ABSTRACT
Objective:
To identify the incidence, risk factors for delirium, and its association with death in the elderly hospitalized with fractures.
Method:
Prospective cohort, with a one-year follow-up of elderly people with clinical or radiological diagnosis of fracture, from an emergency and trauma hospital in the state of Goiás. The outcome delirium was defined by the medical description in the medical record. The predictor variables were demographic, health conditions, and hospitalization complications. A hierarchical multiple analysis was performed using robust Poisson regression, with Relative Risk as a measure of effect.
Results:
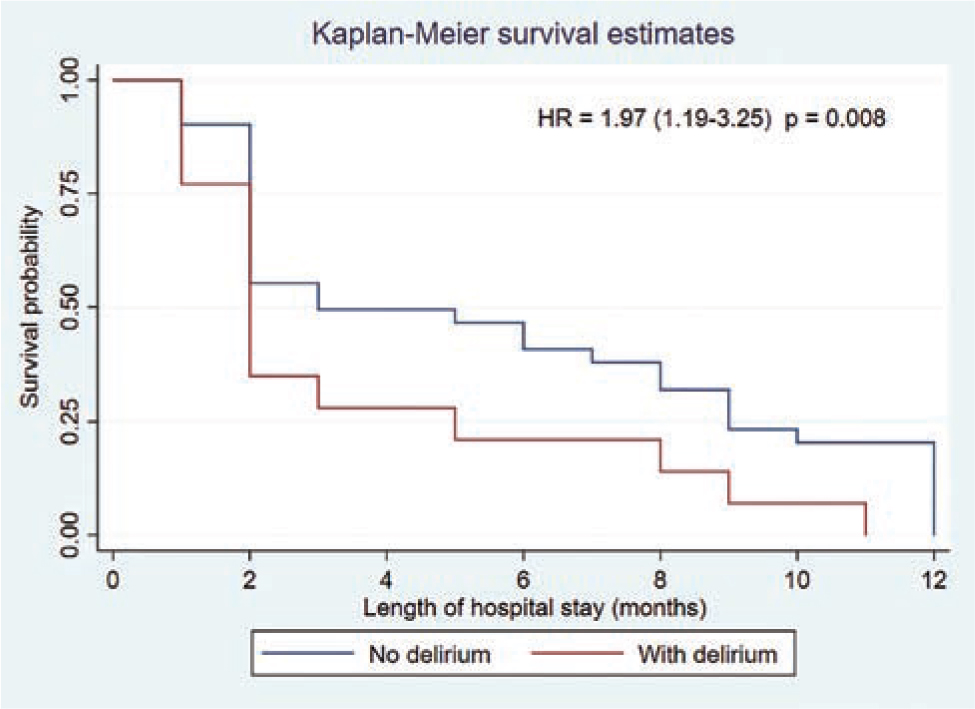
A total of 376 elderly patients were included. The incidence of delirium was 12.8% (n = 48). Risk factors were male gender, age ≥80 years, dementia, heart disease, osteoporosis, chronic obstructive pulmonary disease, high-energy traumas, pneumonia, urinary tract infection, and surgery. The risk of death in the sample was 1.97 times higher (HR: 1.97 95% CI 1.19–3.25) in elderly people with delirium.
Conclusion:
Delirium had an intermediate incidence (12.8%); the risk of death in this group was about 2 times higher in one year after hospital admission. Demographic factors, past history of diseases, surgery, and complications have increased the risk and require monitoring during hospitalization of elderly people with fractures.
DESCRIPTORS
Aged; Fractures, Bone; Hospitalization; Delirium; Mortality; Geriatric Nursing
RESUMEN
Objetivo:
Identificar la incidencia, los factores de riesgo para el delirium y su asociación con el óbito en ancianos hospitalizados con fracturas.
Método:
Cohorte prospectiva, con acompañamiento de un año con ancianos con diagnóstico clínico o radiológico de fractura, de un hospital de urgencias y trauma en Goiás, Brasil. El resultado delirium fue definido por la descripción médica en el registro médico. Las variables predictoras fueron demográficas, condiciones de salud y complicaciones de la hospitalización. Se realizó el análisis de regresión múltiple jerárquica utilizando la regresión de Poisson con varianza robusta, con Riesgo Relativo como medida de efecto.
Resultados:
Fueron incluidos 376 ancianos. La incidencia de delirium fue 12,8% (n = 48). Los factores de riesgo fueron: sexo masculino, edad ≥ 80 años, demencia, cardiopatía, osteoporosis, EPOC, traumas de alta energía, neumonía, infección urinaria y cirugía. El riesgo de óbito en la muestra fue 1,97 veces mayor (HR: 1,97 IC 95% 1,19–3,25) en ancianos con delirium.
Conclusión:
El delirium tuvo una incidencia intermediaria (12,8%); el riesgo de óbito en ese grupo fue aproximadamente 2 veces mayor en un año después de la admisión hospitalaria. Factores demográficos, historia anterior de enfermedades, realización de cirugía y la ocurrencia de complicaciones aumentaron el riesgo y necesitan ser monitoreados durante la hospitalización de ancianos con fracturas.
DESCRITORES
Anciano; Fracturas Óseas; Hospitalización; Delirio; Mortalidad; Enfermería Geriátrica
RESUMO
Objetivo:
Identificar a incidência, os fatores de risco para o delirium e sua associação com óbito em idosos hospitalizados com fraturas.
Método:
Coorte prospectiva, com seguimento de um ano de idosos com diagnóstico clínico ou radiológico de fratura, de um hospital de urgência e trauma de Goiás. O desfecho delirium foi definido pela descrição médica no prontuário. As variáveis preditoras foram demográficas, condições de saúde e complicações da internação. Realizou-se análise múltipla hierarquizada utilizando-se regressão de Poisson robusta, com Risco Relativo como medida de efeito.
Resultados:
Foram incluídos 376 idosos. A incidência de delirium foi 12,8% (n = 48). Os fatores de risco foram: sexo masculino, idade ≥80 anos, demência, cardiopatia, osteoporose, doença pulmonar obstrutiva crônica, acidentes de alta energia, pneumonia, infecção do trato urinário e cirurgia. O risco de óbito na amostra foi 1,97 vezes maior (HR: 1,97 IC 95% 1,19–3,25) em idosos com delírio.
Conclusão:
O delirium teve uma incidência intermediária (12,8%); o risco de óbito nesse grupo foi cerca de 2 vezes maior em um ano após a admissão hospitalar. Fatores demográficos, história pregressa de doenças, realização de cirurgia e ocorrência de complicações aumentaram o risco e precisam ser monitorados durante a internação de idosos com fraturas.
DESCRITORES
Idoso; Fraturas Ósseas; Hospitalização; Delírio; Mortalidade; Enfermagem Geriátrica
INTRODUCTION
Delirium is an acute disorder of attention, awareness, and cognition, which occurs with reduced ability to concentrate or sustain attention, memory deficit, disorientation, and language disorders. This disorder tends to develop in a short period of time and can be classified, according to its clinical manifestations, into hypoactive, hyperactive and mixed(11. Inouye SK, Westendorp RGJ, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-22. https://doi.org/10.1016/S0140-6736(13)60688-1
https://doi.org/10.1016/S0140-6736(13)60...
).
Its incidence ranges from 9 to 50%(22. Neerland BE, Krogset M, Juliebø V, Hylen Ranhoff A, Engedal K, Frihagen F, et al. Perioperative hemodynamics and risk for delirium and new onset dementia in hip fracture patients: a prospective follow-up study. PLoS One 2017;12(7):e01806441. https://doi.org/10.1371/journal.pone.0180641
https://doi.org/10.1371/journal.pone.018...
–44. Folbert EC, Hegeman JH, Gierveld R, van Netten JJ, Velde DV, Ten Duis HJ, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507-15. https://doi.org/10.1007/s00402-017-2646-6
https://doi.org/10.1007/s00402-017-2646-...
) in the elderly with different clinical conditions. Different factors contribute to the occurrence of delirium: more advanced age groups(55. Kubota K, Suzuki A, Ohde S, Yamada U, Hosaka T, Okuno F, et al. Age is the most significantly associated risk factor with the development of delirium in patients hospitalized for more than five days in surgical wards: retrospective cohort study. Ann Surg. 2018;267(5):874-7. https://doi.org/10.1097/SLA.0000000000002347
https://doi.org/10.1097/SLA.000000000000...
–66. Bellelli G, Morandi A, Di Santo SG. “delirium Day”: a nationwide point prevalence study of delirium in older hospitalized patients using an easy standardized diagnostic tool. BMC Med. 2016;14:1-12. https://doi.org/10.1186/s12916-016-0649-8
https://doi.org/10.1186/s12916-016-0649-...
), surgical procedures(22. Neerland BE, Krogset M, Juliebø V, Hylen Ranhoff A, Engedal K, Frihagen F, et al. Perioperative hemodynamics and risk for delirium and new onset dementia in hip fracture patients: a prospective follow-up study. PLoS One 2017;12(7):e01806441. https://doi.org/10.1371/journal.pone.0180641
https://doi.org/10.1371/journal.pone.018...
,77. Levinoff E, Try A, Chabot J. Precipitants of delirium in older inpatients admitted in surgery for post-fall hip fracture: an observational study. J Frailty Aging. 2018;7(1):34-39. https://doi.org/10.14283/jfa.2017.37
https://doi.org/10.14283/jfa.2017.37...
–88. Morino T, Hino M, Yamaoka S, Misaki H, Ogata T, Imai H, et al. Risk factors for delirium after spine surgery: an age-matched analysis. Asian Spine J. 2018;12(4):703-9. https://doi.org/10.31616/asj.2018.12.4.703
https://doi.org/10.31616/asj.2018.12.4.7...
), urinary retention and intestinal constipation(66. Bellelli G, Morandi A, Di Santo SG. “delirium Day”: a nationwide point prevalence study of delirium in older hospitalized patients using an easy standardized diagnostic tool. BMC Med. 2016;14:1-12. https://doi.org/10.1186/s12916-016-0649-8
https://doi.org/10.1186/s12916-016-0649-...
,99. Magny E, Le Petitcorps H, Pociumban M, Bouksani-Kacher Z, Pautas E, Belmin J, et al. Predisposing and precipitating factors for delirium in community-dwelling older adults admitted to hospital with this condition: a prospective case series. PLoS One. 2018;23;13(2):e0193034. https://doi.org/10.1371/journal.pone.0193034
https://doi.org/10.1371/journal.pone.019...
), immobility(66. Bellelli G, Morandi A, Di Santo SG. “delirium Day”: a nationwide point prevalence study of delirium in older hospitalized patients using an easy standardized diagnostic tool. BMC Med. 2016;14:1-12. https://doi.org/10.1186/s12916-016-0649-8
https://doi.org/10.1186/s12916-016-0649-...
,1010. Alamri SH, Ashangity AO, Alshomrani AB, Elmasri AH, Saeed MB, Yahva AS. Ann delirium and correlates of delirium among newly admitted elderly patients: a cross-sectional study in a Saudi general hospital. Ann Saudi Med. 2018;38(1):15-21. https://doi.org/10.5144/0256-4947.2018.15
https://doi.org/10.5144/0256-4947.2018.1...
), pain(1010. Alamri SH, Ashangity AO, Alshomrani AB, Elmasri AH, Saeed MB, Yahva AS. Ann delirium and correlates of delirium among newly admitted elderly patients: a cross-sectional study in a Saudi general hospital. Ann Saudi Med. 2018;38(1):15-21. https://doi.org/10.5144/0256-4947.2018.15
https://doi.org/10.5144/0256-4947.2018.1...
), dehydration(99. Magny E, Le Petitcorps H, Pociumban M, Bouksani-Kacher Z, Pautas E, Belmin J, et al. Predisposing and precipitating factors for delirium in community-dwelling older adults admitted to hospital with this condition: a prospective case series. PLoS One. 2018;23;13(2):e0193034. https://doi.org/10.1371/journal.pone.0193034
https://doi.org/10.1371/journal.pone.019...
–1010. Alamri SH, Ashangity AO, Alshomrani AB, Elmasri AH, Saeed MB, Yahva AS. Ann delirium and correlates of delirium among newly admitted elderly patients: a cross-sectional study in a Saudi general hospital. Ann Saudi Med. 2018;38(1):15-21. https://doi.org/10.5144/0256-4947.2018.15
https://doi.org/10.5144/0256-4947.2018.1...
), use of polypharmacy(1010. Alamri SH, Ashangity AO, Alshomrani AB, Elmasri AH, Saeed MB, Yahva AS. Ann delirium and correlates of delirium among newly admitted elderly patients: a cross-sectional study in a Saudi general hospital. Ann Saudi Med. 2018;38(1):15-21. https://doi.org/10.5144/0256-4947.2018.15
https://doi.org/10.5144/0256-4947.2018.1...
), dementia(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
,1111. Reynish EL, Simona MH, Souza N, Cvoro V, Donnan PT, Guthrie B. Epidemiology and outcomes of people with dementia, delirium and unspecified cognitive impairment in the general hospital: prospective cohort study of 10.014 admissions. BMC Med. 2017;15(1):140. https://doi.org/10.1186/s12916-017-0899-0
https://doi.org/10.1186/s12916-017-0899-...
), reduced caloric and protein intake(66. Bellelli G, Morandi A, Di Santo SG. “delirium Day”: a nationwide point prevalence study of delirium in older hospitalized patients using an easy standardized diagnostic tool. BMC Med. 2016;14:1-12. https://doi.org/10.1186/s12916-016-0649-8
https://doi.org/10.1186/s12916-016-0649-...
), and infections(99. Magny E, Le Petitcorps H, Pociumban M, Bouksani-Kacher Z, Pautas E, Belmin J, et al. Predisposing and precipitating factors for delirium in community-dwelling older adults admitted to hospital with this condition: a prospective case series. PLoS One. 2018;23;13(2):e0193034. https://doi.org/10.1371/journal.pone.0193034
https://doi.org/10.1371/journal.pone.019...
–1010. Alamri SH, Ashangity AO, Alshomrani AB, Elmasri AH, Saeed MB, Yahva AS. Ann delirium and correlates of delirium among newly admitted elderly patients: a cross-sectional study in a Saudi general hospital. Ann Saudi Med. 2018;38(1):15-21. https://doi.org/10.5144/0256-4947.2018.15
https://doi.org/10.5144/0256-4947.2018.1...
).
Although delirium occurs in different settings, the hospital environment is the most common. Its occurrence increases the length of hospital stay(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
,77. Levinoff E, Try A, Chabot J. Precipitants of delirium in older inpatients admitted in surgery for post-fall hip fracture: an observational study. J Frailty Aging. 2018;7(1):34-39. https://doi.org/10.14283/jfa.2017.37
https://doi.org/10.14283/jfa.2017.37...
), the likelihood of readmissions(1212. Gleason LJ, Schmitt EM, Kosar CM. Effect of delirium and other major complications on outcomes after elective surgery in older adults. JAMA Surg. 2015;150(12):134-40. https://doi.org/10.1001/jamasurg.2015.2606
https://doi.org/10.1001/jamasurg.2015.26...
), worsens functionality(44. Folbert EC, Hegeman JH, Gierveld R, van Netten JJ, Velde DV, Ten Duis HJ, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507-15. https://doi.org/10.1007/s00402-017-2646-6
https://doi.org/10.1007/s00402-017-2646-...
), increases deaths(22. Neerland BE, Krogset M, Juliebø V, Hylen Ranhoff A, Engedal K, Frihagen F, et al. Perioperative hemodynamics and risk for delirium and new onset dementia in hip fracture patients: a prospective follow-up study. PLoS One 2017;12(7):e01806441. https://doi.org/10.1371/journal.pone.0180641
https://doi.org/10.1371/journal.pone.018...
,1111. Reynish EL, Simona MH, Souza N, Cvoro V, Donnan PT, Guthrie B. Epidemiology and outcomes of people with dementia, delirium and unspecified cognitive impairment in the general hospital: prospective cohort study of 10.014 admissions. BMC Med. 2017;15(1):140. https://doi.org/10.1186/s12916-017-0899-0
https://doi.org/10.1186/s12916-017-0899-...
,1313. Aslaner MA, Boz M, Çelik A, Ahmedali A, Eroglu S, Metin Aksu N, et al. Etiologies and delirium rates of elderly ED patients with acutely altered mental status: a multicenter prospective study. Am J Emerg Med. 2017;35(1):71-7. https://doi.org/10.1016/j.ajem.2016.10.004
https://doi.org/10.1016/j.ajem.2016.10.0...
–1414. Avelino-Silva TJ, Campora F, Curiati JAE, Jacob-Filho W. Association between delirium superimposed on dementia and mortality in hospitalized older adults: a prospective cohort study. PLoS Med. 2017;14(3):e1002264. https://doi.org/10.1371/journal.pmed.1002264
https://doi.org/10.1371/journal.pmed.100...
) and hospital costs(1515. Zywiel MG, Hurley RT, Perruccio AV, Hancock-Howard RL, Coyte PC, Rampersaud YR. Health economic implications of perioperative delirium in older patients after surgery for a fragility hip fracture. J Bone Joint Surg Am. 2015;97(10):829-36. https://doi.org/10.2106/JBJS.N.00724
https://doi.org/10.2106/JBJS.N.00724...
).
Fractures from low-energy trauma are very prevalent in the elderly and have become an important public health problem because, in addition to expenses, they are related to reduced mobility, worse quality of life, and the occurrence of complications that are difficult to manage in several care settings. Delirium is a frequent complication in the elderly hospitalized with fractures(77. Levinoff E, Try A, Chabot J. Precipitants of delirium in older inpatients admitted in surgery for post-fall hip fracture: an observational study. J Frailty Aging. 2018;7(1):34-39. https://doi.org/10.14283/jfa.2017.37
https://doi.org/10.14283/jfa.2017.37...
,1111. Reynish EL, Simona MH, Souza N, Cvoro V, Donnan PT, Guthrie B. Epidemiology and outcomes of people with dementia, delirium and unspecified cognitive impairment in the general hospital: prospective cohort study of 10.014 admissions. BMC Med. 2017;15(1):140. https://doi.org/10.1186/s12916-017-0899-0
https://doi.org/10.1186/s12916-017-0899-...
–1212. Gleason LJ, Schmitt EM, Kosar CM. Effect of delirium and other major complications on outcomes after elective surgery in older adults. JAMA Surg. 2015;150(12):134-40. https://doi.org/10.1001/jamasurg.2015.2606
https://doi.org/10.1001/jamasurg.2015.26...
) that, individually, correlates with worse outcomes, including death.
Some studies have shown that hospitalizations due to femur and/or hip(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
,77. Levinoff E, Try A, Chabot J. Precipitants of delirium in older inpatients admitted in surgery for post-fall hip fracture: an observational study. J Frailty Aging. 2018;7(1):34-39. https://doi.org/10.14283/jfa.2017.37
https://doi.org/10.14283/jfa.2017.37...
) fractures are among the main causes of hospitalization leading to delirium. However, few studies have analyzed the predictive factors for delirium in the elderly hospitalized with fractures(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
,1616. Jong L, Vajim R, Raats JW, Tmal K, Kujiper TM, Roukema GR. delirium after hip hemiarthroplasty for proximal femoral fracture in elderly patients: risk factos and clinical outcomes. Clin Interv Aging. 2019;26(14):427-35. https://doi.org/10.2147/CIA.S189760
https://doi.org/10.2147/CIA.S189760...
).
Taking the projections of an increase in the proportion of elderly people into account, as well as the fact that fractures are conditions bringing important demands, such as delirium, for the elderly health and for health services, the comprehension of factors precipitating delirium in the hospital environment may help in the proposition of measures to reduce the risk of this complication and consequently improve these patients’ clinical outcome.
Therefore, the objective of this study was to identify the incidence of delirium, its risk factors, and its association with death in the elderly hospitalized with fractures.
METHOD
Design of Study
This is a prospective longitudinal study, with elderly people hospitalized due to fractures over a six-month period. The follow-up of the elderly included in the study was one year, starting on the date of admission.
Population
The population consisted of elderly (age ≥ 60 years) admitted to a reference hospital for urgency and trauma in the city of Goiânia (State of Goiás, Central Brazil) due to any type of fracture, over a period of six months (September 1, 2016 to February 28, 2017).
The aforementioned hospital is large, with 407 hospital beds, a reference for the treatment of highly complex clinical and traumatic emergencies. It is a teaching hospital that receives medical and multiprofessional residency in various specialties every year.
Selection Criteria
During the study period, 1541 elderly people with different medical diagnoses were hospitalized. Of these, all the elderly who had a clinical or radiological diagnosis of fracture described in the medical record, according to the International Statistical Classification of Diseases and Related Health Problems (ICD-10): S02, S12, S22, S32, S42, S52, S62 , S72, S82, S92, T02, T08, T10 and T12 were included. Elderly people who remained in the institution for less than 72 hours were excluded, due to the lack of most variables investigated in this study. Thus, the population of this study was 376 elderly people who had any type of fracture, corresponding to 24.4% of all hospitalizations taking place in a six-month period.
Data Collection
Data were collected in electronic and paper medical records and in the mortality information system (SIM) of the Municipal Health Department of the Municipality of Goiânia. The local Medical Archive Service provided a list of people aged 60 or older hospitalized during the study period. From this list, elderly people diagnosed with a fracture in any location were screened, through the medical description in medical records, with clinical signs, confirmed by X-ray and/or tomography report. For data collection, a structured instrument was used, elaborated based on the literature, previously tested in a pilot study with information on demographic, health and clinical conditions, hospitalization data, mechanisms of trauma and complications during hospitalization. The pilot study data did not integrate the analysis of this research. Death data were collected through SIM using the elderly’s and the mother’s names.
Data Analysis and Treatment
The dependent variable in this study was delirium, defined by the medical entry in the medical records from the time of admission until discharge or death. The incomplete diagnostic hypotheses for delirium were not classified for analysis. Signs of delirium (drowsiness, agitation, and confusion) were collected, but were not included in the outcome.
Independent Variables
Concerning the independent variables, the risk factors analyzed were grouped into: (i) sociodemographic: sex and age group; (ii) health condition: self-reported comorbidities (dementia, heart disease, diabetes, hypertension, osteoporosis, chronic obstructive pulmonary disease), Charlson Index (0-2 and ≥3)(1717. Charlson ME, Szatrowski TP, Peterson J, Jeffrey G. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47(11):1245-51. https://doi.org/10.1016/0895-4356(94)90129-5
https://doi.org/10.1016/0895-4356(94)901...
); polypharmacy, defined by the concomitant use of five or more drugs(1818. Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230. https://doi.org/10.1186/s12877-017-0621-2
https://doi.org/10.1186/s12877-017-0621-...
), medical history of vertigo, previous fractures; (iii) trauma-related factors: fractured bone and trauma mechanism (low-energy trauma that corresponds to falling from standing height, or a high-energy trauma equivalent to falling from heights, motor vehicle collision, collision with motorcyclist, cyclist, and running over of pedestrians); (iv) complications (pneumonia and urinary tract infection) and surgery during hospitalization (yes or no).
For this analysis of the association between delirium and death, the variable delirium was considered exposure, and the variable death from any cause during the follow-up period of the elderly was considered as an outcome.
The collected data were analyzed using the Software for Statistics and data Science (STATA), version 12.0. In the univariate analysis, the magnitude of the association was estimated by the Relative Risk (RR) and its respective confidence intervals (95% CI). The variables with p ≤ 0.20 in the univariate analysis were included in a multiple regression model, with a distal-proximal hierarchical approach,(1919. Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. 1997;26(1):224-7. https://doi.org/10.1093/ije/26.1.224
https://doi.org/10.1093/ije/26.1.224...
) a model that assumes that the variables of the proximal level have a greater relationship with outcome occurrence than those of the intermediate and distal block. Thus, following a distal-proximal direction, demographic characteristics (first level or distal) were used to aggregate the variables related to previous health conditions (second level or intermediate) and the variables that occurred during hospitalization (third level or proximal). Following the inclusion of a new block, the variables of the block already tested were maintained, that is, the later blocks did not influence the previous ones. Variables presenting p value ≤ 0.05, as well as when there were changes in the adjusted PR greater than 10%, were maintained in the model of their respective level. The relationship between delirium and death was presented by the Kaplan Meier curve and the effect of the association was estimated by the Hazard Ratio (HR).
Ethical Aspects
The study was approved by the Ethics Committee of the Hospital de Urgência de Goiânia, opinion 2.874.973/2018. As these are secondary data, the application of the Free and Informed Consent Form was not necessary; therefore, the term of commitment was requested for the use of data for collection in medical records.
RESULTS
During the study period, 1541 medical records of the elderly were evaluated and 376 were included, which met the eligibility criteria. Of this total, 54.3% were women, 66.5% were between 60 and 79 years old with a mean age of 74.7 years (±9.37), 24.3% used 5 or more medications, 21.3% were underweight, 26.0% had 4 or more diseases (Table 1).
Univariate analysis between sociodemographic and health conditions and the occurrence of delirium in elderly people admitted with fractures – Goiânia, GO, Brazil, 2017.
The incidence of delirium was 12.8% (n = 48). As for the type, 20.8% were classified as hypoactive, 37.5% hyperactive, 18.7% mixed, and 23.0% were not informed by the attending physician. Signs of delirium (hypoactivity/drowsiness, confusion and/or psychomotor agitation) were described in 27.7% (n = 104) of the elderly.
In Table 1, the univariate analysis showed an increased risk of delirium for the variables: age group ≥80 years, dementia, heart disease, osteoporosis, and chronic obstructive pulmonary disease (COPD), Charlson index ≥3, polypharmacy, and previous fractures.
Regarding the variables related to hospitalization, there was a greater risk of delirium in the elderly who suffered low-energy trauma, fracture of the femur, had complications such as pneumonia and urinary tract infection (Table 2).
Univariate analysis of sociodemographic and health conditions and the occurrence of delirium in elderly people admitted with fractures – Goiânia, GO, Brazil, 2017.
In the final hierarchical multiple analysis model, the following remained associated with delirium: male patients, 80 years of age or older, dementia, heart disease, osteoporosis, COPD, pneumonia, and surgery (Table 3).
Multiple regression analysis in hierarchical blocks for the occurrence of delirium in patients admitted to the study – Goiânia, GO, Brazil, 2017.
Of the total of 376 hospitalized elderly, 86 (22.9%) died of any cause, and of these, 21 had delirium during hospitalization (24.7%). The occurrence of delirium increased the risk of death by 1.97 (HR: 1.97 95% CI 1.19–3.25, p = 0.008) (Figure 1).
Association between delirium during hospitalization and death from any cause in elderly people with fractures – Goiânia, GO, Brazil, 2017.
DISCUSSION
The incidence of delirium found in this study (12.8%) can be considered as intermediate compared to previous studies(22. Neerland BE, Krogset M, Juliebø V, Hylen Ranhoff A, Engedal K, Frihagen F, et al. Perioperative hemodynamics and risk for delirium and new onset dementia in hip fracture patients: a prospective follow-up study. PLoS One 2017;12(7):e01806441. https://doi.org/10.1371/journal.pone.0180641
https://doi.org/10.1371/journal.pone.018...
–33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
,1111. Reynish EL, Simona MH, Souza N, Cvoro V, Donnan PT, Guthrie B. Epidemiology and outcomes of people with dementia, delirium and unspecified cognitive impairment in the general hospital: prospective cohort study of 10.014 admissions. BMC Med. 2017;15(1):140. https://doi.org/10.1186/s12916-017-0899-0
https://doi.org/10.1186/s12916-017-0899-...
,2020. Dani M, Owen LH, Jackson TA, Rockwood K, Sampson EL, Davis D. Delirium, frailty, and mortality: interactions in a prospective study of hospitalized people. J Gerontol A Biol Sci Med Sci. 2018;73(3):415-8. https://doi.org/10.1093/gerona/glx214
https://doi.org/10.1093/gerona/glx214...
). There is evidence of variation in the incidence of delirium from 9%(2020. Dani M, Owen LH, Jackson TA, Rockwood K, Sampson EL, Davis D. Delirium, frailty, and mortality: interactions in a prospective study of hospitalized people. J Gerontol A Biol Sci Med Sci. 2018;73(3):415-8. https://doi.org/10.1093/gerona/glx214
https://doi.org/10.1093/gerona/glx214...
) to 17%(1111. Reynish EL, Simona MH, Souza N, Cvoro V, Donnan PT, Guthrie B. Epidemiology and outcomes of people with dementia, delirium and unspecified cognitive impairment in the general hospital: prospective cohort study of 10.014 admissions. BMC Med. 2017;15(1):140. https://doi.org/10.1186/s12916-017-0899-0
https://doi.org/10.1186/s12916-017-0899-...
) in emergency services, 28%(22. Neerland BE, Krogset M, Juliebø V, Hylen Ranhoff A, Engedal K, Frihagen F, et al. Perioperative hemodynamics and risk for delirium and new onset dementia in hip fracture patients: a prospective follow-up study. PLoS One 2017;12(7):e01806441. https://doi.org/10.1371/journal.pone.0180641
https://doi.org/10.1371/journal.pone.018...
) to 34%(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
) in patients with fractures, increasing to about 50% in patients with previous health conditions present at admission, such as dementia(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
). In this study, this intermediate incidence can be attributed to the underdiagnosis of delirium, since 28% had clinical criteria for diagnosis. Despite being a widely discussed subject in the literature, in clinical practice the diagnosis and management of delirium are still incipient(2121. Luna AF, Entringer AP, Silva RCL. Prevalência do subdiagnóstico de delirium entre pacientes internados em unidade de terapia intensiva. Rev Enferm UERJ.2016;24(1):e6238. http://dx.doi.org/10.12957/reuerj.2016.6238
http://dx.doi.org/10.12957/reuerj.2016.6...
). As it is a common complication in elderly people with fractures, it is important to recognize the risk factors for its occurrence.
The relationship between advanced age (≥80 years) and delirium corroborates previous studies(55. Kubota K, Suzuki A, Ohde S, Yamada U, Hosaka T, Okuno F, et al. Age is the most significantly associated risk factor with the development of delirium in patients hospitalized for more than five days in surgical wards: retrospective cohort study. Ann Surg. 2018;267(5):874-7. https://doi.org/10.1097/SLA.0000000000002347
https://doi.org/10.1097/SLA.000000000000...
,2222. Santos FS. Mecanismos fisiopatológicos do delirium. Rev Psiquiátr Clin. 2005;32(3):104-12. http://dx.doi.org/10.1590/S0101-60832005000300002
http://dx.doi.org/10.1590/S0101-60832005...
). During the aging process, the elderly have difficulties in maintaining their homeostasis, which leads to a gradual decrease in the physiological reserve and consequent accumulated decline in several physiological systems, leading to the occurrence of delirium(2222. Santos FS. Mecanismos fisiopatológicos do delirium. Rev Psiquiátr Clin. 2005;32(3):104-12. http://dx.doi.org/10.1590/S0101-60832005000300002
http://dx.doi.org/10.1590/S0101-60832005...
). Still in relation to demographic aspects, elderly men had a higher risk of delirium compared to women. This datum may be related to a higher incidence of traffic accidents by men and, consequently, a higher number of admissions to the study site. This finding shall be further explored, as previous studies have shown a higher proportion among women(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
–44. Folbert EC, Hegeman JH, Gierveld R, van Netten JJ, Velde DV, Ten Duis HJ, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507-15. https://doi.org/10.1007/s00402-017-2646-6
https://doi.org/10.1007/s00402-017-2646-...
,1616. Jong L, Vajim R, Raats JW, Tmal K, Kujiper TM, Roukema GR. delirium after hip hemiarthroplasty for proximal femoral fracture in elderly patients: risk factos and clinical outcomes. Clin Interv Aging. 2019;26(14):427-35. https://doi.org/10.2147/CIA.S189760
https://doi.org/10.2147/CIA.S189760...
).
As for comorbidities, elderly people with a previous history of dementia, heart disease, COPD, and osteoporosis had an increased risk of delirium. Previous studies show that dementia is one of the most important risk factors for delirium(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
–44. Folbert EC, Hegeman JH, Gierveld R, van Netten JJ, Velde DV, Ten Duis HJ, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507-15. https://doi.org/10.1007/s00402-017-2646-6
https://doi.org/10.1007/s00402-017-2646-...
,66. Bellelli G, Morandi A, Di Santo SG. “delirium Day”: a nationwide point prevalence study of delirium in older hospitalized patients using an easy standardized diagnostic tool. BMC Med. 2016;14:1-12. https://doi.org/10.1186/s12916-016-0649-8
https://doi.org/10.1186/s12916-016-0649-...
,99. Magny E, Le Petitcorps H, Pociumban M, Bouksani-Kacher Z, Pautas E, Belmin J, et al. Predisposing and precipitating factors for delirium in community-dwelling older adults admitted to hospital with this condition: a prospective case series. PLoS One. 2018;23;13(2):e0193034. https://doi.org/10.1371/journal.pone.0193034
https://doi.org/10.1371/journal.pone.019...
,1616. Jong L, Vajim R, Raats JW, Tmal K, Kujiper TM, Roukema GR. delirium after hip hemiarthroplasty for proximal femoral fracture in elderly patients: risk factos and clinical outcomes. Clin Interv Aging. 2019;26(14):427-35. https://doi.org/10.2147/CIA.S189760
https://doi.org/10.2147/CIA.S189760...
). One study analyzed the risk factors for the occurrence of delirium in patients admitted for hip fractures and the incidence observed was 35% in the group with dementia and 21% in those with no previous dementia(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
). In dementia, there is cortical and subcortical structures impairment and deregulation in the release of neurotransmitters acting on individuals’ homeostasis, leading to functional cognitive decline, which may justify this overlap of delirium with dementia(99. Magny E, Le Petitcorps H, Pociumban M, Bouksani-Kacher Z, Pautas E, Belmin J, et al. Predisposing and precipitating factors for delirium in community-dwelling older adults admitted to hospital with this condition: a prospective case series. PLoS One. 2018;23;13(2):e0193034. https://doi.org/10.1371/journal.pone.0193034
https://doi.org/10.1371/journal.pone.019...
,2222. Santos FS. Mecanismos fisiopatológicos do delirium. Rev Psiquiátr Clin. 2005;32(3):104-12. http://dx.doi.org/10.1590/S0101-60832005000300002
http://dx.doi.org/10.1590/S0101-60832005...
).
Elderly people with COPD also had a higher risk of delirium in this study. A study demonstrated that elderly people hospitalized with COPD more frequently have: recurrent infections, low respiratory infections, hydroelectrolytic disorders, associated cardiac diseases, ventilatory support, longer ICU stays(2323. Medrano MJA, Torres OY, Robles IB, Casas-Méndez LF, Barbé F, Batlle J. Exacerbation of chronic obstructive pulmonary disease: an analysis of the care process in a regional hospital emergency department. Medicine (Baltimore). 2018;97(31):e11601. https://doi.org/10.1097/MD.0000000000011601
https://doi.org/10.1097/MD.0000000000011...
). The combination of these factors can contribute to complications, one of them being delirium(2323. Medrano MJA, Torres OY, Robles IB, Casas-Méndez LF, Barbé F, Batlle J. Exacerbation of chronic obstructive pulmonary disease: an analysis of the care process in a regional hospital emergency department. Medicine (Baltimore). 2018;97(31):e11601. https://doi.org/10.1097/MD.0000000000011601
https://doi.org/10.1097/MD.0000000000011...
).
No studies evaluating the relationship between heart disease and delirium in elderly people with fractures were found. However, previous studies with hospitalized elderly people(2424. Kotfis K, Szylinska A, Listewnik M, Strzelbicka M, Brykcznski M, Rotter I, et al. Early delirium after cardiac surgery: na analysis of incidence and risk factors in elderly (≥65 years) and very elderly (≥80 years) patients. Clin Interv Aging. 2018;30(13):1061-70. https://doi.org/10.2147/CIA.S166909
https://doi.org/10.2147/CIA.S166909...
–2525. Falsini G, Grotti S, Porto I, Toccafondi G, Fraticelli A, Angioli P, et al. Long-term prognostic value of delirium in elderly patients with acute cardiac diseases admitted to two cardiac intensive care units: a prospective study (DELIRIUM CORDIS). Eur Heart J Acute Cardiovasc Care. 2018;7(7):661-70. https://doi.org/10.1177/2048872617695235
https://doi.org/10.1177/2048872617695235...
) show that, among cardiac patients, there is a lower ejection fraction, arrhythmias, and decreased peripheral perfusion(2424. Kotfis K, Szylinska A, Listewnik M, Strzelbicka M, Brykcznski M, Rotter I, et al. Early delirium after cardiac surgery: na analysis of incidence and risk factors in elderly (≥65 years) and very elderly (≥80 years) patients. Clin Interv Aging. 2018;30(13):1061-70. https://doi.org/10.2147/CIA.S166909
https://doi.org/10.2147/CIA.S166909...
), which could explain more frequently confusion disorders. In addition, they show greater hemodynamic instability during the perioperative period, increasing complications and length of hospital stay(2424. Kotfis K, Szylinska A, Listewnik M, Strzelbicka M, Brykcznski M, Rotter I, et al. Early delirium after cardiac surgery: na analysis of incidence and risk factors in elderly (≥65 years) and very elderly (≥80 years) patients. Clin Interv Aging. 2018;30(13):1061-70. https://doi.org/10.2147/CIA.S166909
https://doi.org/10.2147/CIA.S166909...
–2525. Falsini G, Grotti S, Porto I, Toccafondi G, Fraticelli A, Angioli P, et al. Long-term prognostic value of delirium in elderly patients with acute cardiac diseases admitted to two cardiac intensive care units: a prospective study (DELIRIUM CORDIS). Eur Heart J Acute Cardiovasc Care. 2018;7(7):661-70. https://doi.org/10.1177/2048872617695235
https://doi.org/10.1177/2048872617695235...
).
History of osteoporosis has also been associated with delirium. One study observed an association between the reduction of Bone Mineral Density and osteoporosis with cognitive impairment(2626. Wang XF, Wang XJ, Jing YX, Sun LH, Tao B, Wang WQ, et al. The associations between hypovitaminosis D, higher PTH levels with bone mineral densities and risk of the 10-year probability of major osteoporotic fractures in Chinese patients with t2dm. Endocr Pract. 2018;24(4)334-41. https://doi.org/10.4158/EP-2017-0164
https://doi.org/10.4158/EP-2017-0164...
). The hypothesis the authors raised for this association was hormonal changes and an increase in inflammatory markers that are known to alter cognitive function(2626. Wang XF, Wang XJ, Jing YX, Sun LH, Tao B, Wang WQ, et al. The associations between hypovitaminosis D, higher PTH levels with bone mineral densities and risk of the 10-year probability of major osteoporotic fractures in Chinese patients with t2dm. Endocr Pract. 2018;24(4)334-41. https://doi.org/10.4158/EP-2017-0164
https://doi.org/10.4158/EP-2017-0164...
).
During hospitalization, risk factors for delirium were surgery and complications such as pneumonia and urinary tract infection.
Elderly hospitalized with fractures often require a surgical approach; however, their clinical conditions are not always satisfactory as they are under surgical stress. The postoperative period has been associated with delirium and a complicated course of hospitalization(22. Neerland BE, Krogset M, Juliebø V, Hylen Ranhoff A, Engedal K, Frihagen F, et al. Perioperative hemodynamics and risk for delirium and new onset dementia in hip fracture patients: a prospective follow-up study. PLoS One 2017;12(7):e01806441. https://doi.org/10.1371/journal.pone.0180641
https://doi.org/10.1371/journal.pone.018...
–44. Folbert EC, Hegeman JH, Gierveld R, van Netten JJ, Velde DV, Ten Duis HJ, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507-15. https://doi.org/10.1007/s00402-017-2646-6
https://doi.org/10.1007/s00402-017-2646-...
,88. Morino T, Hino M, Yamaoka S, Misaki H, Ogata T, Imai H, et al. Risk factors for delirium after spine surgery: an age-matched analysis. Asian Spine J. 2018;12(4):703-9. https://doi.org/10.31616/asj.2018.12.4.703
https://doi.org/10.31616/asj.2018.12.4.7...
). Investigation among the postoperative risk factors of orthopedic surgery and delirium demonstrated an association with events that occurred during the intraoperative period, such as: blood loss and laboratory changes, mainly of inflammatory markers such as C-reactive protein (CRP)(88. Morino T, Hino M, Yamaoka S, Misaki H, Ogata T, Imai H, et al. Risk factors for delirium after spine surgery: an age-matched analysis. Asian Spine J. 2018;12(4):703-9. https://doi.org/10.31616/asj.2018.12.4.703
https://doi.org/10.31616/asj.2018.12.4.7...
). There is also evidence that elderly people with an ASA classification >3 are at increased risk for delirium(1010. Alamri SH, Ashangity AO, Alshomrani AB, Elmasri AH, Saeed MB, Yahva AS. Ann delirium and correlates of delirium among newly admitted elderly patients: a cross-sectional study in a Saudi general hospital. Ann Saudi Med. 2018;38(1):15-21. https://doi.org/10.5144/0256-4947.2018.15
https://doi.org/10.5144/0256-4947.2018.1...
,1414. Avelino-Silva TJ, Campora F, Curiati JAE, Jacob-Filho W. Association between delirium superimposed on dementia and mortality in hospitalized older adults: a prospective cohort study. PLoS Med. 2017;14(3):e1002264. https://doi.org/10.1371/journal.pmed.1002264
https://doi.org/10.1371/journal.pmed.100...
,2727. Schubert M, Schurch R, Boettger S, Garcia-Nunez D, Schwarz U, Bettex D, et al. A hospital wide evaluation of delirium prevalence and outcomes in acute care patients a cohort study. BMC Health Serv Res. 2018;18(1):550. https://doi.org/10.1186/s12913-018-3345-x
https://doi.org/10.1186/s12913-018-3345-...
). Other studies(2626. Wang XF, Wang XJ, Jing YX, Sun LH, Tao B, Wang WQ, et al. The associations between hypovitaminosis D, higher PTH levels with bone mineral densities and risk of the 10-year probability of major osteoporotic fractures in Chinese patients with t2dm. Endocr Pract. 2018;24(4)334-41. https://doi.org/10.4158/EP-2017-0164
https://doi.org/10.4158/EP-2017-0164...
,2828. Zhu CC, Fang QJ, Zhou QY, Huang CM, Hu MJ, Yuan KM, et al. Nested case-control study on risk factors of postoperative hyperative-type delirium in geriatric orthopedic patients. Zhonghua Yi XueZaZhi. 2018;98(40):3230-4. https://doi.org/10.3760/cma.j.issn.0376-2491.2018.40.003
https://doi.org/10.3760/cma.j.issn.0376-...
) have related delirium in the postoperative period to a higher incidence of pain, immobilization, urinary retention, and bed rest in an intensive care unit.
During the hospitalization period, the elderly who developed pneumonia and UTI had a higher risk of delirium, data that corroborate previous studies(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
,99. Magny E, Le Petitcorps H, Pociumban M, Bouksani-Kacher Z, Pautas E, Belmin J, et al. Predisposing and precipitating factors for delirium in community-dwelling older adults admitted to hospital with this condition: a prospective case series. PLoS One. 2018;23;13(2):e0193034. https://doi.org/10.1371/journal.pone.0193034
https://doi.org/10.1371/journal.pone.019...
–1010. Alamri SH, Ashangity AO, Alshomrani AB, Elmasri AH, Saeed MB, Yahva AS. Ann delirium and correlates of delirium among newly admitted elderly patients: a cross-sectional study in a Saudi general hospital. Ann Saudi Med. 2018;38(1):15-21. https://doi.org/10.5144/0256-4947.2018.15
https://doi.org/10.5144/0256-4947.2018.1...
,1313. Aslaner MA, Boz M, Çelik A, Ahmedali A, Eroglu S, Metin Aksu N, et al. Etiologies and delirium rates of elderly ED patients with acutely altered mental status: a multicenter prospective study. Am J Emerg Med. 2017;35(1):71-7. https://doi.org/10.1016/j.ajem.2016.10.004
https://doi.org/10.1016/j.ajem.2016.10.0...
). Pneumonia and UTI are frequent complications during elderly hospitalization due to different causes(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
,99. Magny E, Le Petitcorps H, Pociumban M, Bouksani-Kacher Z, Pautas E, Belmin J, et al. Predisposing and precipitating factors for delirium in community-dwelling older adults admitted to hospital with this condition: a prospective case series. PLoS One. 2018;23;13(2):e0193034. https://doi.org/10.1371/journal.pone.0193034
https://doi.org/10.1371/journal.pone.019...
–1010. Alamri SH, Ashangity AO, Alshomrani AB, Elmasri AH, Saeed MB, Yahva AS. Ann delirium and correlates of delirium among newly admitted elderly patients: a cross-sectional study in a Saudi general hospital. Ann Saudi Med. 2018;38(1):15-21. https://doi.org/10.5144/0256-4947.2018.15
https://doi.org/10.5144/0256-4947.2018.1...
,1313. Aslaner MA, Boz M, Çelik A, Ahmedali A, Eroglu S, Metin Aksu N, et al. Etiologies and delirium rates of elderly ED patients with acutely altered mental status: a multicenter prospective study. Am J Emerg Med. 2017;35(1):71-7. https://doi.org/10.1016/j.ajem.2016.10.004
https://doi.org/10.1016/j.ajem.2016.10.0...
). Hospitalizations due to fractures are generally prolonged(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
,77. Levinoff E, Try A, Chabot J. Precipitants of delirium in older inpatients admitted in surgery for post-fall hip fracture: an observational study. J Frailty Aging. 2018;7(1):34-39. https://doi.org/10.14283/jfa.2017.37
https://doi.org/10.14283/jfa.2017.37...
), contributing to decreased functionality and mobility, leading to respiratory and urinary complications, for instance. However, in this study, these complications diagnosis was not always concluded before the occurrence of delirium, which suggests that there is an association between these infections and delirium during hospitalization, but without the possibility of inferring causality.
Delirium increased the risk of death in this elderly population hospitalized due to fractures. The relationship between delirium and death in the elderly with different clinical conditions, including fractures, has been discussed in the literature(44. Folbert EC, Hegeman JH, Gierveld R, van Netten JJ, Velde DV, Ten Duis HJ, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507-15. https://doi.org/10.1007/s00402-017-2646-6
https://doi.org/10.1007/s00402-017-2646-...
