue was addressed by an MI model, which is a simulation-based approach for analysing incomplete data with the objective to handle missing data in a way that results in valid statistical inference. These results were very similar to the complete case analyses and support the study findings. One potential limitation is that the variables used for imputation were not good enough. We used the baseline measurement for the outcome as a predictor, and as the Pearson correlation between baseline and post-expansion among the responders was 0.68 for the study outcome nasal airflow, we believe it is a valid approach. The power analysis (not included) was based on skeletal effects of the RME appliances and not on the effect on airways. However, the sample size was large enough to detect statistically significant findings.
Our results represent the short-term effects of the RME treatments. Long-term effects should be studied further.
The design of this prospective study was a randomized clinical trial. The randomization process, in which the patients are randomly assigned in advance, results in a similar distribution of confounding variables between the groups. This reduces the risk of selection bias. Moreover, to further reduce the risk of bias, the ENT unit was blinded to allocation and to which treatment the patients had received.
Clinical implications
When it comes to treating patients with constricted maxilla and upper airway obstruction, it might be wise to use the TBB RME instead of the conventional TB design. This could be more beneficial for the patient.
Generalization
The results of this RCT can be generalized only in a population aged 8–13 years and in the case that the exclusion criteria are met.
Conclusions
The TBB RME induced significantly higher nasal airway flow values than TB RME.
The TBB RME induced significantly lower nasal resistance values than TB RME.
It might be wiser to use TBB RME in cases with constricted maxilla and upper airway obstruction.
Funding
This study was supported by the Uppsala-Örebro Regional Research Council, Sweden, (grant number RFR-72021). The funding sources had no role in design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation of the manuscript. The authors’ work was independent of the funders
Conflict of interest
None to declare.
Acknowledgment
We thank Dr Stig Rudblad and nurse Marie-Louise Eriksson at the ENT unit, Örebro University Hospital, for their assistance with the rhinomanometric examinations.