Published online Oct 16, 2014. doi: 10.12998/wjcc.v2.i10.528
Revised: June 28, 2014
Accepted: July 25, 2014
Published online: October 16, 2014
Primary idiopathic intestinal lymphangiectasia is an unusual disease featured by the presence of dilated lymphatic channels which are located in the mucosa, submucosa or subserosa leading to protein loosing enteropathy.Most often affected were children and generally diagnosed before third year of life but may be rarely seen in adults too. Bilateral pitting oedema of lower limb is the main clinical manifestation mimicking the systemic disease and posing a real diagnostic dilemma to the clinicians to differentiate it from other common systemic diseases like Congestive cardiac failure, Nephrotic Syndrome, Protein Energy Malnutrition, etc. Diagnosis can be made on capsule endoscopy which can localise the lesion but unable to take biopsy samples. Thus, recently double-balloon enteroscopy and biopsy in combination can be used as an effective diagnostic tool to hit the correct diagnosis. Patients respond dramatically to diet constituting low long chain triglycerides and high protein content with supplements of medium chain triglyceride. So early diagnosis is important to prevent untoward complications related to disease or treatment for the sake of accurate pathological diagnosis.
Core tip: Waldmann’s disease is an unusual primary idiopathic intestinal lymphangiectasia, which results in protein loosing enteropathy. Recently, double balloon endoscopy and biopsy in combination is an effective diagnostic tool to hit the correct diagnosis to avoid untoward complications related to disease and treatment due to misdiagnosis. Thus, the clinician should keep in mind this rare condition as a differential diagnosis of oedema.
- Citation: Ingle SB, Hinge (Ingle) CR. Primary intestinal lymphangiectasia: Minireview. World J Clin Cases 2014; 2(10): 528-533
- URL: https://www.wjgnet.com/2307-8960/full/v2/i10/528.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i10.528
Primary Intestinal lymphangiectasia (PIL) was originally described in 1961 by Waldmann et al[1]. It is an unusual cause of protein losing enteropathy either due to congenital malformation or obstruction of lymphatics of intestine[2]. Lymphangectasia is characterised by dilated and proliferating lymphatic channels located in mucosa, submucosa or subserosa leading to protein loosing enteropathy and loss of lymph into gut resulting in to hypoproteinemia, hypogammaglobulinemia, hypoalbuminemia and lymphopenia[3-5]. Peripheral oedema usually symmetrical (lower limb oedema) is the main clinical feature posing a real diagnostic dilemma to the clinicians to differentiate it from other common conditions like congestive cardiac failure, nephrotic syndrome, protein energy malnutrition, etc[3]. Other symptoms are ascites, pleural effusion, weight loss and abdominal pain, diarrhoea with increased faecal loss of protein and fat with increased serum levels of α1-antitrypsin[2,5]. Diagnosis is defined by endoscopic evaluation and confirmed on histopathological evaluation of biopsy of small intestine[1].
Now a day double balloon endoscopy and biopsy is the mainstay to arrive at correct diagnosis.
The worldwide incidence and prevalence of PIL is not known[2,6]. After 1961, as per available literature less than 200 cases were reported[7,8]. Very few familial forms are reported[1,2,9]. There is no specific predilection for sex and race[6]. Most commonly, it has been seen in children and majority of the cases were diagnosed at or before 3 years of age but can be seen in adults also[5,6].
Waldmann’s disease is also called as exudative enteropathy. The pathogenesis is not clear. The proposed hypothetical theories for pathogenesis are.
The basic cause for protein loss in PIL is poorly understood although lymphatic channel malformation/lymphatic hypoplasia leads to obstruction in lymph flow with resultant increase in intraluminal pressure in lymphatic channels[6,10,11]. This, increased intraluminal pressure will cause dilatation of the submucosal,subserosal lymphatic vessels in the intestine finally leading to the rupture of the cystically dilated channels and leading to discharge of the lymph into the bowel lumen[6,12]. Thus, net result is hypoalbuminemia, hypogammaglobinemia and lymphopenia.
