-
PDF
- Split View
-
Views
-
Cite
Cite
Carl Llor, Gloria Rabanaque, Ana López, Josep Maria Cots, The adherence of GPs to guidelines for the diagnosis and treatment of lower urinary tract infections in women is poor, Family Practice, Volume 28, Issue 3, June 2011, Pages 294–299, https://doi.org/10.1093/fampra/cmq107
Close - Share Icon Share
Abstract
Objectives. To assess the adherence of GPs to evidence-based guidelines for the diagnosis and management of lower urinary tract infection (UTI) in women.
Methods. A cross-sectional study was performed from March to July 2009 in primary care offices. Physicians consecutively registered the first six UTI attended during an 8-week period. Age, days with symptoms, episode of infection, associated morbidity, signs and symptoms, diagnostic procedures performed, antibiotic prescription, allergies and referral or not were registered. The type of antibiotic course (short or long) and first-choice treatments were also taken into account.
Results. Of 176 physicians invited to participate, 110 (62.5%) included 658 women with lower UTI. Urine dipstick was performed in 550 cases (83.6%) and urine culture was requested in 235 women (35.7%), with criteria for culture in 49.6% and without criteria in 32.8%. Antibiotic treatment was administered in 634 cases (96.4%). Short courses were given to 385 women (60.7%) and 75 of those with complicated UTI were treated with long courses (66.4%). First-choice antibiotics were administered as empiric treatment in only 92 women with uncomplicated UTI (17.7%).
Conclusions. These results highlight the poor adherence of GPs to the current recommendations of clinical practice guidelines with a high number of inappropriate urine cultures requested and a low utilization of first-choice antibiotics.
Introduction
Urinary tract infections (UTIs) represent a common problem in primary care consultations, mainly among women.1–3 It is estimated that as many as 60% of all women report having had a UTI at least once in their lifetime.4,5 Since this infection is very frequent, its diagnosis and treatment have implications not only for the health of the patients with these infections but also in the development of resistance. Different clinical guidelines have been published with the aim of guiding primary care physicians in the correct diagnosis and treatment of these infections.1,6–8 In general, these guidelines recommend not using urine cultures for uncomplicated infections, to prescribe short-course schedules in uncomplicated cystitis and to administer long drug schedules in cases of risk of complication.
With this type of information available to primary care physicians, the management of lower UTI should logically follow these recommendations. However, the truth is that the management of these infections by many professionals is implemented independently of these guidelines.6,9–16 In a study carried out in 2100 primary care physicians in the USA, the management of UTI varied greatly, with a large number of practitioners requesting unnecessary urine cultures.16 In addition, a large number of practitioners continued to request many unnecessary urine cultures. In this study, only 50% of the physicians had indicated short antibiotic courses for the treatment of uncomplicated lower UTIs. Moreover, lack of adherence may lead to an increase in health care costs.12 Our hypothesis is that there is a similar division between what is done and what should be done in our country. Therefore, the present study was designed to determine the diagnostic and therapeutic approaches undertaken by primary care practitioners for lower UTIs in women.t
Subjects and methods
Study design
A cross-sectional study was carried out by GPs from primary care consulting offices around Spain from March to July 2009. The practitioners were instructed as to how to fill in a data registry related to the first six consecutive women over the age of 14 years with clinical criteria compatible with lower UTI during an 8-week period. Women who were pregnant, immunosuppressed or received concomitant immunosuppressive drugs had chronic renal failure or those with clinical manifestations of pyelonephritis were excluded from the study. The data were registered according to the ‘Audit Project Odense’ (APO) method described by Munck et al.17 following a prospective self-registry methodology. A simple registry sheet was used in which the attending physician reported different specific parameters of the medical visit, including age, days of evolution, episode of infection—first episode, recurrence or relapse and number of episodes in the previous year—history, such as renal lithiasis, diabetes, pyelonephritis in the previous year or UTI during childhood, signs and symptoms present—dysuria, urinary frequency, haematuria, turbid urine, smelly urine, suprapubic pain or vaginal discharge—diagnostic tests performed—presence of leukocytes in the urine dipstick test, presence of nitrites, presence of blood, negative dipstick test (negativity of leukocytes, nitrites and blood), culture requested, none—antibiotic treatment or not, type of antibiotic and schedule indicated, dose and duration of treatment—and finally, possible allergy to penicillin and referral to another setting or not.
