-
PDF
- Split View
-
Views
-
Cite
Cite
D.E. Lolis, S.N. Kalantaridou, G. Makrydimas, A. Sotiriadis, I. Navrozoglou, K. Zikopoulos, E.A. Paraskevaidis, Successful myomectomy during pregnancy, Human Reproduction, Volume 18, Issue 8, 1 August 2003, Pages 1699–1702, https://doi.org/10.1093/humrep/deg318
Close - Share Icon Share
Abstract
BACKGROUND: Although leiomyomas usually remain asymptomatic during pregnancy, they may complicate its course. In this study, pregnancy outcome observed when myomectomy was performed during pregnancy in carefully selected patients is presented. METHODS: A prospective cohort study of 13 women who underwent myomectomy during pregnancy between January 1994 and December 2001. Surgical management of leiomyoma was required on the basis of characteristics of the myoma and symptoms. RESULTS: Among a total of 15 579 women registered at the authors’ prenatal clinic, 622 consecutive pregnant women had sonographically identified myoma; hence, the incidence was 3.9% (95% CI 3.6–4.3%). The vast majority of these women was asymptomatic during pregnancy or managed conservatively (97.4%; 95% CI 96–98%). Among 622 pregnant patients with leiomyoma, 13 presented with complications during pregnancy that required surgical intervention (2.1%; 95% CI 0.9–3.2%), due to increase in lesion size causing discomfort and/or severe abdominal pain not responding to conservative management with analgesic and non‐steroidal anti‐inflammatory drug medication. In 92% of these cases, successful myomectomy was performed and the pregnancy progressed to term without further complications. CONCLUSIONS: These data provide reassurance for pregnant women with uterine myoma. Surgical management of uterine leiomyoma during pregnancy may be successfully performed in carefully selected patients.
Introduction
The prevalence of leiomyoma during pregnancy is reported as ∼2% (Muram et al., 1980; Katz et al., 1989; Rice et al., 1989; Vergani et al., 1994). Until the advent of ultrasound, the diagnosis of these lesions was made clinically, and hence only large myomas—or those associated with adverse pregnancy outcome—were detected.
Although during pregnancy leiomyomas usually remain asymptomatic, they may complicate its course. Indeed, leiomyomas have been associated with an increased frequency of spontaneous abortion, preterm labour, premature rupture of membranes, antepartum bleeding, placental abruption, malpresentation and Caesarean section (Phelan, 1995). The most common complication is the syndrome of ‘painful myoma’; this is due to red or carneous degeneration and occurs in ∼5–8% of myomas during pregnancy (Phelan, 1995). This complication is associated with nausea, vomiting and fever, and usually occurs during the second trimester of pregnancy.
The management of leiomyoma during pregnancy is medical, but in rare circumstances surgical intervention and myomectomy may be required.
The aim of the present study was to evaluate the safety and efficacy of myomectomy during the second trimester of pregnancy. The results are reported of a prospective cohort study based on: (i) a protocol entailing serial scanning of all patients with fibroids diagnosed at routine first trimester sonographic screening; and (ii) a protocol of myomectomy during pregnancy. Thus, pregnancy outcome in carefully selected patients is presented when myomectomy was performed during pregnancy.
Materials and methods
Patients
This prospective cohort study included all eligible women who underwent myomectomy during pregnancy between January 1994 and December 2001 at the Department of Gynecology, Medical School of Ioannina. Routinely, women enrolled into the prenatal clinic at the authors’ institution undergo screening by ultrasound for dating purposes, nuchal translucency testing (Makrydimas and Lolis, 1997) and study of fetal anatomy and growth. In addition, a protocol was instituted entailing serial ultrasound examinations of pregnant women with sonographically detected leiomyoma every 2–4 weeks until term. The sonographic examinations were performed transvaginally when gestational age was <7 weeks, and transabdominally thereafter. The examinations were performed and the results analysed by physicians with specific training in obstetric sonography.
Investigations and surgical approach
The myomas were evaluated for size, number, position, location, relationship to the placenta and echogenic structure (Exacoustos and Rosati, 1993). The classification of the location of a leiomyoma was based on previously described criteria (Benson et al., 2001). Based on previous experience (Lolis et al., 1994), the criteria for deciding to submit to myomectomy during pregnancy were: (i) rapidly growing leiomyoma causing discomfort; (ii) severe abdominal pain (painful myoma) that did not respond to conservative management; (iii) a distance between the leiomyoma and the endometrial cavity >5 mm, in order to avoid opening of the endometrial cavity; and (iv) the provision of a signed consent form, after the patients had been informed of the risks of surgical intervention. Surgery was performed between the 15th and 19th weeks of gestation.
Laparotomy was performed under general endotracheal anaesthesia using a midline incision that extended over the umbilicus. A vertical incision was made over the myoma that was then rapidly and carefully removed using blunt and sharp dissection. Following leiomyoma removal, haemostasis was carefully carried out and the myometrium closed with two layers of interrupted sutures in a front‐to‐back closure using number 2/0 Vicryl sutures. A portion of omentum was secured over the uterine incision to cover the uterine scar (Lolis et al., 1994; Wittich et al., 2000). An intra‐abdominal drain was placed in all patients, and this was removed on the first postoperative day. Fetal monitoring (using ultrasonography) was carried out immediately after surgery to evaluate fetal viability. All patients received uterine relaxants for 4 days, and were discharged on post‐operative day 7. Post‐operatively, patients were followed‐up using ultrasonography at 2‐week intervals.
Statistical analysis
Statistical analysis was performed using a t‐test and Fisher’s exact test; a P‐value <0.05 was considered statistically significant. An incidence ratio and an operative intervention ratio of leiomyoma during pregnancy were calculated. Confidence intervals (CIs) of an observed frequency were calculated using the binomial distribution (Sachs, 1984).
Results
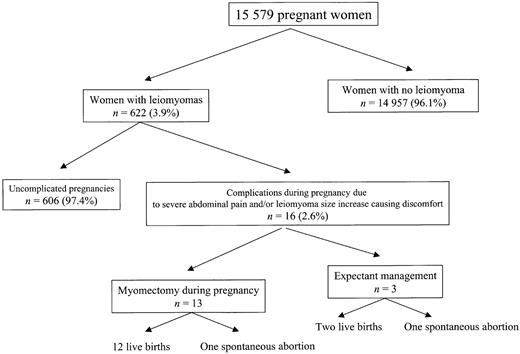
Among 15 579 women registered at the prenatal clinic, 622 consecutive pregnant women had sonographically identified myoma; hence, the incidence was 3.9% (95% CI 3.6–4.3%) (Figure 1). Among pregnant women, the mean age in those with myoma was 32 (range 24–40) years, compared with 28 (range 19–41) years in those without myoma (P < 0.01).
The diagnosis of leiomyoma was made in 183 women (29%) before pregnancy, and in 439 women (71%) at 6–12 weeks gestation. Single leiomyomas were found in 476 cases (76.5%) and multiple leiomyoma in 146 (23.5%). Of these women, the vast majority (606/622; 97.4%, 95% CI 96–98%) were asymptomatic during pregnancy or were managed conservatively. None of the infants had any major structural anomalies.
Among 622 pregnant patients with leiomyomas, 16 presented with complications during pregnancy (2.57%; 95% CI 1.3–3.8%), due to an increase in lesion size causing discomfort and/or severe abdominal pain that did not respond to conservative management with analgesics and non‐steroidal anti‐inflammatory drugs. Six cases presented with a significant increase in lesion size, eight with severe abdominal pain not responding to medical treatment, and two with severe abdominal pain along with an increase in lesion size. Because the distance between the endometrial cavity and the myoma was <5 mm, three of six women with a leiomyoma size increase (by 3, 5 and 6 cm respectively) were managed conservatively with ultrasound monitoring. Two of these women had normal vaginal deliveries at 34 and 38 weeks gestation, with birthweights of 2350 g and 2950 g respectively. The myomas did not increase further in size during the third trimester. The third woman aborted at 22 weeks gestation due to premature rupture of membranes and, because of massive post‐partum haemorrhage, an abdominal hysterectomy was performed.
Of the 622 pregnant women, 13 [mean age 33 (range 25–40) years] underwent laparotomy for uterine myomectomy (2.1%; 95% CI 0.9–3.2%). The characteristics of the women are presented in Table I. Torsion of a pedunculated leiomyoma occurred in two of the 13 cases. Pathological examination of the 13 specimens showed degenerative changes in 10 (77%), the most common findings being hyalinization (n = 3) and red degeneration (n = 2) (Table I).
In one case, uterine contractions appeared on the first post‐operative day, but these did not respond to medical treatment and the patient aborted. All other pregnancies had a good outcome (92.3%), and the procedure and post‐operative course were uncomplicated. In these cases, although the uterine cavities were not entered during surgery, the women delivered by Caesarean section. In one case, an emergency Caesarean section was performed at 29 weeks gestation because of severe vaginal bleeding due to placenta previa. In the other 11 women the pregnancy course was uneventful; neonatal weight ranged from 2500 to 3850 g, and all neonates had good 1‐min and 5‐min Apgar scores.
Overall, one of 13 women with myomectomy during pregnancy aborted spontaneously, whereas only one of 609 women with expectant management aborted (P = 0.041).
No hysterectomy or Caesarean sections were performed at the time of myomectomy, and no blood transfusions were required post‐operatively.
Discussion
Controversy persists among reports of myomectomy being performed during pregnancy. Most myomas remain asymptomatic during pregnancy, and routine ultrasonography performed at this time improves the detection of these lesions and the evaluation of any possible complications. It has been reported that ∼10% of pregnant women with myoma suffer complications related to the presence of these tumours (Katz et al., 1989). Such complications include spontaneous abortion, antepartum bleeding, premature rupture of membranes, preterm labour, placenta previa, post‐partum bleeding and a high incidence of Caesarean deliveries (Muram et al., 1980; Katz et al., 1989; Rice et al., 1989; Exacoustos and Rosati, 1993; Vergani et al., 1994; Benson et al., 2001). The rate of fetal loss is higher in patients with multiple fibroids than in those with a single fibroid (Benson et al., 2001).
In the present study, the incidence of myoma during pregnancy was 3.9%, though only 2.6% of women with myoma developed complications that required surgical intervention. In the vast majority of those women who required surgery, a successful myomectomy was performed and the pregnancy progressed to term without further complications.
As expected, the mean maternal age was higher among women with uterine myoma than in the general obstetric population. The lack of patients with submucosal fibroids may be due to the fact that previously identified submucosal leiomyomas were removed prior to pregnancy. Surgical removal of submucosal fibroids is often performed in the present authors’ department as these tend to be symptomatic and may contribute to failure to conceive and pregnancy loss.
Among the present patients, the most common complication was severe abdominal pain that did not respond to medical therapy. Indications for myomectomy during pregnancy include severe abdominal pain due to torsion of subserous pedunculated myomas or red degeneration not responding to medical treatment, and an increase in myoma size causing abdominal discomfort. It has been reported that if symptoms persist after 72 h of therapy, then surgical intervention must be considered (Burton et al., 1989; Dildy et al., 1992).
There are two basic complications of myomectomy during pregnancy: abortion and haemorrhage. Among the present patients, only one of 13 patients aborted post‐operatively.
Although the presence of myoma has been associated with fetal anomalies (Graham et al., 1980; Romero et al., 1981; Hasbargen et al., 2002), none of the infants in the present study had major structural anomalies.
Pregnant women with myoma should undergo frequent ultrasound evaluation during pregnancy in order to monitor both fetal growth and myoma size. Of note, when serial ultrasonography was used to monitor leiomyomas during pregnancy, only half of the lesions examined showed a significant change in size (Lev‐Toaff et al., 1987). During the first trimester, leiomyomas of all sizes either remained unchanged or increased in size, whereas during the second trimester smaller myomas (2–6 cm) usually remained unchanged or increased in size whilst larger myomas became smaller. During the third trimester, myomas usually remained unchanged or decreased in size, regardless of their initial dimensions. It was noted that, as both size and number of myomas increased, a significantly higher frequency of retained placentas, fetal malpresentations and preterm contractions was identified.
Red or carneous degeneration may present with localized pain and tenderness, fever, and an elevated white blood cell count. In most cases of red degeneration, ultrasound findings reveal cystic spaces in the myomas (Lev‐Toaff et al., 1987; Exacoustos and Rosati, 1993). Although medical therapy— including analgesics, fluids and antibiotics—may be used in the majority of these patients (Katz et al., 1989; Rice et al., 1989; Hasan et al., 1990; Exacoustos and Rosati, 1993; Moise, 1993), in patients with severe abdominal pain or an increase in myoma size causing abdominal pain and discomfort, a timely and well‐planned myomectomy should be an option.
