Published online Nov 26, 2018. doi: 10.12998/wjcc.v6.i14.767
Peer-review started: May 31, 2018
First decision: July 17, 2018
Revised: August 2, 2018
Accepted: October 17, 2018
Article in press: October 16, 2018
Published online: November 26, 2018
To elucidate the effect of antithrombotic therapy (ATT) on bleeding and thromboembolic complications during or after laparoscopic digestive surgery.
Published articles or internationally accepted abstracts between 2000 and 2017 were searched from PubMed, Cochrane Database, and Google Scholar, and studies involving laparoscopic digestive surgery and antiplatelet therapy (APT) and/or anticoagulation therapy (ACT) were included after careful review of each study. Data such as study design, type of surgical procedures, antithrombotic drugs used, and surgical outcome (both bleeding and thromboembolic complications) were extracted from each study.
Thirteen published articles and two internationally accepted abstracts were eligible for inclusion in the systematic review. Only one study concerning elective laparoscopic cholecystectomy in patients with perioperative heparin bridging for ACT showed that the risk of postoperative bleeding was higher compared with those without ACT. The remaining 14 studies reported no significant differences in the incidence of bleeding complications between the ATT group and the group without ATT. The risk of thromboembolic events (TE) associated with laparoscopic digestive surgery in patients receiving ATT was not significantly higher than those with no ATT or interrupted APT.
Laparoscopic digestive surgery in ATT-burdened patients for prevention of bleeding and TE showed satisfactory results. The risk of hemorrhagic complication during or after these procedures in patients with continued APT or heparin bridging was not significantly higher than in patients with no ATT or interrupted APT.
Core tip: In total, 15 published articles and abstracts concerning laparoscopic digestive surgery and antithrombotic therapy were systematically reviewed. These articles demonstrated that the risk of bleeding and thromboembolic complications during or after these procedures in patients with continued antiplatelets or heparin bridging was not significantly higher than in patients with no antithrombotics or interrupted antiplatelets.
- Citation: Fujikawa T, Ando K. Safety of laparoscopic surgery in digestive diseases with special reference to antithrombotic therapy: A systematic review of the literature. World J Clin Cases 2018; 6(14): 767-775
- URL: https://www.wjgnet.com/2307-8960/full/v6/i14/767.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v6.i14.767
Following cancer, heart disease and cerebrovascular disease are the major causes of death worldwide. With the arrival of an aging society in recent years, the number of patients with heart disease and/or cerebrovascular disease who require non-cardiac surgery is increasing. For the purpose of preventing thromboembolic events (TE), most of them receive antithrombotic therapy (ATT), including antiplatelet therapy (APT) and anticoagulation therapy (ACT). Perioperative management of these patients is challenging for surgeons, and they are often at high risk of bleeding and thromboembolic complications[1-4].
Many digestive operations are currently performed laparoscopically. Several reports have shown advantages of laparoscopic digestive surgery, including early recovery of digestive function, reduction of body wall destruction, reduction of postoperative pain, less postoperative complications, and rapid return to daily life[5-9]. During laparoscopic surgery, minimizing surgical blood loss to maintain a dry operative field is exclusively important. Improvement of several techniques and new surgical devices, such as ultrasonic coagulating shears or saline-linked soft-coagulation system, led us to perform various types of advanced laparoscopic digestive operations including colorectal resection, esophagogastrectomy, and hepato-biliary-pancreas surgery. However, optimal management of patients receiving ATT during laparoscopic digestive surgery is still controversial.
The purpose of the current systematic review study is to elucidate the effect of ATT on bleeding and thromboembolic complications during or after laparoscopic digestive surgery.
Articles written in English and published between 2000 and 2017 were collected from PubMed, Cochrane Database and Google Scholar. We also used PubMed and Google Scholar to search internationally accepted English abstracts. The following key words were used for the search: Clopidogrel, aspirin, antiplatelet, anticoagulant, warfarin, bleeding, hemorrhage, gastrointestinal, gastroenterological, digestive and laparoscopic surgery. Articles or abstracts were included when published in peer reviewed journals or when accepted at internationally renowned medical conferences. Types of eligible studies included randomized clinical trials, prospective or retrospective cohort studies, or case-control studies; guidelines, review articles, or case series/reports were not included.
After removing duplicates, articles were systematically excluded by careful review of each study. The quality of each study was assessed depending on study design, and eligible articles and abstracts were determined. Complete data were extracted from each study, which included study design, year of publication, sample size, type of surgical procedures, type of antithrombotic drugs, and surgical outcome (both bleeding and thromboembolic complications).
Research collection and screening was conducted from January 2018 to February 2018. In all, 13 articles and two abstracts were included[10-24]. Among them, there were no randomized clinical trials or prospective cohort studies, and only retrospective cohort studies or case-control studies were seen. Among 15 studies, nine studies examined only APT use, two studies focused on ACT, and four studies investigated both. Concerning APT, patients who had continued preoperative APT were compared with those who did not receive APT. In patients with continued APT, only single antiplatelet agents, such as aspirin, were usually continued. One study focused on clopidogrel alone, and one study investigated aspirin alone. In studies regarding ACT, only warfarin was used, and most patients received heparin bridging perioperatively.