Genetic theory: There are mutations in genes that regulate the process of lymphogenesis[5]. Multiple genes, e.g., vascular endothelial growth factor receptor 3, prospero-related homeobox-transcriptional factor, forkhead transcriptional factor and SOX18 play vital role in lymphogenesis[13]. Mutation of the CCBE1 gene has been identified as a cause of intestinal lymphangiectasia in Hennekam syndrome.
Age-PIL is mainly seen in paediatric age group (usually before 3 years of age) and young adults but may be diagnosed in adults too[2,14-16].
Oedema is the main clinical manifestation. The patient may present with ascites, pleural effusion and pericarditis. Other symptoms are lymphedema, abdominal pain, fatigue, moderate diarrhoea, weight loss and deficiency of fat soluble vitamins may also be present.
Oedema is of pitting type and usually symmetrical in distribution involving lower limb. Sometimes severe oedema involving face, scrotum or vagina[5].
Rarely lymphedema have been described which is elicited by “stemmer’s sign” and it is difficult to differentiate from other systemic causes of oedema[2,5]. Sonographic evidence of fetal ascites had also been reported[2,5,17].
Non-specific clinical features such as fatigue, nausea, vomiting, abdominal pain, weight loss, failure to thrive, moderate diarrhoea with faecal loss of fat along with increased faecal loss of protein, leading to rise in alfa-1- antitrypsin levels and there is deficiency of fat soluble vitamins[5,18].
Hypocalcemia-patients can also develop hypocalcemia and tetany due to vitamin D deficiency[2,6,19]. A case of digital clubbing in PIL was reported[20]. Osteomalacia and osteoporosis associated with PIL was reported[21].
Rare Associations-An association of PIL with celiac sprue was described[5,22]. PIL has been reported as a rare cause of lower gastrointestinal bleeding. In addition iron deficiency may occur[5,18]. Recently proved association with angiodysplasia leading to occult blood loss in PIL[5,23,24].
A case of intestinal lymphangiectasia presenting as abdominal mass was reported[2,5,25]. Recurrent haemolytic uraemic syndrome has been described in association with intestinal lymphangiectasia[2,26]. Patients with PIL are prone to develop infections due to lymphopenia and hypogammaglobulinemia[18,27].
Only two cases of disseminated cryptococcal meningitis and osteomyelitis in-patient with lymphangectasia have been reported in the literature so far[28-30]. Recently another case of cryptococcal meningitis as primary manifestation in a patient with intestinal lymphangiectasia has been reported[30]. Lymphoma may complicate the long term outcome of PIL patients[5,31].
PIL may exist as a part of a genetic syndromes, i.e., Noonan, Von Recklinghausen, Hennekam and Yellow nail syndrome[2,5,14]. Finally, an association with autoimmune poly glandular disease type 1 has been described[5,32,33]. Recently a case of intestinal lymphangiectasia in a patient with infantile systemic hyalinosis syndrome has been reported[34].
Now days, diagnosis of Intestinal lymphangiectasia is based on characteristic findings during a double-balloon enteroscopy with further confirmation by histopathological examination of corresponding biopsy specimens[6,35]. To confirm the primary nature of waldmanns disease we must first exclude the secondary causes of intestinal lymphangiectasia[6].
Capsule endoscopy provides complete examination of small bowel mucosa thus can evaluate the extent of lymphangiectasia[36,37]. However, the drawback of capsular endoscopy is the inability to obtain biopsies. So recently double balloon enteroscopy is evolved.
In view of the drawback of capsular endoscopy, its inability to obtain biopsies, double balloon enteroscopy was evolved which allowed obtaining biopsies from lesions detected by capsular endoscopy[35,36].
Endoscopy reveals scattered white spots, which have been described as a characteristic snowflake appearance, (Figure 1) overlying the small intestinal mucosa[4,38].
