Abstract
Purpose
The purpose of this study was to evaluate the accuracy of breast magnetic resonance imaging (MRI) to predict residual lesion size after neoadjuvant chemotherapy (NAC) and to determine the factors that influence the accuracy of response prediction.
Methods
This study comprised 166 patients who underwent MRI before and after NAC, but before surgery. The longest diameter of the residual cancer was measured using MRI and correlated with pathologic findings. Patients were further divided into subgroups according to various radiologic and histopathologic factors. Pathologic complete response (pCR) was defined as the absence of residual invasive cancer cells. The Pearson correlation was used to correlate tumor size as determined by MRI and pathology, and the Mann-Whitney U test and Kruskal-Wallis test were used to compare MRI-pathologic size discrepancies according to various clinical, histopathologic factors, and MRI findings.
Results
Of the 166 women, 40 achieved pCR. The overall sensitivity, specificity, and accuracy for diagnosing invasive residual disease by using MRI were 96, 65, and 89 %, respectively. The Pearson’s correlation coefficient between the tumor sizes measured using MRI and pathology was 0.749 (P < 0.001). The size discrepancy was significantly greater in patients with estrogen receptor-positive cancer (P = 0.037), in cancers with low nuclear grade (P = 0.007), and in cancers shown as diffuse non-mass–like enhancement on MRI (P = 0.001).
Conclusions
Size prediction is less accurate in cases with estrogen receptor-positive breast cancer, low nuclear grade, and diffuse non-mass–like enhancement on initial MRI.
Similar content being viewed by others
Neoadjuvant chemotherapy (NAC) before surgery has been shown to be effective for locally advanced breast cancer and therefore has been used widely in clinical practice. Its many advantages include in vivo responsiveness to the chosen chemotherapeutic agent,1 an inoperable cancer becoming operable,2 or possible micrometastatic lesion eradication.3 Furthermore, patients who have pathologic complete response (pCR) or minimal residual tumor burden following NAC have a favorable prognosis.4 – 6 With the availability of more effective chemotherapy regimens and targeted therapies, the current goal of NAC is to achieve pCR. For patients who undergo NAC, imaging assessment of response may help to select drug regimens, and information about the residual tumor may help with surgical planning.
Magnetic resonance imaging (MRI) has been used widely to evaluate residual tumor extent after NAC, because dynamic contrast material-enhanced MRI has the ability to differentiate between nonvascularized therapy-induced fibrosis and residual vital tumor.7 However, unfortunately, MRI is not always accurate. The radiologic or histopathologic factors that influence its accuracy need to be elucidated to determine the extent of residual tumor, thus enabling better surgical planning and prediction of prognosis. This also may clarify the strengths and weaknesses of MRI in a NAC setting. Therefore, we evaluated the accuracy of breast MRI for evaluating NAC outcomes by correlating MRI findings with histopathology at post-NAC surgery and determined the factors that influence the accuracy of evaluating the extent of residual lesions.
Methods
Patients and Treatment
This retrospective study was approved by our institutional review board, which waived the requirement of informed consent. Patients who had biopsy-confirmed invasive breast cancer with lesion diameter ≥2 cm on MRI and who underwent MRI before and after NAC, but before surgery, between April 2007 and December 2010, were targeted. We excluded patients with bilateral breast cancer at diagnosis. Finally, 166 patients (mean age, 44.0 years; age range, 23–72 years) were enrolled in our study. Patient characteristics are shown in Table 1.
Four different NAC regimens were employed: adriamycin with cyclophosphamide (AC), adriamycin with docetaxel (AT), adriamycin with cyclophosphamide plus docetaxel (AC-T), or human epidermal growth factor receptor 2 (HER2)/neu monoclonal antibody-based chemotherapy, which included AC-T with trastuzumab, docetaxel with pertuzumab, docetaxel with trastuzumab, or trastuzumab with pertuzumab. All patients were treated with four cycles at 3-week intervals according to their regimen protocols.
MRI Technique
A 3.0-T MRI system (Achieva, Philips Medical Systems, Best, The Netherlands) with a dedicated surface breast coil (Philips Medical Systems) was used for breast MRI. Images were acquired with the patient in the prone position. The MRI protocol included bilateral unenhanced and contrast-enhanced, axial T1-weighted, 3D, fast spoiled gradient-recalled sequences. Immediate contrast-enhanced images were acquired at 1.5 min. Delayed contrast-enhanced images were acquired at 3, 4.5, and 7 min after contrast injection. The following scanning parameters were used: TR/TE, 5.5/2.8; slice thickness, 3 mm; matrix size, 500 × 237; field of view, 300; and flip angle, 12°. For the dynamic contrast enhancement, a 0.1-mmol/kg bolus of gadopentetate dimeglumine (Magnevist; Berlex Laboratories, Wayne, NJ) was injected, followed by a 10-mL saline flush.
Radiologic Assessment
Tumor response was evaluated preoperatively using MRI after NAC was completed. MR images were reviewed by one radiologist (E.S.K.; 7 years of experience interpreting breast MRI). The reviewer was blinded to patient information, including breast cancer subtype, NAC regimen, and final pathologic outcome. MRI examinations of each patient before and after NAC were analyzed in one session to ensure interpretative consistency.
MRI tumor size was measured as the longest diameter. For multiple tumors, we measured the maximal tumor diameters of the five largest lesions and the change in the longest diameter of the composite measurement was recorded. CR was diagnosed when no enhancement or faint enhancement in the previous lesion site equal to that of the background normal tissue was noted. Response categories were CR or non-CR according to MRI findings.
To analyze the effect of the initial MRI pattern on the NAC response, we classified the pretreatment tumor pattern on MRI into single mass, multiple mass, diffuse non-mass–like enhancement, and focal non-mass–like enhancement. Non-mass–like enhancements with >1 quadrant involvement were classified as diffuse non-mass–like enhancements; those with <1 quadrant involvement were assessed as focal non-mass–like enhancements.
Histopathologic Analysis
All patients underwent surgery, irrespective of a response in terms of tumor size, following chemotherapy. Mean time between follow-up MRI and surgery was 14 (range, 3–30) days. Residual disease after NAC was categorized as (1) no residual cancer cells, (2) no residual invasive cancer but ductal carcinoma in situ (DCIS), and (3) residual invasive cancer. pCR was defined as no invasive cancer, thus including categories 1 and 2.8 Estrogen receptor (ER), progesterone receptor (PR), and HER2 expression status were determined from histopathologic reports of core biopsies performed before chemotherapy; nuclear grade, lymphovascular invasion, and presence of extensive intraductal component (EIC) were evaluated in the surgical specimen after NAC.
According to pretreatment core biopsies, tumors were classified into three subgroups according to their receptor status: triple-negative (ER–, PR–, HER2–), HER2-positive (HER2+, ER– or ER+, PR– or PR+), and ER-positive (ER+, HER2–, PR– or PR+). ER and PR were considered positive if ≥10 % of nuclei stained positive. Tumors with HER2 scores of 3+ (strong homogeneous staining) were considered positive. In case of 2+ scores (moderate complete membranous staining in ≥10 % of tumor cells), fluorescence in situ hybridization (FISH) was used to determine HER2 amplification (gene copy number ≥6 per tumor cell).
Statistical Analysis
MRI-measured and pathologic residual tumor sizes were compared using Pearson correlation. For each patient, the size discrepancy between MRI and pathologic measurements was calculated. The Kolmogorov-Smirnov test of normality showed that the size discrepancy in each group sorted according to clinicopathologic variables was not normally distributed. Thus, the Kruskal-Wallis test and Mann-Whitney U test were chosen to perform this analysis. SPSS® version 19 (SPSS Inc., Chicago, IL) was used for all statistical analysis. P < 0.05 was considered statistically significant.
Results
Assessment of Tumor Response and Residual Tumor Size after NAC
Table 2 shows comparisons of the response category based on MRI and pathology results. The study included 166 patients. Of these, 31 (18.7 %) showed CR on follow-up MRI. On pathologic examination, 40 (24.1 %) patients showed pCR. MRI findings could accurately diagnose pCR in 26 patients (true negative). Based on Table 2, the MRI diagnostic rates for post-NAC invasive residual disease were as follows: accuracy, 88.6 %; sensitivity, 96 %; specificity, 65 %; positive predictive value, 89.6 %; and negative predictive value, 83.8 %. Five false-negative diagnoses showed no visible tumor on MRI but residual invasive cancer on pathologic examination. Of these, three (60 %) were ER-positive and two (40 %) were HER2-positive breast cancer. In terms of the initial MRI pattern, three (60 %) were diffuse non-mass–like enhancement. The residual lesion size of all lesions on pathology examination was <1 cm (range, 3–9 mm). There were 14 false-positive diagnoses; eight (57.1 %) were HER2-positive, 4 (28.6 %) were triple-negative, and two (14.3 %) were ER-positive breast cancer. In terms of initial MR imaging pattern, five (35.7 %) were single mass, three (21.4 %) were multiple mass, five (35.7 %) were diffuse non-mass–like enhancement, and one (7.1 %) was focal non-mass–like enhancement. Interestingly, among these 14 false-positive diagnoses, the final pathology for ten (71.4 %) revealed DCIS with variable size (range, 9–65 mm; Fig. 1). The Pearson’s correlation coefficient between MRI-measured and pathology-determined tumor size was 0.749 (P < 0.001), indicating a strong correlation between the tumor sizes calculated by the two methods (Fig. 2).
MRI scans of a 30-year-old woman with invasive ductal carcinoma showing ER-positivity/HER2-negativity who received 4 cycles of AT. a Prechemotherapy sagittal contrast-enhanced maximum-intensity projection MRI scan. The image showed a diffuse non-mass-like enhancement measuring 9.6 cm (arrows). b In the postchemotherapy image, the mass had decreased in size to approximately 3.2 cm and appeared as a focal non-mass-like enhancement in the upper breast (arrows). Response was classified as non-CR. Surgery revealed a focal DCIS of up to 0.9 cm but no invasive tumor. Pathologically, she showed CR and was included in the false-positive diagnosis
Analysis of Factors Influencing the Accuracy of MRI for Predicting Residual Lesion
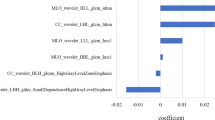
Table 3 shows the discrepancy between tumor sizes based on MRI and pathology measurements according to various clinicopathologic factors. The mean discrepancy was not significantly different according to age, MRI-measured initial tumor size, EIC, and lymphovascular invasion. Measurements tended to be less accurate in patients who had received AT or AC-T, but this difference was not statistically significant (P = 0.305). Statistically significant differences were observed according to breast cancer subtype, nuclear grade, and initial MRI pattern (P = 0.005, 0.007, 0.001, respectively). In terms of tumor subtype, the mean discrepancy was smaller in triple-negative than in ER-positive breast cancer (P = 0.005; Fig. 1). According to initial MRI patterns, diffuse non-mass–like enhancement showed greater discrepancy than the other types (P = 0.001). In low nuclear grade breast cancers, the size discrepancy was bigger (P = 0.007).
Discussion
Several studies have shown that MRI is superior to clinical examination, mammography, and sonography for assessing tumor response following NAC.9 – 12 Furthermore, because achieving pCR is considered the ultimate goal for a favorable prognosis,13 , 14 determining pCR by MRI is important for evaluating NAC response and predicting prognosis. Obviously, an accurate estimation of the residual lesion size is as important as pCR prediction. Thus, we evaluated the accuracy of breast MRI after NAC to predict pCR and its correlation with MRI-measured lesion size. The accuracy rate for predicting pCR was 88.6 %. Pearson’s correlation coefficient between the lesion size measured at follow-up MRI and final pathology was 0.749, a strongly positive correlation (P < 0.001; Fig. 2). Our data suggest that MRI closely depicts the size of malignancy shown at histologic evaluation. However, we also had false-positive and false-negative diagnoses. Our five false-negative diagnoses (no visible mass on MRI, but invasive residual tumor on pathology) were because of the small lesion size (mean, 6.6 mm). Ten (71.4 %) of 14 false-positive lesions revealed to be DCIS were included as pCR. Therefore, small residual lesion size after NAC could result in misinterpretation as pCR and residual DCIS could lead to a false-positive diagnosis. The most debatable issue in the grading classification of pathologic responses after NAC is whether residual DCIS should be considered pCR. Although the impact of DCIS may be negligible with regard to prognosis, it may be an important risk factor for local recurrence after breast-conserving surgery.8 Furthermore, although DCIS and invasive cancer were not differentiated on MRI, only the invasive tumor was regarded as residual disease in pathologic TNM staging. Therefore, in tumors combined with DCIS, overestimation on MRI is inevitable (Fig. 1).
Predictive markers, such as imaging patterns or histopathologic characteristics, may enable tailored therapy in the future and optimized response for those who benefit from chemotherapy. Moreover, elucidating factors that may influence the accuracy of MRI for predicting residual lesion size could be helpful to interpret breast MRI in patients who have received NAC and those with certain combinations of histopathologic or imaging characteristics. Many researchers have studied NAC predictive factors. Colleoni et al. attempted to identify factors predicting response to NAC by analyzing 399 patients sampled prospectively and discovered that initial tumor size is not predictive of pathology response of primary mass.15 ER status and nuclear grade were associated with a high likelihood of complete pathologic response of the primary tumor, independent of the initial tumor size. In a study conducted by Esserman et al.,16 five dominant imaging patterns on pretreatment MRI were noted: circumscribed mass, nodular tissue infiltration, diffuse tissue infiltration, patchy enhancement, and septal spread. Among these, patients with circumscribed mass had the best response to chemotherapy, had the highest grade tumors, and largely displayed ER negativity. Although we did not evaluate the effect of MRI after NAC on the accuracy of lesion size measurement, other authors have studied about that. Based on follow-up MRI, Kim et al.17 classified the tumor pattern as shrinkage, nest or rim, and mixed. They showed that MRI can overestimate residual invasive disease, especially in cases showing a nest or rim pattern in response to chemotherapy or combined lesions with DCIS or multiple scattered nodules. Recently, Loo et al.18 evaluated the relevance of breast cancer subtype on MRI markers of therapy response during NAC in 188 patients with breast cancer and found that MRI visualized the response differently depending on the breast cancer subtype. Changes during NAC correlated well with pathology outcomes for triple-negative and HER2-positive tumors, but not for ER-positive/HER2-negative tumors. They insisted that the imaging characteristics of these subtypes differ as well and that response to chemotherapy can be measured accurately by MRI in some tumors, but not in the largest subgroup, ER-positive/HER2-negative.
In our study, there was no significant difference of size discrepancy between the follow-up MRI and pathology measurements according to initial tumor size (P = 0.066). Triple-negative tumor subtypes were measured most accurately, and ER-positive tumors were the least accurate (P = 0.005). There was little correlation between tumor size measured using MRI and pathology for nuclear grade 1 breast cancer (P = 0.007). Thus, ER-positive breast cancer and low nuclear grade may suggest a poor response following NAC, and MRI may be less accurate in predicting residual lesion size for these cancers. In our study, a diffuse non-mass–like enhancement pattern on initial MRI showed the biggest size discrepancy (P = 0.001). In contrast, single mass or multiple mass patterns were more accurately measured. These findings agree with several previous studies reporting that MRI overestimated nonfocal lesions, including segmental, regional, or diffuse types, which are analogous to the non-mass–like enhancement in our study.19 , 20 Furthermore, correlating with the follow-up MRI pattern, some studies have shown that tumors exhibiting a localized pattern of growth generally shrink concentrically and have higher rates of pCR, whereas tumors that exhibit a diffuse type of growth shrink in a mosaic pattern and have lower rates of pCR.16 , 21 An earlier study demonstrated that MRI-measured size is highly accurate for mass lesions that shrink down to nodules but not as accurate for those that break into scattered cells and clusters.22 In terms of the relationship between tumor morphology and breast cancer subtype, triple-negative breast cancer usually lacks mammographic calcifications associated with DCIS and is more likely to appear as a unifocal mass with a smooth margin or rim-enhancement,23 , 24 and ER-positive/HER2-negative breast cancer is more likely to present as a diffuse lesion.18
Accordingly, we postulate that triple-negative breast cancer commonly presents as a single mass before NAC, shrinks concentrically after NAC, and lesion size prediction is more accurate after this treatment. ER-positive breast cancer commonly presents as diffuse non-mass–like enhancement before treatment, shrinks in a scattered pattern, and lesion size prediction is less accurate after chemotherapy. Although we did not correlate MRI pattern with breast cancer subtype, we believe that our results agree with previous research. Both breast cancer subtype and initial MRI pattern were significant factors that influenced the accuracy of residual lesion measurement.
One interesting thing was the result according to NAC regimen. Although it failed to reach statistical significance, there was a tendency for less accuracy in patients who received AT or AC-T. We suspect that a taxane-induced increase in vascular permeability and capillary protein leakage can lead to augmented gadolinium uptake by the tumor,25 which would produce an over- or underestimation, although some HER2/neu monoclonal antibody-based regimens included docetaxel or paclitaxel in our study.
In conclusion, MRI was a reliable method for evaluating the effect of NAC on pCR and residual lesion size prediction. However, size prediction is less accurate in cases of ER-positive breast cancer and diffuse non-mass–like enhancement on initial MRI. In lesions with low nuclear grade, MRI accuracy also is decreased. In lesions treated with AT or AC-T, accuracy of MRI might be decreased, although there was no statistical significance. Our results show that size prediction using MRI is affected by a combination of clinical and biologic markers and radiological findings. Therefore, if the response following NAC has to be predicted using MRI, the radiologist and the surgeon also must consider the radiologic and histopathologic characteristics of the breast cancer for more accurate and tailored treatment.
References
Chollet P, Amat S, Cure H, de Latour M, Le Bouedec G, Mouret-Reynier MA, et al. Prognostic significance of a complete pathological response after induction chemotherapy in operable breast cancer. Br J Cancer. 2002;86:1041–6.
Fisher B, Brown A, Mamounas E, Wieand S, Robidoux A, Margolese RG, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol. 1997;15:2483–93.
Kim R, Osaki A, Toge T. Current and future roles of neoadjuvant chemotherapy in operable breast cancer. Clin Breast Cancer. 2005;6:223–32.
Rastogi P, Anderson SJ, Bear HD, Geyer CE, Kahlenberg MS, Robidoux A, et al. Preoperative chemotherapy: updates of National Surgical Adjuvant Breast and Bowel Project Protocols B-18 and B-27. J Clin Oncol. 2008;26:778–85.
Jeruss JS, Mittendorf EA, Tucker SL, Gonzalez-Angulo AM, Buchholz TA, Sahin AA, et al. Combined use of clinical and pathologic staging variables to defined outcomes for breast cancer patients treated with neoadjuvant chemotherapy. J Clin Oncol. 2008;26:246–52.
Symmans WF, Peintinger F, Hatzis C, Rajan R, Kuerer H, Valero V , et al. Measurement of residual breast cancer burden to predict survival after neoadjuvant chemotherapy. J Clin Oncol. 2007;25:4414–22.
Padhani AR, Hayes C, Assersohn L, Powles T, Makris A, Suckling J, et al. Prediction of clinicopathologic response of breast cancer to primary chemotherapy at contrast-enhanced MR imaging: initial clinical results. Radiology. 2006;239:361–74.
Jones RL, Lakhani SR, Ring AE, Ashley S, Walsh G, Smith IE. Pathological complete response and residual DCIS following neoadjuvant chemotherapy for breast carcinoma. Br J Cancer. 2006;94:358–62.
Balu-Maestro C, Chapellier C, Bleuse A, Chanalet I, Chauvel C, Largillier R. Imaging in evaluation of response to neoadjuvant breast cancer treatment benefits of MRI. Breast Cancer Res Treat. 2002;72:145–52.
Abraham DC, Jones RC, Jones SE, Cheek JH, Peters GN, Knox SM, et al. Evaluation of neoadjuvant chemotherapeutic response of locally advanced breast cancer by magnetic resonance imaging. Cancer. 1996;78:91–100.
Weatherall PT, Evans GF, Metzger GJ, Saborrian MH, Leitch AM. MRI vs. histologic measurement of breast cancer following chemotherapy: comparison with x-ray mammography and palpation. J Magn Reson Imaging. 2001;13:868–75.
Cocconi G, Di Blasio B, Alberti G, Bisagni G, Botti E, Peracchia G. Problems in evaluating response of primary breast cancer to systemic therapy. Breast Cancer Res Treat. 1984;4:309–13.
Chaturvedi S, McLaren C, Schofield AC, Ogston KN, Sarkar TK, Hutcheon AW, et al. Patterns of local and distant disease relapse in patients with breast cancer treated with primary chemotherapy: do patients with a complete pathological response differ from those with residual tumor in the breast? Breast Cancer Res Treat. 2005; 93:151–8.
von Minckwitz G, Untch M, Loibl S. Update on neoadjuvant/preoperative therapy of breast cancer: experiences from the German Breast Group. Curr Opin Obstet Gynecol. 2012;25(1):66–73.
Colleoni M, Viale G, Zahrieh D, Pruneri G, Gentilini O, Veronesi P, et al. Chemotherapy is more effective in patients with breast cancer not expressing steroid hormone receptors: a study of preoperative treatment. Clin Cancer Res. 2004;10:6622–8.
Esserman L, Kaplan E, Partridge S, Tripathy D, Rugo H, Park J, et al. MRI phenotype is associated with response to doxorubicin and cyclophosphamide neoadjuvant chemotherapy in stage III breast cancer. Ann Surg Oncol. 2001;8:549–59.
Kim HJ, Im YH, Han BK, Choi N, Lee J, Kim JH, et al. Accuracy of MRI for estimating residual tumor size after neoadjuvant chemotherapy in locally advanced breast cancer: relation to response patterns on MRI. Acta Oncol. 2007;46:996–1003.
Loo CE, Straver ME, Rodenhuis S, Muller SH, Wesseling J, Vrancken Peeters MJ, et al. Magnetic resonance imaging response monitoring of breast cancer during neoadjuvant chemotherapy: relevance of breast cancer subtype. J Clin Oncol. 2011;29:660–6.
Partridge SC, Gibbs JE, Lu Y, Esserman LJ, Sudilovsky D, Hylton NM. Accuracy of MRI imaging for revealing residual breast cancer in patients who have undergone neoadjuvant chemotherapy. AJR Am J Roentgenol. 2002;179:1193–9.
Rosen EL, Blackwell KL, Baker JA, Soo MS, Bentley RC, Yu D, et al. Accuracy of MRI in the detection of residual breast cancer after neoadjuvant chemotherapy. AJR Am J Roentgenol. 2003;181:1275–82.
Akashi-Tanaka S, Fukutomi T, Sato N, , Iwamoto E, Watanabe T, Katsumata N, et al. The use of contrast-enhanced computed tomography before neoadjuvant chemotherapy to identify patients likely to be treated safely with breast-conserving surgery. Ann Surg. 2004;239:238–43.
Bahri S, Chen JH, Mehta RS, Carpenter PM, Nie K, Kwon SY, et al. Residual breast cancer diagnosed by MRI in patients receiving neoadjuvant chemotherapy with and without bevacizumab. Ann Surg Oncol. 2009;19:1619–28.
Yang WT, Dryden M, Broglio K, Gilcrease M, Dawood S, Dempsey PJ, et al. Mammographic features of triple receptor-negative primary breast cancers in young premenopausal women. Breast Cancer Res Treat. 2008;111:405–10.
Uematsu T, Kasami M, Yuen S. Triple-negative breast cancer: correlation between MR imaging and pathologic findings. Radiology. 2009;250:638–47.
Delille JP, Slanetz PJ, Yeh ED, Halpern EF, Kopans DB, Garrido L. Invasive ductal breast carcinoma response to neoadjuvant chemotherapy: noninvasive monitoring with functional MR imaging pilot study. Radiology. 2003;228:63–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ko, E.S., Han, BK., Kim, R.B. et al. Analysis of Factors that Influence the Accuracy of Magnetic Resonance Imaging for Predicting Response after Neoadjuvant Chemotherapy in Locally Advanced Breast Cancer. Ann Surg Oncol 20, 2562–2568 (2013). https://doi.org/10.1245/s10434-013-2925-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-013-2925-6