Only one retrospective cohort study used a large number of cases (over 1000 cases), but various types of laparoscopic surgery (mostly laparoscopic cholecystectomy) were included. This is the largest study to date, examining the effects of APT on outcome of abdominal laparoscopic operations. This study demonstrated that there was no significant difference in postoperative bleeding events between patients who continued APT and other patients.
We classified the type of surgery into two categories based on previous reports[10]: Basic laparoscopic surgery (e.g., cholecystectomy, appendectomy, adhesiolysis, hernia repair) and advanced laparoscopic surgery (e.g., colorectal resection, gastrectomy, liver/pancreas resection). The results of basic surgery and advanced surgery are shown in Tables 1 and 2, respectively. Bleeding events included two categories: intraoperative bleeding complications (IBCs; increased surgical blood loss), and postoperative bleeding complications (PBCs; intraabdominal bleeding, gastroenterology bleeding, or abdominal wall hematoma).
| First author of the reports | Year | Surgery type | Drug use and exposure | Bleeding events | TE, mortality |
| Laparoscopic surgery (overall) | |||||
| Fujikawa[10] | 2013 | Abdominal laparoscopic surgery (cholecystectomy (mostly), appendectomy, surgery for GI malignancy, liver resection, splenectomy etc) | Patients with continued use of ASA (n = 52) | PBC 0% in continued ASA vs 2.5% in discontinuation vs 0.7% in control (P = 0.987) | TE 0% in continued ASA vs 0.6% in discontinued ASA vs 0.2% in control (P = 0.625) |
| Patients with discontinuation of APT (n = 160) | Only one mortality in continued ASA group (1.9%) | ||||
| Patients not on APT (control, n = 863) | |||||
| Laparoscopic cholecystectomy | |||||
| Ercan[11] | 2010 | Laparoscopic cholecystectomy (only elective) | Patients with ACT (w/ bridging, n = 44) | PBC 25% in ACT vs 1.5% in control (P < 0.001) | (not mentioned) |
| Patients without ACT (control, n = 1377) | One mortality due to severe bleeding | ||||
| Ono[12] | 2013 | Laparoscopic cholecystectomy (n = 270) or Laparoscopic colorectal cancer resection (n = 218) | Patients with continued ASA (n = 52) | SBL 27 mL in continued ASA vs 17 mL in control (P = 0.430) | No mortality in both groups |
| Patients without ASA (control, n = 436) | |||||
| Anderson[13] | 2014 | Laparoscopic cholecystectomy (elective and emergency) | Patients with continued clopidogrel (n = 36) | No difference in SBL (49 g vs 47 g, P = 0.85) | No TE in both groups |
| Matched patients without clopidogrel (control, n = 36) | PBC 0% in clopidogrel vs 2.8% in control (P = 0.31) | No mortality in both groups | |||
| Noda[14] | 2014 | Early laparoscopic cholecystectomy for acute cholecystitis | Patients with continued use of ATT (n = 21) | No conversion to open surgery | No mortality in both groups |
| Patients without ATT (n = 162) | No PBC in both groups | ||||
| Joseph[15] | 2015 | Emergency laparoscopic cholecystectomy | Patients with continued use of APT (n = 56), including those with preop Plt transfusion (n = 12) | SBL ≥ 100 mL 14.3% in continued ASA vs 9% in control (P = 0.50) | No difference in the rates of overall postop complications (8.9% vs 7.1%, P = 0.80) |
| Patients without APT (control, n = 56) | No mortality in both groups | ||||
| Fujikawa[16] | 2017 | Emergency cholecystectomy including 106 laparoscopic surgery for acute cholecystitis | Patients with continued use of APT (n = 89) | SBL ≥ 500 mL 12% in continued APT vs 5% in control (P = 0.240) | TE 1.1% in continued APT vs 0% in control (P = 0.37) |
| Patients without APT (control, n = 154) | PBC 7% in multiple APT vs 3% in single APT vs 0.6% in control (P = 0.027) | No mortality in both groups | |||
| Sakamoto[17] | 2017 | Laparoscopic cholecystectomy (only elective operation) | Patients with continued single APT (n = 49) | SBL ≥ 200 mL 4.7% in continued APT vs 4.7% in discontinued APT vs 1.5% in control (P = 0.064) | TE 0% in continued APT vs 0.9% in discontinued APT vs 0.2% in control (P = 0.296) |
| Patients with discontinuation of APT (n = 106) | PBC 0% in continued APT vs 0.9% in discontinued APT vs 0.2% in control (P = 0.022) | No mortality in any group | |||
| Patients not on APT (control, n = 653) | |||||
| Yun[18] | 2017 | Laparoscopic cholecystectomy (elective vs emergency) for acute cholecystitis | Patients with continued use of ATT (almost APT, n = 22) | SBL ≥ 100mL 13.6% in continued ATT vs 22.2% in control (P = 0.613) | One case of TE (2.2%) in control |
| Patients with discontinued ATT (almost APT, control, n = 45) | Mortality 4.6% in continued ATT vs 2.2% in control (P > 0.999) | ||||
| Laparoscopic appendectomy | |||||
| Chechik[19] | 2011 | Appendectomy including laparoscopic appendectomy (n = 78) | Patients with continued APT (n = 39) | No difference in SBL or PBC between the groups | No mortality in both groups |
| Patients without APT (control, n = 140) | |||||
| Pearcy[20] | 2017 | Laparoscopic appendectomy (urgent only) | Patients with continued APT (n = 287) | No difference in SBL (31 g vs 26 g) or blood transfusion rate (1% vs 0%) between the groups | Two cases of TE (MI) in continued APT (0.7%) |
| Matched patients without APT (control, n = 287) | No difference in the rates of mortality (1% vs 0%, P = 0.12) | ||||