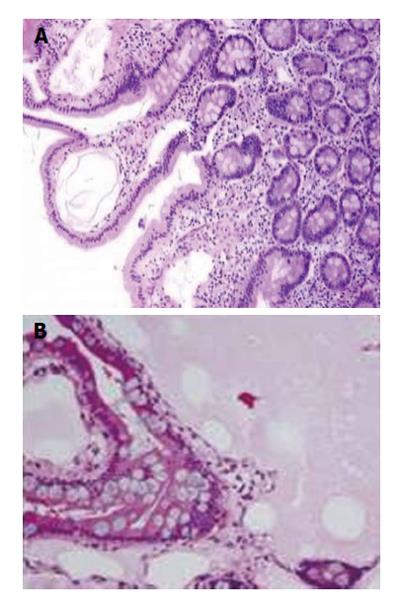
Histopathological examination of biopsies shows dilated lymphatic vessels in mucosa, submucosa and serosa with polyclonal plasma cells confirming the intestinal lymphangiectasia (Figures 2).
Although various methods are available to investigate PIL, careful histopathological examination of biopsies is must to confirm the diagnosis. Various methods to investigate PIL are 99Tc-HSA, 24 h stool alfa-1-antitrypsin clearance, lymphoscintigraphy, ultrasonography (USG), computed tomography (CT) scan, magnetic resonance imaging (MRI).
99Technetium-labelled scintigraphy is useful to arrive at the diagnosis of PIL. Due to high cost and infectious risk, it has replaced with alfa-1-antitrypsin method[2,39].
Lymphoscintigraphy identifies abnormality in lymphatic tree but at present is not a routine method for PIL diagnosis[2,40,41].
On radiographic barium studies, thickened irregular mucosal fold with tiny nodules representing dilated lymphatic suggest the intestinal lymphangiectasia[42].
Imaging with USG/CT scan has shown diffuse thickening of small bowel wall because of engorgement of villi that contain the dilated lymphatic channels[5,43]. CT scan may show “halo sign”. A halo sign that consist of thickened, low-attenuation inner ring representing dilated lymphatics and higher attenuation outer ring, which consist of muscularis propria and serosa[43-45]. Nonenhanced, fluid-sensitive MRI may show bright signal intensity, which corresponds to lymphangiectasia in the mucosa[42,44].
PIL is associated with many laboratory findings which include decreased albumin and total protein levels[2,5,45]. In Addition diminished immunoglobulins IgG, IgA and IgM suggesting B cell depletion and reduced numbers of CD4+ cells as naive CD45RA+ lymphocytes and CD45RO+CD8+T cells reflecting T-cell depletion seen[2,5,46,47].
Finally, a recent report indicates there is failure of compensatory mechanism of production of T lymphocytes by the thymus to overcome the enteric loss of T lymphocytes leading to lymphopenia associated with lymphangiectasia[5,48].
The differential diagnosis of PIL is large and involves many conditions producing protein-losinggastroenteropathy. Much closer differential are those, which involve protein loss associated with impaired intestinal lymphatic drainage. Such conditions include cardiac causes like congestive cardiac failure, constrictive pericarditis and cardiomyopathy[49-52]. Surgical repair of complex congenital heart disease (such as the Fontan procedure for a functional single ventricle), other conditions like lymphenteric fistula[10,53], Whipple’s disease[54], Crohn’s disease[55], sarcoidosis[56], human immunodeficiency virus-related enteropathy[57], intestinal tuberculosis[58], radiation and/or chemotherapy with retroperitoneal fibrosis[59] and portal hypertension or hepatic venous outflow obstruction after liver transplantation and in congenital hepatic fibrosis due to phosphomannose isomerase deficiency[60].
The principal treatment for PIL is diet rich in protein, low in fat with supplementation of medium chain triglyceride. Medium chain triglyceride is directly absorbed in portal venous circulation by passing the intestinal lymphatics, thus provides the energy and lessens lacteal engorgement and lymph loss. A low fat diet reduces lymphatic flow and pressure preventing the lacteal dilation and lymph leakage resulting from their rupture. In some, reversal of clinical and biochemical changes has been seen with this dietary modification. In most patients, dietary treatment is permanently needed. This is found to be more effective in children than adults. In some cases, total parenteral nutrition is needed. Supportive therapy includes albumin infusion and paracentesis.
In patients, not responding to such therapy other options may be used after or in combination with dietary modification. These are octreotide, antiplasmin,tranexemic acid, vitamin D supplementation and surgical resection of segmental or localised intestinal lymphangiectasia[8,11,61].
