-
PDF
- Split View
-
Views
-
Cite
Cite
Angelo Bartoletti, Plinio Fabiani, Paolo Adriani, Francesca Baccetti, Luciano Bagnoli, Gianluca Buffini, Carlo Cappelletti, Paolo Cecchini, Roberto Gianni, Alessandro Lavacchi, Pier Francesco Ticali, Giovanni Maria Santoro, Hospital admission of patients referred to the Emergency Department for syncope: a single-hospital prospective study based on the application of the European Society of Cardiology Guidelines on syncope, European Heart Journal, Volume 27, Issue 1, January 2006, Pages 83–88, https://doi.org/10.1093/eurheartj/ehi474
Close - Share Icon Share
Abstract
Aims To evaluate the applicability and the clinical impact of the European Society of Cardiology (ESC) Guidelines' recommendations for hospital admission of patients with syncope in a District Hospital Emergency Department (ED).
Methods and results From September 2002 to August 2004, 1124 patients with syncope [out of 1308 with transient loss of consciousness (TLC)] were evaluated according to the ESC Guidelines. Overall, 566 patients with syncope (50.1%) were admitted and 558 (49.9%) were discharged. Out of the 1124 patients with syncope, 440 (39.1%) presented at least one ESC Guidelines' criterion for hospitalization. Out of the 440, 393 (89.3%) were admitted, whereas 511 out of the 684 (74.7%) without indication for admission were discharged. A significant difference was found between the adherence rates for admission and for discharge (P<0.001). The appropriateness of the ED medical decision was 69.4% for hospital admission and 91.6% for discharge (P<0.001).
Conclusion Although an acceptable ED adherence to the guidelines' indications was attained, better implementation strategies are still advisable. The ESC Guidelines' indications are applicable to the majority of patients entering the ED for a TLC. In addition, when the guidelines' indications are observed, a high percentage of patients with syncope have still to be hospitalized.
See page 7 for the editorial comment on this article (doi:10.1093/eurheartj/ehi626)
Introduction
The indications for hospitalization are recognized as one of the main issues in the management of syncope.1–8 Recently, the European Society of Cardiology (ESC) provided specific guidelines on syncope.9–10 One of the main goals of the ESC Guidelines was to define the best diagnostic strategies for the different subgroups of patients with syncope, including the related indications for hospital admission. Surprisingly, the clinical impact of such indications has not been specifically assessed until now, the only exception being a preliminary study from our group11 which suggested about half of the patients observed at the Emergency Department (ED) for a syncope having at least one indication for hospital admission consistent with those of the ESC Guidelines. However, our study included only a limited number of patients, and basic aspects such as the guidelines' applicability in the ED, the ED adherence to the guidelines, and the appropriateness of the ED medical decision for admission/discharge were not adequately addressed.
Aims of the present study were: to assess the applicability of the ESC Guidelines' indications for hospital admission on a large series of unselected, consecutive patients observed at the ED for a transient loss of consciousness (TLC); to estimate how many patients with syncope present an appropriate indication for hospitalization after a guidelines-based ED initial evaluation; and to evaluate the adherence to the guidelines and the appropriateness of the ED medical decision regarding admission/discharge of patients with syncope.
Methods
General methodology and study population
The Nuovo San Giovanni di Dio (NSGD) is a 390-bed public single District Hospital, provided with an ED working 24 h a day and all the diagnostic tools with potential indication in patients with a TLC. From August 2002, at the NSGD, a Syncope Unit (SU) was in operation as a multidisciplinary team inclusive of the ED. One of the main targets of the SU was the implementation of the ESC Guidelines on syncope since the earliest hospital phase, i.e. the ED observation period. For this purpose, the guidelines were discussed in dedicated clinical meetings, and specific pathways for TLC were prompted, including the monitoring of all the TLC presentations and the related admissions. Only patients observed within 48 h from symptoms were included in the present study.
ED clinical assessment
All the patients observed for a TLC underwent a clinical evaluation made by the ED physician comprehensive of history, physical examination, blood pressure assessment in both clinostatic and orthostatic position, 12-lead ECG, and routine blood examinations. Further diagnostic investigations, as well as specialist consultations, were performed only when clinically indicated. After the evaluation, the ED physician had to express, whenever possible, a diagnostic appraisal for syncope or non-syncopal attack. Notably, although the ESC Guidelines suggest such a diagnosis as the first clinical step for patients with a TLC,9,10,12 no definite criteria are provided for that. According to the local previous clinical practice, restrictive definitions of non-syncopal attack were applied in our hospital. For patients with a true syncope, the specific indications for hospitalization suggested by the ESC Guidelines9–10 had to be followed and reported on a dedicate patient-form. The records were collected twice a week by two investigators (A.B., P.F.), not involved in the decision to admit/discharge the single patients but with the responsibility of reviewing the patients' data and of evaluating the adherence to the guidelines' indications. A 24-month duration of the monitoring period was decided in order to attain a realistic picture of the daily clinical practice in our ED.
Definitions
According to the ESC Guidelines,9,10 syncope was defined as a spontaneous and TLC, usually associated with fall and with spontaneous, quick, and complete recovery as well. The definitions of cardiac syncope, vaso-vagal syncope, situational syncope, and carotid sinus hypersensitivity were those reported in the ESC Guidelines.9,10 Orthostatic syncope was diagnosed in the case of documented orthostatic hypotension13 associated with syncope or pre-syncope. Syncope associated with haemorrhage or anaemia was diagnosed when a major bleeding requiring haemotransfusion was documented. In all the other cases, the syncope was defined as unknown cause.
Secondary trauma was defined as severe in the case of skull or other major bone segments fracture, intracranial haemorrhage, or internal organ lesions requiring urgent, specific treatment. For all these cases, the indication for hospital admission was clearly therapeutic instead of diagnostic. Therefore, although the ESC Guidelines recommend a diagnostic hospitalization in the case of severe trauma, in the present paper, owing to the restrictive definitions adopted by us, the severe trauma was considered among the therapeutic indications for hospital admission.
Orthostatic hypotension was considered as ‘severe’ just when it was expression of an acute haemorrhage or volume loss requiring prompt specific treatment or in the case of neurological dysfunction requiring diagnostic investigation.9,10
Structural heart disease indicated chronic coronary heart disease, cardiomyopathy (dilated or hypertrophic) or valvular disease with documented left ventricular dysfunction and/or obstacled ventricular afflux and/or efflux, and hypertensive heart disease (high blood pressure with left ventricular hypertrophy and/or dysfunction).
Family history for sudden death was defined as the presence of at least one case of sudden death among relatives aged <50 or multiple cases of sudden death among relatives independent of age.14
Syncope relapses were arbitrarily regarded as frequent in the case of at least 10 syncopal episodes in the patient's lifespan, with at least two episodes during the last year.
Hospitalization criteria
The indications for hospitalization were those defined in the ESC Guidelines.9,10
Data evaluation
The total number of the ED presentations during the monitoring period, as well as that of patients observed for a TLC, was acquired. Among these latter, the patients diagnosed as having a true syncope during the ED stay were separated. Subsequently, the number of patients with syncope actually hospitalized was evaluated (‘observed’ hospitalization). In a second phase, in order to estimate the number of patients with syncope who had to be hospitalized according to the ESC Guidelines, the related indications were acquired by the patients' records. Because various indications for admission coexisted in several patients, these were evaluated according to a clinical priority order (therapeutic before diagnostic indications), and for each patient, only the main indication was taken into account (‘calculated’ hospitalization). In a third phase, in order to evaluate the adherence rate to the guidelines in relation to the specific issue of the hospitalization, the number of patients actually hospitalized among those with indication for admission according to the guidelines was verified. Finally, the appropriateness of the ED medical decision to admit was defined by assessing the number of patients with indication for admission according to the ESC Guidelines among those actually hospitalized. For all these specific issues, the ‘decision to admit’ after the ED observation was regarded as characterizing; therefore, also the patients who refused the hospitalization were considered as admitted.
The following comparisons were planned: ED adherence to the ESC Guidelines' indications for admission vs. those for discharge; appropriateness of the ED decision for admission vs. that for discharge; and ED adherence rate to the therapeutic vs. the diagnostic guidelines' indications for admission.
Statistical analysis
Absolute numbers and percentages were reported to describe the patient population. χ2 test was used to compare categoric variables. All tests were two-sided and a P-value less than 0.05 was considered to be statistically significant. The Bonferroni multiple comparisons test was applied to reduce the possibility of type I error. All statistical analyses were performed using SPSS software (version 11.5, SPSS Inc., Chicago, IL, USA).
Results
Between 1 September 2002 and 31 August 2004, 86 590 patients entered our ED. For 1308 of them (1.5%), the cause of presentation was a TLC occurring during the preceding 48 h. Out of these 1308 patients, 131 (10%) were diagnosed as having a non-syncopal attack, whereas for 53 (4.1%), it was not possible to ascertain if a true TLC had happened. The remaining 1124 patients (85.9%) with a true syncope were included in the study.
The median ED observation time, for the 1124 patients with syncope, was 4 h (range 1–24). At the end of the ED stay, hospital admission was proposed to 566 patients (50.1%), whereas the remaining 558 (49.9%) were directly discharged from ED.
Overall, 440 patients out of the 1124 with syncope (39.1%) were found to have at least one indication to hospital admission according to the ESC Guidelines (Figure 1). The indications for hospitalization were (i) for therapeutic purpose in 141 patients (12.5%), of whom 64 with cardiac syncope (Table 1); (ii) for severe comorbidities in 79 (7.1%); (iii) for diagnostic purpose in 170 (15.1%); and (iv) ‘occasional’ hospitalization in 50 (4.4%). The remaining 684 patients with syncope (60.9%) did not meet the ESC Guidelines' criteria for hospitalization.
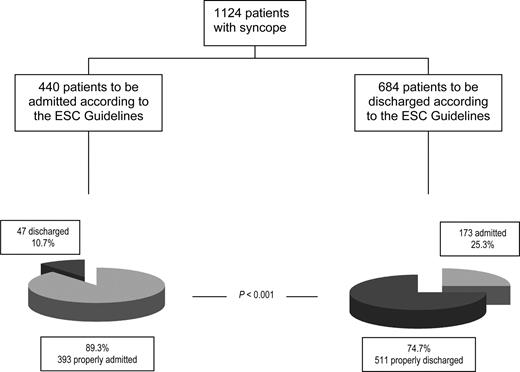
Overall, 393 patients out of the 440 (89.3%) with indication for hospitalization according to the ESC Guidelines were actually admitted, whereas 511 patients out of the 684 (74.7%) without indication for admission were actually discharged from the ED (Figure 2). A significant difference was found between the adherence rate for admission and that for discharge (P<0.001). The adherence rate to the ESC Guidelines, subdivided for each group of indications for hospital admission, is reported in Table 2. The adherence rate regarding therapeutic indications was significantly higher than that related to the diagnostic ones (94.5 vs. 84.1%, P<0.001).
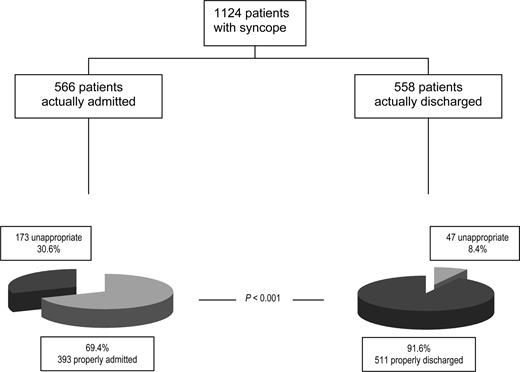
The appropriateness of the ED medical decision (Figure 3) was 69.4% for hospital admission and 91.6% for discharge (P<0.001 vs. hospital admission).
Discussion
The main finding of the present study is that an acceptable, although suboptimal, adherence to the ESC Guidelines' indications is possible since the earliest hospital phase. Furthermore, the ESC Guidelines on syncope are applicable since the patients' ED presentation. Thus, further observations on a guidelines-based management of patients with syncope since the ED stay are warranted.
