Abstract
Objectives
To identify and evaluate intervention studies (ie, experimental study in which the participants undergo some kind of intervention in order to evaluate its impact) that target mental and/or physical health outcomes in women who have experienced stillbirth and to provide specific recommendations for future research and intervention work.
Methods
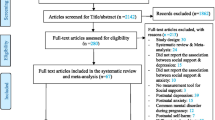
A librarian conducted an initial search using CINAHL, Cochrane Library, PsycInfo, PubMed, SocIndex, and Web of Knowledge in the spring of 2016. Reference mining provided further articles. Articles were eligible if they were: (1) published in English, (2) published in a peer-reviewed journal, (3) published in 1980 or later, (4) an intervention that evaluated (qualitative or quantitative methods) mental and/or physical health, and (5) included women who had experienced a stillbirth (in utero fetal death at ≥20 weeks of gestation).
Results
The combined searches produced 2733 articles (including duplicates). After duplicate articles were removed (n = 928), the research team screened the titles, abstracts, and full texts (when necessary) for eligibility (n = 1805). Two articles were identified that met our eligibility criteria.
Conclusion for Practice
There is a lack of intervention research in women with stillbirth. It is imperative to develop and implement interventions to improve both mental and physical health in this population, especially in the interconception period (ie, stillbirth aftercare). Future intervention research is needed to determine appropriate support and efficacious delivery of support interventions, feasibility and effectiveness of physical activity interventions and complementary approaches, appropriate timing and dose of interventions, and culturally sensitive interventions appropriate for racial/ethnic minority women with stillbirth.
Similar content being viewed by others
References
Silver RM, Varner MW, Reddy U, et al. Work-up of stillbirth: a review of the evidence. Obstet Gynecol. 2007;196(1):433–444.
American Congress of Obstetricians and Gynecologists. ACOG Issues New Guidelines on Managing Stillbirths, http://www.acog.org/About-ACOG/News-Room/News-Releases/2009/ACOG-Issues-New-Guidelines-on-Managing-Stillbirths. Published February 20, 2009. Accessed May 1, 2016.
Froen J, Cacciatore J, McClure E, et al; Lancet’s Stillbirths Series steering committee. Stillbirths: why they matter. Lancet. 2011;377(9774):1353–1366.
Scheidt CE, Hasenburg A, Kunze M, et al. Are individual differ-ences of attachment predicting bereavement outcome after perinatal loss? A prospective cohort study. J Psychosom Res. 2012;73(5):375–382.
MacDorman MF, Kirmeyer SE, Wilson EC. Fetal and perinatal mortality, United States, 2006. Natl Vital Stat Rep. 2012;60(8):1–22.
Stillbirth Collaborative Research Network Writing Group. Causes of death among stillbirths. JAMA. 2011;306(22):2459–2468.
Cacciatore J. Psychological effects of stillbirth. Semin Fetal Neonatal Med. 2013;18(2):76–82.
Wayment HA, Vierthaler J. Attachment style and bereavement reactions. J Loss Trauma. 2002;7(2):129–149.
Gold KJ, Johnson TR. Mothers at risk: maternal mental health outcomes after perinatal death. Obstetr Gynecol. 2014;123 suppl 1:6S–6S.
Hvidtjorn D, Wu C, Schendel D, Thorlund Parner E, Brink Henriksen T. Mortality in mothers after perinatal loss: a population-based follow-up study. BJOG. 2016;123(3):393–398.
Kotelchuck M. Improving the Health of Women following Pregnancy: Inter-Conception Care. 2013. http://www.hrsa.gov/advisorycommittees/mchbadvisory/InfantMortality/Meetings/ 20130424/kotelchuck.pdf. Accessed May 1, 2016.
Dunn AL, Trivedi MH, Kampert JB, Clark CG, Chambliss HO. Exercise treatment for depression: efficacy and dose response. Am J Prev Med. 2005;28(1):1–8.
Teychenne M, York R. Physical activity, sedentary behavior, and postnatal depressive symptoms: a review. Am J Prev Med. 2013;45(2):217–227.
Evenson KR. Towards an understanding of change in physical activity from pregnancy through postpartum. Psychol Sport Exerc. 2011;12(1):36–45.
Lewis B, Avery M, Jennings E, Sherwood N, Martinson B, Crain AL. The effect of exercise during pregnancy on maternal out-comes: practical implications for practice. Am J Lifestyle Med. 2008;2(5):441–455.
Huberty J, Coleman J, Rolfsmeyer K, Wu S. A qualitative study exploring women’s beliefs about physical activity after stillbirth. BMC Pregnancy Childbirth. 2014;14:26–26.
Craft LL, Perna FM. The benefits of exercise for the clinically depressed. Prim Care Companion J Clin Psychiatry. 2004;6(3):104–111.
Da Costa D, Ireland K. Perceived benefits and barriers to leisure-time physical activity during pregnancy in previously inactive and active women. Women Health. 2013;53(2):185–202.
Burden C, Bradley S, Storey C, et al. From grief, guilt pain and stigma to hope and pride—a systematic review and meta-analysis of mixed-method research of the psychosocial impact of stillbirth. BMC Pregnancy Childbirth. 2016;16:1.