To conclude PIL is an idiopathic protein loosing enteropathy either due to genetic defect or due to lymphatic obstruction. Careful endoscopic examination and meticulous histopathological evaluation is mandatory to arrive at correct pathological diagnosis to decide the proper treatment plan. One should keep in mind this rare condition as a differential diagnosis of oedema.
P- Reviewer: Kai K, Mubarak M S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
| 1. | Waldmann TA, Steinfeld JL, Dutcher TF, Davidson JD, Gordon RS. The role of the gastrointestinal system in “idiopathic hypoproteinemia”. Gastroenterology. 1961;41:197-207. [PubMed] [Cited in This Article: ] |
| 2. | Vignes S, Bellanger J. Primary intestinal lymphangiectasia (Waldmann’s disease). Orphanet J Rare Dis. 2008;3:5. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 157] [Cited by in F6Publishing: 175] [Article Influence: 10.9] [Reference Citation Analysis (36)] |
| 3. | Katoch P, Bhardwaj S. Lymphangiectasia of small intestine presenting as intussusception. Indian J Pathol Microbiol. 2008;51:411-412. [PubMed] [Cited in This Article: ] |
| 4. | Abramowsky C, Hupertz V, Kilbridge P, Czinn S. Intestinal lymphangiectasia in children: a study of upper gastrointestinal endoscopic biopsies. Pediatr Pathol. 1989;9:289-297. [PubMed] [Cited in This Article: ] |
| 5. | Freeman HJ, Nimmo M. Intestinal lymphangiectasia in adults. World J Gastrointest Oncol. 2011;3:19-23. [PubMed] [Cited in This Article: ] |
| 6. | Lai Y, Yu T, Qiao XY, Zhao LN, Chen QK. Primary intestinal lymphangiectasia diagnosed by double-balloon enteroscopy and treated by medium-chain triglycerides: a case report. J Med Case Rep. 2013;7:19. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Lee J, Kong MS. Primary intestinal lymphangiectasia diagnosed by endoscopy following the intake of a high-fat meal. Eur J Pediatr. 2008;167:237-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Wen J, Tang Q, Wu J, Wang Y, Cai W. Primary intestinal lymphangiectasia: four case reports and a review of the literature. Dig Dis Sci. 2010;55:3466-3472. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 9. | Le Bougeant P, Delbrel X, Grenouillet M, Leou S, Djossou F, Beylot J, Lebras M, Longy-Boursier M. Familial Waldmann’s disease. Ann Med Interne (Paris). 2000;151:511-512. [PubMed] [Cited in This Article: ] |
| 10. | Mistilis SP, Skyring AP, Stephen DD. Intestinal lymphangiectasia mechanism of enteric loss of plasma-protein and fat. Lancet. 1965;1:77-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 80] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Jeffries GH, Chapman A, Sleisenger MH. Low-fat diet in intestinal lymphangiectasia. its effect on albumin metabolism. N Engl J Med. 1964;270:761-766. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 89] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Toskes P. Gastrointestinal diseases: malabsorption. In Cecil Textbook of Medicine. 18th edition. Wyngaarden J, Smith L (eds). Philadelphia: WB Saunders 1988; 732-745. [Cited in This Article: ] |
| 13. | Hokari R, Kitagawa N, Watanabe C, Komoto S, Kurihara C, Okada Y, Kawaguchi A, Nagao S, Hibi T, Miura S. Changes in regulatory molecules forlymphangiogenesis in intestinal lymphangiectasia with enteric protein loss. J Gastroenterol Hepatol. 2008;23:e88-95. [PubMed] [Cited in This Article: ] |
