Abstract
Background
This study sought to clarify the distribution of intrahepatic micrometastases and elucidate an adequate hepatectomy margin for colorectal carcinoma liver metastases.
Methods
Intrahepatic micrometastases in resected specimens from 90 patients who underwent hepatectomy for colorectal carcinoma liver metastases were examined retrospectively. Intrahepatic micrometastases were defined as microscopic lesions spatially separated from the gross tumor. Distances from these lesions to the hepatic tumor borders were measured histologically, and the density of intrahepatic micrometastases (number of lesions/mm2) calculated relative to the advancing tumor border in a zone <1 cm from the border (close) or ≥1 cm away (distant). Median follow-up time was 127 months.
Results
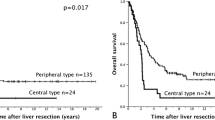
A total of 294 intrahepatic micrometastases were detected in 52 (58%) patients; 95% of these occurred in the close zone. The density of intrahepatic micrometastases was significantly higher in the close zone (mean 74.8 × 10−4 lesions/mm2) than in the distant zone (mean 7.4 × 10−4 lesions/mm2; P < 0.001). Hepatectomy margin status was positive by 0 cm in 10 patients or negative by <1 cm in 51, and by ≥1 cm in 29 patients. The median survival times were 18, 33, and 89 months in patients with hepatectomy margins 0 cm, <1 cm, and ≥1 cm, respectively. Hepatectomy margin status independently influenced survival (P < 0.001) and disease-free survival (P < 0.001).
Conclusion
The currently recommended ≥1 cm hepatectomy margin should remain the goal for resections of colorectal carcinoma liver metastases, based on the distribution of intrahepatic micrometastases and survival risk.





Similar content being viewed by others
References
Charnsangavej C, Clary B, Fong Y, et al. Selection of patients for resection of hepatic colorectal metastases: expert consensus statement. Ann Surg Oncol 2006; 13:1261–8
Fong Y, Fortner J, Sun RL, et al. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg 1999; 230:309–18; discussion 318–21
Choti MA, Sitzmann JV, Tiburi MF, et al. Trends in long-term survival following liver resection for hepatic colorectal metastases. Ann Surg 2002; 235:759–66
Pawlik TM, Scoggins CR, Zorzi D, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg 2005; 241:715–24
Korita PV, Wakai T, Shirai Y, et al. Intrahepatic lymphatic invasion independently predicts poor survival and recurrences after hepatectomy in patients with colorectal carcinoma liver metastases. Ann Surg Oncol 2007; 14:3472–80
Hughes KS, Simon R, Songhorabodi S, et al. Resection of the liver for colorectal carcinoma metastases: a multi-institutional study of indications for resection. Registry of Hepatic Metastases. Surgery 1988; 103:278–88
Ekberg H, Tranberg KG, Andersson R, et al. Determinants of survival in liver resection for colorectal secondaries. Br J Surg 1986; 73:727–31
Cady B, Jenkins RL, Steele GD Jr, et al. Surgical margin in hepatic resection for colorectal metastasis: a critical and improvable determinant of outcome. Ann Surg 1998; 227:566–71
Wray CJ, Lowy AM, Mathews JB, et al. The significance and clinical factors associated with a subcentimeter resection of colorectal liver metastases. Ann Surg Oncol 2005; 12:1–7
Shirabe K, Takenaka K, Gion T, et al. Analysis of prognostic risk factors in hepatic resection for metastatic colorectal carcinoma with special reference to surgical margin. Br J Surg 1997; 84:1077–80
Altendorf-Hofmann A, Scheele J. A critical review of the major indicators of prognosis after resection of hepatic metastases from colorectal carcinoma. Surg Oncol Clin North Am 2003; 12:165–92, xi
Yamamoto J, Sugihara K, Kosuge T, et al. Prognostic support for limited hepatectomy in the treatment of liver metastases from colorectal cancer. Ann Surg 1995; 221:74–8
Kokudo N, Miki Y, Sugai S, et al. Genetic and histological assessment of surgical margins in resected liver metastases from colorectal carcinoma: minimum surgical margins for successful resection. Arch Surg 2002; 137:833–40
Nanko M, Shimada H, Yamaoka H, et al. Micrometastatic colorectal cancer lesions in the liver. Surg Today 1998; 28:707–13
Sasaki A, Aramaki M, Kawano K, et al. Prognostic significance of intrahepatic lymphatic invasion in patients with hepatic resection due to metastases from colorectal carcinoma. Cancer 2002; 95:105–11
Ambiru S, Miyazaki M, Isono T, et al. Hepatic resection for colorectal metastases: analysis of prognostic factors. Dis Colon Rectum 1999; 42:632–9
Yokoyama N, Shirai Y, Ajioka Y, et al. Immunohistochemically detected hepatic micrometastases predict a high risk of intrahepatic recurrence after resection of colorectal carcinoma liver metastases. Cancer 2002; 94:1642–7
Elias D, Cavalcanti A, Sabourin JC, et al. Results of 136 curative hepatectomies with a safety margin of less than 10 mm for colorectal metastases. J Surg Oncol 1998; 69:88–93
Hamady ZZ, Cameron IC, Wyatt J, et al. Resection margin in patients undergoing hepatectomy for colorectal liver metastasis: a critical appraisal of the 1 cm rule. Eur J Surg Oncol 2006; 32:557–63
Bodingbauer M, Tamandl D, Schmid K, et al. Size of surgical margin does not influence recurrence rates after curative liver resection for colorectal cancer liver metastases. Br J Surg 2007; 94:1133–8
Figueras J, Burdio F, Ramos E, et al. Effect of subcentimeter nonpositive resection margin on hepatic recurrence in patients undergoing hepatectomy for colorectal liver metastases: evidences from 663 liver resections. Ann Oncol 2007; 18:1190–5
Greene FL, Page DL, Fleming ID, et al. AJCC Cancer Staging Manual, 6th ed. New York: Springer-Verlag; 2002
Nagakura S, Shirai Y, Yamato Y, et al. Simultaneous detection of colorectal carcinoma liver and lung metastases does not warrant resection. J Am Coll Surg 2001; 193:153–60
Nagakura S, Shirai Y, Suda T, et al. Multiple repeat resections of intra- and extrahepatic recurrences in patients undergoing initial hepatectomy for colorectal carcinoma metastases. World J Surg 2002; 26:141–7
Terminology Committee of the International Hepato-Pancreato-Biliary Association: Chairman, Strasberg SM. The Brisbane 2000 Terminology of Liver Anatomy and Resections. HPB 2000; 2:333–9
Wakai T, Shirai Y, Sakata J, et al. Anatomic resection independently improves long-term survival in patients with T1-T2 hepatocellular carcinoma. Ann Surg Oncol 2007; 14:1356–65
Taylor M, Forster J, Langer B, et al. A study of prognostic factors for hepatic resection for colorectal metastases. Am J Surg 1997; 173:467–71
Therneau TM, Grambsch PM, Fleming TR. Martingale based residuals for survival models. Biometrika 1990; 77:147–60
Cleveland WS. Robust locally weighted regression and smoothing scatterplots. J Am Stat Assoc 1979; 74:829–36
Shirai Y, Wakai T, Ohtani T, et al. Colorectal carcinoma metastases to the liver. Does primary tumor location affect its lobar distribution? Cancer 1996; 77:2213–6
Are C, Gonen M, Zazzali K, et al. The impact of margins on outcome after hepatic resection for colorectal metastasis. Ann Surg 2007; 246:295–300
Busquets J, Pelaez N, Alonso S, et al. The study of cavitational ultrasonically aspirated material during surgery for colorectal liver metastases as a new concept in resection margin. Ann Surg 2006; 244:634–5
Gayowski TJ, Iwatsuki S, Madariaga JR, et al. Experience in hepatic resection for metastatic colorectal cancer: analysis of clinical and pathologic risk factors. Surgery 1994; 116:703–10
Ohlsson B, Stenram U, Tranberg KG. Resection of colorectal liver metastases: 25-year experience. World J Surg 1998; 22:268–77
DeMatteo RP, Palese C, Jarnagin WR, et al. Anatomic segmental hepatic resection is superior to wedge resection as an oncologic operation for colorectal liver metastases. J Gastrointest Surg 2000; 4:178–84
Yasui K, Shimizu Y. Surgical treatment for metastatic malignancies. Anatomical resection of liver metastasis: indications and outcomes. Int J Clin Oncol 2005; 10:86–96
Kokudo N, Tada K, Seki M, et al. Anatomical major resection versus nonanatomical limited resection for liver metastases from colorectal carcinoma. Am J Surg 2001; 181:153–9
Zorzi D, Mullen JT, Abdalla EK, et al. Comparison between hepatic wedge resection and anatomic resection for colorectal liver metastases. J Gastrointest Surg 2006; 10:86–94
Finch RJ, Malik HZ, Hamady ZZ, et al. Effect of type of resection on outcome of hepatic resection for colorectal metastases. Br J Surg 2007; 94:1242–8
Sugiura T, Nagino M, Oda K, et al. Hepatectomy for colorectal liver metastases with macroscopic intrabiliary tumor growth. World J Surg 2006; 30:1902–8
Okano K, Yamamoto J, Moriya Y, et al. Macroscopic intrabiliary growth of liver metastases from colorectal cancer. Surgery 1999; 126:829–34
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wakai, T., Shirai, Y., Sakata, J. et al. Appraisal of 1 cm Hepatectomy Margins for Intrahepatic Micrometastases in Patients with Colorectal Carcinoma Liver Metastasis. Ann Surg Oncol 15, 2472–2481 (2008). https://doi.org/10.1245/s10434-008-0023-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-008-0023-y