| First author of the reports | Year | Surgery type | Drug use and exposure | Bleeding events | TE, mortality |
| Laparoscopic liver resection | |||||
| Fujikawa[24] | 2017 | Laparoscopic liver resection vs open liver resection | Patients with ATT (n = 100) | SBL ≥ 500 mL 23% in those with ATT vs 27% in control (P = 0.468) | TE 1% in ATT vs 1.3% in control (P = 0.310) |
| Patients without ATT (control, n = 158) | PBC 4.6% in those with ATT vs 4.3% in control | Mortality 1% in ATT vs 0% in control (P = 0.350) | |||
| Laparoscopic colorectal cancer resection | |||||
| Ono[12] | 2013 | Laparoscopic colorectal cancer resection (n = 218) or laparoscopic cholecystectomy (n = 270) | Patients with continued ASA (n = 52) | SBL 27 mL in continued ASA vs 17 mL in control (P = 0.430) | No mortality in both groups |
| Patients without ASA (control, n = 436) | |||||
| Shimoike[21] | 2016 | Colorectal cancer surgery including laparoscopic surgery (n = 191) | Patients with APT (n = 148) | PBC 0.7% in those with APT vs 0.9% in control (P = 1.000) | TE 0.7% in APT vs 0% in control (P = 0.301) |
| Patients without APT (control, n = 343) | No mortality in both groups | ||||
| Laparoscopic gastrectomy | |||||
| Takahashi[22] | 2017 | Laparoscopic gastrectomy | Patients with ATT (continued in high risk, n = 12) | No difference in SBL or PBC between the groups | No difference in overall complications between the groups |
| Patients without ATT (n = 34) | No mortality in both groups | ||||
| Gerin[23] | 2015 | Laparoscopic sleeve gastrectomy | Patients with ACT (n = 15) | PBC 6.7% in ACT vs 3.3% in control (P = 0.60) | No mortality in both groups |
| Matched patients without ACT (control, n = 30) | |||||
In basic laparoscopic surgeries, only two types of surgery (cholecystectomy and appendectomy) were included. Laparoscopic cholecystectomy was the most commonly reported overall, and a total of eight studies were included[11-15,17,18,24]. Research on laparoscopic appendectomy included two case-control studies[19,20].
For laparoscopic cholecystectomy, warfarin was described in three studies. With only one study, the risk of PBC in ACT patients was significantly higher than those without ACT[11]. In the remaining two studies, the proportion of IBC or PBC did not increase, even with heparin bridging[14,18]. In terms of APT, seven studies focusing on aspirin and/or thienopyridine were included[12-14,17,18,24,25]. IBC was examined as an outcome in six of them, and PBC was analyzed in four studies. None of the studies demonstrated an increase in IBC or PBC when APT (mostly aspirin monotherapy) was continued preoperatively. In two laparoscopic appendectomy studies[19,20], they were exclusively performed in an emergency setting. Both studies focused on preoperative APT continuation and showed that neither IBC nor PBC increased with continued APT.
These findings suggested that when basic laparoscopic digestive operations were performed, the risk of either IBC or PBC in patients undergoing preoperative continued monotherapy for APT or heparin bridging for ACT was not significantly higher than in those without ATT or interrupted APT.
Concerning advanced laparoscopic surgery, only limited numbers of studies were found in three types of surgery; one study on laparoscopic liver resection[16], two studies on laparoscopic colorectal cancer resection[12,21], and two studies regarding laparoscopic gastrectomy[22,23]. Fujikawa et al[16] conducted a retrospective cohort study using liver resection cases (including laparoscopic and open surgery). The authors found that neither IBC nor PBC increased in the case of laparoscopic liver resection, even with aspirin monotherapy for APT and/or heparin bridging for ACT. In two studies of laparoscopic colorectal cancer resection, the effect of APT on IBC or PBC was assessed, and the authors found that APT continuation did not significantly affect hemorrhagic complications[12,21].
Among two papers regarding laparoscopic gastrectomy, Takahashi et al[22] examined the difference in IBC and PBC between the ATT group and the group without ATT. The ATT group included preoperative APT continuation and heparin substitution for ACT, but there was no significant difference in IBC or PBC between the groups. Finally, Gerin et al[23] examined the difference in PBC during laparoscopic sleeve gastrectomy between the warfarin group and the group without warfarin. PBC occurred in 6.7% of patients who received ACT, whereas 3.3% of patients without ACT experienced PBC (P = 0.60).
Among 15 included studies, the incidence of perioperative TE and the mortality rate was described in eight and 14 studies, respectively. In basic laparoscopic surgeries, the TE rate was 0%-2.2% in the continued APT group and 0%-0.2% in the control group. Six out of eight studies showed no mortality in the entire cohort. In the remaining two studies, there was no difference in mortality between the groups. In advanced laparoscopic surgery, the incidence of TE was identical between the groups, with only one expired case (1% of the ATT group). Overall, the risk of TE associated with laparoscopic digestive surgery for patients receiving ATT was not significantly higher than those without ATT or interrupted APT.