| 14. | Al Sinani S, Rawahi YA, Abdoon H. Octreotide in Hennekam syndrome-associated intestinal lymphangiectasia. World J Gastroenterol. 2012;18:6333-6337. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 20] [Cited by in F6Publishing: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Boursier V, Vignes S. [Limb lymphedema as a first manifestation of primary intestinal lymphangiectasia (Waldmann’s disease)]. J Mal Vasc. 2004;29:103-106. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 16. | Tift WL, Lloyd JK. Intestinal lymphangiectasia. Long-term results with MCT diet. Arch Dis Child. 1975;50:269-276. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 66] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Schmider A, Henrich W, Reles A, Vogel M, Dudenhausen JW. Isolated fetal ascites caused by primary lymphangiectasia: a case report. Am J Obstet Gynecol. 2001;184:227-228. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Xinias I, Mavroudi A, Sapountzi E, Thomaidou A, Fotoulaki M, Kalambakas A, Karypidou E, Kollios K, Pardalos G, Imvrios G. Primary intestinal lymphangiectasia: is it always bad? Two cases with different outcome. Case Rep Gastroenterol. 2013;7:153-163. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Lu YY, Wu JF, Ni YH, Peng SS, Shun CT, Chang MH. Hypocalcemia and tetany caused by vitamin D deficiency in a child with intestinal lymphangiectasia. J Formos Med Assoc. 2009;108:814-818. [PubMed] [Cited in This Article: ] |
| 20. | Wiedermann CJ, Kob M, Benvenuti S, Carella R, Lucchin L, Piazzi L, Chilovi F, Mazzoleni G. Digital clubbing in primary intestinal lymphangiectasia: a case report. Wien Med Wochenschr. 2010;160:431-436. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Li XP, Shen WB, Long MQ, Meng XW, Lian XL, Yu M. Osteomalacia and osteoporosis associated with primary intestinal lymphangiectasis. Chin Med J (Engl). 2012;125:1836-1838. [PubMed] [Cited in This Article: ] |
| 22. | Perisic VN, Kokai G. Coeliac disease and lymphangiectasia. Arch Dis Child. 1992;67:134-136. [PubMed] [Cited in This Article: ] |
| 23. | Maamer AB, Baazaoui J, Zaafouri H, Soualah W, Cherif A. Primary intestinal lymphangiectasia or Waldmann’s disease: a rare cause of lower gastrointestinal bleeding. Arab J Gastroenterol. 2012;13:97-98. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Macdonald J, Porter V, Scott NW, McNamara D. Small bowel lymphangiectasia and angiodysplasia: a positive association; novel clinical marker or shared pathophysiology? J Clin Gastroenterol. 2010;44:610-614. [PubMed] [Cited in This Article: ] |
| 25. | Rao R, Shashidhar H. Intestinal lymphangiectasia presenting as abdominal mass. Gastrointest Endosc. 2007;65:522-523, discussion 523. [PubMed] [Cited in This Article: ] |
| 26. | Kalman S, Bakkaloğlu S, Dalgiç B, Ozkaya O, Söylemezoğlu O, Buyan N. Recurrent hemolytic uremic syndrome associated with intestinal lymphangiectasia. J Nephrol. 2007;20:246-249. [PubMed] [Cited in This Article: ] |
| 27. | Dierselhuis MP, Boelens JJ, Versteegh FG, Weemaes C, Wulffraat NM. Recurrent and opportunistic infections in children with primary intestinal lymphangiectasia. J Pediatr Gastroenterol Nutr. 2007;44:382-385. [PubMed] [Cited in This Article: ] |
| 28. | Cole SL, Ledford DK, Lockey RF, Dass A, Kooper J. Primary gastrointestinal lymphangiectasia presenting as cryptococcal meningitis. Ann Allergy Asthma Immunol. 2007;98:490-492. [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Oehler RL, Maldonado A, Mastorides SM, Reed JL. Cryptococcalosteomyelitis complicating intestinal lymphangiectasia. Infect Dis ClinPract. 2007;15:125-128. [Cited in This Article: ] |
| 30. | Jabeen SA, Murthy A, Kandadai RM, Meena AK, Borgohain R, Uppin MS. Cryptoccocal menigitis as a primary manifestation in a patient with intestinal lymphangictasia. Ann Indian Acad Neurol. 2012;15:218-220. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Bouhnik Y, Etienney I, Nemeth J, Thevenot T, Lavergne-Slove A, Matuchansky C. Very late onset small intestinal B cell lymphoma associated with primary intestinal lymphangiectasia and diffuse cutaneous warts. Gut. 2000;47:296-300. [PubMed] [Cited in This Article: ] |
