Published online Jan 7, 2022. doi: 10.12998/wjcc.v10.i1.71
Peer-review started: August 10, 2021
First decision: September 2, 2021
Revised: October 21, 2021
Accepted: November 23, 2021
Article in press: November 23, 2021
Published online: January 7, 2022
Surgical site infection is a rare but serious complication associated with total joint arthroplasty (TJA). There are limited data on the effectiveness of intrawound irrigation with vancomycin solution (1000 mg/L; 2 L) before wound closure for preventing acute surgical site infection following primary total hip arthroplasty (THA) and total knee arthroplasty (TKA).
To investigate the effectiveness of prophylactic intraoperative application of vancomycin (1000 mg/L; 2 L) solution vs. plain irrigation in reducing the incidence of acute surgical site infection following primary THA and TKA.
A retrospective review of 2725 consecutive patients undergoing THA or TKA from January 2012–December 2019 was performed. These patients received either intrawound irrigation with normal saline before wound closure between January 2012 and December 2015 (group 1, 1018 patients; 453 undergoing THA and 565 undergoing TKA) or intrawound irrigation with vancomycin solution (1000 mg/L) before wound closure between January 2016 and December 2019 (group 2, 1175 patients; 512 undergoing THA and 663 undergoing TKA). The outcomes were the incidences of postoperative surgical site infection and wound healing complications within 3 mo of primary TJA.
There were no significant demographic differences between the 2 groups. There was a significantly higher incidence of acute infection at the surgical site in patients who received intrawound irrigation with normal saline before wound closure than in those who received intrawound irrigation with vancomycin solution (1000 mg/L; 2 L) before wound closure (overall incidence of infection: group 1, 2.46% vs group 2, 0.09%, P < 0.001). There was no significant difference in the incidence of wound healing complications between the two groups.
Prophylactic irrigation with vancomycin solution (1000 mg/L; 2 L) significantly decreases the incidence of acute surgical site infection after primary TJA. This strategy is a safe, efficacious, and inexpensive method for reducing the incidence of acute surgical site infection after TJA.
Core Tip: Prophylactic irrigation with vancomycin solution (1000 mg/L; 2 L) significantly decreases the incidence of acute surgical site infection after primary total joint arthroplasty (TJA). This represents a safe, efficacious, and inexpensive method for reducing the incidence of acute surgical site infection after TJA.
- Citation: Duan MY, Zhang HZ. Vancomycin lavage for the incidence of acute surgical site infection following primary total hip arthroplasty and total knee arthroplasty. World J Clin Cases 2022; 10(1): 71-78
- URL: https://www.wjgnet.com/2307-8960/full/v10/i1/71.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i1.71
Total joint arthroplasty (TJA) is highly effective for reducing pain and improving quality of life in patients requiring joint replacement[1]. However, implant infections remain a relatively rare but devastating complication associated with this procedure[2-5]. Although improved sterile techniques, wound protection, minimization of contamination, and prophylactic antibiotics (systemic or local antibiotics) have markedly reduced the incidence of surgical site infection following TJA, implants may become infected by direct contact with an infected wound during the procedure or by spread of a superficial wound infection to the fascia lata or bloodborne contamination during or after the procedure[6]. Intraoperative contamination of the surgical wound by bacterial seeding from the air of the operating room, the skin of the patient, or fallen debris or hair from surgical staff is an important cause of surgical site infection following TJA[7-10]. In addition, TJA can lead to hematoma formation, which creates conditions that encourage bacterial growth[10,11], and bacteria can form biofilms that protect them from antimicrobials and the patients’ immune response, thus making eradication difficult.
The incidence of postoperative wound infection is estimated to be 0.5%-2% following primary TJA and 3%-7% following revision TJA[6,7,12]. Local application of an antibiotic solution may reduce the contamination of wounds with commensal bacteria from the patient’s skin or with airborne bacteria during TJA. Prior studies have demonstrated that compared with plain irrigation, lavage of the surgical wound with diluted vancomycin before closure can decrease the rate of infection following arthroscopic surgery[13-20]. Therefore, the purpose of this retrospective study was to investigate the effectiveness of prophylactic intraoperative application of vancomycin (1000 mg/L; 2 L) solution vs. plain irrigation in reducing the incidence of acute surgical site infection following primary total hip arthroplasty (THA) and total knee arthroplasty (TKA).
