-
PDF
- Split View
-
Views
-
Cite
Cite
M. Watanabe, K. Nishida, Y. Kimura, M. Miyazaki, H. Baba, Salvage lymphadenectomy for cervical lymph node recurrence after esophagectomy for squamous cell carcinoma of the thoracic esophagus, Diseases of the Esophagus, Volume 25, Issue 1, 1 January 2012, Pages 62–66, https://doi.org/10.1111/j.1442-2050.2011.01215.x
Close - Share Icon Share
Summary
Prognosis of patients with recurrent esophageal cancer is usually unsatisfactory. We have successfully treated five patients with cervical node recurrence after esophagectomy with multimodal treatment including salvage lymphadenectomy. In order to clarify the efficacy of salvage surgery for cervical node recurrence, we have reviewed the clinical course and prognosis of these patients. From August 2004 to December 2007, 30 patients with 33 recurrent sites were treated in the Department of Surgery, Iizuka Hospital. Among these patients, there were five patients with recurrence limited within the cervical nodes. Salvage cervical lymphadenectomy was performed for all five patients. Curative resection was achieved in four patients and reduction surgery followed by planned chemoradiotherapy was performed in another patient. All stations including the suspicious node were dissected and a partial sternotomy was added for one patient whose recurrent tumor was located in the right recurrent nerve node. There was no mortality and one minor complication (subcutaneous hemorrhage) was observed. Median duration of hospital stay was 7 days. Adjuvant chemotherapy was performed for all patients. Median follow-up period was 54 months and all patients are alive without relapse of the disease. Salvage cervical lymphadenectomy is a safe and effective treatment for patients with cervical node recurrence after esophagectomy.
Introduction
Esophageal squamous cell carcinoma (ESCC) is one of the most difficult malignancies to be treated among gastrointestinal tract cancers. One of the reasons is an aggressive lymphatic spread of this disease because of the existence of well-developed lymphatic vessels longitudinally running through the esophageal wall.1,2 As metastasis to the cervical lymph node is frequently observed events in cancer originated from the thoracic esophagus, three-field lymph node dissection (3F-LD) has been widely accepted in Japan.3,4 Although there have been a lot of reports that indicated the efficacy of 3F-LD,5–7 all of them are retrospective studies, and a randomized control trial to prove the superiority of 3F-LD compared with two-field dissection has not yet been conducted.
Among the cervical lymph node stations, lymph nodes along the recurrent laryngeal nerve (cervical paraesophageal nodes) are known to be one of the most frequent metastatic sites from thoracic ESCC.2–7 Moreover, metastasis to the station can cause serious symptoms including hoarseness, aspiration, and suffocation. Therefore, there are little controversies in the necessity of the cervical paraesophageal node dissection during esophagectomy. The Japanese Classification of Esophageal Cancer has stated that the term ‘3F-LD’ should not be applied when only the cervical paraesophageal nodes were dissected in the neck.8 It means that these nodes should be dissected even in 2F-LD. In contrast, metastasis to the supraclavicular nodes is less frequent and seldom causes serious symptoms, and therefore an efficacy of preventive dissection of these nodes is still controversial.9
Lymph node recurrence as well as hematogenic metastasis is one of the most frequent patterns of recurrence after esophagectomy. Recurrence limited within the cervical lymph nodes is sometimes observed, especially in cases without preventive cervical lymph node dissection, and an optimal treatment strategy for such patients has not been clarified. Although there are a few reports that suggested a survival benefit of salvage lymph node dissection for such patients,10–12 the efficacy of this strategy has not yet been established.
We have routinely performed 3F-LD during esophagectomy since April 2004, when the authors’ team arrived in the Iizuka Hospital. Although there was no isolated cervical node recurrence among our own surgical cases during the study period, we experienced five cases with recurrent ESCC limited within the cervical lymph nodes, who underwent esophagectomy in the other institutes or at the period before the introduction of 3F-LD. Surgical resection of recurrent disease in the cervical nodes is less invasive, if invasion to the surrounding organs including the conduit, anastomosis, remnant esophagus, and trachea did not exist. When such invasion was observed, chemoradiotherapy (CRT) should be considered. Lymph nodes in the four patients did not invade the surrounding organs confirmed by imaging studies and that in the remaining was recurrence after CRT. Therefore, all patients were treated with salvage cervical node dissection followed by chemotherapy or CRT.
In this article, we demonstrate our experience of the multimodality treatment including salvage surgery and discuss the efficacy of this strategy.
Patients and Methods
Patients
From April 2004 to March 2008, 30 patients with 33 recurrent sites were treated in the Department of Surgery, Iizuka Hospital (Table 1). Among these patients, there were eight patients with cervical node recurrence, and three of them also suffered from recurrent diseases other than the cervical nodes. All five patients with recurrence limited within the cervical nodes were investigated in this study. All of them had undergone 2F-LD, two of them underwent esophagectomy in the other institutes and three were treated before the introduction of 3F-LD.
Patterns and sites of recurrence after esophagectomy
| Patterns and sites of recurrence . | Cases N = 30 (%) . |
|---|---|
| Hematogenic | 9 (33.3) |
| Liver | 6 |
| Lung | 3 |
| Lymphatic | 18 (60.0) |
| Cervical | 8 |
| Mediastinal | 9 |
| Abdominal | 2 |
| Local | 3 (10.0) |
| Pleural | 3 (10.0) |
| Patterns and sites of recurrence . | Cases N = 30 (%) . |
|---|---|
| Hematogenic | 9 (33.3) |
| Liver | 6 |
| Lung | 3 |
| Lymphatic | 18 (60.0) |
| Cervical | 8 |
| Mediastinal | 9 |
| Abdominal | 2 |
| Local | 3 (10.0) |
| Pleural | 3 (10.0) |
Patterns and sites of recurrence after esophagectomy
| Patterns and sites of recurrence . | Cases N = 30 (%) . |
|---|---|
| Hematogenic | 9 (33.3) |
| Liver | 6 |
| Lung | 3 |
| Lymphatic | 18 (60.0) |
| Cervical | 8 |
| Mediastinal | 9 |
| Abdominal | 2 |
| Local | 3 (10.0) |
| Pleural | 3 (10.0) |
| Patterns and sites of recurrence . | Cases N = 30 (%) . |
|---|---|
| Hematogenic | 9 (33.3) |
| Liver | 6 |
| Lung | 3 |
| Lymphatic | 18 (60.0) |
| Cervical | 8 |
| Mediastinal | 9 |
| Abdominal | 2 |
| Local | 3 (10.0) |
| Pleural | 3 (10.0) |
Clinical and pathologic classification of ESCC
Staging of the disease and grading of lymph nodes were diagnosed according to the Japanese Classification of Esophageal Cancer (10th edition).9
Diagnosis of recurrence
Diagnosis of recurrence was based on physical examinations and imaging studies including cervical ultrasonography (US) and computed tomography (CT), whereas the value of tumor markers (CEA, SCC and CYFRA 19–9) and 18F-fluorodeoxy glucose positron emission tomography were used as assistance.
Surgical procedures
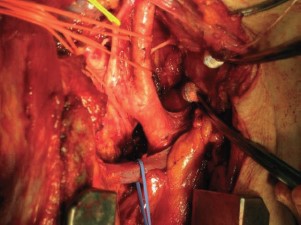
All 5 patients underwent salvage lymph node dissection. The range of the dissection included the lymphatic stations containing the metastatic nodes, and the other stations were also dissected if there had been any suspicious nodes on imaging studies. For a patient with metastasis to the right recurrent nerve node, an inverted L-shaped partial sternotomy from the top of the sternum to the second intercostal space was added (Fig. 1).
Operative field after dissection of lymph nodes along the right recurrent nerve. An inverted L-shaped partial sternotomy was added to obtain a good view of full length of the recurrent nerve.
Adjuvant therapy
All but one patient have not received postoperative treatment after the esophagectomy. One patient who had been diagnosed as microscopic residual disease in the mediastinum has undergone postoperative CRT. After the salvage lymph node dissection, four patients who underwent curative resection of the recurrent diseases were treated with two courses of adjuvant chemotherapy using nedaplatin and 5-fluorouracil. One patient who underwent reduction surgery was treated by planned CRT (Case 1).
Follow-up
All patients were followed up in the outpatient clinic at least every 3 months. The median follow-up period was 54 months.
Results
Backgrounds of the patients were shown in Table 2. Pathological stage at the time of first operation varied from I to IVa. Adjuvant therapy has not been applied in four patients whose tumors had been curatively resected, whereas Case 1 underwent postoperative CRT because of microscopic residual disease in the mediastinum. There were three patients with supraclavicular node recurrence, one patient with recurrent nerve node recurrence, and one with upper deep cervical node recurrence. Unilateral recurrence was observed in four patients and bilateral one was seen in one patient. Disease free interval varied from 5 months to 7 years and 9 months.
Backgrounds of patients with cervical lymph node recurrence after esophagectomy
| Case . | Age . | Sex . | Pathological stage . | Adjuvant therapy . | Disease-free interval . | Site of recurrence† . |
|---|---|---|---|---|---|---|
| 1 | 60 | Female | T4N3M0, stage IVa | CRT | 5M | 104L |
| 2 | 64 | Female | T3N2M0, stage III | – | 1Y 9M | 104R |
| 3 | 65 | Female | T3N2M0, stage III | – | 3Y 7M | 104L |
| 4 | 66 | Male | T1bN0M0, stage I | – | 7Y 9M | 102upRL |
| 5 | 54 | Male | T2N0M0, stage II | – | 3Y 7M | 101R |
| Case . | Age . | Sex . | Pathological stage . | Adjuvant therapy . | Disease-free interval . | Site of recurrence† . |
|---|---|---|---|---|---|---|
| 1 | 60 | Female | T4N3M0, stage IVa | CRT | 5M | 104L |
| 2 | 64 | Female | T3N2M0, stage III | – | 1Y 9M | 104R |
| 3 | 65 | Female | T3N2M0, stage III | – | 3Y 7M | 104L |
| 4 | 66 | Male | T1bN0M0, stage I | – | 7Y 9M | 102upRL |
| 5 | 54 | Male | T2N0M0, stage II | – | 3Y 7M | 101R |
Numbers indicate lymph node stations according to Japanese guideline. 101, cervical paraesophageal lymph nodes; 102up, upper deep cervical lymph nodes; 104, supraclavicular lymph nodes; 106rec, recurrent nerve lymph nodes; CRT, chemoradiotherapy; L, left; R, right.
Backgrounds of patients with cervical lymph node recurrence after esophagectomy
| Case . | Age . | Sex . | Pathological stage . | Adjuvant therapy . | Disease-free interval . | Site of recurrence† . |
|---|---|---|---|---|---|---|
| 1 | 60 | Female | T4N3M0, stage IVa | CRT | 5M | 104L |
| 2 | 64 | Female | T3N2M0, stage III | – | 1Y 9M | 104R |
| 3 | 65 | Female | T3N2M0, stage III | – | 3Y 7M | 104L |
| 4 | 66 | Male | T1bN0M0, stage I | – | 7Y 9M | 102upRL |
| 5 | 54 | Male | T2N0M0, stage II | – | 3Y 7M | 101R |
| Case . | Age . | Sex . | Pathological stage . | Adjuvant therapy . | Disease-free interval . | Site of recurrence† . |
|---|---|---|---|---|---|---|
| 1 | 60 | Female | T4N3M0, stage IVa | CRT | 5M | 104L |
| 2 | 64 | Female | T3N2M0, stage III | – | 1Y 9M | 104R |
| 3 | 65 | Female | T3N2M0, stage III | – | 3Y 7M | 104L |
| 4 | 66 | Male | T1bN0M0, stage I | – | 7Y 9M | 102upRL |
| 5 | 54 | Male | T2N0M0, stage II | – | 3Y 7M | 101R |
Numbers indicate lymph node stations according to Japanese guideline. 101, cervical paraesophageal lymph nodes; 102up, upper deep cervical lymph nodes; 104, supraclavicular lymph nodes; 106rec, recurrent nerve lymph nodes; CRT, chemoradiotherapy; L, left; R, right.
An extent of salvage lymph node dissection and results of pathological diagnosis are shown in Table 3. For three patients with supraclavicular node recurrence, only the particular station was dissected. For the other patients, all stations containing suspicious nodes were dissected. The number of metastatic nodes was one in three patients and three in two patients. Complete resection was performed in four patients and reduction surgery was done for one patient. In the latter case, complete resection of the recurrent tumor had been considered to be impossible because the tumor invaded the brachial plexus. However, as the recurrent tumor was as large as 4 cm in diameter and the caudal margin of the tumor was included within the radiation field of postoperative CRT, the radiation oncologist judged that control of the disease cannot be achieved by CRT alone. Therefore, a strategy of reduction surgery followed by planned CRT targeting the residual disease was selected.