| 32. | Bereket A, Lowenheim M, Blethen SL, Kane P, Wilson TA. Intestinal lymphangiectasia in a patient with autoimmune polyglandular disease type I and steatorrhea. J Clin Endocrinol Metab. 1995;80:933-935. [PubMed] [Cited in This Article: ] |
| 33. | Makharia GK, Tandon N, Stephen Nde J, Gupta SD, Tandon RK. Primary intestinal lymphangiectasia as a component of autoimmune polyglandular syndrome type I: a report of 2 cases. Indian J Gastroenterol. 2007;26:293-295. [PubMed] [Cited in This Article: ] |
| 34. | Alreheili K, AlMehaidib A, Alsaleem K, Banemi M, Aldekhail W, Al-Mayouf SM. Intestinal lymphangiectasia in a patient with infantile systemic hyalinosis syndrome: a rare cause of protein-losing enteropathy. Ann Saudi Med. 2012;32:206-208. [PubMed] [Cited in This Article: ] |
| 35. | Oh TG, Chung JW, Kim HM, Han SJ, Lee JS, Park JY, Song SY. Primary intestinal lymphangiectasia diagnosed by capsule endoscopy and double balloon enteroscopy. World J Gastrointest Endosc. 2011;3:235-240. [PubMed] [Cited in This Article: ] |
| 36. | Gay G, Delvaux M, Frederic M. Capsule endoscopy in non-steroidal anti-inflammatory drugs-enteropathy and miscellaneous, rare intestinal diseases. World J Gastroenterol. 2008;14:5237-5244. [PubMed] [Cited in This Article: ] |
| 37. | Chamouard P, Nehme-Schuster H, Simler JM, Finck G, Baumann R, Pasquali JL. Videocapsule endoscopy is useful for the diagnosis of intestinal lymphangiectasia. Dig Liver Dis. 2006;38:699-703. [PubMed] [Cited in This Article: ] |
| 38. | Asakura H, Miura S, Morishita T, Aiso S, Tanaka T, Kitahora T, Tsuchiya M, Enomoto Y, Watanabe Y. Endoscopic and histopathological study on primary and secondary intestinal lymphangiectasia. Dig Dis Sci. 1981;26:312-320. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 42] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 39. | Chiu NT, Lee BF, Hwang SJ, Chang JM, Liu GC, Yu HS. Protein-losingenteropathy: diagnosis with 99mTc-labeled humanserum albumin scintigraphy. Radiology. 2001;219:86-90. [Cited in This Article: ] |
| 40. | So Y, Chung JK, Seo JK, Ko JS, Kim JY, Lee DS, Lee MC. Different patterns of lymphoscintigraphic findings in patients with intestinal lymphangiectasia. Nucl Med Commun. 2001;22:1249-1254. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 41. | Burnand KG, McGuinness CL, Lagattolla NR, Browse NL, El-Aradi A, Nunan T. Value of isotope lymphography in the diagnosis of lymphoedema of the leg. Br J Surg. 2002;89:74-78. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 42. | Steines JC, Larson JH, Wilkinson N, Kirby P, Goodheart MJ. Intestinal lymphangiectasia mimicking primary peritoneal carcinoma. Am J Obstet Gynecol. 2010;203:e9-e11. [PubMed] [Cited in This Article: ] |
| 43. | Yang DM, Jung DH. Localized intestinal lymphangiectasia: CT findings. AJR Am J Roentgenol. 2003;180:213-214. [PubMed] [Cited in This Article: ] |
| 44. | Holzknecht N, Helmberger T, Beuers U, Rust C, Wiebecke B, Reiser M. Cross-sectional imaging findings in congenital intestinal lymphangiectasia. J Comput Assist Tomogr. 2002;26:526-528. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 45. | Strober W, Wochner RD, Carbone PP, Waldmann TA. Intestinal lymphangiectasia: a protein-losing enteropathy with hypogammaglobulinemia, lymphocytopenia and impaired homograft rejection. J Clin Invest. 1967;46:1643-1656. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 151] [Cited by in F6Publishing: 158] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 46. | Heresbach D, Raoul JL, Genetet N, Noret P, Siproudhis L, Ramée MP, Bretagne JF, Gosselin M. Immunological study in primary intestinal lymphangiectasia. Digestion. 1994;55:59-64. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 34] [Cited by in F6Publishing: 36] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 47. | Fuss IJ, Strober W, Cuccherini BA, Pearlstein GR, Bossuyt X, Brown M, Fleisher TA, Horgan K. Intestinal lymphangiectasia, a disease characterized by selective loss of naive CD45RA+ lymphocytes into the gastrointestinal tract. Eur J Immunol. 1998;28:4275-4285. [PubMed] [Cited in This Article: ] |