Ellis A, Chebsey C, Storey C, et al. Systematic review to under-stand and improve care after stillbirth: a review of parents’ and healthcare professionals’ experiences. BMC Pregnancy Childbirth. 2016;16:16.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. P LoS Med. 2009;6(7):e1000097.
Cacciatore J. The unique experiences of women and their families after the death of a baby. Soc Work Health Care. 2010;49(2):134–148.
Cacciatore J. Effects of support groups on post traumatic stress responses in women experiencing stillbirth. Omega (Westport). 2007;55(1):71–90.
Cacciatore J, Bushfield S. Stillbirth: the mother’s experience and implications for improving care. J Soc Work End Life Palliat Care. 2007;3(3):59–79.
Cacciatore J, Frøen J, Killian M. Condemning self, condemning other: blame and mental health in women suffering stillbirth. J Ment Health Couns. 2013;35:342–359.
Cacciatore J, Rådestad I, Frederik Froen J. Effects of contact with stillborn babies on maternal anxiety and depression. Birth. 2008;35(4):313–320.
Cacciatore J, Schnebly S, Froen JF. The effects of social support on maternal anxiety and depression after stillbirth. Health Soc Care Commun. 2009;17(2):167–176.
Crawley R, Lomax S, Ayers S. Recovering from stillbirth: the effects of making and sharing memories on maternal mental health. J Reprod Lnfant Psychol. 2013;31(2):195.
Gravensteen IK, Helgadottir LB, Jacobsen E, Sandset PM, Eke-berg Ø. Long-term impact of intrauterine fetal death on quality of life and depression: a case-control study. BMC Pregnancy Childbirth. 2012;12:43.
Hogue CJ, Parker CB, Willinger M, et al; Eunice Kennedy Shriver National Institute of Child Health and Human Development Stillbirth Collaborative Research Network Writing Group. The association of stillbirth with depressive symptoms 6–36 months post-delivery. Paediatr Perinat Epidemiol. 2015;29(2):131–143.
Horsch A, Jacobs I, McKenzie-McHarg K. Cognitive predictors and risk factors of PTSD following stillbirth: a short-term long-itudinal study. J Trauma Stress. 2015;28(2):110–117.
Hsu M, Tseng Y, Banks JM, Kuo L. Interpretations of stillbirth. J Adv Nurs. 2004;47(4):408–416.
Huberty J, Leiferman J, Gold K, Rowedder L, Cacciatore J, McClain D. Physical activity and depressive symptoms after still-birth: informing future interventions. BMC Pregnancy Childbirth. 2014;14:391–391.
Huberty JL. Informing future interventions for physical activity and depression symptoms after stillbirth. J Obstetr Gynecol Neonatal Nurs. 2015;44(S1):S63–S64.
Hunfeld JA, Taselaar-Kloos AK, Agterberg G, Wladimiroff JW, Passchier J. Trait anxiety, negative emotions, and the mothers’ adaptation to an infant born subsequent to late pregnancy loss: a case-control study. Prenat Diagn. 1997;17(9):843–851.
Hunfeld JA, Wladimiroff JW, Passchier J. The grief of late pregnancy loss. Patient Educ Couns. 1997;31(1):57–64.
Kuti O, Ilesanmi CE. Experiences and needs of Nigerian women after stillbirth. Lnt J Gynecol Obstet. 2011;113(3):205–207.
Lake M, Knuppel RA, Murphy J, Johnson TM. The role of a grief support team following stillbirth. Am J Obstet Gynecol. 1983;146(8):877–881.
Lake MF, Johnson TM, Murphy J, Knuppel RA. Evaluation of a perinatal grief support team. Obstet Gynecol. 1987;157(5):1203–1206.
Nordlund E, Börjesson A, Cacciatore J, Pappas C, Randers I, Râdestad I. When a baby dies: motherhood, psychosocial care and negative affect. Br J Midwifery. 2012;20(11):780–784.
Râdestad I, Säflund K, Wredling R, et al. Holding a stillborn baby: mothers’ feelings of tenderness and grief. Br J Midwifery. 2009;17(3):178–180.
Râdestad I, Steineck G, Nordin C, Sjögren B. Psychological com-plications after stillbirth—influence of memories and immediate management: population based study. BMJ. 1996;312(7045):1505–1508.
Râdestad I, Surkan PJ, Steineck G, Cnattingius S, Onelöv E, Dickman PW. Long-term outcomes for mothers who have or have not held their stillborn baby. Midwifery. 2009;25(4):422–429.
Radestad I. Stillbirth: care and long-term psychological effects. Br J Midwifery. 2001;9(8):474–480.
Roberts LR, Montgomery SB. Mindfulness-based Intervention for Perinatal Grief after Stillbirth in Rural India. Issues Ment Health Nurs. 2015;36(3):222–230.
Sutan R, Amin RM, Ariffin KB, Teng TZ, Kamal MF, Rusli RZ. Psychosocial impact of mothers with perinatal loss and its contributing factors: an insight. J Zhejiang Univ Sci. 2010;11(3):209–217.
Säflimd K, Wredling R. Differences within couples’ experience of their hospital care and well-being three months after experiencing a stillbirth. Acta Obstet Gynecol Scand. 2006;85(10):1193–1199.
Stringham JG, Riley JH, Ross A. Silent birth: mourning a stillborn baby. Soc Work. 1982;27(4):322–327.
Surkan PJ, Radestad I, Cnattingius S, et al. Events after stillbirth in relation to maternal depressive symptoms: a brief report. Birth. 2008;35(2):153–157.
Surkan P, Radestad I, Cnattingius S, Steineck G, Dickman P. Social support after stillbirth for prevention of maternal depres-sion. Acta Obstet Gynecol Scand. 2009;88(12):1358.
Sutan R, Miskam HM. Psychosocial impact of perinatal loss among Muslim women. BMC Womens Health. 2012;12:15.
Trulsson O, Rådestad I. The silent child: mother’s experiences before, during and after stillbirth. Birth. 2004;31(3):189.
Tseng Y, Chen C, Wang H. Taiwanese women’s process of recovery from stillbirth: a qualitative descriptive study. Res Nurs Health. 2014;37(3):219–228.
Uren TH, Wastell CA. Attachment and meaning-making in peri-natal bereavement. Death Stud. 2002;26(4):279–308.
Gravensteen I, Helgadottir L, Jacobsen E, Rådestad I, Sandset PM, Ekeberg O. Women’s experiences in relation to stillbirth and risk factors for long-term post-traumatic stress symptoms: a retrospective study. BMJ Open. 2013;3(10):e003323.
Debackere KJ, Hill PD, Kavanaugh KL. The parental experience of pregnancy after perinatal loss. J Obstet Gynecol Neonatal Nurs. 2008;37(5):525–537.
Arsenault DC, Marshall R. One foot in-one foot out: weathering the storm of pregnancy after perinatal loss. Res Nurs Health. 2000;23(6):473–485.
Malicka I, Kozlowska A, Wozniewski M, Rymaszewska J, Szczepanska-Gieracha J. The role of social support in women’s health and recovery processes. Psychol Health Med. 2016;21(1):81–91.
Muller ED, Thompson CL. The experience of grief after bereave-ment: a phenomenological study with implications for mental health counseling. J Ment Health Couns. 2003;25(3):183–203.
Smith C, Hancock H, Blake-Mortimer J, Eckert K. A randomised comparative trial of yoga and relaxation to reduce stress and anxiety. Complement Ther Med. 2007;15(2):77–83.
Kinser PA, Bourguignon C, Whaley D, Hauenstein E, Taylor AG. Feasibility, acceptability, and effects of gentle hatha yoga for women with major depression: findings from a randomized con-trolled mixed-methods study. Arch Psychiatr Nurs. 2013;27(3):137–147.
Kowalska J, Olszowa D, Markowska D, Teplik M, Rymaszewska J. Physical activity and childbirth classes during a pregnancy and the level of perceived stress and depressive symptoms in women after childbirth. Psychiatr Pol. 2014;48(5):889–900.
Evenson KR, Barakat R, Brown WJ, et al. Guidelines for physical activity during pregnancy: comparisons from around the world. Am J Lifestyle Med. 2014;8(2):102–121.
Hayes L, Bell R, Robson S, Poston L; UPBEAT Consortium. Association between physical activity in obese pregnant women and pregnancy outcomes: the UPBEAT pilot Study. Ann Nutr Metab. 2014;64(3–4):239–246.
Cnattingius S, Villamor E. Weight change between successive pregnancies and risks of stillbirth and infant mortality: a nation-wide cohort study. Lancet. 2016;387(10018):558–565.
Carrera L, Diéez-Domingo J, Montanana V, Monleón Sancho J, Minguez J, Monleón J. Depression in women suffering perinatal loss. Int J Gynecol Obstet. 1998;62(2):149–153.
Cacciatore J, Lacasse JR, Lietz CA, McPherson J. A parent’s tears: primary results from the traumatic experiences and resiliency study. Omega (Westport). 2014;68(3):183–205.
Christiansen D, Elklit A, Olff M. Parents bereaved by infant death: PTSD symptoms up to 18 years after the loss. Gen Hosp Psychiatry. 2013;35(6):605–611.
Haakstad LA, Voldner N, Bo K. Stages of change model for participation in physical activity during pregnancy. J Pregnancy. 2013;2013:193170–193177.
Gold KJ, Leon I, Boggs ME, Sen A. Depression and posttrau-matic stress symptoms after perinatal loss in a population-based sample. J Womens Health (Larchmt). 2016;25(3):263–269.
Carmichael SL, Blumenfeld YJ, Mayo J, et al; March of Dimes Prematurity Research Center at Stanford University School of Medicine. Prepregnancy obesity and risks of stillbirth. PLoS One. 2015;10(10):e0138549.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huberty, J.L., Matthews, J., Leiferman, J. et al. When a Baby Dies: A Systematic Review of Experimental Interventions for Women After Stillbirth. Reprod. Sci. 24, 967–975 (2017). https://doi.org/10.1177/1933719116670518
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719116670518