To the best of our knowledge, this is the first systematic review that assesses the effect of ATT on bleeding and thromboembolic complications during and after laparoscopic digestive surgery. The present review summarized results of various types of laparoscopic digestive surgery in patients receiving ATT for the prevention of thromboembolism. The risk of hemorrhagic or thromboembolic complications during or after these procedures in patients with continued APT or heparin bridging was not significantly higher than in patients with no ATT or interrupted APT. There are some promising results for both basic and laparoscopic surgery. However, in terms of advanced laparoscopic surgery, such as colorectal resection or liver resection, there is scarce evidence.
ATT includes two types of medications, classified as antiplatelets and anticoagulants. Antiplatelets decrease platelet aggregation and prevent thrombus formation, and they are generally used for primary and secondary prevention of cardiovascular and cerebrovascular diseases, such as myocardial infarction or cerebral infarction. Antiplatelets include thienopyridine (e.g., clopidogrel, ticlopidine, or prasugrel), type III phosphodiesterase inhibitor (e.g., cilostazol), acetylsalicylic acid (aspirin), and other non-steroidal anti-inflammatory agents[10,26]. On the other hand, anticoagulants interfere with the native clotting cascade and prevent blood clotting, and they are generally used for atrial fibrillation, deep vein thrombosis, cardiac endoprostheses, and acute coronary syndrome. These include vitamin K antagonists (e.g., warfarin), heparin derivatives (e.g., fondaparinux), direct thrombin inhibitors (e.g., dabigatran), and factor Xa inhibitors (e.g., rivaroxaban, apixaban, edoxaban)[26,27]. The two latter types are now increasingly used and are referred to as direct-acting oral anticoagulants (DOACs) or non-vitamin K antagonist oral anticoagulants (NOACs). The types of antithrombotics, specific agents, and duration of action are summarized in Table 3.
| Class of agents | Type | Specific agents | Duration of action |
| Antiplatelets | |||
| Thienopyridines | Clopidogrel (Plavix), Ticlopidine (Panardine), Prasugrel (Effient) | 5-7 d1 | |
| Type III PDE inhibitor | Cilostazol (Pretal) | 2 d | |
| Acetylsalicylic acid | Aspirin | 7-10 d | |
| Other NSAIDs | Ibuprofen (Brufen, Advil), Loxoprofen (Loxonin), Diclofenac (Voltaren), etc | Varies | |
| Anticoagulants | |||
| Vitamin K antagonist | Warfarin (Coumadin) | 5 d | |
| Heparin derivatives | Fondaparinux (Arixtra) | 1.5-2 d | |
| DOACs | |||
| Direct thrombin inhibitor | Dabigatran (Pradaxa) | 1-2 d | |
| Factor Xa inhibitors | Rivaroxaban (Xarelto), Apixaban (Eliquis), Edoxaban (Lixiana) | 1-2 d | |
So far, there has been scarce evidence concerning the definite protocols or guidelines for each specific gastroenterological surgical procedure, including laparoscopic surgery. Thanks to the development of techniques and various energy devices, indication of laparoscopic digestive surgery is now expanded not only to basic procedures but also relatively advanced digestive operations[6,8,9]. During laparoscopic surgery, minimizing surgical blood loss to maintain a dry operative field is required, and thus, this procedure results in less surgical blood loss and a lower incidence of postoperative complications[16]. Although the optimal management of patients receiving ATT during laparoscopic digestive surgery is still controversial, rigorous antithrombotic management, such as continued aspirin monotherapy for APT or heparin bridging for ACT, is considered to be safe and feasible.
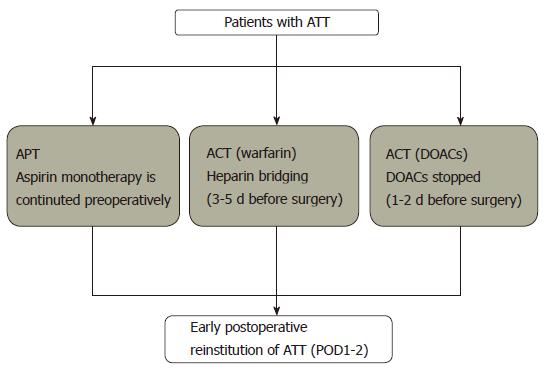
Using several recently updated guidelines concerning antithrombotics as references[26-30], the recommended protocol of perioperative management for patients undergoing ATT in the case of elective open or laparoscopic digestive surgery is shown in Figure 1. The management generally consists of three approaches according to types of ATT; APT, warfarin, and DOACs. In patients with thromboembolic risks, aspirin monotherapy is continued in patients with APT, and warfarin is substituted by heparin bridging 3-5 d before surgery. In the case of DOACs, ATT is stopped 1-2 d before surgery (with some modification needed if decreased renal function exists); if the thromboembolic risk is very high, heparin bridging might be considered. Postoperatively, every antithrombotic agent is reinstituted as soon as possible (POD1-2).