Sites of dissected and metastatic lymph nodes in addition to the number of metastatic lymph nodes
| Case . | Dissected nodes† . | Metastatic nodes† . | Number of metastatic/dissected nodes . |
|---|---|---|---|
| 1 | 104L | 104L | 1/5 |
| 2 | 104R | 104R | 3/6 |
| 3 | 104L | 104L | 1/4 |
| 4 | 102upRL, 102midRL, 104RL | 102upRL | 3/18 |
| 5 | 101R, 104R, 106recR, 106pre | 101R | 1/13 |
| Case . | Dissected nodes† . | Metastatic nodes† . | Number of metastatic/dissected nodes . |
|---|---|---|---|
| 1 | 104L | 104L | 1/5 |
| 2 | 104R | 104R | 3/6 |
| 3 | 104L | 104L | 1/4 |
| 4 | 102upRL, 102midRL, 104RL | 102upRL | 3/18 |
| 5 | 101R, 104R, 106recR, 106pre | 101R | 1/13 |
Numbers indicate lymph node stations according to Japanese guideline. 101, cervical paraesophageal lymph nodes; 102up, upper deep cervical lymph nodes; 102mid, middle deep cervical lymph nodes; 104, supraclavicular lymph nodes; 106rec, recurrent nerve lymph nodes; 106pre, pretracheal lymph nodes; L, left; R, right.
Sites of dissected and metastatic lymph nodes in addition to the number of metastatic lymph nodes
| Case . | Dissected nodes† . | Metastatic nodes† . | Number of metastatic/dissected nodes . |
|---|---|---|---|
| 1 | 104L | 104L | 1/5 |
| 2 | 104R | 104R | 3/6 |
| 3 | 104L | 104L | 1/4 |
| 4 | 102upRL, 102midRL, 104RL | 102upRL | 3/18 |
| 5 | 101R, 104R, 106recR, 106pre | 101R | 1/13 |
| Case . | Dissected nodes† . | Metastatic nodes† . | Number of metastatic/dissected nodes . |
|---|---|---|---|
| 1 | 104L | 104L | 1/5 |
| 2 | 104R | 104R | 3/6 |
| 3 | 104L | 104L | 1/4 |
| 4 | 102upRL, 102midRL, 104RL | 102upRL | 3/18 |
| 5 | 101R, 104R, 106recR, 106pre | 101R | 1/13 |
Numbers indicate lymph node stations according to Japanese guideline. 101, cervical paraesophageal lymph nodes; 102up, upper deep cervical lymph nodes; 102mid, middle deep cervical lymph nodes; 104, supraclavicular lymph nodes; 106rec, recurrent nerve lymph nodes; 106pre, pretracheal lymph nodes; L, left; R, right.
Operative morbidity and duration of hospital stay are summarized in Table 4. There was no operative mortality. Subcutaneous hemorrhage, which was improved without any interventions, was observed in one patient. Skin ulcer related to irradiation was observed in Case 1 who underwent CRT for residual disease. Median duration of hospital stay was 7 days. A long hospital stay was needed in Case 1 because of CRT following the salvage operation, control of severe pain and treatment for radiation-induced skin ulcer. However, owing to these treatments, a complete remission of the recurrent tumor was finally achieved and the patient was discharged without any analgesics.
Postoperative morbidity and duration of hospital stay
| Case . | Residual disease . | Complication . | In hospital day . |
|---|---|---|---|
| 1 | + | Skin ulcer (caused by radiation) | 119 days† |
| 2 | − | None | 4 days |
| 3 | − | Subcutaneous hemorrhage | 7 days |
| 4 | − | None | 7 days |
| 5 | − | None | 7 days |
| Case . | Residual disease . | Complication . | In hospital day . |
|---|---|---|---|
| 1 | + | Skin ulcer (caused by radiation) | 119 days† |
| 2 | − | None | 4 days |
| 3 | − | Subcutaneous hemorrhage | 7 days |
| 4 | − | None | 7 days |
| 5 | − | None | 7 days |
Including postoperative chemoradiotherapy.
Postoperative morbidity and duration of hospital stay
| Case . | Residual disease . | Complication . | In hospital day . |
|---|---|---|---|
| 1 | + | Skin ulcer (caused by radiation) | 119 days† |
| 2 | − | None | 4 days |
| 3 | − | Subcutaneous hemorrhage | 7 days |
| 4 | − | None | 7 days |
| 5 | − | None | 7 days |
| Case . | Residual disease . | Complication . | In hospital day . |
|---|---|---|---|
| 1 | + | Skin ulcer (caused by radiation) | 119 days† |
| 2 | − | None | 4 days |
| 3 | − | Subcutaneous hemorrhage | 7 days |
| 4 | − | None | 7 days |
| 5 | − | None | 7 days |
Including postoperative chemoradiotherapy.
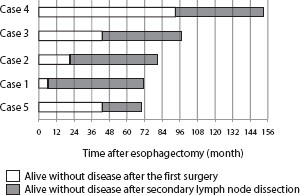
Long-term results of the patients are shown in Figure 2. All five patients including Case 1 are still alive without any recurrent diseases. The survival periods after initial esophagectomy were beyond 5 years in all patients, and the median survival period after the salvage treatment was 60 months.
Long-term results of patients who underwent salvage treatment for their cervical node recurrence. All patients are alive for more than 5 years after initial esophagectomy and are alive without disease after the salvage treatment.
Discussion
Cervical lymph node metastasis from thoracic ESCC has been reported to be a frequent event. Sannohe et al. have first reported in 1981 that thoracic ESCC frequently metastasized to supraclavicular or paracardiac lymph nodes and that jumping metastasis to the neck or the abdominal lymph nodes without intrathoracic involvement was not rare.13 In order to achieve local disease control, 3F-LD during esophagectomy has been introduced in several institutes in Japan since the 1980s. These studies have revealed that cervical lymph node metastasis was observed in 16 to 37% of patients with thoracic ESCC.3–7
Subsequently, several reports that investigated the long-term results of 3F-LD have demonstrated that many of patients with ESCC who have cervical lymph node metastasis can be cured by esophagectomy with 3F-LD.13–15 These results indicate that cervical lymph node metastasis may be cured by surgery. However, the efficacy of secondary cervical node dissection has not been established yet. In this study, we have demonstrated that long-term survival has been achieved by salvage cervical node dissection followed by chemotherapy. There are two other reports that described the usefulness of the salvage surgery against cervical node recurrence. Komatsu et al. treated five patients with the supraclavicular lymph node recurrence with salvage surgery and reported that no local recurrence was observed and long-term survival was obtained in two of them.12 Yano et al. reported the result of treatment for 35 patients with the cervical lymph node recurrence, and concluded that substantial survival can be attained by locoregional treatment if it was a solitary node recurrence.11 These results support the efficacy of the salvage surgery for cervical node recurrence.
The need of preventive supraclavicular lymph node dissection for patients who undergo esophagectomy is still controversial. Several reports that demonstrated the survival benefit of 3F-LD compared with 2F-LD have been published not only from Japan3–5,7 but also from the Western countries.6,16 Udagawa et al. reported that 3F-LD was one of the independent prognostic indicators after esophagectomy.17 On the contrary, Law and Wong reviewed the recurrence pattern of thoracic ESCC and concluded that the benefit from cervical node dissection was very limited.9 In order to clarify the efficacy of preventive cervical node dissection, a randomized control trial that compares 3F-LD with 2F-LD is needed. If the cervical lymph node recurrence could be cured by salvage treatment, such a comparative study can be performed safely.
In our opinion, there are three important points to achieve a successful salvage treatment. At first, an early diagnosis of the cervical node recurrence is essential. It could be obtained from the interval physical examination and US. Especially, an accuracy of US diagnosis on the cervical lymph node metastasis is excellent and it has been reported to be as high as 87.6–94.0%.18,19 Second, lymph node dissection but not ‘pickup’ lymphadenectomy should be performed. There are two reasons; one is that an extracapsular carcinomatous invasion from lymph node metastasis is not rare, and another is that metastasis to multiple nodes within a station is sometimes observed. In this study, we have dissected at least four lymph nodes in each case and multiple nodal metastases were observed in two cases. Third, adjuvant chemotherapy should be done after the salvage surgery. Although survival benefit of chemotherapy for recurrent disease after esophagectomy has not yet been proven, it has been reported that adjuvant chemotherapy prolonged disease-free survival of patients after esophagectomy in node-positive esophageal cancer.20 The adjuvant chemotherapy we performed might have contributed the long-term survival of the patients in this study.
Recently, neoadjuvant chemotherapy or CRT has become a standard strategy for advanced esophageal cancer. Four of five cases in this study have not undergone adjuvant therapy and only 1 patient underwent postoperative CRT for microscopic residual disease. Whether we should perform adjuvant therapy after curative resection of recurrent diseases of patients who had undergone neoadjuvant therapy is still controversial. Although there is no evidence, in our opinion nodal recurrence must be considered as an expression of systemic relapse and thus adjuvant chemotherapy should be performed.
In conclusion, salvage lymph node dissection followed by chemotherapy is an efficient treatment strategy for patients with cervical node recurrence after esophagectomy.