The most important feature of the ED clinical observation for syncope is the final decision regarding hospital admission or discharge; therefore, the appropriateness of such decision and the adherence to the specific indications of the guidelines are the standard on which it is possible to evaluate the quality of the process. Our study suggests that an acceptable adherence to the main indications of the guidelines is already possible in a well-trained ED. Overall, as a consequence of a slight excess of the number of patients actually hospitalized, the adherence rate in our ED was greater for admission than for discharge. This is justified by the consideration that any new structure (such as our SU) instituted in a Public Hospital should first of all ensure the safety of any related clinical pathway. Thus, the adherence to the guidelines observed in our ED seems, in perspective, susceptible of further improvement provided that better implementation strategies are used to achieve this goal. In contrast, our result was achieved without a corresponding compromise of the appropriateness. As a consequence, the overall hospitalization rate for syncope in our ED was 50.1%, a value similar to that observed in the most recent population studies, ranging from 46 to 67.6%.1–5,7,8,15–18 Furthermore, although the main investigators of the study were not involved in the decision to admit or discharge the single patients, such a performance was also maintained over a long (24 months) time interval. These latter aspects are an exclusive feature of our study and are noteworthy to ensure that our results could be reproduced by any ED in the daily clinical practice. Finally, the adherence rate to the guidelines observed in our ED was significantly higher for the therapeutic indications for hospital admission than for the diagnostic ones. This is justified by the restrictive definitions adopted for any subgroup of such indications, which made the attribution of the different criteria to the single patients less subjective.
A further aspect of basic importance is relative to the applicability of the ESC Guidelines. Provided that the guidelines' criteria are referred only to patients with a true syncope, the practical impact of the guidelines depends on the relative frequency of true syncope and non-syncopal conditions in the population of patients with TLC. Overall, 85.9% of our patients were diagnosed as having a true syncope since the ED observation, so that it was possible to evaluate them according to the specific ESC Guidelines. Our findings are consistent with those of 16% of ‘syncope-like conditions’ and 84% of true syncope observed among patients entering the ED for TLC in the recent multicentric EGSYS study.5,18 These data strongly suggest that the diagnostic criteria of the ESC Guidelines on syncope are applicable from the very beginning of the hospital stay to the large majority of the real world, unselected patients entering the ED of any District Hospital for a TLC.
Finally, our data show that, even after a guidelines-based initial evaluation, a high proportion of patients observed at the ED for syncope (39.1% in the present series) still have some appropriate indication for hospitalization. In the present paper, the number of calculated hospitalizations was largely influenced by those patients who, regardless of the ultimate mechanism of syncope, were found to have severe comorbidities needing a specific, prompt treatment. In such cases, the syncope was clearly the first clinical manifestation of a definite, underlying disease. Nevertheless, because in all our patients the syncope was the main clinical symptom leading to the ED presentation, we chose to include (although in a well separate group) also these patients in our study, in order to attain a more realistic picture of the real-world population of patients entering the ED for a syncope.
Limitations of the study
Our study has important limitations. First of all, it was a single centre study. Although the patients' enrolment and the data collection were so far accurate, our series and the related case-mix cannot be considered fully representative of the entire population of patients entering the ED of any District Hospital for both a syncope or a TLC. Secondly, the observation period was limited to a defined time-window; however, our study lasted 2 years, whereas other studies had shorter enrolment periods.1,4,5,16–18 Thirdly, our analysis of the calculated indications for hospitalization was retrospective. Finally, our findings would have been more interesting if a comparison had been made with the pre-guidelines application period in our hospital. Unfortunately, this was not possible because many ED physicians were yet applying the ESC Guidelines on syncope even before the formalization of the SU in our hospital. As a consequence, such a comparison would have weakened the true impact of the guidelines. Thus, only the hospitalization rate by the most recent population studies on syncope was taken as a reference. It is likely that, to replicate in other hospitals the results of the present study, a preliminary period of aggressive ED education is needed.
Conclusions
Our study gives a global picture of the real-world population of patients presenting to the ED for syncope. Any strategy aimed to improve the hospital management of this frequent clinical symptom will need the ED involved in a guidelines-based, early stratification of patients. The results of our study suggest that better implementation strategies are needed in the real world in order to achieve a good adherence to the recommendations of the guidelines.
Acknowledgement
The authors wish to acknowledge the contribution of Professional Nurses Miria Brutai and Barbara Rigacci for the data collection.