In conclusion, the present data provide reassurance for pregnant women with uterine myoma. The surgical management of uterine leiomyoma during pregnancy may be performed successfully in carefully selected patients, and this seems to lead to an improvement in pregnancy outcome.
Figure 1. The study design.
Characteristics of patients and pregnancy outcome
| Patient no. | Age (years) | Symptoms before myomectomy | Location and number of leiomyomas | Gestational age at myomectomy (weeks) | Weight of largest leiomyoma (g) | Surgery and pathology findings | Week of delivery | Outcome (birth weight; g) |
| 1 | 34 | Severe abdominal pain | 2 intramural myomas in the anterior wall (one in the anterior lower uterine segment) | 16 | 585 | Hyaline degeneration | 37 | Live birth (3340) |
| 2 | 31 | Severe abdominal pain | 1 fundal subserous, 1 intramural in the posterior wall | 15 | 135 | Degenerative changes with inflammatory reaction | 39 | Live birth (3600) |
| 3 | 38 | Increase in size (7 cm growth) and severe abdominal pain | 1 fundal pedunculated, 2 intramural in the anterior uterine wall | 19 | 1500 | Red degeneration | 37 | Live birth (2970) |
| 4 | 35 | Severe abdominal pain | 1 fundal intramural | 16 | 105 | Mild hyaline degeneration | 36 | Live birth (3000) |
| 5 | 40 | Severe abdominal pain | 1 intramural in the anterior lower uterine wall | 15 | 1570 | Cystic degeneration | 15 | Abortion |
| 6 | 29 | Increase in size (3 cm growth) causing discomfort | 1 fundal intramural | 15 | 450 | Leiomyoma without degenerative changes | 37 | Live birth (2740) |
| 7 | 27 | Increase in size (4 cm growth) causing discomfort | 1 subserous, and 1 intramural in the anterior uterine wall | 16 | 520 | Leiomyoma without degenerative changes | 38 | Live birth (3180) |
| 8 | 25 | Severe abdominal pain | 1 fundal pedunculated, and 2 intramural in the anterior uterine wall | 16 | 170 | Torsion with extensive necrotic degeneration | 39 | Live birth (3515) |
| 9 | 25 | Severe abdominal pain | 1 pedunculated in the anterior uterine wall | 16 | 625 | Torsion with necrosis | 39 | Live birth (3190) |
| 10 | 33 | Severe abdominal pain | 1 intramural in the anterior lower uterine wall | 19 | 300 | Leiomyoma without degenerative changes | 38 | Live birth (2920) |
| 11 | 37 | Increase in size (6 cm growth) causing discomfort | 2 fundal subserous and 1 intramural in the posterior uterine wall | 17 | 1100 | Cystic degeneration | 38 | Live birth (3520) |
| 12 | 37 | Severe abdominal pain | 1 intramural in the anterior uterine wall | 16 | 2100 | Red degeneration | 38 | Live birth (3000) |
| 13 | 37 | Increase in size (8 cm growth) and severe abdominal pain | 1 fundal intramural | 15 | 2274 | Extensive hyaline degeneration; foci with haemorrhagic infiltration | 29 | Live birth (1606) |
| Patient no. | Age (years) | Symptoms before myomectomy | Location and number of leiomyomas | Gestational age at myomectomy (weeks) | Weight of largest leiomyoma (g) | Surgery and pathology findings | Week of delivery | Outcome (birth weight; g) |
| 1 | 34 | Severe abdominal pain | 2 intramural myomas in the anterior wall (one in the anterior lower uterine segment) | 16 | 585 | Hyaline degeneration | 37 | Live birth (3340) |
| 2 | 31 | Severe abdominal pain | 1 fundal subserous, 1 intramural in the posterior wall | 15 | 135 | Degenerative changes with inflammatory reaction | 39 | Live birth (3600) |
| 3 | 38 | Increase in size (7 cm growth) and severe abdominal pain | 1 fundal pedunculated, 2 intramural in the anterior uterine wall | 19 | 1500 | Red degeneration | 37 | Live birth (2970) |
| 4 | 35 | Severe abdominal pain | 1 fundal intramural | 16 | 105 | Mild hyaline degeneration | 36 | Live birth (3000) |
| 5 | 40 | Severe abdominal pain | 1 intramural in the anterior lower uterine wall | 15 | 1570 | Cystic degeneration | 15 | Abortion |
| 6 | 29 | Increase in size (3 cm growth) causing discomfort | 1 fundal intramural | 15 | 450 | Leiomyoma without degenerative changes | 37 | Live birth (2740) |
| 7 | 27 | Increase in size (4 cm growth) causing discomfort | 1 subserous, and 1 intramural in the anterior uterine wall | 16 | 520 | Leiomyoma without degenerative changes | 38 | Live birth (3180) |
| 8 | 25 | Severe abdominal pain | 1 fundal pedunculated, and 2 intramural in the anterior uterine wall | 16 | 170 | Torsion with extensive necrotic degeneration | 39 | Live birth (3515) |
| 9 | 25 | Severe abdominal pain | 1 pedunculated in the anterior uterine wall | 16 | 625 | Torsion with necrosis | 39 | Live birth (3190) |
| 10 | 33 | Severe abdominal pain | 1 intramural in the anterior lower uterine wall | 19 | 300 | Leiomyoma without degenerative changes | 38 | Live birth (2920) |
| 11 | 37 | Increase in size (6 cm growth) causing discomfort | 2 fundal subserous and 1 intramural in the posterior uterine wall | 17 | 1100 | Cystic degeneration | 38 | Live birth (3520) |
| 12 | 37 | Severe abdominal pain | 1 intramural in the anterior uterine wall | 16 | 2100 | Red degeneration | 38 | Live birth (3000) |
| 13 | 37 | Increase in size (8 cm growth) and severe abdominal pain | 1 fundal intramural | 15 | 2274 | Extensive hyaline degeneration; foci with haemorrhagic infiltration | 29 | Live birth (1606) |
Characteristics of patients and pregnancy outcome
| Patient no. | Age (years) | Symptoms before myomectomy | Location and number of leiomyomas | Gestational age at myomectomy (weeks) | Weight of largest leiomyoma (g) | Surgery and pathology findings | Week of delivery | Outcome (birth weight; g) |
| 1 | 34 | Severe abdominal pain | 2 intramural myomas in the anterior wall (one in the anterior lower uterine segment) | 16 | 585 | Hyaline degeneration | 37 | Live birth (3340) |
| 2 | 31 | Severe abdominal pain | 1 fundal subserous, 1 intramural in the posterior wall | 15 | 135 | Degenerative changes with inflammatory reaction | 39 | Live birth (3600) |
| 3 | 38 | Increase in size (7 cm growth) and severe abdominal pain | 1 fundal pedunculated, 2 intramural in the anterior uterine wall | 19 | 1500 | Red degeneration | 37 | Live birth (2970) |
| 4 | 35 | Severe abdominal pain | 1 fundal intramural | 16 | 105 | Mild hyaline degeneration | 36 | Live birth (3000) |
| 5 | 40 | Severe abdominal pain | 1 intramural in the anterior lower uterine wall | 15 | 1570 | Cystic degeneration | 15 | Abortion |
| 6 | 29 | Increase in size (3 cm growth) causing discomfort | 1 fundal intramural | 15 | 450 | Leiomyoma without degenerative changes | 37 | Live birth (2740) |
| 7 | 27 | Increase in size (4 cm growth) causing discomfort | 1 subserous, and 1 intramural in the anterior uterine wall | 16 | 520 | Leiomyoma without degenerative changes | 38 | Live birth (3180) |
| 8 | 25 | Severe abdominal pain | 1 fundal pedunculated, and 2 intramural in the anterior uterine wall | 16 | 170 | Torsion with extensive necrotic degeneration | 39 | Live birth (3515) |
| 9 | 25 | Severe abdominal pain | 1 pedunculated in the anterior uterine wall | 16 | 625 | Torsion with necrosis | 39 | Live birth (3190) |
| 10 | 33 | Severe abdominal pain | 1 intramural in the anterior lower uterine wall | 19 | 300 | Leiomyoma without degenerative changes | 38 | Live birth (2920) |
| 11 | 37 | Increase in size (6 cm growth) causing discomfort | 2 fundal subserous and 1 intramural in the posterior uterine wall | 17 | 1100 | Cystic degeneration | 38 | Live birth (3520) |
| 12 | 37 | Severe abdominal pain | 1 intramural in the anterior uterine wall | 16 | 2100 | Red degeneration | 38 | Live birth (3000) |
| 13 | 37 | Increase in size (8 cm growth) and severe abdominal pain | 1 fundal intramural | 15 | 2274 | Extensive hyaline degeneration; foci with haemorrhagic infiltration | 29 | Live birth (1606) |
| Patient no. | Age (years) | Symptoms before myomectomy | Location and number of leiomyomas | Gestational age at myomectomy (weeks) | Weight of largest leiomyoma (g) | Surgery and pathology findings | Week of delivery | Outcome (birth weight; g) |
| 1 | 34 | Severe abdominal pain | 2 intramural myomas in the anterior wall (one in the anterior lower uterine segment) | 16 | 585 | Hyaline degeneration | 37 | Live birth (3340) |
| 2 | 31 | Severe abdominal pain | 1 fundal subserous, 1 intramural in the posterior wall | 15 | 135 | Degenerative changes with inflammatory reaction | 39 | Live birth (3600) |
| 3 | 38 | Increase in size (7 cm growth) and severe abdominal pain | 1 fundal pedunculated, 2 intramural in the anterior uterine wall | 19 | 1500 | Red degeneration | 37 | Live birth (2970) |
| 4 | 35 | Severe abdominal pain | 1 fundal intramural | 16 | 105 | Mild hyaline degeneration | 36 | Live birth (3000) |
| 5 | 40 | Severe abdominal pain | 1 intramural in the anterior lower uterine wall | 15 | 1570 | Cystic degeneration | 15 | Abortion |
| 6 | 29 | Increase in size (3 cm growth) causing discomfort | 1 fundal intramural | 15 | 450 | Leiomyoma without degenerative changes | 37 | Live birth (2740) |
| 7 | 27 | Increase in size (4 cm growth) causing discomfort | 1 subserous, and 1 intramural in the anterior uterine wall | 16 | 520 | Leiomyoma without degenerative changes | 38 | Live birth (3180) |
| 8 | 25 | Severe abdominal pain | 1 fundal pedunculated, and 2 intramural in the anterior uterine wall | 16 | 170 | Torsion with extensive necrotic degeneration | 39 | Live birth (3515) |
| 9 | 25 | Severe abdominal pain | 1 pedunculated in the anterior uterine wall | 16 | 625 | Torsion with necrosis | 39 | Live birth (3190) |
| 10 | 33 | Severe abdominal pain | 1 intramural in the anterior lower uterine wall | 19 | 300 | Leiomyoma without degenerative changes | 38 | Live birth (2920) |
| 11 | 37 | Increase in size (6 cm growth) causing discomfort | 2 fundal subserous and 1 intramural in the posterior uterine wall | 17 | 1100 | Cystic degeneration | 38 | Live birth (3520) |
| 12 | 37 | Severe abdominal pain | 1 intramural in the anterior uterine wall | 16 | 2100 | Red degeneration | 38 | Live birth (3000) |
| 13 | 37 | Increase in size (8 cm growth) and severe abdominal pain | 1 fundal intramural | 15 | 2274 | Extensive hyaline degeneration; foci with haemorrhagic infiltration | 29 | Live birth (1606) |
References
Benson, C.B., Chow, J.S., Chang‐Lee, W., Hill, J.A. and Doubilet, P.M. (
Burton, C.A., Grimes, D.A. and March, C.M. (
Dildy, G.A., Moise, K.J., Smith, L.G., Kirshon, B. and Carpenter, R.J. (
Exacoustos, C. and Rosati, P. (
Graham, J.M., Miller, M.E., Stephan, M.J. and Smith, D.W. (
Hasan, F., Arumugam, K. and Sivanesaratnam, V. (
Hasbargen, U., Strauss, A., Summerer‐Moustaki, M., Baretton, G., Roth, U., Kimming, R. and Hepp, H. (
Katz, V.L., Dotters, D.J. and Droegemueller, W. (
Lev‐Toaff, A.S., Coleman, G.B., Arger, P.H., Mintz, M.C., Arenson, R.L. and Toaff, M.E. (
Lolis, D., Zikopoulos, K. and Paraskevaidis, E. (
Makrydimas, G. and Lolis, D. (
Moise, K.J., Jr (
Muram, D., Gillieson, M. and Walters, J.H. (
Rice, J.P., Kay, H.H. and Mahony, B.S. (
Romero, R., Chervenak, F.A., DeVore, G., Tortora, M. and Hobbins, J.C. (
Vergani, P., Chidrini, A., Strobelt, N., Roncaglia, N., Locatelli, A., Lapinski, R.H. and Mangioni, C. (