| 48. | Vignes S, Carcelain G. Increased surface receptor Fas (CD95) levels on CD4+ lymphocytes in patients with primary intestinal lymphangiectasia. Scand J Gastroenterol. 2009;44:252-256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 49. | Davidson JD, Waldmann TA, Goodman DS, Gordon RS. Protein-losing gastroenteropathy in congestive heart-failure. Lancet. 1961;1:899-902. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 125] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 50. | Valberg LS, Corbett WE, McCorriston JR, Parker JO. Excessive loss of plasma protein into the gastrointestinal tract associated with primary myocardial disease. Am J Med. 1965;39:668-673. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 22] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 51. | Müller C, Globits S, Glogar D, Klepetko W, Knoflach P. Constrictive pericarditis without typical haemodynamic changes as a cause of oedema formation due to protein-losing enteropathy. Eur Heart J. 1991;12:1140-1143. [PubMed] [Cited in This Article: ] |
| 52. | Wilkinson P, Pinto B, Senior JR. Reversible protein-losing enteropathy with intestinal lymphangiectasia secondary to chronic constrictive pericarditis. N Engl J Med. 1965;273:1178-1181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 78] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 53. | Feldt RH, Driscoll DJ, Offord KP, Cha RH, Perrault J, Schaff HV, Puga FJ, Danielson GK. Protein-losing enteropathy after the Fontan operation. J Thorac Cardiovasc Surg. 1996;112:672-680. [PubMed] [Cited in This Article: ] |
| 54. | Laster L, Waldmann TA, Fenster LF, Singleton JW. Albumin metabolism in patients with Whipple’s disease. J Clin Invest. 1966;45:637-644. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 26] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 55. | Steinfeld JL, Davidson JD, Gordon RS, Greene FE. The mechanism of hypoproteinemia in patients with regional enteritis and ulcerative colitis. Am J Med. 1960;29:405-415. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 111] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 56. | Popović OS, Brkić S, Bojić P, Kenić V, Jojić N, Djurić V, Djordjević N. Sarcoidosis and protein losing enteropathy. Gastroenterology. 1980;78:119-125. [PubMed] [Cited in This Article: ] |
| 57. | Stockmann M, Fromm M, Schmitz H, Schmidt W, Riecken EO, Schulzke JD. Duodenal biopsies of HIV-infected patients with diarrhoea exhibit epithelial barrier defects but no active secretion. AIDS. 1998;12:43-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 64] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 58. | Ploddi A, Atisook K, Hargrove NS. Intestinal lymphangiectasia in intraabdominal tuberculosis. J Med Assoc Thai. 1988;71:518-523. [PubMed] [Cited in This Article: ] |
| 59. | Rao SS, Dundas S, Holdsworth CD. Intestinal lymphangiectasia secondary to radiotherapy and chemotherapy. Dig Dis Sci. 1987;32:939-942. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 29] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 60. | de Koning TJ, Dorland L, van Berge Henegouwen GP. Phosphomannoseisomerase deficiency as a cause of congenital hepatic fibrosis and protein-losing enteropathy. J Hepatol. 1999;31:557. [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 61. | Aoyagi K, Iida M, Matsumoto T, Sakisaka S. Enteral nutrition as a primary therapy for intestinal lymphangiectasia: value of elemental diet and polymeric diet compared with total parenteral nutrition. Dig Dis Sci. 2005;50:1467-1470. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |