-
PDF
- Split View
-
Views
-
Cite
Cite
Shunsuke Yamada, Atsushi Suga, Yoshimasa Inoue, Masayuki Iwazaki, Importance of preoperative assessment of pulmonary venous anomaly for safe video-assisted lobectomy, Interactive CardioVascular and Thoracic Surgery, Volume 10, Issue 6, June 2010, Pages 851–854, https://doi.org/10.1510/icvts.2009.221804
Close - Share Icon Share
Abstract
During the treatment of 86 patients with video-assisted thoracoscopic surgery (VATS) anatomical resection (include segmentectomy) within the last two years, we have encountered five patients (5.8%) with anomalous venous returns. Anomalous returns included: 1) common trunk of the left pulmonary vein; 2) right middle pulmonary vein (V4) draining into the inferior pulmonary vein (IPV); 3) left lingular vein (V4+5) draining into the IPV; 4) right posterior pulmonary vein (V2) draining directly into the left atrium; and 5) left upper lobe vein draining into the left innominate vein. If a surgeon were to perform VATS lobectomy without paying attention to these anomalies according to the affected lobe, serious surgical complications might result. Multi-detector row angiography is useful for recognizing such anomalies before surgery and allow safe VATS lobectomy.
1. Introduction
Video-assisted thoracoscopic surgery (VATS) lobectomy is becoming more common, since early-stage lung cancer is indicated for this procedure in many institutions [1]. For successful completion of VATS lobectomy, accurate knowledge of the anatomy of the segmental branches of pulmonary arteries in the individual patient before surgery is important [2]. The pulmonary veins (PVs) display many variant anatomies. However, surgeons typically expect a venous drainage system with two upper and lower lobe veins, with the middle lobe vein joining the upper lobe vein. Attention thus may not be paid to venous anomalies before VATS lobectomy. However, some anomalies are associated with serious surgical morbidity for patients with lobectomy, if the surgeon does not take care with these anomalies during surgery. We encountered five cases with anomalous venous return during VATS anatomical resection (lobectomy or segmentectomy), representing a surgical risk for the development of serious complication. Multidetector-row computed tomography (MD-CT) angiography is able to correctly depict these anomalies and allows safe performance of VATS procedures.
2. Patients and methods
2.1. Cases
Between May 2007 and July 2009, sagittal and coronal two-dimensional maximum intensity projections (MIPs) generated from enhanced MDCT (64-detector row CT) volumetric data were used to assess pulmonary vessels for 86 patients with VATS anatomical resection (segmentectomy or lobectomy), to allow safe VATS procedures. Our study protocol was as follows. First, 700 mg/kg of contrast medium (300 mg/ml) was injected at 3.5 ml/s. Second, 30 ml of saline was injected at 3 ml/s over 10 s, and scanning was initiated. Five patients (5.8%) showed individual anomalous venous return with a potential for surgical complications, if the surgeons did not take care with these anomalies during planned VATS procedures. Patient characteristics, planned operative procedure and type of venous anomaly are listed in Table 1 .
Patient characteristics of anomalus venous drainage
| Patient | Sex | Age, years | Diagnosis | VATS surgery | Anomalus pulmonary venous drainage |
| 1 | M | 74 | MT | LLL | Common trunk drain into LA |
| 2 | M | 36 | Sarcoid | RLL | V4 drain into IPV |
| 3 | M | 72 | LCa | LLL | V4+5 drain into IPV |
| 4 | M | 62 | TB | Rt S6seg | V2 drain into LA |
| 5 | F | 72 | MT | Lt S6 extended seg | Left upper lobe vein drains into left innominate vein |
| Patient | Sex | Age, years | Diagnosis | VATS surgery | Anomalus pulmonary venous drainage |
| 1 | M | 74 | MT | LLL | Common trunk drain into LA |
| 2 | M | 36 | Sarcoid | RLL | V4 drain into IPV |
| 3 | M | 72 | LCa | LLL | V4+5 drain into IPV |
| 4 | M | 62 | TB | Rt S6seg | V2 drain into LA |
| 5 | F | 72 | MT | Lt S6 extended seg | Left upper lobe vein drains into left innominate vein |
VATS, video-assisted thoracoscopic surgery; MT, metastatic tumor; LLL, left lower lobectomy; LA, left atrium; Sarcoid, sarcoidosis; RLL, right lower lobectomy; IPV, inferior pulmonary vein; LCa, lung carcimona; TB, tuberculoma; Rt S6seg, right superior segmentectomy; Lt S6 extended seg, left extended superior segmentectomy.
Patient characteristics of anomalus venous drainage
| Patient | Sex | Age, years | Diagnosis | VATS surgery | Anomalus pulmonary venous drainage |
| 1 | M | 74 | MT | LLL | Common trunk drain into LA |
| 2 | M | 36 | Sarcoid | RLL | V4 drain into IPV |
| 3 | M | 72 | LCa | LLL | V4+5 drain into IPV |
| 4 | M | 62 | TB | Rt S6seg | V2 drain into LA |
| 5 | F | 72 | MT | Lt S6 extended seg | Left upper lobe vein drains into left innominate vein |
| Patient | Sex | Age, years | Diagnosis | VATS surgery | Anomalus pulmonary venous drainage |
| 1 | M | 74 | MT | LLL | Common trunk drain into LA |
| 2 | M | 36 | Sarcoid | RLL | V4 drain into IPV |
| 3 | M | 72 | LCa | LLL | V4+5 drain into IPV |
| 4 | M | 62 | TB | Rt S6seg | V2 drain into LA |
| 5 | F | 72 | MT | Lt S6 extended seg | Left upper lobe vein drains into left innominate vein |
VATS, video-assisted thoracoscopic surgery; MT, metastatic tumor; LLL, left lower lobectomy; LA, left atrium; Sarcoid, sarcoidosis; RLL, right lower lobectomy; IPV, inferior pulmonary vein; LCa, lung carcimona; TB, tuberculoma; Rt S6seg, right superior segmentectomy; Lt S6 extended seg, left extended superior segmentectomy.
2.1.1. Patient 1
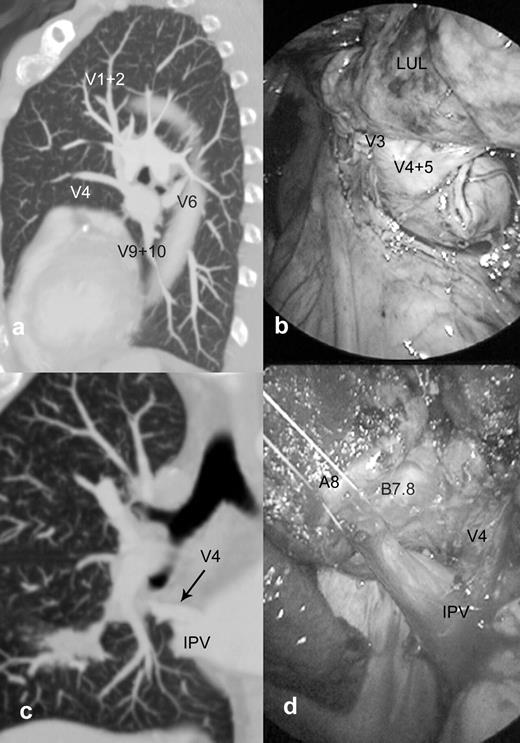
A 74-year-old man with a history of colon cancer demonstrated a well-circumscribed pulmonary nodule (14 mm) in the left lower lobe on chest CT. Since the tumor was located in the lung hilum, VATS left lower lobectomy (LLL) was planned instead of a wedge resection. MDCT MIP showed that the draining veins from the left upper and lower lobes contributed to a common venous trunk draining to the left atrium (LA) on the left side (Fig. 1a ). Care was required in preserving draining lobe veins from the left upper lobe. In surgical findings, PV in the posterior lung hilum was somewhat broad, but seemed anatomically normal for the inferior pulmonary vein (IPV). We exposed this vein adequately, and the dissected peripherally. The venous trunk was short, and showed both draining branches from the upper and lower lobes. After the major fissure between upper and lower lobe was stapled, the two branches (V6 and V8+V9–10) from the lower lobe were identified, then divided simultaneously under the lower bronchus using an end-stapler (Fig. 1b).
Patient 1: common venous trunk on the left side for a patient with planned VATS left lower lobectomy. Sagittal maximum intensity projections (MIP) clearly show the venous trunk continuing from the upper and lower lobe veins (a). Two branches (V6 and V8+V9–10) of drainage veins from the lower lobe are stapled together, with preservation of the venous braches of the left upper lobe (b). Patient 2: right V4 anomalous venous drainage for a patient with planned VATS right lower lobectomy. Coronal MIP shows V4 draining into the cephalic side of the inferior pulmonary vein (IPV) (c). In surgery, the right middle lobe vein was confirmed to drain into the inferior pulmonary vein, after dividing the anterior portion of the major fissure and taping the lower lobe vein (d).
2.1.2. Patient 2
A 36-year-old man demonstrated an ill-defied pulmonary lesion (35 mm) in the right lower lobectomy (RLL) on chest CT. In this case, transbronchial lung biopsy (TBLB) did not allow pathological diagnosis. However, the lesion showed accumulation of 18-fluorodeoxy glucose on positron emission tomography, so lung carcinoma (C-T2NoMo) was strongly suspected. Since the tumor was located in the lung hilum, VATS RLL was planned, and additional lymph node dissection was planned if the lesion was confirmed as lung cancer during surgery. On preoperative examinations, MDCT MIP showed the right V4 draining into the cephalic side of the IPV (Fig. 1c). Care was required to preserve V4 during the process of dividing the IPV in VATS procedures. In terms of surgical findings, an aberrant PV, differing from the lower lobe veins, drained into the IPV from the cephalic side. After anterior portion of the major fissure was stapled, and this anomalous vein was confirmed to be the middle lobe vein (V4). The lower lobe vein was carefully divided using an end-stapler (Fig. 1d).
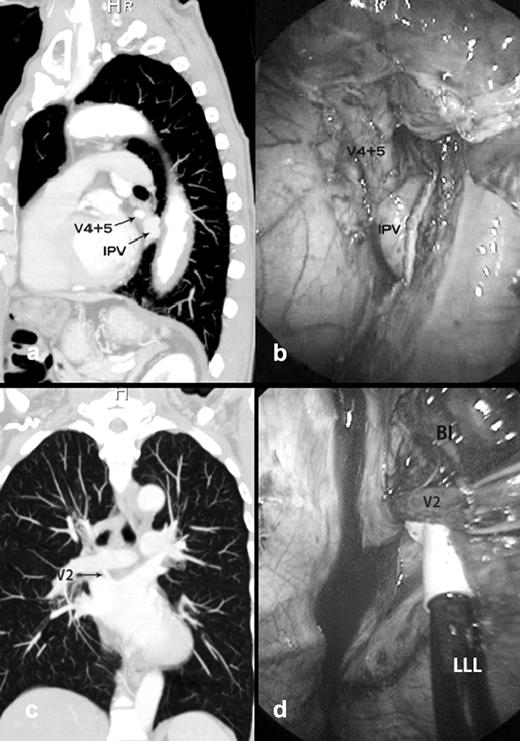
2.1.3. Patient 3
A 72-year-old man with lung cancer (C-T2N0M0) demonstrated a pulmonary nodule (diameter, 40 mm) on the left lower lobe. VATS LLL and lymph node dissection were planned. MDCT angiography showed that the left lingual vein (V4+5) drained into the proximal and ventral trunks of the IPV (Fig. 2a ). The IPV was dissected circumferentially, and V4+5 was confirmed. The PV branch of the lower lobe was divided using an end-stapler just below the insertion of the IPV (Fig. 2b). In this case, the major fissure was inadequate. Therefore, after the lower lobe arteries and bronchus were stapled individually, the lower portion of the major fissure (S4+5 between S8) was stapled, taking care not to injure V4+5 in the video view.
Patient 3: left V4+5 anomalous venous drainage for a patient with planned VATS left lower lobectomy (LLL). Sagittal MIP shows the left inguinal vein (V4+5) draining into the ventral side of the inferior pulmonary vein (IPV) (a). In surgery, the pulmonary venous branch of the left lower lobe was stapled (b). Patient 4: right V2 anomalous venous drainage for a patient with planned VATS S6 segmentectomy. Coronal MIP shows V2a in the right upper lobe descending crossing behind the bronchus intermedius (BI), and draining directly into the left atrium (c). In surgery, the aberrant V2 was dissected from the membranes of the BI on the posterior aspect of lung hilum (d).
2.1.4. Patient 4
A 62-year-old man demonstrated a pulmonary nodule (10 mm) in the right superior segment (S6). Bronchoscopic examination did not allow pathological diagnosis, but this nodule showed accumulation of 18-fluorodeoxy glucose on positron emission tomography. For diagnostic and therapeutic purposes, VATS S6 segmentectomy on the right side was planned. MDCT angiography showed that V2 crossed the posterior of the bronchus intermedius (BI) and drained into the LA (Fig. 2c). As the major fissure was obscured and incomplete, we had concerns were held regarding the risk of V2 injury during the surgical procedure. During inter-lobar plasty (between S6 and S1+2) using an end-stapler and separation of lung parenchyma from the BI, we carefully dissected the lung parenchyma on the posterior aspect of the lung hilum, and identified the anomalous vessel on the membrane portion of the BI (Fig. 2d). This vessel was ligated and cut before dividing the major fissure.
2.1.5. Patient 5
A 72-year-old woman with pulmonary metastasis as a result of colon cancer was admitted to our hospital. She appeared healthy and asymptomatic. Axial CT showed the tumor (diameter, 19 mm) located at S6 near S10 segments of the left lower lobe. MDCT MIP showed an left upper lobe vein draining into the left brachiocephalic vein. Echocardiographs showed mild enlargement of the right ventricle (RV) without tricuspid regurgitation. Electrocardiography showed no abnormalities. Since this patient only showed evidence of a mild increase in RV volume, VATS left S6 extended segmentectomy was planned.