All the physicians were shown how to register the visits with UTI. Likewise, they were given a manual of instructions and a protocol for filling in the registry sheets. At least one of the items in the sections on episodes, history, signs and symptoms, diagnostic tests and others had to be checked. On the other hand, in the antibiotics and schedule sections, only the items performed were indicated. The importance of reporting the antibiotic prescribed, its presentation in milligrams as well as the duration of the schedule in 1 day in a single dose up to 7 days was highlighted.
Definitions considered
Uncomplicated lower UTI was considered as infection with no previous history of interest, isolated episode and foreseen to be cured with the usual short-course empiric treatment. In cases of recurrence, uncomplicated UTIs were considered as infrequent reinfections (up to three infections in 1 year).7,8 Complicated UTI was considered as infection occurring in patients with a history of metabolic disturbances or with structural or functional urinary tract alterations, which may carry a poor outcome with the usual short-course antibiotics. Frequent recurrent infections (more than three episodes in the previous year) were also considered as complicated infections.7,8
Criteria to perform determination with a reactive strip were considered when the clinical manifestations were typical of UTI and were accompanied by vaginal symptoms—in which case the probability of UTI decreases 50%—and in cases of clinical manifestations unspecific for UTI. In these latter cases, a negative dipstick test ruled out the diagnosis.18,19 On the other hand, if the clinical manifestations were typical of UTI without the presence of vaginal symptoms, the probability of UTI is of at least 90%, making the use of the urine dipstick test unnecessary.20,21 Criteria of urine culture were frequent recurrence (>3/year), relapse, symptoms of cystitis with a negative dipstick test and a history with suspicion of potentially complicated subclinical pyelonephritis, such as lithiasis, functional or structural urinary tract alterations, UTI during childhood, diabetes or pyelonephritis within the last year.7,8
First-choice treatment included the following antimicrobial schedules:7,13 single-dose fosfomycin trometamol 3 g, calcium fosfomycin 500 mg t.i.d. for 7 days, nitrofurantoin 50–100 mg q.i.d. for 7 days, norfloxacin 400 mg b.i.d. for 3 days, ciprofloxacin 250 mg b.i.d. for 3 days and amoxicillin + clavulanic acid 500/125 mg t.i.d. for 5 days. The first three antibiotics are included in the guidelines for the treatment of uncomplicated UTI in Spain since the resistance of the most frequent urinary pathogens, mainly Escherichia coli, to these antibiotics is very low.22 Short courses were considered as any presentation of fosfomycin trometamol, the schedule of 3 days of quinolones or 5-day β-lactam regimens. The 5-day regimen of nitrofurantoin 50–100 mg q.i.d. was also included.23 Long courses were considered in patients with risk factors of complicated UTI. The data were analysed with the SPSS v.15 statistical program with descriptive analysis of the results.
Results
Physicians
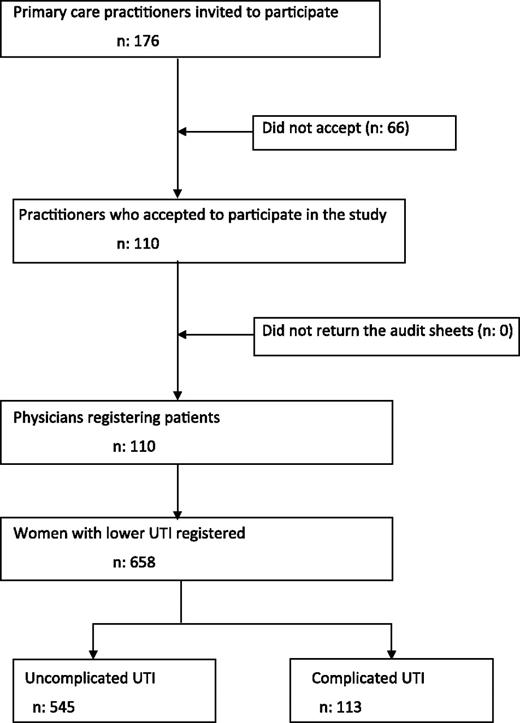
A total of 176 primary care physicians were invited to voluntarily participate, with 110 including patients (62.5%). The mean age of the practitioners participating was 46.6 ± 8.2 years and 60 were women (54.5%). Figure 1 shows the general scheme of the study.
