-
PDF
- Split View
-
Views
-
Cite
Cite
Naoko Nagano, Taira Yamamoto, Atsushi Amano, Ken Kikuchi, Infected aneurysm of the aortic arch with purulent pericarditis caused by Streptococcus pneumoniae, Interactive CardioVascular and Thoracic Surgery, Volume 10, Issue 3, March 2010, Pages 459–461, https://doi.org/10.1510/icvts.2009.224980
Close - Share Icon Share
Abstract
A 76-year-old woman had a chest pain and high fever, and was admitted to the intensive care unit diagnosed as acute pericarditis. Enhanced CT-scan showed a 47-mm aneurysm in the aortic arch which seemed to be impending rupture and the part of the aorta looked like a pseudoaneurysm. Emergent total aortic arch replacement with a rifampicin-bonded Dacron graft was performed. Pericardial effusion was purulent and the aorta was infected with pus discharge in the aortic wall. There were some ulcerations on the surface of the luminal wall of the aorta. One of them was penetrating into the pericardial space causing a pseudoaneurysm. Both pericardial effusion and excised aortic wall were sent to culture study and resulted in positive for Streptococcus pneumoniae. The infection of the aorta, with erosion into the pericardial space, seemed to be the cause of purulent pericarditis. Antibiotic therapy was commenced immediately after surgery and continued for four weeks. Though she had neurological deficit after surgery, her infection was well controlled and there was no recurrence of infection 11 months after surgery.
1. Introduction
Infected aortic aneurysm is rare but life-threatening disease. Its aggressive presentation and difficulty of treatment have been reported.
2. Case report
A 76-year-old woman had a chest pain and high fever. A chest X-ray was checked but there was no enlargement of mediasternal shadow. Three months later, her chest pain became worse and echocardiography was performed. There was no abnormality with her heart including surrounding tissue. Two weeks later, she was almost bedridden at home due to general fatigue and chest pain. She was noticed to have friction rub on auscultation of her heart. Echocardiography was performed again, which showed pericardial effusion and thickened pericardium. Following CT-scan showed an aortic aneurysm with the diameter of 47 mm in the aortic arch.
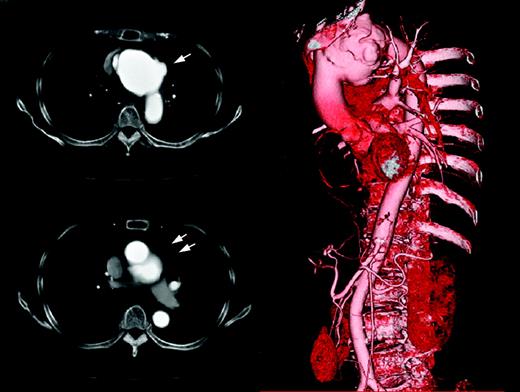
She was admitted to the intensive care unit due to acute pericarditis. The enhanced CT-scan was taken, which showed the aortic aneurysm in the aortic arch and the shape of the aneurysm was irregular with some ulcerations. The part of the aorta seemed to be a pseudoaneurysm (Fig. 1 ). She developed cardiac tamponade and impending rupture of the aneurysm. Her white blood cell (WBC) count was 30.5×103/μl and C-reactive protein was 28.97 mg/dl suggesting existence of aggressive infection. Her past medical history was remarkable for ulcerative colitis for which she underwent total colectomy and colostomy 27 years previous. After this surgery she had been doing well without any special medication.
Enhanced CT-scan taken on admission. The infected aortic aneurysm was seen in the aortic arch with pseudoaneurysm (arrows).