Conflict of interest: none declared.
Figure 1 Indications for hospitalization according to the 2001 ESC Guidelines on syncope.
Figure 2 ED adherence to the ESC Guidelines on syncope indications for hospitalization.
Figure 3 Appropriateness of the ED medical decision to admit/discharge.
Causes of cardiac syncope after the ED initial evaluation
| Sinus node dysfunction | 8 |
| Advanced AV block | 22 |
| Pacemaker/ICD failure | 2 |
| Supraventricular tachycardia | 1 |
| Ventricular tachycardia | 5 |
| Cardiac ischaemia-related syncope | 15 |
| Massive pulmonary embolism | 9 |
| Cardiac tamponade | 2 |
| Total | 64 |
| Sinus node dysfunction | 8 |
| Advanced AV block | 22 |
| Pacemaker/ICD failure | 2 |
| Supraventricular tachycardia | 1 |
| Ventricular tachycardia | 5 |
| Cardiac ischaemia-related syncope | 15 |
| Massive pulmonary embolism | 9 |
| Cardiac tamponade | 2 |
| Total | 64 |
ICD, implantable automatic defibrillator.
Causes of cardiac syncope after the ED initial evaluation
| Sinus node dysfunction | 8 |
| Advanced AV block | 22 |
| Pacemaker/ICD failure | 2 |
| Supraventricular tachycardia | 1 |
| Ventricular tachycardia | 5 |
| Cardiac ischaemia-related syncope | 15 |
| Massive pulmonary embolism | 9 |
| Cardiac tamponade | 2 |
| Total | 64 |
| Sinus node dysfunction | 8 |
| Advanced AV block | 22 |
| Pacemaker/ICD failure | 2 |
| Supraventricular tachycardia | 1 |
| Ventricular tachycardia | 5 |
| Cardiac ischaemia-related syncope | 15 |
| Massive pulmonary embolism | 9 |
| Cardiac tamponade | 2 |
| Total | 64 |
ICD, implantable automatic defibrillator.
Adherence rate to the Guidelines' indications for hospital admission subdivided for the subgroups
| . | Guidelines . | ED . |
|---|---|---|
| Therapeutic hospitalization | 141 | 129 (91.5%) |
| Hospitalization for comorbidities | 79 | 79 (100%) |
| Therapeutic subtotal | 220 | 208 (94.5%) |
| Diagnostic hospitalization | 170 | 145 (85.3%) |
| ‘Occasional’ hospitalization | 50 | 40 (80%) |
| Diagnostic subtotal | 220 | 185 (84.1%)* |
| Total | 440 | 393 (89.3%) |
| . | Guidelines . | ED . |
|---|---|---|
| Therapeutic hospitalization | 141 | 129 (91.5%) |
| Hospitalization for comorbidities | 79 | 79 (100%) |
| Therapeutic subtotal | 220 | 208 (94.5%) |
| Diagnostic hospitalization | 170 | 145 (85.3%) |
| ‘Occasional’ hospitalization | 50 | 40 (80%) |
| Diagnostic subtotal | 220 | 185 (84.1%)* |
| Total | 440 | 393 (89.3%) |
*p<0.001 among therapeutic and diagnostic subtotals.
Adherence rate to the Guidelines' indications for hospital admission subdivided for the subgroups
| . | Guidelines . | ED . |
|---|---|---|
| Therapeutic hospitalization | 141 | 129 (91.5%) |
| Hospitalization for comorbidities | 79 | 79 (100%) |
| Therapeutic subtotal | 220 | 208 (94.5%) |
| Diagnostic hospitalization | 170 | 145 (85.3%) |
| ‘Occasional’ hospitalization | 50 | 40 (80%) |
| Diagnostic subtotal | 220 | 185 (84.1%)* |
| Total | 440 | 393 (89.3%) |
| . | Guidelines . | ED . |
|---|---|---|
| Therapeutic hospitalization | 141 | 129 (91.5%) |
| Hospitalization for comorbidities | 79 | 79 (100%) |
| Therapeutic subtotal | 220 | 208 (94.5%) |
| Diagnostic hospitalization | 170 | 145 (85.3%) |
| ‘Occasional’ hospitalization | 50 | 40 (80%) |
| Diagnostic subtotal | 220 | 185 (84.1%)* |
| Total | 440 | 393 (89.3%) |
*p<0.001 among therapeutic and diagnostic subtotals.
References
Ammirati F, Colivicchi F, Minardi G, De Lio L, Terranova A, Scaffidi G, Rapino S, Proietti F, Bianchi C, Uguccioni M, Carunchio A, Azzolini P, Neri R, Accogli S, Sunseri L, Orazi S, Mariani M, Fraioli R, Calcagno S, De Luca F, Santini M. The management of syncope in the hospital: the OESIL (Osservatorio Epidemiologico della Sincope nel Lazio) study.
Kenny RA, O'Shea D, Walker HF. Impact of a dedicated syncope and falls facility for older adults on emergency beds.
Blanc JJ, L'Her C, Touiza A, Garo B, L'Her E, Mansourati J. Prospective evaluation and outcome of patients admitted for syncope over a 1 year period.
Del Greco M, Cozzio S, Scillieri M, Caprai F, Scivales A, Disertori M. Diagnostic pathway of syncope and analysis of Guidelines impact in a district general hospital. The ECSIT study (Epidemiology and costs of syncope in Trento).
Disertori M, Brignole M, Menozzi C, Raviele A, Rizzon P, Santini M, Proclemer A, Tomasi C, Rossillo A, Taddei F, Scivales A, Migliorini R, De Santo T. Management of patients with syncope referred urgently to general hospitals.
Bartoletti A, Del Rosso A. Cosa potrebbero fare le Associazioni Cardiologiche per migliorare la gestione del paziente con sincope?
Shen WK, Decker WW, Smars PA, Goyal DG, Walker AE, Hodge DO, Trusty GM, Brekke KM, Jahangir A, Brady PA, Munger TM, Gersh BJ, Hammill SC, Frye RL. Syncope Evaluation in the Emergency Department Study (SEEDS). A multidisciplinary approach to syncope management.
Elesber AA, Decker WW, Smars PA, Hodge DO, Shen WK. Impact of the application of the American College of Emergency Physicians recommendations for the admission of patients with syncope on a retrospectively studied population presenting to the emergency department.
Brignole M, Alboni P, Benditt D, Bergfeldt L, Blanc JJ, Bloch Thomsen PE, van Dijk JG, Fitzpatrick A, Hohnloser S, Janousek J, Kapoor W, Kenny RA, Kulakowski P, Moya A, Raviele A, Sutton R, Theodorakis G, Wieling W. Task Force on Syncope, European Society of Cardiology. Guidelines on management (diagnosis and treatment) of syncope.
Brignole M, Alboni P, Benditt DG, Bergfeldt L, Blanc JJ, Bloch Thomsen PE, van Dijk JG, Fitzpatrick A, Hohnloser S, Janousek J, Kapoor W, Kenny RA, Kulakowski P, Masotti G, Moya A, Raviele A, Sutton R, Theodorakis G, Ungar A, Wieling W. Guidelines on management (diagnosis and treatment) of syncope—Update 2004.
Bartoletti A, Fabiani P, Gianni R, Cappelletti C, Santoro GM, Fortini A, Adriani P, Baccetti F, Buffini G, Lavacchi A, Ticali PF, Vigano S. After the 2001 European Society of Cardiology Guidelines: is it possible to reduce the number of patients with syncope to be hospitalised?
Brignole M, Thijs R, Wieling W, Benditt D, van Dijk JG, on behalf of the Task Force on Syncope of the European Society of Cardiology. Is a syncope a syncope?
The Consensus Committee of the American Autonomic Society and the American Academy of Neurology. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple systemic atrophy.
Kapoor WN, Karpf M, Wieand S, Peterson J, Levey G. A prospective evaluation and follow-up of patients with syncope.
Ammirati F, Colivicchi F, Santini M. Diagnosing syncope in clinical practice. Implementation of a simplified diagnostic algorithm in a multicentre prospective trial—the OESIL 2 study (Osservatorio Epidemiologico della Sincope nel Lazio).
Crane SD. Risk stratification of patients with syncope in an accident and emergency department.