Urinary tract infections
Clinical data were collected from a total of 658 women with lower UTI, with a mean age of 46.5 ± 19.3 years and a mean of 3.4 ± 6.8 days of evolution. A total of 322 infections corresponded to a first episode (48.9%). The most frequent history reported was the presence of recurrent cystitis in 152 cases (23.1%), followed by diabetes mellitus (70; 10.6%) with 372 of the cases studied (56.5%) having no previous history of infection. The most frequent symptom described was the presence of dysuria (539 patients; 81.9%), followed by urinary frequency (464 cases; 70.5%) and suprapubic pain (218; 33.1%).
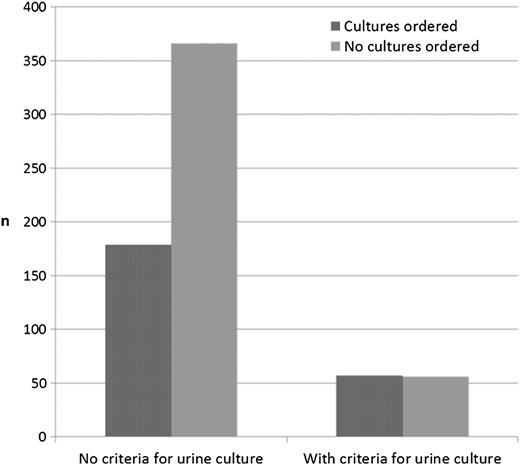
A urine dipstick test was performed in 550 women (83.6%), being positive for leukocytes in 478 cases (86.9%), nitrites in 325 (59.1%) and for blood in 279 cases (50.7%). Urine cultures were requested in 235 of the women studied (35.7%), with the addition of urine dipstick determination in 160 (Table 1). Only 33 women did not undergo either of these tests (5%). Figure 2 shows the correlation between the request for urine culture and the appropriateness of the request. Urine culture was requested in 56 of the 113 women with criteria (49.6%) and in 179 of the 545 women without criteria for this test (32.8%; Table 1).
Diagnostic procedures requested and antibiotics prescribed in women with lower UTIs depending on the type of the infection
| Uncomplicated UTIa (n = 545) | Complicated UTI (n = 113) | Total (n = 658) | |
| Dipsticks requested, n (%) | 456 (83.7) | 94 (83.2) | 550 (83.6) |
| Cultures ordered, n (%) | 179 (32.8) | 56 (49.6) | 235 (35.7) |
| First-choice treatments prescribed, n (%) | 92 (17.7) | 19 (16.8) | 111 (17.5) |
| Short-course treatments prescribed, n (%) | 347 (66.6) | 38 (33.6) | 385 (60.7) |
| Long-course treatments, n (%) | 174 (33.4) | 75 (66.4) | 249 (39.3) |
| Uncomplicated UTIa (n = 545) | Complicated UTI (n = 113) | Total (n = 658) | |
| Dipsticks requested, n (%) | 456 (83.7) | 94 (83.2) | 550 (83.6) |
| Cultures ordered, n (%) | 179 (32.8) | 56 (49.6) | 235 (35.7) |
| First-choice treatments prescribed, n (%) | 92 (17.7) | 19 (16.8) | 111 (17.5) |
| Short-course treatments prescribed, n (%) | 347 (66.6) | 38 (33.6) | 385 (60.7) |
| Long-course treatments, n (%) | 174 (33.4) | 75 (66.4) | 249 (39.3) |
Antibiotics were prescribed in 521 uncomplicated infections.
Diagnostic procedures requested and antibiotics prescribed in women with lower UTIs depending on the type of the infection
| Uncomplicated UTIa (n = 545) | Complicated UTI (n = 113) | Total (n = 658) | |
| Dipsticks requested, n (%) | 456 (83.7) | 94 (83.2) | 550 (83.6) |
| Cultures ordered, n (%) | 179 (32.8) | 56 (49.6) | 235 (35.7) |
| First-choice treatments prescribed, n (%) | 92 (17.7) | 19 (16.8) | 111 (17.5) |
| Short-course treatments prescribed, n (%) | 347 (66.6) | 38 (33.6) | 385 (60.7) |
| Long-course treatments, n (%) | 174 (33.4) | 75 (66.4) | 249 (39.3) |
| Uncomplicated UTIa (n = 545) | Complicated UTI (n = 113) | Total (n = 658) | |
| Dipsticks requested, n (%) | 456 (83.7) | 94 (83.2) | 550 (83.6) |
| Cultures ordered, n (%) | 179 (32.8) | 56 (49.6) | 235 (35.7) |
| First-choice treatments prescribed, n (%) | 92 (17.7) | 19 (16.8) | 111 (17.5) |
| Short-course treatments prescribed, n (%) | 347 (66.6) | 38 (33.6) | 385 (60.7) |
| Long-course treatments, n (%) | 174 (33.4) | 75 (66.4) | 249 (39.3) |
Antibiotics were prescribed in 521 uncomplicated infections.
Antibiotic treatment was administered in 634 cases (96.4%; Table 2). All the patients with complicated infections were given antibiotic treatment. First-choice drug schedules were prescribed in 111 cases (17.5%) and in 92 women with uncomplicated infections (17.7%). Globally, short courses were given to 385 women (60.7%). Of all the patients with uncomplicated cystitis, 347 received short regimens (66.6%). Long drug courses were prescribed in 249 women (39.3%), being administered in 75 of the 113 cases presenting complicated UTI (66.4%). In total, 10.8% of the women with complicated UTI were referred to another setting.
Antibiotic regimens prescribed and their duration
| Antibiotic regimen | Treatment duration | |||||
| Single-dose, n (%) | 2 days, n (%) | 3 days, n (%) | 5 days, n (%) | 7 days, n (%) | Total, n (%) | |
| Trometamol fosfomycin 3 g o.d. | 58 (19.4) | 241 (80.6) | 0 (—) | 0 (—) | 0 (—) | 299 (100) |
| Amoxicillin + clavulanic acid 500–875/125 mg t.i.d. | 0 (—) | 0 (—) | 0 (—) | 22 (22.7) | 75 (77.3) | 97 (100) |
| Norfloxacin 400 mg b.i.d. | 0 (—) | 0 (—) | 18 (24.0) | 6 (8.0) | 51 (68.0) | 75 (100) |
| Ciprofloxacin 500 mg b.i.d. | 0 (—) | 0 (—) | 1 (1.6) | 26 (41.3) | 36 (57.1) | 63 (100) |
| Trometamol fosfomycin 2 g o.d. | 9 (40.9) | 13 (59.1) | 0 (—) | 0 (—) | 0 (—) | 22 (100) |
| Ciprofloxacin 250 mg b.i.d. | 0 (—) | 0 (-) | 0 (-) | 7 (46.7) | 8 (53.3) | 15 (100) |
| Calcium fosfomycin 500 mg t.i.d. | 0 (—) | 0 (—) | 0 (—) | 0 (—) | 13 (100) | 13 (100) |
| Cefixime 400 mg o.d. | 0 (—) | 0 (—) | 0 (—) | 2 (28.6) | 5 (71.4) | 7 (100) |
| Levofloxacin 250–500 mg o.d. | 0 (—) | 0 (—) | 0 (—) | 0 (—) | 2 (100) | 2 (100) |
| Nitrofurantoin 100 mg q.i.d. | 0 (—) | 0 (—) | 0 (—) | 2 (100) | 0 (—) | 2 (100) |
| Other antibiotics | 0 (—) | 0 (—) | 2 (5.1) | 29 (74.4) | 8 (20.5) | 39 (100) |
| Total | 67 (10.6) | 254 (40.1) | 21 (3.3) | 94 (14.8) | 198 (31.2) | 634 (100) |
| Antibiotic regimen | Treatment duration | |||||
| Single-dose, n (%) | 2 days, n (%) | 3 days, n (%) | 5 days, n (%) | 7 days, n (%) | Total, n (%) | |
| Trometamol fosfomycin 3 g o.d. | 58 (19.4) | 241 (80.6) | 0 (—) | 0 (—) | 0 (—) | 299 (100) |
| Amoxicillin + clavulanic acid 500–875/125 mg t.i.d. | 0 (—) | 0 (—) | 0 (—) | 22 (22.7) | 75 (77.3) | 97 (100) |
| Norfloxacin 400 mg b.i.d. | 0 (—) | 0 (—) | 18 (24.0) | 6 (8.0) | 51 (68.0) | 75 (100) |
| Ciprofloxacin 500 mg b.i.d. | 0 (—) | 0 (—) | 1 (1.6) | 26 (41.3) | 36 (57.1) | 63 (100) |
| Trometamol fosfomycin 2 g o.d. | 9 (40.9) | 13 (59.1) | 0 (—) | 0 (—) | 0 (—) | 22 (100) |
| Ciprofloxacin 250 mg b.i.d. | 0 (—) | 0 (-) | 0 (-) | 7 (46.7) | 8 (53.3) | 15 (100) |
| Calcium fosfomycin 500 mg t.i.d. | 0 (—) | 0 (—) | 0 (—) | 0 (—) | 13 (100) | 13 (100) |
| Cefixime 400 mg o.d. | 0 (—) | 0 (—) | 0 (—) | 2 (28.6) | 5 (71.4) | 7 (100) |
| Levofloxacin 250–500 mg o.d. | 0 (—) | 0 (—) | 0 (—) | 0 (—) | 2 (100) | 2 (100) |
| Nitrofurantoin 100 mg q.i.d. | 0 (—) | 0 (—) | 0 (—) | 2 (100) | 0 (—) | 2 (100) |
| Other antibiotics | 0 (—) | 0 (—) | 2 (5.1) | 29 (74.4) | 8 (20.5) | 39 (100) |
| Total | 67 (10.6) | 254 (40.1) | 21 (3.3) | 94 (14.8) | 198 (31.2) | 634 (100) |
Antibiotic regimens prescribed and their duration
| Antibiotic regimen | Treatment duration | |||||
| Single-dose, n (%) | 2 days, n (%) | 3 days, n (%) | 5 days, n (%) | 7 days, n (%) | Total, n (%) | |
| Trometamol fosfomycin 3 g o.d. | 58 (19.4) | 241 (80.6) | 0 (—) | 0 (—) | 0 (—) | 299 (100) |
| Amoxicillin + clavulanic acid 500–875/125 mg t.i.d. | 0 (—) | 0 (—) | 0 (—) | 22 (22.7) | 75 (77.3) | 97 (100) |
| Norfloxacin 400 mg b.i.d. | 0 (—) | 0 (—) | 18 (24.0) | 6 (8.0) | 51 (68.0) | 75 (100) |
| Ciprofloxacin 500 mg b.i.d. | 0 (—) | 0 (—) | 1 (1.6) | 26 (41.3) | 36 (57.1) | 63 (100) |
| Trometamol fosfomycin 2 g o.d. | 9 (40.9) | 13 (59.1) | 0 (—) | 0 (—) | 0 (—) | 22 (100) |
| Ciprofloxacin 250 mg b.i.d. | 0 (—) | 0 (-) | 0 (-) | 7 (46.7) | 8 (53.3) | 15 (100) |
| Calcium fosfomycin 500 mg t.i.d. | 0 (—) | 0 (—) | 0 (—) | 0 (—) | 13 (100) | 13 (100) |
| Cefixime 400 mg o.d. | 0 (—) | 0 (—) | 0 (—) | 2 (28.6) | 5 (71.4) | 7 (100) |
| Levofloxacin 250–500 mg o.d. | 0 (—) | 0 (—) | 0 (—) | 0 (—) | 2 (100) | 2 (100) |
| Nitrofurantoin 100 mg q.i.d. | 0 (—) | 0 (—) | 0 (—) | 2 (100) | 0 (—) | 2 (100) |
| Other antibiotics | 0 (—) | 0 (—) | 2 (5.1) | 29 (74.4) | 8 (20.5) | 39 (100) |
| Total | 67 (10.6) | 254 (40.1) | 21 (3.3) | 94 (14.8) | 198 (31.2) | 634 (100) |
| Antibiotic regimen | Treatment duration | |||||
| Single-dose, n (%) | 2 days, n (%) | 3 days, n (%) | 5 days, n (%) | 7 days, n (%) | Total, n (%) | |
| Trometamol fosfomycin 3 g o.d. | 58 (19.4) | 241 (80.6) | 0 (—) | 0 (—) | 0 (—) | 299 (100) |
| Amoxicillin + clavulanic acid 500–875/125 mg t.i.d. | 0 (—) | 0 (—) | 0 (—) | 22 (22.7) | 75 (77.3) | 97 (100) |
| Norfloxacin 400 mg b.i.d. | 0 (—) | 0 (—) | 18 (24.0) | 6 (8.0) | 51 (68.0) | 75 (100) |
| Ciprofloxacin 500 mg b.i.d. | 0 (—) | 0 (—) | 1 (1.6) | 26 (41.3) | 36 (57.1) | 63 (100) |
| Trometamol fosfomycin 2 g o.d. | 9 (40.9) | 13 (59.1) | 0 (—) | 0 (—) | 0 (—) | 22 (100) |
| Ciprofloxacin 250 mg b.i.d. | 0 (—) | 0 (-) | 0 (-) | 7 (46.7) | 8 (53.3) | 15 (100) |
| Calcium fosfomycin 500 mg t.i.d. | 0 (—) | 0 (—) | 0 (—) | 0 (—) | 13 (100) | 13 (100) |
| Cefixime 400 mg o.d. | 0 (—) | 0 (—) | 0 (—) | 2 (28.6) | 5 (71.4) | 7 (100) |
| Levofloxacin 250–500 mg o.d. | 0 (—) | 0 (—) | 0 (—) | 0 (—) | 2 (100) | 2 (100) |
| Nitrofurantoin 100 mg q.i.d. | 0 (—) | 0 (—) | 0 (—) | 2 (100) | 0 (—) | 2 (100) |
| Other antibiotics | 0 (—) | 0 (—) | 2 (5.1) | 29 (74.4) | 8 (20.5) | 39 (100) |
| Total | 67 (10.6) | 254 (40.1) | 21 (3.3) | 94 (14.8) | 198 (31.2) | 634 (100) |
Discussion
Main findings
In this audit performed in our country, primary care physicians demonstrated poor adherence to the current recommendations for the diagnosis and management of UTIs. With regard to diagnosis, a high number of unnecessary urine cultures were requested and with respect to treatment, the use of first-choice antibiotic schedules was low as was the administration of short antibiotic courses in uncomplicated cases of cystitis.
Limitations
The results of this study should be interpreted with caution because of a series of limitations. The most important is the low percentage of primary care physicians who accepted to participate. Participation was voluntary and the prescription habits may not have represented those usually carried out by primary care physicians as a whole. Different studies have shown that primary care physicians who participate in audits may be more interested in research than those who do not.24 One of the main reasons for refusing to participate in this type of study is precisely the lack of time.25 Nonetheless, the inclusion of a case in this study did not require >1 minute. Another limitation is that it was financially supported by a pharmaceutical laboratory, which may explain why the most frequently prescribed treatment in this study was fosfomycin, although the resistance of urinary pathogens in Spain has led this antibiotic to be the most frequently administered and the most frequently sold over the counter in the pharmacies in uncomplicated UTIs.26 The objective of this study was not to determine the antibiotic most often prescribed in UTIs but rather whether physicians follow the current guidelines in this type of infection. Another limitation of the study was that the clinical outcomes of the patients were not taken into account. Although we did not measure health outcomes, the registry sheet included the referral of patients to hospital. Another limitation, which should be regarded in this type of study, is that the mere fact of performing an audit may influence prescribing habits. However, the reliability of the APO methodology demonstrated in different projects carried out in other European countries is very high and is very well correlated with real prescription in medical offices.27
Comparison with other studies
Similar to physician behaviour seen in prior studies, our attending physicians were not judicious in ordering urine dipstick analyses or urine cultures.6,10,16,20 Many dipstick tests were ordered for patients who, based on history and examination, already had a 90% probability of UTI.20 The current recommendations are very clear. In the absence of risk factors of complicated UTI and in cases with clear clinical manifestations of cystitis (two or more symptoms) and in the absence of vaginal symptoms, empiric treatment may be started without the need for another laboratory test.20 In addition, despite the high probability of infection demonstrated by positive results on urine dipstick testing, physicians frequently ordered urine cultures. In cases of uncomplicated lower UTI, these tests should not be requested because of their cost, time and effort and the results of urine cultures do not imply a change in the treatment implemented. The participating primary care physicians may have doubted about the safety of not treating infections with antibiotics. Given the high rates of resistance of the urinary pathogens in Spain, results of urine culture with analysis of the susceptibility could have assured the practitioners as to the appropriateness of the antibiotic. Another reason why primary care physicians request unnecessary urine cultures is probably to avoid the possibility of new relapses, although this attitude is not logical in cases of uncomplicated infection.