,1616. Jong L, Vajim R, Raats JW, Tmal K, Kujiper TM, Roukema GR. delirium after hip hemiarthroplasty for proximal femoral fracture in elderly patients: risk factos and clinical outcomes. Clin Interv Aging. 2019;26(14):427-35. https://doi.org/10.2147/CIA.S189760
https://doi.org/10.2147/CIA.S189760...
,2929. Shield L, Henderson V, Caslake R. Comprehensive geriatric assessment for prevention of delirium after hip fracture: a systematic review of randomised controlled trials. J Am Geriatric Soc. 2017;65(7):1559-65. https://doi.org/10.1111/jgs.14846
https://doi.org/10.1111/jgs.14846...
). Studies show that the death rate is high in the elderly with fractures, with a high proportion in those with delirium(44. Folbert EC, Hegeman JH, Gierveld R, van Netten JJ, Velde DV, Ten Duis HJ, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507-15. https://doi.org/10.1007/s00402-017-2646-6
https://doi.org/10.1007/s00402-017-2646-...
,1616. Jong L, Vajim R, Raats JW, Tmal K, Kujiper TM, Roukema GR. delirium after hip hemiarthroplasty for proximal femoral fracture in elderly patients: risk factos and clinical outcomes. Clin Interv Aging. 2019;26(14):427-35. https://doi.org/10.2147/CIA.S189760
https://doi.org/10.2147/CIA.S189760...
). A study observed that in one year the death rate in patients with fractures was 19%, increasing to 39% in those with delirium(1616. Jong L, Vajim R, Raats JW, Tmal K, Kujiper TM, Roukema GR. delirium after hip hemiarthroplasty for proximal femoral fracture in elderly patients: risk factos and clinical outcomes. Clin Interv Aging. 2019;26(14):427-35. https://doi.org/10.2147/CIA.S189760
https://doi.org/10.2147/CIA.S189760...
). It was found in a study that patients hospitalized with delirium were three times more likely to die when compared to those who did not have delirium(2727. Schubert M, Schurch R, Boettger S, Garcia-Nunez D, Schwarz U, Bettex D, et al. A hospital wide evaluation of delirium prevalence and outcomes in acute care patients a cohort study. BMC Health Serv Res. 2018;18(1):550. https://doi.org/10.1186/s12913-018-3345-x
https://doi.org/10.1186/s12913-018-3345-...
). Despite the high rate, it is not clear in the literature whether delirium is directly related to the outcome death or whether it can be an indicator of severity of comorbidities and of health conditions and complications(33. Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
https://doi.org/10.2147/CIA.S115945...
–44. Folbert EC, Hegeman JH, Gierveld R, van Netten JJ, Velde DV, Ten Duis HJ, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507-15. https://doi.org/10.1007/s00402-017-2646-6
https://doi.org/10.1007/s00402-017-2646-...
,99. Magny E, Le Petitcorps H, Pociumban M, Bouksani-Kacher Z, Pautas E, Belmin J, et al. Predisposing and precipitating factors for delirium in community-dwelling older adults admitted to hospital with this condition: a prospective case series. PLoS One. 2018;23;13(2):e0193034. https://doi.org/10.1371/journal.pone.0193034
https://doi.org/10.1371/journal.pone.019...
,2929. Shield L, Henderson V, Caslake R. Comprehensive geriatric assessment for prevention of delirium after hip fracture: a systematic review of randomised controlled trials. J Am Geriatric Soc. 2017;65(7):1559-65. https://doi.org/10.1111/jgs.14846
https://doi.org/10.1111/jgs.14846...
–3030. Kennedy M, Enander RA, Tadiri SP, Wolfe RE, Shapiro NI, Marcantonio ER. Delirium risk prediction, health care utilization and mortality of elderly emergency department patients. J Am Geriatric Soc. 2014;62(3):462-9. https://doi.org/10.1111/jgs.12692
https://doi.org/10.1111/jgs.12692...
). Together, these factors can increase the occurrence of deaths.
As limitations of this study, we can mention the collection of data in medical records, which hindered the application of standardized instruments for detecting delirium. In addition, the lack of information in medical records stands out, which made it impossible to investigate variables such as disabilities. To overcome these limitations, some precautions, such as standardizing the formulary, collecting the medical diagnosis, conducting a pilot test, were taken to ensure the reliability of the data collected.
CONCLUSION
The findings of this study demonstrated a 12.8% incidence of delirium in elderly people with fractures. Demographic factors, previous history of diseases, surgery and the occurrence of complications during hospitalization were risk factors for delirium during hospitalization. The occurrence of delirium increased the risk of death by 1.97 times and was, during hospitalization, a predictor for death from any cause among the elderly after one year of follow-up of hospital admission.
Together, the findings signal the need for health conditions assessment and monitoring of complications such as pneumonia and UTI for the early identification of delirium and its consequent management.
The multiprofessional team, having diverse knowledge in specific areas and daily monitoring these patients’ progression, shall work in the identification of these risk factors for the prevention of delirium and intervene so that they are controlled or minimized in the face of targeted assistance.
Moreover, considering that the incidence of delirium after fractures decreases when using multidimensional assessment of the elderly, it is recommended that geriatric assessment protocols be implemented in large hospitals such as this one for clinical assessment and monitoring of hospitalized elderly with fractures.
REFERENCES
-
1.Inouye SK, Westendorp RGJ, Saczynski JS. Delirium in elderly people. Lancet. 2014;383(9920):911-22. https://doi.org/10.1016/S0140-6736(13)60688-1
» https://doi.org/10.1016/S0140-6736(13)60688-1 -
2.Neerland BE, Krogset M, Juliebø V, Hylen Ranhoff A, Engedal K, Frihagen F, et al. Perioperative hemodynamics and risk for delirium and new onset dementia in hip fracture patients: a prospective follow-up study. PLoS One 2017;12(7):e01806441. https://doi.org/10.1371/journal.pone.0180641
» https://doi.org/10.1371/journal.pone.0180641 -
3.Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421-30. https://doi.org/10.2147/CIA.S115945
» https://doi.org/10.2147/CIA.S115945 -
4.Folbert EC, Hegeman JH, Gierveld R, van Netten JJ, Velde DV, Ten Duis HJ, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507-15. https://doi.org/10.1007/s00402-017-2646-6
» https://doi.org/10.1007/s00402-017-2646-6 -
5.Kubota K, Suzuki A, Ohde S, Yamada U, Hosaka T, Okuno F, et al. Age is the most significantly associated risk factor with the development of delirium in patients hospitalized for more than five days in surgical wards: retrospective cohort study. Ann Surg. 2018;267(5):874-7. https://doi.org/10.1097/SLA.0000000000002347
» https://doi.org/10.1097/SLA.0000000000002347 -
6.Bellelli G, Morandi A, Di Santo SG. “delirium Day”: a nationwide point prevalence study of delirium in older hospitalized patients using an easy standardized diagnostic tool. BMC Med. 2016;14:1-12. https://doi.org/10.1186/s12916-016-0649-8
» https://doi.org/10.1186/s12916-016-0649-8 -
7.Levinoff E, Try A, Chabot J. Precipitants of delirium in older inpatients admitted in surgery for post-fall hip fracture: an observational study. J Frailty Aging. 2018;7(1):34-39. https://doi.org/10.14283/jfa.2017.37
» https://doi.org/10.14283/jfa.2017.37 -
8.Morino T, Hino M, Yamaoka S, Misaki H, Ogata T, Imai H, et al. Risk factors for delirium after spine surgery: an age-matched analysis. Asian Spine J. 2018;12(4):703-9. https://doi.org/10.31616/asj.2018.12.4.703
» https://doi.org/10.31616/asj.2018.12.4.703 -
9.Magny E, Le Petitcorps H, Pociumban M, Bouksani-Kacher Z, Pautas E, Belmin J, et al. Predisposing and precipitating factors for delirium in community-dwelling older adults admitted to hospital with this condition: a prospective case series. PLoS One. 2018;23;13(2):e0193034. https://doi.org/10.1371/journal.pone.0193034
» https://doi.org/10.1371/journal.pone.0193034 -
10.Alamri SH, Ashangity AO, Alshomrani AB, Elmasri AH, Saeed MB, Yahva AS. Ann delirium and correlates of delirium among newly admitted elderly patients: a cross-sectional study in a Saudi general hospital. Ann Saudi Med. 2018;38(1):15-21. https://doi.org/10.5144/0256-4947.2018.15
» https://doi.org/10.5144/0256-4947.2018.15 -
11.Reynish EL, Simona MH, Souza N, Cvoro V, Donnan PT, Guthrie B. Epidemiology and outcomes of people with dementia, delirium and unspecified cognitive impairment in the general hospital: prospective cohort study of 10.014 admissions. BMC Med. 2017;15(1):140. https://doi.org/10.1186/s12916-017-0899-0
» https://doi.org/10.1186/s12916-017-0899-0 -
12.Gleason LJ, Schmitt EM, Kosar CM. Effect of delirium and other major complications on outcomes after elective surgery in older adults. JAMA Surg. 2015;150(12):134-40. https://doi.org/10.1001/jamasurg.2015.2606
» https://doi.org/10.1001/jamasurg.2015.2606 -
13.Aslaner MA, Boz M, Çelik A, Ahmedali A, Eroglu S, Metin Aksu N, et al. Etiologies and delirium rates of elderly ED patients with acutely altered mental status: a multicenter prospective study. Am J Emerg Med. 2017;35(1):71-7. https://doi.org/10.1016/j.ajem.2016.10.004
» https://doi.org/10.1016/j.ajem.2016.10.004 -
14.Avelino-Silva TJ, Campora F, Curiati JAE, Jacob-Filho W. Association between delirium superimposed on dementia and mortality in hospitalized older adults: a prospective cohort study. PLoS Med. 2017;14(3):e1002264. https://doi.org/10.1371/journal.pmed.1002264
» https://doi.org/10.1371/journal.pmed.1002264 -
15.Zywiel MG, Hurley RT, Perruccio AV, Hancock-Howard RL, Coyte PC, Rampersaud YR. Health economic implications of perioperative delirium in older patients after surgery for a fragility hip fracture. J Bone Joint Surg Am. 2015;97(10):829-36. https://doi.org/10.2106/JBJS.N.00724
» https://doi.org/10.2106/JBJS.N.00724 -
16.Jong L, Vajim R, Raats JW, Tmal K, Kujiper TM, Roukema GR. delirium after hip hemiarthroplasty for proximal femoral fracture in elderly patients: risk factos and clinical outcomes. Clin Interv Aging. 2019;26(14):427-35. https://doi.org/10.2147/CIA.S189760
» https://doi.org/10.2147/CIA.S189760 -
17.Charlson ME, Szatrowski TP, Peterson J, Jeffrey G. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47(11):1245-51. https://doi.org/10.1016/0895-4356(94)90129-5
» https://doi.org/10.1016/0895-4356(94)90129-5 -
18.Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230. https://doi.org/10.1186/s12877-017-0621-2
» https://doi.org/10.1186/s12877-017-0621-2 -
19.Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. 1997;26(1):224-7. https://doi.org/10.1093/ije/26.1.224
» https://doi.org/10.1093/ije/26.1.224 -
20.Dani M, Owen LH, Jackson TA, Rockwood K, Sampson EL, Davis D. Delirium, frailty, and mortality: interactions in a prospective study of hospitalized people. J Gerontol A Biol Sci Med Sci. 2018;73(3):415-8. https://doi.org/10.1093/gerona/glx214
» https://doi.org/10.1093/gerona/glx214 -
21.Luna AF, Entringer AP, Silva RCL. Prevalência do subdiagnóstico de delirium entre pacientes internados em unidade de terapia intensiva. Rev Enferm UERJ.2016;24(1):e6238. http://dx.doi.org/10.12957/reuerj.2016.6238
» http://dx.doi.org/10.12957/reuerj.2016.6238 -
22.Santos FS. Mecanismos fisiopatológicos do delirium Rev Psiquiátr Clin. 2005;32(3):104-12. http://dx.doi.org/10.1590/S0101-60832005000300002
» http://dx.doi.org/10.1590/S0101-60832005000300002 -
23.Medrano MJA, Torres OY, Robles IB, Casas-Méndez LF, Barbé F, Batlle J. Exacerbation of chronic obstructive pulmonary disease: an analysis of the care process in a regional hospital emergency department. Medicine (Baltimore). 2018;97(31):e11601. https://doi.org/10.1097/MD.0000000000011601
» https://doi.org/10.1097/MD.0000000000011601 -
24.Kotfis K, Szylinska A, Listewnik M, Strzelbicka M, Brykcznski M, Rotter I, et al. Early delirium after cardiac surgery: na analysis of incidence and risk factors in elderly (≥65 years) and very elderly (≥80 years) patients. Clin Interv Aging. 2018;30(13):1061-70. https://doi.org/10.2147/CIA.S166909
» https://doi.org/10.2147/CIA.S166909 -
25.Falsini G, Grotti S, Porto I, Toccafondi G, Fraticelli A, Angioli P, et al. Long-term prognostic value of delirium in elderly patients with acute cardiac diseases admitted to two cardiac intensive care units: a prospective study (DELIRIUM CORDIS). Eur Heart J Acute Cardiovasc Care. 2018;7(7):661-70. https://doi.org/10.1177/2048872617695235
» https://doi.org/10.1177/2048872617695235 -
26.Wang XF, Wang XJ, Jing YX, Sun LH, Tao B, Wang WQ, et al. The associations between hypovitaminosis D, higher PTH levels with bone mineral densities and risk of the 10-year probability of major osteoporotic fractures in Chinese patients with t2dm. Endocr Pract. 2018;24(4)334-41. https://doi.org/10.4158/EP-2017-0164
» https://doi.org/10.4158/EP-2017-0164 -
27.Schubert M, Schurch R, Boettger S, Garcia-Nunez D, Schwarz U, Bettex D, et al. A hospital wide evaluation of delirium prevalence and outcomes in acute care patients a cohort study. BMC Health Serv Res. 2018;18(1):550. https://doi.org/10.1186/s12913-018-3345-x
» https://doi.org/10.1186/s12913-018-3345-x -
28.Zhu CC, Fang QJ, Zhou QY, Huang CM, Hu MJ, Yuan KM, et al. Nested case-control study on risk factors of postoperative hyperative-type delirium in geriatric orthopedic patients. Zhonghua Yi XueZaZhi. 2018;98(40):3230-4. https://doi.org/10.3760/cma.j.issn.0376-2491.2018.40.003
» https://doi.org/10.3760/cma.j.issn.0376-2491.2018.40.003 -
29.Shield L, Henderson V, Caslake R. Comprehensive geriatric assessment for prevention of delirium after hip fracture: a systematic review of randomised controlled trials. J Am Geriatric Soc. 2017;65(7):1559-65. https://doi.org/10.1111/jgs.14846
» https://doi.org/10.1111/jgs.14846 -
30.Kennedy M, Enander RA, Tadiri SP, Wolfe RE, Shapiro NI, Marcantonio ER. Delirium risk prediction, health care utilization and mortality of elderly emergency department patients. J Am Geriatric Soc. 2014;62(3):462-9. https://doi.org/10.1111/jgs.12692
» https://doi.org/10.1111/jgs.12692
Publication Dates
-
Publication in this collection
20 Aug 2021 -
Date of issue
2021
History
-
Received
25 Oct 2020 -
Accepted
24 Mar 2021