3. Results
Surgical findings of pulmonary venous anomaly corresponded with those from MDCT angiography in the first four cases (Patients 1–4). In Patient 5, the anomalous PV was not examined during VATS procedures. All procedures were able to be performed on schedule, under videoscopic guidance (5 mm, 30° rigid thoracoscope) with 3–4 ports (5 or 10 mm), without need for mini-thoracotomy. After wrapping in a surgical bag, the specimen was extracted by enlarging the port wound. In all cases, intraoperative pathological examinations for surgical specimens were performed. Pathological diagnoses of specimens were listed in Table 1. In three cases with malignant tumors (Patients 1, 3 and 5), the operations proved curative. No intraoperative complications were encountered in any procedures. All patients displayed an uneventful postoperative course. Follow-up at six months showed that Patient 5 was asymptomatic, and echo- and electrocardiography revealed no evidence of increased shunt volume compared with previous imaging findings.
4. Discussion
Clinically, some variant anatomies of the PV pose a potential surgical risk for patients undergoing lobectomy, if the surgeon happens to overlook the anomalies. We identified a common trunk draining from the upper, middle and lower lobes [3], the middle lobe vein draining directly into the IPV [4, 5], the lingual segmental vein (V4+5) draining into the left IPV [4], and the right upper lobe vein, which crosses behind the BI, draining into the LA [6, 7]. When a lobectomy is performed for patients with these anomalous veins, unexpected vessel injury or incorrect ligation of drainage veins might result if the surgeon overlooks the anomalies, potentially leading to uncontrolled bleeding or severe lung edema that could become life-threatening [8, 9]. Compared with thoracotomy, VATS lobectomy under video-view limits inspection of the surgical field. We cannot expose the hilar structure sufficiently to identify the whole anatomy under the same view. Surgical procedures through thoracoports make homeostasis following vessel injury more complicated. As a result, surgical morbidity might be increased. Partial anomalous pulmonary venous connection (PAPVC) (Patient 5) is a relatively uncommon congenital anomaly. Most patients are associated with other heart defects, and are symptomatic because of right ventricular volume overload due to left-to-right shunting [10, 11]. Conversely, we must be careful of patients with asymptomatic PAPVC as in Patient 5, who show mild left-to-right shunting and might only be discovered incidentally during evaluation for other medical conditions in late adulthood. Asymptomatic PAPVC, which is located in a different lobe, may be problematic after major lung resection because of right ventricular volume overload caused by the increase in left-to-right shunting. In Patient 5, the deeply located lesion was strongly suspected to represent a metastatic tumor (MT), and we then selected S6 extended segmentectomy knowing the curability of malignant tumor and the preservation of the draining veins from basal segments. If asymptomatic PAPVC is located in an affected lobe, care must be taken to prevent injury of the unanticipated anomalous PV in the lung hilum. In this study, we developed venous anomalous drainage in five of the 86 patients (5.8%). These results show that the variant anatomy of the PV is not as rare as was previously believed. For successful completion of VATS lobectomy, careful preoperative assessment of the venous return is crucial. Conventional enhanced CT might identify these anomalies, if the surgeon is well-versed in recognizing such anomalies [5]. However, finding these anomalies is difficult anatomically, as the anatomy of the pulmonary hilum is complex and variations of venous anomalies are numerous. Development of the MDCT scanner has allowed contiguous thin-section CT to be performed throughout the entire lung facilitating the generation of MDCT-MIP images from volumetric data within a few minutes [12]. Contrast-enhanced MDCT-MIP (sagittal and coronal imaging) shows two-dimensional findings of the anatomy of the pulmonary vessels, particularly the smaller and more peripheral the course, in greater detail [13]. The ability to trace proximal and distal portions allows identification of whether the vessel represents a PA or PV. However, when PA and PV show nearly equivalent attenuation, PV anatomy is sometimes difficult to evaluate. Following injection of contrast medium, injection of 30 ml of saline (over 10 s) before exposure was useful to efficiently reveal image interpretations of PA and PV images. In four of the present cases (Patients 1–4), surgical findings of anomalous pulmonary draining veins in the lung hilum corresponded with those shown on MIP images. This study confirmed the following two points on MDCT angiography for preoperative assessment of venous drainage, especially for patients with VATS lobectomy. First, we confirmed the existence of four lobe veins (SPV and IPV) draining into the LA on both sides. Second, we looked for any aberrant vessel draining to the affected lung hilum from the adjacent lobe. When VATS lobectomy is planned, careful preoperative assessment of venous return is essential. MDCT angiography can provide detailed information for the PV, and is considered a useful examination for assessing abnormalities of venous return.