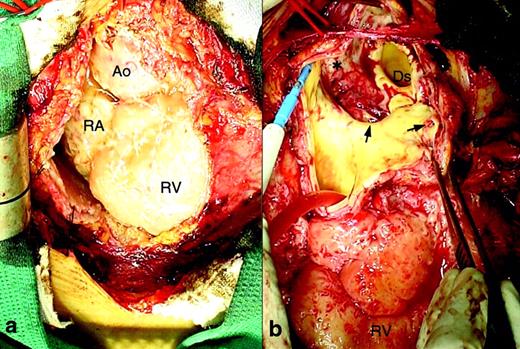
Though her general condition was extremely poor, there was no choice except for proceeding to emergent surgery to prevent rupture of the aneurysm. Median sternotomy was made and femoro-femoral bypass was initiated. When the pericardium was opened, massive cloudy yellowish pericardial effusion gushed out from the pericardial space. The pericardium was heavily thickened and epicardium showed severe acute infection (Fig. 2a ). After deep hypothermic circulatory arrest was instituted, the aorta was opened at the aortic arch. The aortic wall was thickened and there was purulent discharge from the aortic wall. There were some ulcerations on the surface of the luminal wall of the aorta (Fig. 2b). One of them was penetrating to the outside of the aortic wall into the pericardial space causing pseudoaneurysm. Atherosclerotic change of the aortic wall was also obvious. The infected aortic wall was excised as much as we could and total aortic arch replacement with a rifanpicin-bonded Dacron graft was performed. Omental flap coverage of the Dacron graft was considered but it was abandoned because there was no available omentum for the chest due to her previous colectomy. The chest was closed after massive irrigation.
Intraoperative photographs. (a) Pericardium was heavily thickened and epicardium showed active infection with white fibrin-like deposition. (b) The aorta was opened at the aortic arch. The aortic wall was thickened and there was purulent discharge from the aortic wall. There were dirty mucus (*) and ulcerations (arrows) on the surface of the luminal wall of the aorta. Ao, ascending aorta; RA, right atrium; RV, right ventricle; Ds, distal arch.
According to the result of gram-stain, intravenous benzylpenicillin was commenced immediately and continued for four weeks following oral antibiotics. Pericardial effusion and excised aortic wall were sent to culture and both of them were positive for Streptococcus pneumoniae. The patient recovered with some neurological deficit including verbal difficulty and right-sided weakness. Postoperative reconstructed 3D CT-scan showed successful repair of the aortic arch. Her C-reactive protein was persistently down after surgery and by the time she left our hospital it was 0.41 mg/dl. She was transferred to a rehabilitation hospital on postoperative day 48 and she remained well without any recurrence of infection 11 months after surgery. The mechanism of her infection remained unknown.
3. Discussion
Infected aortic aneurysms are rare, which comprise only 0.7∼1.3% [1, 2] of all aortic aneurysms. Its aggressive presentation and difficulty of treatment have been reported previously [2]. Reportedly, operative mortality was 10∼36% [2–5] and morbidity was 60–70% [2, 5]. Early diagnosis, timely surgical intervention and intensive antibiotic therapy are essential for the treatment of infected aortic aneurysms [3–5].
In our case, despite the aggressive infection we performed in situ graft replacement because the aneurysm was located in the aortic arch. Cryopreserved homografts, refanpicin-bonded grafts and silver coated grafts are favorable choices under such circumstances as they are infection resistant [6–8]. Unfortunately, availability of cryopreserved homografts in Japan is very limited. Silver coated grafts are not commercially available in Japan at the moment. Because of these reasons, a rifampicin-bonded graft was chosen for the patient. Endovascular treatment could be a choice of treatments for the aneurysm if it is located in the descending or infrarenal abdominal aorta [9], but not for the aneurysm in the aortic arch. Conservative treatment was once considered, but her increasing chest pain seemed to be a symptom of impending rupture. As mortality is highly associated with rupture [4], surgical intervention needs to be performed before rupture.
Infected aneurysm with purulent pericarditis is an extremely rare presentation. Shroyer et al. [10] reported postmortem examinations of a similar case as, ‘… the aortic pseudoaneurysm originated at the site of an ulcerated atherosclerotic plaque. … infection of the aortic lesion, with erosion into the pericardial space, was the apparent cause of purulent pericarditis’. Our operative findings were exactly compatible with their examinations and positive culture results of Streptococcus pneumoniae from both pericardial effusion and excided aortic wall support this theory.
In summary, we had a case of infected aortic aneurysm with purulent pericarditis. Emergent operation was successfully performed and postoperative antibiotic therapy was effective. Although she remained well 11 months after surgery, long-term follow-up is mandatory.