SPECIAL ARTICLE
Intensive care provision: a global problem
Andrew RhodesI; Rui Paulo MorenoII
ICritical Care Medicine, St George's Healthcare NHS Trust and St George's, University of London, UK
IINeurocritical Intensive Care Unit, Hospital de São José, Centro Hospitalar de Lisboa Central, E.P.E. - Lisboa, Portugal
Corresponding author
Recently, many countries have described a growing gap between the supply and the demand of intensivists and the consequent capability of the country to provide adequate intensive care.(1,2) This gap is mainly driven by the increasing population size of many nations, together with the recognition that life expectancy is increasing in tandem with the proliferation of the so-called "civilisation" diseases, such as diabetes, coronary heart disease, stroke and obesity. These aged groups of patients, who have (or will have) significant comorbid diseases, are the very population that present to intensive care medicine in North America and in most European countries; often being admitted to the hospital because of an acute illness or a complication after major elective surgery.(3) The proper use of intensive care medicine can save a significant number of these patients and may enable them to return to an active life; however, these efforts will also consume a great deal of resources for a group of patients who may not benefit. Unless this increased demand for beds is appropriately managed, there will be problems, as a skilled and trained staff will not have been identified and be available. Consequently, healthcare providers will need to either provide intensive care using untrained and unqualified staff, or they will need to change to a model of providing intensive care that uses professional groups with delegated competency from physicians working according to protocols and guidelines. Either option will permit these healthcare providers to operate with limited understanding of their work and the available treatment alternatives for any specific patient.
The first step towards planning for a change (in this case, an increase in the provided services) is to understand what is currently provided. Unfortunately, this understanding is rarely present and needs to be urgently addressed. Recent studies assessing the provision of intensive care between countries and the surgical outcomes provide interesting insights into this issue.(4-6) Most of these studies have been designed to look at European populations; however, many of the salient factors present in Europe likely exist in Brazil, and the lessons derived from these studies are equally relevant.
If intensive care bed numbers are restricted - either formally or informally-patient selection must occur; this practice is commonly referred to as rationing.(7) When intensive care is not available, services react in different manners, including the early or premature discharge of patients already in the service, delayed admission of presenting patients, changing thresholds for the withdrawal of care, cancellation of elective patients who are planned to be admitted after routine surgery or restriction of admission to certain patient groups based on the type and conditions of health insurance.(8) None of these reactions are desirable, and many will likely reduce the quality of care that the service provides and may ultimately affect patient outcomes. Data from the previous decade in the United Kingdom have acknowledged these weaknesses (at least in the UK system) and have documented the effect that this reaction has on the outcome of surgical patients who required critical care after surgery. In 2006, Pearse et al.(9) reported on data extracted from large databases documenting UK practice. These researchers delineated a group of patients who were at high risk for complications and death post-surgery. Interestingly, they found that few of these patients were admitted to a critical care facility after surgery and that 85% of the patients who died were never admitted to a critical care unit. Some of these patients may have been inappropriate for referral to and care in an intensive care environment; however, it seems unlikely that none of them would have benefited from this step-up care. Unfortunately, this pattern is unlikely to be specific to the UK.
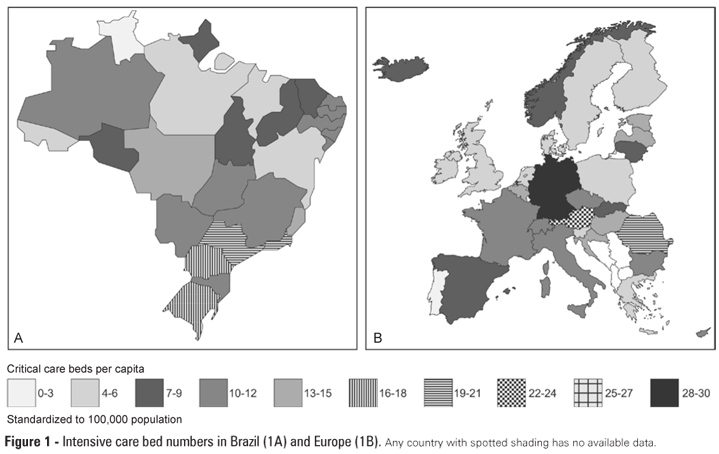
To comprehend this problem, two important pieces of information need to be understood: 1) how many critical care beds are required for a population; and 2) whether the organisation of the current service is optimal for the patient groups being treated. Unfortunately It is difficult to fully understand the numbers of beds required for a given population. Several authors have attempted to look at this problem by comparing practices and provision between various countries to identify differences that may help to answer these questions. In 2008, Wunsch et al. examined intensive care bed provision in several Western countries.(6) They found that some countries possessed markedly more intensive care beds even when corrected for the population size than did other countries; in particular, the USA had almost six times the numbers of beds than did the UK. They also identified relationships between the economic strength of the individual countries, the size of hospitals and the number of intensive care beds provided. They also demonstrated that those countries with restricted numbers of beds seemed to have increased mortality rates in septic patients who were admitted to the intensive care unit. Rhodes et al. recently pursued this path of research, although they focused on all European countries.(5) They demonstrated that there was marked heterogeneity in intensive care provision even within a discrete geographical area, such as Europe. The overall numbers identified were similar to the results of Wunsch, although they identified a number of problems in collating the data, which should in reality be available for each country. The number of intensive care beds varied between 4.2/100,000 inhabitants in Portugal and 29/100,000 in Germany). This difference is too large to be explained by patient characteristics; other explanations are required, such as differences in the way intensive care is provided to different patient groups and the absence of a consistent definition as to what an intensive care bed is. Although everyone agreed as to what a typical intensive care patient was, different countries had different thresholds for defining a hospital bed as an intensive care bed, which was often related to funding mechanisms and professional and specialty-specific political pressures. There must be a standard definition that can be applied to every healthcare setting.
A recent study (EuSOS) published in the Lancet evaluated how surgical patients are admitted to critical care facilities in Europe and how this practice affects the patient outcome.(4) A large observational study of almost 50,000 patients in nearly every European country assessed surgical outcomes to determine how these outcomes related to pre-operative issues and critical care use. Similar to previous studies, the investigators found large discrepancies in the mortality rates among countries after surgery, which persisted despite adjusting for a large number of relevant pre-operative problems. Additionally, they found wide discrepancies in the use of intensive care postoperatively; 70% more elective patients in Germany were admitted to the intensive care unit than in the UK.
Considering the disparate information that has been reported, we propose some interesting questions. Germany has approximately seven times the number of intensive care beds than Portugal.(4,5) They admit more patients to the intensive care unit after elective surgery, and they observe better outcomes for these patients. Is there a causal link between these facts, or is it simply an association? If the relationship is causal, then some important issues must be studied as Portugal might be sub-optimally providing for their population. If there is no link, then perhaps Germany is over providing this expensive resource.
If these differences are to be found within Europe, then what are the implications for other countries? According to the Associação de Medicina Intensiva Brasileira (AMIB) census data from 2010 (www.amib.com.br, accessed 10 November 2012), the numbers of intensive care beds in Brazil are higher than in Europe (13 versus 11.5 per 100,000 people). Brazil, however, is an interesting country; although geographically large, with a large population and a growing economy, Brazil delivers its health care in a more heterogeneous fashion than the European countries; there is a marked difference between the rich and well-populated cities in the south of the country and the poorer regions in the north (Figure 1). Additionally, there are differences between private and public hospitals and the type of health insurance for each patient. These differences in healthcare provision may also directly relate to the differences in access to intensive care and eventually to outcomes of critical illnesses; these differences may explain why the results of intensive care are so heterogeneous and worse than those found in most European countries.(3,10)
What should be changed and what is the role of National and International Societies of Intensive Care Medicine in developing research and education and lobbying governments to change this situation? In addition to serving as healthcare professionals, our role is to advocate and represent our patients.(11) To execute this role efficiently, we must know if the country can afford to expand their critical care provision, and we must understand how the country can deliver this care. These important questions must be answered. When we obtain these answers, then we can plan accordingly and deliver the services that the population rightfully deserves.
REFERENCES
- 1. Angus DC, Kelley MA, Schmitz RJ, White A, Popovich J Jr; Committee on Manpower for Pulmonary and Critical Care Societies (COMPACCS). Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: can we meet the requirements of an aging population? JAMA. 2000;284(21):2762-70.
- 2. Laake JH, Dybwik K, Flaatten HK, Fonneland IL, Kvåle R, Strand K. Impact of the post-World War II generation on intensive care needs in Norway. Acta Anaesthesiol Scand. 2010;54(4):479-84.
- 3. Adhikari NK, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults. Lancet. 2010;376(9749):1339-46.
- 4. Pearse RM, Moreno RP, Bauer P, Pelosi P, Metnitz P, Spies C, Vallet B, Vincent JL, Hoeft A, Rhodes A; European Surgical Outcomes Study (EuSOS) group for the Trials groups of the European Society of Intensive Care Medicine and the European Society of Anaesthesiology. Mortality after surgery in Europe: a 7 day cohort study. Lancet. 2012;380(9847):1059-65.
- 5. Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012;38(10):1647-53.
- 6. Wunsch H, Angus DC, Harrison DA, Collange O, Fowler R, Hoste EA, et al. Variation in critical care services across North America and Western Europe. Crit Care Med. 2008;36(10):2787-93, e1-9.
- 7. Eastman N, Philips B, Rhodes A. Triaging for adult critical care in the event of overwhelming need. Intensive Care Med. 2010;36(6):1076-82.
- 8. Rhodes A, Moreno RP, Azoulay E, Capuzzo M, Chiche JD, Eddleston J, Endacott R, Ferdinande P, Flaatten H, Guidet B, Kuhlen R, León-Gil C, Martin Delgado MC, Metnitz PG, Soares M, Sprung CL, Timsit JF, Valentin A; Task Force on Safety and Quality of European Society of Intensive Care Medicine (ESICM). Prospectively defined indicators to improve the safety and quality of care for critically ill patients: a report from the Task Force on Safety and Quality of the European Society of Intensive Care Medicine (ESICM). Intensive Care Med. 2012;38(4):598-605.
- 9. Pearse RM, Harrison DA, James P, Watson D, Hinds C, Rhodes A, et al. Identification and characterisation of the high-risk surgical population in the United Kingdom. Critical Care. 2006;10(3):R81.
- 10. Vincent JL, Rello J, Marshall J, Silva E, Anzueto A, Martin CD, Moreno R, Lipman J, Gomersall C, Sakr Y, Reinhart K; EPIC II Group of Investigators. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302(21):2323-9.
- 11. Moreno RP, Rhodes A, Chiche JD. The ongoing H1N1 flu pandemic and the intensive care community: challenges, opportunities, and the duties of scientific societies and intensivists. Intensive Care Med. 2009;35(12):2005-8.
Publication Dates
-
Publication in this collection
30 Jan 2013 -
Date of issue
Dec 2012