After institutional review board approval, we reviewed data for 2725 consecutive patients undergoing primary THA or primary TKA between January 2012 and December 2019 with a minimum of 3 mo of follow-up. One surgeon performed all the procedures in the given time period. Patients were identified, and data related to patient demographics, baseline characteristics, and comorbidities and operative data were collected from medical records. These cases were retrospectively reviewed for the occurrence of surgical site infections within 3 mo after surgery.
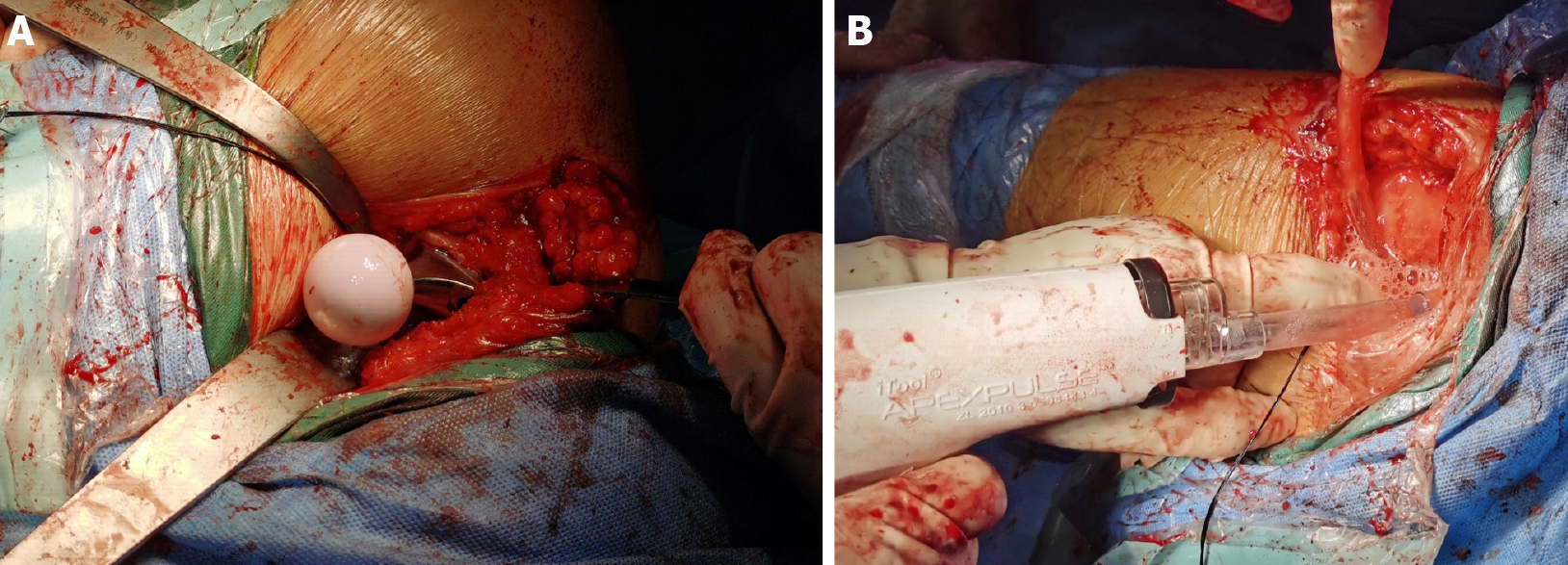
Each patient received standard antibiotic prophylaxis (2 g cefazolin) approximately 30 min before surgery. Antibiotic-loaded cement was used in patients with a higher risk for infection due to a body mass index of > 35, diabetes mellitus, or rheumatoid arthritis. The first 1018 patients (453 undergoing THA and 565 undergoing TKA) received irrigation with 2 L of normal saline after hardware implantation during THA between January 2012 and December 2015 (control group); the subsequent 1175 patients (512 undergoing THA and 663 undergoing TKA) received irrigation with 2 L of vancomycin (1000 mg/L) before wound closure between January 2016 and December 2019 (vancomycin group). Postoperatively, all patients were provided routine antibiotics (1000 mg cefazolin/8 h or 1000 mg vancomycin/12 h for patients who were allergic to penicillin) for 24 h (Figure 1).