Recent updated guidelines concerning antithrombotic management during non-cardiac surgery[26,27,31-33] showed that the prevention of TE is more important than bleeding complications, as it might cause death or severe sequelae. Concerning implantation of a coronary stent, recent American College of Cardiology/American Heart Association (commonly known as ACC/AHA) and European Society of Cardiology (commonly known as ESC) guideline state that we should continue antiplatelet medications, at least aspirin monotherapy, in the perioperative period for patients with high risk of thromboembolism[30], but most institutions practically choose to discontinue APT in the case of major digestive surgery with bleeding risks. Discontinuing aspirin or clopidogrel may lead to an increased risk of acute myocardial infarction, cerebral infarction, and subsequent death[34,35]. Although some studies, including the POISE-2 study, have reported that a modest increase in bleeding risk was observed in continued APT patients during non-cardiac surgery[36,37], most studies have shown that there was no increase in significant bleeding events[38,39]. Thus, sufficient consideration and emphasis should be placed on the prevention of thromboembolism caused by cessation of antithrombotic drugs, rather than the risk of perioperative bleeding.
Concerning patients with ACT, heparin bridging is a common management for warfarin[40]. Recently, a large-scale randomized controlled trial (BRIDGE study) showed that heparin bridging was not recommended in the case of low bleeding risk surgery due to increased bleeding risks[25]. However, this study included relatively small numbers of major digestive surgery, and it could not conclude that heparin bridging is unnecessary in major general or abdominal surgery. In the current review, only one study concerning warfarin use and laparoscopic cholecystectomy showed an elevated risk of postoperative bleeding when heparin bridging was used[11]. The remaining studies demonstrated the safety of ACT bridging without an increase in severe bleeding complications. Especially in patients with high thromboembolic risks, heparin bridging might be considered to avoid critical thromboembolic complications.
In the present review, there was no report regarding patients who received DOACs during laparoscopic digestive surgery. Currently, DOACs are increasingly prescribed for the purpose of preventing arterial or venous thromboembolism. In large clinical trials, DOACs have been shown to have lower rates of intracranial hemorrhage compared to warfarin[41-44]. Furthermore, in cases of intracranial bleeding, there are reports that hematoma sizes were small in patients receiving DOACs compared to those with warfarin administration[45,46]. This difference is mainly due to the difference in mechanism of action in the blood clotting cascade. A sufficient understanding of these pharmacological characteristics, which is remarkably different from warfarin, is of paramount importance for surgeons. A recently published review and an ongoing prospective study[47,48] suggests safety and feasibility of perioperative management of DOACs during noncardiac surgery, which is rather simple compared with those of warfarin. Still, the detailed assessment of perioperative management protocol, such as the necessity of bridging anticoagulation, has not yet conducted and should be investigated further. In addition, these reports or reviews did not show results according to the procedure types. Safety of every surgical type, including laparoscopic digestive surgery, should be assessed in the future.
Currently, there are only limited numbers of studies concerning the management of ATT-prescribed patients during laparoscopic digestive surgery. As the population ages and the morbidity of cardiovascular disease increases, this patient population is expanded further. Definite protocols or guidelines should be established using reliable studies with good design. In the future, a well-designed prospective randomized study or multicenter cohort study is mandatory to elucidate the safety and feasibility of laparoscopic digestive surgery.
In conclusion, laparoscopic digestive surgery in ATT-burdened patients for the prevention of bleeding and TE showed satisfactory results. The risk of hemorrhagic complication during or after these procedures in patients with continued APT or heparin bridging was not significantly higher than in patients with no ATT or interrupted APT.
Recently, many digestive surgical procedures are being performed laparoscopically. However, the effect of antithrombotic therapy (ATT) on perioperative bleeding complications during laparoscopic surgery is still largely unclear.
The risk of bleeding complications in ATT is related to the perioperative use of antiplatelet therapy (APT) or anticoagulation therapy (ACT). To safely perform laparoscopic digestive surgery in patients with ATT, optimal perioperative management of antithrombotic drugs should be established.
The main objective of the present study is to elucidate the effect of ATT on bleeding and thromboembolic complications during or after laparoscopic digestive surgery.
Published articles or internationally accepted abstracts between 2000 and 2017 were searched, and studies involving laparoscopic digestive surgery and ATT were included after careful review of each study. Data including study design, type of surgical procedures, type of antithrombotic drugs, and surgical outcome were analyzed.
In total, 15 studies were included. Only one study concerning laparoscopic cholecystectomy showed that patients with heparin bridging for ACT had a higher risk of postoperative bleeding. The remaining 14 studies reported continued APT or that heparin bridging for ACT did not affect the incidence of bleeding complication. The risk of thromboembolic events after laparoscopic digestive surgery in patients receiving ATT was not significantly higher than those with no ATT or interrupted APT.
The risk of hemorrhagic complication during or after these procedures in patients with continued APT or heparin bridging was not significantly higher than in patients with no ATT or interrupted APT.
The definite protocol or guidelines should be established using reliable studies with good design. In the future, a well-designed prospective randomized study or multicenter cohort study is mandatory to elucidate the safety and feasibility of laparoscopic digestive surgery.
PRISMA Checklist: The manuscript was prepared and revised according to the PRISMA 2009 Checklist.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Huang LY S- Editor: Dou Y L- Editor: Filipodia E- Editor: Song H
| 1. | Thachil J, Gatt A, Martlew V. Management of surgical patients receiving anticoagulation and antiplatelet agents. Br J Surg. 2008;95:1437-1448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 81] [Cited by in F6Publishing: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Kałuza GL, Joseph J, Lee JR, Raizner ME, Raizner AE. Catastrophic outcomes of noncardiac surgery soon after coronary stenting. J Am Coll Cardiol. 2000;35:1288-1294. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 541] [Cited by in F6Publishing: 561] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 3. | Fujikawa T, Tanaka A, Abe T, Yoshimoto Y, Tada S, Maekawa H. Effect of antiplatelet therapy on patients undergoing gastroenterological surgery: thromboembolic risks versus bleeding risks during its perioperative withdrawal. World J Surg. 2015;39:139-149. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Mita K, Ito H, Murabayashi R, Sueyoshi K, Asakawa H, Nabetani M, Kamasako A, Koizumi K, Hayashi T. Postoperative bleeding complications after gastric cancer surgery in patients receiving anticoagulation and/or antiplatelet agents. Ann Surg Oncol. 2012;19:3745-3752. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Kiviluoto T, Sirén J, Luukkonen P, Kivilaakso E. Randomised trial of laparoscopic versus open cholecystectomy for acute and gangrenous cholecystitis. Lancet. 1998;351:321-325. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 290] [Cited by in F6Publishing: 244] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 6. | Guller U, Jain N, Hervey S. Laparoscopic vs Open Colectomy. Outcomes Comparison Based on Large Nationwide Databases. Arch Surg. 2003;138:1179. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 166] [Cited by in F6Publishing: 164] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 7. | Kapischke M, Caliebe A, Tepel J, Schulz T, Hedderich J. Open versus laparoscopic appendicectomy. Surg Endosc. 2006;20:1060-1068. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Klarenbeek BR, Veenhof AA, de Lange ES, Bemelman WA, Bergamaschi R, Heres P, Lacy AM, van den Broek WT, van der Peet DL, Cuesta MA. The Sigma-trial protocol: a prospective double-blind multi-centre comparison of laparoscopic versus open elective sigmoid resection in patients with symptomatic diverticulitis. BMC Surg. 2007;7:16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009;250:831-841. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 836] [Cited by in F6Publishing: 835] [Article Influence: 55.7] [Reference Citation Analysis (0)] |
| 10. | Fujikawa T, Tanaka A, Abe T, Yoshimoto Y, Tada S, Maekawa H, Shimoike N. Does antiplatelet therapy affect outcomes of patients receiving abdominal laparoscopic surgery? Lessons from more than 1,000 laparoscopic operations in a single tertiary referral hospital. J Am Coll Surg. 2013;217:1044-1053. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 11. | Ercan M, Bostanci EB, Ozer I, Ulas M, Ozogul YB, Teke Z, Akoglu M. Postoperative hemorrhagic complications after elective laparoscopic cholecystectomy in patients receiving long-term anticoagulant therapy. Langenbecks Arch Surg. 2010;395:247-253. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Ono K, Idani H, Hidaka H, Kusudo K, Koyama Y, Taguchi S. Effect of aspirin continuation on blood loss and postoperative morbidity in patients undergoing laparoscopic cholecystectomy or colorectal cancer resection. Surg Laparosc Endosc Percutan Tech. 2013;23:97-100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Anderson K, Jupiter DC, Abernathy SW, Frazee RC. Should clopidogrel be discontinued before laparoscopic cholecystectomy? Am J Surg. 2014;208:926-931; discussion 930-931. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Noda T, Hatano H, Dono K, Shimizu J, Oshima K, Tanida T, Miyake M, Komori T, Kawanishi K, Morita S. Safety of early laparoscopic cholecystectomy for patients with acute cholecystitis undergoing antiplatelet or anticoagulation therapy: a single-institution experience. Hepatogastroenterology. 2014;61:1501-1506. [PubMed] [Cited in This Article: ] |
| 15. | Joseph B, Rawashdeh B, Aziz H, Kulvatunyou N, Pandit V, Jehangir Q, O’Keeffe T, Tang A, Green DJ, Friese RS. An acute care surgery dilemma: emergent laparoscopic cholecystectomy in patients on aspirin therapy. Am J Surg. 2015;209:689-694. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Fujikawa T, Kawamoto H, Kawamura Y, Emoto N, Sakamoto Y, Tanaka A. Impact of laparoscopic liver resection on bleeding complications in patients receiving antithrombotics. World J Gastrointest Endosc. 2017;9:396-404. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Sakamoto Y, Fujikawa T, Kawamoto H, Yoshimoto Y, Tanaka A. The safety and feasibility of elective laparoscopic cholecystectomy in patients with antiplatelet therapy: Lessons from more than 800 cases in a single tertiary referral hospital. In: World Congress of Surgery 2017; International Society of Surgery ISS/SIC, 2017: PE413. [Cited in This Article: ] |
| 18. | Yun JH, Jung HI, Lee HU, Baek MJ, Bae SH. The efficacy of laparoscopic cholecystectomy without discontinuation in patients on antithrombotic therapy. Ann Surg Treat Res. 2017;92:143-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Chechik O, Inbar R, Danino B, Lador R, Greenberg R, Avital S. Anti-platelet therapy: no association with increased blood loss in patients undergoing open or laparoscopic appendectomy. Isr Med Assoc J. 2011;13:342-344. [PubMed] [Cited in This Article: ] |
| 20. | Pearcy C, Almahmoud K, Jackson T, Hartline C, Cahill A, Spence L, Kim D, Olatubosun O, Todd SR, Campion EM. Risky business? Investigating outcomes of patients undergoing urgent laparoscopic appendectomy on antithrombotic therapy. Am J Surg. 2017;214:1012-1015. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Shimoike N, Shimoike N, Fujikawa T, Yoshimoto Y, Tanaka A. Does antiplatelet therapy affect short-term and long-term outcomes of patients undergoing surgery for colorectal cancer? - Surgical radicality versus perioperative antiplatelet-related morbidity risks. J Gastroenterol Hepatol Res. 2016;5:1962-1969. [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Takahashi K, Ito H, Katsube T, Tsuboi A, Hashimoto M, Ota E, Mita K, Asakawa H, Hayashi T, Fujino K. Associations between antithrombotic therapy and the risk of perioperative complications among patients undergoing laparoscopic gastrectomy. Surg Endosc. 2017;31:567-572. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Gerin O, Rebibo L, Dhahri A, Regimbeau JM. The Safety of Laparoscopic Sleeve Gastrectomy in Patients Receiving Chronic Anticoagulation Therapy: A Case-Matched Study. Obes Surg. 2015;25:1686-1692. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 24. | Fujikawa T, Yoshimoto Y, Kawamura Y, Nishimura T, Kawamoto H, Yamamoto T, Emoto N, Sakamoto Y, Tanaka A. Impact of antiplatelet therapy on increased blood loss and bleeding complication in patients undergoing urgent cholecystectomy for acute cholecystitis. In: 12th Biennial E-AHPBA Congress 2017; European-African Hepato Pancreato Biliary Association, 2017: P43.04. [Cited in This Article: ] |
| 25. | Douketis JD, Spyropoulos AC, Kaatz S, Becker RC, Caprini JA, Dunn AS, Garcia DA, Jacobson A, Jaffer AK, Kong DF. Perioperative Bridging Anticoagulation in Patients with Atrial Fibrillation. N Engl J Med. 2015;373:823-833. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 785] [Cited by in F6Publishing: 695] [Article Influence: 77.2] [Reference Citation Analysis (0)] |
| 26. | ASGE Standards of Practice Committee, Acosta RD, Abraham NS, Chandrasekhara V, Chathadi KV, Early DS, Eloubeidi MA, Evans JA, Faulx AL, Fisher DA, Fonkalsrud L, Hwang JH, Khashab MA, Lightdale JR, Muthusamy VR, Pasha SF, Saltzman JR, Shaukat A, Shergill AK, Wang A, Cash BD, DeWitt JM. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016;83:3-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 417] [Cited by in F6Publishing: 388] [Article Influence: 48.5] [Reference Citation Analysis (1)] |
| 27. | Fujimoto K, Fujishiro M, Kato M, Higuchi K, Iwakiri R, Sakamoto C, Uchiyama S, Kashiwagi A, Ogawa H, Murakami K. Guidelines for gastroenterological endoscopy in patients undergoing antithrombotic treatment. Dig Endosc. 2014;26:1-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 262] [Cited by in F6Publishing: 304] [Article Influence: 30.4] [Reference Citation Analysis (0)] |
| 28. | Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, Dunn AS, Kunz R. Perioperative management of antithrombotic therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e326S-e350S. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1138] [Cited by in F6Publishing: 1031] [Article Influence: 85.9] [Reference Citation Analysis (0)] |
| 29. | Korte W, Cattaneo M, Chassot PG, Eichinger S, von Heymann C, Hofmann N, Rickli H, Spannagl M, Ziegler B, Verheugt F. Peri-operative management of antiplatelet therapy in patients with coronary artery disease: joint position paper by members of the working group on Perioperative Haemostasis of the Society on Thrombosis and Haemostasis Research (GTH), the working group on Perioperative Coagulation of the Austrian Society for Anesthesiology, Resuscitation and Intensive Care (ÖGARI) and the Working Group Thrombosis of the European Society for Cardiology (ESC). Thromb Haemost. 2011;105:743-749. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 142] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 30. | Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, Granger CB, Lange RA, Mack MJ, Mauri L. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention, 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery, 2012 ACC/AHA/ACP/AATS/PCNA/SCAI/STS Guideline for the Diagnosis and Management of Patients With Stable Ischemic Heart Disease, 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction, 2014 AHA/ACC Guideline for the Management of Patients With Non-ST-Elevation Acute Coronary Syndromes, and 2014 ACC/AHA Guideline on Perioperative Cardiovascular Evaluation and Management of Patients Undergoing Noncardiac Surgery. Circulation. 2016;134:e123-e155. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 746] [Cited by in F6Publishing: 907] [Article Influence: 113.4] [Reference Citation Analysis (0)] |
| 31. | Kushner FG, Hand M, Smith SC Jr, King SB 3rd, Anderson JL, Antman EM, Bailey SR, Bates ER, Blankenship JC, Casey DE Jr, Green LA, Jacobs AK, Hochman JS, Krumholz HM, Morrison DA, Ornato JP, Pearle DL, Peterson ED, Sloan MA, Whitlow PL, Williams DO; American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2009 focused updates: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction (updating the 2004 guideline and 2007 focused update) and ACC/AHA/SCAI guidelines on percutaneous coronary intervention (updating the 2005 guideline and 2007 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Catheter Cardiovasc Interv. 2009;74:E25-E68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 32. | Polkowski M, Larghi A, Weynand B, Boustière C, Giovannini M, Pujol B, Dumonceau JM; European Society of Gastrointestinal Endoscopy (ESGE). Learning, techniques, and complications of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline. Endoscopy. 2012;44:190-206. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 196] [Cited by in F6Publishing: 206] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 33. | Spyropoulos AC, Douketis JD, Gerotziafas G, Kaatz S, Ortel TL, Schulman S; Subcommittee on Control of Anticoagulation of the SSC of the ISTH. Periprocedural antithrombotic and bridging therapy: recommendations for standardized reporting in patients with arterial indications for chronic oral anticoagulant therapy. J Thromb Haemost. 2012;10:692-694. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 61] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 34. | Ho PM, Peterson ED, Wang L, Magid DJ, Fihn SD, Larsen GC, Jesse RA, Rumsfeld JS. Incidence of death and acute myocardial infarction associated with stopping clopidogrel after acute coronary syndrome. JAMA. 2008;299:532-539. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 276] [Cited by in F6Publishing: 256] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 35. | Ferrari E, Benhamou M, Cerboni P, Marcel B. Coronary syndromes following aspirin withdrawal: a special risk for late stent thrombosis. J Am Coll Cardiol. 2005;45:456-459. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 284] [Cited by in F6Publishing: 234] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 36. | Devereaux PJ, Mrkobrada M, Sessler DI, Leslie K, Alonso-Coello P, Kurz A, Villar JC, Sigamani A, Biccard BM, Meyhoff CS. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014;370:1494-1503. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 586] [Cited by in F6Publishing: 537] [Article Influence: 53.7] [Reference Citation Analysis (0)] |
| 37. | Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet. 2000;355:1295-1302. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 773] [Cited by in F6Publishing: 681] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 38. | Wolf AM, Pucci MJ, Gabale SD, McIntyre CA, Irizarry AM, Kennedy EP, Rosato EL, Lavu H, Winter JM, Yeo CJ. Safety of perioperative aspirin therapy in pancreatic operations. Surgery. 2014;155:39-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 39. | Fang X, Baillargeon JG, Jupiter DC. Continued Antiplatelet Therapy and Risk of Bleeding in Gastrointestinal Procedures: A Systematic Review. J Am Coll Surg. 2016;222:890-905.e11. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 40. | Baron TH, Kamath PS, McBane RD. Management of antithrombotic therapy in patients undergoing invasive procedures. N Engl J Med. 2013;368:2113-2124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 317] [Cited by in F6Publishing: 270] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 41. | Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, Pogue J, Reilly PA, Themeles E, Varrone J. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139-1151. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7917] [Cited by in F6Publishing: 7731] [Article Influence: 515.4] [Reference Citation Analysis (0)] |
| 42. | Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, Breithardt G, Halperin JL, Hankey GJ, Piccini JP. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883-891. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6519] [Cited by in F6Publishing: 6505] [Article Influence: 500.4] [Reference Citation Analysis (2)] |
| 43. | Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, Al-Khalidi HR, Ansell J, Atar D, Avezum A. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981-992. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6075] [Cited by in F6Publishing: 6117] [Article Influence: 470.5] [Reference Citation Analysis (0)] |
| 44. | Giugliano RP, Ruff CT, Braunwald E, Murphy SA, Wiviott SD, Halperin JL, Waldo AL, Ezekowitz MD, Weitz JI, Špinar J. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093-2104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3447] [Cited by in F6Publishing: 3500] [Article Influence: 318.2] [Reference Citation Analysis (0)] |
| 45. | Komori M, Yasaka M, Kokuba K, Matsuoka H, Fujimoto S, Yoshida M, Kameda K, Shono T, Nagata S, Ago T. Intracranial hemorrhage during dabigatran treatment. Circ J. 2014;78:1335-1341. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 46. | Hagii J, Tomita H, Metoki N, Saito S, Shiroto H, Hitomi H, Kamada T, Seino S, Takahashi K, Baba Y. Characteristics of intracerebral hemorrhage during rivaroxaban treatment: comparison with those during warfarin. Stroke. 2014;45:2805-2807. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 104] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 47. | Verma A, Ha ACT, Rutka JT, Verma S. What Surgeons Should Know About Non-Vitamin K Oral Anticoagulants: A Review. JAMA Surg. 2018;153:577-585. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 48. | Douketis JD, Spyropoulos AC, Anderson JM, Arnold DM, Bates SM, Blostein M, Carrier M, Caprini JA, Clark NP, Coppens M. The Perioperative Anticoagulant Use for Surgery Evaluation (PAUSE) Study for Patients on a Direct Oral Anticoagulant Who Need an Elective Surgery or Procedure: Design and Rationale. Thromb Haemost. 2017;117:2415-2424. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |