Suspected sepsis: summary of NICE guidance
BMJ 2016; 354 doi: https://doi.org/10.1136/bmj.i4030 (Published 11 August 2016) Cite this as: BMJ 2016;354:i4030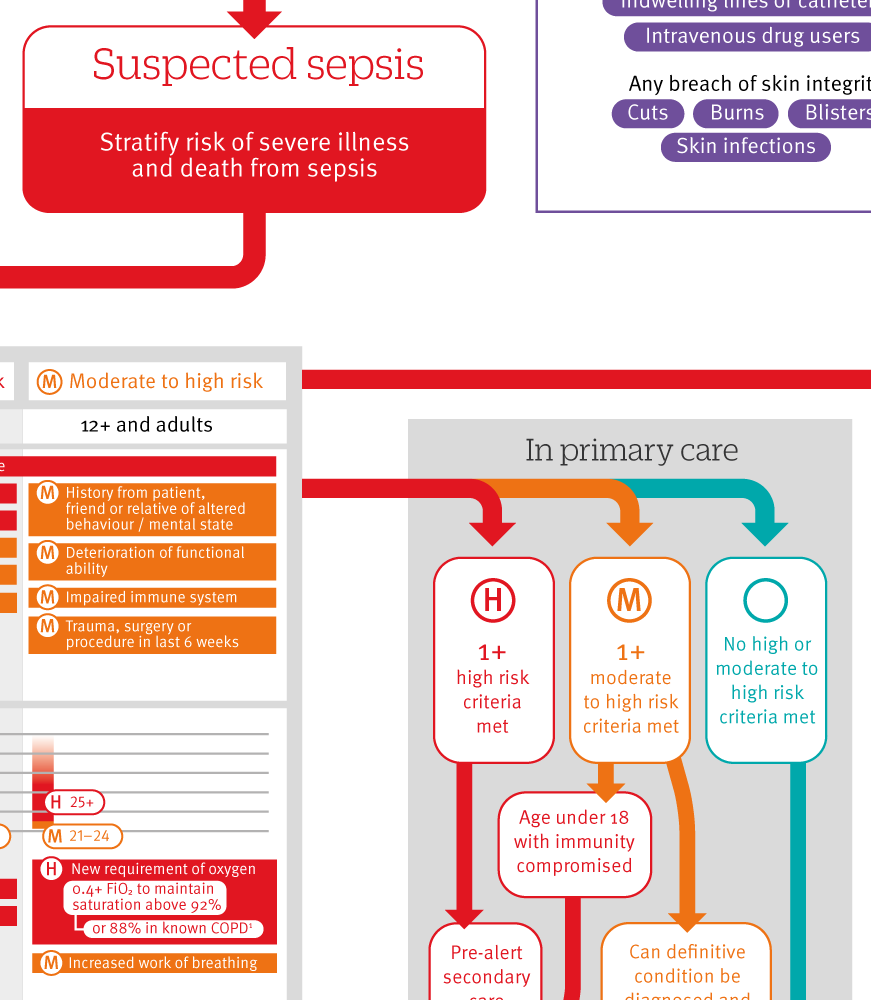
Infographic summary
Click here to see an infographic, summarising risk assessment and management of people with suspected sepsis.
- Andreas Freitag, senior research fellow1,
- Margaret Constanti, senior health economist1,
- Norma O’Flynn, clinical director1,
- Saul N Faust, professor of paediatric immunology and infectious diseases, director2
- on behalf of the Guideline Development Group
- 1National Guideline Centre, Royal College of Physicians, London NW1 4LE, UK
- 2NIHR Wellcome Trust Clinical Research Facility, Faculty of Medicine, University of Southampton and University Hospital Southampton NHS Foundation Trust, Southampton, UK
- Correspondence to: SN Faust, s.faust{at}soton.ac.uk
What you need to know
“Think sepsis” in any person with suspected infection
Sepsis may present with non-specific symptoms and signs and without fever
Have a high index of suspicion of sepsis in those who are aged <1 year or >75 years, pregnant, or immunocompromised, and those who have a device or line in situ or have had recent surgery
Use risk factors and any indicators of clinical concern to decide if full assessment is required
Offer people at high risk of sepsis broad spectrum antibiotics and intravenous fluids in hospital
The UK Parliamentary and Health Service Ombudsman inquiry “Time to Act” found failures in the recognition, diagnosis, and early management of those who died from sepsis,1 which triggered this guidance. In sepsis the body’s immune and coagulation systems are switched on by an infection and cause one or more body organs to malfunction with variable severity. The condition is life threatening. Although most people with infection do not have and will not develop sepsis, non-specific signs and symptoms can lead to late recognition of people who might have sepsis. We would like clinicians to “think sepsis” and recognise symptoms and signs of potential organ failure when they assess someone with infection, in a similar way to thinking “Could this chest pain be cardiac in origin?”
This guidance provides a pragmatic approach for patients with infection who are assessed in the community, emergency departments, and hospitals by a wide range of general and specialist healthcare professionals. It includes guidance on assessment of risk factors followed by a detailed structured assessment of potential clinical signs and symptoms of concern.
Definitions of sepsis have been developed,2 but these offer limited explanation on how to confirm or rule out the diagnosis in general clinical settings or in the community.3 Current mechanisms to diagnose sepsis and …
Log in
Log in using your username and password
Log in through your institution
Subscribe from £173 *
Subscribe and get access to all BMJ articles, and much more.
* For online subscription
Access this article for 1 day for:
£38 / $45 / €42 (excludes VAT)
You can download a PDF version for your personal record.