Acute infections that occurred within the period of interest were classified as superficial or deep. Superficial infections were defined as infections in which the sutures and anastomosis of the fascial layer were intact without pus or fistula draining from the subfascial layer during debridement. Deep infections were defined as infections involving the drainage of pus from the subfascial layer, with the subfascial layer being open. Superficial wound infections were managed with superficial debridement and antibiotics. Deep infections were treated with debridement, an antibiotic-loaded bone cement spacer, and two-stage revision. Postoperative wound complications such as minor fat liquefaction or erythema were treated with routine wound care. The 3-mo period investigated in this study was defined as the acute infection phase based on the authors’ clinical experience, which indicates that 95% of infections occur within this time frame.
All analyses were conducted using SPSS version 21.0 software. Between-group differences for continuous variables were evaluated using Student’s t-test. Between-group differences in the rate of surgical site infection were assessed using the χ2 test with Yates; correction or the χ2 test alone when the sample size was < 20 or any value was < 5. Statistical significance was defined as P < 0.05.
There were no significant differences in sex, age, duration of surgical procedure, or use of antibiotic-loaded cement between the two groups (Table 1). There was a significantly higher incidence of acute infection at the surgical site in patients who received intrawound irrigation with normal saline prior to wound closure than in patients who received intrawound irrigation with vancomycin solution (1000 mg/L; 2 L) prior to wound closure (Table 2). The overall incidence of infection in group 1 was 2.46%, and that in group 2 was 0.09% (P < 0.001).
| Risk factor | Group 1 (n = 1018) | Group 2 (n = 1175) | P value |
| Sex, male (%) | 46.95 | 48.09 | 0.5971 |
| Age (mean ± SD), yr | 59.59 ± 10.25 | 59.98 ± 10.38 | 0.3702 |
| BMI (mean ± SD), kg/m2 | 27.50 ± 4.67 | 27.83 ± 4.82 | 0.1022 |
| Antibiotic-loaded cement usage (%) | 18.96 | 20.26 | 0.4461 |
| Indication for primary TJA (%) | |||
| Osteoarthritis | 81.34 | 80.85 | 0.7341 |
| Avascular necrosis | 4.91 | 4.34 | 0.5251 |
| Inflammatory | 2.95 | 2.13 | 0.2211 |
| Other | 10.80 | 12.68 | 0.1751 |
All patients with acute infection at the surgical site presented with surgical site pain and fever. All 25 patients with infection at the surgical site yielded positive bacteriologic cultures. In the normal saline group, sixteen patients were positive for Staphylococcus epidermidis, and 9 patients were positive for Staphylococcus aureus. In this same group, 80% (20/25) of the patients with postoperative infection developed the infection within 3 wk (9-20 d).
Only one patient in the vancomycin group had an acute superficial infection at the surgical site (occurring within 2 wk), and the infecting organism was Staphylococcus epidermidis.
No significant differences in wound healing or the incidence of complications were observed between the vancomycin group and the normal saline group.
This retrospective review of patients undergoing primary TJA, which was undertaken by a single-surgeon team over a ten-year period, suggests that compared with irrigation with normal saline alone, intraoperative irrigation with vancomycin solution (1000 mg/L; 2 L) can significantly reduce the incidence of acute infection of the surgical site following primary THA and primary TKA (2.46% vs 0.09%, P < 0.01).