Another result of note in this study was the poor decisions with regard to doses and schedules of first-choice antibiotics and short regimens in uncomplicated lower UTI in adult women. Similar to what occurred in the diagnosis, the primary care physicians participating in this study were probably doubtful regarding the use of short-course regimens, mainly single doses, for fear of relapse. On the other hand, the schedule for nitrofurantoin is of 6 hours, which may represent a problem for patient compliance and may explain why only two physicians prescribed this antibiotic. In a recent study published in Holland, the authors identified a series of barriers to follow the guidelines, one of which was the lack of appropriateness of the boxes of antibiotics for short-course treatment.28 For example, in Spain, quinolones are not available in boxes of six tablets and amoxicillin plus clavulanic acid cannot be bought in boxes of 15. In contrast, fosfomycin trometamol is available in one or two sachets. Nonetheless, the percentage of use of first-choice drugs according to the recommendations in the present study is comparable to other studies undertaken in other countries, being from 9 to 40.5% in the study by Kahan et al.12 and 25% in the study by Grover et al.6 It has been demonstrated that short treatment courses in uncomplicated cystitis in women achieve a similar percentage of clinical cure without a significant increase in recurrence, favouring compliance with fewer adverse effects and a lower cost, although bacteriological eradication is lower.29,30 Even in elderly women, short drug courses or single doses have shown to be equally effective as the long courses with the advantage of having fewer secondary effects.31 In the English and American guidelines, the short schedules are of choice. In our setting, differences with respect to the patterns of bacterial resistance should be taken into account to thereby adapt the recommendations.32 With the high resistance to these drugs in Spain, the use of amoxicillin, pipemidic acid, first-generation cephalosporins and trimethoprim-sulfamethoxazole is no longer recommended while the lowest resistances of the most frequent urinary pathogens being towards nitrofurantoin and fosfomycin. On the other hand, in recent years, the resistance of E. coli towards the association of amoxicillin and clavulanic acid and towards quinolones has increased.33 According to the recommendations of the Infectious Diseases Society of America and the study by Guay,34 when the rates of resistance surpass 20 and 25%, respectively, the antibiotic should be substituted. Since resistance to quinolones in some Spanish communities is already greater than this percentage, mainly in elderly women, nitrofurantoin and fosfomycin should be recommended.35
Adherence to clinical practice guidelines undoubtedly aids primary care physicians to carry out a more rational use of antibiotics in these infections. McIsaac et al.36 reported that adherence to guidelines would represent a reduction in unnecessary antibiotic prescription and avoid 59% of the urine cultures requested. Butler et al.37 described how a reduction in antibiotic prescription carries a parallel decrease in resistance, in this case, with ampicillin. The increasing rates of resistance, cross-resistance and multiresistance shown by urinary pathogens are a severe problem, which should be palliated with the rational choice of almost always empiric antimicrobials based on solid local epidemiological data. On the other hand, the administration of any of the previous antibiotics should be made over a 7-day period in patients with risk factors of complicated UTI. In situations other than these, short drug courses should be prescribed and if possible with antibiotics with low rates of bacterial resistance and showing great effectiveness against the principal uropathogens.
Implications for future research
After having determined physician behaviour regarding the diagnosis and treatment of UTIs, it is necessary to know whether these results can be reproduced in other geographical areas. On the other hand, qualitative investigation is required to determine why physicians request so many diagnostic tests, dipsticks and urine cultures and why they are doubtful as to use of first-choice treatment, mainly in uncomplicated UTIs, extending the work of Lugtenberg et al.28 to our setting and others. Only in this way will we be able to carry out strategies to change the attitudes of primary care physicians and encourage rational use of the health care resources available in this disease.
Declaration
Funding: Zambon pharmaceutical company funded this study.
Ethical approval: The study completely fulfilled all the regulations referring to observational studies. All the data included in the database were encoded to ensure confidentiality. Approval was obtained from the Ethical Board of the Spanish Society of Family Medicine (0013/08). During the study, patients did not undergo any intervention. Therefore, the patients were not asked for informed consent. However, patients were informed about the objective of the project and they were told that specific clinical information related to the consultation would be entered into a database.
Conflict of interest: The funders had no role in the design and conduct of the study, data collection, management, analysis or interpretation of the data and preparation, review or approval of the manuscript.
We wish to thank the GPs who participated in this study. Responsibility: all the authors had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- antibiotics
- patient referral
- hypersensitivity
- urinary tract infections
- diagnostic techniques and procedures
- primary health care
- infections
- diagnosis
- guidelines
- morbidity
- lower urinary tract infections
- clinical practice guideline
- urine culture
- urinary tract infection, acute
- evidence-based practice
- dipstick test, urine