High concentrations of antibiotics in the surgical wound are necessary to prevent infection throughout the operation from incision to wound closure[18]. Unfortunately, intravenous application yields a relatively low concentration of antibiotics at the surgical site over time (generally above the minimal inhibitory concentration for < one hour)[18]. Minimal toxicity is not associated with the generation of microbial resistance[21,22]. Surgical wounds contain areas that are not reachable by intra
Intraoperative contamination of the wound is an important risk factor for surgical site infection after joint replacement[7-10]. Wound contamination may result from commensal organisms (present on the patient’s skin), airborne bacteria, and occasionally, debris or hair falling from the surgical staff[7-10]. Prophylactic antibiotics have been used to reduce surgical site infections. However, the overuse and misuse of antibiotics in recent years has led to the development of antibiotic-resistant pathogens. Irrigation of surgical wounds with antiseptics has been used to prevent infections during the treatment of open fractures and other surgically related conditions. Vancomycin is an effective prophylactic systemic antibiotic that is used during total knee or hip arthroplasty and drastically reduces the risk of infection[14-17]. Intrawound application of vancomycin powder has been proven to reduce infection rates following spine surgery and to decrease the incidence of surgical site infections; however, the data regarding the use of vancomycin powder during primary TJA are controversial[19,21-25]. In 2010, a prospective, controlled study evaluating the safety and effectiveness of an absorbable calcium hydroxyapatite (Hac) layer mixed with vancomycin and applied to the articular surface of prosthetic implants in preventing deep infections after non-cemented TKA was conducted[19]. Vancomycin paste (a mixture of 2 g absorbable Hac and 1-2 g vancomycin) was applied to the implants in the study group. The rate of early infection was 0% in the study group and 4.1% in the control group. This study shows that local anti-infection treatment is an effective supplement to systemic antibiotic therapy for the prevention of deep infections in non-cemented TKA. The pharmacokinetics of vancomycin powder in thirty-four TJA patients who received 2 g of vancomycin powder intraoperatively were investigated[23]. Serum and wound concentrations were measured at multiple intervals in the 24-h period after closure. The wound concentrations were 922 μg/mL 3 h after closure and 207 μg/mL at 24 h. Vancomycin powder application during TJA produced high therapeutic intrawound concentrations while yielding low systemic levels. However, in 2017, the safety of using vancomycin powder to reduce infection rates was investigated by reviewing the incidence of acute postoperative complications[24]. It was found that compared with control treatment, vancomycin powder was associated with an increased rate of sterile wound complications (4.4% vs 0%)[24]. The rate of prosthetic joint infection (PJI) was decreased with the use of vancomycin powder (5.5% vs 0.7%). Researchers therefore do not recommend for or against the use of vancomycin powder at the time of wound closure to prevent PJI. Furthermore, a controlled trial was conducted to investigate the efficacy and side effects of local high-dose vancomycin powder application to the joint to prevent PJI following TKA[25]. They found that intrawound administration of vancomycin powder did not decrease the occurrence of PJI following primary TKA and caused aseptic wound complications. Thus, the use of intrawound and intravenous agents for the prevention of PJI after primary TKA is not recommended.
In the present study, no surgical site infections occurred during the 3 mo after surgery in primary TJA patients who received intrawound irrigation with vancomycin solution before wound closure. Intrawound irrigation with vancomycin solution (1000 mg/L; 2 L) before wound closure may create a potent bactericidal environment by producing a high local tissue concentration of antibiotics. A similar technique during TJA was recently described[18]. A study involving > 2000 patients was performed to evaluate the effectiveness of local antibiotic irrigation during surgery for the prevention of acute postoperative infections after TJA. The intraoperative protocol included irrigation with normal saline containing 1000 mg/L vancomycin and 250000 units/L polymyxin at a rate of 2 L per hour. The researchers found that the use of antibiotic irrigation during arthroplasty surgery was highly effective in preventing infection and reported that irrigation with local antibiotics can prevent acute infection, even with prolonged operating times during revision procedures. However, there was a lack of a control group in the study.
This study showed that the prophylactic use of vancomycin solution can significantly decrease the incidence of acute surgical site infection following primary THA and TKA. However, the present investigation had several limitations. First, it was a retrospective study. Second, all patients had a minimum follow-up of 3 mo (acute infection); a longer follow-up period will help detect delayed infections. Third, other factors, such as hip joint materials (ceramic-ceramic and metal-polyethylene), affected the scores in the study, which might have influenced the results between the 2 groups. A prospective, double-blind randomized controlled trial would eliminate these potentially confounding factors.
Prophylactic irrigation with vancomycin solution (1000 mg/L; 2 L) significantly reduces the incidence of infection after primary TJA. This strategy is a safe, efficacious, and inexpensive method for reducing the incidence of surgical site infection after TJA.
Total joint arthroplasty (TJA) is highly effective for reducing pain and improving quality of life in patients requiring joint replacement. However, implant infections remain a relatively rare but devastating complication associated with this procedure. Although improved sterile techniques, wound protection, minimization of contamination, and prophylactic antibiotics (systemic or local antibiotics) have markedly reduced the incidence of surgical site infection following TJA, implants may become infected by direct contact with an infected wound during the procedure or by spread of a superficial wound infection to the fascia lata or bloodborne contamination during or after the procedure. Intraoperative contamination of the surgical wound by bacterial seeding from the air of the operating room, the skin of the patient, or fallen debris or hair from surgical staff is an important cause of surgical site infection following TJA. In addition, TJA can lead to hematoma formation, which creates conditions that encourage bacterial growth, and bacteria can form biofilms that protect them from antimicrobials and the patients’ immune response, thus making eradication difficult.
The incidence of postoperative wound infection is estimated to be 0.5%-2% following primary TJA and 3%–7% following revision TJA. Local application of an antibiotic solution may reduce the contamination of wounds with commensal bacteria from the patient’s skin or with airborne bacteria during TJA. Prior studies have demonstrated that compared with plain irrigation, lavage of the surgical wound with diluted vancomycin before closure can decrease the rate of infection following arthroscopic surgery.
Prior studies have demonstrated that compared with plain irrigation, lavage of the surgical wound with diluted vancomycin before closure can decrease the rate of infection following arthroscopic surgery.
One surgeon performed all the procedures in the given time period. Patients were identified, and data related to patient demographics, baseline characteristics, and comorbidities and operative data were collected from medical records. These cases were retrospectively reviewed for the occurrence of surgical site infections within 3 mo after surgery. Each patient received standard antibiotic prophylaxis (2 g cefazolin) approximately 30 min before surgery. Antibiotic-loaded cement was used in patients with a higher risk for infection due to a body mass index of > 35, diabetes mellitus, or rheumatoid arthritis.
There were no significant differences in sex, age, duration of surgical procedure, or use of antibiotic-loaded cement between the two groups. There was a significantly higher incidence of acute infection at the surgical site in patients who received intrawound irrigation with normal saline prior to wound closure than in patients who received intrawound irrigation with vancomycin solution prior to wound closure. The overall incidence of infection in group 1 was 2.46%, and that in group 2 was 0.09%.
Prophylactic irrigation with vancomycin solution significantly reduces the incidence of infection after primary TJA. This strategy is a safe, efficacious, and inexpensive method for reducing the incidence of surgical site infection after TJA.
Prophylactic irrigation with vancomycin solution is a safe, efficacious, and inexpensive method for reducing the incidence of surgical site infection after TJA.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Duca FD S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Småbrekke A, Espehaug B, Havelin LI, Furnes O. Operating time and survival of primary total hip replacements: an analysis of 31,745 primary cemented and uncemented total hip replacements from local hospitals reported to the Norwegian Arthroplasty Register 1987-2001. Acta Orthop Scand. 2004;75:524-532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Davis JS. Management of bone and joint infections due to Staphylococcus aureus. Intern Med J. 2005;35 Suppl 2:S79-S96. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 70] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Perencevich EN, Sands KE, Cosgrove SE, Guadagnoli E, Meara E, Platt R. Health and economic impact of surgical site infections diagnosed after hospital discharge. Emerg Infect Dis. 2003;9:196-203. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 332] [Cited by in F6Publishing: 336] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 4. | Krause R, Hoenigl M, Valentin T, Zollner-Schwetz I. Debridement, antibiotic therapy, and implant retention in Staphylococcus aureus prosthetic joint infections. Clin Infect Dis. 2013;56:1842-1843. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004;351:1645-1654. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2193] [Cited by in F6Publishing: 2045] [Article Influence: 102.3] [Reference Citation Analysis (0)] |
| 6. | Gaine WJ, Ramamohan NA, Hussein NA, Hullin MG, McCreath SW. Wound infection in hip and knee arthroplasty. J Bone Joint Surg Br. 2000;82:561-565. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 85] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 7. | Ridgeway S, Wilson J, Charlet A, Kafatos G, Pearson A, Coello R. Infection of the surgical site after arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:844-850. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 313] [Cited by in F6Publishing: 321] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 8. | McLorinan GC, Glenn JV, McMullan MG, Patrick S. Propionibacterium acnes wound contamination at the time of spinal surgery. Clin Orthop Relat Res. 2005;67-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 66] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Charnley J, Eftekhar N. Postoperative infection in total prosthetic replacement arthroplasty of the hip-joint. With special reference to the bacterial content of the air of the operating room. Br J Surg. 1969;56:641-649. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 312] [Cited by in F6Publishing: 329] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 10. | Soohoo NF, Zingmond DS, Lieberman JR, Ko CY. Optimal timeframe for reporting short-term complication rates after total knee arthroplasty. J Arthroplasty. 2006;21:705-711. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Galat DD, McGovern SC, Hanssen AD, Larson DR, Harrington JR, Clarke HD. Early return to surgery for evacuation of a postoperative hematoma after primary total knee arthroplasty. J Bone Joint Surg Am. 2008;90:2331-2336. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 70] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Jämsen E, Huhtala H, Puolakka T, Moilanen T. Risk factors for infection after knee arthroplasty. A register-based analysis of 43,149 cases. J Bone Joint Surg Am. 2009;91:38-47. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 339] [Cited by in F6Publishing: 308] [Article Influence: 20.5] [Reference Citation Analysis (0)] |
| 13. | Davis N, Curry A, Gambhir AK, Panigrahi H, Walker CR, Wilkins EG, Worsley MA, Kay PR. Intraoperative bacterial contamination in operations for joint replacement. J Bone Joint Surg Br. 1999;81:886-889. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 96] [Cited by in F6Publishing: 123] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 14. | Pérez-Prieto D, Portillo ME, Torres-Claramunt R, Pelfort X, Hinarejos P, Monllau JC. Contamination occurs during ACL graft harvesting and manipulation, but it can be easily eradicated. Knee Surg Sports Traumatol Arthrosc. 2018;26:558-562. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 15. | Baron JE, Shamrock AG, Cates WT, Cates RA, An Q, Wolf BR, Bollier MJ, Duchman KR, Westermann RW. Graft Preparation with Intraoperative Vancomycin Decreases Infection After ACL Reconstruction: A Review of 1,640 Cases. J Bone Joint Surg Am. 2019;101:2187-2193. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 43] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 16. | Offerhaus C, Balke M, Hente J, Gehling M, Blendl S, Höher J. Vancomycin pre-soaking of the graft reduces postoperative infection rate without increasing risk of graft failure and arthrofibrosis in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2019;27:3014-3021. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 17. | Figueroa D, Figueroa F, Calvo R, Lopez M, Goñi I. Presoaking of Hamstring Autografts in Vancomycin Decreases the Occurrence of Infection Following Primary Anterior Cruciate Ligament Reconstruction. Orthop J Sports Med. 2019;7:2325967119871038. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Whiteside LA. Prophylactic peri-operative local antibiotic irrigation. Bone Joint J. 2016;98-B:23-26. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 31] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 19. | Assor M. Noncemented total knee arthroplasty with a local prophylactic anti-infection agent: a prospective series of 135 cases. Can J Surg. 2010;53:47-50. [PubMed] [Cited in This Article: ] |
| 20. | Patel NN, Guild GN 3rd, Kumar AR. Intrawound vancomycin in primary hip and knee arthroplasty: a safe and cost-effective means to decrease early periprosthetic joint infection. Arthroplast Today. 2018;4:479-483. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 21. | Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J. Diagnosing periprosthetic joint infection: has the era of the biomarker arrived? Clin Orthop Relat Res. 2014;472:3254-3262. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 255] [Cited by in F6Publishing: 264] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 22. | Greenblatt DJ, Koch-Weser J. Clinical pharmacokinetics (second of two parts). N Engl J Med. 1975;293:964-970. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 108] [Cited by in F6Publishing: 132] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 23. | Johnson JD, Nessler JM, Horazdovsky RD, Vang S, Thomas AJ, Marston SB. Serum and Wound Vancomycin Levels After Intrawound Administration in Primary Total Joint Arthroplasty. J Arthroplasty. 2017;32:924-928. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 24. | Dial BL, Lampley AJ, Green CL, Hallows R. Intrawound Vancomycin Powder in Primary Total Hip Arthroplasty Increases Rate of Sterile Wound Complications. Hip Pelvis. 2018;30:37-44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 25. | Hanada M, Nishikino S, Hotta K, Furuhashi H, Hoshino H, Matsuyama Y. Intrawound vancomycin powder increases post-operative wound complications and does not decrease periprosthetic joint infection in primary total and unicompartmental knee arthroplasties. Knee Surg Sports Traumatol Arthrosc. 2019;27:2322-2327. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |