Abstract
Brazil is a country of continental dimensions with a large heterogeneity of climates and massive mixing of the population. Almost the entire national territory is located between the Equator and the Tropic of Capricorn, and the Earth axial tilt to the south certainly makes Brazil one of the countries of the world with greater extent of land in proximity to the sun. The Brazilian coastline, where most of its population lives, is more than 8,500 km long. Due to geographic characteristics and cultural trends, Brazilians are among the peoples with the highest annual exposure to the sun. Epidemiological data show a continuing increase in the incidence of non-melanoma and melanoma skin cancers. Photoprotection can be understood as a set of measures aimed at reducing sun exposure and at preventing the development of acute and chronic actinic damage. Due to the peculiarities of Brazilian territory and culture, it would not be advisable to replicate the concepts of photoprotection from other developed countries, places with completely different climates and populations. Thus the Brazilian Society of Dermatology has developed the Brazilian Consensus on Photoprotection, the first official document on photoprotection developed in Brazil for Brazilians, with recommendations on matters involving photoprotection.
Dermatology; Protection; Solar radiation; Sun protection factor
CHAPTER I
ELECTROMAGNETIC SPECTRUM AND SOLAR RADIATION INTRODUCTION AND CONCEPTS
Electromagnetic radiations are classified according to the length or frequency of wave propagation. For example, radio waves, microwaves, infrared, visible light, ultraviolet, X rays and gamma rays are names of radiation bands, ordered from the longer to the shorter wavelength. They can also be ordered from the smaller to the larger frequency, since wavelength and frequency are inversely proportional.
Infrared, visible light and ultraviolet radiations comprise almost the total radiation emanating from the sun. According to the International Radiation Commission (CIE, from the French Comission Internacional de l'Eclairage), this set of radiations is called optical radiation.11. Sliney DH; International Commission on Illumination. Radiometric Quantities and Units Used in Photobiology and Photochemistry: Recommendations of the Commission Internationale de l'Eclairage (International Commission on Illumination). Photochem Photobiol. 2007;83:425-32. Only a fraction, less than 1% of solar radiation, does not consist of optical radiation and, therefore, aggregates other bands like microwaves, X rays or gamma rays. Generally, the solar radiation reaching the top of terrestrial atmosphere is basically composed of:
■ Ultraviolet radiation (UVR), characterized by wavelength radiations between 100 and 400 nm**, represents about 10% of total solar radiation reaching the top of the atmosphere, but suffers intensive attenuation until it reaches the surface. UVR is accountable for a series of important photochemical and photobiological reactions;
■ Visible radiation, comprised of wavelengths between 400 and 780 nm, represents 40% of the radiation emanating from the sun and is defined as any radiation able to cause a visual sensation. Compared to other wavelengths, visible radiation undergoes less attenuation when going through the atmosphere of the Earth;
■ Infrared radiation, a wide band with wavelengths longer than 780 nm, represents the remaining 50% of solar radiation. Infrared radiation is strongly absorbed by water vapor and carbon gas present in significant amounts in the atmosphere, being therefore intimately connected with climate changes in the planet.
■ **nm = nanometer. A nanometer is equivalent to one billionth of a meter, that is, 1 nm = 10-9. Another widely used submultiple is one millionth of the meter, called micrometer (µ m = 10-6 m = 1000nm)
It is important to note that these percentages concerning quantities of each radiation band show small variations related to cycles and disturbances of solar activity. In addition, there are no precise limits for the spectral band of visible radiation, since these limits depend on the quantity of radiant energy reaching the retina and the sensitivity of the observer. The lower limit is usually between 360 and 400 nm, while the upper limit is between 760 and 830 nm.
In the specific case of UVR, the terms UVA, UVB and UVC were introduced in 1930 by Committee 41 of CIE because of the different photobiologic effects of these spectral bands.22. International Commission on Illumination [Internet]. CIE 134/1999 TC 6-26 report: Standardization of the Terms UV-A1, UV-A2 and UV-B. [cited 2014 Out 29]. Available from: http://div6.cie.co.at/?i_ca_id=611&pubid=179
http://div6.cie.co.at/?i_ca_id=611&pubid...
Therefore, the UVR was divided into:
■ UV-C, between 100 and 280 nm;
■ UV-B, between 280 and 315 nm; and
■ UV-A, between 315 and 400 nm.
The same limits and designations of these spectral bands are also adopted by the International Organization for Standardization (ISO, 2007). CIE highlights the importance of international standardization, since such bands are widely used in different medical and scientific research fields and, although some investigators use the 320 nm limit for the division of UVA and UVB bands, the norm adopted in 1930 is still the one recommended.
Another very common division found in literature concerns the UVA band, which is divided into two parts: UVA1 (315-340 nm) and UVA2 (340-400 nm). This division is based on recent research that shows different types of photobiologic interaction between such bands and the DNA. Although this division may have some practical value, neither CIE nor ISO recommend the division of UVA radiation into these two sub-bands.22. International Commission on Illumination [Internet]. CIE 134/1999 TC 6-26 report: Standardization of the Terms UV-A1, UV-A2 and UV-B. [cited 2014 Out 29]. Available from: http://div6.cie.co.at/?i_ca_id=611&pubid=179
http://div6.cie.co.at/?i_ca_id=611&pubid...
,33. International Organization for Standardization. ISO 20473: Optics and photonics -Spectral bands; 2007.
Besides the fact that it is the smallest part of solar radiation that reaches the top of the atmosphere, UVR is strongly attenuated by the terrestrial atmosphere and reaches the surface in quantities that are small, but sufficient to provide significant photobiologic effect. UVC is completely absorbed by the oxygen and ozone present in the stratosphere, while UVB radiation undergoes strong absorption by ozone and is intensively scattered by molecules.
Therefore, superficial UVR is mostly composed of UVA radiation that, while also being actively spread by the molecules present in the atmosphere, undergoes smaller ozone absorption. In addition to these, several other environmental factors also interact with UVR, as shown below.
ENVIRONMENTAL FACTORS THAT INFLUENCE ULTRAVIOLET RADIATION
It is important to emphasize that the superficial UVR levels depend on a group of meteorological, geographic and temporal factors. Therefore, we cannot evaluate the influence of each of these environmental factors separately, but only as a group of elements that may depend on and influence each other.
Ozone
Ozone, the main absorber of UVR, is produced for the most part in the terrestrial stratosphere of the equatorial region of the planet. However, due to the transportation mechanisms existing in the high atmosphere, a great part of the produced ozone is transported to higher latitudes. Therefore, the equatorial region of the planet has smaller quantities of ozone than higher latitude regions and the poles.
Ozone layer is the name given to the region with high concentration of this gas in the Earth's atmosphere, located at a height between 15 and 30 km. This layer contains between 80 and 90% of the total ozone in the terrestrial atmosphere and is responsible for the intensive absorption of UVB radiation and part of the extinction of UVC radiation. The rest of the ozone is mostly found in regions close to the terrestrial surface.
During the 1980 decade, scientists observed that the ozone layer was strongly diminished in high latitude regions, especially in the poles. It was found that this drastic reduction, that may reduce by 80 to 90% the total concentration of the gas in the atmosphere, is mainly produced by the free chlorine released by chlorofluorocarbons (CFC), gases created by man and intensively used as manufacturing propellents and refrigerating fluids in the entire planet.
The presence of chlorine (or bromine) in great quantities in the atmosphere unbalances the ozone formation and destruction chain, accelerating its destruction process. With less ozone, there is less absorption of UVR and, therefore, increased presence of superficial radiation. Comparisons of ozone contents measured between 1964-1980 and 2002-2005 show an average decrease of 3.5% in the ozone content of the Earth's atmosphere, more intensively in high latitudes and less representative in the tropics.44. World Meteorological Organization. Scientific Assessment of Ozone Depletion: 2010, Global Ozone Research and Monitoring Project-Report No. 52. Geneva, Switzerland: WHO; 2011. 516 p.
With the objective of slowing down this process of ozone destruction, in 1987 the Montreal Protocol (http://www.protocolodemontreal.org.br/) was established to forbid the production and consumption of CFCs and other gases that destroy the ozone layer. Adhesion of the nations to the Protocol was massive and the elimination of CFC consumption has allowed a recovery of ozone levels in the entire planet. It is foreseen that by the middle of this century the ozone layer will be completely recovered to levels existing prior to production of CFCs.55. Bais AF, Tourpali K, Kazantzidis A, Akiyoshi H, Bekki S, Braesicke P, et al. Projections of UV radiation changes in the 21st century: impact of ozone recovery and cloud effects Atmos. Chem Phys. 2001;11:7533-45. A study by UK Chemistry and Aerosols shows that the Montreal Protocol will prevent the onset of two million new skin cancer cases until the year 2030.66. van Dijk A, Slaper H, den Outer PN, Morgenstern O, Braesicke P, Pyle JA, et al. Skin Cancer Risks Avoided by the Montreal Protocol -Worldwide Modeling Integrating Coupled Climate-Chemistry Models with a Risk Model for UV. Photochem Photobiol. 2013;89:234-46.
Altitude
The higher the altitude of a location, the thinner is the atmosphere above it and, consequently, the larger the quantity of UVR reaching the surface. In situations of clear and cloudless skies, the UVR flux may increase between 5 and 10% for each 1000 m altitude. Nevertheless, this altitude-related increase in URV may vary to values close to 20% per kilometer, as it depends on a series of other factors, such as the quantity of ozone in the lower layers of the atmosphere, the type of surface that reflects UV radiation, the particulates present in the atmosphere and even the position of the sun.77. Pfeifer MT, P. Koepke, Reuder J. Effects of altitude and aerosol on UV radiation. J Geophys Res. 2006:111;D01203.
The time of day and the season of the year
In a clear sky situation, the "higher" the Sun is in the sky, the higher the levels of UV radiation are. This means that the farther the Sun is from the horizon, the shorter the optical pathway the radiation has to cross in the atmosphere. Under these conditions, UVR undergoes less interaction with gases and particulates and, consequently, is less attenuated. Therefore, at times close to solar noon, UVR reaches its highest daytime values.
The same reasoning may be used to evaluate the variation of UVR fluxes in relation to the season of the year. In the summer, the Sun reaches higher positions in relation to the horizon than in the winter and, consequently, the UVR flux is more intense. The differences between the seasons of the year become more relevant as the latitude becomes higher. That is, in the tropics there is little difference between the position of the Sun in the summer and in the winter, while in higher latitudes this difference is quite significant.
Clouds
The UVR levels in clear sky days, that is, when there are no clouds, are usually higher. However, the presence of clouds tends to attenuate UVR and diminish the quantity of surface radiation. Nevertheless, the attenuance levels may vary considerably and the clouds do not always exert adequate protection against UVR. Deep and dark clouds, as seen in rainstorms, may almost totally attenuate UVR fluxes, but thinner and lighter clouds can attenuate them only partially.
Due to this great variability, it is not possible to provide a parameter or an UVR attenuation percentage for nebulosity. There are even particular situations when the presence of cumulus or cirrus clouds may trigger a UVR intensification phenomenon and, for a short period of time, make UVR fluxes superior to those that would be observed on a clear sky day.
Aerosols
Solid or liquid particles found in the atmosphere are called aerosols. Soot emitted by automobiles, motorcycles and trucks or burning biomass, suspended soil dust or even sea salt from evaporated ocean water are examples of atmospheric aerosols. These particles interact with UVR, most often reflecting the radiation to other directions. However, some types of aerosols are also able to absorb part of the incident UVR.
Thus, polluted environments or those with suspended dust may show UVR attenuation in relation to clear sky situations. Some studies demonstrate that polluted locations, such as São Paulo(SP)88. Corrêa MP, Plana-Fattori A. Uma análise das variações do índice ultravioleta em relação às observações de conteúdo de ozônio e da espessura óptica dos aerossóis sobre a cidade de São Paulo. Rev Bras Meteorol. 2006;21:24-32. or Mexico City,99. Acosta LR and Evans WFJ. Design of the Mexico City UV monitoring network: UVB measurements at ground level in the urban environment. J Geophys Res. 2000;105:5017-26. may present situations with around 20% of the incident UVR. Nevertheless, such decrease of UVR is observed in periods of intense pollution and aerosols should not be considered as protective agents concerning sun exposure.
Surface reflection (albedo)
The term 'albedo' is used to express the relationship between the radiation reflected by a surface and the radiation such surface receives from the Sun. Therefore, UVR is reflected in different ways, depending on the surface it incides on. This is the reason why albedo may be a determining factor in the evaluation of the quantity of radiation reaching an individual. Very light colored surfaces, such as freshly fallen snow, may reflect up to 90% of the incident radiation; therefore, wearing adequate protection for the eyes and skin is required in environments like mountains and ski tracks.
As regards the environments typically observed in Brazil, the urban and blacktop paved areas generally present 3 to 5% albedo. Sand has albedo variable between 2 and 12%, depending on sand type and humidity. Grassy surfaces present low albedo, around 1 to 4%, but light colored concrete may reflect between 10 and 20% of the UV radiation.1010. Corrêa MP, Ceballos JC. UVB surface albedo measurements using biometers. Rev Bras Geof. 2008;26:411-6.
ULTRAVIOLET INDEX (UVI)
The ultraviolet index (UVI) is a scale of values recommended by WHO (World Health Organization), related to the intensity of UV radiation that induces the onset of erythema in human skin.1111. Unep.org [Internet]. Global solar UV Index: A Practical Guide. A joint recommendation of the World Health Organization,World Meteorological Organization, United Nations Environment Programme, and the International Commission on Non-Ionizing Radiation Protection. Geneva: WHO; 2002. 28 p. [Cited 2014 30 Oct]. Available from: http://www.unep.org/pdf/solar_Index_Guide.pdf.
http://www.unep.org/pdf/solar_Index_Guid...
This scale has the purpose of simplifying information of UVR levels to the lay public according to a table of whole values, where zero is the smallest value while the largest value is usually represented by the symbol 11+. However, it is important to emphasize that there is no upper limit. The higher the value, the greater is the potential of solar damage to skin and eyes.
The variables that influence the calculation or measurement of UVI are those introduced in the previous subchapter. That is, the total ozone content of the atmosphere is taken into account, as well as the geographic position of the location (the closer it is to the Equator line, the higher the UVI); the altitude of the surface (at high altitudes, higher UVI are observed); the time of day (most of the UVR reaches the surface at times close to solar noon); season of the year (the UVI escalates in the summer and diminishes in the winter); atmospheric conditions (the UVI are generally higher in days of cloudless skies); and type of surface.
The use of this scale is an important tool to orient the population regarding the risks of excessive solar exposure. It is especially useful for those groups that are more vulnerable to the damaging effects of UVR, like people with low phototypes (I and II), children, the elderly and tourists, people with history of great cumulative solar exposure and/or skin cancer, etc.
The UVI scale and WHO general recommendations for photoprotection are shown in figure 1.
The category designated "low UVI" usually happens at times close to dawn and sunset, in addition to moments when a great mass of dense clouds covers the sky. However, it is always very important to be extremely careful in evaluating UVI when there are clouds, since nebulosity may not significantly attenuate UVR or even intensify radiation levels in short periods of time. It should be remembered that WHO recommends sun protection measures when UVI values are over 3.
ULTRAVIOLET RADIATION EMMITED BY LAMPS AND ARTIFICIAL SOURCES
Ever since the second half of last century, studies about the UVR emitted by artificial sources have been carried out to clarify the relationship between the use of fluorescent lamps and the incidence of cutaneous melanoma. Such studies reflect the concern about the possibility of increased risk of incidence of skin cancer, melanoma and non melanoma, in individuals exposed to UVR emitted by these lamps.
In 1988, for example, Swerdlow et al. already pointed to a connection between skin cancer and exposure to indoor tanning methods.1212. Swerdlow AJ, English JS, MacKie RM, O'Doherty CJ, Hunter JA, Clark J, et al. Fluorescent lights, ultraviolet lamps, and risk of cutaneous melanoma. BMJ. 1988;297:647-50. Nevertheless, a short time before, in 1985, English et al. showed that there is no connection between the incidence of melanomas and exposure to fluorescent lamps regularly used at home and in the office.1313. English DR, Rouse IL, Xu Z, Watt JD, Holman CD, Heenan PJ, et al. Cutaneous malignant melanoma and fluorescent lighting. J Natl Cancer Inst. 1985;74:1191-7. In 1990, Diffey indicated the main situations of UV radiation risk derived from artificial sources: artificial tanning chambers, medical and dental phototherapy, industrial photoprocesses, sterilization and disinfection, laboratory investigation, insect traps and lighting for environments in general.1414. Diffey BL. Human exposure to ultraviolet radiation. Semin Dermatol. 1990;9:2-10.
The types of lamps found in the market are halogen quartz lamps, incandescent lamps with a tungsten filament, tube fluorescent and compact fluorescent lamps. In all of the continents, discussions regarding the rational use of energy are increasingly frequent subjects and a priority in government agendas. In this scenario, incandescent lamps with a tungsten filament are being replaced by compact fluorescent lamps due to their low energy consumption, both for domestic and commercial use.1515. Eadie E, Ferguson J, Moseley H. A preliminary investigation into the effect of exposure of photosensitive individuals to light from compact fluorescent lamps. Br J Dermatol. 2009;160:659-64.
Few papers have been published related to UVR emission by artificial lighting sources. The quantities of UVA and UVB emitted by commonly used lamps are very small and totally blocked by the protective membrane currently included in the glass casing of lamps. Thus, there are no reports about UVR emission by the lamps found on the market.1616. Sayre RM, Dowdy JC, Poh-Fitzpatrick M. Dermatological risk of indoor ultraviolet exposure from contemporary lighting sources. Photochem Photobiol. 2004;80:47-51.,1717. Klein RS, Werth VP, Dowdy JC, Sayre RM. Analysus of compact fluorescent lights for use by patients with phtosensitive conditions. Photochem Photobiol. 2009;85:1004-10.
Although they do not emit UV radiation, the lamps are visible light emitting sources and present variations within the electromagnetic spectrum that may affect individuals with other skin diseases, such as melasma, for example, depending on exposure intensity and frequency.1818. Sklar LR, Almutawa F, Lim HW, Hamzavi I. Lim and Iltefat Hamzavi. Effects of ultraviolet radiation, visible light, and infrared radiation on erythema and pigmentation: a review. Photochem Photobiol Sci. 2013;12:54-64. At any rate, it is important to emphasize that there is no relationship between exposure to common artificial lamps at home and in the office and skin cancer.
CHARACTERISTICS OF SOLAR RADIATION IN BRAZIL
A significant set of data collected in the last few years in several regions of Brazil allows us to trace the behavior of ultraviolet solar radiation in Brazilian soil more accurately. We will see that these data show a great need to better educate our population regarding the risks of solar exposure without adequate protection.
In Brazil, there is generous offer of ultraviolet radiation. UVR roughly presents higher values for smaller geographic latitudes, but other factors like altitude, season of the year, time of day and meteorologic characteristics such as presence of clouds and atmospheric pollution also influence the intensity of solar radiation. Despite these variations, UVR levels in clear sky conditions are always very high in every season of the year and in almost the entire Brazilian territory.1919. de Paula Corrêa M, Ceballos JC. solar Ultraviolet Radiation Measurements in One of the Most Populous Cities of the World: Aspects Related to Skin Cancer Cases and Vitamin D Availability. Photochem Photobiol. 2010;86:438-44.
Taking into account geographic position, the North and Northeast regions present the highest cumulative doses of ultraviolet radiation. This means that, in those regions, UVR levels are high and vary little during the entire year. On the other hand, in the South and Southeast regions the effect of the seasons of the year is quite perceptible, so that UVR levels show great variability between winter and summer.2020. de Paula Corrêa M, Pires LC. Doses of erythemal ultraviolet radiation observed in Brazil. Int J Dermatol. 2013;52:966-73.
It is important to highlight the fact that, in the summer, the Southeast region presents record UVR intensity observed in the country, with levels even higher than in the Northeast region. This occurs due to the geographic position of the Brazilian Southeast region. The city of São Paulo (SP), for example, is at 23º latitude south and this angle coincides with the angle of inclination of the planet in relation to the sun. Therefore, in the summer, the sun reaches its highest point at noon and, consequently, in a clear sky day, UVR levels are more intense.
The UV radiation distribution here presented considered only the geographic positions of Brazilian regions. However, it is important to take into account also the meteorologic factors, such as the occurrence of rainy seasons, with the presence of deep clouds that significantly attenuate UV radiation. The Central region of Brazil, for example, may receive great incidence of solar radiation during the dry seasons (autumn and winter), as there is less rainfall and an even larger number of clear sky days.
This daytime UVR variability due to the presence or absence of clouds influences the cumulative radiation dose to which an individual is exposed. According to WHO, the recommended daily dose of UV radiation a person should be exposed to is 108 J/m2. UVR readings collected in São Paulo (SP), Ilhéus (BA) and Itajubá (MG) between 2005 and 2009, demonstrated that the daily means of UV radiation are similar, around 3300 and 3800 J/m2, with smaller variation in value amplitude in the Northeast when compared to the Southeast region. In the summer, the daily means are still larger and may reach values over 7000 J/m2. It is a reason for concern to observe that, even in the winter, a person exposed without protection in the period between 8:00 a.m. and 5:00 p.m., may receive a UVR dose higher than recommended. This is a reality for many Brazilian workers.2020. de Paula Corrêa M, Pires LC. Doses of erythemal ultraviolet radiation observed in Brazil. Int J Dermatol. 2013;52:966-73.
In our country, the cultural trend of solar exposure on beaches is still very popular. Most of the tourists visit Brazilian beaches in the period of greater incidence of UVR, being subject to large UVR quantities and their related hazards. An experiment carried out at the Ponta Negra beach, in Natal (RN), is a clear example of the high UV radiation levels to which an individual may be exposed. In readings taken in the morning, the cumulative dose registered between 9:40 a.m. and noon was 5250 J/m2, that is, over 50 times the maximum daily dose recommended by WHO and almost 12 times the necessary dose to trigger erythema in an individual of phototype IV.2020. de Paula Corrêa M, Pires LC. Doses of erythemal ultraviolet radiation observed in Brazil. Int J Dermatol. 2013;52:966-73. However, it is important to point out that this kind of dose is not observed only at seaside resorts, but also in urban centers.
Awareness of this UVR incidence pattern, as well as the cumulative daily dose Brazilians are apt to receive, are fundamental tools to define skin care policies.
In Brazil, the UVI observed in cloudless days and at solar noon is frequently found at extreme levels during the summer in all of the country. In winter, the North and Northeast regions may present UVI at these same extreme levels, while in the South and Southeast mean UVI levels may be observed.1919. de Paula Corrêa M, Ceballos JC. solar Ultraviolet Radiation Measurements in One of the Most Populous Cities of the World: Aspects Related to Skin Cancer Cases and Vitamin D Availability. Photochem Photobiol. 2010;86:438-44.,2121. Corrêa MP. (Medidas de radiação UV na praia de Ponta Negra, Natal/RN realizadas em 13 de março de 2011). Comunicação pessoal.
22. Silva A. Medidas de radiação solar ultravioleta em Belo Horizonte e saúde pública. Rev Bras Geof. 2008;26:417-25.-2323. Silva A, Kirchhoff VWJH, Echer E, Leme NP. Variação Sazonal da Radiação Ultravioleta solar Biologicamente Ativa. Rev Bras Geof 2000;18:64-74. Figure 2 shows the distribution of maximum UVI in the country on a day in August 2013. Daily UVI data are available at the site of the Center for Weather Forecast and Climatic Studies of the National Institute for Space Research.2424. Cptec.inpe.br [Internet]. Instituto Nacional de Pesquisas espaciais (INPE). Centro de previsão de tempo e estudos climáticos. [acesso 30 out 2014]. Disponível em: http://www.cptec.inpe.br/
http://www.cptec.inpe.br/...
Satellites and Environmental Systems Division – Center for Weather Forecasts and Climate Studies of the National Institute for Space Research. Available at: http://satelite.cptec.inpe.br/uv/
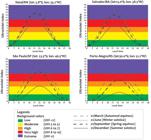
Figure 3 presents mean ultraviolet index values for clear sky conditions (without clouds) on solstice and equinox days, in four Brazilian locations.2525. Madronich, S., Implications of recent total atmospheric ozone measurements for biologically active ultraviolet radiation reaching the Earth's surfasse. Geophys Res Lett. 1992;19:37-40.
Ultraviolet index (UVI) for clear sky conditions (without clouds) on solstice and equinox days in four Brazilian locations. Calculations carried out with the radiation transference model NCAR/ACD TUV: Tropospheric Ultraviolet & Visible Radiation Model 25, with mean data on total ozone content between the years 2004 and 2012 informed by GES-DISC/NASA (sensor OMI - Ozone Monitoring Instrument)
It is important to point out some elements in figure 3. In the summer (solid line), UVI values on clear sky days reach extreme values in all of the regions in the country. In the spring and fall such values may also be reached, mainly in the North and Northeast regions, and even in the Southeast region. Even when such figures present particular situations of cloudless and clear sky, these values are commonly observed and recorded in the literature. In addition, times usually recommended for sun exposure (before 10:00 a.m. and after 4:00 p.m.) may also present high and very high UVI values and, consequently, cause damage to the skin and eyes.
Excessive sun exposure and ignorance of these data by the greater part of the population have been considered the main factors in the increasing incidence of skin cancer.2626. Brasil. Ministério da Saúde. Instituto Nacional de Câncer (INCA). Coordenação de Prevenção e Vigilância de Câncer. Estimativas 2010: Incidência de Câncer no Brasil. Rio de Janeiro: INCA, 2009. 98 p. Encouraging the population to take the necessary precautions based on conscious sun exposure may reduce the undesirable consequences of this practice.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION
-
Research on solar radiation characteristics in Brazil should be encouraged to better understand the sun exposure peculiarities faced by Brazilians, producing public photoprotection policies adapted to our reality.
-
The Ultraviolet Index should be better divulged to the Brazilian population, by means of printed and electronic communication media, as a form of orientation regarding daily photoprotection, suggesting the use of photoprotective measures that meet the specific conditions of that location and on that specific day.
-
The dermatologists and the scientific community should be aware of the solar radiation peculiarities in Brazil, avoiding the automatic incorporation of concepts originated in countries that have climates distinct from ours.
-
SBD (Sociedade Brasileira de Dermatologia) agrees that the use of tanning chambers for esthetic purposes should be forbidden in Brazil.
-
However, the use of artificial radiation for the treatment of some skin diseases should be permitted, under the guidance of the dermatologist in charge.
CHAPTER 2
EFFECTS OF SOLAR RADIATION ON THE SKIN (ULTRAVIOLET RADIATION, VISIBLE LIGHT AND INFRARED RADIATION)
INTRODUCTION
The reactions caused by sunlight on the skin are many and may be both positive and negative. They depend, among other factors, on radiation intensity and wavelength, as well as on the type of skin of each individual. Moreover, it is a known fact that the dose of energy depends on the time of exposure, the proximity to the sun and radiation wavelength (the longer it is, the greater the penetration of light in the skin).
The effects of ultraviolet radiation (UVR) on the skin may be considered immediate (acute) and delayed (chronic). The immediate ones are erythema, increased skin temperature, skin thickening, immediate pigmentation, persistent pigmentation, delayed tanning and vitamin D production,2727. Hönigsmann H. Erythema and pigmentation. Photodermatol Photoimmunol Photomed. 2002;18:75-81.,2828. Suh KS, Roh HJ, Choi SY, Jeon YS, Doh KS, Bae JH, et al. A long-term evaluation of erythema and pigmentation induced by ultraviolet radiations of different wavelengths. Skin Res Technol. 2007;13:360-8. while the delayed ones are photoaging and skin cancer.2929. Matsumura Y, Ananthaswamy HN. Short-term and long-term cellular and molecular events following UV irradiation of skin: implications for molecular medicine. Expert Rev Mol Med. 2002;4:1-22.
30. Svobodova A, Walterova D, Vostalova J. Ultraviolet light induced alteration to the skin. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2006;150:25-38.-3131. Katiyar SK. UV-induced immune suppression and photocarcinogenesis: chemoprevention by dietary botanical agents. Cancer Lett. 2007;255:1-11. In addition, visible light (VL, 400-780 nm) and infrared radiation (IR, 780 - 1 mm) also exert both acute and chronic effects over the skin, which have also been intensively studied.3232. Sklar LR, Almutawa F, Lim HW, Hamzavi I. Effects of ultraviolet radiation, visible light, and infrared radiation on erythema and pigmentation: a review. Photochem Photobiol Sci. 2013;12:54-64.
FACTORS THAT INFLUENCE ULTRAVIOLET RADIATION EFFECTS ON THE SKIN
The classification proposed by Fitzpatrick for skin types (Chart 1) is a numerical scheme used to describe skin response to sunlight.3333. Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-71. It meets the purpose of evaluation of erythema and pigmentation formation secondary to UV radiation exposure, but it is not fully adequate for the evaluation of a mixed race population. In this sense, currently different authors report that the classification proposed by Fitzpatrick is not exactly related to the color of the skin in those of non-Caucasian origin, particularly the Hispanic and Asian populations. A study carried out with a small Brazilian population group3434. Schalka S, dos Reis VM, Cucé LC. The influence of the amount of sunscreen applied and its sun protection factor (SPF): evaluation of two sunscreens including the same ingredients at different concentrations. Photodermatol Photoimmunol Photomed. 2009;25:175-80. demonstrated that the erythematogenic response of this population differed from Fitzpatrick's classification.
In spite of this, this classification is still used, since there is no other that is more apropriate. Phototypes I and II burn more easily than tan. Thus, individuals with these types of skin have an increased incidence of skin cancer when compared to those with higher phototypes, who tan more easily than burn. The reason for this may be explained by the finding that skins that are more melanocompetent have reduced UVR penetration and faster DNA repair rates, when compared to lighter skins.3535. Sheehan JM, Cragg N, Chadwick CA, Potten CS, Young AR. Repeated ultraviolet exposure affords the same protection against DNA photodamage and erythema in human skin types II and IV but is associated with faster DNA repair in skin type IV. J Invest Dermatol. 2002;118:825-9.
Another important observation is that UVR penetration also varies according to the irradiated part of the body, due to the different thicknesses of the corneal layer, as well as of the entire epidermis, in different body areas. In this sense, there is greater penetration in areas where the epidermis is thinner.2727. Hönigsmann H. Erythema and pigmentation. Photodermatol Photoimmunol Photomed. 2002;18:75-81.,2828. Suh KS, Roh HJ, Choi SY, Jeon YS, Doh KS, Bae JH, et al. A long-term evaluation of erythema and pigmentation induced by ultraviolet radiations of different wavelengths. Skin Res Technol. 2007;13:360-8.,3636. Waterston K, Naysmith L, Rees JL. Variation in skin thickness may explain some of the within-person variation in ultraviolet radiation-induced erythema at different body sites. J Invest Dermatol. 2005;124:1078. Furthermore, other factors are important when the effects of UVR and VL on the skin are evaluated, such as age, gender, degree of hydration, UVR or VL dose (variable according to the time of day), latitude, reflection rate of environmental surface (for example, sand versus snow), temperature and the use of photosensitizing medications.2727. Hönigsmann H. Erythema and pigmentation. Photodermatol Photoimmunol Photomed. 2002;18:75-81.,3737. Broekmans WM, Vink AA, Boelsma E, Klöpping-Ketelaars WA, Tijburg LB, van't Veer P, et al. Determinants of skin sensitivity to solar irradiation. Eur J Clin Nutr. 2003;57:1222-9.
Erythema
It is an acute reaction, accompanied by edema, local burning sensation and, in more intense cases, onset of vesicles and blisters. The light skinned individuals react more intensively than those who are dark skinned.
The erythema begins after a latency period of 2 to 7 hours, when the skin is exposed to a single and intense radiation dose, which persists for hours or days. The maximum intensity of erythema occurs in around 12-24 hours, then declines. An increased radiation dose diminishes the threshold period and increases the persistence of the erythematous reaction.2727. Hönigsmann H. Erythema and pigmentation. Photodermatol Photoimmunol Photomed. 2002;18:75-81.,3232. Sklar LR, Almutawa F, Lim HW, Hamzavi I. Effects of ultraviolet radiation, visible light, and infrared radiation on erythema and pigmentation: a review. Photochem Photobiol Sci. 2013;12:54-64.
Sunburn is an acute inflammatory reaction characterized, at first, by vascular dilation, increased vascular permeability and migration of polymorphonuclear leukocytes. The main factor responsible for this is UVB (280-315 nm), with smaller participation of UVA (315-400 nm). As a result of UVB action, vascular dilation substances are formed, particularly prostaglandins, determining the threshold period, which may be partly delayed by drugs that inhibit prostaglandin synthesis, such as acetylsalicylic acid and indomethacin.
UVA and infrared (IR) radiation exert their action directly over the vessels of the dermis, determining vascular dilation and erythema, without interference of mediators. The erythema appears later and may become gradually more intense. The action of UVR on epidermal cells is over the DNA, where it is absorbed mainly by pyrimidines, with DNA chain break. Later on there is repair by enzymatic mechanisms such as repair by excision, photoreactivation and recombination. Accompanying the immediate erythema caused by intense sun exposure, the body temperature rises and is followed by sudoresis for regulation by IR action. If the radiation is very intense, sunstroke may occur.2727. Hönigsmann H. Erythema and pigmentation. Photodermatol Photoimmunol Photomed. 2002;18:75-81.,3030. Svobodova A, Walterova D, Vostalova J. Ultraviolet light induced alteration to the skin. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2006;150:25-38.,3232. Sklar LR, Almutawa F, Lim HW, Hamzavi I. Effects of ultraviolet radiation, visible light, and infrared radiation on erythema and pigmentation: a review. Photochem Photobiol Sci. 2013;12:54-64.
Sunstroke
It is a group of symptoms that may occur after intense exposure to sunlight, resulting in excessive escalation of body temperature, which could be fatal. Usually the body is cooled by sweat, but in some situations this mechanism is not sufficient. In these cases, the body temperature of an individual may rise rapidly and damage vital organs.
There are environmental variations that also interfere in the ability of the body to cool itself in high temperature environments, such as, for example, the presence of increased air humidity. In addition, other factors interfere in the body temperature regulation ability, such as age (it is smaller in children and the elderly), obesity, fever and dehydration.
The main sunstroke symptoms are: abnormally high body temperature, erythematous skin, tachycardia, cephalea, dyspnea, vertigo, nausea, vomit, dehydration, confusion and loss of consciousness.3838. Becker JA, Stewart LK. Heat-related illness. Am Fam Physician. 2011;83:1325-30.
39. Glazer JL. Management of heatstroke and heat exhaustion. Am Fam Physician. 2005;71:2133-40.-4040. Wexler RK. Evaluation and treatment of heat-related illnesses. Am Fam Physician. 2002;65:2307-14.
Pigmentation
Pigmentation, which should be differentiated from delayed tanning (DT), presents a biphasic response. Immediate pigment darkening (IPD) occurs in minutes of exposure to UVA and VL, and may last up to two hours. IPD is followed by Persistent Pigment Darkening (PPD), with a peak in two hours that may last for 24 hours. DT occurs between three and five days after sun exposure, may persist for several weeks and even for months.2727. Hönigsmann H. Erythema and pigmentation. Photodermatol Photoimmunol Photomed. 2002;18:75-81.,3232. Sklar LR, Almutawa F, Lim HW, Hamzavi I. Effects of ultraviolet radiation, visible light, and infrared radiation on erythema and pigmentation: a review. Photochem Photobiol Sci. 2013;12:54-64.
IPD and PPD are derived from the Meirowsky phenomenon, where photo-oxidation of melanin previously formed in the melanosomes takes place, as well as its transference from the melanocytes to the keratinocytes. They depend on UVA and also on VL.2727. Hönigsmann H. Erythema and pigmentation. Photodermatol Photoimmunol Photomed. 2002;18:75-81.
Differently from IPD and PPD, DT happens because there is an increase in melanin production by the melanocytes, which have had their number, size and activity increased. DT may disappear in months or years, in accordance with individual characteristics. DT depends on UVB, as well as on UVA and VL.2727. Hönigsmann H. Erythema and pigmentation. Photodermatol Photoimmunol Photomed. 2002;18:75-81.
The ability to acquire pigmentation (IPD, PPD and DT) is influenced by genetic factors and is stronger in darker skins.2727. Hönigsmann H. Erythema and pigmentation. Photodermatol Photoimmunol Photomed. 2002;18:75-81.,3232. Sklar LR, Almutawa F, Lim HW, Hamzavi I. Effects of ultraviolet radiation, visible light, and infrared radiation on erythema and pigmentation: a review. Photochem Photobiol Sci. 2013;12:54-64.
Photoimmunosuppression
The immunosuppression caused by UVR has been more frequently described since 1970, when Kripke demonstrated the absence of tumor rejection by mice previously irradiated with UVR.4141. D'Orazio J, Jarrett S, Amaro-Ortiz A, Scott T. UV Radiation and the Skin. Int J Mol Sci. 2013;14:12222-48.
Furthermore, UVR causes suppression of the immune response of the skin to several antigens, like microorganisms, protein complexes or even haptens. Information on UVR action over immune response is obtained mainly by means of studies with animals.
Immunosuppression caused by UVR may affect the skin, internal organs, lymphatic and blood tissues. The immune function may be diminished, depending on UVR wavelength, on UVB, UVA2 (315 - 340 nm) and UVA1(340 - 400 nm), energy dose (erythematous or suberythematous), frequency of URV exposure and area of irradiation.
UVB alters Langerhans cells in number, morphology and their main function, which is antigen presentation. These alterations have also been described regarding exposure to UVA.
Immunosupression by UVR is mainly modulated by IL-1β, TNF-α, IL-10 and IL-12. The modification in antigen presentation by Langerhans cells, particularly influenced by IL-10, activates Th2 lymphocytes, to the detriment of Th1. This unbalance leads to more IL-10 and IL-4 production.4242. Dumay O, Karam A, Vian L, Moyal D, Hourseau C, Stoebner P, et al. Ultraviolet AI exposure of human skin results in Langerhans cell depletion and reduction of epidermal antigen-presenting cell function: partial protection by a broad-spectrum sunscreen. Br J Dermatol. 2001;144:1161-8. IL-12 seems to have the tendency to neutralize IL-10 action, inhibiting UVR-induced immunosuppression.
Immunosuppression or tolerance induced by UVR seems to be conducted by suppressor/regulatory cells, particularly CD4+ CD25+ and Tr-1.4343. Schwarz A, Beissert S, Grosse-Heitmeyer K, Gunzer M, Bluestone JA, Grabbe S, et al. Evidence for functional relevance of CTLA-4 in ultraviolet-radiation-induced tolerance. J Immunol. 2000;165:1824-31.
It is believed that the urocanic acid, undergoing photoisomerization from the form trans to the form cis when exposed to UVR, may increase IL-10 production, becoming, therefore, a photoimmunosuppression agent.
The immunosuppression triggered by UVR leads to alterations of cell response to allergenic and infectious antigens, while allowing the promotion of skin carcinogenesis, which turns UVR into a complete carcinogen (induction/promotion).4141. D'Orazio J, Jarrett S, Amaro-Ortiz A, Scott T. UV Radiation and the Skin. Int J Mol Sci. 2013;14:12222-48.
Photoaging
Skin aging involves intrinsic and extrinsic factors. Intrinsic or chronologic aging is defined as a set of clinical, histological and physiological alterations that take place in the skin non exposed to the sun. Clinically, the skin is atrophic and shows loss of elasticity. The epidermis becomes thinner and the dermoepidermal junction is straightened and flattened, becoming more fragile.4444. Khavkin J, Ellis DA. Aging skin: histology, physiology, and pathology. Facial Plast Surg Clin North Am. 2011;19:229-34. The tissue reparation process becomes slower, due to diminution of fibroblast metabolism. There is less capacity for proliferation of keratinocytes and fibroblasts, due to smaller response to growth factors. There is also diminution of vitamin D3 synthesis, caused by smaller production of 7-dehydrocholesterol in the altered epidermis.4545. Quan T, He T, Kang S, Voorhees JJ, Fisher GJ. solar ultraviolet irradiation reduces collagen in photoaged human skin by blocking transforming growth factor-beta type II receptor/Smad signaling. Am J Pathol. 2004;165:741-51.
Extrinsic aging or photoaging consists in the development of deep wrinkles, skin thickening, dilation of blood vessels and onset of multiple pigmented lesions in photoexposed areas. It is the outcome of a combination of damage caused by UV radiation associated with intrinsic alterations.3232. Sklar LR, Almutawa F, Lim HW, Hamzavi I. Effects of ultraviolet radiation, visible light, and infrared radiation on erythema and pigmentation: a review. Photochem Photobiol Sci. 2013;12:54-64. Within the cells, protein codes are stored in the nuclei and mitochondria. Mitochondria are organelles producing adenosine triphosphate (A TP), an energetic molecule. The reactive oxygen species (ROS) are products of this process and may damage lipids, proteins and the DNA itself.4646. Ray AJ, Turner R, Nikaido O, Rees JL, Birch-Machin MA. The spectrum of mitochondrial DNA deletions is a ubiquitous marker of ultraviolet radiation exposure in human skin. J Invest Dermatol. 2000;115:674-9.
Mitochondrial DNA presents a high mutation rate, due to its deficiency in histones, low repair capacity and proximity to ROS. This unbalance between the oxidative stress and the enzymes that eliminate free radicals has been held responsible as one of the causes of mitochondrial damage.4747. Koch H, Wittern KP, Bergemann J. In human keratinocytes the Common Deletion reflects donor variabilities rather than chronologic aging and can be induced by ultraviolet A irradiation. J Invest Dermatol. 2001;117:892-7. Mutations in mitochondrial DNA are observed in larger quantity in photoexposed skin, when compared to photoprotected skin, and apparently UVA is the most involved. As a consequence of this process, skin aging takes place.4848. Berneburg M, Plettenberg H, Medve-König K, Pfahlberg A, Gers-Barlag H, Gefeller O, et al. Induction of the photoaging-associated mitochondrial common deletion in vivo in normal human skin J Invest Dermatol. 2004;122:1277-83.
Skin that is little or not photoexposed undergoes a continuous remodeling of dermal collagen. The enzymes responsible for degradation and remodeling of collagen fibers are known as metalloproteinases (MMPs) of the extracellular matrix and are produced by fibroblasts, keratinocytes, macrophages, mastocytes, endothelial cells and eosinophils.3030. Svobodova A, Walterova D, Vostalova J. Ultraviolet light induced alteration to the skin. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2006;150:25-38. In photoaging, there is increased synthesis of metalloproteinases, with more collagen breakdown and degradation. This process is stimulated by biochemical pathways through UVR action, with release of several interleukins (IL) and growth factor receptors, such as the epidermal growth factor receptor (EGFR), tumor necrosis factor α (TNF-α), platelet activation factor (PAF), IL-1 and insulin. The accumulation of ROS stimulates the κβ nuclear factor (NF-κβ), which in turn stimulates production of IL-1, IL-5 and TNF-α, generating an inflammatory process in the photoexposed skin and, consequently, more ROS production.4545. Quan T, He T, Kang S, Voorhees JJ, Fisher GJ. solar ultraviolet irradiation reduces collagen in photoaged human skin by blocking transforming growth factor-beta type II receptor/Smad signaling. Am J Pathol. 2004;165:741-51.,4949. Rittié L, Fisher GJ. UV-light-induced signal cascades and skin aging. Ageing Res Rev. 2002;1:705-20.
The UV radiation is able to activate EGFR by means of its phosphorilation. After this event, GTP (guanosine 5'-triphosphate) binding proteins are activated, stimulating MAP kinase cascades (MAPKs). These kinases stimulate transcription of protein activating pathway - 1 (AP-1). The transcription of several MMP families is regulated by the AP-1 complex, formed after UVR. Thus begins the role of MMPs in the degradation of extracellular matrix proteins.4949. Rittié L, Fisher GJ. UV-light-induced signal cascades and skin aging. Ageing Res Rev. 2002;1:705-20.
Profibrotic cytokine TGF-β regulates multiple cellular functions, including differentiation, proliferation and synthesis of the main extracellular matrix proteins, that is, collagen and elastin. In human skin, TGF-β inhibits proliferation of keratinocytes and stimulates fibroblasts. It also inhibits production of some MMPs, thus preventing collagen breakdown. However, UVR is able to inhibit the TGF-β pathway, resulting in decrease of pro-collagen I and increase of MMP synthesis, leading to progressive degradation of collagen fibers.4545. Quan T, He T, Kang S, Voorhees JJ, Fisher GJ. solar ultraviolet irradiation reduces collagen in photoaged human skin by blocking transforming growth factor-beta type II receptor/Smad signaling. Am J Pathol. 2004;165:741-51.,5050. Massagué J. How cells read TGF-beta signals. Nat Rev Mol Cell Biol. 2000;1:169-78.
In conclusion, chronically irradiated skin may become metabolically more active, leading to epidermal hyperplasia, irregular pigmentation, telangiectasias, elastosis, collagen reduction and wrinkles. Studies have evidenced that wearing sunscreen prevents these alterations associated with photoaging.5151. Boyd AS, Naylor M, Cameron GS, Pearse AD, Gaskell SA, Neldner KH. The effects of chronic sunscreen use on the histologic changes of dermatoheliosis. J Am Acad Dermatol. 1995;33:941-6.,5252. Seité S, Fourtanier AM. The benefit of daily photoprotection. J Am Acad Dermatol. 2008;58:S160-6.
Photocarcinogenesis
Photocarcinogenesis consists in the development of skin cancers induced by UVR.3232. Sklar LR, Almutawa F, Lim HW, Hamzavi I. Effects of ultraviolet radiation, visible light, and infrared radiation on erythema and pigmentation: a review. Photochem Photobiol Sci. 2013;12:54-64. UVR produces radical complexes, such as hydroxyl, aqueous electrons, hydrogen radicals and superoxide. These products, in their great majority, are produced by direct and indirect photosensitive reactions inducing DNA breakdown and base damage, being therefore lethal and mutagenic. In the skin, melanin is an important chromophore, which acts as a filter in the absorption of UVA, UVB and VL radiation. Melanin strongly absorbs visible radiation, helping to transform this energy in heat and dispersing it among hairs and blood vessels (capillaries). It also helps to eliminate radicals, such as hydroxyl and oxygen molecules, preserving the DNA against formation of pyrimidine bases.3030. Svobodova A, Walterova D, Vostalova J. Ultraviolet light induced alteration to the skin. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2006;150:25-38.,5353. Hussein MR. Ultraviolet radiation and skin cancer: molecular mechanisms. J Cutan Pathol. 2005;32:191-205.
The sensitivity of somatic cells to UVR is due to defects in pyrimidine dimer reparation induced by UVR. It is noteworthy that exposure to UVB leads to formation of cyclobutane - pyrimidine dimers and pyrimidine-pyridone photoproducts, as the main lesions to DNA. The incorrect repair of these products leads to mutations. Furthermore, the UVR may also produce non dimer photoproducts, like cytosine photohydrates, purine photoproducts and single-stranded DNA breakdown.5454. de Laat A, van Tilburg M, van der Leun JC, van Vloten WA, de Gruijl FR. Cell cycle kinetics following UVA irradiation in comparison to UVB and UVC irradiation. Photochem Photobiol. 1996;63:492-7.
55. Anderson RR, Parrish JA. The optics of human skin. J Invest Dermatol. 1981;77:13-9.-5656. Kanofsky JR, Sima P. Singlet oxygen production from the reactions of ozone with biological molecules. J Biol Chem. 1991;266:9039-42. As regards UVA radiation, its exact role in carcinogenesis is still unkmown.
In this sense, although the photons in the UVA spectrum are less energetic than UVB ones, it is believed that they can still produce mutations and cancer. As the DNA can absorb little of the UVA energy, the lesions typical of UVB, like pyrimidine dimers, are not important in carcinogenesis caused by UVA. It is assumed that UVA genotoxicity would be induced by indirect mechanisms, where free oxygen radicals are generated after the photons are absorbed by still unidentified photosensitizers.5757. de Gruijl FR, van der Leun JC. Physical variables in experimental photocarcinogenesis and quantitative relationships between stages of tumor development. Front Biosci. 2002;7:d1525-30. When these mutations affect the function of oncogenes and of tumor suppressor genes, such as TP53, PTCH1, BRM and RAS, there is a loss of cellular cycle control, with possible keratinocyte and melanocyte transformation and the onset of tumors.5858. Krämer M, Stein B, Mai S, Kunz E, König H, Loferer H, et al. Radiation-induced activation of transcription factors in mammalian cells. Radiat Environ Biophys. 1990;29:303-13.
The photoexposed skin is susceptible both to non-melanoma skin cancers, such as basal cell cancer and squamous cell cancer, and to melanoma. The non-melanoma skin cancers have been strongly linked to UV radiation exposure, since both UVA and UVB cause DNA damage and immunosuppression.5959. Chen AC, Halliday GM, Damian DL. Non-melanoma skin cancer: carcinogenesis and chemoprevention. Pathology. 2013;45:331-41. As to melanoma, a direct relationship has been demonstrated between UVR exposure and the risk to develop this type of tumor. However, there seems to be an association with acute and intense exposure.6060. Lotti T, Bruscino N, Hercogova J, de Giorgi V. Controversial issues on melanoma. Dermatol Ther. 2012;25:458-62.
Effects of visible light
VL is the part of electromagnetic radiation visible to the human eye and it represents around 40% of all solar radiation reaching the surface of the Earth.6161. Mahmoud BH, R-UVolo E, Hexsel CL, Liu Y, Owen MR, Kollias N, et al. Impact of long-wavelength UVA and visible light on melanocompetent skin. J Invest Dermatol. 2010;130:2092-7. Its effects on the skin have been extensively studied.
It was observed that, in large doses, VL causes cutaneous erythema. When a source of light emitting 98.3% of VL, 1.5% of infrared radiation and 0.19% of UVA-1 was used, Mahmoud et al. demonstrated that the type of skin is the main factor determining the intensity and duration of this signal. VL induces erythema in skins with phototypes IV to VI, which disappears within a two-hour period. In these types of skin, the degree of erythema escalates with the increase of VL doses. However, it cannot be induced in phototype II skin, even at high fluencies.
The authors proposed that perhaps VL induces a reaction inside the chromophores that generates heat, and then increased concentrations of melanin in higher phototypes would result in more production of heat, leading to vasodilation and erythema.6161. Mahmoud BH, R-UVolo E, Hexsel CL, Liu Y, Owen MR, Kollias N, et al. Impact of long-wavelength UVA and visible light on melanocompetent skin. J Invest Dermatol. 2010;130:2092-7.
As regards pigmentation, limited information is available on the role of VL. In a study by Ramasubramaniam et al.6262. Ramasubramaniam R, Roy A, Sharma B, Nagalakshmi S. Are there mechanistic differences between ultraviolet and visible radiation induced skin pigmentation? Photochem Photobiol Sci. 2011;10:1887-93. in India, it was observed that immediate pigmentation induced by VL was not significantly different from that produced by UV radiation, and that the spectra of action of VL and UVR upon inducing pigmentation were similar. Nevertheless, when compared to VL, UVR is 25 times more efficient to induce pigmentation. The investigators also concluded that the persistent pigmentation response afforded by VL is significantly less intense than that induced by UVR.6262. Ramasubramaniam R, Roy A, Sharma B, Nagalakshmi S. Are there mechanistic differences between ultraviolet and visible radiation induced skin pigmentation? Photochem Photobiol Sci. 2011;10:1887-93. Likewise, Mahmoud et al. also found evidence that pigmentation can be induced by VL.6161. Mahmoud BH, R-UVolo E, Hexsel CL, Liu Y, Owen MR, Kollias N, et al. Impact of long-wavelength UVA and visible light on melanocompetent skin. J Invest Dermatol. 2010;130:2092-7.
It seems that VL also contributes to free radical production. A study carried out in 2006 with simulated solar radiation on ex-vivo skin revealed that the presence of ascorbate radicals was directly proportional to irradiation. The production of this radical by UVR and VL in the corneal layer was approximately 67% and 35%, respectively.6363. Haywood R. Relevance of sunscreen application method, visible light and sunlight intensity to free-radical protection: A study of ex vivo human skin. Photochem Photobiol. 2006;82:1123-31.
Finally, there was evidence that VL, together with IR, promotes an increase in MMPs, diminishing the expression of procollagen type I, therefore contributing to photoaging.6464. Cho S, Lee MJ, Kim MS, Lee S, Kim YK, Lee DH, et al. Infrared plus visible light and heat from natural sunlight participate in the expression of MMPs and type I procollagen as well as infiltration of inflammatory cell in human skin in vivo. J Dermatol Sci. 2008;50:123-33.
Although artificial sources emit visible light, there are no studies demonstrating that the dose received is sufficient to lead to the above described effects.
Effects of infrared radiation
Infrared radiation (IR) consists in wavelengths longer than 780 nm and up to 1 mm, representing approximately 50% of the solar radiation that reaches the Earth. It has been divided into IR-A (780-1400 nm), IR-B (1400-3000 nm) and IR-C (3000 to 1 mm). IR-A and IR-B can penetrate the epidermis, the dermis and the subcutaneous tissue, while IR-C is almost completely absorbed by the epidermis due to the presence of water. IR exposure is noticed by human beings through heat sensation.6565. Schieke SM, Schroeder P, Krutmann J. Cutaneous effects of infrared radiation: from clinical observations to molecular response mechanisms. Photodermatol Photoimmunol Photomed. 2003;19:228-34.
Studies have revealed that IR can cause temporary erythema, probably secondary to vasodilation by thermal effect.6666. Lee HS, Lee DH, Cho S, Chung JH. Minimal heating dose: a novel biological unit to measure infrared irradiation. Photodermatol Photoimmunol Photomed. 2006;22:148-52.,6767. Pujol JA, Lecha M. Photoprotection in the infrared radiation range. Photodermatol Photoimmunol Photomed. 1992-1993;9:275-8. Another important observation is that infrared radiation, especially IR-A, contributes to photoaging. The mechanisms involved in this process have been investigated. It is assumed that they include: metalloproteinase-1 induction without induction of its inhibitor, the tissue inhibitor of metalloproteinase-1, which results in collagen breakdown,6868. Schroeder P, Lademann J, Darvin ME, Stege H, Marks C, Bruhnke S, et al. Infrared radiation-induced matrix metalloproteinase in human skin: implications for protection. J Invest Dermatol. 2008;128:2491-7.disorder in electron flow of the mitochondrial electron transport chain, leading to an inadequate production of energy by dermal fibroblasts;6969. Krutmann J, Schroeder P. Role of mitochondria in photoaging of human skin: the defective powerhouse model. J Investig Dermatol Symp Proc. 2009;14:44-9. angiogenesis stimulation and increased number of mastocytes.7070. Krutmann J, Morita A, Chung JH. Sun exposure: what molecular photodermatology tells us about its good and bad sides. J Invest Dermatol. 2012;132:976-84.
Finally, there was evidence that the IR-A seems to be associated with oxidative stress. Darvin et al. proposed that free radical formation would be influenced by the increased temperature occurring during IR radiation.7171. Darvin ME, Haag SF, Lademann J, Zastrow L, Sterry W, Meinke MC. Formation of free radicals in human skin during irradiation with infrared light. J Invest Dermatol. 2010;130:629-31. Jung et al. examined the heat effects on the association between IR and free radical formation in in vitro model of human fibroblast. They demonstrated that IR exposure at a temperature of 37ºC did not induce free radicals; however, at temperatures of 39ºC or higher, free radicals were produced.7272. Jung T, Höhn A, Piazena H, Grune T. Effects of water-filtered infrared A irradiation on human fibroblasts. Free Radic Biol Med. 2010;48:153-60.
Photodermatoses
Several skin diseases can be influenced by sunlight.7373. Murphy GM. Investigation of photosensitive disorders. Photodermatol Photoimmunol Photomed. 2004;20:305-11.
Idiopathic photodermatoses:
Polymorphic light eruption
Actinic prurigo
Solar urticaria
Hydroa vacciniforme
Chronic actinic dermatitis
Phototoxic contact dermatitis
Photoallergic contact dermatitis
Photosensitivity caused by medications - by toxicity or allergy
It occurs with diuretics, antibiotics, antipsychotics, sedatives, anti-hypertensives, non-hormonal anti-inflammatories, oral hypoglycemic agents and others.
Genophotodermatoses:
Xeroderma pigmentosum
Trichothiodystrophy
Cutaneous porphyria
Kindler-Weary syndrome
Bloom syndrome
Rothmund-Thomson syndrome
Cockayne syndrome
Diseases that are aggravated by sunlight
Melasma
Vitiligo
Lupus erythematosus
Dermatomyositis
Reticular erythematous mucinosis (REM)
Eczema
Seborrheic dermatitis
Psoriasis
Pityriasis rubra pilaris
Acne vulgaris
Rosacea
Lichen planus
Endemic pemphigus foliaceus
Bullous pemphigoid
Familial benign chronic pemphigus (Hailey-Hailey disease)
Grover disease
Pellagra
Carcinoid syndrome
Cutaneous T-cell linphoma
Disseminated superficial actinic porokeratosis
Darier's disease
Polymorphus erythema
Hartnup syndrome
Diseases caused by UVR immunosuppression
Herpes simplex
Viral exanthema
Verruca plana
Skin carcinomas
RECOMMENDATIONS OF THE BRAZILIAN SOCIETY OF DERMATOLOGY
-
Studies that can better assess the characteristics of the Brazilian population regarding the effects of solar radiation should be encouraged, especially the search for more adequate skin type classification methods when compared to Fitzpatrick's Classification.
-
As regards public health, the escalation of skin neoplasm incidence in the Brazilian population and the importance of solar radiation in the development of such diseases justify the concern about implementation of photoprotection actions.
-
SBD recommends the development of investigations that can better clarify the effect of non-ultraviolet radiation on the skin.
PHOTOPROTECTION
GENERAL CONCEPT
Although it has not been clearly defined in literature, photoprotection could be understood as a group of measures directed to reducing sun exposure and preventing the development of acute and chronic actinic damage.
The following are considered photoprotective measures: photoprotection education (photoeducation), topic photoprotection, oral photoprotection and mechanic photoprotection (achieved by roofs and glass, clothes and accessories).
The success of an adequate photoprotection program depends on the combination of the largest possible number of measures, taking into account the profile of the patient, including age, phenotypical characteristics (phenotype, color of skin, eyes and hair), habits, professional activity, geographic location of domicile, individual and familial antecedents of sun exposure-related diseases.
It is up to the healthcare professional, particularly the dermatologist, to identify and promote measures that are appropriate for the patient or the population group involved.
The following chapters seek to present, in condensed form, the main characteristics of different photoprotection measures, their indications and the recommendations of the Brazilian Society of Dermatology (Sociedade Brasileira de Dermatologia - SBD) for each situation.
CHAPTER 3
PHOTOEDUCATION
INTRODUCTION
The term "photoeducation" was introduced in 1988 to integrate the basic photoprotection concepts, determining why, where and how important protection against harmful effects of UV radiation (UVR) is. Over time the photoeducation concept was expanded, with emphasis on the positive and negative effects of sun exposure.7474. Stengel FM. Fotoeducación:un paso más allá dela fotoprotección. Arch Argent Dermatol. 1988;38:345-9.,7575. Stengel FM, Fernandez JF. Education and behavioral change for sun protection. J Cosmet Dermatol. 2005;4:83-8.
The consequences of excessive photoexposure depend on genetic, behavioral and geographic situation factors, as well as on the influence of external agents, such as concomitant diseases, transplants and use of medications. Among the negative effects of the mentioned photoexposure above the acceptable levels are premature aging, influence on the immunological status and mainly the onset of skin cancers.
Skin cancer is the neoplasm with the highest incidence in several countries in the world, including Brazil, with increased morbidity and mortality deriving from its progression. Multiple factors seem to be related to these findings, among them the change of habits of the population regarding solar exposure, estethical valuation of skin tanning and especially the increased exposure to ultraviolet radiation (UVR).7676. Fabris MR, Durães ES, Martignago BC, Blanco LF, Fabris TR. Assessment of knowledge of skin cancer prevention and its relation with sun exposure and photo protection amongst gym academy members on the South of Santa Catarina, Brazil. An Bras Dermatol. 2012;87:36-43.,7777. Glanz K, Maddock JE, Lew RA, Murakami-Akatsuka L. A randomized trial of the Hawaii Sun smart program's impact on outdoor recreation staff. J Am Acad Dermatol. 2001;44:973-8.
There are estimates that, in the whole world, 45% of the cancers that may be prevented are cutaneous and that most of the deaths caused by melanoma could be avoided.7777. Glanz K, Maddock JE, Lew RA, Murakami-Akatsuka L. A randomized trial of the Hawaii Sun smart program's impact on outdoor recreation staff. J Am Acad Dermatol. 2001;44:973-8.
78. Kullavanijaya P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.-7979. Lucci A, Citro HW, Wilson L. Assessment of knowledge of melanoma risk factors, prevention, and detection principles in Texas teenagers. J Surg Res. 2001;97:179-83. In this sense, several studies have emphasized the need for educational photoprotection measures for the population.8080. Melia J, Pendry L, Eiser JR, Harland C, Moss S. Evaluation of primary intervention initiatives for skin cancer: a review from a UK perpective. Br J Dermatol. 2000;143:701-8.,8181. Koh HK, Geller AC. The public health future of melanoma control. J Am Acad Dermatol. 2011;65:S3-5. Even patients who have already been diagnosed with cutaneous neoplasms have diverse behaviors regarding careful awareness of sun exposure and they do not always change their routine, including tanning habits.8282. Day AK, Wilson CJ, Hutchinson AD, Roberts RM. The role of skin cancer knowledge in sun-related behaviours: a systematic review. J Health Psychol. 2014;19:1143-62
ACTIONS FOR THE YOUNG PUBLIC
Several factors turn children and adolescents into a quite important public for photoeducation campaigns: solar exposure at the beginning of life has a crucial impact on the onset of skin cancer; children are more receptive than adults to receive guidance regarding prevention; photoprotection habits acquired in childhood and adolescence may modify behaviors and even affect the attitudes of the parents.8383. Benvenuto-Andrade C, Zen B, Fonseca G, De Villa D, Cestari T. Sun exposure and sun protection habits among high-school adolescents in Porto Alegre, Brazil. Photochem Photobiol. 2005;81:630-5.
84. Buller DB, Cokkinides V, Hall HI, Hartman AM, Saraiya M, Miller E, et al. Prevalence of sunburn, sun protection, and indoor tanning behaviors among Americans: review from national surveys and case studies of 3 states. J Am Acad Dermatol. 2011;65:S114-23.-8585. Lin JS, Eder M, Weinmann S. Behavioral counseling to prevent skin cancer: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;154:190-201.
There are several models that have been succesful in this regard, involving measures like sending mail and information, continued education programs at school and even national programs to encourage photoprotection.8686. Glanz K, Steffen AD, Schoenfeld E, Tappe KA. Randomized Trial of Tailored Skin Cancer Prevention for Children: The Project SCAPE Family Study. J Health Commun. 2013;18:1368-83.
87. Crane LA, Asdigian NL, Barón AE, Aalborg J, Marcus AC, Mokrohisky ST, et al. Mailed intervention to promote sun protection of children: a randomized controlled trial. Am J Prev Med. 2012;43:399-410.
88. Norman GJ, Adams MA, Calfas KJ, Covin J, Sallis JF, Rossi JS, et al. A randomized trial of a multicomponent intervention for adolescent sun protection behaviors. Arch Pediatr Adolesc Med. 2007;161:146-52.-8989. Crane LA, Deas A, Mokrohisky ST, Ehrsam G, Jones RH, Dellavalle R, et al. A randomized intervention study of sun protection promotion in well-child care. Prev Med. 2006;42:162-70.
It is of fundamental importance to adopt measures in accordance with the age group of the population. Information directed to children younger than 8 years of age should have a different approach than that directed to preadolescents and adolescents. Two systematic reviews concluded that educational measures to improve behavior concerning solar protection in elementary school and recreational activities were effective.9090. Stoebner-Delbarre A, Defez C, Borrel E, Sancho-Garnier H, Guillot B; Groupe EPICES. Prevention of skin cancer programs: Analysis of the impact of randomized trials. Ann Dermatol Venereol. 2005;132:641-7.,9191. Saraiya M, Glanz K, Briss PA, Nichols P, White C, Das D, et al. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiations: A systematic review. Am J Prev Med. 2004;27:422-66.
There are studies showing that small modifications in child behavior promoted with educational models implemented in schools, such as the SunWise School Program, developed by the US Environmental Protection Agency, significantly reduce the risk for skin cancer, consequently reducing expenses with this health problem for society.9292. Kyle JW, Hammitt JK, Lim HW, Geller AC, Hall-Jordan LH, Maibach EW, et al. Economic evaluation of the US Environmental Protection Agency's SunWise program: sun protection education for young children. Pediatrics. 2008;121:e1074-84.
There are few randomized studies to assess actions in health related to photoprotection and photoeducation, but evidences suggest that the participation of schools is essential.9393. Buendía-Eisman A, Feriche-Fernández E, Muñoz-Negro JE, Cabrera-León A, Serrano-Ortega S. Evaluation of a school intervention program to modify sun exposure behaviour. Actas Dermosifiliogr. 2007;98:332-44. They are the easiest way to reach children and adolescents. In this regard, it is interesting to have the contents inserted into science and human physiology programs, with the relative depth of their degree of understanding. Transmission of knowledge may take many varied forms, including theater plays and dramatizations that allow active participation. They are ludic and the most appropriate for some age groups.
The content should focus the fact that there are benefits and drawbacks, and that the intensity of damage depends on the resistance of the skin and of individual habits.9494. Townsend JS, Pinkerton B, McKenna SA, Higgins SM, Tai E, Steele CB, et al. Targeting children through school-based education and policy strategies: comprehensive cancer control activities in melanoma prevention. J Am Acad Dermatol. 2011;65:S104-13. In addition, schools are important intervention locations, as the students spend a lot of time in outdoor activities.9292. Kyle JW, Hammitt JK, Lim HW, Geller AC, Hall-Jordan LH, Maibach EW, et al. Economic evaluation of the US Environmental Protection Agency's SunWise program: sun protection education for young children. Pediatrics. 2008;121:e1074-84.,9595. Buller DB, Geller AC, Cantor M, Buller MK, Rosseel K, Hufford D, et al. Sun protection policies and environmental features in US elementary schools. Arch Dermatol. 2002;138:771-4. The experience of other countries shows interesting alternatives, like the USA where the CDC (Centers for Disease Control and Prevention) prepared a routine of norms to guide schools in the implementation of programs for skin cancer prevention.9696. Cdc.gov [Internet]. Centers for Disease Control and Prevention. Sun safety for America's youth toolkit. Atlanta (GA). July 2009. [cited 2013 Jun 29]. Available from: http://www.cdc.gov/cancer/skin/pdf/toolkit/SunSafetyToolkit_MainText.pdf.
http://www.cdc.gov/cancer/skin/pdf/toolk...
The World Health Organization (WHO) has also divulged guidelines for an initiative entitled "Solar Protection and Schools: How to make a difference". In this sense there are not only guidelines regarding the importance of this type of strategy but also a practical manual about implementing these practices in the schools.9797. who.int [Internet]. World Health Oganization. Sun protection and schools: how to make a difference. Geneva: WHO; 2003. [cited 2014 Oct 30]. http://www.who.int/uv/publications/en/sunprotschools.pdf.
http://www.who.int/uv/publications/en/su...
Examples of other actions targeted at skin cancer prevention and directed at children include initiatives like the Brazilian Society of Dermatology (Sociedade Brasileira de Dermatologia - SBD) children section in their website and the campaign "The Sun, a Friend of the Children (Sol Amigo da Infância)" which, in addition to the distribution of comic books, sponsored teacher training and the preparation of a law project.9898. Sbd.org.br [Internet]. Sociedade Brasileira de Dermatologia. SBD Kids. [acesso 29 Jun 2013]. Disponível em: http://www.sbd.org.br/acoes/sbd-kids/.
http://www.sbd.org.br/acoes/sbd-kids/...
There is a law project currently going through the motions to be approved that aims at establishing the program "Skin Cancer Prevention - The Sun, a Friend of the Children" as a mandatory extracurricular activity for preschool and elementary I and II children at public and private school networks. According to this project, dermatologists certified by the Brazilian Medical Association (Associação Médica Brasileira) will conduct teacher training on the adequate content for children and adolescents.
Another important aspect to be considered regarding photoeducation is that the strategies should be adapted to reach adolescents, including orientation about the harmful effects of indoor tanning.9999. Reynolds KD, Buller DB, Yaroch AL, Maloy J, Geno CR, Cutter GR. Effects of program exposure and engagement with tailored prevention communication on sun protection by young adolescents. J Health Commun. 2008;13:619-36.
100. Balk SJ, Fisher DE, Geller AC. Teens and indoor tanning: a cancer prevention opportunity for pediatricians. Pediatrics. 2013;131:772-85.-101101. Armstrong AW, Idriss NZ, Kim RH. Effects of video-based, online education on behavioral and knowledge outcomes in sunscreen use: a randomized controlled trial. Patient Educ Couns. 2011;83:273-7. A study carried out in Brazil showed that adolescents are aware of the damage caused by the sun but, despite this fact, believe that tanning improves the appearance and justifies the risk.8383. Benvenuto-Andrade C, Zen B, Fonseca G, De Villa D, Cestari T. Sun exposure and sun protection habits among high-school adolescents in Porto Alegre, Brazil. Photochem Photobiol. 2005;81:630-5. In other countries, the scenario is similar: despite the knowledge about the harmful results of excessive sun exposure, behavior changes among the adolescents are unsatisfactory.102102. Suppa M, Cazzaniga S, Fargnoli MC, Naldi L, Peris K. Knowledge, perceptions and behaviours about skin cancer and sun protection among secondary school students from Central Italy. J Eur Acad Dermatol Venereol. 2013;27:571-9.
The orientation programs should also be included in the educational content, by means of guided study such as review work, search on the Internet and participation in the creation of educational tools like websites and through the social networks.103103. Buendía Eisman A, Arias Santiago S, Moreno-Gimenez JC, Cabrera-León A, Prieto L, Castillejo I, et al. An Internet-based programme to promote adequate UV exposure behaviour in adolescents in Spain. J Eur Acad Dermatol Venereol. 2013;27:442-53. It is recommended to promote lectures with specialists trained in the language of young people, mainly medical students, who would be more appropriate than older educators. In addition, it is important to offer the possibility of clearing doubts, including availability for private talks, showing alternatives to the esthetic aspect of tanning.
ACTIONS FOR THE ADULT POPULATION
There are few randomized clinical studies that assess photoeducation interventions in adults.8585. Lin JS, Eder M, Weinmann S. Behavioral counseling to prevent skin cancer: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;154:190-201. Most of them are based on computer models to generate orientation, which varied from 15 minute sessions to counseling given by professionals in person, in writing or by telephone.104104. Glazebrook C, Garrud P, Avery A, Coupland C, Williams H. Impact of a multimedia intervention "Skinsafe" on patients' knowledge and protective behav- iors. Prev Med. 2006;42:449-54.
105. Glanz K, Schoenfeld ER, Steffen A. A randomized trial of tailored skin cancer prevention messages for adults: Project SCAPE. Am J Public Health. 2010;100:735-41.
106. Prochaska JO, Velicer WF, Redding C, Rossi JS, Goldstein M, DePue J, et al. Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive regular mammo- grams. Prev Med. 2005;41:406-16.
107. Prochaska JO, Velicer WF, Rossi JS, Redding CA, Greene GW, Rossi SR, et al. Multiple risk expert systems interventions: impact of simultaneous stage- matched expert system interventions for smoking, high-fat diet, and sun exposure in a population of parents. Health Psychol. 2004;23:503-16.-108108. Geller AC, Emmons KM, Brooks DR, Powers C, Zhang Z, Koh HK, et al. A randomized trial to improve early detection and prevention practices among siblings of melanoma patients. Cancer. 2006;107:806-14. The behavior differences in relation to sun exposure after the interventions, although statistically significant, were small and it is still not clear if they are clinically representative.8585. Lin JS, Eder M, Weinmann S. Behavioral counseling to prevent skin cancer: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;154:190-201.
As regards young adults, studies conducted with college students focused the issue of attempting to change standards based on the appearance, that is, highlighted the harmful effects of ultraviolet radiation in photoaging, rather than messages related to skin cancer prevention.109109. Hillhouse J, Turrisi R, Stapleton J, Robinson J. A randomized controlled trial of an appearance-focused intervention to prevent skin cancer. Cancer. 2008;113:3257-66.
110. Mahler HI, Kulik JA, Gerrard M, Gibbons FX. Long-term effects of appearance-based interventions on sun protection behaviors. Health Psychol. 2007;26:350-60.
111. Stapleton J, Turrisi R, Hillhouse J, Robinson JK, Abar B. A comparison of the efficacy of an appearance-focused skin cancer intervention within indoor tanner subgroups identified by latent profile analysis. J Behav Med. 2010;33:181-90.-112112. Turrisi R, Mastroleo NR, Stapleton J, Mallett K. A comparison of 2 brief intervention approaches to reduce indoor tanning behavior in young women who indoor tan very frequently. Arch Dermatol. 2008;144:1521-4. The interventions varied from fact sheets to 30-minute videos. When groups that used artificial tanning were evaluated after the intervention there was a 35% decrease; however, the follow-up period of these studies was short.109109. Hillhouse J, Turrisi R, Stapleton J, Robinson J. A randomized controlled trial of an appearance-focused intervention to prevent skin cancer. Cancer. 2008;113:3257-66.,111111. Stapleton J, Turrisi R, Hillhouse J, Robinson JK, Abar B. A comparison of the efficacy of an appearance-focused skin cancer intervention within indoor tanner subgroups identified by latent profile analysis. J Behav Med. 2010;33:181-90.,112112. Turrisi R, Mastroleo NR, Stapleton J, Mallett K. A comparison of 2 brief intervention approaches to reduce indoor tanning behavior in young women who indoor tan very frequently. Arch Dermatol. 2008;144:1521-4.
Most of the interventions that were effective in promoting behavior modifications regarding photo-protection incorporated the use of computers. All of the studies with young adults focused the concern with the appearance, emphasizing the harmful effects of sun regarding premature aging. There is evidence that this argument makes this population group more sensitive to guidance, especially the women. It is interesting to highlight that interventions regarding photoeducation should vary in accordance with gender and age.8585. Lin JS, Eder M, Weinmann S. Behavioral counseling to prevent skin cancer: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;154:190-201.
Another group of people who are particularly susceptible to the risk of excessive sun exposure are workers who are engaged in outdoor activities; data show the increase of pre-neoplastic lesions and nonmelanocytic neoplasms.113113. Fartasch M, Diepgen TL, Schmitt J, Drexler H. The relationship between occupational sun exposure and non-melanoma skin cancer: clinical basics, epidemiology, occupational disease evaluation, and prevention. Dtsch Arztebl Int. 2012;109:715-20. These individuals are traditionally more resistant to change of habits and wearing photoprotection because they believe it is a waste of time or it is uncomfortable.
The perception of attitudes taken by the hiring company, like the implementation of programs, is a strong factor of change for its employees, more marked in those with lighter phototypes, in women, in those with a better educational level and those that always work in open areas.114114. Reeder AI, Gray A, McCool JP. Occupational sun protection: workplace culture, equipment provision and outdoor workers' characteristics. J Occup Health. 2013;55:84-97.,115115. Falk M, Anderson CD. Influence of age, gender, educational level and self-estimation of skin type on sun exposure habits and readiness to increase sun protection. Cancer Epidemiol. 2013;37:127-32.
Results of other countries cannot always be extrapolated to Brazil, but we know that our problems are similar, the climate may be very adverse in several regions of the country and that some companies already include photoprotection among their occupational safety requirements. The result of these initiatives may bring relevant data to the upcoming campaigns and health policies.
A questionnaire was recently proposed and validated to estimate the current and past characteristics of photoexposure, as well as photoprotection practices (Sun Exposure and Behaviour Inventory - SEBI).116116. Jennings L, Karia PS, Jambusaria-Pahlajani A, Whalen FM, Schmults CD. The Sun Exposure and Behaviour Inventory (SEBI): validation of an instrument to assess sun exposure and sun protective practices. J Eur Acad Dermatol Venereol. 2013;27:706-15. This instrument may become very useful in studies about the incidence of skin cancer and risk modifications, as it will allow data comparison, currently very difficult due to the different methods and evaluations used in the studies.
LAY MEDIA APPROACH
The impact of written and/or visualized information is very important regarding knowledge, perception of risk and behavior modifications. Studies carried out in Austria demonstrated that printed media, television, radio and family are the most relevant in terms of adherence to changes, much more than medical advice. The Internet is more used by male individuals, while women are more attentive to printed material in magazines and information supplied by companies that manufacture sunscreens. At the same time, most of the interviewed believe that the doctor is the most reliable source of information and that flyers or posters attract little attention.117117. Jung GW, Senthilselvan A, Salopek TG. Ineffectiveness of sun awareness posters in dermatology clinics. J Eur Acad Dermatol Venereol. 2010;24:697-703.
These results demonstrate that the photoeducation approach should include different resources and that the doctor must be an actor adequately trained in multiple techniques to guarantee a lasting promotion of good health habits.118118. Haluza D, Cervinka R. Perceived relevance of educative information on public (skin) health: a cross-sectiona l questionnaire survey. J Prev Med Public Health. 2013;46:82-8.
Educational campaigns targeted at different types of public have been promoted in several countries, in an effort to diminish the tendency of increase in skin neoplasm cases. Although these campaigns have increased attention regarding cutaneous cancer, they have not resulted in behavior modification, and the majority of the people continue to rely only on sunscreen as protection, even increasing the time of exposure because they believe they are protected.119119. Murphy GM. Photoprotection: public campaigns in Ireland and the U.K. Br J Dermatol. 2002;146:31-3.,120120. Thomas K, Hevey D, Pertl M, Ní Chuinneagáin S, Craig A, Maher L. Appearance matters: the frame and focus of health messages influences beliefs about skin cancer. Br J Health Psychol. 2011;16:418-29.
Being tanned continues to have a strong impact on the perception of physical attractiveness, especially among adolescents and young adults.120120. Thomas K, Hevey D, Pertl M, Ní Chuinneagáin S, Craig A, Maher L. Appearance matters: the frame and focus of health messages influences beliefs about skin cancer. Br J Health Psychol. 2011;16:418-29. There is great contribution of the media to that effect, attributing a positive esthetic appeal to outdoor activities in the sun, showing opinion leaders and fashion models always tanned. Furthermore, it is commonly believed that darker skins show imperfections less and the general aspect is improved by sharper contrast with clothes and even the scenario.120120. Thomas K, Hevey D, Pertl M, Ní Chuinneagáin S, Craig A, Maher L. Appearance matters: the frame and focus of health messages influences beliefs about skin cancer. Br J Health Psychol. 2011;16:418-29.
In order to achieve modification of tanning habits, the concept of "being tanned is a synonym of beauty" should be modified. Direct or subliminary messages should be positive and perceived as rewards, since individuals rarely respond to negative affirmations, without an immediate benefit.
The attitude of emphasizing the advantages of careful solar exposure to preserve health and beauty, as well as detailed description of the consequences of excessive sun exposure in terms of pigment alterations, drying of skin and premature onset of wrinkles may be more effective than warnings about a distant and not confirmed risk of neoplasms.121121. Jung GW, Senthilselvan A, Salopek TG. Likelihood of dermatology patients to inquire about sun protection measures during a regular clinic visit. J Cutan Med Surg. 2011;15:266-74.,122122. Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27:237-51.
The complicity of lay persons who are not part of the medical environment, mainly those the public identifies with in real life or would like to resemble brings results of great significance. Different forms of communication at premium times, through channels accessible to all types of public, examples of real situations that are repeated and associated with success and attractiveness have a great chance of being effective for that purpose.
Health education and prevention may be easily integrated into doctor-patient communication. However, this measure alone does not have the required coverage. Mass communication requires a coherent, direct and always consistent speech, regardless of the professional involved.
In order to achieve this goal it is necessary for messages to be based on supporting material prepared by specialists, not only regarding the medical aspect but also the communication. They should be conveyed in all possible ways, from schools and universities, above all taking the opportunities offered by the media, as TV, radio and newspapers. Associations of specialists, such as the Brazilian Society of Dermatology, are able to supply and divulge routines to contact communication media keeping the content uniform.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Actions targeted at photoeducation should be divided into four large groups: Children and Adolescents, Adults, Outdoor Workers and Media Actions.
-
Actions for the public composed of Children and Adolescents:
-
The school should participate in this type of education and it is the easiest way to reach children and adolescents.
-
Actions targeted at children younger that 8 years of age should have a different focus than those targeted at preadolescents and adolescents.
-
Incorporate into the school curriculum a space for education regarding photoprotection and photoeducation.
-
Adolescents should receive orientation about the harmful effects of tanning.
-
Establish a long-term photoeducation program combining SBD and governmental initiatives, as well as third sector non-governmental institutions.
-
-
Actions for the adult population:
-
When targeted at young adults, the harmful effects of ultraviolet radiation in photoaging should be emphasized more than messages related to skin cancer prevention.
-
The participation of public figures increases adherence to and visibility of campaigns, which was confirmed in our National Skin Cancer Campaign. Nevertheless, such participations should be continued.
-
Keep photoprotection guidance as part of the permanent campaign of SBD.
-
Include Photobiology and Photoprotection classes in the Undergraduate Medical curriculum. SBD could contribute with the preparation of the plan and minimum content of this presentation.
-
-
Actions for outdoor workers
-
Develop education projects on photoprotection to be presented at the companies that employ workers who are engaged in outdoor activities.
-
Develop projects to better assess methods able to measure the level of solar radiation to which outdoor workers are exposed.
-
Offer continuous training to doctors of companies with the above described profile.
-
Promote efforts, together with governmental authorities, to create specific legislation about sunscreen transformation and photoprotective measures like wearing Personal Protective Equipment (PPE) for outdoor workers.
-
-
Media Actions:
-
Offer training programs to specialized media about the effects of solar radiation and prevention mechanisms.
-
Develop within the roll of SBD members, through the department of photobiology, a group of dermatologists especially prepared to respond to media requests and give interviews or clarification as SBD spokespersons.
-
Prepare and keep available to members the norms of conduct and posture before the media, as well as detailed instructions regarding the position of SBD on photoprotection issues, so that the message is clear and uniform.
-
CHAPTER 4
SUNSCREENS
INTRODUCTION
Historically, sunscreens have been idealized to prevent sunburn in labor activities and to prolong outdoor leisure and sport time spent in the sun, in addition to permiting a certain degree of tanning. The first formulas date back to 1928 and aimed at reducing the incidence of UVR-B, the main inducer of erythema and DNA damage, on the skin.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
It was only in the 70s that commercial scale production of topical sunscreen was started, making their use popular. Studies in the 80s evidenced the importance of UVR-A in photoaging and its coadjuvant role in cutaneous carcinogenesis.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
Conceptually, topical sunscreen (or sunscreen) are products that are applied on the skin, composed of substances that interfere with solar radiation, reducing its biological effects on the tissues.124124. Monteiro EO. Filtros solares e fotoproteção. RBM Rev Bras Med. 2010;67:5-18.
CHAPTER 4 A -
FORMULATION OF TOPICAL SUNSCREEN
UV FILTERS
Ultraviolet filters are the elements present in photoprotector formulas that interfere directly with the incident solar radiation through absorption, reflection or dispersion of energy.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
From the structural viewpoint, ultraviolet filters may be organic or inorganic compounds. The organic actives (or chemical filters) absorb UVR photons, promoting an alteration in their molecular structure. The inorganic actives (or physical filters) have a mineral origin and promote the reflection of UVR to the external part of the tissue.125125. Shaat NA. The chemistry of ultraviolet filters In: Shaat NA. Sunscreens: regulation and commercial development. 3. ed. Boca Raton: Taylor and Francis; 2005. p. 217-39.
Organic filters are conjugated aromatic compounds that operate through a molecular mechanism of UVR absorption and return of this energy to the environment by means of emission of longer and less energetic wavelengths, such as visible light and infrared radiation.125125. Shaat NA. The chemistry of ultraviolet filters In: Shaat NA. Sunscreens: regulation and commercial development. 3. ed. Boca Raton: Taylor and Francis; 2005. p. 217-39.
Compared to inorganic filters, they present a greater potential of sensitization, greater risk of percutaneous absorption and smaller photostability, strongly dependent on its chemical structure and combination of actives in the formula.125125. Shaat NA. The chemistry of ultraviolet filters In: Shaat NA. Sunscreens: regulation and commercial development. 3. ed. Boca Raton: Taylor and Francis; 2005. p. 217-39.
More recently, a new generation of organic filters was presented, with larger photostability and lower potential of dermal permeation, substantially reducing the risk for development of sensitization.125125. Shaat NA. The chemistry of ultraviolet filters In: Shaat NA. Sunscreens: regulation and commercial development. 3. ed. Boca Raton: Taylor and Francis; 2005. p. 217-39.
Depending on their molecular structure, the organic filters may better absorb UVB or UVA radiation. Some more recent molecules are able to produce peaks of UVA and UVB absorption and, for that reason, are called broad spectrum filters.125125. Shaat NA. The chemistry of ultraviolet filters In: Shaat NA. Sunscreens: regulation and commercial development. 3. ed. Boca Raton: Taylor and Francis; 2005. p. 217-39.
Inorganic filters present a minimum potential for allergic sensitization and high photostability. However, their reflective properties may cause excessive shine and a whitish aspect, limiting their exclusive use to formulas due to the low cosmetic acceptance.126126. Schlossman D, Sho Y. Inorganic ultraviolet filters In: Shaat NA. Sunscreens: regulation and commercial development. 3. ed. Boca Raton: Taylor and Francis, 2005. p. 239-81.
Inorganic filters like zinc oxide and titanium dioxide act on the surface of the skin, reflecting incident radiation; nevertheless, when micronized, they may permeate the corneal layer and in addition to reflection, act by diffraction and dispersion.
The size of the particles of the inorganic filters is, therefore, a factor that determines their effect. The smaller the particle, the better the skin coverage and, consequently, reflection; but refraction is worse. Therefore, reflection and refraction are inversely related. The efficiency of inorganic filters is related to the size and dispersion of their particles.126126. Schlossman D, Sho Y. Inorganic ultraviolet filters In: Shaat NA. Sunscreens: regulation and commercial development. 3. ed. Boca Raton: Taylor and Francis, 2005. p. 239-81.
When micronized, these filters diminish the whitish appearance of the skin and favor the stability of the emulsion. They may be coated with silicone, silica, aluminum oxide, estearic acid, aluminum estearate, among others, improving the dispersion of the filter, avoiding agglomeration of particles and altering the rheology of the emulsion. Titanium dioxide, for example, can only be associated with avobenzone when coated with silica and dimeticone. On the other hand, only some inorganic filters with particle sizes larger than 200 nm are able to reflect in the visible light range, therefore offering protection.126126. Schlossman D, Sho Y. Inorganic ultraviolet filters In: Shaat NA. Sunscreens: regulation and commercial development. 3. ed. Boca Raton: Taylor and Francis, 2005. p. 239-81.
The different photoprotector actives also present curves characteristic of UVR absorbance. Usually, commercial sunscreen use a composition of physical and chemical filters to expand the photoprotection spectrum (UVA and UVB), explore synergistic properties and minimize the adverse effects linked to a specific active.
In Brazil, sunscreen are categorized by the Brazilian Health Surveillance Agency (ANVISA) as cosmetics (risk degree: 2), which waives the need for a medical prescription to be sold. However, there are regulations concerning the UV filters permitted and the need for studies to be carried out to ascertain their safety and efficacy.127127. Agência Nacional de Vigilância Sanitária (Brasil). Resolução nº 211, de 14 de Julho de 2005. Estabelece a Definição e a Classificação de Produtos de Higiene Pessoal, Cosméticos e Perfumes, conforme Anexo I e II desta Resolução e dá outras definições. Diario Oficial da União jul 2005.,128128. Brasil. Agência Nacional de Vigilância Sanitária. Resolução - RDC no 30, de 1o de junho de 2012. Aprova o Regulamento Técnico Mercosul sobre Protetores solares em Cosméticos e dá outras providências. Diario Oficial da União jun 2012. [acesso 6 Nov 2014]. Disponível em: http://portal.anvisa.gov.br/wps/wcm/connect/e15afe804c58f17fb8f0f8dc39d59d3e/Resolu%C3%A7%C3%A3o+RDC+N%C2%BA+30,+de+1%C2%BA+de+Junho+de+2012.pdf?MOD=AJPERES.
http://portal.anvisa.gov.br/wps/wcm/conn...
Chart 2 lists 33 actives regulated by ANVISA for commercial use in Brazil.
In addition to protection against ultraviolet radiation, there has been interest about actives able to interfere with visible light and infrared radiation.
Filters able to protect against visible light act only by a reflection mechanism, producing a whitish aspect with low cosmetic acceptance. As an alternative, formulators use different pigments as active blockers in this radiation range, that give an appearance of makeup foundation to the formula, limiting its use by some individuals, mainly those of the male sex.
Up to the moment, there are no ANVISA approved substances able to absorb, disperse or reflect in the infrared range. Sunscreen that have the ability to protect against infrared radiation achieve it through the addition of ingredients that can reduce cellular or molecular damage derived from this radiation.
The different photoprotective actives present characteristics of solubility, compatibility among themselves, their vehicles and supplements, besides curves of solar spectrum absorbance that rule the choice of topical photoprotector formulation components.129129. Kenneth K, Palefsky I. Formulation sunscreens products In: Shaat NA. Sunscreens: regulation and commercial development. 3rd ed. Boca Raton: Taylor and Francis; 2005. p. 353-85.
Technologies for vehiculation of actives
The processes of vehiculation of actives based on particles allow the control of molecule release at different tissue levels. The different polymers behave as vectors of the actives and divide into monolithic type and reservoir type.
In monolithic vectors, the active is adsorbed by the particle surface. According to the size of the polymeric particles used, the vectors may be classified as microparticles (1-250 micra) and nanoparticles (1-100 nm).
In systems of controlled release like the reservoir type, the active is involved by a membrane or another colloidal complex such as liposomes, cyclodextrine, nanocapsules and microemulsions).
Micro and nanoencapsulation of organic filters is a strategy to improve retention in the skin, provide photostability and increase effectiveness for favoring the formation of a film on the surface of the tissue.
The use of solid lipidic nanoparticles, for example, reduces systemic absorption of oxybenzone, increasing its concentration in the corneal layer and demanding smaller concentrations of the active to reach the desired effectiveness.130130. Teixeira SMMCG. Veiculação de filtros solares utilizados na fotoproteção. [dissertação]. Porto (PT): Universidade Fernando Pessoa; 2012.
The capture of organic actives in silica microspheres, for example, improves solubility of actives in water, reducing chemical incompatibility problems among actives and tissue hypersensitivity reactions.
COMPOSITION OF SUNSCREEN AND PHARMACEUTICAL FORMULAS
A pharmaceutical formula is composed of active ingredient, vehicle and excipients (emollients/solvents, emulsifiers, moisturizers, preservatives, fragrance, stabilizers, therapeutic supplements, among others). The substance that will develop the desired therapeutic activity is called active ingredient. The vehicle is the excipient appearing in the formula in the largest amount, promoting incorporation of the other components. It does not have a specific effect, but may interfere in the final result of the formula and in photoprotective activity.130130. Teixeira SMMCG. Veiculação de filtros solares utilizados na fotoproteção. [dissertação]. Porto (PT): Universidade Fernando Pessoa; 2012.
Depending on the vehicle used (according to its composition and physical-chemical state), the type of formula, as well as the type of skin it is recommended for may be identified. The other components, called excipients or additives, should be inert; however, they have an important role in the preparation, stability, appearance, safety and effect of the product.
Emulsifiers, auxiliary ingredients, fragrance and preservatives are examples of excipients. The choice of vehicle, excipients and pharmaceutical formula should take into account the active ingredient chosen, the objective of the treatment and the characteristics' of the patient that will use the product.131131. Prista LN, Alves AC, Morgado R. Técnicas Farmacêuticas e Farmácia Galênica. Vol II, 3. ed. Lisboa: Fundação Calouste Gulbenkian; 1990.,132132. Associação Nacional de Farmacêuticos Magistrais. Manual de Recomendações para Aviamento de Formulações Magistrais: Boas Práticas de Manipulação. São Paulo: ANFARMAG; 1997.
Some polymers are added to the formula to control spreadability, absorption and formation of film on the skin, which should be homogeneous and stable in conditions of sweat, heat and minimal physical contact. The quality of film formation is one of the most important characteristics for continuance of the photoprotector effect.
The solvents (emulsifiers) used in the formulas to make the mixture of organic filters with the vehicle possibly interfere in the characteristic absorption curve of actives, as well as in the photoprotective measures of the formula. It is a known fact that even order, speed, technique and temperature of the mixture of formula components generate final products with different properties and may interfere in the effectiveness of the photoprotector, which should alert dermatologists regarding the reliability of sunscreen masterful formulas.
Topical sunscreen may be used in different pharmaceutic formulas.129129. Kenneth K, Palefsky I. Formulation sunscreens products In: Shaat NA. Sunscreens: regulation and commercial development. 3rd ed. Boca Raton: Taylor and Francis; 2005. p. 353-85.
130. Teixeira SMMCG. Veiculação de filtros solares utilizados na fotoproteção. [dissertação]. Porto (PT): Universidade Fernando Pessoa; 2012.
131. Prista LN, Alves AC, Morgado R. Técnicas Farmacêuticas e Farmácia Galênica. Vol II, 3. ed. Lisboa: Fundação Calouste Gulbenkian; 1990.
132. Associação Nacional de Farmacêuticos Magistrais. Manual de Recomendações para Aviamento de Formulações Magistrais: Boas Práticas de Manipulação. São Paulo: ANFARMAG; 1997.
133. Cross SE, Innes B, Roberts MS, Tsuzuki T, Robertson TA, McCormick P. Human skin penetration of sunscreens nanoparticles: in vitro assessment of a novel micronized zinc oxide formulations. Skin Pharmacol Physiol. 2007;20:148-54.-134134. Kibbe AH. Handbook of Pharmaceutical Excipients. 3. ed. Washington: APhA and PP; 2000.
Oils: The first sunscreen preparations used oil as vehicle. They were popularly known as tanning lotions. They are monophasic formulations with good spreadability, easy application and very stable when incorporating liposoluble actives. In such cases, manipulation is simple and can be done at room temperature. Unfortunately, the easy application results in low effectiveness as it leaves a thin transparent film on the skin, with reduced SPF. The cosmetic effect is also a limiting factor.
Gels: Gels are vehicles composed of a liquid phase, usually water or alcohol, and another solid, represented by gelling agents. The latter are most often polymeric substances, interpenetrated by a liquid so as to modify their physical state (rheology). According to the quantity of gelling agents present in a formula, different types of rheological effects may be obtained. A smaller quantity will obtain serum, after that a fluid, then a gel and a larger quantity, starch gel. In addition to modifying the physical state of the formula, the quantity of gelling agent may result in a "sticky", inadequate formula.
The photoprotective gels incorporate hydrosoluble actives that actually are compounds insoluble in water that, associated with solubilizers (usually non ionic surfactants), allow their incorporation. Hydroalcoholic bases, on the other hand, may allow the dissolution of liposoluble molecules in alcohol, and in this manner be solubilized in water. These vehicles may be classified, regarding the type of disperser used, into hydrophilic or hydrogels; alcoholic and hydrophobic or oil gels. The photoprotective gels should have a pleasant appearance, easy application and removal, fast drying, smoothness and elasticity. Their main indication is for oily or acneic skins.
Emulsions: Emulsions are composed of an oily phase and a watery phase, not miscible, that through the action of an emulsifying agent form a homogeneous mixture. These special surfactants allow two systems that are immiscible to disperse and form a stable product. The composition of this pharmaceutic formula presents then a dispersed phase and an interface. This vehicle has the properties of being versatile, cosmetically pleasant and compatible with the incorporation of lipo- and hydrosoluble substances, which make it one of the most prescribed topical pharmaceutic formula.
Emulsions may be classified in several ways: by the physical aspect they may be liquid (fluid emulsions or milks) or pasty (creams); by the pH they may be acid, alkaline or neutral. However, the most commonly used classification takes into consideration the proportion between the oily and the watery phases, that is, they may be grouped according to the predominant dispersing media. This way oil in water or water in oil emulsions may be obtained. Nowadays, the outstanding emulsions are: silicone in water, propylene glycol in silicone, triphasic emulsions, microemulsions and polymeric emulsions, often called pseudo-emulsions. Sunscreens may be incorporated into any of them, as long as the adequate pharmacotechnique is employed.
The oil in water emulsions (O/W) present low greasiness, produce a refreshing effect, dry rapidly and may be easily washed in water. Such advantages are due to the fact that the continuous phase of the emulsion is watery, and the dispersive phase, oily. The water in oil emulsions (W/O) have a greater percentage of oil, and this is the continuous phase. They make the skin greasier and shiny; repeal water and offer protection against humidity and cold. However, they are thermolabile.
Cream Gel: The cream gels result from the incorporation of a gelling agent into an emulsion. They are very popular in photoprotective formulations, especially in tropical countries, for imparting the sensory effect of gels and the softness of emulsions, without their disadvantages (stickiness and greasiness, respectively). They are indicated for daily use in sunscreen, including for people with oily skin, as they incorporate fat sequestering agents.
Mousses: A mousse is typically a fluid emulsion to which a propellent was added. They require special flasks with a valve that, when pressed, releases an elegant, easy to use and easily spreadable foam.
Aerosols: Aerosols are colloidal dispersions of a liquid in the atmosphere. They are usually oily, which may enhance their spreadability, but make the skin greasy. Modern formulas, with silicone or similar substances, have been employed as sunscreen that have good acceptance but questionable results, not only by the difficulty in assessing the amount applied, but also for its irregular distribution on the skin. They are more useful when used to reinforce the effect of a photoprotector worn in the form of emulsion or gel, when a reapplication is necessary.
Sticks: Composed of waxes and oils, they have a solid or semisolid structure to which inorganic and/or liposoluble organic filters are incorporated. This association results in products that are quite water resistant. They are indicated for application on the lips, as lip pencil, dorsum of the nose, or other restricted skin areas.
Powders and Foundations: These are cosmetic products designed for makeup, reducing skin shine, giving it uniform color and texture, besides protecting from solar radiation. Inorganic filters are usually incorporated into face powders; however, both organic and inorganic filters may be used in fluid foundations and compact powders.
Chart 3 summarizes characteristics of formulas connected with the vehicles utilized.
OTHER ACTIVES IN SUNSCREEN FORMULAS
One of the issues involved is adherence of the user to daily and routine wearing of sunscreen.135135. Draelos ZD. Compliance and sunscreens. Dermatol Clin. 2006;24:101-4. Many times, sunscreens are perceived as sticky or uncomfortable products to wear. At the same time, the patients do not perceive the benefits derived from their use, since prevention of photo damage and skin cancer occur mainly on a long term basis.136136. Draelos ZD. The multifunctional value of sunscreen-containing cosmetics. Skin Therapy Lett. 2011;16:1-3. In this regard, sunscreen containing other actives in the same formula have been developed by the pharmaceutical industry with the intention of offering, in addition to photoprotective properties, benefits that may be felt in the short term, thus encouraging frequent use and guaranteeing better protection against the sun.
Moisturizers in sunscreen
Topical moisturizers are substances designed to improve and maintain the cutaneous barrier.137137. Lodén M. The clinical bennefit of moisturizers. J Eur Acad Dermatol Venereol. 2005;19:672-88. They are used to restore the barrier function of the epidermis, cover small cutaneous microfissures, provide a soft protective film and increase the amount of water in the epidermis, while improving the appearance and tactile properties of the skin.138138. Kraft JN, Lynde CW. Moisturizers: what they are and a practical approach to product selection. Skin Therapy Lett. 2005;10:1-8. Occlusive substances like dimethicone and petrolatum, as well as moisturizers, such as glycerol and propylene glycol, among others, may be used for this purpose.
Studies demonstrate that products containing moisturizers and sunscreens in the same formulation are able to provide effective photoprotection against actinic damage.139139. Seite S, Fourtanier A, Rougier A. Photoprotection in moisturizers and daily-care products. G Ital Dermatol Venereol. 2010;145:631-6. At the same time, they may be useful in helping to maintain and restore the epidermal barrier. Such characteristics encourage acceptance and adherence of the user, favoring routine application of the product.
Antioxidants
Free radicals are species that present unpaired electrons. In live systems, free radicals are represented mainly by reactive oxygen species (ROS). They are extremely unstable and tend to rapidly react with neighboring molecules, donating one electron (oxidation). When not neutralized by antioxidants, they may lead to cascading reactions with subsequent cellular damage.140140. Polefka TG, Meyer TA, Agin PP, Bianchini RJ. Cutaneous oxidative stress. J Cosmet Dermatol. 2012;11:55-64.
In addition to endogenous sources of free radicals (mainly mitochondrial oxidative metabolism) there are exogenous sources, among them ultraviolet radiation (UVR).140140. Polefka TG, Meyer TA, Agin PP, Bianchini RJ. Cutaneous oxidative stress. J Cosmet Dermatol. 2012;11:55-64. There are several studies that ascertain the participation of UVR, through excessive ROS production, into degenerative molecular and cellular processes that lead to photoaging, immunosupression and carcinogenesis.140140. Polefka TG, Meyer TA, Agin PP, Bianchini RJ. Cutaneous oxidative stress. J Cosmet Dermatol. 2012;11:55-64.
141. Yaar M, Gilchrest BA. Photoageing: mechanism, prevention and therapy. Br J Dermatol. 2007;157:874-87.
142. Watson RE, Griffiths CE. Pathogenic aspects of cutaneous photoaging. J Cosmet Dermatol. 2005;4:230-6.-143143. Chen L, Hu JY, Wang SQ.The role of antioxidants in photoprotection: a critical review. J Am Acad Dermatol. 2012;67:1013-24.
Although there are endogenous control mechanisms of cellular oxidative stress in face of more extreme situations, these mechanisms may be overcharged and fail.143143. Chen L, Hu JY, Wang SQ.The role of antioxidants in photoprotection: a critical review. J Am Acad Dermatol. 2012;67:1013-24. In this regard, besides physical and chemical filters, other photoprotective strategies are being investigated, among them the antioxidants (AOx).
The beneficial effect of AOx associated with sunscreen has been demonstrated in humans.144144. Wu Y, Matsui MS, Chen JZ, Jin X, Shu CM, Jin GY, et al. Antioxidants add protection to a broad-spectrum sunscreen. Clin Exp Dermatol. 2011;36:178-87.,145145. Matsui MS, Hsia A, Miller JD, Hanneman K, Scull H, Cooper KD, et al. Non-sunscreen photoprotection: antioxidants add value to a sunscreen. J Investig Dermatol Symp Proc. 2009;14:56-96. Moreover, there is vast literature about the antioxidant ability of some substances.146146. Lin JY, Selim MA, Shea CR, Grichnik JM, Omar MM, Monteiro-Riviere NA, et al. UV photoprotection by combination topical antioxidants vitamin C and vitamin E. J Am Acad Dermatol. 2003;48:866-74.
147. Katiyar SK, Matsui MS, Elmets CA, Mukhtar H. Polyphenolic antioxidant (-)-epigallocatechin-3-gallate from green tea reduces UVB-induced inflammatory responses and infiltration of leukocytes in human skin. Photochem Photobiol. 1999;69:148-53.
148. Olsen EA, Katz HI, Levine N, Nigra TP, Pochi PE, Savin RC, et al. Tretinoin emollient cream for photodamaged skin: results of 48-week, multicenter, double-blind studies. J Am Acad Dermatol. 1997;37:217-26.-149149. Wang SQ, Stanfield JW, Osterwalder U. In vitro assessments of UVA protection by popular sunscreens available in the United States. J Am Acad Dermatol. 2008;59:934-42.Nevertheless, creating formulations that combine sunscreen and AOx while guaranteeing the effectiveness of both in the final product is still a challenge.143143. Chen L, Hu JY, Wang SQ.The role of antioxidants in photoprotection: a critical review. J Am Acad Dermatol. 2012;67:1013-24.,149149. Wang SQ, Stanfield JW, Osterwalder U. In vitro assessments of UVA protection by popular sunscreens available in the United States. J Am Acad Dermatol. 2008;59:934-42.
Usually, AOx are naturally unstable and should remain stable and bioavailable in the final formulation. At the same time, AOx must penetrate the corneal layer and remain in adequate concentrations in the epidermis and dermis as long as it is desired that sunscreen continue on the surface of the skin for appropriate protection. From a legal viewpoint, when this benefit is mentioned on labels, it becomes necessary to ascertain its safety and bioavailability in the formula.
In vivo studies are required to determine the best AOx to be used in these formulas and how these products will be formulated to guarantee the effectiveness of all components.
Repellents in sunscreen
According to ANVISA, repellents are classified as cosmetics and follow a specific legislation150150. Agência Nacional de Vigilância Sanitária (Brasil). Resolução nº 19, de 10 de Abril de 2013. Dispõe sobre os requisitos técnicos para a concessão de registro de produtos cosméticos repelentes de insetos e dá outras providências. Diario Oficial da União abr 2013. which determines the allowed ingredients and concentrations, while demanding safety and effectiveness studies. As happens with sunscreen, ANVISA also determines that repellent labels should include certain mandatory information.
The best known repellent active is diethyltoluamide (DEET), which presents toxicity and effectiveness against several mosquito species like Anopheles, Phlebotomus, Aedes, Culicidae, ticks and fleas.151151. Hexsel CL, Bangert SD, Hebert AA, Lim HW. Current sunscreen issues: 2007 food and drug administraion sunscreen labelling recommendations and combination sunscreen/insect repelente products. 2008;59:316-23.,152152. Pollack RJ, Kiszewski AE, Spielman A. Repelling mosquitoes. N Engl J Med. 2002;347:2-3.
Regarding the addition of solar protection actives in repellents, although the ingredients may be used in a formula, there are a few details to be considered: the ability of the sunscreen to filter ultraviolet radiation may be diminished by repellents such as DEET, which is the most common, while the toxicity of the repellent is increased by the sunscreen, especially in children.153153. Kasichayanula S, House JD, Wang T, Gu X. Percutaneous characterization of the insect repellent DEET and the sunscreen oxybenzone from topical skin application. Toxicol Appl Pharmacol. 2007;223:187-94.,154154. Chen T, Burczynski FJ, Miller DW, Gu X. Percutaneous permeation comparison of repellents picaridin and DEET in concurrent use with sunscreen oxybenzone from commercially available preparations. Pharmazie. 2010;65:835-9.
The problem is exacerbated by the application instructions, which are a paradox: while sunscreen should be generously and frequently applied (every two hours or more often, if necessary), insect repellents (DEET) should be applied no more frequently than every two to six hours, depending on the concentration.151151. Hexsel CL, Bangert SD, Hebert AA, Lim HW. Current sunscreen issues: 2007 food and drug administraion sunscreen labelling recommendations and combination sunscreen/insect repelente products. 2008;59:316-23.,155155. Murphy ME, Montemarano AD, Debboun M, Gupta R. The effect of sunscreen on the efficacy of insect repellent: A clinical trial. J Am Acad Dermatol. 2000;43:219-22.
There are other repellent actives, like essences and icaridin, but their benefits when associated with sunscreen have not been defined yet.
CONCLUSIONS
The challenges of the pharmaceutical industry connected with topical photoprotector formulations involve the photostability of organic filters, broadening the effectiveness spectrum and parameters, incorporating active ingredients, improving cosmetic and sensory aspects, individualizing vehicles, besides nanotechnology for vehiculation of actives and the use of substances that increase the effectiveness of actives, without increasing their concentration in the product (enhancers or boosters).
Finally, the ideal photoprotector formulation should take into consideration aspects like efficiency for the proposed indication, scope of protection spectrum (UVA and UVB), safety and tolerability for topical use, stability, no staining of clothes, adequate cosmetics, pleasant fragrance, resistance to water, spread-ability, high extinction coefficient, substantivity*** and affordable cost.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
124. Monteiro EO. Filtros solares e fotoproteção. RBM Rev Bras Med. 2010;67:5-18.-125125. Shaat NA. The chemistry of ultraviolet filters In: Shaat NA. Sunscreens: regulation and commercial development. 3. ed. Boca Raton: Taylor and Francis; 2005. p. 217-39.,139139. Seite S, Fourtanier A, Rougier A. Photoprotection in moisturizers and daily-care products. G Ital Dermatol Venereol. 2010;145:631-6.,140140. Polefka TG, Meyer TA, Agin PP, Bianchini RJ. Cutaneous oxidative stress. J Cosmet Dermatol. 2012;11:55-64.
Photoprotector manipulation requires not only knowledge of pharmacotechnique, but also of regulation and market aspects. On the other hand, the dermatologist, as prescriber, has the role of evaluating the diverse products available in the market, indicating the most adequate for each situation. The magistral prescription for sunscreen lacks safety regarding information about the actual protection factor required and labeled, as it is unfeasible to determine the protection factor in the small amounts produced and the different compositions of actives used.
CHAPTER 4B
EVALUATION OF SAFETY AND EFFICACY OF SUNSCREEN
Necessary safety requirements for ultraviolet filters
Brazil has an official list of ingredients classified as ultraviolet filters, which are allowed for use in formulations.127127. Agência Nacional de Vigilância Sanitária (Brasil). Resolução nº 211, de 14 de Julho de 2005. Estabelece a Definição e a Classificação de Produtos de Higiene Pessoal, Cosméticos e Perfumes, conforme Anexo I e II desta Resolução e dá outras definições. Diario Oficial da União jul 2005. This list has as reference the European list of allowed ingredients for sunscreens.
For a molecule to be approved for topical use in a photoprotector, a safety dossier must be presented to ANVISA containing standardized topical and systemic toxicological studies, besides evaluation of cutaneous permeation, whose absence makes systemic effects impossible.
Follows Chart 4, with the required studies for safety evaluation of raw material to be used in sunscreens.156156. Agência Nacional de Vigilância Sanitária. Guia de Avaliação de Segurança de produto cosmético. 2 ed. Brasília: Anvisa; 2003.
Any of the effects cited above may be demonstrated by toxicological tests. According to calculations, data base and complementary toxicological tests, dose/concentration and route of administration are then established.156156. Agência Nacional de Vigilância Sanitária. Guia de Avaliação de Segurança de produto cosmético. 2 ed. Brasília: Anvisa; 2003. Thus the importance of toxicological studies of a cosmetic raw material before its use in formulations.
All of the substances on ANVISA's list of ingredients for sunscreens are free from systemic toxicity and carcinogenesis when used topically and in the recommended concentrations.
Endocrine effects of sunscreens
Schlumpf et al.157157. Schlumpf M, Cotton B, Conscience M, Haller V, Steinmann B, Lichtensteiger W. In vitro and in vivo estrogenicity of UV screens. Environ Health Perspect. 2001;109:239-44. published, in 2001, a scientific article with the title: "Estrogenicidade in vivoe in vitro de filtros ultravioleta", in which the authors evaluated the estrogenic potential of benzophenone-3 (B3), avobenzone (BMDM), 4-methylbenzylidene camphor (4-MBC), octyl methoxycinnamate (OMC), homosalate (HMS) and octyl dimethyl PABA filters, through in vitroreadings and experiments in guinea pigs.
In vitro readings were made with culture of breast cancer cells. In this experiment, the authors observed estrogenic potential in all filters, except in avobenzone.
In the in vivo study, a slight increase of uterine weight (estrogenic action) was observed with oral use of benzophenone-3 filter and a moderate increase with filters 4-MBC and OMC. Filters avobenzone, octyl-PABA and homosalate did not affect uterine weight with oral use.
When use was topical, the only filter that caused changes in uterine weight was 4-MBC.
Based on the findings of Schlumpf et al., the Scientific Committee On Consumer Safety (SCCS) organized, in July of 2001, a panel of experts in toxicology to evaluate the real estrogenic potential of these ingredients and verify the need for changing permission regarding its use in photoprotective formulations.158158. Scientific Comission of Consumer safety. European commission. Opinion on the Evaluation of Potentially Estrogenic Effects of UV-filters adopted by the SCCNFP during the 17th Plenary meeting of 12 June 2001.
The conclusion of the Committee was that the organic filters evaluated and authorized for use in cosmetic formulations in the European Union did not present estrogenic effects that could pose risks to human health. The results obtained by Schlumpf in his study arose from the use of excessively elevated doses of active ingredients, topically or orally, unlike the usual exposition to the ingredients when in normal use conditions.
This way, these products were not prohibited in the European Union or anywhere else, being amply used in sunscreen formulations for many years.
ANVISA standardization: safety in sunscreens
Sunscreens are considered cosmetic according to Brazilian law (risk degree: 2), that is, with greater risk of interaction with human skin.127127. Agência Nacional de Vigilância Sanitária (Brasil). Resolução nº 211, de 14 de Julho de 2005. Estabelece a Definição e a Classificação de Produtos de Higiene Pessoal, Cosméticos e Perfumes, conforme Anexo I e II desta Resolução e dá outras definições. Diario Oficial da União jul 2005. Every product categorized as solar filter must obey a specific law that regulates labeling, FPS and UVA protection determination method.128128. Brasil. Agência Nacional de Vigilância Sanitária. Resolução - RDC no 30, de 1o de junho de 2012. Aprova o Regulamento Técnico Mercosul sobre Protetores solares em Cosméticos e dá outras providências. Diario Oficial da União jun 2012. [acesso 6 Nov 2014]. Disponível em: http://portal.anvisa.gov.br/wps/wcm/connect/e15afe804c58f17fb8f0f8dc39d59d3e/Resolu%C3%A7%C3%A3o+RDC+N%C2%BA+30,+de+1%C2%BA+de+Junho+de+2012.pdf?MOD=AJPERES.
http://portal.anvisa.gov.br/wps/wcm/conn...
When a manufacturer applies for registration with ANVISA, he should send the studies and a draft of the product label for evaluation.
Therefore, any product, regardless of the manufacturer or country of origin, must adapt itself to the norm of the law. If the product has any additional allegation (example: protection against invisible light, hypoallergenic, for oily skin, etc.) it must present evidence for that allegation.128128. Brasil. Agência Nacional de Vigilância Sanitária. Resolução - RDC no 30, de 1o de junho de 2012. Aprova o Regulamento Técnico Mercosul sobre Protetores solares em Cosméticos e dá outras providências. Diario Oficial da União jun 2012. [acesso 6 Nov 2014]. Disponível em: http://portal.anvisa.gov.br/wps/wcm/connect/e15afe804c58f17fb8f0f8dc39d59d3e/Resolu%C3%A7%C3%A3o+RDC+N%C2%BA+30,+de+1%C2%BA+de+Junho+de+2012.pdf?MOD=AJPERES.
http://portal.anvisa.gov.br/wps/wcm/conn...
,156156. Agência Nacional de Vigilância Sanitária. Guia de Avaliação de Segurança de produto cosmético. 2 ed. Brasília: Anvisa; 2003.
ANVISA recommends that some safety studies be developed to ensure greater safety for the consumer, like studies on photoirritation and photosensitization.156156. Agência Nacional de Vigilância Sanitária. Guia de Avaliação de Segurança de produto cosmético. 2 ed. Brasília: Anvisa; 2003. The ingredients in sunscreens are developed seeking to reduce adverse reactions to a minimum, and when these occur, they must not be systemic but occur on the application site.
According to Schauder and Ippen,159159. Schauder S, Ippen H. Contact and photocontact sensitivity to sunscreens. Review of a 15-year experience and of the literature. Contact Dermatitis. 1997;37:221-32. the typical patients with adverse reaction to sunscreens are women with history of photodermatosis, such as polymorphous light eruption, for they are continuous users and on skin already inflamed, with altered cutaneous barrier. The most common type of described reaction is photosensitization.160160. Avenel-Audran M. Sunscreen products: Finding the allergen. Eur J Dermatol. 2010;20:161-6.
Nanotechnology in sunscreens
Nanotechnology in sunscreens allowed enhancement of product cosmetics, better transparency and spreadability, besides better stability when delivered in nanospheres.
The technical groups that regulate the use of this technology in countries such as the USA, European Union and Japan, which have been discussing nanotechnology in cosmetics, divide the safety concern in two big groups: nanovectorized ingredients, through nanocapsules, such as liposomes and nanospheres; and nanoparticles, which are the nanoparticulate active ingredient itself.161161. Kaur IP, Agrawal R. Nanotechnology: a new paradigm in cosmeceuticals. Recent Pat Drug Deliv Formul. 2007;1:171-82.
The first ones have a toxicological profile identical to the molecule without the delivery system, and would not need complementary studies; regarding the nanoparticulate active ingredient, the particles which have been studied for sunscreens are titanium dioxide and zinc oxide.161161. Kaur IP, Agrawal R. Nanotechnology: a new paradigm in cosmeceuticals. Recent Pat Drug Deliv Formul. 2007;1:171-82.
Nanoparticulate titanium dioxide and zinc oxide have been intensely studied and current evidences indicate that there is no substantially greater permeation of the skin than the active ingredient in its conventional form.162162. Andersson-Willman B, Gehrmann U, Cansu Z, Buerki-Thurnherr T, Krug HF, Gabrielsson S, et al. Effects of subtoxic concentrations of TiO2 and ZnO nanoparticles on human lymphocytes, dendritic cells and exosome production. Toxicol Appl Pharmacol. 2012;264:94-103.
However, there seem to be risks in the inhalation of titanium dioxide, in manufacturing conditions, although not for the end user. In Brazil, some forums are being created in ANVISA to discuss the theme and to capacitate future national discussions on the subject.
EVALUATION OF THE EFFICACY OF SUNSCREEN
The benefits of wearing sunscreens in the prevention and treatment of different conditions or dermatological diseases are already well established in the literature.
Its most immediate and evident benefit is the prevention of sunburn, which, by the way, was the motivation behind the researchers in the beginning of the twentieth century to develop products capable of avoiding it, particularly for aquatic and leisure activities.163163. Roelandts R. History of human photobiology In: Lim HW, Hönigsmann H, Hawk JLM. Photodermatology. New York: Informa Healthcare USA; 2007. p 1-13.
As regards public health, on the other hand, the main benefit of the correct use of sunscreens is the prevention of cutaneous cancer. Studies show that the continuous use of sunscreens is capable of preventing the development of non-melanoma skin cancer and cutaneous melanoma.164164. Vainio H, Miller AB, Bianchini F. An international evaluation of the cancer-preventive potential of sunscreens. Int J Cancer. 2000;88:838-42.
165. Rigel DS. The effect of sunscreen on melanoma risk. Dermatol Clin. 2002;20:601-6.-166166. Diffey BL. Sunscreen and melanoma: The future looks bright. Br J Dermatol. 2005;153:378-81.
The quantification of the efficacy of a sunscreen is essential to determine its effectiveness in the prevention of solar damage, that is, what is its ability to protect the skin from deleterious effects of the sun.
To choose a method capable of determining its efficacy, one must have in mind the desired marker (end point). In other words, which damage are we considering when measuring sunscreen efficacy?
We can didactically divide photoprotecting methods into three broad categories:
In vivo methods: Methods that use the evaluation of a biological end point triggered by solar radiation, verifying the capability of the product to suppress or reduce the event. It may be considered an ideal method, as long as it is a relevant marker, of easy observation, rapid onset and measurable by a method with reproducibility and repeatability.
Spectrophotometric Methods: Due to the ability of sunscreens to reflect or absorb radiation, readings that use spectrophotometry may be particularly useful, especially in the development of formulations or in conditions in which in vivo readings do not meet the minimum methodological requirements.
In vitro Methods: By means of cell cultures or specific reagents, in vitro methods are an alternative, in specific conditions, for evaluating molecular or cellular alterations triggered by solar radiation, and when the protection ability afforded by a photoprotector cannot be evaluated by in vivo methods.
Even though, as said above, the main benefit from using a sunscreen is the prevention of skin cancer, a disease that develops slowly and insidiously, the in vivo model does not represent the best method for quantification of its efficacy.
The first method developed and validated for evaluating the efficacy of a sunscreen was the Solar Protection Factor (SPF), which quantifies the protection against solar erythema (sunburn), considering (MED) the minimal erythemal dose. MED is the necessary amount of UVR to produce a minimal erythema on the skin. In 1978, a study for determination of the SPF was standardized for the first time by the American agency Food and Drugs Administration (FDA) as being the numerical ratio between the MED of skin photoprotected by sunscreen (applied in the quantity of 2mg/cm2) and the MED of non-photoprotected skin.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.,167167. Food and Drug Administration. Department of Health, Education and Welfare, FDA. Sunscreen drug products for over-the-counter drugs: proposed safety, effective and labeling conditions. Federal register.43/166.38206-38269.25 August 1978. Available from:http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Over-theCounterOTCDrugs/StatusofOTCRulemakings/ucm090127.pdf
http://www.fda.gov/downloads/Drugs/Devel...
SPF = MED (protected skin)/MED (non-protected skin)
The proposed study was performed using a group of 20 volunteers with phototypes I-III (Fitzpatrick Scale), submitted to increasing doses of UVR through an artificial source of light called "solar simulator". The radiation is applied to skin areas photoprotected with solar filter (2 mg/cm2) and to unprotected areas. After an exposure period of 16 to 24 hours, a MED reading is performed for both areas and its ratio is calculated. The average values found in the group of volunteers is the SPF of the tested product.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
After the proposed method was published by the FDA, different international regulatory agencies and other institutions proposed their methods for calculating the efficacy of a sunscreen. We highlight, among them, the method described in 1994 by the European Union through the Comité de Liaison des Associations Européennes de l'Industrie de la Parfumerie - COLIPA, which received, in 2005, its last update and the name International Sun Protection Factor Test Method (ISPF).123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
Despite their differences, FDA and COLIPA/Internacional methods produce similar results and, in practice, we can say they generate equivalent SPF values.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
Since then the methodologies described by the North Americans (FDA) and Europeans (COLIPA) became references in determining SPF in several countries, being internationally accepted. The FDA (used in USA) and COLIPA (used in Europe and in other countries) methods were updated in 2011168168. Food and Drug Administration. Department of Health and Human Services, FDA. Sunscreen Drug Product for Over-The-Counter Human Use, Final Rule, Federal Register vol. 1978N-0038. Available from: http://www.fda.gov/OHRMS/DOCKETS/98fr/cd031.pdf
http://www.fda.gov/OHRMS/DOCKETS/98fr/cd...
and 2006,169169. International Sun Protector Factor Test Method. International SPF Test Method 2006 (COLIPA - CTFA SA - JCIA - CTFA US) respectively. In Brazil, through Resolution RDC 30 published by ANVISA in 2012,128128. Brasil. Agência Nacional de Vigilância Sanitária. Resolução - RDC no 30, de 1o de junho de 2012. Aprova o Regulamento Técnico Mercosul sobre Protetores solares em Cosméticos e dá outras providências. Diario Oficial da União jun 2012. [acesso 6 Nov 2014]. Disponível em: http://portal.anvisa.gov.br/wps/wcm/connect/e15afe804c58f17fb8f0f8dc39d59d3e/Resolu%C3%A7%C3%A3o+RDC+N%C2%BA+30,+de+1%C2%BA+de+Junho+de+2012.pdf?MOD=AJPERES.
http://portal.anvisa.gov.br/wps/wcm/conn...
all products named solar filters must present studies that prove their efficacy through at least one of the two international methodologies or their current updates, FDA 2011 or COLIPA 2006.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
In addition to the SPF test, the water resistance test evaluates if a sunscreen is capable of maintaining its efficacy (SPF) even after periods of immersion in water. This evaluation is particularly important for products designed for intentional exposure to the sun: aquatic activities and sport activities. According to the FDA, a "water resistant" sunscreen is the one which maintains its photoprotecting properties after two 20-minute immersions in water, whereas a "very resistant" filter is still effective even after four 20-minute immersions.168168. Food and Drug Administration. Department of Health and Human Services, FDA. Sunscreen Drug Product for Over-The-Counter Human Use, Final Rule, Federal Register vol. 1978N-0038. Available from: http://www.fda.gov/OHRMS/DOCKETS/98fr/cd031.pdf
http://www.fda.gov/OHRMS/DOCKETS/98fr/cd...
Two methods are internationally more accepted to determine it: the one described by the FDA in its most recent monograph (2011)168168. Food and Drug Administration. Department of Health and Human Services, FDA. Sunscreen Drug Product for Over-The-Counter Human Use, Final Rule, Federal Register vol. 1978N-0038. Available from: http://www.fda.gov/OHRMS/DOCKETS/98fr/cd031.pdf
http://www.fda.gov/OHRMS/DOCKETS/98fr/cd...
and used in the USA territory and the method described by COLIPA in 2004,170170. European Cosmetics Association. COLIPA Guidelines. Guidelines for evaluating sun product water resistance. October 2004. used in the European Union and in other countries around the world.
Basically, the method for determination of water resistance reproduces the SPF test described above, introducing two other areas: non-protected skin areas and skin area protected by the sunscreen being studied, applied in the amount of 2 mg/cm2, with two irradiations before and two after immersion in a bathtub with swirling water. This way, the SPF value is determined before immersion (in both areas irradiated before the immersion) and after immersion. According to the method proposed by the FDA, in case the intention is that a sunscreen will have the "water resistant" or "very water resistant" attributes, the SPF value on the label must be the SPF value found in the irradiated areas after the immersion period.
In the guidelines published by COLIPA in 2004, however, if the product being studied does not present a reduction of its pre-immersion SPF value greater or equal to 50% in the post-immersion calculation, then the product may inform the "water resistant" or "very water resistant" qualifications, if the immersion period is, respectively, 40 or 80 minutes.170170. European Cosmetics Association. COLIPA Guidelines. Guidelines for evaluating sun product water resistance. October 2004.
Since it is a measure against sunburn, an event that essentially arises from UVB radiation, SPF is not considered an adequate method for assessing the protection level against UVA radiation. We know that UVA radiation is extremely important when speaking about photoaging, photodermatoses and prevention of skin cancer, which arises mainly from UVB radiation but is also influenced by UVA.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
The concern of researchers in finding a method capable of quantifying the photoprotecting efficacy of solar filters in the UVA band arose between the 80's and 90's of the last century, in view of the emerging evidences, at the time, of damage caused by UVA radiation at the same time that the first filters capable of protecting in this band were launched in the market.
Described by Moyal et al., the Persistent Pigment Darkening (PPD) 171171. Moyal D, Chardon A, Kollias N. Determination of UVA protection factors using the persistent pigment darkening (PPD) as the end point (part 1):calibration of the method. Photodermatol Photoimmunol Photomed. 2000 Dec;16:245-9.,172172. Moyal D, Chardon A, Kollias N. UVA protecion efficacy of sunscreens can be determinated by the persistent pigment darkening (PPD) method (part 2). Photodermatol Photoimmunol Photomed. 2000;16:250-5. method evaluates sunscreen protection against persistent pigmentation, a phenomenon that arises exclusively from UVA radiation.
The rationale of the PPD method, currently designated UVA Protection Factor (UVA-PF), is similar to SPF. Two areas are evaluated in each volunteer, one non-protected skin area and another skin area protected by the studied sunscreen applied in the quantity of 2 mg/cm2. The areas are irradiated with an artificial source of light which emits exclusively UVA radiation. After 2 hours a reading is performed of both areas to determine the Minimal Pigmentary Dose (MPD), that is, the least amount of energy sufficient to produce evident pigmentation.171171. Moyal D, Chardon A, Kollias N. Determination of UVA protection factors using the persistent pigment darkening (PPD) as the end point (part 1):calibration of the method. Photodermatol Photoimmunol Photomed. 2000 Dec;16:245-9.,173173. European Cosmetics Association. COLIPA Method for the in vitro determination of UVA protection provided by sunscreen products. COLIPA Guideline, 2009.
Nowadays, the method described by Moyal et al.171171. Moyal D, Chardon A, Kollias N. Determination of UVA protection factors using the persistent pigment darkening (PPD) as the end point (part 1):calibration of the method. Photodermatol Photoimmunol Photomed. 2000 Dec;16:245-9.,172172. Moyal D, Chardon A, Kollias N. UVA protecion efficacy of sunscreens can be determinated by the persistent pigment darkening (PPD) method (part 2). Photodermatol Photoimmunol Photomed. 2000;16:250-5. is considered a reference to quantify UVA protection in Japan and in the European Union. COLIPA approved, in 2005, an in vitrospectrophotometric method named in vitro PPD,173173. European Cosmetics Association. COLIPA Method for the in vitro determination of UVA protection provided by sunscreen products. COLIPA Guideline, 2009. which demonstrated equivalent results to those initially described, found with in vivo PPD.174174. Moyal D, Wichrowski K, Tricaud C. In vivo persistent pigment darkening method: a demonstration of the reproducibility of the UVA protection factors results at several testing laboratories. Photodermatol Photoimmunol Photomed. 2006;22:124-8.
Besides the PPD method, the method described by Diffey175175. Diffey BL, Tanner PR, Matts PJ, Nash JF. In vitro assessment of the broad-spectrum ultraviolet protection of sunscreen products. J Am Acad Dermatol. 2000;43:1024-35. and later modified by COLIPA,173173. European Cosmetics Association. COLIPA Method for the in vitro determination of UVA protection provided by sunscreen products. COLIPA Guideline, 2009. named Critical Wavelength (CWL), is considered an important method for the quantification of broad spectrum protection. CWL is a spectrophotometric method which determines the spectral curve of a product applied on a polymethylmethacrylate (PMMA) plate, whose surface was submitted to blasting to produce a specific rugosity similar to the human skin.
A determined amount of the product is applied to the plate and then submitted to UV radiation in special equipment, before determination of the spectral curve. Previous radiation is necessary for the joint assessment of photostability of the product, relevant information when we deal with UVA radiation, that is, we evaluate the product curve after submitting it to determined levels of radiation.173173. European Cosmetics Association. COLIPA Method for the in vitro determination of UVA protection provided by sunscreen products. COLIPA Guideline, 2009.
With the determination of the spectral curve of the product, after irradiation in the band of 290 to 400nm, the whole area under the curve is calculated and the point that represents 90% of this area is determined. This point is named CWL. The larger this value, that is, the closer to the maximum (400 nm), the greater is the broad spectrum coverage of this product. Currently, it is recommended that the ideal minimum point be 370 nm, that is, for a product to present a good UVA and UVB coverage it must have a critical wavelength greater or equal to 370 nm.173173. European Cosmetics Association. COLIPA Method for the in vitro determination of UVA protection provided by sunscreen products. COLIPA Guideline, 2009.
Another relevant reading is the determination of photostability, defined as the capability of a sunscreen to maintain its photoprotecting efficacy even after periods of radiation exposure.176176. Gaspar LR, Maia Campos PM. Evaluation on the photostability of different UV filter combinations in a sunscreen. Int J Pharm. 2006;307:123-8.
We know that many products may lose their efficacy with continuous exposure to radiation, which occurs particularly within the UVA band. To quantify photostability, spectrophotometric readings are performed before and after the exposure of the plate to the source of UV radiation. In case an important variation of spectral curves does not occur, we can say the product is photostable.
Besides the determination of photoprotecting efficacy in UVB (SPF), UVA (PPD or UVA-PF and CWL), water resistance and photostability, other measurements may be performed in a complementary way.
They are usually measurements performed in vitro (specific media or cell cultures) and may be recommended for evaluating effects that are complementary, but inherent to a sunscreen, such as genomic protection and antioxidant protection.
With recent publications demonstrating the capability of longer wavelength radiations, non-ultraviolet, to produce deleterious effects on the skin, the interest for methods capable of quantifying the efficacy of a sunscreen in these wavelengths has grown.
We currently know that visible light has relevant participation in the process of skin pigmentation,177177. Mahmoud BH, Hexsel CL, Hamzavi IH, Lim HW. Effects of visible light on the skin. Photochem Photobiol. 2008;84:450-62. interfering with the triggering of pigmentary dermatoses such as melasma and postinflammatory hyperchromia. The efficacy of a photoprotector in the protection against visible light has been evaluated by spectrophotometric methods,178178. Schalka S, Addor FAS, Agelune CM, Pereira VMC. Sunscreen protection against visible light: a new proposal for Evaluation. Surg Cosmet Dermatol 2012;3:45-52. but until the present moment, a consensually validated model in literature does not exist and is still an object of research.
Regarding infrared radiation, we currently know about its potential oxidative effect, participating in the generation of free radicals and its consequent damage to molecular and cellular structures which will, in the long term, trigger photoaging.179179. Schieke SM, Schroeder P, Krutmann J. Cutaneous effects of infrared radiation: from clinical observations to molecular response mechanisms. Photodermatol Photoimmunol Photomed. 2003;19:228-34. Methods capable of quantifying the protection of solar filters against infrared radiation effects are not yet established; there are only proposals for quantification of the protecting ability against the increase of matrix metalloproteinases through a medium of cell cultures.179179. Schieke SM, Schroeder P, Krutmann J. Cutaneous effects of infrared radiation: from clinical observations to molecular response mechanisms. Photodermatol Photoimmunol Photomed. 2003;19:228-34.
A project for harmonization of photoprotecting efficacy evaluating methods is currently in effect, sponsored by ISO (International Standards Organization),180180. International Organization for Standardization. ISO/TC 217 - Cosmetics WG7 - Sun protection test methods, 1998. by a technical committee, with the participation of researchers of several countries, including Brazil. This project aims to standardize and harmonize all photoprotecting efficacy evaluation methods of sunscreens, so that consistent results are produced with worldwide uniformization.
At the present moment, the following have already been published: method for determination of the Solar Protection Factor (SPF), in vivoUVA protection (UVA-PF) and in vitro UVA protection. Methods to determine the Solar Protection Factor (SPF) in vitro, water resistance and photostability are still under the process of validation.
In order for a sun screen to have its registration approved by ANVISA, its documentation and studies must be previously submitted and evaluated. In Brazil, as well as in different countries in the world, sun screens are classified as cosmetics.
Regarding the presentation of photoprotecting efficacy studies, sunscreen manufacturers must submit the studies and label wording to ANVISA, according to Brazilian law of photoprotection, RDC 30, published in 2012, with its most important points described in chart 5.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
SBD agrees with the classification of sunscreens as cosmetic products for greater universalization of access to consumers.
-
All ingredients recognized by ANVISA have adequate use safety, with no evidences of carcinogenic or estrogenic effects, if used topically, in adequate concentrations, in sun screens.
-
In light of current knowledge, there is no evidence about the risk of using inorganic nanoparticulate solar filters in topical sunscreen.
-
Topical sunscreen must present an adequate safety profile in conformity with ANVISA legislation and corroborative safety studies should be performed.
-
Antioxidants may be added to sunscreens as an additional benefit; however, evidence of its efficacy on these products is necessary.
-
The new Brazilian law on photoprotection, RDC 30, of 2012, meets the most recent methodological requirements, in consonance with the main international regulatory agencies.
-
SBD agrees with restrictions to the wording of the label proposed by the RDC, like the prohibition of the term "sunblocker" or any other term that suggests total protection, which could lead the user to a false sensation of absolute security.
-
The harmonization process that is in effect, sponsored by ISO, is a breakthrough in the search for methods that meet the principles of universalization.
-
SBD recommends that dermatologists be careful when prescribing sunscreen, opting for those that follow ANVISA regulations.
CHAPTER 5
ORAL PHOTOPROTECTION
Solar exposure is capable of causing damage to the skin. Clinically, these alterations can be seen in photoexposed areas (deep wrinkles, increased skin fragility, solar melanoses, sagging) when compared to photoprotected skin areas.181181. Bouilly-Gauthier D, Jeannes C, Maubert Y, Duteil L, Queille-Roussel C, Piccardi N, et al. Benefits of a dietary supplement on UV-induced skin damage. Br J Dermatol. 2010;163:536-43.
Ultraviolet radiation (UVR) is responsible for acute and chronic cutaneous alterations. Acute alterations result from direct impact of UVR on biological chromophores such as DNA, leading to structural damage and release of proinflammatory cytokines, enzymes and immunosuppressive factors.182182. Petit-Frère C, Clingen PH, Grewe M, Krutmann J, Roza L, Arlett CF, et al. Induction of IL6 produc- tion by UV radiation in normal epidermal keratinocytes and in a human keratinocyte line is mediated by DNA damage. J Invest Dermatol. 1998;111:354-9.
183. Schwarz A, Schwarz T. Molecular determinants of UV-induced immunosuppression. Exp Dermatol. 2002;11:9-12.-184184. Rabe JH, Mamelak AJ, McElgunn PJ, Morison WL, Sauder DN. Photoaging: mechanisms and repair. J Am Acad Dermatol. 2006;55:1-19. Chronic alterations result from cumulative damage and cellular inability to repair, leading to photoaging and cancer. All these effects may be induced either by exposure to ultraviolet A (UVA) or ultraviolet B (UVB) radiation, due to direct modifications of cell structures or by generating reactive oxygen species (ROS).185185. Pillai S, Oresajo C, Hayward J. Ultraviolet radiation and skin aging: role of reactive oxygen species, inflammation and protease activation, and strategies for prevention of inflammation induced: a review. Int J Cosmet Sci. 2005;27:17-34.-186186. Biesalski HK, Berneburg M, Grune T, Kerscher M, Krutmann J, Raab W, et al. Hohenheimer Consensus Talk. Oxidative and premature skin ageing. Exp Dermatol. 2003;12 Suppl 3:3-15.
It is estimated that approximately 50% of the damage induced by UVR results from production of ROS, leading to molecular and cellular damage which will interfere with solar erythema, pigmentation and photodermatoses, in the short-term, and in the long-term with photocarcinogenesis and photoaging.187187. Bernstein EF, Brown DB, Schwartz MD, Kaidbey K, Ksenzenko SM. The polyhydroxy acid gluconolactone protects against ultraviolet radiation in an in vitro model of cutaneous photoaging. Dermatol Surg. 2004;30:189-95
Recent studies demonstrate that photoprotective measures are capable of preventing biological damage generated by suberythematogenic doses of UVR and deterioration of dermal tissues.188188. Seité S, Christiaens F, Bredoux C, Compan D, Zucchi H, Lombard D, et al. A broad-spectrum sunscreen prevents cumulative damage from repeated exposure to suberythe- mal solar ultraviolet radiation representative of temperate latitudes. J Eur Acad Dermatol Venereol. 2010;24:219-22.
According to Gilaberte and Gonzáles, the main current innovations in photoprotection are divided into two categories: 1) the introduction of new ingredients to traditional topical sunscreen, and 2) the use of oral formulations capable of delivering systemic photoprotection.189189. Gilaberte Y, González S. Update on Photoprotection Actas Dermosifiliogr. 2010;101:659-72.
According to reports in the literature, the following products listed in chart 6 may exert systemic photoprotection activity.189189. Gilaberte Y, González S. Update on Photoprotection Actas Dermosifiliogr. 2010;101:659-72.
The role of nutrition in the skin appearance has always been a topic of interest for scientists and physicians worldwide over the centuries. The skin is able to reflect the general state of health and show evidence of aging. The powerful antioxidant action of vitamins, carotenoids, tocopherols, flavonoids and a great variety of vegetable extracts, which have been used extensively by the industry in topical agents as well as in oral supplements, with the goal of extending youth and enhancing skin appearance, has been demonstrated. The main strategy of prevention against free radicals comes down to a healthy lifestyle (calorie restriction, body care and performing regular physical exercises) associated with conditions of low stress, balanced nutritional diet and food rich in antioxidants.190190. Schagen SK, Zampeli VA, Makrantonaki E, Zouboulis CC. Discovering the link between nutrition and skin aging. Dermatoendocrinol. 2012;4:298-307.
There is evidence that some substances, when administered orally, could exert a preventative action against UVR-induced cutaneous damage without causing adverse effects. The action mechanism is varied, acting in different phases of signalization, resulting in antioxidant, anti-inflammatory and immunomodulating action.189189. Gilaberte Y, González S. Update on Photoprotection Actas Dermosifiliogr. 2010;101:659-72.
Several substances of botanical origin, used as topical sunscreen, seem to present similar effectiveness when administered orally. Within this group alcaloids would be included, such as caffeine, Polypodium leucotomos extract, polyphenols and carotenoids.189189. Gilaberte Y, González S. Update on Photoprotection Actas Dermosifiliogr. 2010;101:659-72.
Oral photoprotection is a term used to designate the isolated use or a combination of several active ingredients which have demonstrated the capability of minimizing the damage caused by solar radiation in the skin.
Next, we will cover the main substances described in the literature which could present evidences of exerting oral photoprotecting activity.
It is important to emphasize that none of the substances that will be described can claim to replace the use of topical sunscreen, since none of them has the capability of preventing UVR penetration in the skin. To this day they are capable of acting, in some way, as coadjuvants in the photoprotection process.
VITAMINS
L-ascorbic acid (vitamin C)
Soluble in water, photosensitive and the most important antioxidant in the hydrophilic phase, it is not naturally synthesized by the human body and, therefore, its adequate intake is necessary in the diet and essential for good health. The main natural sources of vitamin C would be fresh fruit and vegetables, such as citrus fruit, gooseberry, rosehips, guava, chili or parsley. The stability of vitamin C molecule depends on its condition of aggregation and formulation. It can be used orally or topically to obtain beneficial results in the skin. Vitamin C is a cofactor for lysyl and prolyl hydroxylase, which stabilize the structure of the collagen triple helix.190190. Schagen SK, Zampeli VA, Makrantonaki E, Zouboulis CC. Discovering the link between nutrition and skin aging. Dermatoendocrinol. 2012;4:298-307.,191191. Draelos ZD. Nutrition and enhancing youthful- appearing skin. Clin Dermatol. 2010;28:400-8.
Topical ascorbic acid is used in a range of cosmetic products, such as whiteners, anti-aging and photoprotecting formulations. The use of vitamin C in topical products is difficult due to its quick reductive capability and the degradation that occurs in the presence of oxygen even before it is applied to the skin.192192. Makrantonaki E, Zouboulis C. Skin alterations and diseases in advanced age. Drug Discov Today Dis Mech. 2008;5:e153-62.
Protection from UVR by topical vitamin C has been described in the literature.191191. Draelos ZD. Nutrition and enhancing youthful- appearing skin. Clin Dermatol. 2010;28:400-8.,193193. Pinnell SR. Cutaneous photodamage, oxidative stress, and topical antioxidant protection. J Am Acad Dermatol. 2003;48:1-19. The idea behind sunscreen is to aggregate the filter protection to antioxidant action. However, the study of Wang et al. indicates that broader studies on formulations are necessary, for in many products the desired effects are not verified.194194. Wang SQ, Osterwalder U, Jung K. Ex vivo evaluation of radical sun protection factor in popular sunscreens with antioxidants. J Am Acad Dermatol. 2011;65:525-30.
Cutaneous protection only with the use of oral vitamin C is not proven by literature. Nevertheless some studies were performed with the combined use of vitamins C and E, described as follows.
Tocopherols (vitamin E)
The vitamin E complex corresponds to a group of 8 compounds called tocopherols. Tocopherol is a liposoluble antioxidant which links itself to membranes and is a scavenger of highly reactive oxygen species. Like vitamin C, it is a natural antioxidant, non-enzymatic and endogenous. Vitamin E acts synergically with vitamin C. When molecules activated by UVR oxidize cellular components, an induction of lipid peroxidation chain reaction in polyunsaturated fatty acid-rich membranes occurs. The antioxidant Dalpha-tocopherol is oxidized to tocoferoxyl radical, a process that can be regenerated by vitamin C.195195. Fryer MJ. Evidence for the photoprotective effects of vitamin E. Photochem Photobiol. 1993;58:304-12.,196196. Chan AC, Tran K, Raynor T, Ganz PR, Chow CK. Regeneration of vitamin E in human platelets. J Biol Chem. 1991;266:17290-5.
Besides ascorbic acid, glutathione and coenzyme Q10 can also recycle tocopherol. Great amounts of tocopherol are available in vegetables, vegetable oils, such as wheat germ oil, sunflower oil, safflower oil and seed, corn, and in some kinds of meat. Natural ingestion of vitamin E helps against collagen cross linking and lipid peroxidation, which are related with cutaneous aging. By means of the process described above, D-alpha-tocopherol is involved in the stabilization of cell membranes by oxidation inhibition of polyunsaturated fatty acids, like arachidonic acid of phospholipidic membranes.190190. Schagen SK, Zampeli VA, Makrantonaki E, Zouboulis CC. Discovering the link between nutrition and skin aging. Dermatoendocrinol. 2012;4:298-307.
Topical application of vitamin E is described as a way to reduce erythema, sunburn cells, induced UVB cutaneous damage and photocarcinogenesis in most published studies.192192. Makrantonaki E, Zouboulis C. Skin alterations and diseases in advanced age. Drug Discov Today Dis Mech. 2008;5:e153-62.
There are several clinical studies which tested the effects of tocopherol. Data may seem controversial, however high doses of oral vitamin E seem to affect the response to UVB in humans.197197. Scarmo S, Cartmel B, Lin H, Leffell DJ, Welch E, Bhosale P, et al. Significant correlations of dermal total carotenoids and dermal lycopene with their respective plasma levels in healthy adults. Arch Biochem Biophys. 2010;504:34-9.
Mireles-Rocha et al., in their study, compared the oral use of 1200 IU/day of alpha-tocopherol (group 1), 2g/day of vitamin C (group 2) and the combination of both (group 3) for one week. The results demonstrated an elevation of minimal erythemal dose of 60 to 65 mJ/cm2 in group 1 and 50 to 70 mJ/cm2 in group 3. There was no difference in group 3.198198. Mireles-Rocha H, Galindo I, Huerta M, Trujillo-Hernández B, Elizalde A, Cortés-Franco R. UVB photoprotection with antioxidants: effects of oral therapy with dalpha-tocopherol and ascorbic acid on the minimal erythema dose. Acta Derm Venereol. 2002;82:21-4.
In a 3-month-long study, Placzek et al. observed the effects of combination of ascorbic acid (vitamin C - 2g/day) with D-tocopherol (vitamin E - 1000 IU/day) administered orally to human volunteers with epidermal damage induced by UVB. The treatment was well tolerated and could be used in the prevention of deleterious effects of UVB radiation (formation of thymine dimers) and skin cancer, according to the authors.199199. Placzek M, Gaube S, Kerkmann U, Gilbertz KP, Herzinger T, Haen E, et al. Ultraviolet B-induced DNA damage in human epidermis is modified by the antioxidants ascorbic acid and D-alpha-tocopherol. J Invest Dermatol. 2005;124:304-7.
The treatment with oral combination of vitamin C and E enhances the photoprotecting effects if compared with monotherapy. The authors recommend that this synergistic interchange of several antioxidants must be considered in future research on cutaneous photoprotection.200200. Eberlein-König B, Ring J. Relevance of vitamins C and E in cutaneous photoprotection. J Cosmet Dermatol. 2005;4:4-9.
CAROTENOIDS
Carotenoids are vitamin A derivatives such as beta-carotene, astaxanthin, lycopene and retinol, which are highly effective antioxidants and have had their photoprotecting properties documented.201201. Ribaya-Mercado JD, Garmyn M, Gilchrest BA, Russell RM. Skin lycopene is destroyed preferentially over beta-carotene during ul- traviolet irradiation in humans. J Nutr. 1995;125:1854-9.
202. Sies H, Stahl W. Carotenoids and UV protection. Photochem Photobiol Sci. 2004;3:749-52.-203203. Sies H, Stahl W. Nutritional protection against skin damage from sunlight. Annu Rev Nutr. 2004;24:173-200. The findings of Scarmo et al. suggest that the human skin is relatively rich in lycopene and beta-carotene if compared to lutein and zeaxanthin, possibly reflecting the function of hydrocarbon in photoprotection of human skin.197197. Scarmo S, Cartmel B, Lin H, Leffell DJ, Welch E, Bhosale P, et al. Significant correlations of dermal total carotenoids and dermal lycopene with their respective plasma levels in healthy adults. Arch Biochem Biophys. 2010;504:34-9.
Beta-carotene
Beta-carotene is the main component of the carotenoid group, a natural dye which can be found in the diet. Some examples of foods rich in beta-carotene are fruits and vegetables such as carrot, pumpkin, sweet potato, mango and papaya.204204. Alaluf S, Heinrich U, Stahl W, Tronnier H, Wiseman S. Dietary carotenoids contribute to normal human skin color and UV photosensitivity. J Nutr. 2002;132:399-403.
Compared with other carotenoids, the main action of beta-carotene is its pro-vitamin A activity. It can be cleaved by enzyme BCM01 in two molecules of all-trans-retinol. There is no difference between natural beta-carotene and the chemically synthesized one. Furthermore, beta-carotene can also act as a lipidic free antiradical and singlet oxygen scavenger, as demonstrated in vitro.205205. Grune T, Lietz G, Palou A, Ross AC, Stahl W, Tang G, et al. Beta-carotene is an important vitamin A source for humans. J Nutr. 2010;140:2268S-2285S.
Beta-carotene is considered an endogenous photoprotector and its efficacy in the prevention of induced erythema formation has been demonstrated in several studies.202202. Sies H, Stahl W. Carotenoids and UV protection. Photochem Photobiol Sci. 2004;3:749-52.,203203. Sies H, Stahl W. Nutritional protection against skin damage from sunlight. Annu Rev Nutr. 2004;24:173-200.,206206. Köpcke W, Krutmann J. Protection from sunburn with beta-Carotene-a meta-analysis. Photochem Photobiol. 2008;84:284-8.,207207. Stahl W, Heinrich U, Jungmann H, Sies H, Tronnier H. Carotenoids and carotenoids plus vitamin E protect against ultraviolet light-induced erythema in humans. Am J Clin Nutr. 2000;71:795-8.
Systemic photoprotection action of beta-carotene depends on the dose and duration of treatment. In studies documenting action against UV-induced erythema, supplementation with carotenoids was performed with a duration of at least 7 weeks, with doses greater than 12mg/day.207207. Stahl W, Heinrich U, Jungmann H, Sies H, Tronnier H. Carotenoids and carotenoids plus vitamin E protect against ultraviolet light-induced erythema in humans. Am J Clin Nutr. 2000;71:795-8.
208. Mathews-Roth MM, Pathak MA, Parrish J, Fitzpatrick TB, Kass EH, Toda K, et al. A clinical trial of the effects of oral beta-carotene on the responses of human skin to solar radiation. J Invest Dermatol. 1972;59:349-53.
209. Lee J, Jiang S, Levine N, Watson RR. Carotenoid supplementation reduces erythema in human skin after simulated solar radiation exposure. Proc Soc Exp Biol Med. 2000;223:170-4.-210210. Heinrich U, Gärtner C, Wiebusch M, Eichler O, Sies H, Tronnier H, et al. Supplementation with beta- carotene or a similar amount of mixed carotenoids protects humans from UV-induced erythema. J Nutr. 2003;133:98-101.
In studies with a treatment period of only 3 to 4 weeks, the photoprotecting effects were not demonstrated.211211. Wolf C, Steiner A, Hönigsmann H. Do oral carotenoids protect human skin against ultraviolet ery- thema, psoralen phototoxicity, and ultraviolet-induced DNA damage? J Invest Dermatol. 1988;90:55-7.
Moreover, supplementation with beta-carotene may significantly reduce mitochondrial mutation in human dermal fibroblasts after UV radiation.212212. Eicker J, Kürten V, Wild S, Riss G, Goralczyk R, Krutmann J, et al. Betacarotene supplementation protects from photoaging-associated mitochondrial DNA mutation. Photochem Photobiol Sci. 2003;2:655-9.
Astaxanthin
Astaxanthin can be foind in microalgae, yeast, salmon, trout, shrimp, crayfish and crustaceans. It is biosynthesized by microalgae and phytoplanktons, which are eaten by zooplankton and crustaceans. They accumulate astaxanthin and are ingested by fish that obtain astaxanthin in the food chain.213213. Lorenz RT, Cysewski GR. Commercial potential for Haematococcus microalgae as a natural source of astaxanthin. Trends Biotechnol. 2000;18:160-7.
Astaxanthin has considerable potential and promising applications in human health and nutrition. A protecting potential against several diseases has been attributed to it.214214. Higuera-Ciapara I, Félix-Valenzuela L, Goycoolea FM. Astaxanthin: a review of its chemistry and applications. Crit Rev Food Sci Nutr. 2006;46:185-96.
The UV protecting action of algae extracts containing 14% of astaxanthins compared to synthetic astaxanthin was investigated. The authors report that pre-incubation with synthetic astaxanthin or with algae extract could prevent UVA induced alterations in activity of cellular superoxide dismutase and a decrease in the amount of glutathione in the cells.215215. Lyons NM, O'Brien NM. Modulatory effects of an algal extract containing astaxanthin on UVA-irradiated cells in culture. J Dermatol Sci. 2002;30:73-84.
In the study carried out by Câmera et al., the damage modulation related to UVA by astaxanthin, canthaxanthin and beta-carotene for photoprotection in human dermal fibroblasts was compared.216216. Camera E, Mastrofrancesco A, Fabbri C, Daubrawa F, Picardo M, Sies H, et al. Astaxanthin, canthaxan- thin and beta-carotene differently affect UVA-induced oxidative damage and expression of oxidative stress- responsive enzymes. Exp Dermatol. 2009;18:222-31.
Astaxanthin demonstrated a significant photoprotecting effect in fighting UVA-induced alterations in broad areas. Uptake of astaxanthin by fibroblasts was greater than by canthaxanthin and beta-carotene, leading to the belief that the effect of astaxanthin in photooxidative alterations was greater than that of other substances. A recent study of Suganuma et al. demonstrated that astaxanthin could interfere with the expression of elastase/neutral endopeptidase of cutaneous fibroblasts and with type 1 UVA-induced matrix metalloproteinases.217217. Suganuma K, Nakajima H, Ohtsuki M, Imokawa G. Astaxanthin attenuates the UVA-induced up-regula- tion of matrix-metalloproteinase-1 and skin fibroblast elastase in human dermal fibroblasts. J Dermatol Sci. 2010;58:136-42. Both studies suggest that the effects of UVA radiation, such as skin sagging and formation of creases can be prevented or at least minimized by oral or topical administration of astaxanthins.217217. Suganuma K, Nakajima H, Ohtsuki M, Imokawa G. Astaxanthin attenuates the UVA-induced up-regula- tion of matrix-metalloproteinase-1 and skin fibroblast elastase in human dermal fibroblasts. J Dermatol Sci. 2010;58:136-42.
Lycopene
Lycopene is a bright red carotenoid pigment found in tomatoes and other red fruits besides vegetables and red carrots, watermelons and papayas, but not in strawberries and cherries. In spite of lycopene being a carotene chemically, it does not have vitamin A activity. Beta-carotene and lycopene are the main carotenoids present in the blood and tissues, capable of modulating cutaneous properties when ingested as a food supplement or diet products. Even though it cannot be compared to solar filters, there is evidence that it can protect the skin against solar erythemas, enhancing cutaneous defense against UVR damage.218218. Stahl W, Heinrich U, Aust O, Tronnier H, Sies H. Lycopene-rich products and dietary photoprotection. Photochem Photobiol Sci. 2006;5:238-42.
A study demonstrated that the concentration of lycopene in the plasma and in tissues can be compared to or superior to beta-carotene. When the skin is exposed to oxidative stress produced by UVR, there is greater destruction of lycopene than beta-carotene, suggesting the role of lycopene in mitigating the oxidative damage.201201. Ribaya-Mercado JD, Garmyn M, Gilchrest BA, Russell RM. Skin lycopene is destroyed preferentially over beta-carotene during ul- traviolet irradiation in humans. J Nutr. 1995;125:1854-9.
In 2001, Stahl et al. studied the benefits of ingesting 40mg of tomato paste per day (16mg of lycopene), demonstrating significant reduction of erythema induced by ultraviolet radiation.218218. Stahl W, Heinrich U, Aust O, Tronnier H, Sies H. Lycopene-rich products and dietary photoprotection. Photochem Photobiol Sci. 2006;5:238-42.
Lutein
Lutein is a xanthophyllic carotenoid with potent antioxidant activity. In an animal model, oral supplementation of lutein was able to accumulate in the skin, diminishing the generation of free radicals after ultraviolet exposure.219219. Lee EH, Faulhaber D, Hanson KM, Ding W, Peters S, Kodali S, et al. Dietary lutein reduces ultraviolet radiation-induced inflammation and immunosuppression. J Invest Dermatol. 2004;122:510-7.
In 2007, a comparative study on the use of lutein associated with zeaxanthin in topical, oral or both forms was conducted, demonstrating that all groups presented an improvement of cutaneous elasticity; however, the group which combined oral and topical treatment presented a synergistic effect with higher degree of antioxidant action and enhancement of cutaneous hydration. Studies have been conducted aiming at demonstrating other possible cutaneous effects of lutein, such as: cell proliferation reduction, anti-inflammatory and immunosuppressing activity and inhibition of photocarcinogenesis.220220. Palombo P, Fabrizi G, Ruocco V, Ruocco E, Fluhr J, Roberts R, et al. Beneficial long-term effects of combined oral/topical antioxidant treatment with the carotenoids lutein and zeaxanthin on human skin: a double-blind, placebo-controlled study. Skin Pharmacol Physiol. 2007;20:199-210.
POLYPHENOLS
Polyphenols have attracted the attention of researchers on aging in the last decade, mainly for their antioxidant features, being ingested in great amounts in diets and by the increasing number of studies demonstrating their possible participation in preventing several diseases associated with oxidative stress, like cancer, cardiovascular and neurodegenerative diseases.221221. Manach C, Scalbert A, Morand C, Rémésy C, Jiménez L. Polyphenols: food sources and bioavailability. Am J Clin Nutr. 2004;79:727-47.
Their daily intake can be up to 1g/day, which is much higher than any other class of phytochemicals or antioxidants. Polyphenols are found mainly in fruits and plant-derived beverages such as fruit juice, coffee, tea and red wine. Vegetables, cereals, chocolate and legumes are also sources of polyphenols.222222. Scalbert A, Williamson G. Dietary intake and bioavail- ability of polyphenols. J Nutr. 2000;130:2073S-85S.,223223. Scalbert A, Johnson IT, Saltmarsh M. Polyphenols: antioxidants and beyond. Am J Clin Nutr. 2005;81:215S-217S.
Thousands of molecules containing the polyphenol structure have been identified in plants involved in the defense against UV radiation or pathogen aggression. Depending on the number of phenolic rings and the manner in which they are interlinked, polyphenols can be divided into different functional groups, such as phenolic acids, flavonoids, stilbene (resveratrol) and lignans (linseed).221221. Manach C, Scalbert A, Morand C, Rémésy C, Jiménez L. Polyphenols: food sources and bioavailability. Am J Clin Nutr. 2004;79:727-47. The flavonoids are also divided into flavones, isoflavones and flavonones, each with a slight difference in their chemical structure.191191. Draelos ZD. Nutrition and enhancing youthful- appearing skin. Clin Dermatol. 2010;28:400-8.
Laboratory studies of different polyphenols, such as green tea, grape seed, proanthocyanidins, resveratrol, silymarin, genistein, evaluated in animal models about cutaneous inflammation, oxidative stress and ultraviolet-induced DNA damage, suggest that these polyphenols combined with the protection of solar filters present the ability of protecting the skin against adverse effects from UV radiation, including the risk for cutaneous cancer.224224. Nichols JA, Katiyar SK. Skin photoprotection by natural polyphenols: anti-inflammatory, antioxidant and DNA repair mechanisms. Arch Dermatol Res. 2010;302:71-83.
The adjacent action mechanism of polyphenols has been discussed in the last decades. One of the strongest theories states that polyphenol cellular response occurs by direct interaction with receptors or enzymes involved in signal transduction, resulting in the modification of redox status of cells, which may trigger a series of redox-dependent reactions.225225. Halliwell B, Rafter J, Jenner A. Health promotion by flavonoids, tocopherols, tocotrienols, and other phenols: direct or indirect effects? Antioxidant or not? Am J Clin Nutr. 2005;81:268S-76S.,226226. Moskaug JØ, Carlsen H, Myhrstad MC, Blomhoff R. Polyphenols and glutathione synthesis regula- tion. Am J Clin Nutr. 2005;81:277S-283S.
As antioxidants, polyphenols may enhance cell survival, while pro-oxidants may induce apoptosis and prevent tumor growth.223223. Scalbert A, Johnson IT, Saltmarsh M. Polyphenols: antioxidants and beyond. Am J Clin Nutr. 2005;81:215S-217S.,227227. Lambert JD, Hong J, Yang GY, Liao J, Yang CS. Inhibition of carcinogenesis by polyphenols: evidence from laboratory investigations. Am J Clin Nutr. 2005;81:284S-291S.
Studies in animals demonstrated that continuous oral administration of epigallocatechin-3-gallate increases minimal erythemal dose and decreases photoaging and photocarcinogenesis induced by UVB radiation.228228. Jeon HY, Kim JK, Kim WG, Lee SJ. Effects of oral epigallocatechin gallate supplementation on the minimal eruthema dose and UV-induced skin damage. Skin Pharmacol Physiol. 2009;22:137-41.
Oral genistein also seems to diminish UVB-induced carcinogenesis in animal models.229229. Wei H, Saladi R, Lu Y, Wang Y, Palep SR, Moore J, et al. Isoflavone genistein: photoprotection and clinical implications in dermatology. J Nutr. 2003;133:3811S-3819S.
Oral administration of quercetin diminishes the production of oxidative stress in animals exposed to UVA and UVB radiation.230230. Erden Inal M, Kahraman A. The protective effect of flavonol quercetin against ultraviolet A induced oxidative stress in rats. Toxicology. 2000;154:21-9.,231231. Erden Inal M, Kahraman A, Köken T. Beneficial effects os quercetin on oxidative stress induced by ultraviolet A. Clin Exp Dermatol. 2001;26:536-9.
Pycnogenol is a source of flavonoids, extracted from maritime pine bark (Frances Pinus pinaster). It has attracted attention due to its potent antioxidant action, with its demonstrated capability of modulating UV-induced erythema and expression of nuclearkappa-B factor.232232. Saliou C, Rimbach G, Moini H, McLaughlin L, Hosseini S, Lee J, et al. solar ultraviolet-induced erythema in human skin and nuclear factor-kappa-B-dependent gene expression in keratinocytes are modulated by a French maritime pine bark extract. Free Radic Biol Med. 2001;30:154-60.
PROBIOTICS
The term probiotics is defined as "live microorganisms which, when consumed in adequate amounts, confer a beneficial health effect on the host".233233. Fuller R. Probiotics in man and animals. J Appl Bacteriol. 1989;66:365-78. The main probiotics used by humans and animals are enterococci, lactobacilli and bifidobacteria, which are part of the natural flora of the intestinal tract. Prebiotics are nonviable food components, which confer healthy benefits to hosts, associated with microbiota modulation.
Clinical studies using bacterial probiotics (Lactobacillus johnsoniiNCC 533) to modulate homeostasis of the cutaneous immune system, altered due to UV exposure by solar simulator in humans, suggest that certain probiotics may help in preserving cutaneous homeostasis by modulating the skin immune system.234234. Guéniche A, Benyacoub J, Buetler TM, Smola H, Blum S. Supplementation with oral probiotic bac- teria maintains cutaneous immune homeostasis after UV exposure. Eur J Dermatol. 2006;16:511-7.
235. Peguet-Navarro J, Dezutter-Dambuyant C, Buetler T, Leclaire J, Smola H, Blum S, et al. Supplementation with oral probiotic bacteria protects human cutaneous immune homeostasis after UV exposure-double blind, randomized placebo controlled clinical trial. Eur J Dermatol. 2008;18:504-11.-236236. Guéniche A, Philippe D, Bastien P, Blum S, Buyukpamukcu E, Castiel-Higounenc I. Probiotics for photoprotection. Dermatoendocrinol. 2009;1:275-9.
This specific strain of Lactobacillus johnsonii associated with carotenoids (β-carotene: 4.8 mg/day; lycopene: 2 mg) was able to prevent the reduction in density of UV-induced Langerhans cells in human volunteers.181181. Bouilly-Gauthier D, Jeannes C, Maubert Y, Duteil L, Queille-Roussel C, Piccardi N, et al. Benefits of a dietary supplement on UV-induced skin damage. Br J Dermatol. 2010;163:536-43.
COMBINATION OF ANTIOXIDANTS
Morganti, in a randomized, double-blind, placebo controlled study describes the comparison of the treatment with an antioxidant complex (ascorbic acid, tocopherol, alpha-lipoic acid, melatonin, emblica), topical and/or systemic, for 8 weeks in 30 volunteers. An in vitro study was also performed (induced ROS by irradiating leukocytes with UVB radiation). He concludes that both seem to act as good sunscreen.237237. Morganti P, Bruno C, Guarneri F, Cardillo A, Del Ciotto P, Valenzano F. Role of topical and nutritional supplement to modify the oxidative stress. Int J Cosmet Sci. 2002;24:331-9.
Greul et al. described that the repeated use of a combination of antioxidants such as carotenoids (beta-carotene and lycopene), vitamins C and E, selenium and proanthocyanidins could reduce UVB-induced erythema and the expression of type 1 and type 9 matrix metalloproteinases.238238. Greul AK, Grundmann JU, Heinrich F, Pfitzner I, Bernhardt J, Ambach A, et al. Photoprotection of UV-irradiated human skin: an antioxidative combination of vitamins E and C, carotenoids, selenium and proanthocyanidins. Skin Pharmacol Appl Skin Physiol. 2002;15:307-15.
The combination of vitamin C, vitamin E, pycnogenol and primrose oil was studied in an animal model under chronic UVB radiation exposure. The study demonstrated that the complex would be capable of inhibiting the expression of matrix metalloproteinase and increase the synthesis of collagen, reducing wrinkle formation.239239. Cho HS, Lee MH, Lee JW, No KO, Park SK, Lee HS, et al. Anti-wrinkling effects of the mixture of vitamin C, vitamin E, pycnogenol and evening primrose oil, and molecular mechanisms on hairless mouse skin caused by chronic ultraviolet B irradiation. Photodermatol Photoimmunol Photomed. 2007;23:155-62.
Special attention has been given to complexes containing antioxidants, however choosing active ingredients, how to combine them and their doses still remain a challenge, so further studies are necessary.240240. Rona C, Berardesca E. Aging skin and food supplements: the myth and the truth. Clin Dermatol. 2008;26:641-647.
ESSENTIAL FATTY ACIDS (vitamin F)
Essential fatty acids are long-chain polyunsaturated fatty acids derived from linolenic (omega-3), linoleic (omega-6) and oleic acids. They are not produced by the human body and must be consumed in the daily diet. They are present in foods such as fish, linseed, hemp oil, soybean oil, canola oil, chia seed, sunflower seed, salmon and tuna.190190. Schagen SK, Zampeli VA, Makrantonaki E, Zouboulis CC. Discovering the link between nutrition and skin aging. Dermatoendocrinol. 2012;4:298-307.
In a study which evaluated fish oil action over UV-induced prostaglandin metabolism, 13 patients with polymorphous light eruption received supplementation for 3 months. The authors demonstrated the reduction of UV-induced inflammation, possibly due to decreasing levels of prostaglandin E.241241. Rhodes LE, Durham BH, Fraser WD, Friedmann PS. Dietary fish oil reduces basal and ultraviolet B-generated PGE2 levels in skin and increases the threshold to provocation of polymorphic light eruption. J Invest Dermatol. 1995;105:532-5.
Oral administration of an antioxidant group containing vitamin C, vitamin E, pycnogenol and primrose oil inhibited significantly the formation of wrinkles caused by chronic UVB irradiation through inhibition of UVB-induced metalloproteinases.239239. Cho HS, Lee MH, Lee JW, No KO, Park SK, Lee HS, et al. Anti-wrinkling effects of the mixture of vitamin C, vitamin E, pycnogenol and evening primrose oil, and molecular mechanisms on hairless mouse skin caused by chronic ultraviolet B irradiation. Photodermatol Photoimmunol Photomed. 2007;23:155-62.
POLYPODIUM LEUCOTOMOS
Polypodium leucotomos is a botanic extract, originated from a tropical fern which grows in areas of Central and South America, more frequently in altitudes from 700 to 1,300 meters. It has been described by botanical expeditions since the 18th century and was used by the natives in infusions due to its antiphlogistic and antitumoral action.242242. Gonzalez S, Pathak MA. Inhibition of ultraviolet-induced formation of reactive oxygen species, lipid peroxidation, erythema and skin photosemsitization by Polipodium leucotomos. Photodermatol Photoimmunol Photomed. 1996;12:45-56.
243. Gonzales S, Pathak MA, Cuevas J, Villarrubia VG, Fitzpatrick TB. Topical or oral administration with an extract of Polypodium leucomotos prevents acute sunburn and psoralen-induced phototoxic reactions as weel as depletion of Langerhans cells in human skin. Photodermatol Photoimmunol Photomed. 1997;13:50-60.-244244. Gonzalez S, Gilaberte Y, Philips N, Juarranz A. Fernblock, a nutriceutical with photoprotective properties and potential preventive agent for skin photoaging and photoinduced skin cancers. Int J Mol Sci. 2011;12:8466-75.
As of the 90's, studies with the P. leucotomos extract began to appear, conducted by Harvard teachers Fitzpatrick, Phatak e Gonzáles. It contains several pharmacological markers, among them phenolic derivatives, such as chlorogenic acid, vanillic acid, caffeic acid and ferulic acid.244244. Gonzalez S, Gilaberte Y, Philips N, Juarranz A. Fernblock, a nutriceutical with photoprotective properties and potential preventive agent for skin photoaging and photoinduced skin cancers. Int J Mol Sci. 2011;12:8466-75.,245245. Garcia F, Pivel JP, Guerrero A, Brieva A, Martinez-Alcazar MP, Caamano-Somoza M, et al. Phenolic components and antioxidant activity of Fernblock, an aqueous extract of the aerial parts of the fern Polypodium leucotomos. Methods Find Exp Clin Pharmacol. 2006;28:157-60.
Since then, a series of scientific studies was published in the literature, demonstrating the several action mechanisms of this phytoextract: antioxidant action, immunoprotecting action, DNA protection and reorganization of skin architecture.244244. Gonzalez S, Gilaberte Y, Philips N, Juarranz A. Fernblock, a nutriceutical with photoprotective properties and potential preventive agent for skin photoaging and photoinduced skin cancers. Int J Mol Sci. 2011;12:8466-75.
245. Garcia F, Pivel JP, Guerrero A, Brieva A, Martinez-Alcazar MP, Caamano-Somoza M, et al. Phenolic components and antioxidant activity of Fernblock, an aqueous extract of the aerial parts of the fern Polypodium leucotomos. Methods Find Exp Clin Pharmacol. 2006;28:157-60.
246. Middelkamp-Hup MA, Pathak MA, Parrado C, Garcia-Caballero T, Rius-Díaz F, Fitzpatrick T, et al. Orally administered Polypodium leucomotos extract decreases psoralen-UVA-induced phototoxicity, pigmentation, and damage of human skin. J Am Acad Dermatol 2004;50:41-9.
247. Middelkamp-Hup MA, Pathak MA, Parrado C, Goukassian D, Rius-DÍaz F, Mihm MC, et al. Oral polypodium leucomotos extract decreases ultraviolet- induced damage of human skin. J Am Acad Dermatol. 2004;51:910-8.
248. Capote R, Alonso-Lebrero JL, García F, Brieva A, Pivel JP, González S. Polypodium leucotomos extract inhibits trans-urocanic acid photoisomerization and photodecomposition. J Photochem Photobiol B. 2006;82:173-179.-249249. Alonso-Lebrero JL, Domínguez-Jiménez C, Tejedor R, Brieva A, Pivel JP. Photoprotective properties of a hydrophilic extract of the fern Polypodium leucotomos on human skin cells. J Photochem Photobiol B. 2003;70:31-7.
In 1996, the antioxidant action of Polypodium leucotomos could be demonstrated through its capability of reduction of superoxide anion (55%), lipid per-oxidation (50%) and singlet oxygen (10%). More recently, the ability of caffeic acid and ferulic acid to inhibit the lipid peroxidation chain was demonstrated. Ferulic acid was also shown to be a potent UV photons absorber.242242. Gonzalez S, Pathak MA. Inhibition of ultraviolet-induced formation of reactive oxygen species, lipid peroxidation, erythema and skin photosemsitization by Polipodium leucotomos. Photodermatol Photoimmunol Photomed. 1996;12:45-56.
243. Gonzales S, Pathak MA, Cuevas J, Villarrubia VG, Fitzpatrick TB. Topical or oral administration with an extract of Polypodium leucomotos prevents acute sunburn and psoralen-induced phototoxic reactions as weel as depletion of Langerhans cells in human skin. Photodermatol Photoimmunol Photomed. 1997;13:50-60.-244244. Gonzalez S, Gilaberte Y, Philips N, Juarranz A. Fernblock, a nutriceutical with photoprotective properties and potential preventive agent for skin photoaging and photoinduced skin cancers. Int J Mol Sci. 2011;12:8466-75.
In 2004, a study with 10 volunteers demonstrated that the presence of Polypodium leucotomos was capable of decreasing the depletion of Langerhans cells. Its inhibiting action in the photoisomerization of urocanic acid was also evaluated, demonstrating its immunomodulatory action.246246. Middelkamp-Hup MA, Pathak MA, Parrado C, Garcia-Caballero T, Rius-Díaz F, Fitzpatrick T, et al. Orally administered Polypodium leucomotos extract decreases psoralen-UVA-induced phototoxicity, pigmentation, and damage of human skin. J Am Acad Dermatol 2004;50:41-9.,247247. Middelkamp-Hup MA, Pathak MA, Parrado C, Goukassian D, Rius-DÍaz F, Mihm MC, et al. Oral polypodium leucomotos extract decreases ultraviolet- induced damage of human skin. J Am Acad Dermatol. 2004;51:910-8.
The capability of inhibiting the formation of sunburn cells and the formation of thymine dimers revealed the DNA protection potential exerted by Polypodium leucotomos. A study done with a culture of fibroplasts and keratinocytes suggested that Polypodium leucotomos would have a protecting effect over fibroblasts.249249. Alonso-Lebrero JL, Domínguez-Jiménez C, Tejedor R, Brieva A, Pivel JP. Photoprotective properties of a hydrophilic extract of the fern Polypodium leucotomos on human skin cells. J Photochem Photobiol B. 2003;70:31-7.
Based on the action mechanisms described, several clinical indications have been employed for its utilization, such as reduction of solar erythema, phototherapy erythema and polymorphous light eruption. It has also been indicated as a coadjuvant treatment for diseases like vitiligo, psoriasis and melasma.244244. Gonzalez S, Gilaberte Y, Philips N, Juarranz A. Fernblock, a nutriceutical with photoprotective properties and potential preventive agent for skin photoaging and photoinduced skin cancers. Int J Mol Sci. 2011;12:8466-75.,250250. Caccialanza M, Recalcati S, Piccinno R. Oral polypodium leucotomos extract photoprotective activity in 57 patients with idiopathic photodermatoses. G Ital Dermatol Venereol. 2011;146:85-7.,251251. Ahmed AM, Lopez I, Perese F, Vasquez R, Hynan LS, Chong B, Pandya AG. A Randomized, Double-Blinded, Placebo-Controlled Trial of Oral Polypodium leucotomos Extract as an Adjunct to Sunscreen in the Treatment of Melasma. JAMA Dermatol. 2013;149:981-3.
Its plasma peak is 2 hours and its half-life 6 hours, with its greatest effect happening between 2 to 4 hours after ingestion. Its dose varies from 1 to 5 tablets (250 mg), depending on skin involvement and degree of solar exposure.
OTHER SUBSTANCES MENTIONED IN THE LITERATURE
Chocolate - cocoa beans are rich in polyphenols (catechins, epicatechins, and procyanidins) and known for their antioxidant properties; however, great part of these properties are lost during the manufacturing process of chocolate.252252. Andrés-Lacueva C, Monagas M, Khan N, Izquierdo-Pulido M, Urpi-Sarda M, Permanyer J, et al. Flavanol and flavonol contents of cocoa powder products: influence of the manufacturing process. J Agric Food Chem. 2008;56:3111-7. A study published in 2009 described that the daily consumption of chocolate, especially processed so as to preserve its flavonoids, would be capable of doubling the minimal erythemal dose when compared to a control group that consumed conventional dark chocolate.253253. Williams S, Tamburic S, Lally C. Eating chocolate can significantly protect the skin from UV light. J Cosmet Dermatol. 2009;8:169-73.
Caffeine - some epidemiological studies corroborate experimental evidences that caffeine consumption would have a protective action against skin cancer.254254. Abel E, Hendrix S, McNeelyS, Johnson K, Rosenberg C, Mossavar-Rahmani Y, et al. Daily coffee consumption and prevalence of nonmelanoma skin câncer in Caucasian women. Eur J Cancer Prev. 2007;16:446-52. Experimentally, both topical and oral caffeine promote apoptosis of keratinocytes irradiated by UVB, suggesting its action in the prevention of photocarcinogenesis.255255. Kerzendorfer C, O'Driscoll M. UV-B and caffeine: inhibiting the DNA damage response to protect against the adverse effects of UV-B. J Invest Dermatol. 2009;129:1611-3.
Acetylsalicylic acid, indomethacin and ibuprofen - the efficacy of the use of non-hormonal anti-inflammatory drugs in the treatment of sunburns has been postulated, however it still lacks a proper evaluation in randomized trials. Few observational studies report a reduction of post-UVB irradiation erythema, if started before or immediately after irradiation.256256. Edwards EK Jr, Horwitz SN, Frost P. Reduction of the erythema response to ultraviolet light by nonsteroidal antiinflammatory agents. Arch Dermatol Res. 1982;272:263-7.
NEW STRATEGIES OF SYSTEMIC PHOTOPROTECTION
New systemic substances that enhance photoprotection measures have been studied and melanin stimulators stand out in this field. Tanning is the main physiological photoprotecting response of the skin. Tanned skin promotes SPF between 2 and 4, reducing photoinduced DNA damage. Thus it is believed that melanin stimulation without solar exposure may reduce this damage.189189. Gilaberte Y, González S. Update on Photoprotection Actas Dermosifiliogr. 2010;101:659-72.
The analogues of the alpha-melanocyte stimulating hormone (α-MSH) can be used for stimulation of melanogenesis. Three fragments (melanotan I, II and III) demonstrated in vitro agonist action to melanocortin-1 receptor and the capability of stimulating melanogenesis.257257. Abdel-Malek Z, Ruwe A, Kavanagh-Starner R, Kadekaro AL, Swope V, Haskell-Luevano C, et al. Alpha-MSH tripeptide analogs activate the melanocortin 1 receptor and reduce UV-induced DNA damage in human melanocytes. Pigment Cell Melanoma Res. 2009;22:635-44.Melanotan I, administered in the dose of 20 mg, twice daily, for 60 days, demonstrated an increase in tolerance to solar exposure and a reduction of adverse effects in patients who carry erythropoietic protoporphyria.258258. Harms J, Lautenschlager S, Minder C, Minder E. An Alpha-melanocyte-stimulating hormone analogue in erytropoietic protoporphyria. N Eng J Med. 2009;360:306-7.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Oral use products may be available for prescription by dermatologists to prevent photoinduced skin damage.
-
The term oral photoprotection is not the most adequate, for it generates confusion with the action mechanism of topical sunscreen, completely distinct from the action of oral use products.
-
SBD suggests the name Solar nutraceuticals or Solar Nutricosmetics as an alternative to the name "oral photoprotector".
-
These products must not be used as a guarantee of protection against solar exposure, for they are not substitutes for topical sunscreen or mechanical protection. There is no evidence that these substances have the capability of preventing UVR from penetrating the skin.
-
The recommendation for use of these products must be made by a dermatologist, guiding the selection of the most adequate active ingredients, dosage and usage time, always according to the needs and characteristics of the patient.
CHAPTER 6
MECHANICAL OR OTHER PHOTOPROTECTION MEANS
The use of photoprotective measures capable of offering a physical or mechanical barrier to solar radiation, avoiding its incidence on the skin, may be named mechanical photoprotection.
Among the mechanical photoprotection measures, we can include the use of clothing, hats, sunglasses, natural or artificial coverage and glass, as we will see in the next items.
Photoprotection through the use of clothing
Photoprotection by means of clothing and hats is the oldest, most common and easiest way to be achieved and should be divulged as excellent protection against UVR (ultraviolet radiation).259259. Gies P. Photoprotection by clothing. Photodermatol Photoimmunol Photomed. 2007;23:264-74.
260. Morison WL. Photoprotection by clothing. Dermatol Ther. 2003:16:16-22.-261261. Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.
The use of clothing as a sun barrier is secular knowledge and may be proven by merely observing drawings from the time of old Egyptian and Medo-Persian civilizations, in which socially privileged people wisely covered themselves with clothing and head ornaments, which protected them from UVR and conferred them status. These habits lasted until the industrial revolution and the beginning of the 20th century, when the cult of tanned skin as a symbol of health and beauty was established and ever larger skin areas were exposed to the sun.259259. Gies P. Photoprotection by clothing. Photodermatol Photoimmunol Photomed. 2007;23:264-74.
The use of clothes and hats as UVR protection factors should be considered a first-line choice for protection against UVA and especially UVB.262262. Palm M, Donoghue M. Uptade on photoprotection. Dermatologic Therapy. 2007;20;360-376.
Among the advantages of the use of clothes, safety and the certainty of uniformity and continuity of offered protection should be emphasized. It starts immediately upon wearing them, without the need for a period of solar pre-exposure, and continues if one remains dressed, as opposed to solar filters, which require some waiting time and reapplications. Clothing is practical in several moments and situations.
Another interesting factor is the low economic investment required, when compared with other forms of protection. The disadvantage is that only the area covered by cloth is protected, and this fact becomes relevant in a country where people tend to diminish the size of clothes during summer, mainly in recreational and sports activities performed outdoors, like in Brazilian beaches.263263. Wang SQ, Balagula Y, Osterwalder U. Photoprotection: a review of the current and future technologies. Dermatol Ther. 2010;23:31-47.
In recent years, interest has grown over the importance of clothes as a protective barrier against UVR in scientific circles, mainly in special situations, such as during childhood, when early protection is paramount in the prevention of cancer. This viewpoint was reinforced by some studies, like one carried out with children from nurseries in Germany, who presented reduction of melanocytic lesions proportionally to greater use of clothes.264264. Ghazi S, Couteau C, Paparis E, Coiffard LJM. Interest of external photoprotection by means of clothing and sunscreen products in young children. J Eur Acad Dermatol Venereol. 2012;26:1026-30.
265. Criado P, Melo J, Oliveira Z N. Topical photoprotection in childhood and adolescence. J Pediatr. 2012;88:203-10.-266266. Bauer J, Büttner P, Wiecker TS, Luther H, Garbe C. Effect of Sunscreen and Clothing the Nunber of Melanocitic Nevi in 1812 germa Children Attendin Day. Am J Epidemiol. 2005;161:620-7. In countries such as Australia, where educational campaigns about children wearing more clothes have been promoted for several years, the search for adequate clothing for outdoor activities by the parents has become very popular, especially on beaches.265265. Criado P, Melo J, Oliveira Z N. Topical photoprotection in childhood and adolescence. J Pediatr. 2012;88:203-10.
In several countries advances have already been made for normatization of adequate uniforms for workers in risk situations, like those who exert their activities outdoors (construction workers, healthcare agents, postmen, etc.) or those exposed to artificial radiation sources (welders).267267. Gambichler T, Laperre J, Hoffmann K. The European standard for sun-protective clothing : EN 13758. J Eur Acad Dermatol Venereol. 2006;20:125-130.
268. Kütting B, Drexler H. UV-induced skin cancer at workplace and evidence-based prevention. Int Arch Occup Environ Health. 2010;83:843-54.
269. Bauer A, Diepgen TL, Schmitt J. Is occupational solar ultraviolet irradiation a relevant risk factor for basal cell carcinoma? A systematic review and meta-analysis of the epidemiological literature. Br J Dermatol. 2011;165:612-25.-270270. Adam J. Sun-protective clothing. J Cutan Med Surg. 1998;3:50-3.
The tendency of these campaigns is to extend and emphasize the importance of wearing adequate clothes, especially in moments of leisure, and increase the concern about the issue for the group of patients with photosensitivity disorders.259259. Gies P. Photoprotection by clothing. Photodermatol Photoimmunol Photomed. 2007;23:264-74.,262262. Palm M, Donoghue M. Uptade on photoprotection. Dermatologic Therapy. 2007;20;360-376.,271271. Purim K, Leite N. Fotoproteção e exercício físico. Rev Bras Med Esporte. 2010;16-3.
Clothes block UVR in different degrees, depending on the material they are made of, in addition to factors related to their use.
Among the factors that increase the protection offered by clothes is the composition of synthetic fabrics (polyester and nylon) and weave density. The thicker, more closely knit and compacted the weave is, the greater the photoprotection will be, which is the most important aspect to determine a high SPF. In practice, this idea is applied when choosing closely knit, heavy and dense fabrics for outdoor workers' uniforms, usually made of denim, that in spite of having cotton in its composition, provides good protection due to its very dense weave.
Dark colors, such as black, dark blue, dark red and dark green, have high concentration of dyes and absorb more UVR than light tones, like white, beige and pastel colors, even with the same fabric weave and composition. Some fabrics, like cotton and linen, when washed for the first time may shrink and close the spaces between their threads, which would increase protection. However, clothes that are washed and worn too often are prone to protect less, for the weave becomes loose and open.
Factors that may diminish the protective capability against UVR are open and thin weave, very frequent with natural fibers like cotton, natural silks and wool; we also have, as a factor that decreases protection, humidity and stretching of products because fabrics that are moistened and submitted to tension offer poorer protection.
Chart 7 presents the main factors that interfere with the protective capability of fabrics.261261. Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.
More recently, fabrics produced with threads treated with ultraviolet filters have been offered, ensuring a superior protection and reducing the influence of environmental factors mentioned above in the protection offered by clothing.
Another alternative is the introduction of additives when washing clothes, together with soap and softeners, offering an increment in protection to the washed fabric.259259. Gies P. Photoprotection by clothing. Photodermatol Photoimmunol Photomed. 2007;23:264-74.,261261. Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.
262. Palm M, Donoghue M. Uptade on photoprotection. Dermatologic Therapy. 2007;20;360-376.-263263. Wang SQ, Balagula Y, Osterwalder U. Photoprotection: a review of the current and future technologies. Dermatol Ther. 2010;23:31-47.,271271. Purim K, Leite N. Fotoproteção e exercício físico. Rev Bras Med Esporte. 2010;16-3.
272. Alves LM, Aegerter MA, Hata K. In vitro determination of sun protection factor (SPF) of solar moderators. An Bras Dermatol. 1991;66:313-9.
273. Mansur JS, Breder MNR, Mansur MCA, Azulay RD. Determination of sun protecting factor in human beings and by spectrophotometry: comparison between of the two methods. An Bras Dermatol. 1986;61:167-72.-274274. Balogh TS, Velasco MVA, Pedriali CA, Kaneko TM, Baby AR. Proteção à radiação ultravioleta: recursos disponíveis na atualidade em fotoproteção. An Bras Dermatol. 2011;86:732-42.
To quantify the protection capability of a given article of clothing, in 1996, the Australian Radiation Protection and Nuclear Safety Agency (ARPANSA) presented the first regulation regarding the UV protection power offered by clothing - the norm AS/NZS4399:1996.275275. Australian/New Zealand Standard® [Internet]. AS/NZS 4399:1996. Sun protective clothing-Evaluation and classification. [cited 2014 Oct 30]. Available from: http://www.saiglobal.com/pdftemp/previews/osh/as/as4000/4300/4399.pdf
http://www.saiglobal.com/pdftemp/preview...
The protection capability is based on radiation transmission by the cloth, obtaining the ultraviolet protection factor (UPF).
According to the method proposed by ARPANSA, the UPF is determined through a spectrophotometric technique, in which the transmission of energy of the cloth evaluated between wavelengths which comprise the UV range (290-400 nm) is calculated.262262. Palm M, Donoghue M. Uptade on photoprotection. Dermatologic Therapy. 2007;20;360-376.,263263. Wang SQ, Balagula Y, Osterwalder U. Photoprotection: a review of the current and future technologies. Dermatol Ther. 2010;23:31-47.,275275. Australian/New Zealand Standard® [Internet]. AS/NZS 4399:1996. Sun protective clothing-Evaluation and classification. [cited 2014 Oct 30]. Available from: http://www.saiglobal.com/pdftemp/previews/osh/as/as4000/4300/4399.pdf
http://www.saiglobal.com/pdftemp/preview...
276. Hatua P, Majumdar A, Das A. Predicting the ultraviolet radiation protectio by polyester-cotton blended woven fabrics using nonlinear regression and artificial neural network models. Photodermatol Photoimmunol Photomed. 2013;29:182-9.-277277. Hatch KL, Osterwalder U. Garments as solar ultraviolet radiation screening materials. Dermatol Clin. 2006;24:85-100.
The UPF number reveals the ability to prevent radiation transmittance through the cloth. It is expressed in units whose number is inversely proportional to the amount of radiation which travels through the fabric. Clothes with 40-50 UPF allow a transmittance of only 2.6%, providing excellent skin protection.
Based on the different categories of cloth protection related to UPF indexes and UVR blockage, the Australian norm AS/NZS 4399, in 1996, presented the following parameters (Table 1): clothes with UPF 15 and 20 block from 93.3% to 95.8% of UVR, that is, offer good protection; clothes with UPF 20, 30 and 35 block 95.9% to 97.4% of UVR, that is, they offer very good protection; and clothes with UPF 40, 45, 50 and 50+ block more than 97% of UVR, therefore provide excellent protection. Products with UPF lower than 15 are not considered and factors over 50 are considered 50+.
After the Australian norm, which established standards of UPF above 15, other countries created their regulations based on the typical radiation incidence of each region, like the United Kingdom (UPF 15), United States (UPF 30) and Europe, which estipulated as a safe standard a UPF of 40+. These standards must be on labels attached to clothes accompanied by the norm number (EN 13758), as countries claim that, at this level, factors that are not tested, like humidity and stretching, would be compensated and provide safety in extreme situations in all geographic areas.267267. Gambichler T, Laperre J, Hoffmann K. The European standard for sun-protective clothing : EN 13758. J Eur Acad Dermatol Venereol. 2006;20:125-130.
There is no Brazilian standard yet to quantify the protection factor provided by clothing.
PROTECTION PROVIDED BY HATS
When there is solar exposure, the use of hats is recommended for it protects the scalp, especially in case of bald patients, and also helps to protect ears, face and neck.
The model and size of hat brim is the most determining factor of protection level offered against UVR. A hat with a brim wider than 7.5 cm may offer protection comparable to SPF 7 for the nose, 3 for the malar regions, 5 for the neck and 2 for the chin. On the other hand, a hat with medium brim, between 2.5 and 7.5 cm, may provide protection comparable to SPF 3 for the nose, 2 for the neck and malar regions and no protection for the chin region. Narrow brims, with less that 2.5 cm, will offer insignificant protection, comparable to SPF 1.5 for the nose and none for other facial areas.
Models with circular brim are excellent for protection of the back of neck. Caps, popular mainly with children and adolescents, offer little protection in the posterior region of cephalic segment.
The product or fabric from which hats are made also interferes with the level of protection. As with clothing, a hat made from closely woven fabric offers greater protection and as with clothing, again, fabrics used in the making of hats can be treated to provide greater absorption of UVR.259259. Gies P. Photoprotection by clothing. Photodermatol Photoimmunol Photomed. 2007;23:264-74.,261261. Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.,273273. Mansur JS, Breder MNR, Mansur MCA, Azulay RD. Determination of sun protecting factor in human beings and by spectrophotometry: comparison between of the two methods. An Bras Dermatol. 1986;61:167-72.,278278. Teixeira SP, Fotoproteção. RBM Rev Bras Med. 2010;10:115-22.
PROTECTION PROVIDED BY SUN GLASSES
Studies show that solar radiation can be potentially dangerous for ocular structures, especially cornea, lens and retina.279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54. After solar exposure, photochemical reactions may happen in these structures, leading to acute and chronic damage.261261. Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.,279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54.,280280. Dain SJ. Sunglasses and sunglass standards. Clin Exp Optom. 2003;86:77-90.
Acute lesions are: photokeratitis (by UVC and UVB radiation) and solar retinitis (by direct exposure to visible light). Chronic damage include cataract, pterygium, macular degeneration and skin cancer.261261. Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.,279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54.
Different ocular tissues absorb different wavelengths of UV radiation. The cornea absorbs mainly UVR with wavelengths below 295 nm. Excessive exposure to UVB radiation may cause conjunctivitis and permanent damage to the cornea. Wavelengths between 295 and 400 nm penetrate deeper and may cause damage to the lens, such as cataract.261261. Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.,279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54. Visible and infrared light cause damage to the retina.
The main photoprotective measure to prevent damage by solar radiation to the eyes is wearing sunglasses. The efficacy of sun glasses against UVR depends on size, radiation absorbing materials (which are incorporated into the lens) and posterior surface reflection of the lens.261261. Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.
Australia published the first norm for sunglasses in 1971. In 1997, the last Australian normative project (AS1067) was modified and largely revised to reflect the European norm in effect (EN 1836:1997).279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54.The first norm in the United States was published in 1972 by the American National Standards Institute (ANSIZ80.3:1972). In 2001, the most recent version was published. The ANSI Z80.3 is voluntary and not followed by all manufacturers.279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54. The International Organization for Standardization is preparing an international norm.261261. Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.,279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54.
In order to promote adequate ocular protection, it is recommended, by the main eye health organizations of the United States, to wear sun glasses which absorb 99% to 100% of all UV spectrum (up to 400nm), and additional protection for the retina must be provided by lenses that reduce transmission of blue and violet light.261261. Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.
There is no standard for the color of the lens. Sunglasses with too dark lenses may cause pupil dilation and increase opening of the eyelid, resulting in greater lens exposure to UV radiation.279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54. Glasses should ideally protect all the area around the eye, widening ocular and eyebrow protection.279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54. Only the Australian norm AS1067 recommends in its publication measures related to the size of lens.279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54. Expensive sun glasses do not necessarily provide better UV protection.261261. Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.,279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54.
There is no adequate regulation for the manufacture and labeling of sunglasses in Brazil yet.
PROTECTION PROVIDED BY ARTIFICIAL AND NATURAL SHADE
Using shade or structures that provide shade as a way of decreasing direct exposure to UV radiation is simple and usually effective. However, it is not recommended to consider shade as the sole strategy for protection. The reason is that there may be a significant amount of radiation that is diffused within the shade and through its sides.281281. Turnbull DJ, Parisi AV. Increasing the ultraviolet protection provided by shade structures. J Photochem Photobiol B. 2005;78:61-7.
The size of the structure (umbrella or cabin) and the area of lateral entrance has direct influence on the amount of UV light that is dispersed into the shade. The type of fabric, color and thickness also influence protection. Other considerable factors are the position of the person in the shade and how long this exposure lasted.281281. Turnbull DJ, Parisi AV. Increasing the ultraviolet protection provided by shade structures. J Photochem Photobiol B. 2005;78:61-7.
The proportion of radiation dispersed inside the structures goes up as the angle of sunlight incidence increases. The fact of being in the shade and the perception of decrease in temperature do not necessarily mean total protection against solar radiation.
Resources that may diminish the damage from radiation within the shade are protective clothing, glasses and hats. Other resources are vegetation and polycarbonate structures.
Polycarbonate may act as a resource for lateral protection in structures that provide shade and, this way, diminish radiation dispersed within them.281281. Turnbull DJ, Parisi AV. Increasing the ultraviolet protection provided by shade structures. J Photochem Photobiol B. 2005;78:61-7.
Vegetation may also be a form of solar protection and depends on density of leaves and their height.
PROTECTION PROVIDED BY GLASS PANELS
Glass panels are ceramic materials and therefore part of a wide class of materials, with diverse applications, from civil construction to biological implants - the bioactive glasses.282282. Lambert R, Pereira MM, Mansur HS. Biomateriais; fundamento e aplicações. Rio de Janeiro: Cultura Médica; 2006.
We are interested in glasses used in civil construction (windows and glass panels), in automobiles and in eye glasses, for they represent the interface between the skin and sun radiation, and for that reason, it is imperative to know the capability of these glasses to block solar radiation, especially UV.279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54.
Some characteristics of the glass material may exert influence over UV radiation protection properties, such as: type, color, layers and coating of the glass.279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54.
Types of glass
Some of the main types of glass used in windows are:
Clear glass: it is transparent and colorless. Its main characteristic is the capability of providing protection against the elements while allowing transmission of visible light inside. Depending on its thickness, clear glass transmits more than 90% of visible light (between 400-780 nm) and up to 83% of solar heat.279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54.
Printed glass: obtained through continuous pouring of glass mass, the surface is engraved with the most varied textures by means of metal rollers.283283. Kein RS, Werth VP, Dowdy JC, Sayre RM. Analysus of compact fluorescent lights for use by patients with phtosensitive conditions. Photochem Photobiol. 2009;85:1004-10.
Laminated glass: it is produced by associating two layers of glass to a plastic layer (PVB - polyvinyl butyral), under heat and pressure. Once glass and plastic are fused together, the result is a glass which acts as a single unit, usually very similar to the common clear glass. The benefit of the laminated glass is that, if broken, its fragments remain adhered to the PVB layer instead of being scattered, reducing the risk of accidents. PVB filters approximately 99% of ultraviolet radiation without diminishing transmission of visible light.284284. Kimlin MG, Parisi AV. Ultraviolet radiation penetrating vehicle glass: a field based comparative study. Phys Med Biol 1999;44:917-926.
Tempered glass: it is obtained through gradual heating and sudden cooling in a tempering oven (vertical or horizontal) and essentially is a safety glass. In case of breakage, it is fragmented in mildly sharp and very small pieces.284284. Kimlin MG, Parisi AV. Ultraviolet radiation penetrating vehicle glass: a field based comparative study. Phys Med Biol 1999;44:917-926.
Some studies have reported the importance of glasses in blocking UVB radiation and certain range of the UVA band.279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54. Other investigations have corroborated the importance of glass as a photoprotecting agent against undesired biological effects.284284. Kimlin MG, Parisi AV. Ultraviolet radiation penetrating vehicle glass: a field based comparative study. Phys Med Biol 1999;44:917-926.
Duarte et al.285285. Duarte I, Rotter A, Malvestiti A, Silva M. The role of glass as a barrier against the transmission of ultraviolet radiation: an experimental study. Photodermatol Photoimmunil Photomed. 2009;25:181-4., in a study published in 2008, demonstrated that all types of glass reduced UVA transmission. Laminated glass was the most efficient in totally blocking ultraviolet A radiation, which could be explained by its production characteristics: association of two glass sheets and one sheet of plastic (PVB - polyvinyl butyral), which turns it into an effective barrier against UVA.284284. Kimlin MG, Parisi AV. Ultraviolet radiation penetrating vehicle glass: a field based comparative study. Phys Med Biol 1999;44:917-926.
Colors present great influence in radiation transmission. The green glass sample totally blocks UVA radiation, and the yellow glass one allows only 1.3% through.285285. Duarte I, Rotter A, Malvestiti A, Silva M. The role of glass as a barrier against the transmission of ultraviolet radiation: an experimental study. Photodermatol Photoimmunil Photomed. 2009;25:181-4. In glass manufacturing, additives may be used for dying. Fe3+ confers a brownish-yellow coloring, whereas the mixture of Fe3+ and Fe2+ results in green. Other dyes may be added to obtain other colors. The Fe2+ ion absorbs light in the infrared region, whereas Fe3+ absorbs light in the ultraviolet egion. This way, samples containing Fe3+ in paint pigments are more efficient in diminishing UVA transmission.286286. Almutawa F, Buabbas H. Photoprotection: clothing and glass. Dermatol Clin. 2014;32:439-48.,287287. Kniess CT, Kuhnen NC, Riella HG. Estudo do efeito da quantidade de óxido de ferro em cinzas pesadas de carvão mineral na obtenção de vitrocerâmicos. Quim Nova. 2002;25:926-30.
Regarding glass thickness, UVA radiation transmission diminishes when the former increases, but is of little significance when compared with other analyzed variables.
Plastic films with 35% and 20% visibility (visible light transmission) filter UVA below 370 and 380 nm, respectively.284284. Kimlin MG, Parisi AV. Ultraviolet radiation penetrating vehicle glass: a field based comparative study. Phys Med Biol 1999;44:917-926. UVB radiation is totally blocked by all glass samples used, at any distance from the emitting source, for its penetrance power is smaller than UVA's.279279. Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54.,284284. Kimlin MG, Parisi AV. Ultraviolet radiation penetrating vehicle glass: a field based comparative study. Phys Med Biol 1999;44:917-926.,285285. Duarte I, Rotter A, Malvestiti A, Silva M. The role of glass as a barrier against the transmission of ultraviolet radiation: an experimental study. Photodermatol Photoimmunil Photomed. 2009;25:181-4.Besides, the distance of the glass from the light emitting source influences in a significant way the amount of basal radiation, and the greater the distance, the smaller the irradiation and, therefore, the smaller the transmission of UV by the glasses. This fact can be explained by the great dissipation of energy that occurs at greater distances in environmental conditions.284284. Kimlin MG, Parisi AV. Ultraviolet radiation penetrating vehicle glass: a field based comparative study. Phys Med Biol 1999;44:917-926.
Applying the results above to an everyday situation, the UVB radiation on an individual inside a car with closed windows is null. Even in the case of UVA radiation, the transmission is insufficient to produce actinic damage since besides the glass blocking an important portion of radiation, small alterations in the distance to the light source already diminish the irradiation significantly.
In view of these considerations, internal environments with glass can be considered safe for photoprotection, an important finding in the field of occupational medicine, where the use of glass cabins in professional vehicles, for example, would be a preventative health measure for workers.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
The use of mechanical measures of photoprotection is an efficient photoprotective strategy, safe and economical.
-
The introduction of the largest possible number of mechanical solar protection measures should be stimulated, particularly in case of more susceptible populations, like children and outdoor workers.
-
Even though it does not belong directly to the work scope of a dermatologist, as a professional responsible for a complete photoprotection program, he/she must always recommend eye and periorbital protection through the use of adequate sunglasses.
-
From a regulatory viewpoint, SBD recommends that technical norms and pertinent legislation must be presented for regulation of solar protection provided by clothes and hats for use in recreational or professional activities, sunglasses and umbrellas.
-
From a public health standpoint, SBD encourages educative actions aiming to promote a greater use of mechanical photoprotective measures as an accessible photoprotecting strategy for all the population, with the necessary efficiency and safety.
CHAPTER 7
PRACTICAL ASPECTS OF PHOTOPROTECTION ORIENTATION
CHAPTER 7A - GENERAL MEASURES
The prescription of sunscreen, as well as all the orientation about photoprotective measures, are part of the routine of dermatologists in their assistance activities. The correct orientation provided to patients will ensure more efficient results of the dermatological treatment prescribed.
There are different conditions in which the dermatologist must guide his patients concerning photoprotection; the most important are listed below:288288. Jou PC, Feldman RJ, Tomecki KJ. UV protection and sunscreens: what to tell patients. Cleve Clin J Med. 2012;79:427-36.
289. Wolf R, Wolf D, Morganti P, Ruocco V. Sunscreens. Clin Dermatol. 2001;19:452-459.-290290. Orentreich D, Leone AS, Arpino G, Burack H. Sunscreens: practical applications. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.537-59.
Treatment and prevention of cutaneous neoplasms in predisposed patients.
Treatment and prevention of photoaging within a more complete cosmiatric program.
Treatment and prevention of photodermatoses or photo-induced dermatoses.
Prevent development of photoirritation or photosensitization arising from other dermatological treatments proposed, such as the use of topical retinoids, psoralens and photodynamic therapy.
Prevention of post-inflammatory hyperchromia in cosmiatric treatments, particularly ablative ones.
Orientation within a more complete photoprotection program, for either a child or adult population, for outdoor recreational or sport activities.
Orientation for prevention of actinic damage in workers whose activities are partially outdoors.
In all of the situations described, there will be particularities when selecting the most adequate sunscreen, in relation to product use and other photoprotective measures offered, which will be tackled in the following chapters.
In general, however, the selection of the most adequate photoprotector and guidance regarding its correct use is always up to the dermatologist.
Selecting Sunscreens
As stated in previous chapters, every sunscreen sold in Brazil is registered by ANVISA, based on a technical dossier, for corroboration the safety and efficacy of the product. This way, one should always assume that every product registered in the country has the safety and efficacy profile minimally required.128128. Brasil. Agência Nacional de Vigilância Sanitária. Resolução - RDC no 30, de 1o de junho de 2012. Aprova o Regulamento Técnico Mercosul sobre Protetores solares em Cosméticos e dá outras providências. Diario Oficial da União jun 2012. [acesso 6 Nov 2014]. Disponível em: http://portal.anvisa.gov.br/wps/wcm/connect/e15afe804c58f17fb8f0f8dc39d59d3e/Resolu%C3%A7%C3%A3o+RDC+N%C2%BA+30,+de+1%C2%BA+de+Junho+de+2012.pdf?MOD=AJPERES.
http://portal.anvisa.gov.br/wps/wcm/conn...
With the wide range of products available in the Brazilian market, the adequate selection of a sunscreen by the prescribing dermatologist in each specific case must be based on two sources of information:
- Formulation of product (active ingredients, vehicle ingredients, presence of antioxidants or other secondary actives or yet the galenic form of the product), including the cosmeticity of the product.
- Product labeling attributes and additional studies performed.
LABELING ATTRIBUTES
Solar Protection Factor
The evaluation of data on the label of a sunscreen is a valuable tool for the dermatologist when selecting the most appropriate sunscreen in each situation.
The most important information is the Solar Protection Factor (SPF), mandatory item when labeling products.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
The SPF, as previously stated, represents the ratio between the minimal erythemal dose of protected skin and non-protected skin in a group of volunteers, and, in practice it is the expression of UVR additional exposure time that the user would have to produce an erythema with the use of the product, compared with the time that this same user would need to produce the same degree of erythema without the product.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
Thus a particular user, upon applying a hypothetical SPF 30 protector, could expose himself 30 times more until producing the same level of erythema that he would produce without wearing sunscreen.291291. Koshy JC, Sharabi SE, Jerkins D, Cox J, Cronin SP, Hollier LH Jr. Sunscreens: evolving aspects of sun protection. Journal of pediatric health care: official publication of National Association of Pediatric Nurse Associates & Practitioners. 2010;24:343-6.
The discussion over the ideal SPF value is old in the literature. Publications from the 90's of past century used mathematical models to justify that products with SPF over 30 presented only marginal UVB absorption gain if compared to SPF value increase.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
Nowadays, however, this concept has been completely disqualified in the literature, for different reasons, so we emphasize the three main ones:292292. Osterwalder U, Herzog B. Sun protection factors: world wide confusion. Br J Dermatol. 2009;161:13-24.
1. Transmittance (energy that travels through a sunscreen) is more relevant than the absorbance (energy that is retained by a sunscreen).
The absorbance of a certain sunscreen (that is, the amount of energy retained by a sunscreen), within the erythematogenic spectrum of UV radiation, can be calculated by the following equation:123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
A = (1 - 1/SPF)x100
This way, products with SPF over 30 would have only a slight increase in absorbance within the range capable of producing erythema, the reason why not using high SPF products at the time was justified.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
What Osterwalder and Herzog292292. Osterwalder U, Herzog B. Sun protection factors: world wide confusion. Br J Dermatol. 2009;161:13-24. and other authors recommend, nonetheless, is that we consider as the most important data not absorbance, but transmittance, defined as the amount of energy that travels through the photoprotecting film and reaches the skin:123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.,292292. Osterwalder U, Herzog B. Sun protection factors: world wide confusion. Br J Dermatol. 2009;161:13-24.
T = (1/SPF)x100
From this perspective, a product with SPF 30 would let through twice the radiation than a product of SPF 60, justifying then the use of products with high SPF.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.,292292. Osterwalder U, Herzog B. Sun protection factors: world wide confusion. Br J Dermatol. 2009;161:13-24.
Figure 4 demonstrates graphically the relationship between absorbance and transmittance of sunscreen.292292. Osterwalder U, Herzog B. Sun protection factors: world wide confusion. Br J Dermatol. 2009;161:13-24.
Relationship between sun protection factor (SPF) and ultraviolet (UV) effect: UV radiation percentage absorbed by the photoprotector (absorbance) and UV radiation percentage transmitted by the photoprotector that reaches the skin (transmittance), in relation to SPF values
Adapted source: Ostewalder U, Herzog B. 2009. 292292. Osterwalder U, Herzog B. Sun protection factors: world wide confusion. Br J Dermatol. 2009;161:13-24.
2. SPF is a measure of protection against sunburn, not against skin cancer. 123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
Although acknowledged as the most relevant photoprotection measure, SPF represents the capability of a sunscreen in protecting against sunburn.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
Today we know that the radiation spectrum responsible for carcinogenesis is not exactly equal to the erythematogenic spectrum and, in addition, the amount of energy necessary to produce molecular alterations in the DNA is smaller than the Minimal Erythemal Dose.293293. Kullavanijya P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.
Due to these factors, the authors do not recommend a limitation of the SPF value, if we consider that the main benefit of a sunscreen in the long-term is prevention of cutaneous cancer.
3. The amount applied in practice by users is much smaller than recommended and used in the studies to determine SPF.3434. Schalka S, dos Reis VM, Cucé LC. The influence of the amount of sunscreen applied and its sun protection factor (SPF): evaluation of two sunscreens including the same ingredients at different concentrations. Photodermatol Photoimmunol Photomed. 2009;25:175-80.,123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
The determination of the SPF is done through methods validated and published in the literature, but that do not represent the reality of wearing these products in practice, for users do not apply sufficient amounts, do not apply evenly on the whole skin surface or do not reapply the product with the due frequency.3434. Schalka S, dos Reis VM, Cucé LC. The influence of the amount of sunscreen applied and its sun protection factor (SPF): evaluation of two sunscreens including the same ingredients at different concentrations. Photodermatol Photoimmunol Photomed. 2009;25:175-80.,123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.,289289. Wolf R, Wolf D, Morganti P, Ruocco V. Sunscreens. Clin Dermatol. 2001;19:452-459.
The main interference factor in the efficacy of a sunscreen (that is, SPF) is the amount applied.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
Different studies have already demonstrated that there is a relevant difference between the laboratory conditions for the performance of the SPF test and the consumer real use conditions, especially regarding the amount applied.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.,289289. Wolf R, Wolf D, Morganti P, Ruocco V. Sunscreens. Clin Dermatol. 2001;19:452-459.
Users actually apply from 30% to 50% of the recommended amount of 2 mg/cm2.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.,289289. Wolf R, Wolf D, Morganti P, Ruocco V. Sunscreens. Clin Dermatol. 2001;19:452-459.
Studies published show that insufficient application leads to a significant drop in the efficacy of the sunscreen, that is, its real SPF.3434. Schalka S, dos Reis VM, Cucé LC. The influence of the amount of sunscreen applied and its sun protection factor (SPF): evaluation of two sunscreens including the same ingredients at different concentrations. Photodermatol Photoimmunol Photomed. 2009;25:175-80.,294294. Groves GA, Agin PP, Sayre PM. In vitro and In vivo methods to define sunscreen protection. Australas J Dermatol. 1979;20:112-9.
295. Diffey BL. Sunscreens: use and misuse. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.523-534.-296296. Lautenschlager S, Wulf HC, Pittelkow MR. Photoprotection. Lancet. 2007;370:528-37.
Schalka et al. published a study demonstrating that insufficient application of sunscreen leads to exponential reduction of real SPF, becoming the main interference factor in photoprotector efficacy.3434. Schalka S, dos Reis VM, Cucé LC. The influence of the amount of sunscreen applied and its sun protection factor (SPF): evaluation of two sunscreens including the same ingredients at different concentrations. Photodermatol Photoimmunol Photomed. 2009;25:175-80.
To compensate this drop, the authors recommend that products with higher SPF should be used by consumers, mainly in situations when there is excessive sun exposure or users are too sensitive.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.,189189. Gilaberte Y, González S. Update on Photoprotection Actas Dermosifiliogr. 2010;101:659-72.
The American Academy of Dermatology recommends, since 2009, the use of sunscreens with SPF over 30, considering the facts exposed above.123123. Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
UVA Protection
Besides the SPF value, a very important fact when choosing a sunscreen is UVA protection.
As mentioned before, the new Brazilian photoprotection legislation determines that a product, in order to declare UVA protection or broad spectrum protection, must present a UVA-PF value greater than a third of the SPF value and a critical wavelength greater than 370 nm.128128. Brasil. Agência Nacional de Vigilância Sanitária. Resolução - RDC no 30, de 1o de junho de 2012. Aprova o Regulamento Técnico Mercosul sobre Protetores solares em Cosméticos e dá outras providências. Diario Oficial da União jun 2012. [acesso 6 Nov 2014]. Disponível em: http://portal.anvisa.gov.br/wps/wcm/connect/e15afe804c58f17fb8f0f8dc39d59d3e/Resolu%C3%A7%C3%A3o+RDC+N%C2%BA+30,+de+1%C2%BA+de+Junho+de+2012.pdf?MOD=AJPERES.
http://portal.anvisa.gov.br/wps/wcm/conn...
,288288. Jou PC, Feldman RJ, Tomecki KJ. UV protection and sunscreens: what to tell patients. Cleve Clin J Med. 2012;79:427-36.
These considerations are based on different studies that point to an equilibrium in UVB and UVA protection when these measures are met.288288. Jou PC, Feldman RJ, Tomecki KJ. UV protection and sunscreens: what to tell patients. Cleve Clin J Med. 2012;79:427-36.,297297. Lowe NJ. An overview of ultraviolet radiation, sunscreens, and photo-induced dermatoses. Dermatol Clin. 2009;24:9-17.
It is for the dermatologist, therefore, to select products that meet this demand, requesting additional data from the manufacturer.
Water resistance
As stated previously, the measure of water resistance is complementary to SPF and must be required for products aimed at intentional sun exposure, that is, products for sport and leisure outdoor or aquatic activities.
Within the study methodology, as already stated, a loss of photoprotecting efficacy is accepted, which may reach up to 50% of pre-immersion SPF value. For this reason, it is recommended that even with a prescription of water resistant or very water resistant products, reapplication be done after long periods of immersion.288288. Jou PC, Feldman RJ, Tomecki KJ. UV protection and sunscreens: what to tell patients. Cleve Clin J Med. 2012;79:427-36.,295295. Diffey BL. Sunscreens: use and misuse. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.523-534.,296296. Lautenschlager S, Wulf HC, Pittelkow MR. Photoprotection. Lancet. 2007;370:528-37.
Photostability
Determining stability is not yet a requirement for registering sunscreens in Brazil.
However, we know that products advertised for intense or extensive sun exposure, like for outdoor activities, must have their photostability evaluated in order to assure consumers they are safe for use in these conditions.288288. Jou PC, Feldman RJ, Tomecki KJ. UV protection and sunscreens: what to tell patients. Cleve Clin J Med. 2012;79:427-36.,296296. Lautenschlager S, Wulf HC, Pittelkow MR. Photoprotection. Lancet. 2007;370:528-37.,297297. Lowe NJ. An overview of ultraviolet radiation, sunscreens, and photo-induced dermatoses. Dermatol Clin. 2009;24:9-17.
It is recommended that the dermatologist request photostability data from the manufacturer.
Additional studies performed
As the indication spectrum of sun screens within the dermatological practice grows, new evaluation methods are continuously proposed with the goal of demonstrating additional sunscreen benefits.
Among these additional studies, we can find clinical evaluations of specific populations, such as melasma or photodermatoses carriers, in vivo studies for evaluation of benefits such as oiliness reduction, moisturizing potential or repair of the cutaneous barrier, spectrophotometric studies like evaluation of protection against visible light efficacy or studies in vitro to demonstrate antioxidant efficacy, efficacy against infrared radiation effects or efficacy in protecting DNA, among others.
The dermatologist should request and evaluate these studies before the prescription and orientation of patients.
GUIDANCE ON THE USE OF SUNSCREEN
Amount to be applied
The recommended amount of sunscreen in order to evenly coat the skin, considering its irregularities, is 2 mg/cm2. Different studies show that with this amount it is possible to achieve a 1mm coating on the whole skin surface.3939. Glazer JL. Management of heatstroke and heat exhaustion. Am Fam Physician. 2005;71:2133-40.
For an average adult of 70 kg and 170 cm tall, the necessary amount to coat the whole body would be 35 to 40 grams.290290. Orentreich D, Leone AS, Arpino G, Burack H. Sunscreens: practical applications. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.537-59.
On the other hand, as mentioned earlier, in practice users apply much smaller amounts of sunscreen, with expressive decrease of the real protection achieved.55. Bais AF, Tourpali K, Kazantzidis A, Akiyoshi H, Bekki S, Braesicke P, et al. Projections of UV radiation changes in the 21st century: impact of ozone recovery and cloud effects Atmos. Chem Phys. 2001;11:7533-45.
Consequently, according to scientific publications and as a recommendation of regulatory agencies, users should be encouraged to apply larger amounts of sunscreen.
One of the recommended strategies is using the "teaspoon rule", in which we consider the application of 1 teaspoon on the cephalic segment and on each of the upper limbs, as well as 2 teaspoons on trunk/back and on each of the lower limbs, as depicted in Figure 5.298298. Isedeh P, Osterwalder U, Lim HW. Teaspoon rule revisited: proper amount of sunscreen application. Photodermatol Photoimmunol Photomed. 2013;29:55-6.
Adapted source: Isedeh P, et al. 2013. 298298. Isedeh P, Osterwalder U, Lim HW. Teaspoon rule revisited: proper amount of sunscreen application. Photodermatol Photoimmunol Photomed. 2013;29:55-6.
Another proposed strategy is recommending the application of a photoprotector in two layers, one after the other, doubling the amount applied, getting closer to the amount of 2 mg/cm2.
Initial application
The initial application is strategic for successful photoprotection, with published studies demonstrating that a correct first application may compensate for eventual mistakes in the reapplication.295295. Diffey BL. Sunscreens: use and misuse. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.523-534.
As shown above, studies for determination of SPF and UVA-PPD require an interval of 15 minutes between application of the product and beginning of exposure, justifying this interval also for practical orientation.55. Bais AF, Tourpali K, Kazantzidis A, Akiyoshi H, Bekki S, Braesicke P, et al. Projections of UV radiation changes in the 21st century: impact of ozone recovery and cloud effects Atmos. Chem Phys. 2001;11:7533-45.
We know, however, that some sunscreens demonstrate their effectiveness immediately after application, without the need for the 15-minute interval. As long as it is demonstrated by a clinical study, this recommendation may be given by the dermatologist to his patient.
Another important aspect in the application of a photoprotector is the uniformity of its application, preventing the fact that some areas are forgotten or receive insufficient application due to lack of attention.290290. Orentreich D, Leone AS, Arpino G, Burack H. Sunscreens: practical applications. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.537-59.
Due to all these factors, it is recommended that the application of sunscreen be done, preferably, before exposure to the sun and, when wearing them on the body, with the least possible quantity of clothes.
Reapplication
Reapplication of a sunscreen is very relevant as it is known that there is a decline in the protecting effect with time, sun exposure and due to environmental factors (clothes, towels, wind, water among others).290290. Orentreich D, Leone AS, Arpino G, Burack H. Sunscreens: practical applications. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.537-59.,295295. Diffey BL. Sunscreens: use and misuse. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.523-534.
This decrease in protection may vary widely, depending on protector formulation and activities exerted by the user.
Because it is something difficult to assess, it is understood that the 2-hour time interval be suggested as a general recommendation to the population, even acknowledging that, for some products and in some situations, the interval for reapplication could be wider.288288. Jou PC, Feldman RJ, Tomecki KJ. UV protection and sunscreens: what to tell patients. Cleve Clin J Med. 2012;79:427-36.,290290. Orentreich D, Leone AS, Arpino G, Burack H. Sunscreens: practical applications. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.537-59.,295295. Diffey BL. Sunscreens: use and misuse. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.523-534.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
General Measures
-
There is no photoprotective measure that, independently, guarantees adequate photoprotection; for this reason, SBD recommends that the combination of the largest possible number of measures is the most correct strategy.
-
In all conditions, SBD does not recommend sun exposure in the period between 10:00 a.m. and 3:00 p.m. (consider daylight saving time when necessary). Depending on the time of year (summer) and the site of exposure, an even larger period of restriction should be considered.
a. Brazilian Northeast: Guide the beginning of restriction from 9:00 a.m. due to geographical position..
b. Brazilian Midwest or states with daylight saving time: Guide the maintenance of restriction until 04:00 p.m..
-
Wearing clothes and hats or caps must be always encouraged, as recommended in a specific chapter.
-
Wearing sunglasses is recommended for prevention of actinical damage to the eyes.
-
Use of natural shade (tree covering) or artificial (umbrellas, tents, buildings or others) should always be prescribed as additional measures.
-
The correct use of sunscreen is an essential measure and its selection and prescription is the responsibility of the dermatologist.
-
When choosing an adequate photoprotector, the dermatologist should consider the following characteristics:
-
The choice of the most adequate galenic form (cream, lotion, gel, spray, baton or other) must be based on the characteristics of the patient regarding manner of use and area to receive application.
-
Evaluation of formulation ingredients, particularly of ultraviolet filters present, may be necessary in particular situations such as for sensitive patients or with a history of allergy, or yet specific populations like children and pregnant women. For the general population, however, the efficacy data are the main source of information to the dermatologist when selecting the most appropriate solar screen.
-
Solar Protection Factor: Main point about product efficacy and reference when choosing the sunscreen.
-
The choice of SPF depends on phenotypic characteristics of the patient, usage profile, exposure area and period that the user will be exposed to the sun.
-
SBD recommends the use of sun screens of at least SPF 30.
-
Products with higher SPF must be available for specific situations, like patients with greater sensitivity to the sun, personal or familial history of skin cancer, patients in treatment for photodermatoses or during cosmiatric treatment and patients exposed to a higher amount of solar radiation due to professional or leisure activities.
-
Protectors with SPF lower than 30 my be indicated in special situations and to special populations, such as Afrodescendant patients.
-
-
SBD recommends prescription of solar filters with UVA protection or broad spectrum protection that meet the Brazilian legislation on photoprotection, featuring UVA-PF of at least 1/3 of the SPF value and critical wavelength equal or greater than 370 nm.
-
Water resistant or very water resistant products should be used in recreational outdoor activities like sports and by swimmers.
-
SBD recommends the prescription of products that demonstrate photostability through specific tests.
-
-
8. In addition to correct choice, as mentioned previously, usage orientation is essential.
-
The first application of the product is fundamental and must be done with greater attention and care, for at least 15 minutes before exposure, preferably without clothes or with the least clothing possible. If the manufacturer states the "immediate protection" feature, the 15-minute interval can be suppressed.
-
The amount to be applied should be oriented by the dermatologist, recommending one of the two alternatives below:
-
Application in two layers: To increase the amount applied, the dermatologist may prescribe sunscreen application the way the patient is used to, but requesting an immediate reapplication.
-
Use the teaspoon rule, as previously described.
-
-
SBD recommends, in a general way, reapplication of sunscreen every 2 hours or after long immersion periods. Different reapplication intervals may be suggested by the manufacturer as long as demonstrated in specific tests.
-
CHAPTER 7B
ORIENTATION ABOUT PHOTOPROTECTION FOR SPECIFIC GROUPS OR AREAS
INTRODUCTION
Specific groups require special consideration when we speak of photoprotection. The type of sun exposure, skin characteristics and individual habits, as well as the diversity of photoprotective measures, demand individualized assessment in choosing ideal measures to be recommended. It is up to the dermatologist to consider all the particularities at the time of guiding patients regarding photoprotective measures. In terms of public health and photoeducation, we must also consider population groups when engaging in action for photoprotection.
Guidance on photoprotection for different population groups and also for specific skin areas, which need special care, are presented below.
Pregnancy
Pregnancy constitutes a scenario of changing hormonal levels and predisposes the occurrence of physiological or pathological modifications of the skin, like melasma. It is assumed that one of the causes for this predisposition would be the high levels of melanocyte-stimulating hormone in this period.300300. Purim KS, Avelar MF. [Photoprotection, melasma and quality of life in pregnant women]. Rev Bras Ginecol Obstet. 2012;34:228-34. In fact, it is estimated that half of pregnant women suffer from melasma.299299. Lakhdar H, Zouhair K, Khadir K, Essari A, Richard A, Seite S, et al. Evaluation of the effectiveness of a broad-spectrum sunscreen in the prevention of chloasma in pregnant women. J Eur Acad Dermatol Venereol. 2007;21:738-42. Whereas general prevalence of melasma in Latinamerican women is around 1.5% to 33%, among pregnant ones this rate rises to 50% or even 80%.299299. Lakhdar H, Zouhair K, Khadir K, Essari A, Richard A, Seite S, et al. Evaluation of the effectiveness of a broad-spectrum sunscreen in the prevention of chloasma in pregnant women. J Eur Acad Dermatol Venereol. 2007;21:738-42.
300. Purim KS, Avelar MF. [Photoprotection, melasma and quality of life in pregnant women]. Rev Bras Ginecol Obstet. 2012;34:228-34.
301. Pichardo R, Vallejos Q, Feldman SR, Schulz MR, Verma A, Quandt SA, et al. The prevalence of melasma and its association with quality of life in adult male Latino migrant workers. Int J Dermatol. 2009;48:22-6.-302302. Urasaki MBM. Alterações fisiológicas da pele percebidas por gestantes assistidas em serviços públicos de saúde. Acta Paul Enferm. 2010;23:519-25.
Even if it seems an obvious choice, solar protection as a measure to avoid the onset or worsening of melasma during pregnancy is not frequently investigated. A study performed in Chile at a prenatal clinic evaluated melasma incidence in pregnant women, wearing an SPF 10 sunscreen or placebo. The frequency of melasma onset in the two groups was statistically similar, but considering only women who applied the filter correctly, there was significant difference.303303. Abarca J, Odilla Arrollo C, Blanch S, Arellano G. [Melasma in pregnancy: reduction of its appearance with the use of a broad-spectrum photoprotective agent]. Med Cutan Ibero Lat Am. 1987;15:199-203.
In a cohort clinical study, without a control group, a team of researchers from a pharmaceutical sunscreen manufacturer laboratory oriented the use of the product by 185 pregnant women every two hours for six months, with 12 of them having a history of melasma. At six months, 2 new cases of melasma occurred, and 8 of the 12 who already had melasma saw improvement. At six months, 1 more case of melasma occurred, totaling 1.6%. At the end of pregnancy, there were 5 cases (2.7%), which the authors299299. Lakhdar H, Zouhair K, Khadir K, Essari A, Richard A, Seite S, et al. Evaluation of the effectiveness of a broad-spectrum sunscreen in the prevention of chloasma in pregnant women. J Eur Acad Dermatol Venereol. 2007;21:738-42. considered much lower than the rate found in pregnant women in another study performed in the same region (53%), but without sunscreen.304304. Khadir K, Amal S, Hali F, Nejjam F, Lakhdar H. Les signes dermatologiques physiologiques de la grossesse. Ann Dermatol Venerol. 1999;126:15-9. However, the study did not use a comparison control group.
It is possible that guidance for solar protection during pregnancy is being neglected by health professionals. In a study with 109 puerperal women in southern Brazil, it was verified that most of them used to get exposed to the sun at noon for approximately one hour. More than 70% of them did not wear sunscreen and only one woman applied it more than once per day. In an interview, they said the reason for not wearing sun screen was lack of habit. Around 15% of them used other forms of protection, mostly sunglasses. The ones with lighter skin protected themselves more from the midday sun and used more sun screen. Only 35% of the women reported receiving information about risks of sun exposure during prenatal care and none received prescription for sunscreen. Of the 25 patients with melasma, 20 (80%) developed lesions during pregnancy, most of them with a habit of one to two-hour daily sun exposure, and only six used solar filters.300300. Purim KS, Avelar MF. [Photoprotection, melasma and quality of life in pregnant women]. Rev Bras Ginecol Obstet. 2012;34:228-34.
Concern about safety for pregnant women to wear solar filters has been considered by researchers.
Substances approved by the different international regulatory agencies and by ANVISA were exhaustively evaluated as to their toxicological risk, including the risk of teratogenicity, and are considered safe for use during pregnancy.
An additional preoccupation is the recent introduction of nanoparticulate ingredients for use in sunscreens.
Different articles305305. Sambandan DR, Ratner D. Sunscreens: an overview and update. J Am Acad Dermatol. 2011;64:748-58.
306. Boisen AM, Shipley T, Jackson P, Hougaard KS, Wallin H, Yauk CL, et al. NanoTIO(2) (UV-Titan) does not induce ESTR mutations in the germline of prenatally exposed female mice. Part FibreToxicol. 2012;9:19.
307. Hougaard KS, Jackson P, Jensen KA, Sloth JJ, Loschner K, Larsen EH, et al. Effects of prenatal exposure to surface-coated nanosized titanium dioxide (UV-Titan). A study in mice. Part Fibre Toxicol. 2010;7:16.-308308. Umezawa M, Tainaka H, Kawashima N, Shimizu M, Takeda K. Effect of fetal exposure to titanium dioxide nanoparticle on brain development - brain region information. J Toxicol Sci. 2012;37:1247-52. have already been published about the safety of nanoparticles in sunscreen, but there are no studies yet specifically related to nanoparticles in photoprotetors for use during pregnancy.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Solar protection must be properly oriented during pregnancy, especially due to the risk of developing melasma and other pigmentary diseases.
-
Mechanical solar protection (clothes, hat, sunglasses) and sunscreen must be recommended in all pregnancy periods.
-
Sunscreens that follow ANVISA norms can be recommended for use during pregnancy.
-
Nanoparticulate sunscreen use should be avoided until their safety is well established.
-
Sunscreens with SPF higher than 30 and with UVA protection are recommended.
-
Recommend to a pregnant woman with past or current history of melasma the same care as for patients with melasma, as set by a specific item.
Breastfed babies and children
It has classically been informed in literature that as much as 80% of UV radiation most of us receive during our lifetime occur up to 18 years of age.309309. Stern RS, Weinstein MC, Baker SG. Risk reduction for nonmelanoma skin cancer with childhood sunscreen use. Archives of dermatology. 1986;122(5):537-45.
310. Wesson KM, Silverberg NB. Sun protection education in the United States: what we know and what needs to be taught. Cutis. 2003;71:71-4,77.-311311. Quatrano NA, Dinulos JG. Current principles of sunscreen use in children. Cur Opin Pediatr. 2013;25:122-9. This affirmation is divulged in medical articles and general literature but recently it has been proposed that this was an interpretation mistake of the original publication of Stern et al.309309. Stern RS, Weinstein MC, Baker SG. Risk reduction for nonmelanoma skin cancer with childhood sunscreen use. Archives of dermatology. 1986;122(5):537-45. in 1986.
Based on a mathematical model, the authors concluded that the habit of wearing sunscreen in the first 18 years of life reduced by 78% the incidence of skin cancer during lifetime. Actually, when we think of UVR, apparently less than 25% of it is received in this period.312312. Godar DE, Urbach F, Gasparro FP, van der Leun JC. UV doses of young adults. Photochem Photobiol. 2003;77:453-7.,313313. Parisi AV, Meldrum LR, Wong JC, Aitken J, Fleming RA. Effect of childhood and adolescent ultraviolet exposures on cumulative exposure in South East Queensland schools. Photodermatol Photoimmunol Photomed. 2000;16:19-24. This increased risk is possibly due to the number of sunburn episodes in childhood and adolescence.
Photoprotection education for this age group is essential for habit formation and to avoid the cumulative effects of UVR. Studies demonstrate that around 83% of children have sunburns in the summer, a percentage that drops to 36% among adolescents.291291. Koshy JC, Sharabi SE, Jerkins D, Cox J, Cronin SP, Hollier LH Jr. Sunscreens: evolving aspects of sun protection. Journal of pediatric health care: official publication of National Association of Pediatric Nurse Associates & Practitioners. 2010;24:343-6.The incidence of melanoma and non melanoma skin cancer in patients with sunburn history is well documented, a metanalysis having been published in 2008 based on population studies.314314. Dusza SW, Halpern AC, Satagopan JM, Oliveria SA, Weinstock MA, Scope A, et al. Prospective study of sunburn and sun behavior patterns during adolescence. Pediatrics. 2012;129:309-17.
315. Pustisek N, Sikanic-Dugic N, Hirsl-Hecej V, Domljan ML. Acute skin sun damage in children and its consequences in adults. Coll Antropol. 2010;34 Suppl 2:233-7.-316316. Dennis LK, Vanbeek MJ, Beane Freeman LE, Smith BJ, Dawson DV, Coughlin JA. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Ann Epidemiol. 2008;18:614-27.
Many studies also warn about the insufficient and inadequate wearing of sunscreen by this age group.291291. Koshy JC, Sharabi SE, Jerkins D, Cox J, Cronin SP, Hollier LH Jr. Sunscreens: evolving aspects of sun protection. Journal of pediatric health care: official publication of National Association of Pediatric Nurse Associates & Practitioners. 2010;24:343-6.sunscreen, according to recommendations of the American Academy of Pediatrics and the American Academy of Dermatology (Charts 8 and 9) are allowed after the age of six months. Until two years of age the wearing of inorganic protectors is preferable for having smaller potential of cutaneous permeation when compared with organic protectors.265265. Criado P, Melo J, Oliveira Z N. Topical photoprotection in childhood and adolescence. J Pediatr. 2012;88:203-10.,317317. Balk SJ, Council on Environmental Health; Section on Dermatology. Ultraviolet Radiation: a Hazard to Children and Adolescents. Pediatrics. 2011;127:e791-e817.
318. HealthyChildren.org/American Academy of Pediatrics [Internet]. Sun Safety: Information for Parents About Sunburn & Sunscreen, 2014. [cited 2014 Oct 30]. Available from: http://www.healthychildren.org/English/safety-prevention/atplay/Pages/Sun-Safety.aspx
http://www.healthychildren.org/English/s...
-319319. American Academy of Dermatology [Internet]. Stats and facts - Prevention and care: Sunscreens 2013. [cited 2014 Oct 30]. Available from: http://www.aad.org/media-resources/stats-and-facts/prevention-and-care/sunscreens
http://www.aad.org/media-resources/stats...
Recommendation of the American Academy of Pediatrics for photoprotection of breastfed babies and children
Recommendation of the American Academy of Dermatology for photoprotection of breastfed babies and children
There is evidence that wearing sunscreens in childhood and adolescence reduces the incidence of skin cancer, besides actinic damage. More stable formulations, resistant to water and sand, make the incorporation of sunscreen use into the routine of children easier. Photoprotection measures such as clothes, hats, sunglasses and staying in the shade should also be encouraged.314314. Dusza SW, Halpern AC, Satagopan JM, Oliveria SA, Weinstock MA, Scope A, et al. Prospective study of sunburn and sun behavior patterns during adolescence. Pediatrics. 2012;129:309-17.,315315. Pustisek N, Sikanic-Dugic N, Hirsl-Hecej V, Domljan ML. Acute skin sun damage in children and its consequences in adults. Coll Antropol. 2010;34 Suppl 2:233-7.
In the period around solar noon all sun exposure should be avoided, even when wearing photoprotector, due to the high UVR rate. A simple rule that helps to identify this time is the "shadow rule"; the smaller the child's shadow projected on the ground in relation to its height, the greater the risk incurred. Sun exposure should be avoided in the period when the shadow projected on the ground is smaller than the child's height. 265265. Criado P, Melo J, Oliveira Z N. Topical photoprotection in childhood and adolescence. J Pediatr. 2012;88:203-10.,320320. Holloway L. Atmospheric sun protection factor on clear days: its observed dependence on solar zenith angle and its relevance to the shadow rule for sun protection. Photochem photobiol. 1992;56:229-34.
Besides direct exposure, there is great worldwide concern regarding adolescents that use artificial tanning chambers (over 2 million adolescents per year, only in the United States). As of 2011, their use was forbidden for people younger than 18 years of age in the states of California and Vermont, as well as in the United Kingdom.321321. Agência Nacional de Vigilância Sanitária. ANVISA/MS. Resolução nº 56, de 9 de novembro de 2009. Brazil was the first country in the world to forbid the use of artificial tanning for esthetical purposes; it has been forbidden since 2009.321321. Agência Nacional de Vigilância Sanitária. ANVISA/MS. Resolução nº 56, de 9 de novembro de 2009.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION
Photoprotection in Childhood
-
Photoprotection of the pediatric population is fundamental and should be part of well-child care, as well as be oriented by a dermatologist.
-
Three age groups are considered for photoprotection recommendations:
-
Breastfed babies younger than 6 months.
-
should not be directly exposed to the sun.
-
when necessary, it is recommended they wear clothes and hats that cover the skin.
-
wearing sunscreen is not recommended for this age group; it may be prescribed and oriented by the dermatologist in exceptional situations.
-
-
Children older than 6 months - general measures
-
should not be directly exposed to the sun in the period between 10:00 a.m. and 3:00 p.m.
-
use the "shadow rule": if the shadow of its body is smaller than its height, the child should not be exposed to the sun.
-
the use of mechanical photoprotection measures, like wearing clothes, hats and staying in the shade are essential in a photoprotection program for this age group.
-
photoprotection should always be recommended when necessary. Always recommend sunscreens with SPF above 30 and UVA protection. Whenever possible, opt for products indicated for the pediatric population.
-
Children from 6 months to 2 years of age: preference for products composed totally or for the most part of inorganic filters. Products in the form of cream and sticks are particularly recommended.
-
Children older than 2 years of age: wear products with an adequate balance of organic and inorganic filters, high substantivity (water resistance), easy application and spreadability. Creamy lotions and aerosol products are better accepted. Particular attention should be paid to adequate application of aerosols.
-
-
Sunscreens should be applied wearing the least quantity of clothes possible, 15 to 30 minutes before sun exposure and reapplied every 2 hours or after immersion in water.
-
Recommend application of a generous quantity of sun protector or application in two consecutive layers, as already explained, to reach a quantity close to 2 mg/cm2.
-
Complexion of African descent people
People of African descent ethnicity have a lower risk for development of skin cancer. However, once affected, their mortality rate is significantly higher and the prognosis worse.321321. Agência Nacional de Vigilância Sanitária. ANVISA/MS. Resolução nº 56, de 9 de novembro de 2009.
322. Halder RM, Bridgeman-Shah S. Skin cancer in African Americans. Cancer. 1995;75(2 Suppl):667-73.
323. Baumann L, Rodriguez D, Taylor SC, Wu J. Natural considerations for skin of color. Cutis; cutaneous medicine for the practitioner. 2006;78(6 Suppl):2-19.
324. Battie C, Gohara M, Verschoore M, Roberts W. Skin cancer in skin of color: an update on current facts, trends, and misconceptions. J Drugs Dermatol. 2013;12:194-8.-325325. Bradford PT. Skin cancer in skin of color. Dermatol Nurs. 2009;21:170-7, 206; quiz 178. The late diagnosis may result from the perception of diminished cancer risk among these individuals.4242. Dumay O, Karam A, Vian L, Moyal D, Hourseau C, Stoebner P, et al. Ultraviolet AI exposure of human skin results in Langerhans cell depletion and reduction of epidermal antigen-presenting cell function: partial protection by a broad-spectrum sunscreen. Br J Dermatol. 2001;144:1161-8.
A study carried out in California with randomly selected people of African descent ethnicity revealed that 46% of them had perception of zero risk for skin cancer, and 76% believed they had low risk (up to 25%). People with perception of high risk for cancer had history of prior skin cancer or sun sensitive skin. However, even among those with a higher level of concern, only 9.2% routinely wore SPF 15 sunscreen (against 6.3% of those who believed they were at a low risk).
Women, especially older and with a higher educational level, had a greater tendency to wear sunscreen. Thus, the study showed that wearing sunscreen was not dependent on perception of cancer risk nor economical variables, but only on gender, age and educational level.327327. Pichon LC, Corral I, Landrine H, Mayer JA, Adams-Simms D. Perceived skin cancer risk and sunscreen use among African American adults. J Health Psychol. 2010;15:1181-9.
Another study corroborated this multiplicity of factors involved in the behavior of wearing a photoprotector: in a telephone survey carried out in the USA it was found that ethnicity and/or race, gender, income, education and reactivity of skin to sunburn affected the habit of wearing sun protector: only 25% of the sample "always" wore the product, and the participants with African descent ethnicity skin, non Hispanic, wore protector 7 times less than Caucasians, who burned easily. The study showed that, among people with history of severe sunburn (with blisters), ethnicity did not affect the habit of wearing sunscreen.328328. Summers P, Bena J, Arrigain S, Alexis AF, Cooper K, Bordeaux JS. Sunscreen use: Non-Hispanic Blacks compared with other racial and/or ethnic groups. Arch Dermatol. 2011;147:863-4.
In a seaside city of Santa Catarina, the parents of preschool students were interviewed regarding sun protection. The study revealed that white children had a significantly larger tendency to wear and to reapply sunscreen. The fact of studying in private schools and having a higher income were also associate factors. The type of skin was not associated with the SPF of the protector.329329. Batista T, Fissmer MC, Porton KR, Schuelter-Trevisol F. Assessment of sun protection and skin cancer prevention among preschool children. Rev Paul Pediatr. 2013;31:17-23.
If protection against skin cancer were due only to the quantity of melanin in the skin, there would be a linear relationship between the skin tone and risk for cancer, which could never be verified. On the contrary, it seems that the risk for skin cancer does not depend only on the melanin barrier to radiation, but is a complex process that involves immunosuppression decreased by sun exposure, susceptibility to burns and capacity of response to DNA damage (repair).324324. Battie C, Gohara M, Verschoore M, Roberts W. Skin cancer in skin of color: an update on current facts, trends, and misconceptions. J Drugs Dermatol. 2013;12:194-8.,326326. Dominguez AR, Pandya A. Need for more education for latinos regarding sun-safe behaviors. Arch Dermatol 2011;147:820.
Research is going in this direction, but as long as there are no objective answers about the role played by each of these factors in protection against cancer and skin aging, preventing sunburns and immunosuppression caused by sun exposure is prudent; therefore, sun protection is an important tool for people of all skin colors.326326. Dominguez AR, Pandya A. Need for more education for latinos regarding sun-safe behaviors. Arch Dermatol 2011;147:820.
In addition to the discussion about photoprotection and skin cancer prevention for individuals with African descent ethnicity skin, another factor related to UVR exposure in dark-skinned individuals are the hyperpigmentation disorders, such as postinflammatory hyperpigmentation and melasma. Actually, it is the main motivation for recommendation of photoprotective measures for these population groups.324324. Battie C, Gohara M, Verschoore M, Roberts W. Skin cancer in skin of color: an update on current facts, trends, and misconceptions. J Drugs Dermatol. 2013;12:194-8.,326326. Dominguez AR, Pandya A. Need for more education for latinos regarding sun-safe behaviors. Arch Dermatol 2011;147:820.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Photoprotective measures, including wearing sunscreen, should be recommended for individuals of any skin color, including those of African descent ethnicity.
-
The dermatologist should pay special attention to skin photoprotection of African descent ethnicity patients, for the greater risk of onset of pigmentary dermatoses as well as the risk, although reduced, for the onset of cutaneous neoplasms.
Sport activities
Athletes who practice outdoor activities receive a considerable dose of UVR. Adequate photoprotective measures should be taken for this group in view of the high degree of exposure associated with intense sudoresis.330330. Moehrle M. Outdoor sports and skin cancer. Clin Dermatol. 2008;26:12-5.
Sudoresis induced by heat and by the physical activity may contribute significantly to skin damage caused by UVR, since it increases sensitivity and risk for sunburn. This is probably due to hydration of the stratum corneum with decrease of reflection and dispersion.331331. Moehrle M, Koehle W, Dietz K, Lischka G. Reduction of minimal erythema dose by sweating. Photodermatol Photoimmunol Photomed. 2000;16:260-2.
A study with 290 college athletes showed that, although 96% of them agreed that sunscreen decreased skin cancer rates, over 50% of them had never worn sunscreen and 75% of those who did wore it less than 3 times per week. The most frequent justification for not wearing it (39%) was the desire to have tanned skin.332332. Wysong A, Gladstone H, Kim D, Lingala B, Copeland J, Tang JY. Sunscreen use in NCAA collegiate athletes: identifying targets for intervention and barriers to use. Prev Med. 2012;55:493-6.
Due to reapplication difficulties and the long time of exposure, wearing clothes made of fabrics with ultraviolet protection and adequate caps or hats, in addition to sunglasses, which protect not only the eyes but the periorbital and malar regions as well, are essential.330330. Moehrle M. Outdoor sports and skin cancer. Clin Dermatol. 2008;26:12-5.
When we talk about sunscreen, the ideal for those who practice sports is one that provides greater adherence, due to constant sweating and water activities. The spray form is often preferred because it dries easily and is quickly applied, in spite of not having the same adhesion of a filter with greater substantivity; it is reserved for subsequent reapplications. As regards the burning sensation in the eyes, inorganic filters are believed to be less irritating and thicker vehicles used as base or a stick keep the product on the place of application and are favorites for this specific region.135135. Draelos ZD. Compliance and sunscreens. Dermatol Clin. 2006;24:101-4.
The athletes who practice water sports are more affected by UVR, as a consequence of little protection provided by clothes, constant contact with the water and reflection of sunlight on the surface of the water. Some products use inverse emulsion (oils in the external emulsion phase) to increase the resistance of the product to the water. Inverse emulsions and those based on insoluble particles may not be cosmetically satisfactory like the traditional emulsions of organic filters, but they may provide more protection.333333. Loden M, Beitner H, Gonzalez H, Edstrom DW, Akerstrom U, Austad J, et al. Sunscreen use: controversies, challenges and regulatory aspects. Br J Dermatol. 2011;165:255-62.
In a Danish study with 24 volunteers submitted to physical activity and submersion in a bathtub, the SPF of the inorganic and organic sunscreen was reduced by 38% and 41%, respectively, after 4 hours, and 55% and 58% after 8 hours.334334. Bodekaer M, Faurschou A, Philipsen PA, Wulf HC. Sun protection factor persistence during a day with physical activity and bathing. Photodermatol Photoimmunol Photomed. 2008;24:296-300.
ANVISA, in RDC 30/2012, requests that allegations concerning water resistance be ascertained by specific methodologies defined in this new regulation. The manufacturers may indicate on their labels the expressions: "Water Resistant", "Very Water Resistant", "Water/Sweat Resistant" or "Water/Perspiration Resistant", as long as this characteristic is ascertained.128128. Brasil. Agência Nacional de Vigilância Sanitária. Resolução - RDC no 30, de 1o de junho de 2012. Aprova o Regulamento Técnico Mercosul sobre Protetores solares em Cosméticos e dá outras providências. Diario Oficial da União jun 2012. [acesso 6 Nov 2014]. Disponível em: http://portal.anvisa.gov.br/wps/wcm/connect/e15afe804c58f17fb8f0f8dc39d59d3e/Resolu%C3%A7%C3%A3o+RDC+N%C2%BA+30,+de+1%C2%BA+de+Junho+de+2012.pdf?MOD=AJPERES.
http://portal.anvisa.gov.br/wps/wcm/conn...
For a patient with this profile, the ideal is to wear adequate clothing with UV protection.
Portable UVA/UVB meters have been sold in the last few years targeted to the practice of sports. In 1976, the first polysulfone-based adhesives were used; however, their use was restricted to research due to the need for a spectrophotometer to assess their absorbance and capture only between 280-315nm (UVB).335335. Davis A, Deane GH, Diffey BL. Possible dosimeter for ultraviolet radiation. Nature. 1976;261(5556):169-70.
Currently, bracelets made of encapsulated benzyl-viologen, that changes color according to exposure to ultraviolet radiation are being sold in Europe and are calibrated to assess in real time if the patient with phototype II has reached the maximum recommended UV dose.336336. Mills A, McFarlane M, Schneider S. A viologen-based UV indicator and dosimeter. Anal Bioanal Chem. 2006;386:299-305. In 2004, the use of electronic meters that store UVA and UVB readings at pre-established intervals was started for research purposes, allowing reuse and discharge of data to a computer for analysis.337337. Heydenreich J, Wulf HC. Miniature personal electronic UVR dosimeter with erythema response and time-stamped readings in a wristwatch. Photochem Photobiol. 2005;81:1138-44. Recently, this equipment began to be sold in New Zealand for personal use.338338. Scienterra Limited [Internet]. UV Dosimeter 2013. [cited 2014 Oct 30]. Available from: http://scienterra.com/#/home/4567276438/UV-Dosimeter/3113961.
http://scienterra.com/#/home/4567276438/...
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Photoprotection in sports should be carried out in a careful and detailed manner, with the specificity required by the activity of choice.
-
In terms of public health, it is recommended to not engage in outdoor sport activities in the period between 10:00 a.m. and 3:00 p.m. and/or with high UV index.
-
Actions should be proposed to associations organizing great sport events, such as the Brazilian Soccer Confederation and the Brazilian Olympic Committee, to define photoprotective strategies for the athletes and the viewing public.
-
The postponement of great sport events, such as soccer matches, to schedules after 05:00 p.m., specially during the summer, is one of the most efficient measures.
-
Mechanical photoprotective measures like clothes, hats and sunglasses should always be part of the orientation to athletes.
-
Wearing sunscreen is highly recommendable, with some specific characteristics:
-
High SPF, if possible above 50.
-
Balanced and proportional UVA protection.
-
Products of high photostability, for the long time of exposure.
-
sunscreen very resistant to water.
-
Vehicles in thicker creams and sticks may be an interesting option for the face, to reduce complaints about burning eyes.
-
For body use, products easy to apply, like creamy lotions and aerosols, are recommended.
-
Products for application on wet skin, that present inverse emulsion (oils in the external phase of the emulsion), may be recommended for water sports.
-
Melasma
Exposure to UV radiation is widely recognized as a risk factor for the onset of melasma.299299. Lakhdar H, Zouhair K, Khadir K, Essari A, Richard A, Seite S, et al. Evaluation of the effectiveness of a broad-spectrum sunscreen in the prevention of chloasma in pregnant women. J Eur Acad Dermatol Venereol. 2007;21:738-42.,305305. Sambandan DR, Ratner D. Sunscreens: an overview and update. J Am Acad Dermatol. 2011;64:748-58.,339339. Vázquez M, Sánchez JL. The efficacy of a broad-spectrum sunscreen in the treatment of melasma. Cutis. 1983;32:92,95-6.
340. Cestari T, Arellano I, Hexsel D, Ortonne JP; Latin American Pigmentary Disorders Academy. Melasma in Latin America: options for therapy and treatment algorithm. J Eur Acad Dermatol Venereol. 2009;23:760-72.
341. Ball Arefiev KL, Hantash BM. Advances in the treatment of melasma: a review of the recent literature. Dermatol Surg. 2012;38(7 Pt 1):971-84.-342342. Guinot C, Cheffai S, Latreille J, Dhaoui MA, Youssef S, Jaber K, et al. Aggravating factors for melasma: a prospective study in 197 Tunisian patients. J Eur Acad Dermatol Venereol. 2010;24:1060-9. Recently, studies have shown the participation of visible light in pigmentation and oxidative damage, as well as its interference in hyperpigmentary dermatoses, like melasma and post-inflammatory hipercromia.178178. Schalka S, Addor FAS, Agelune CM, Pereira VMC. Sunscreen protection against visible light: a new proposal for Evaluation. Surg Cosmet Dermatol 2012;3:45-52.
Melasma treatment, or lightening of spots is not the object of this consensus; several products and procedures have been used340340. Cestari T, Arellano I, Hexsel D, Ortonne JP; Latin American Pigmentary Disorders Academy. Melasma in Latin America: options for therapy and treatment algorithm. J Eur Acad Dermatol Venereol. 2009;23:760-72.,343343. Sheth VM, Pandya AG. Melasma: a comprehensive update: part II. J Am Acad Dermatol. 2011;65:699-714; quiz 715.,344344. Ni Z, Mu Y, Gulati O. Treatment of melasma with Pycnogenol. Phytother Res. 2002;16:567-71. with the purpose of inhibiting the activity of melanocytes, interrupt melasma formation and promote degradation of melanosomes.340340. Cestari T, Arellano I, Hexsel D, Ortonne JP; Latin American Pigmentary Disorders Academy. Melasma in Latin America: options for therapy and treatment algorithm. J Eur Acad Dermatol Venereol. 2009;23:760-72.,344344. Ni Z, Mu Y, Gulati O. Treatment of melasma with Pycnogenol. Phytother Res. 2002;16:567-71. Therefore, at the same time that an attempt is made to lighten the existing spots, their darkening and fomation of new spots should be prevented by ensuring appropriate photoprotection340340. Cestari T, Arellano I, Hexsel D, Ortonne JP; Latin American Pigmentary Disorders Academy. Melasma in Latin America: options for therapy and treatment algorithm. J Eur Acad Dermatol Venereol. 2009;23:760-72.,343343. Sheth VM, Pandya AG. Melasma: a comprehensive update: part II. J Am Acad Dermatol. 2011;65:699-714; quiz 715. or even camouflage (makeup that affords total sunblock action).136136. Draelos ZD. The multifunctional value of sunscreen-containing cosmetics. Skin Therapy Lett. 2011;16:1-3.,343343. Sheth VM, Pandya AG. Melasma: a comprehensive update: part II. J Am Acad Dermatol. 2011;65:699-714; quiz 715.
Since the risk factor present in all melasma patients is sun exposure, the role of sunscreen is well established as an important part of the treatment, based on the principle of avoiding triggering or exacerbating hyperpigmentation factors, especially aggression by UV radiation.343343. Sheth VM, Pandya AG. Melasma: a comprehensive update: part II. J Am Acad Dermatol. 2011;65:699-714; quiz 715.,344344. Ni Z, Mu Y, Gulati O. Treatment of melasma with Pycnogenol. Phytother Res. 2002;16:567-71. Recurrence after intense exposure is a common problem in melasma.345345. Gupta AK, Gover MD, Nouri K, Taylor S. The treatment of melasma: A review of clinical trials. J Am Acad Dermatol. 2006;55:1048-65.
In 1983, researchers of Porto Rico proposed to verify specifically whether wearing sunscreens would impact melasma treatment, evaluating the need for it to be used together with the topical treatment. In a randomized, double-blind clinical study, hydroquinone was administered to 59 women, when half of them also received sunscreen and the other half placebo. Among those who wore a filter 96.3% improved, against 80.8% of those who used placebo, without significant difference between the groups.339339. Vázquez M, Sánchez JL. The efficacy of a broad-spectrum sunscreen in the treatment of melasma. Cutis. 1983;32:92,95-6.
After that, photoprotection continued to be part of the treatment in all the world. In fact, around 80% of the patients experience some improvement only wearing sunscreens, even when receiving placebo as depigmentation treatment (against 100% of patients receiving filter plus hydroquinone, glycolic acid and antioxidants).346346. Guevara IL, Pandya AG. Safety and efficacy of a 4% hydroquinone combined with 10% glycolic acid, antioxidants, and sunscreen in the treatment of melasma. Int J Dermatol. 2003;42:966-72. A systematic review of the literature shows that sunscreens are indispensable in the approach to melasma, even though the topical treatment is necessary.345345. Gupta AK, Gover MD, Nouri K, Taylor S. The treatment of melasma: A review of clinical trials. J Am Acad Dermatol. 2006;55:1048-65.
In fact, wearing a broad spectrum sunscreen with SPF above 30 is included as first line of the treatment algorithm proposed by the Latin American Pigmentary Disorders Academy.340340. Cestari T, Arellano I, Hexsel D, Ortonne JP; Latin American Pigmentary Disorders Academy. Melasma in Latin America: options for therapy and treatment algorithm. J Eur Acad Dermatol Venereol. 2009;23:760-72.Except for the above mentioned study, a systematic review of the literature published in 2006 shows that the clinical studies of melasma do not even consider replacing sunscreen with placebo anymore,345345. Gupta AK, Gover MD, Nouri K, Taylor S. The treatment of melasma: A review of clinical trials. J Am Acad Dermatol. 2006;55:1048-65. but are all based on the comparison of depigmentation treatments, topical or mechanical. Investigations show that sunscreens added to hydroquinone and retinol formulations have their potency to protect against UV radiation preserved.347347. Stanfield JW, Feldman SR, Levitt J. Sun protection strength of a hydroquinone 4%/retinol 0.3% preparationn containing sunscreens. J Drugs Dermatol. 2006;5:321-4.
A study carried out in 2008178178. Schalka S, Addor FAS, Agelune CM, Pereira VMC. Sunscreen protection against visible light: a new proposal for Evaluation. Surg Cosmet Dermatol 2012;3:45-52.,348348. Mahmoud BH, R-UVolo E, Hexsel CL, Liu Y, Owen MR, Kollias N, Lim HW, Hamzavi IV. Impact of long-wavelenght UVA and visible light on melanocompetent skin. J Invest Dermatol. 2010;130:2092-7.evidenced that long UVA radiation (340-400 nm) and visible light (400-700 nm) are able to promote immediate skin pigmentation, having as chromophores not only melanin, but also oxihemoglobin.178178. Schalka S, Addor FAS, Agelune CM, Pereira VMC. Sunscreen protection against visible light: a new proposal for Evaluation. Surg Cosmet Dermatol 2012;3:45-52.,348348. Mahmoud BH, R-UVolo E, Hexsel CL, Liu Y, Owen MR, Kollias N, Lim HW, Hamzavi IV. Impact of long-wavelenght UVA and visible light on melanocompetent skin. J Invest Dermatol. 2010;130:2092-7.
sunscreen were developed to protect from UVR skin damage,178178. Schalka S, Addor FAS, Agelune CM, Pereira VMC. Sunscreen protection against visible light: a new proposal for Evaluation. Surg Cosmet Dermatol 2012;3:45-52. but protection against visible light is limited and recent studies reveal the importance of such care. A study carried out by Schalka et al., in 2012,178178. Schalka S, Addor FAS, Agelune CM, Pereira VMC. Sunscreen protection against visible light: a new proposal for Evaluation. Surg Cosmet Dermatol 2012;3:45-52. evaluated the effectiveness of white and colored sunscreen in protecting against visible light by means of the spectrophotometric evaluation of the absorption curve of products, value of photoprotection and colorimetric characteristics, for quantification of protection within this specific radiation range. The conclusion was that the value of the sun protection factor (FPS) has no direct relationship with protection against visible light, but with the potential translucency of the product.178178. Schalka S, Addor FAS, Agelune CM, Pereira VMC. Sunscreen protection against visible light: a new proposal for Evaluation. Surg Cosmet Dermatol 2012;3:45-52.
The inorganic filters, for their reflective ability, could be an option against visible light, depending on the size of their particles. Thus, only large and visible particles (pigmentary) would be able to protect against visible light.349349. Shaath N. Sunscreens: regulation and comercial development. 3rd ed. Boca Raton: T&F informa; 2005. p. 325. Therefore, the incorporation of absorbing pigments to sunscreen increases the photoprotective ability of these products.178178. Schalka S, Addor FAS, Agelune CM, Pereira VMC. Sunscreen protection against visible light: a new proposal for Evaluation. Surg Cosmet Dermatol 2012;3:45-52.
Protection against UVA and UVB radiation is the main point of the treatment.299299. Lakhdar H, Zouhair K, Khadir K, Essari A, Richard A, Seite S, et al. Evaluation of the effectiveness of a broad-spectrum sunscreen in the prevention of chloasma in pregnant women. J Eur Acad Dermatol Venereol. 2007;21:738-42.,339339. Vázquez M, Sánchez JL. The efficacy of a broad-spectrum sunscreen in the treatment of melasma. Cutis. 1983;32:92,95-6.
340. Cestari T, Arellano I, Hexsel D, Ortonne JP; Latin American Pigmentary Disorders Academy. Melasma in Latin America: options for therapy and treatment algorithm. J Eur Acad Dermatol Venereol. 2009;23:760-72.-341341. Ball Arefiev KL, Hantash BM. Advances in the treatment of melasma: a review of the recent literature. Dermatol Surg. 2012;38(7 Pt 1):971-84.,350350. Rendon M, Berneburg M, Arellano I, Picardo M. Treatment of melasma. J Am Acad Dermatol. 2006;54(5 Suppl 2):S272-81. According to recent studies, broad spectrum sun protector, UVA and UVB, with at least SPF 30, containing inorganic filter, like titanium dioxide or zinc oxide, should be used by patients with melasma and be frequently reapplied.299299. Lakhdar H, Zouhair K, Khadir K, Essari A, Richard A, Seite S, et al. Evaluation of the effectiveness of a broad-spectrum sunscreen in the prevention of chloasma in pregnant women. J Eur Acad Dermatol Venereol. 2007;21:738-42.,340340. Cestari T, Arellano I, Hexsel D, Ortonne JP; Latin American Pigmentary Disorders Academy. Melasma in Latin America: options for therapy and treatment algorithm. J Eur Acad Dermatol Venereol. 2009;23:760-72.
341. Ball Arefiev KL, Hantash BM. Advances in the treatment of melasma: a review of the recent literature. Dermatol Surg. 2012;38(7 Pt 1):971-84.
342. Guinot C, Cheffai S, Latreille J, Dhaoui MA, Youssef S, Jaber K, et al. Aggravating factors for melasma: a prospective study in 197 Tunisian patients. J Eur Acad Dermatol Venereol. 2010;24:1060-9.-343343. Sheth VM, Pandya AG. Melasma: a comprehensive update: part II. J Am Acad Dermatol. 2011;65:699-714; quiz 715.,350 350. Rendon M, Berneburg M, Arellano I, Picardo M. Treatment of melasma. J Am Acad Dermatol. 2006;54(5 Suppl 2):S272-81.Organic and inorganic filters may act synergically to enhance SPF value.305305. Sambandan DR, Ratner D. Sunscreens: an overview and update. J Am Acad Dermatol. 2011;64:748-58. Formulations containing opaque filters and absorbing pigments may allow photoprotection against visible light.178178. Schalka S, Addor FAS, Agelune CM, Pereira VMC. Sunscreen protection against visible light: a new proposal for Evaluation. Surg Cosmet Dermatol 2012;3:45-52.
Nevertheless, adherence is a sensitive issue when we are dealing with protection against sun radiation, as application and reapplication of solar filters on the skin should be done adequately, which can be laborious and costly.351351. Costa FB, Weber MB. Evaluation of solar exposure and sun-protection behaviors among university students in the Metropolitan Region of Porto Alegre, Brazil. An Bras Dermatol. 2004;79:149-55. Failure to adhere to the use of sunscreen may lead to aggravation of hyperpigmentation in melasma. Field research has already verified that patients with melasma expose themselves to the sun at inappropriate times (from 11:00 a.m. to 4:00 p.m.), which may worsen the problem, and only a minority reapplies the product along the day (48.2%).342342. Guinot C, Cheffai S, Latreille J, Dhaoui MA, Youssef S, Jaber K, et al. Aggravating factors for melasma: a prospective study in 197 Tunisian patients. J Eur Acad Dermatol Venereol. 2010;24:1060-9.
In men, the situation is more critical, as they tend to avoid more complex and time consuming treatments, and among them the use of products that interfere with shaving may be problematic. Because they are less concerned with appearance and health, they protect themselves less than women and should be advised about sun exposure as an aggravating factor.352352. Vachiramon V, Suchonwanit P, Thadanipon K. Melasma in men. J Cosmet Dermatol. 2011;11:151-7.
Therefore, the dermatologist should use all possible strategies to improve adherence of patients with melasma to protective measures, beginning with non exposure to the sun. Clarification regarding the best times to be in the sun are essential, as well as the duration of protection and the consequent need for reapplication. However, the patient cannot always refrain from being exposed to the sun in given periods, simply because he may be en route or carrying out professional activities.342342. Guinot C, Cheffai S, Latreille J, Dhaoui MA, Youssef S, Jaber K, et al. Aggravating factors for melasma: a prospective study in 197 Tunisian patients. J Eur Acad Dermatol Venereol. 2010;24:1060-9. In such cases, the recommendation to wear hats, sunglasses and adequate clothing expands protection and should always be part of the prescription.340340. Cestari T, Arellano I, Hexsel D, Ortonne JP; Latin American Pigmentary Disorders Academy. Melasma in Latin America: options for therapy and treatment algorithm. J Eur Acad Dermatol Venereol. 2009;23:760-72.
In addition to the mandatory recommendation to wear sun protector with SPF above 30 and balanced UVA protection, whenever possible wearing sunscreen that protect against visible light should be recommended.178178. Schalka S, Addor FAS, Agelune CM, Pereira VMC. Sunscreen protection against visible light: a new proposal for Evaluation. Surg Cosmet Dermatol 2012;3:45-52.
Vegetable extracts containing monomeric phenolic compounds and flavonoids, in addition to phenolic acids, that have antioxidant and anti-inflammatory action243243. Gonzales S, Pathak MA, Cuevas J, Villarrubia VG, Fitzpatrick TB. Topical or oral administration with an extract of Polypodium leucomotos prevents acute sunburn and psoralen-induced phototoxic reactions as weel as depletion of Langerhans cells in human skin. Photodermatol Photoimmunol Photomed. 1997;13:50-60.,341341. Ball Arefiev KL, Hantash BM. Advances in the treatment of melasma: a review of the recent literature. Dermatol Surg. 2012;38(7 Pt 1):971-84.,344344. Ni Z, Mu Y, Gulati O. Treatment of melasma with Pycnogenol. Phytother Res. 2002;16:567-71. have also been investigated. Polypodium leucotomos extract has been studied and a clinical trial showed its ability to protect the skin against acute sunburn action but also in the prevention and treatment of pigmentary dermatoses, such as melasma.243243. Gonzales S, Pathak MA, Cuevas J, Villarrubia VG, Fitzpatrick TB. Topical or oral administration with an extract of Polypodium leucomotos prevents acute sunburn and psoralen-induced phototoxic reactions as weel as depletion of Langerhans cells in human skin. Photodermatol Photoimmunol Photomed. 1997;13:50-60.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Photoprotection is fundamental in the treatment and prevention of melasma.
-
The dermatologist should use all possible strategies to improve adherence of patients with melasma to protective measures, beginning with non exposure to the sun. Clarification regarding the best times to be in the sun are essential, as well as the duration of protection and the consequent need for reapplication.
-
The use of mechanical measures like hats is a recommendation that extends protection and should always be part of the prescription.
-
In case of melasma, the sun protector should have the following characteristics:
-
High SPF, preferably above 50.
-
UVA protection proportionately elevated.
-
If possible, offer colored sunscreen, in the a form of makeup foundation ot compact cream.
-
Use products that protect in the visible light range.
-
-
Orientation regarding application and reapplication of the product for melasma patients is the same offered as general orientation.
-
The use of oral photoprotective agents with proven effectiveness in prevention and treatment of melasma may be recommended as adjuvant measure.
Sensitive skin
Ever since sunscreen began to be sold, many actives have been introduced alone or combined in their formulations. With the dissemination of knowledge about the effects of UV radiation and awareness campaigns for prevention of skin cancer, there was great consumption escalation, and new forms of presentation were introduced in the market.
Special situations like filters for daily use, makeup with filters, protectors resistant to water and sand, photostable and with better cosmetic acceptability led to greater adherence. However, new and numerous actives appeared in pharmaceutical forms, enhancing the allergenic potential of products.353353. Scheuer E, Warshaw E. Sunscreen allergy: A review of epidemiology, clinical characteristics, and responsible allergens. Dermatitis : contact, atopic, occupational, drug : official journal of the American Contact Dermatitis Society, North American Contact Dermatitis Group. 2006;17:3-11.
Sensitive skin is understood by some authors as the cutaneous manifestation with more exuberant symptomatology than signs, which includes the burning or stinging sensation on the face after application of a single or a group of facial products, without presence of frankly established erythema, thus differing from clinical pictures of contact dermatitis irritation.354354. Inamadar AC, Palit A. Sensitive skin: an overview. Indian J Dermatol Venereol Leprol. 2013;79:9-16.
Many patients perceive themselves as having "sensitive skin" without in fact presenting the clinical picture related to this dermatosis. Furthermore, nearly 20% of contact allergies attributed to cosmetics cite sunscreens, requiring a differential etiological diagnosis. Adult women with actinic damage present more allergies, while they are more rare in children.355355. Victor FC, Cohen DE, Soter NA. A 20-year analysis of previous and emerging allergens that elicit photoallergic contact dermatitis. J Am Acad Dermatol. 2010;62:605-10.
Among the substances, minerals such as titanium dioxide are rarely allergenic, but there is evidence that others, such as PABA (paraminobenzoic acid), may be very allergenic.356356. Avenel-Audran M, Dutartre H, Goossens A, Jeanmougin M, Comte C, Bernier C, et al. Octocrylene, an emerging photoallergen. Arch Dermatol. 2010;146:753-7.
The "Guide for Safety Evaluation of Cosmetic Products (Guia para Avaliação de Segurança de Produtos Cosméticos)" of the National Agency for Sanitary Vigilance (Agência Nacional de Vigilância Sanitária - Anvisa) defines the characteristics and the necessary safety tests (cumulative irritability, sensitization, phototoxicity, cutaneous photoallergy and safety trials using it in sensitive skin populations) that the cosmetic should present to have an "Indicated for sensitive skin" label.156156. Agência Nacional de Vigilância Sanitária. Guia de Avaliação de Segurança de produto cosmético. 2 ed. Brasília: Anvisa; 2003.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Photoprotection for sensitive skin patients should preferably use products with an "Indicated for sensitive skin" label, as required by ANVISA.
-
Protectors with fragrance are not recommended for sensitive skin patients.
Contact Dermatitis
Adverse reactions caused by sensitization to sunscreen, as mentioned before, are not common. Among the contact dermatitides, those of the irritative type are more frequent than those of the sensitization type.
The main etiological agent for sensitization to sunscreen (finished product) are perfumes, when present in their composition, followed by preservatives. The specific active ingredients for sun protection (UV filters) rarely are sensitizers.357357. Metry DW, Hebert AA. Topical therapies and medications in the pediatric patient. Pediatr Clin North Am. 2000;47:867-76.
Among the photoprotective actives, those derived from paraminobenzoic acid, the benzophenones, the octocrylene and the avobenzone are more frequently related to sensitization.353353. Scheuer E, Warshaw E. Sunscreen allergy: A review of epidemiology, clinical characteristics, and responsible allergens. Dermatitis : contact, atopic, occupational, drug : official journal of the American Contact Dermatitis Society, North American Contact Dermatitis Group. 2006;17:3-11.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Photoprotection for patients with history of contact dermatitis caused by sunscreens should be preferably achieved with products that contain only inorganic filters and without fragrance.
-
Contact tests may be recommended for adequate investigation.
Rosacea
Rosacea is a chronic disorder, characterized by erythema, papules, pustules and telangiectasias; it predominates in the central face and varies from mild to exuberant forms, such as the rhinophyma, more frequent in men. It predominates in women in the 30 to 50 years old age group and it is estimated that from 1.5 to 10 % of the population is affected with this disorder.358358. Kennedy Carney C, Cantrell W, Elewski BE. Rosacea: a review of current topical, systemic and light-based therapies. G Ital Dermatol Venereol. 2009;144:673-88.
Although its pathogenesis is not completely defined, genetic and environmental factors have an impact in the exacerbation of the clinical picture. Foods like chocolate, coffee, some seasonings, tea, alcohol, systemic medications, such as cholinergic agents, vasodilators, rifampicin, emotional factors, physical exercises and solar radiation, among others, are factors associated with worsening of symptoms.358358. Kennedy Carney C, Cantrell W, Elewski BE. Rosacea: a review of current topical, systemic and light-based therapies. G Ital Dermatol Venereol. 2009;144:673-88.
Therapy includes from topical medication to surgical procedures. In every form, patients are oriented regarding triggering factors and the importance of wearing the adequate sun protector.
Products that associate specific actives for topical treatment and sunscreens can and should be used; evidence shows better outcomes with this association.359359. Tan JK, Girard C, Krol A, Murray HE, Papp KA, Poulin Y, et al. Randomized placebo-controlled trial of metronidazole 1% cream with sunscreen SPF 15 in treatment of rosacea. J Cutan Med Surg. 2002;6:529-34.
Due to greater sensitivity and alterations in the cutaneous barrier function, patients with rosacea may present sensitivity to cosmetic and makeup products; however, makeup with sun protector may be used, always giving preference to those that are non alcoholic. Makeup with greenish tones is important to reduce the appearance of facial erythema. The National Rosacea Society, in the USA, recommends wearing makeup that includes UV radition protection, formulations without perfume, hypoallergenic and alcohol-free.360360. Nichols K, Desai N, Lebwohl MG. Effective sunscreen ingredients and cutaneous irritation in patients with rosacea. Cutis. 1998;61:344-6.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Photoprotection for patients with rosacea should follow the same principles of photoprotection for individuals with sensitive skin.
-
If possible, opt for less oily and non alcoholic preparations, such as cream gel.
Acne and oily skin
There are few studies in the literature on acne, oily skin and sun protection.
Individuals with a tendency to have oily skin, mainly adolescents, avoid wearing sunscreen because they believe this type of product worsens or triggers acne, which is more frequent in this age group.135135. Draelos ZD. Compliance and sunscreens. Dermatol Clin. 2006;24:101-4.,361361. Castanedo-Cazares JP, Torres-Alvarez B, Briones-Estevis S, Moncada B. [Inconsistency in sun protection factor (SPF) index in Mexico. The case of sunscreens for oily skin]. Gac Med Mex. 2005;141:111-4. There is great variety of products available in the market, offering options of skin protectors with this tendency.362362. Stechschulte SA, Kirsner RS, Federman DG. Sunscreens for non-dermatologists: what you should know when counseling patients. Postgrad Med. 2011;123:160-7.
In 2005, an experimental study with human subjects was carried out in Mexico to verify if the SPF informed on the packages of 12 products actually afforded the promised protection. All of the products were allegedly "non-comedogenic" or "not oily" and were targeted to the adolescent population, more prone to acne. None of the analyzed products complied with what their packages promised: the product that was closer to what it declared was a filter with several active substances (titanium dioxide, octocrylene, Mexoryl and others) that offered a 15.6 SPF, while it informed SPF 20 protection.361361. Castanedo-Cazares JP, Torres-Alvarez B, Briones-Estevis S, Moncada B. [Inconsistency in sun protection factor (SPF) index in Mexico. The case of sunscreens for oily skin]. Gac Med Mex. 2005;141:111-4.
Protectors in the form of gel, cream gel or fluid are ideal for patients with oily and acneic skin. It is important for patients with acne to avoid inorganic filters, due to their dense and oily consistency.135135. Draelos ZD. Compliance and sunscreens. Dermatol Clin. 2006;24:101-4. New technologies are being used to enhance product cosmetic characteristics and make them less oily, which may improve adherence to protector wearing by this group of individuals. Among these technologies, the use of silica and its derivatives has been very well accepted by users since it reduces the "oily touch" of the product, decreasing residual shine while adsorbing exceeding oiliness.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Photoprotection for patients with oily or acneic skin should be achieved with products especially developed for this purpose and that demonstrate the promised effect, like control or reduction of skin oiliness, through specific studies.
-
Vehicles in the form of gel, cream gel or fluid are the most recommended for this group of patients.
Vitiligo
Patients with vitiligo have a diminished risk of developing skin cancer, both melanoma and non melanoma, during their lifetime, and although there are isolated reports stating the contrary, apparently phototherapy does not increase the risk, as demonstrated in epidemiological study.363363. Teulings HE, Overkamp M, Ceylan E, Nieuweboer-Krobotova L, Bos JD, Nijsten T, et al. Decreased risk of melanoma and nonmelanoma skin cancer in patients with vitiligo: a survey among 1307 patients and their partners. Br J Dermatol. 2013;168:162-71.
A possible explanation for this would be that patients with vitiligo tend to protect themselves more with clothes exactly because they know that the skin in the regions with lesions is more sensitive to the sun and is easily severely burned, generating actinic damage.364364. Yashiro K, Nakagawa T, Takaiwa T, Inai M. Actinic keratoses arising only on sun-exposed vitiligo skin. Clin Exp Dermatol. 1999;24:199-201.
Vitiligo treatment has as principle the activation and migration of melanocytes from the borders of the depigmented lesion, penetrating 2 to 3 mm into the lesion; the larger reserves of melanocytes are close to hair follicles; therefore hairless areas (palms, soles of feet) respond poorly to the treatment.365365. Hercogova J, Buggiani G, Prignano F, Lotti T. A rational approach to the treatment of vitiligo and other hypomelanoses. Dermatol Clin. 2007;25:383-92, ix.,366366. Nordlund JJ, Halder RM, Grimes P. Management of vitiligo. Dermatol Clin. 1993;11:27-33.
The guidelines of the American Academy of Dermatology are that a broad spectrum photoprotector be applied after the therapy session with psoralene and phototherapy, before the patient leaves the office, since inadvertent and unprotected sun exposure, six to eight hours after the session, may cause phototoxicity and blisters.366366. Nordlund JJ, Halder RM, Grimes P. Management of vitiligo. Dermatol Clin. 1993;11:27-33.Due to the sensitivity of depigmented skin, both to UVA and UVB rays, the broad spectrum photoprotector is mandatory for patients with vitiligo, to prevent sunburns. However, all the exposed skin, and not only the lesions, should be protected.366366. Nordlund JJ, Halder RM, Grimes P. Management of vitiligo. Dermatol Clin. 1993;11:27-33.
Sunscreen protection brings with it another benefit: one of the complaints of patients having phototherapy is the increased contrast between the area of the lesion and normal skin, which tans under radiation. Thus, when irradiating the lesion, the treatment would darken the normal skin as well. By diminishing tanning of the normal skin, this contrast is less marked. The protection factor has to be at least 15 for skins type I or II, and wearing protective clothes and hats is recommended.365365. Hercogova J, Buggiani G, Prignano F, Lotti T. A rational approach to the treatment of vitiligo and other hypomelanoses. Dermatol Clin. 2007;25:383-92, ix. Camouflage of lesions with products containing pigments may be used.365365. Hercogova J, Buggiani G, Prignano F, Lotti T. A rational approach to the treatment of vitiligo and other hypomelanoses. Dermatol Clin. 2007;25:383-92, ix.,366366. Nordlund JJ, Halder RM, Grimes P. Management of vitiligo. Dermatol Clin. 1993;11:27-33.
Some patients with very large lesions may opt for depigmentation of the skin without lesion. In such cases, photoprotection, including wearing sunscreen and avoiding outdoor activities, are measures to be taken for a whole lifetime8686. Glanz K, Steffen AD, Schoenfeld E, Tappe KA. Randomized Trial of Tailored Skin Cancer Prevention for Children: The Project SCAPE Family Study. J Health Commun. 2013;18:1368-83. and the patient should be made aware of this fact.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Photoprotection for patients with vitiligo is mandatory, especially in the affected areas.
-
The dermatologist should advise about the use of mechanical photoprotective measures, associated with the use of topical sunscreen with high SPF and balanced UVA protection.
-
Special attention should be paid to photoprotection after the phototherapy sessions.
Specific areas
Scalp and hair
Hair offers natural protection to the scalp, particularly hair in darker tones. Bald patients or those with light and thinning hair need to wear sunscreen on the areas of the scalp without hair, due to the high exposure of the region, even though it was not exposed in childhood and adolescence.367367. Trueb RM. Is androgenetic alopecia a photoaggravated dermatosis? Dermatology. 2003;207:343-8.
Concerning hair photoprotection, the approach does not aim at prevention of skin cancer, as hair does not undergo neoplastic processes.368368. Draelos ZD. Sunscreens and hair photoprotection. Dermatol Clin. 2006;24:81-4. Nevertheless, there is a cosmetic importance. The most often reported effects are alterations in coloration due to oxidation of hair pigmentation, pheomelanin and eumelanin, forming oxymelanin.369369. Signori V. Review of the current understanding of the effect of ultraviolet and visible radiation on hair structure and options for photoprotection. Journal of cosmetic science. 2004;55:95-113.Furthermore, UVR damages hair lipids, leading to dryness and increased fragility; the lipid film is responsible for the shine and malleability of hair. Without this protection, hair is subject to static electricity and fractures when it is combed, which makes the hair frizzy.368368. Draelos ZD. Sunscreens and hair photoprotection. Dermatol Clin. 2006;24:81-4.
Hair photoprotection is achieved with the same active ingredients used on the skin, added to formulations for hair use, like conditioners, gels, sprays. The main problem is the difficulty to manufacture a homogeneous film that will protect the entire surface of hairs, besides the problem of creating a formula with good adherence to the cuticle, but without making it very oily.
The products that tend to remain in the hair after it is washed, like gels, sprays and particularly the creamy ones, offer even greater protection when compared to the others, but it is still insufficient. This dilemma has led researchers to inquire if hair photoprotection could be achieved in any other way, perhaps through the internal structure of the hair shaft.368368. Draelos ZD. Sunscreens and hair photoprotection. Dermatol Clin. 2006;24:81-4.,370370. Maillan P. UV protection of artificially coloured hair using a leave-on formulation. Int J Cosmet Sci. 2002;24:117-22.
Ears
The ears are the fifth most common location affected by non melanoma skin cancers of the cephalic segment, responsible for around 5% of cases, according to recent study with more than 600 patients at the University of Cornell.371371. Ragi JM, Patel D, Masud A, Rao BK. Nonmelanoma skin cancer of the ear: frequency, patients' knowledge, and photoprotection practices. Dermatol Surg. 2010;36:1232-9. The proportion regarding gender in these cases was 17.6 men to 1 woman, due to the natural protection of hair. The most affected areas were the helix and antihelix regions, with little higher prevalence of squamous cell than basal cell (1:0.7) carcinomas.
Periorbital region
The periorbital region, besides being a frequent site for skin cancer, shows signs of aging and special care is necessary for this region due to its high sensitivity.372372. Bucay VW, Day D. Adjunctive skin care of the brow and periorbital region. Clin Plast Surg. 2013;40:225-36.
Exposing the human eye to solar radiation without due protection, in an intense or continuous and repeated way, may cause pathological changes such as photokeratitis and cataract. For an adequate eye protection against solar radiation effects, it is recommended to wear sunglasses, preferably those that demonstrate the capability of absorbing over 99% of ultraviolet radiation.373373. Tuchinda C, Srivannaboon S, Lim HW. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol. 2006;54:845-54. This measure would also be effective in diminishing the risk of emergence of cutaneous neoplasms in the periorbital region.374374. Lagerlund M, Dixon HG, Simpson JA, Spittal M, Taylor HR, Dobbinson SJ. Observed use of sunglasses in public outdoor settings around Melbourne, Australia: 1993 to 2002. Prev Med. 2006;42:291-6.
Preference is given to application of inorganic sun screens, due to their low allergic and irritant potential.372372. Bucay VW, Day D. Adjunctive skin care of the brow and periorbital region. Clin Plast Surg. 2013;40:225-36.
Another possibility is the use of makeup with inorganic protectors that play the role of barrier and absorb some sweat in the region, avoiding its contact with the eyes.375375. O'Donoghue MN. Eye cosmetics. Dermatol Clin. 2000;18:633-9.
Lips
The lower lip is a frequent site of neoplastic and preneoplastic actinic lesions. In a study with 362 beach workers from Rio Grande do Norte, around 27.1% had lip lesions.376376. Lucena EE, Costa DC, da Silveira EJ, de Lima KC. [Prevalence and factors associated with orolabial lesions in beach workers]. Rev Saude Publica. 2012;46:1051-7.
Use of lip protector is paramount for patients under intense sun exposure, particularly those that present a more protruding lower lip. It was demonstrated that the regular use of lipsticks with sunscreen reduce the frequency of lip cancer. These lipsticks must meet criteria such as broad spectrum protection and photostability.377377. Maier H, Schauberger G, Martincigh BS, Brunnhofer K, Honigsmann H. Ultraviolet protective performance of photoprotective lipsticks: change of spectral transmittance because of ultraviolet exposure. Photodermatol Photoimmunol Photomed. 2005;21:84-92.
As to the safety of lip protectors, there are experimental in vivo studies which show that the concentration of octyl methoxycinnamate - one of the most common components of lip sunscreen - necessary to cause fertility problems in rats was 450 mg/kg, demonstrating its low toxicity potential.378378. Schneider S, Deckardt K, Hellwig J, Kuttler K, Mellert W, Schulte S, et al. Octyl methoxycinnamate: two generation reproduction toxicity in Wistar rats by dietary administration. Food Chem Toxicol. 2005;43:1083-92.
Notwithstanding, in vitro studies evaluating the safety of ingesting inorganic protectors demonstrate that repeated mucosa exposures to low concentrations of zinc oxide result in persistent DNA damage,379379. Hackenberg S, Zimmermann FZ, Scherzed A, Friehs G, Froelich K, Ginzkey C, et al. Repetitive exposure to zinc oxide nanoparticles induces dna damage in human nasal mucosa mini organ cultures. Environ Mol Mutag. 2011;52:582-9. and the exposure of intestinal cells to titanium dioxide result in loss of villi, which could lead to malnutrition and malabsorption.380380. Koeneman BA, Zhang Y, Westerhoff P, Chen Y, Crittenden JC, Capco DG. Toxicity and cellular responses of intestinal cells exposed to titanium dioxide. Cell Biol Toxicol. 2010;26:225-38.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Photoprotection in specific areas should receive special attention of the dermatologist.
-
For individuals partially or totally bald, regular use of hats and photoprotetors on the scalp should be recommended.
-
The goal of hair photoprotection is esthetic maintenance of hair, and can be done with the same active ingredients used for the skin, added to formulations for hair care, such as conditioners, gels and sprays.
-
Photoprotection of ears can be done with regular sunscreen or products in a stick format.
-
In order to protect the periorbital regions, the use of sunglasses associated with sunscreen in a stick format should be recommended, as it presents greater adhesiveness to the skin, reducing the risk of stinging eyes.
-
Solar protection of lips is relevant and should be reinforced during intentional sun exposure or for outdoor workers, due to the risk of developing squamous cell carcinoma. Use of high-SPF sunscreen sticks is advised.
CHAPTER 8
SUN AND VITAMIN D
INTRODUCTION
Vitamin D is obtained by human beings from sunlight, diet (mainly fish and fortified milk) and supplements. Its action as a hormone and its regulation involving parathyroid hormone (PTH), calcium and phosphorus has many important physiological consequences, especially concerning skeletal health.
However, vitamin D receptors were evident in the majority of body cells and enzymes capable of converting circulating 25-hydroxyvitamin D (25 (OH) D) to its active form 1.25 dihydroxyvitamin D (1.25 (OH) D), leading to endless new findings about its function.381381. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-81.
Besides its protecting role against bone fractures, rickets, osteomalacia and osteoporosis, vitamin D is now proposed as a reducer of a spectrum of chronic diseases, including internal cancers, cardiovascular diseases, autoimmune diseases, metabolic disorders and mental diseases.382382. Holick MF. Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79:362-371.,383383. Grant WB. An estimate of premature cancer mortality in the U.S. due to inadequate doses of solar ultraviolet-B radiation. Cancer. 2002;94:1867-75.
Its importance was demonstrated in immunology and infectious diseases, and its deficiency associated with, for example, the increase of tuberculosis rates.384384. Liu PT, Stenger S, Li H, Wenzel L, Tan BH, Krutzik SR, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006;24:1770-1773.,385385. Wilkinson RJ, Llewelyn M, Toossi Z, Patel P, Pasvol G, Lalvani A, et al. Influence of vitamin D deficiency and vitamin D receptor polymorphisms on tuberculosis among Gujarati Asians in west London: a case-control study. Lancet. 2000;355:618-21. A recent study reported that incidence of flu in winter decreases when the adequate status of vitamin D is maintained.386386. Aloia JF, Li-Ng M. Re. epidemic influenza and vitamin D. Epidemiol Infect. 2007;135:1095-6.
At the same time that numerous indications of vitamin D for prevention and/or therapy of diseases appeared, its minimum value, considered as normal by researchers, led to an alarming insufficiency epidemic.387387. Ginde AA, Liu MC, Camargo CA Jr. Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004. Arch Intern Med. 2009;169:626-32.,388388. Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US population: 1988-1994 compared with 2000-2004. Am J Clin Nutr. 2008;88:1519-27.
It is assumed that public health campaigns about solar protection and changes in lifestyle may play a role in this reduction. Important aspects of ambient sunlight, photoprotection and status of vitamin D will be analyzed here.
Metabolism
More than 90% of vitamin D is obtained by skin production through sunlight.389389. Reichrath J. The challenge resulting from positive and negative effects of sunlight: how much solar UV exposure is appropriate to balance between risks of vitamin D deficiency and skin cancer? Prog Biophys Mol Biol. 2006;92:9-16.
When a photon of ultraviolet B light (UVB) (290-315 nm) reaches the skin, it photoisomerizes the 7-dehydrocholesterol (7-DHC) in the cell's membrane to precholecalciferol (previtamin D3), which is rapidly converted, through heat-isomerization, in cholecalciferol (vitamin D3). Peak blood levels of vitamin D3 occur after one day and is stored in body fat later on for release when necessary.
Vitamin D2 (ergosterol), originating from yeast and plants is obtained in the diet and follows the same metabolic pathway of vitamin D3. Vitamin D3 enters the circulation via vitamin D binding protein, is hydroxylated in the liver to calcidiol (25 (OH) D), and again hydroxylated, mainly in the kidneys, to its active form, calcitriol (1.25 (OH) D).390390. Holick MF. Environmental factors that influence the cutaneous production of vitamin D. Am J Clin Nutr. 1995;61:638S-645S.
However, both previtamin D3 and vitamin D3 are sensitive to UV radiation, and continuous exposure to UVB causes its photodegradation in the skin to inactive products.391391. Webb AR, DeCosta BR, Holick MF. Sunlight regulates the cutaneous production of vitamin D3 by causing its photodegredation. J Clin Endocrinol Metab. 1989;68:882-7.
Vitamin D3 maximum cutaneous synthesis is limited to 15-20% of the initial 7-DHC concentration, with less than one minimal erythema dose (MED) production plateau.390390. Holick MF. Environmental factors that influence the cutaneous production of vitamin D. Am J Clin Nutr. 1995;61:638S-645S.,392392. Webb AR. Who, what, where and when-influences on cutaneous vitamin D synthesis. Prog Biophys Mol Biol. 2006;92:17-25.
Serum concentration of 25 (OH) D is the value used to determine the status of vitamin D, as well as 1.25 (OH) D, which is under rigorous endocrine system control. The minimum recommended level of 25 (OH) D is currently controversial and under discussion. The implications of vitamin D deficiency remain uncertain and many suppositions are still uncorroborated.
The American Academy of Pediatrics and the American Society of Endocrinology consider the concentration of 20 ng/mL as the cutoff point for deficiency; on the other hand the American Institute of Medicine proposes that 16 ng/mL is the appropriate minimum level. The Society of Endocrinology recommends an additional classification of 21 to 29 ng/mL as insufficiency of vitamin D.393393. Chiu YE, Havens PL, Siegel DH, Ali O, Wang T, Holland KE, et al. Serum 25-hydroxyvitamin D concentration does not correlate with atopic dermatitis severity. J Am Acad Dermatol. 2013;69:40-6.
These values were associated with lower risk of fractures and suppression of PTH elevation, a deficiency marker which stimulates the production of 1.25 (OH) D for maintenance of intestinal calcium absorption.394394. Hollis BW. Assessment of vitamin D status and definition of normal circulating range of 25-hydroxyvitamin D. Curr Opin Endocrinol Diabetes Obes. 2008;15:489-94.
A level below 30 ng/mL (75 nmol/L) is considered "insufficient" by most specialists, and less than 20 ng/mL (50 nmol/L) is considered "deficient".395395. Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84:18-28.,396396. Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet. 1998;351:805-6.
Intoxication by vitamin D, associated with hypercalcemia and hyperphosphatemia, is extremely rare and may be caused by doses greater than 50,000 UI per day and a level of (25 (OH) D) above 150 ng/mL.381381. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-81.
Photodegradation of vitamin D3 produced by the skin avoids intoxication by vitamin D through sun exposure. With the whole body exposed to a single minimal erythema dose, the equivalent to about 10,000 IU to 20,000 IU of oral ingestion is produced.381381. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-81.,397397. Vieth R. Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. Am J Clin Nutr. 1999;69:842-56.
Estimates vary, but around half of MED of direct sunlight on arms and legs can produce the equivalent to around 3,000 IU of vitamin D3.381381. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-81.
Midday sun exposure twice a week, for 5-30 minutes, was suggested as sufficient for adequate production of vitamin D in white populations. Notwithstanding, as we will discuss, the need for exposure time suffers diverse influences and may be variable.381381. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-81.
Coincidentally, cutaneous synthesis of vitamin D3, as well as erythema (sunburn) occurs at its maximum approximately in the same wavelength of 296 nm of UVB, even though the action spectrum of erythema is extended to the UVA spectrum.398398. Parrish JA, Jaenicke KF, Anderson RR. Erythema and mel- anogenesis action spectra of normal human skin. Photochem Photobiol. 1982;36:187-91.,399399. Fioletov VE, McArthur LJ, Mathews TW, Marrett L. On the relationship between erythemal and vitamin D action spectrum weighted ultraviolet radiation. J Photochem Photobiol B. 2009;95:9-16.
With solar radiation, cutaneous synthesis of vitamin D3 reaches a maximum plateau after a short lapse of time, less than one MED.400400. Gilchrest BA. Sun exposure and vitamin D sufficiency. Am J Clin Nutr. 2008;88:570S-577S.
The whole skin is capable of synthesizing vitamin D, therefore when the entire body is exposed in an appropriate way, production occurs more rapidly and with less risk of burns than when, for example, only the head is exposed. If only 10% of the skin is exposed to adequate UVB radiation, the synthesis of vitamin D will take 10 times longer than it would take if the whole body were exposed.392392. Webb AR. Who, what, where and when-influences on cutaneous vitamin D synthesis. Prog Biophys Mol Biol. 2006;92:17-25.
The amount of time necessary, considered as "adequate" exposure, will depend on several factors, including personal, behavioral and environmental ones (Chart 10).
ENVIRONMENTAL FACTORS THAT AFFECT CUTANEOUS PRODUCTION OF VITAMIN D
Solar zenith angle: latitude, season, time of day
Before UVB solar radiation reaches the skin to start the synthesis of vitamin D, it must travel through the atmosphere.
The main determinant of potential UVB radiation available is the sun angle in the sky compared to the vertical or solar zenith angle (zenith). The more directly above the position of the sun, the smaller the solar zenith angle is, the shorter the path run by UV radiation and the smaller the possibility of absorption or deflection of photons before reaching the skin is.392392. Webb AR. Who, what, where and when-influences on cutaneous vitamin D synthesis. Prog Biophys Mol Biol. 2006;92:17-25.
Three factors influence the solar zenith angle: latitude, season and time of day. In higher latitudes and mainly during winter, the sun is not so verticalized in the sky at noon in comparison to what occurs in lower latitudes. Thus, UVB radiation travels a long distance through the stratospheric ozone layer and atmosphere, being attenuated until reaching the surface of the Earth.
Thieden et al. recently analyzed ambient UV radiation and healthy Danish indoor workers, with personal dosimeters (sensitive to erythema spectrum) to record UV exposure throughout the year.401401. Thieden E, Philipsen PA, Wulf HC. Ultraviolet radiation exposurepattern in winter compared with summer based on time-stamped personal dosimeter readings. Br J Dermatol. 2006;154:133-8.
The data revealed that six months of winter represent only 10% of yearly ambient UV radiation and less than 3% of total erythematous doses in subjects, in comparison with summer months. The individuals tend to avoid going out with the skin exposed and, this way, receive only 0.82% of available UV radiation during the winter.
Observing the results of a study in the North (latitude 42-46 º N) and South (33-34 º N) of the United States, the yearly ambient UV radiation available in Denmark (56 º N) was of 3,757 erythematous doses, in comparison with 6,193 in the North of the United States and 8,710 in the South, showing that total doses of UV radiation are much larger in lower latitudes.401401. Thieden E, Philipsen PA, Wulf HC. Ultraviolet radiation exposurepattern in winter compared with summer based on time-stamped personal dosimeter readings. Br J Dermatol. 2006;154:133-8.,402402. Godar DE, Wengraitis SP, Shreffler J, Sliney DH. UV doses of Americans. Photochem Photobiol. 2001;73:621-9.
In the United States, the dose of UV radiation observed during winter was 2330% of the total annual UV dose (compared with 10% in Denmark), accounting for smaller variation of maximum zenith angles over a year in the United States than in Denmark.
Evidence in vitro about the influence of zenith angles in the production of vitamin D came from Webb et al., who exposed a solution of 7-DHC to solar radiation in Edmonton, Canada (52 º N), Boston (42 º N) and Los Angeles (34 º N), USA, and San Juan, Puerto Rico (18 º N).403403. Webb AR, Kline L, Holick MF. Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab. 1988;67:373-8.
Their experiments showed that photoconversion of 7-DHC to previtamin D3 was at its maximum in the months of June and July. In Boston, it was demonstrated that, from November to February, pre-vitamin D3 was not detected. In Edmonton, further to the North, the production of previtamin D3 stopped in October and did not restart until mid-April, whereas in Los Angeles and Puerto Rico previtamin D3 production occurred year-round.
Besides latitude and season, Luet al. demonstrated the influence of time of day.404404. Lu Z, Chen TC, Holick MF. Influence of season and time of day on the synthesis of vitamin D3. In: Holick MF, Kligman A, editors. Proceedings of the Biologic Effects of Light Symposium. Berlin: Walter De Gruyter & Co; 1992. p. 48-52. Measuring production of previtamin D3 in sunny days in Boston, they discovered that the synthesis started at 07:00 a.m. during the winter and lasted until 5:00 p.m.. In the months of spring and autumn, the window for photo-conversion started several hours later, around 09:00 a.m. and lasted only until 3:00 p.m.. The window narrowed seasonally until the synthesis diminished completely.
The decrease of solar zenith angle, either by latitude increase, season (winter) or time of day, is the cause of this vitamin D production decrease phenomenon.
A series of studies published in scientific literature has shown the relationship between sun exposure, skin cancer and synthesis of vitamin D. However, the scarcity of medical data, particularly in developing countries, makes global evaluation of sun exposure impact on vitamin D serum levels difficult.
According to a study published by Paula Correa et al.,405405. de Paula Corrêa M, Ceballos JC. solar ultraviolet radiation measurements in one of the most populous cities of the world: aspects related to skin cancer cases and vitamin D availability. Photochem Photobiol. 2010;86:438-44. which evaluated UVB radiation levels in the city of São Paulo (SP) - Brazil, during a period of 3 years, non-intentional exposure to outdoor environment for 10 minutes daily, hands and face only, would be enough for adequate production of vitamin D in a phototype II individual.
Data presented by this study considered cloudy and rainy days; hence, only 10 minutes of hands and face exposure outdoors, whatever the weather, would be sufficient for vitamin D production in the city of São Paulo.
This study presented measurements of UV index in the period from 2005 to 2008. It was found that 65% of UV index measured within 2 hours at noon, local time, during summer, was too elevated (8 < UVI < 10), and many times extreme levels were demonstrated (UVI > 11), according to World Health Organization (WHO).
During the winter, 40% of readings around noon showed high or very high levels. In spite of recent worrying statistics, which showed that non-melanoma skin cancers correspond to around 28% of more than one million new cancer cases, solar protection is not considered a relevant problem in these urban areas.
UV radiation readings demonstrated that, in all months, its levels are high enough to guarantee adequate vitamin D production in human skin, during incidental sun exposure.
In short, UV radiation levels observed in the city of São Paulo indicate that prevention of solar superexposure is necessary in any time of the year, with the synthesis of vitamin D guaranteed with a minimum exposure of about 10 minutes per day.405405. de Paula Corrêa M, Ceballos JC. solar ultraviolet radiation measurements in one of the most populous cities of the world: aspects related to skin cancer cases and vitamin D availability. Photochem Photobiol. 2010;86:438-44.
Altitude
Higher altitudes result in shorter distances and less dense atmosphere, favoring the passage of UVB radiation. There is a 4% increase of the amount that reaches exposed skin for each 300m increase in altitude.406406. World Health Organization. Global solar UV index. A practical guide. Geneva, Switzerland: World Health Organization; 2002.
Even though it is not a perfect reading of UVB radiation or the capability of synthesizing vitamin D, the UV index is a non-tridimensional representation of erythemal action of the weighted irradiance spectrum. The greater values of UV index (20-25) were detected in Mauna Loa Observatory, in Hawaii (altitude 11,155 feet, latitude 21 º N) and in the area of Peruvian Altiplano (altitude 12,800 feet, latitude 15 º N).399399. Fioletov VE, McArthur LJ, Mathews TW, Marrett L. On the relationship between erythemal and vitamin D action spectrum weighted ultraviolet radiation. J Photochem Photobiol B. 2009;95:9-16.
Although the vitamin D synthesis potential may be better in higher altitudes, a study demonstrated that adult Tibetans, who live in relatively low latitudes and high altitudes (altitude over 12 thousand feet, latitude 29-32 º N), had low levels of 25 (OH) D, with 40-100% below 30 ng/mL, depending on the population.407407. Norsang G, Ma L, Dahlback A, Zhuoma C, Tsoja W, Porojnicu A, et al. The vitamin D status among Tibetans. Photochem Photobiol. 2009;85:1028-31.
Nomads presented the lowest levels, all of them below 30 ng/mL and 80% below 12 ng/mL, while farmers presented the most elevated levels, 40% below 30 ng/mL and none below 12 ng/mL.
Tibetan diet is extremely poor in vitamin D and the cold weather makes covering most of the skin mandatory. According to the authors' conclusion, these factors are responsible for low levels of vitamin D, even though they see five times more yearly UVB radiation than Norwegians, who live farther north and in very low altitudes.407407. Norsang G, Ma L, Dahlback A, Zhuoma C, Tsoja W, Porojnicu A, et al. The vitamin D status among Tibetans. Photochem Photobiol. 2009;85:1028-31.
Atmospheric conditions
UV radiation travels an atmospheric distance, being dispersed and absorbed along the way. UVB radiation, with a shorter wavelength, experiments greater attenuation than UVA radiation and the visible light spectrum, which present longer wavelengths.392392. Webb AR. Who, what, where and when-influences on cutaneous vitamin D synthesis. Prog Biophys Mol Biol. 2006;92:17-25.
UVB radiation crosses a non-homogeneous atmosphere and its characteristics have significant influence over the amount that reaches the surface of the Earth - a factor that probably became particularly important during the Industrial Revolution. The advent of coal-burning plants and black clouds of smoke hovering over London in the 17th century brought awareness about bone-deforming diseases/rickets.408408. O'Riordan JL. Rickets in the 17th century. J Bone Miner Res. 2006;21:1506-10.
Rickets occurs due to bone mineralization deficient in calcium phosphate, which may be secondary to vitamin D deficiency or malnutrition. Even though it has been probably described since antiquity, the increase in cases with the onset of smoky air, in the end of 17th century, started the speculation that pollution was the culprit, although its mechanism was unknown and vitamin D had not been totally discovered yet.408408. O'Riordan JL. Rickets in the 17th century. J Bone Miner Res. 2006;21:1506-10.
It is reasonable to assume, today, that blockage of UVB rays, due to the absorption of particulate material over the cities, plays a role in the manifestation. However, tall buildings and narrow streets, together with indoor work, certainly diminished the sun exposure of the population.
The ozone in the stratosphere is especially important, since it absorbs essentially all UV radiation with wavelengths shorter than 290 nm (synthesis of previtamin D3 is possible up to 270 nm) and attenuates UVB radiation over 290 nm.409409. MacLaughlin JA, Anderson RR, Holick MF. Spectral character of sunlight modulates photosynthesis of previtamin D3 and its photoisomers in human skin. Science. 1982;216:1001-3.,410410. Engelsen O, Brustad M, Aksnes L, Lund E. Daily duration of vitamin D synthesis in human skin with relation to latitude, total ozone, altitude, ground cover, aerosols and cloud thickness. Photochem Photobiol. 2005;81:1287-90.
Higher concentrations of ozone are usually found in higher latitudes, towards the poles and lower concentrations in the tropics. Ozone levels anywhere may change up to 20% per day, with wind and pollution patterns which may produce ozone and other UVB attenuating substances.381381. Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-81.
One hundred and twenty one (121) postmenopausal women inhabiting urban and rural areas were studied in Belgium, where ozone levels in the troposphere, due to pollution, are three levels greater in Brussels than on the other side of the country.411411. Manicourt DH, Devogelaer JP. Urban tropospheric ozone increases the prevalence of vitamin D deficiency among Belgian postmenopausal women with outdoor activities during summer. J Clin Endocrinol Metab. 2008;93:3893-9.
Even with greater sun exposure, urban women had much higher prevalence of 25 (OH) D below 30 ng/mL (84 vs 38%, p < 0.001).
Levels of 25 (OH) D in women who lived in rural areas was twice the levels of urban women, and the sun exposure required to reach equivalent levels of 25 (OH) D was three times greater in urban women than in those who lived in rural areas.
Cloud coverage is also important in determining available UVB radiation for the synthesis of vitamin D - low and thick clouds have a higher capability to reduce the amount of UVB that reaches the ground. In truth, a dense cloud coverage may prevent 99% of UVB radiation from reaching the soil, thus making cutaneous synthesis of vitamin D impossible, even over the Equator line.410410. Engelsen O, Brustad M, Aksnes L, Lund E. Daily duration of vitamin D synthesis in human skin with relation to latitude, total ozone, altitude, ground cover, aerosols and cloud thickness. Photochem Photobiol. 2005;81:1287-90.
Nevertheless, clouds may also reflect UV radiation, and so does the ground covering, a phenomenon known as "albedo".392392. Webb AR. Who, what, where and when-influences on cutaneous vitamin D synthesis. Prog Biophys Mol Biol. 2006;92:17-25.
Snow is capable of reflecting 90% of UV radiation, considerably increasing the amount of UVB radiation that reaches the skin, the equivalent to an altitude increase of 3,000 meters. Sand, cement and other construction materials reflect approximately 20%, whereas soil, rocks and vegetation reflect a lot less.392392. Webb AR. Who, what, where and when-influences on cutaneous vitamin D synthesis. Prog Biophys Mol Biol. 2006;92:17-25.
CONSTITUTIONAL FACTORS THAT AFFECT THE CUTANEOUS PRODUCTION OF VITAMIN D
Skin pigmentation
The degree of skin pigmentation and age influence vitamin D production.
The onset of rickets and vitamin D deficiency among dark-skinned and Indian populations, immigrants of latitude north cities in the United States and United Kingdom, while similar populations in their countries of origin did not have this problem led to speculation that the increase of skin pigmentation could predispose dark-skinned individuals to vitamin D deficiency.412412. Dunnigan MG, Paton JP, Haase S, Mcnicol GW, Gardner MD, Smith CM. Late rickets and osteomalacia in the Pakistani community in Glasgow. Scott Med J. 1962;7:159-67.
413. Bachrach S, Fisher J, Parks JS. An outbreak of vitamin D deficiency rickets in a susceptible population. Pediatrics. 1979;64:871-7.
414. Rudolf M, Arulanantham K, Greenstein RM. Unsuspected nutritional rickets. Pediatrics 1980: 66: 72-76.-415415. Hodgkin P, Kay GH, Hine PM, Lumb GA, Stanbury SW. Vitamin-D deficiency in Asians at home and in Britain. Lancet. 1973;2:167-71.
Although diet has been many times a confusing factor, an investigation was proposed to elucidate the role of melanin concentration in photoproduction of vitamin D. Melanin absorbs UV radiation in the epidermis, which limits the number of available photons to convert 7-DHC molecules in previtamin D3.
Fitzpatrick phototype is commonly used to classify the type of skin, describing the melanin content in the epidermis and cutaneous reaction (tanning or burning) to UV radiation after a prolonged non-exposure period.416416. Walker SL, Hawk JLM, Young AR. Acute and chronic effects of ultraviolet radiation on the skin. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitz-patrick's dermatology in general medicine. 6th ed. New York, NY: McGraw-Hill, 2003:1275-1282. 589. These phototypes also indicate propensity to solar damage and vitamin D production.
Phototypes I and II present light skin, which burns easily and rarely tans, whereas phototype III presents light skin, however with more ability to tan, and, therefore, will have less UV radiation damage later. Phototypes IV-VI present darker skin, with a larger amount of melanin, that tans easily and rarely burns.
In theory, higher phototypes tend to diminish in the population as the distance from the Equator increases, with greater prevalence of light skin in higher latitudes, where UVB must be maximized for vitamin D production and dark skin in equatorial regions, where UV radiation is widely available during the whole year.415415. Hodgkin P, Kay GH, Hine PM, Lumb GA, Stanbury SW. Vitamin-D deficiency in Asians at home and in Britain. Lancet. 1973;2:167-71.
Consequently, the risk of sunburns and skin cancer is greater when light-skinned individuals travel to lower latitudes, and deficiency of vitamin D, as mentioned above, is more prevalent in polar regions.
An initial study by Clemens et al., in 1982, exposed several black and white patients to a single dose of ultraviolet radiation.417417. Clemens TL, Adams JS, Henderson SL, Holick MF. Increased skin pigment reduces the capacity of skin to synthesize vitamin D3. Lancet. 1982;1:74-6. In white individuals, serum levels of 25 (OH) D increased 30% to 50% compared to basal levels within 24 to 48 hours after exposure, whereas in black individuals it did not have any effect.
After an UV radiation exposure six times greater than the one white patients received, only one of the black patients presented an increase of 25 (OH) D 24 hours later, although smaller than in all of the white individuals with the initial dose only.
This was the first time that skin pigmentation limitation of in vivo vitamin D production capacity was corroborated. The same group divulged data revealing that pigmented skin (ex vivo?) requires longer UV radiation exposure periods to produce similar levels of previtamin D3 in comparison with light skin.418418. Holick MF, MacLaughlin JA, Doppelt SH. Regulation of cutaneous previtamin D3 photosynthesis in man: skin pigment is not an essential regulator. Science. 1981;211:590-3.
Relatively less Vitamin D3 is produced per exposure unit to UV radiation, however, after repeated UV doses, high concentrations of melanin do not prevent vitamin D levels from reaching values considered sufficient.
This was confirmed by Lo et al., who determined MED in six Pakistani and Indian immigrants (phototypes III-V) and four white controls (phototypes II-III) in the United Kingdom, and next irradiated the whole body of each individual with 1.5 MED of UV radiation.419419. Lo CW, Paris PW, Holick MF. Indian and Pakistani immigrants have the same capacity as Caucasians to produce vitamin D in response to ultraviolet irradiation. Am J Clin Nutr. 1986;44:683-5.
Both groups had similar increases in vitamin D levels on the following day and there were no significant differences in serum concentrations of vitamin D between the two groups. Even though greater total exposure to UV radiation was necessary for higher phototypes (MED for the darkest patient was five times larger than the smallest control), the total capacity for vitamin D production was not affected by skin type and it is similar in response to equivalent MED.
Age
The decreasing levels of vitamin D in the elderly is well known, with multiple factors involved, including lack of sun exposure, malnutrition and malabsorption.420420. MacLaughlin J, Holick MF. Aging decreases the capacity of the skin to produce vitamin D3. J Clin Invest. 1985;76:1536-8.,421421. Weisman Y, Schen RJ, Eisenberg Z, Edelstein S, Harell A. Inadequate status and impaired metabolism of vitamin D in the elderly. Isr J Med Sci. 1981;17:19-21.
The reduction of efficiency in synthesizing vitamin D with age was analyzed in several studies, showing that, even with abundant sun exposure, serum levels of 25 (OH) D are smaller in healthy older people when compared to younger controls. Seasonal variations also diminish or even disappear with advancing age.421421. Weisman Y, Schen RJ, Eisenberg Z, Edelstein S, Harell A. Inadequate status and impaired metabolism of vitamin D in the elderly. Isr J Med Sci. 1981;17:19-21.,422422. Lester E, Skinner RK, Wills MR. Season variation in serum- 25-hydroxyvitamin-D in the elderly in Britain. Lancet. 1977;1:979-80.
The capability for synthesizing vitamin D is based on the availability of 7-DHC. MacLaughlin and Holick demonstrated that, with aging, there is a reduction in quantity of 7-DHC in the epidermis; likewise, the potential for vitamin D3 production.420420. MacLaughlin J, Holick MF. Aging decreases the capacity of the skin to produce vitamin D3. J Clin Invest. 1985;76:1536-8.
The authors obtained skin samples of six patients, all phototype III, with identical surface areas, and measured the quantity of 7-DHC, which decreased approximately in half from age 21 to 88. Next, the specimens were exposed to equal amounts of UV radiation and the resultant synthesis of previtamin D3 was quantified.
By using as a reference a skin sample from an 8-year-old patient, an 18-year-old man produced 80% of previtamin D3 amount, a 77-year-old patient 37% and another 82-year-old patient 40%, allowing the possibility of inferring the decreasing capability of previtamin D3 synthesis by 2.5 times in the last years of life.
As decreasing skin thickness occurs with aging 422422. Lester E, Skinner RK, Wills MR. Season variation in serum- 25-hydroxyvitamin-D in the elderly in Britain. Lancet. 1977;1:979-80.
423. Dattani JT, Exton-Smith AN, Stephen JM. Vitamin D status of the elderly in relation to age and exposure to sunlight. Hum Nutr Clin Nutr. 1984;38:131-7.-424424. Shuster S, Black MM, McVitie E. The influence of age and sex on skin thickness, skin collagen and density. Br J Dermatol. 1975;93:639-43. one could suppose that the reduction of pre-vitamin D3 synthesis capability would be related to this thinning; however, the authors showed that the synthesis of previtamin D3 is linearly related to concentration of 7-DHC and not with cutaneous thickness.
However, Need et al. found positive correlation between skin thickness and serum levels of 25 (OH) D, but did not test cutaneous response to sun exposure and match it with vitamin D production.425425. Need AG, Morris HA, Horowitz M, Nordin C. Effects of skin thickness, age, body fat, and sunlight on serum 25-hydroxyvitamin D. Am J Clin Nutr. 1993;58:882-5.
Despite vitamin D production becoming less efficient with advancing age, Webb et al. demonstrated that it is possible for elderly white nurses residing in Boston to maintain adequate levels of 25 (OH) D (defined as > 15 ng/mL in their 1990 study) through-out the year, by means of casual sun exposure, without the need for oral supplementation.426426. Webb AR, Pilbeam C, Hanafin N, Holick MF. An evaluation of the relative contributions of exposure to sunlight and of diet to the circulating concentrations of 25hydroxyvitamin D in an elderly nursing home population in Boston. Am J Clin Nutr. 1990 Jun;51:1075-81.
Oral supplementation of vitamin D drastically reduced the number of patients with levels below 15 ng/mL (to less than 5%) during the whole year, however, it minimized in a more intense way the seasonal decrease in winter, when up to 40% of the supplemented group presented 25 (OH) D serum concentrations smaller than 15 ng/mL.
This value is well below reference values used nowadays, and article data did not allow the percentage of patients with values over 20 or 30 ng/mL to be determined.
Conditions that occur with the decrease of 7-DHC
Intuitively, one may suppose that malabsorption syndromes or drugs to reduce cholesterol could diminish the concentration of 7-DHC in the skin, but this does not seem to be true.
A study involving vitamin D-deficient patients carrying Crohn's disease, primary biliary cirrhosis and idiopathic pseudo-obstruction, showed normal 7-DHC skin concentrations (actually, elevated in comparison with controls), hence the low 7-DHC concentration was not the cause of vitamin D deficiency in this population of patients.427427. Paterson CR, Moody JP, Pennington CR. Skin content of 7-dehydrocholesterol in patients with malabsorption. Nutrition. 1997;13:771-3.
In a study on pravastatin, an inhibitor of HMG-CoA reductase, or statin, serum increase of vitamin D3 after several doses of whole body UV radiation, was identical in patients using the medication for 3 months and in controls, although the concentration of 7-DHC in the skin was not measured.428428. Dobs AS, Levine MA, Margolis S. Effects of pravastatin, a new HMG-CoA reductase inhibitor, on vitamin D synthesis in man. Metabolism. 1991;40:524-8.
No decreasing levels of 25 (OH) D were found in the studies involving vitamin D and statins. By the way, the use of statin has been associated with the increase of 25 (OH) levels, although the mechanism has not been fully understood yet.430430. Montagnani M, Loré F, Di Cairano G, Gonnelli S, Ciuoli C, Montagnani A, et al. Effects of pravastatin treatment on vitamin D metabolites. Clin Ther 1994;16:824-829.
431. Pérez-Castrillón JL, Vega G, Abad L, Sanz A, Chaves J, Hernandez G, et al. Effects of atorvastatin on vitamin D levels in patients with acute ischemic heart disease. Am J Cardiol. 2007;99:903-5.-432432. Aloia JF, Li-Ng M, Pollack S. Statins and vitamin D. Am J Cardiol. 2007;100:1329.
A select group that presents decreasing skin 7-DHC levels is the one with sunburned patients. A study that exposed biopsies of scars from burns to UVB radiation, showed that the 7-DHC concentration in the burned skin was less than half the one presented by the control group (normal skin) (p = 0.016).433433. Klein GL, Chen TC, Holick MF, Langman CB, Price H, Celis MM. Synthesis of vitamin D in skin after burns. Lancet. 2004;363:291-2.
Conversion of 7-DHC to previtamin D3 was only 64% in comparison with controls (p = 0.004), suggesting that besides the decrease in 7-DHC, there is a mechanism not yet elucidated that reduces the conversion of 7-DHC to previtamin D3.
Healthy skin, adjacent to cicatricial areas, also presented reduction of 7-DHC and photoconversion to previtamin D3, but to a lesser extent. Vitamin D deficiency and its consequences are commonly observed in patients with burn scars which cover over 40% of the body surface; this may be due to diminished synthesis capability.434434. Klein GL, Herndon DN, Goodman WG, Langman CB, Phillips WA, Dickson IR, et al. Histomorphometric and biochemical characterization of bone following acute severe burns in children. Bone. 1995;17:455-60.,435435. Klein GL, Langman CB, Herndon DN. Vitamin D depletion following burn injury in children: a possible factor in post- burn osteopenia. J Trauma. 2002;52:346-50.
BEHAVIORAL FACTORS THAT AFFECT CUTANEOUS PRODUCTION OF VITAMIN D
Avoid the sunlight
Preventing exposure to UVB radiation may be done in several ways, either by avoiding it completely (staying indoors), covering the skin with clothes or applying a sunscreen.
To illustrate the potential effect of complete absence of UVB radiation over vitamin D levels, we mention two studies, in which healthy members from submarine tripulations presented a reduction of 40% in serum concentration of 25 (OH) D after two months under water, independently from food fortification.436436. Preece MA, Tomlinson S, Ribot CA, Pietrek J, Korn HT, Davies DM, et al. Studies of vitamin D deficiency in man. Q J Med. 1975;44:575-89.,437437. Dlugos DJ, Perrota PL, Horn WG. Effects of the submarine environment on renalstone risk factors and vitamin D metabolism. Undersea Hyperb Med. 1995;22:145-52
In some groups, for example patients with severe reaction to sunlight, the photoprotecting behavior is mandatory. Due to photosensitivity, many patients with cutaneous lupus erythematosus actively avoid sunlight.
Cusack et al. interviewed 52 patients with cutaneous lupus erythematosus about several behavioral and physical characteristics, then measured serum levels of 25 (OH) D (end of summer).438438. Cusack C, Danby C, Fallon JC, Ho WL, Murray B, Brady J, et al. Photoprotective behaviour and sunscreen use: impact on vitamin D levels in cutaneous lupus erythematosus. Photodermatol Photoimmunol Photomed. 2008;24:260-7. Serum levels of 25 (OH) below 30 ng/mL were found in 67% of the individuals (average of 25.3 ng/mL), with most significant decrease in patients that physically avoided sunlight (use of hats, protection clothes, avoiding midday sun) (p = 0.004) and a little less in patients that used sunscreen daily (p = 0.042).
A study of Kamen et al. demonstrated that, in patients with systemic lupus erythematosus, photosensitivity was the second predictor of critically low 25 (OH) D levels, with an odds ratio of 12.9 (p < 0.01), second only to kidney disease (odds ratio 13.3, p < 0.01).439439. Kamen DL, Cooper GS, Bouali H, Shaftman SR, Hollis BW, Gilkeson GS. Vitamin D deficiency in systemic lupus erythematosus. Autoimmun Rev. 2006;5:114-7. The ones most affected by adverse effects of the sun probably take the greatest precautions to minimize exposure and therefore have the lowest levels of vitamin D.
Systemic immunosuppression in patients that received transplant of solid organs has been associated with an increased risk of skin cancer, thus avoiding sunlight is recommended to these patients.440440. Walder BK, Robertson MR, Jeremy D. Skin cancer and immunosuppression. Lancet. 1971;2:1282-3.
Querings et al. measured serum levels of 25 (OH) D at the end of winter in 31 31-year-old kidney transplant patients and in sex-matched controls.441441. Querings K, Girndt M, Geisel J, Georg T, Tilgen W, Reichrath J. 25-Hydroxyvitamin D-deficiency in renal transplant recipients. J Clin Endocrinol Metab. 2006;91:526-9. All transplanted patients reported practicing solar protection with the use of sunscreens, avoiding the sun and wearing protective clothes.
Transplanted patients presented significant lower levels of 25 (OH) D in comparison with controls (average concentration of 10.9 ng/ml vs20.0 ng/ml, p = 0.007). Nevertheless, the decrease in sun exposure is only one of several potential contributing factors in these patients. The use of glucocorticoids, for example, increases the breaking of 25 (OH) D. Vitamin D deficiency has also been demonstrated in patients who received bone marrow transplant.442442. Segal E, Baruch Y, Kramsky R, Raz B, Ish-Shalom S. Vitamin D deficiency in liver transplant patients in Israel. Transplant Proc. 2001;33:2955-6.,443443. Massenkeil G, Fiene C, Rosen O, Michael R, Reisinger W, Arnold R. Loss of bone mass and vitamin D deficiency after hematopoietic stem cell transplantation: standard prophylactic measures fail to prevent osteoporosis. Leukemia. 2001;15:1701-5.
A third group of patients who practice strict photoprotection is the one which presents inherent tendency for skin cancer formation, including patients with xeroderma pigmentosum (XP) and basal cell nevus syndrome (BCNS).
Querings and Reichrath conducted a small study about three patients with XP and BCNS, finding they had serum levels of 25 (OH) D significantly reduced (average of 9.5 ng/mL).444444. Querings K, Reichrath J. A plea for the analysis of vitamin-D levels in patients under photoprotection, including patients with xeroderma pigmentosum (XP) and basal cell nevus syndrome (BCNS). Cancer Causes Control. 2004;15:219. It was again demonstrated that photoprotection is associated with reduced vitamin D serum levels.
On the other hand, Sollitto et al. showed that eight patients with XP, who practiced rigorous solar protection measures, were capable of maintaining low levels of 25 (OH) D (average serum concentration of 17.8 ng/ml), without the need for supplementation.445445. Sollitto RB, Kraemer KH, DiGiovanna JJ. Normal vitamin D levels can be maintained despite rigorous photoprotection: six years' experience with xeroderma pigmentosum. J Am Acad Dermatol. 1997;37:942-7.
At the time the study was published, the 10 to 55 ng/mL range was considered normal. Sollitto et al. stated that adequate levels of vitamin D could be maintained in the absence of any supplementation and/or exposure to UV rays, even though these patients were young (27 years old in average, within the range of 14-49), active and had an estimated daily vitamin D intake of 307 IU. Due to greater recommended concentrations today (20 to 30 ng/mL), these patients would be considered vitamin D deficient.445445. Sollitto RB, Kraemer KH, DiGiovanna JJ. Normal vitamin D levels can be maintained despite rigorous photoprotection: six years' experience with xeroderma pigmentosum. J Am Acad Dermatol. 1997;37:942-7.
A broad investigation, with more than 1,400 white women, conducted by Glass et al. in the United Kingdom, analyzed the relationship between vitamin D, skin pigmentation and exposure to UV rays.446446. Glass D, Lens M, Swaminathan R, Spector TD, Bataille V. Pigmentation and vitamin D metabolism in Caucasians: low vitamin D serum levels in fair skin types in the UK. PLoS One. 2009;4:e6477.It was noticed that higher phototypes (III and IV) presented higher serum levels of 25 (OH) D (average of 32.9 ng/ml), when compared to low phototypes (types I and II) (average of 28.5 ng/mL, p < 0.0001).
Data revealed a behavioral tendency in dark-skinned patients to seek the sun, which was positively correlated with vitamin D status. Malvy et al. conducted a similar study in France, involving 1,191 individuals and also observed that serum levels of 25 (OH) D were lower in light-skinned individuals (p < 0.024).447447. Malvy DJ, Guinot C, Preziosi P, Galan P, Chapuy MC, Maamer M, et al. Relationship between vitamin D status and skin phototype in general adult population. Photochem Photobiol. 2000;71:466-9. Studies about individuals who work in the sun, such as farmers and lifeguards, revealed high levels of 25 (OH) D, with average concentrations between 54 and 65 ng/mL.397397. Vieth R. Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. Am J Clin Nutr. 1999;69:842-56.
In spite of greater sun exposure being related with higher levels of vitamin D, the interesting results from Binkley et al. suggest that abundant exposure may not be sufficient to enhance vitamin D status in all subjects.448448. Binkley N, Novotny R, Krueger D, Kawahara T, Daida YG, Lensmeyer G, et al. Low vitamin D status despite abundant sun exposure. J Clin Endocrinol Metab. 2007;92:2130-5.
The authors measured serum levels of 25 (OH) D in 93 young adults of distinct racial profiles, recruited from a skate shop in Honolulu, Hawaii (latitude 21 º N). The individuals were 24 years old on average and exposed themselves to the sun for around 28.9 hours per week (self-reported); in at least seven of these hours they wore a sunscreen. The score of solar index was calculated by the amount of time exposed to the sun combined with the exposed body area.
The average concentration of 25 (OH) D was 31.6 ng/mL. By using a 30 ng/mL cutoff point for sufficiency, 51% of the individuals presented low levels of vitamin D. The quartile of participants with the smallest concentrations of 25 (OH) D (average of 20.7 ng/mL versus 35.2 ng/mL, p < 0.0001) exposed themselves to the sun for less time (score 7.2 vs 12.3, p < 0.05) than other subjects of the study.
White participants presented more elevated levels of 25 (OH) D (average of 37.1 ng/mL, p < 0.01), when compared to Asians with darker skin (24.7 ng/ml) or mixed race individuals (28.9 ng/ml). However, a statistic correlation was not found between serum levels of 25 (OH) D and age, color of skin, hours of sun exposure without sunscreen, total sun exposure or solar index. Diet was not considered in this study.
Due to the fact that all participants are young, skin concentrations of 7-DHC could be considered as adequate; this way, the substantial variability suggests there are probably other influencing factors in the cutaneous production of vitamin D or of its subsequent metabolism, which has not been understood completely yet.
Different genetic requirements for execution of vitamin D physiological functions may exist, as well as the need for a lower optimal level in some populations. For example, African-Americans have lower 25 (OH) D levels than whites, but have greater bone density and fewer number of fractures due to osteoporosis.449449. Aloai JF. African Americans, 25-hydroxyvitamin D and osteoporosis: a paradox. Am J Clin Nutr. 2008;88:545S-550S.
It is believed that there are differences in calcium metabolism efficiency, for even when compared to whites who have similar bone density, African-Americans still present fewer fractures, lower levels of bone turnover markers and lower renal calcium excretion.
Clothing
Clothing is an additional barrier which UVB radiation must break to reach the 7-DHC. Similar to SPF, equivalent UV protection factors, or UPF, can be attributed to different kinds of clothes. The weave of a fabric may be closed or open, determining the level of protection that clothing provides - "coverage factor".450450. Morison WL. Photoprotection by clothing. Dermatol Ther. 2003;16:16-22.
Increased thickness is another characteristic that diminishes transmission of radiation. Fabric stretching diminishes thickness and opens spaces, reducing the efficacy proportionally to the amount of stretching. If well made, thick jeans may have a UPF 1000, whereas a light cotton t-shirt may have an UPF smaller than 10.451451. Sayre RM, Huges SNG. Sun protective apparel: advancements in sun protection. Skin Cancer J. 1993:8:41-7.
Darker colors absorb UV radiation better, thus may offer greater UPF in a same fabric. The composition of the fabric determines how absorbent it is, for example, polyester protects more than cotton, and natural cotton is more efficient than bleached cotton (natural cotton has pigments that absorb UVB radiation).452452. Gambichler T, Hatch KL, Avermaete A, Altmeyer P, Hoffmann K. Influence of wetness on the ultraviolet protection factor (UPF) of textiles: in vitro and in vivo measurements. Photodermatol Photoimmunol Photomed. 2002;18:29-35.
Additives, such as titanium dioxide and fluorescent whitening agents may be used by the manufacturers to enhance UPF. When fabric is wet due to perspiration or contact with water it responds differently and UPF may be reduced by half, for example in a white t-shirt, or increased, in other types of clothes.453453. Matsuoka LY, Wortsman J, Dannenberg MJ, Hollis BW, Lu Z, Holick MF. Clothing prevents ultraviolet-B radiation- dependent photosynthesis of vitamin D3. J Clin Endocrinol Metab. 1992;75:1099-103.,454454. Salih FM. Effect of clothing varieties on solar photosynthesis of previtamin D3: an in vitro study. Photodermatol Photoimmunol Photomed. 2004;20:53-8.
Washing and wearing cotton fabrics increases UPF, possibly doubling it after 10 washing cycles, especially due to shrinkage but also due to buildup of dirt, oils and detergent particles.455455. Parisi AV, Wilson CA.Pre-vitamin D3 effective ultraviolet transmission through clothing during simulated wear. Photodermatol Photoimmunol Photomed. 2005;21:303-10.
Most of the research focuses on the analysis of clothing and UPF, but does not approach vitamin D. Matsuoka et al. demonstrated that clothes prevent vitamin D production from 7-DHC.453453. Matsuoka LY, Wortsman J, Dannenberg MJ, Hollis BW, Lu Z, Holick MF. Clothing prevents ultraviolet-B radiation- dependent photosynthesis of vitamin D3. J Clin Endocrinol Metab. 1992;75:1099-103.
Volunteers wearing jogging clothing, which covered the whole body, were exposed to UVB irradiation (1 MED) and did not present elevation of vitamin D serum levels, independently of the kind of fabric (wool, cotton, polyester) or color (black or white). Even after increasing UVB radiation to 6 MEDs, the individuals did not present measurable increase of vitamin D levels, leading the authors to conclude that clothing made cutaneous photoproduction of vitamin D significantly difficult.
As part of this study, direct transmission of UVB was measured: black wool blocked more than 98% of the radiation and white cotton fabric blocked only 47%. Even so, there was not any evidence of 7-DHC conversion to previtamin D3 in vitro or in human volunteers.
Salih covered cuvettes containing 7-DHC with several fabrics used in traditional Oman clothes and measured the conversion to previtamin D3 after sun exposure in several periods.
Fabrics were made of polyester, a mix of cotton with polyester or wool. UVB radiation attenuation varied from 71.4 to 99.9%, and the type of thread was the most important factor in this attenuation. Sixty minutes of sun exposure provided 8% conversion of 7-DHC to previtamin D3 in uncovered cuvettes. Maximum conversion of 7-DHC to previtamin D3 in covered cuvettes was of 1.7%, while some fabrics did not allowing any conversion.454454. Salih FM. Effect of clothing varieties on solar photosynthesis of previtamin D3: an in vitro study. Photodermatol Photoimmunol Photomed. 2004;20:53-8.
Parisi and Wilson obtained similar results, with maximum transmission of 0.22 MED through cotton t-shirts in mannequins, in comparison with 14.5 MED in the outside surface of the t-shirt, after 3 hours of irradiation.455455. Parisi AV, Wilson CA.Pre-vitamin D3 effective ultraviolet transmission through clothing during simulated wear. Photodermatol Photoimmunol Photomed. 2005;21:303-10.
They concluded that 0.22 MED may be below the necessary threshold for previtamin D3 synthesis, even though the study was done from 09:30 a.m. to 12:30 p.m. during summer and could have yielded better results if done closer to midday or longer.455455. Parisi AV, Wilson CA.Pre-vitamin D3 effective ultraviolet transmission through clothing during simulated wear. Photodermatol Photoimmunol Photomed. 2005;21:303-10.
Sunscreen
Adequate application of sun screen may avoid damage caused by UV radiation in the skin, but the same blocked UVB is also necessary for vitamin D production.456456. Sedrani SH, Elidrissy AW, El Arabi KM. Sunlight and vitamin D status in normal Saudi subjects. Am J Clin Nutr. 1983;38:129-32.
457. Fonseca V, Tongia R, el-Hazmi M, Abu-Aisha H. Exposure to sunlight and vitamin D deficiency in Saudi Arabian women. Postgrad Med J. 1984;60:589-91.
458. MacNeal RJ, Dinulos JG. Update on sun protection and tanning in children. Curr Opin Pediatr. 2007;19:425-9.-459459. Thompson SC, Jolley D, Marks R. Reduction of solar keratoses by regular sunscreen use. N Engl J Med. 1993;329:1147-51. Although we suspect intuitively that the adequate use of sunscreen precludes sufficient synthesis of vitamin D, there are few studies that analyze this question.460460. Naylor MF, Boyd A, Smith DW, Cameron GS, Hubbard D, Neldner KH. High sun protection factor sunscreens in the suppression of actinic neoplasia. Arch Dermatol. 1995;131:170-5.,461461. Darlington S, Williams G, Neale R, Frost C, Green A. A randomized controlled trial to assess sunscreen application and betacarotene supplementation in the prevention of solar keratoses. Arch Dermatol. 2003;139:451-5.
Matsuoka et al. presented in vitro and in vivoevidence that application of para-aminobenzoic acid (PABA), a common ingredient of older sun screens, prevents cutaneous synthesis of vitamin D.462462. Matsuoka LY, Ide L, Wortsman J, MacLaughlin JA, Holick MF. Sunscreens suppress cutaneous vitamin D3 synthesis. J Clin Endocrinol Metab. 1987;64:1165-8. Ethanol or ethanol + PABA 5% were applied in pieces of human skin and then exposed to simulated solar radiation. Synthesis of previtamin D3 was completely blocked in pieces treated with solar filter; as for the non-treated pieces, 15% of 7-DHC was converted to previtamin D3 in the basal layer of epidermis.
Eight white individuals received separately 1 MED of UV radiation on the whole body. Four subjects applied a PABA-based sunscreen, SPF 8, one hour before exposure. One day after exposure, serum levels of vitamin D3 increased significantly in the four non-treated subjects, but remained unchanged in the individuals who used sunscreen (p < 0.01). Even though there were few patients in the study, the results provide evidence of vitamin D synthesis suppression with the use of PABA-based sunscreens.
Matsuoka et al. published another study one year later.463463. Matsuoka LY, Wortsman J, Hanifan N, Holick MF. Chronic sunscreen use decreases circulating concentrations of 25-hydroxyvitamin D. A preliminary study. Arch Dermatol. 1988;124:1802-4. The authors compared 20 white-skinned individuals with personal history of skin cancer, who over the past 12 months had applied PABA-based sun screens on all exposed body parts, to controls who lived in the same household or neighborhood and were of the same age.
Users of solar filters presented less than half the average 25 (OH) D serum levels compared with controls (16.1 VS 36.6 ng/mL, p < 0.001), in dosage taken in the summer. It is important to emphasize that 25 (OH) levels were not analyzed in the beginning of the study or before the use of sunscreen. The amount of sun exposure was estimated by researchers and direct measurement was not done. The individuals with a history of skin cancer probably put more effort in avoiding sunlight than their partners and neighbors, confusing the results.464464. Norval M, Wulf HC. Does chronic sunscreen use reduce vitamin D to insufficient levels? Br J Dermatol. 2009;161:732-6.
Matsuoka et al. did a third study, similar to the first one, in which an SPF 15 sunscreen was applied on different skin areas of white patients (phototype III), one hour before receiving slightly less than one MED on the whole body.465465. Matsuoka LY, Wortsman J, Hollis BW. Use of topical sunscreen for the evaluation of regional synthesis of vitamin D3. J Am Acad Dermatol. 1990;22:772-5.
Once more, they measured vitamin D3 levels (instead of 25 (OH) D) before and 24 hours after sun exposure and found that wearing sunscreen on all the body prevented the synthesis of vitamin D3. Applying sunscreen to all areas, except for the head and neck or arms, caused a slight but statistically insignificant increase in vitamin D3 (p > 0.05). Significant increase of vitamin D3 serum levels occurred only when more than 19% of total body surface was free of solar protection (p < 0.05).
Holick et al. estimated that adequate application of an SPF 8 solar filter reduces production of vitamin D by more than 90%, and a reduction of 99% is achieved when SPF 15 is applied.466466. Holick MF, Matsuoka LY, Wortsman J. Regular use of sun- screen on vitamin D levels. Arch Dermatol. 1995;131:1337-9.
Evidence that the application of a solar filter would make vitamin D synthesis difficult, from research which analyzed individual doses in controlled environments were apparently sound, but the results of larger scale studies were not consistent with these findings.
The first double-blind randomized clinical trial on the subject was conducted by Marks et al., in 1995, in Australia, and involved more than 100 patients, to whom SPF 17 sunscreens or placebo were designated.467467. Marks R, Foley PA, Jolley D, Knight KR, Harrison J, Thompson SC. The effect of regular sunscreen use on vitamin D levels in an Australian population. Arch Dermatol. 1995;131:415-21.
All participants in the study presented a history of at least one solar keratosis and were older than 40 years of age. Serum levels of 25 (OH) D and 1.25 (OH) D were obtained at the beginning of the trial and seven months later, after the Australian summer. The adequate use of sun screen was verified by periodic weighing of packagings.
The results showed that the use of solar filter did not prevent seasonal increase of 25 (OH) D. The responses were similar in both groups, independently from distribution by age, gender, sun exposure or skin type. Even so, in the placebo group there was a statistically significant increase of 1.25 (OH) D (p = 0.0009) serum levels, which rose by 4.5 ng/mL, whereas, in the group that used sunscreens, the increase was only 0.5 pg/ ml.
Levels of 1.25 (OH) D remained within the reference range (12.5-51.7 pg/mL) in all participants and there was no statistical difference between global levels of 1.25 (OH), either at the start or end of research. Seasonal increase of 1.25 (OH) D was an unexpected finding. 1.25 (OH) D is considered free from personal fluctuations, probably due to rigorous control via feedback.467467. Marks R, Foley PA, Jolley D, Knight KR, Harrison J, Thompson SC. The effect of regular sunscreen use on vitamin D levels in an Australian population. Arch Dermatol. 1995;131:415-21.
468. Chesney RW, Rosen JF, Hamstra AJ, Smith C, Mahaffey K, DeLuca HF. Absence of seasonal variation in serum concentrations of 1,25-dihydroxyvitamin D despite a rise in 25-hydroxyvitamin D in summer. J Clin Endocrinol Metab. 1981;53:139-42.-469469. Tjellesen L, Nielsen B, Christiansen C. Seasonal fluctuations in serum concentrations of vitamin D metabolites. Br Med J (Clin Res Ed). 1982;284:196-7.
The authors were not able to offer an explanation for changes in 1.25 (OH) D levels. However, the most important finding shows that the marker for vitamin D deficiency, 25 (OH) D, was not affected due to use of sunscreen. The authors argued that adequate sun exposure was obtained through UVB radiation fractions which crossed the skin (based on SPF) due to occasional forgetfulness or inadequate protector applications.468468. Chesney RW, Rosen JF, Hamstra AJ, Smith C, Mahaffey K, DeLuca HF. Absence of seasonal variation in serum concentrations of 1,25-dihydroxyvitamin D despite a rise in 25-hydroxyvitamin D in summer. J Clin Endocrinol Metab. 1981;53:139-42.
Maia et al. evaluated serum concentrations of 25 (OH) D and parathyroid hormone (PTH) in groups of individuals, with and without orientation for photoprotection, residents of the city of São Paulo, Brazil. The authors found a significant difference between levels of 25 (OH) D, which were greater in the photo-exposed group, 35.4ng/mL [21.86 - 72.20] in comparison with the photoprotected one, 29.2 ng/mL [23.10 - 45.80]. There was also a difference regarding PTH, larger in the photoexposed group, 29.8pg/mL [18.98 - 73.94], than in the photoprotected one, 19.24 pg/mL [8.06 - 66.18].470470. Maia M, Maeda S, Marçon CR. Correlation between photoprotection and concentrations of 25-hydroxyvitamin D and parathyroid hormone. An Bras Dermatol. 2007;82:233-7.
In spite of these differences, there were no vitamin D deficient individuals in the sample and PTH levels remained within normalcy levels. The conclusion was that everyday solar ultraviolet radiation was enough to provide for an adequate synthesis of 25 (OH) D.470470. Maia M, Maeda S, Marçon CR. Correlation between photoprotection and concentrations of 25-hydroxyvitamin D and parathyroid hormone. An Bras Dermatol. 2007;82:233-7.
A preliminary cross-sectional study, carried on by Kligman et al., reported that the use of solar filter by the elderly in Arizona was positively associated with levels of 25 (OH) D.471471. Kligman EW, Watkins A, Johnson K, Kronland R. The impact of lifestyle factors on serum 25-hydroxy vitamin D levels in older adults: a preliminary study. Fam Pract Res J. 1989;9:11-9.
Another similar study, based in questionnaires, was done by Kimlin et al., involving a wide range of Australian individuals, with ages between 18-87.472472. Kimlin M, Harrison S, Nowak M, Moore M, Brodie A, Lang C. Does a high UV environment ensure adequate vitamin D status? J Photochem Photobiol B. 2007 Dec 14;89:139-47. The authors did not find any statistically significant association between the status of 25 (OH) D and the use of sunscreens, and as for the participants who wore a sunscreen, they presented some of the highest levels of 25 (OH) D. In this case, it was supposed that the use of sunscreens was probably an indication of increased sun exposure.
A cross-sectional study investigated the connection between obesity and decrease of vitamin D serum levels in hundreds of elders residents of Boston (USA). Coincidentally, the authors found that the use of sun screens was not associated to vitamin D levels. On the other hand, time of sun exposure and area of exposed body surface were positively correlated, as expected.473473. Harris SS, Dawson-Hughes B. Reduced sun exposure does not explain the inverse association of 25-hydroxyvitamin D with percent body fat in older adults. J Clin Endocrinol Metab. 2007;92:3155-7.
An explanation for lack of negative correlation (and sometimes positive correlation) between the status of vitamin D and the use of sunscreens was supplied by Thieden et al. The authors concluded that the sunscreen was frequently applied on days when great amounts of sun exposure were foreseen, with the goal of avoiding sunburns. Thus, the use of protector was associated with more frequent and longer exposure to sunlight.474474. Thieden E, Philipsen PA, Sandby-Møller J, Wulf HC. Sunscreen use related to UV exposure, age, sex, and occupation based on personal dosimeter readings and sunexposure behavior diaries. Arch Dermatol. 2005;141:967-73.
Therefore, a behavior of actively seeking for sunlight would be capable of neutralizing any vitamin D synthesis attenuation which a sun filter, theoretically, could cause. Additionally, Bech-Thomsen and Wulf analyzed a sample of bathers, demonstrating that a sunscreen was not applied in the recommended doses to obtain the advertised classification protection (SPF).475475. Bech-Thomsen N, Wulf HC. Sunbathers' application of sunscreen is probably inadequate to obtain the sun protection factor assigned to the preparation. Photodermatol Photoimmunol Photomed. 1992-1993;9:242-4.
A survey performed by Stender et al. revealed that users of solar filters oftentimes presented sunburns again, demonstrating an improper or inadequate use, besides greater sun exposure in comparison with individuals who used sunscreen less often.476476. Stender IM, Lock-Andersen J, Wulf HC. Sun-protection behavior and selfassessed burning tendency among sun- bathers. Photodermatol Photoimmunol Photomed. 1996;12:162-5.
Farrerons et l. compared 24 elderly who wore a sunscreen (SPF 15) with 19 controls, for more than 2 years. Not limited to vitamin D, they also analyzed secondary markers (PTH, biological bone markers).477477. Farrerons J, Barnadas M, Rodríguez J, Renau A, Yoldi B, López-Navidad A,et al. Clinically pre- scribed sunscreen (sun protection factor 15) does not decrease serum vitamin D concentration sufficiently either to induce changes in parathyroid function or in metabolic markers. Br J Dermatol. 1998;139:422-7.
The authors reported that the decrease of 25 (OH) D status in sunscreen users was a little larger than in controls; the latter had a slightly larger increase in 25 (OH) D levels in the summer months (p < 0.05). Notwithstanding, the changes of serum levels of 1.25 (OH) D were unimportant in both groups, and there was no evidence of secondary hyperparathyroidism during the winter or bone metabolism changes in any of the participants.
In a follow-up study, several years later, Farrerons et al. evaluated the bone mass of 10 sun screen users and 18 controls for more than 2 years. No significant differences were observed in the bone mass of both groups.478478. Farrerons J, Barnadas M, López-Navidad A, Renau A, Rodríguez J, Yoldi B, et al. Sun- screen and risk of osteoporosis in the elderly: a two-year follow-up. Dermatology. 2001;202:27-30.
They came to the conclusion that even though the SPF 15 sunscreen discreetly diminishes serum concentrations of 25 (OH), this reduction was not either clinically significant or increased the risk of bone mass loss. Despite being good indicators of vitamin D status, PTH and bone mass may not be adequate measurements to determine sufficiency, in light of other emerging potential benefits of vitamin D.
CONCLUSION
Prevention of sunlight exposure has been related to diminution of serum levels of 25 (OH) D. However, the issue was analyzed only in laboratories and there is still no clear evidence of clinical consequences. Outside of controlled experiments, the use of solar protector did not negatively correlate with vitamin D serum levels.
Contrariwise, it was shown to be a marker of sun exposure and was associated with elevated concentrations of 25 (OH) D. Many external factors affect the quantity of available UVB and its capability for photosynthesis of vitamin D, besides the influence on the potential response of each individual. Therefore, it is difficult to make generic affirmations correlating the duration of sun exposure and vitamin D status.
Recommendations regarding "ideal" exposure seem to be excessively simplified, given the complexity and the individuality of final determination of the synthesis of vitamin D. With the continuous expansion of discoveries about vitamin D functions, the definition of "adequate" remains indefinite. Indirect markers previously considered for evaluation of deficiencies, such as high PTH, probably did not analyze the clinical picture effectively.
The risk for solar damage and skin cancer with excessive UV radiation exposure, as well as the available oral vitamin D supplementation make the establishment of guidelines for definition of ideal and safe sun exposure levels, necessary to keep up adequate vitamin D concentrations, even more difficult.
FINAL CONSIDERATIONS
Vitamin D benefits
The only benefit clearly related to vitamin D is its relationship with bone health through participation in calcium metabolism. Appropriate vitamin D levels are related to rickets and osteoporosis prevention.
The evidence that vitamin D reduces the risk for onset of chronic non skeletal diseases is inconsistent, inconclusive and does not meet cause-effect relationship criteria.479479. Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 Report on Dietary Reference Intakes for Calcium and Vitamin D from the Institute of Medicine: What Clinicians Need to Know. J Clin Endocrinol Metab. 2011;96:53-8.
Vitamin D serum levels
The definition of vitamin D deficiency, based on 25 (OH) D serum levels, is a motive for controversy in literature. Levels above 30 ng/ml (> 75 nmol/l) are considered satisfactory by all the authors. Levels lower than 20 ng/ml (< 50 nmol/l) may be consensually considered as vitamin D deficiency, since 97.5% of the population is above this level.
The controversy is related to values between 20 and 30 ng/ml, in which some authors define an intermediate situation, designed as "unsatisfactory level". The variation of the cutoff point may produce an expressive increase in the number of individuals classified as vitamin deficient, as presented in some alarmist statistics.
Global epidemiological data show that only around 30% of subjects present vitamin D rates lower than 20 ng/ml and, therefore, may be consensually classified as deficient.480480. Binkley N, Ramamurthy R, Krueger D. Low Vitamin D Status: Definition, Prevalence, Consequences, and Correction. Endocrinol Metab Clin North Am. 2010;39:287-301.
Sun exposure and vitamin D
Ultraviolet radiation type B (UVB), with action peak at 296 nm, acts on vitamin D metabolism, transforming 7-dehydrocholesterol in precholecalciferol (pre-vitamin D3) in the epidermis. From this point, a sequence of metabolic hydroxylation reactions will take place in the liver and kidneys, until the active form of vitamin D (1.25-dihydrocholecalciferol) is produced.
The estimated UVB dose required for production of 1000 IU of Vitamin D is 0.25 Mínimal Erythema Dose (MED), when about 25% of total body area is exposed. It is, therefore, considered small if compared to the dose necessary to produce erythema.
In a country with high levels of solar insolation, such as Brazil, a few minutes of exposure to the external environment, whatever the weather and only hands and face, would be sufficient for vitamin D production. Therefore we should be more concerned with the risks related to solar exposure than with the risks related to non exposure.
As regards the time for sun exposure, we know that the UVB radiation level in the period before 10 o'clock in the morning and after 3 o'clock in the afternoon (daylight saving time not considered) is minimal and does not justify solar exposure during these periods, particularly with the intention to produce vitamin D.
Sun exposure and development of skin cancer
The incidence of non melanoma and melanoma skin cancer has grown all over the world for decades, being the most frequent among human body cancers.
The causal nexus relationship between sun exposure and squamous cell carcinoma is very well established in the literature. Furthermore, different studies also point to the participation of solar radiation in the onset of basal cell carcinoma and cutaneous melanoma.
Solar protection and vitamin D
We know that the adequate use of sunscreen significantly reduces the amount of UVB radiation that reaches the cutaneous surface and may theoretically interfere in vitamin D production. However, in practice we know that the regular use of sunscreen does not lead to vitamin D deficiency.
The possible justification found would be that, as users do not apply the sunscreen in the proper amount and with the recommended frequency and regularity, a sufficient amount of UVB radiation would reach the skin surface for production of vitamin D.
Therefore, wearing sunscreen as customarily done by users could not be considered as a factor predisposing to development of vitamin D deficiency.
RECOMMENDATIONS OF THE BRAZILIAN CONSENSUS ON PHOTOPROTECTION:
-
Intentional and unprotected sun exposure should not be considered as source for production or to prevent vitamin D deficiency.
-
The use of sunscreen with SPF higher than 30 should be recommended to all patients older that 6 months of age, when exposed to the sun. There should not be sun exposure without adequate use of sunscreen. Children younger than 6 months of age should not be directly exposed to the sun and should not make regular use of sunscreen.
-
Patients considered as being at risk for development of deficiency of vitamin D should be monitored by periodical exams and may use diet or vitamin supplementation sources for prevention of vitamin D deficiency.
-
The following are considered as risk factors for development of vitamin D deficiency:
-
Infants receiving exclusive breastfeeding.
-
The elderly (older skin produces less vitamin D).
-
Individuals with low sun exposure.
-
Extreme climate conditions.
-
Rigorous use of photoprotective measures.
-
Covering the skin for religious practice reasons.
-
People with dark skin (phototypes V and VI).
-
Patients with malabsorption syndrome.
-
The morbidly obese.
-
-
The recommended daily doses of vitamin D for deficiency prevention in individuals at risk are:
-
0-12 months: 400 IU/day.
-
1 to 70 years of age: 600 IU/day.
-
> 70 years of age: 800 IU/day.
-
-
Finally, SBD understands that the policies for prevention of skin cancer, by means of Photoprotection Awareness, is a priority measure in terms Public Health for Brazil, particularly in the Dermatology area.
-
SBD continues advise the population to avoid sun exposure without adequate protection, especially in the period of greater risk, between 10:00 am. and 3:00 pm.
-
*
Study carried out by the Brazilian Society of Dermatology (Sociedade Brasileira de Dermatologia - SBD) - Rio de Janeiro (RJ), Brazil.
-
[***]
The ability of a sunscreen to remain effective during use, especially after exposure to water, is very important in the composition of the vehicle, as it favors adhesion of the active sunscreen principle to the corneal layer. The most effective substances in sunscreens are liposoluble. -
Financial Support: None
-
How to cite this article: Schalka S, Steiner D, Ravelli FN, Steiner T, Terena AC, Marçon CR, et al. Brazilian Consensus on Photoprotection. An Bras Dermatol. 2014;89(6 Suppl 1):S6-73.
References
-
1Sliney DH; International Commission on Illumination. Radiometric Quantities and Units Used in Photobiology and Photochemistry: Recommendations of the Commission Internationale de l'Eclairage (International Commission on Illumination). Photochem Photobiol. 2007;83:425-32.
-
2International Commission on Illumination [Internet]. CIE 134/1999 TC 6-26 report: Standardization of the Terms UV-A1, UV-A2 and UV-B. [cited 2014 Out 29]. Available from: http://div6.cie.co.at/?i_ca_id=611&pubid=179
» http://div6.cie.co.at/?i_ca_id=611&pubid=179 -
3International Organization for Standardization. ISO 20473: Optics and photonics -Spectral bands; 2007.
-
4World Meteorological Organization. Scientific Assessment of Ozone Depletion: 2010, Global Ozone Research and Monitoring Project-Report No. 52. Geneva, Switzerland: WHO; 2011. 516 p.
-
5Bais AF, Tourpali K, Kazantzidis A, Akiyoshi H, Bekki S, Braesicke P, et al. Projections of UV radiation changes in the 21st century: impact of ozone recovery and cloud effects Atmos. Chem Phys. 2001;11:7533-45.
-
6van Dijk A, Slaper H, den Outer PN, Morgenstern O, Braesicke P, Pyle JA, et al. Skin Cancer Risks Avoided by the Montreal Protocol -Worldwide Modeling Integrating Coupled Climate-Chemistry Models with a Risk Model for UV. Photochem Photobiol. 2013;89:234-46.
-
7Pfeifer MT, P. Koepke, Reuder J. Effects of altitude and aerosol on UV radiation. J Geophys Res. 2006:111;D01203.
-
8Corrêa MP, Plana-Fattori A. Uma análise das variações do índice ultravioleta em relação às observações de conteúdo de ozônio e da espessura óptica dos aerossóis sobre a cidade de São Paulo. Rev Bras Meteorol. 2006;21:24-32.
-
9Acosta LR and Evans WFJ. Design of the Mexico City UV monitoring network: UVB measurements at ground level in the urban environment. J Geophys Res. 2000;105:5017-26.
-
10Corrêa MP, Ceballos JC. UVB surface albedo measurements using biometers. Rev Bras Geof. 2008;26:411-6.
-
11Unep.org [Internet]. Global solar UV Index: A Practical Guide. A joint recommendation of the World Health Organization,World Meteorological Organization, United Nations Environment Programme, and the International Commission on Non-Ionizing Radiation Protection. Geneva: WHO; 2002. 28 p. [Cited 2014 30 Oct]. Available from: http://www.unep.org/pdf/solar_Index_Guide.pdf.
» http://www.unep.org/pdf/solar_Index_Guide.pdf -
12Swerdlow AJ, English JS, MacKie RM, O'Doherty CJ, Hunter JA, Clark J, et al. Fluorescent lights, ultraviolet lamps, and risk of cutaneous melanoma. BMJ. 1988;297:647-50.
-
13English DR, Rouse IL, Xu Z, Watt JD, Holman CD, Heenan PJ, et al. Cutaneous malignant melanoma and fluorescent lighting. J Natl Cancer Inst. 1985;74:1191-7.
-
14Diffey BL. Human exposure to ultraviolet radiation. Semin Dermatol. 1990;9:2-10.
-
15Eadie E, Ferguson J, Moseley H. A preliminary investigation into the effect of exposure of photosensitive individuals to light from compact fluorescent lamps. Br J Dermatol. 2009;160:659-64.
-
16Sayre RM, Dowdy JC, Poh-Fitzpatrick M. Dermatological risk of indoor ultraviolet exposure from contemporary lighting sources. Photochem Photobiol. 2004;80:47-51.
-
17Klein RS, Werth VP, Dowdy JC, Sayre RM. Analysus of compact fluorescent lights for use by patients with phtosensitive conditions. Photochem Photobiol. 2009;85:1004-10.
-
18Sklar LR, Almutawa F, Lim HW, Hamzavi I. Lim and Iltefat Hamzavi. Effects of ultraviolet radiation, visible light, and infrared radiation on erythema and pigmentation: a review. Photochem Photobiol Sci. 2013;12:54-64.
-
19de Paula Corrêa M, Ceballos JC. solar Ultraviolet Radiation Measurements in One of the Most Populous Cities of the World: Aspects Related to Skin Cancer Cases and Vitamin D Availability. Photochem Photobiol. 2010;86:438-44.
-
20de Paula Corrêa M, Pires LC. Doses of erythemal ultraviolet radiation observed in Brazil. Int J Dermatol. 2013;52:966-73.
-
21Corrêa MP. (Medidas de radiação UV na praia de Ponta Negra, Natal/RN realizadas em 13 de março de 2011). Comunicação pessoal.
-
22Silva A. Medidas de radiação solar ultravioleta em Belo Horizonte e saúde pública. Rev Bras Geof. 2008;26:417-25.
-
23Silva A, Kirchhoff VWJH, Echer E, Leme NP. Variação Sazonal da Radiação Ultravioleta solar Biologicamente Ativa. Rev Bras Geof 2000;18:64-74.
-
24Cptec.inpe.br [Internet]. Instituto Nacional de Pesquisas espaciais (INPE). Centro de previsão de tempo e estudos climáticos. [acesso 30 out 2014]. Disponível em: http://www.cptec.inpe.br/
» http://www.cptec.inpe.br/ -
25Madronich, S., Implications of recent total atmospheric ozone measurements for biologically active ultraviolet radiation reaching the Earth's surfasse. Geophys Res Lett. 1992;19:37-40.
-
26Brasil. Ministério da Saúde. Instituto Nacional de Câncer (INCA). Coordenação de Prevenção e Vigilância de Câncer. Estimativas 2010: Incidência de Câncer no Brasil. Rio de Janeiro: INCA, 2009. 98 p.
-
27Hönigsmann H. Erythema and pigmentation. Photodermatol Photoimmunol Photomed. 2002;18:75-81.
-
28Suh KS, Roh HJ, Choi SY, Jeon YS, Doh KS, Bae JH, et al. A long-term evaluation of erythema and pigmentation induced by ultraviolet radiations of different wavelengths. Skin Res Technol. 2007;13:360-8.
-
29Matsumura Y, Ananthaswamy HN. Short-term and long-term cellular and molecular events following UV irradiation of skin: implications for molecular medicine. Expert Rev Mol Med. 2002;4:1-22.
-
30Svobodova A, Walterova D, Vostalova J. Ultraviolet light induced alteration to the skin. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2006;150:25-38.
-
31Katiyar SK. UV-induced immune suppression and photocarcinogenesis: chemoprevention by dietary botanical agents. Cancer Lett. 2007;255:1-11.
-
32Sklar LR, Almutawa F, Lim HW, Hamzavi I. Effects of ultraviolet radiation, visible light, and infrared radiation on erythema and pigmentation: a review. Photochem Photobiol Sci. 2013;12:54-64.
-
33Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869-71.
-
34Schalka S, dos Reis VM, Cucé LC. The influence of the amount of sunscreen applied and its sun protection factor (SPF): evaluation of two sunscreens including the same ingredients at different concentrations. Photodermatol Photoimmunol Photomed. 2009;25:175-80.
-
35Sheehan JM, Cragg N, Chadwick CA, Potten CS, Young AR. Repeated ultraviolet exposure affords the same protection against DNA photodamage and erythema in human skin types II and IV but is associated with faster DNA repair in skin type IV. J Invest Dermatol. 2002;118:825-9.
-
36Waterston K, Naysmith L, Rees JL. Variation in skin thickness may explain some of the within-person variation in ultraviolet radiation-induced erythema at different body sites. J Invest Dermatol. 2005;124:1078.
-
37Broekmans WM, Vink AA, Boelsma E, Klöpping-Ketelaars WA, Tijburg LB, van't Veer P, et al. Determinants of skin sensitivity to solar irradiation. Eur J Clin Nutr. 2003;57:1222-9.
-
38Becker JA, Stewart LK. Heat-related illness. Am Fam Physician. 2011;83:1325-30.
-
39Glazer JL. Management of heatstroke and heat exhaustion. Am Fam Physician. 2005;71:2133-40.
-
40Wexler RK. Evaluation and treatment of heat-related illnesses. Am Fam Physician. 2002;65:2307-14.
-
41D'Orazio J, Jarrett S, Amaro-Ortiz A, Scott T. UV Radiation and the Skin. Int J Mol Sci. 2013;14:12222-48.
-
42Dumay O, Karam A, Vian L, Moyal D, Hourseau C, Stoebner P, et al. Ultraviolet AI exposure of human skin results in Langerhans cell depletion and reduction of epidermal antigen-presenting cell function: partial protection by a broad-spectrum sunscreen. Br J Dermatol. 2001;144:1161-8.
-
43Schwarz A, Beissert S, Grosse-Heitmeyer K, Gunzer M, Bluestone JA, Grabbe S, et al. Evidence for functional relevance of CTLA-4 in ultraviolet-radiation-induced tolerance. J Immunol. 2000;165:1824-31.
-
44Khavkin J, Ellis DA. Aging skin: histology, physiology, and pathology. Facial Plast Surg Clin North Am. 2011;19:229-34.
-
45Quan T, He T, Kang S, Voorhees JJ, Fisher GJ. solar ultraviolet irradiation reduces collagen in photoaged human skin by blocking transforming growth factor-beta type II receptor/Smad signaling. Am J Pathol. 2004;165:741-51.
-
46Ray AJ, Turner R, Nikaido O, Rees JL, Birch-Machin MA. The spectrum of mitochondrial DNA deletions is a ubiquitous marker of ultraviolet radiation exposure in human skin. J Invest Dermatol. 2000;115:674-9.
-
47Koch H, Wittern KP, Bergemann J. In human keratinocytes the Common Deletion reflects donor variabilities rather than chronologic aging and can be induced by ultraviolet A irradiation. J Invest Dermatol. 2001;117:892-7.
-
48Berneburg M, Plettenberg H, Medve-König K, Pfahlberg A, Gers-Barlag H, Gefeller O, et al. Induction of the photoaging-associated mitochondrial common deletion in vivo in normal human skin J Invest Dermatol. 2004;122:1277-83.
-
49Rittié L, Fisher GJ. UV-light-induced signal cascades and skin aging. Ageing Res Rev. 2002;1:705-20.
-
50Massagué J. How cells read TGF-beta signals. Nat Rev Mol Cell Biol. 2000;1:169-78.
-
51Boyd AS, Naylor M, Cameron GS, Pearse AD, Gaskell SA, Neldner KH. The effects of chronic sunscreen use on the histologic changes of dermatoheliosis. J Am Acad Dermatol. 1995;33:941-6.
-
52Seité S, Fourtanier AM. The benefit of daily photoprotection. J Am Acad Dermatol. 2008;58:S160-6.
-
53Hussein MR. Ultraviolet radiation and skin cancer: molecular mechanisms. J Cutan Pathol. 2005;32:191-205.
-
54de Laat A, van Tilburg M, van der Leun JC, van Vloten WA, de Gruijl FR. Cell cycle kinetics following UVA irradiation in comparison to UVB and UVC irradiation. Photochem Photobiol. 1996;63:492-7.
-
55Anderson RR, Parrish JA. The optics of human skin. J Invest Dermatol. 1981;77:13-9.
-
56Kanofsky JR, Sima P. Singlet oxygen production from the reactions of ozone with biological molecules. J Biol Chem. 1991;266:9039-42.
-
57de Gruijl FR, van der Leun JC. Physical variables in experimental photocarcinogenesis and quantitative relationships between stages of tumor development. Front Biosci. 2002;7:d1525-30.
-
58Krämer M, Stein B, Mai S, Kunz E, König H, Loferer H, et al. Radiation-induced activation of transcription factors in mammalian cells. Radiat Environ Biophys. 1990;29:303-13.
-
59Chen AC, Halliday GM, Damian DL. Non-melanoma skin cancer: carcinogenesis and chemoprevention. Pathology. 2013;45:331-41.
-
60Lotti T, Bruscino N, Hercogova J, de Giorgi V. Controversial issues on melanoma. Dermatol Ther. 2012;25:458-62.
-
61Mahmoud BH, R-UVolo E, Hexsel CL, Liu Y, Owen MR, Kollias N, et al. Impact of long-wavelength UVA and visible light on melanocompetent skin. J Invest Dermatol. 2010;130:2092-7.
-
62Ramasubramaniam R, Roy A, Sharma B, Nagalakshmi S. Are there mechanistic differences between ultraviolet and visible radiation induced skin pigmentation? Photochem Photobiol Sci. 2011;10:1887-93.
-
63Haywood R. Relevance of sunscreen application method, visible light and sunlight intensity to free-radical protection: A study of ex vivo human skin. Photochem Photobiol. 2006;82:1123-31.
-
64Cho S, Lee MJ, Kim MS, Lee S, Kim YK, Lee DH, et al. Infrared plus visible light and heat from natural sunlight participate in the expression of MMPs and type I procollagen as well as infiltration of inflammatory cell in human skin in vivo. J Dermatol Sci. 2008;50:123-33.
-
65Schieke SM, Schroeder P, Krutmann J. Cutaneous effects of infrared radiation: from clinical observations to molecular response mechanisms. Photodermatol Photoimmunol Photomed. 2003;19:228-34.
-
66Lee HS, Lee DH, Cho S, Chung JH. Minimal heating dose: a novel biological unit to measure infrared irradiation. Photodermatol Photoimmunol Photomed. 2006;22:148-52.
-
67Pujol JA, Lecha M. Photoprotection in the infrared radiation range. Photodermatol Photoimmunol Photomed. 1992-1993;9:275-8.
-
68Schroeder P, Lademann J, Darvin ME, Stege H, Marks C, Bruhnke S, et al. Infrared radiation-induced matrix metalloproteinase in human skin: implications for protection. J Invest Dermatol. 2008;128:2491-7.
-
69Krutmann J, Schroeder P. Role of mitochondria in photoaging of human skin: the defective powerhouse model. J Investig Dermatol Symp Proc. 2009;14:44-9.
-
70Krutmann J, Morita A, Chung JH. Sun exposure: what molecular photodermatology tells us about its good and bad sides. J Invest Dermatol. 2012;132:976-84.
-
71Darvin ME, Haag SF, Lademann J, Zastrow L, Sterry W, Meinke MC. Formation of free radicals in human skin during irradiation with infrared light. J Invest Dermatol. 2010;130:629-31.
-
72Jung T, Höhn A, Piazena H, Grune T. Effects of water-filtered infrared A irradiation on human fibroblasts. Free Radic Biol Med. 2010;48:153-60.
-
73Murphy GM. Investigation of photosensitive disorders. Photodermatol Photoimmunol Photomed. 2004;20:305-11.
-
74Stengel FM. Fotoeducación:un paso más allá dela fotoprotección. Arch Argent Dermatol. 1988;38:345-9.
-
75Stengel FM, Fernandez JF. Education and behavioral change for sun protection. J Cosmet Dermatol. 2005;4:83-8.
-
76Fabris MR, Durães ES, Martignago BC, Blanco LF, Fabris TR. Assessment of knowledge of skin cancer prevention and its relation with sun exposure and photo protection amongst gym academy members on the South of Santa Catarina, Brazil. An Bras Dermatol. 2012;87:36-43.
-
77Glanz K, Maddock JE, Lew RA, Murakami-Akatsuka L. A randomized trial of the Hawaii Sun smart program's impact on outdoor recreation staff. J Am Acad Dermatol. 2001;44:973-8.
-
78Kullavanijaya P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.
-
79Lucci A, Citro HW, Wilson L. Assessment of knowledge of melanoma risk factors, prevention, and detection principles in Texas teenagers. J Surg Res. 2001;97:179-83.
-
80Melia J, Pendry L, Eiser JR, Harland C, Moss S. Evaluation of primary intervention initiatives for skin cancer: a review from a UK perpective. Br J Dermatol. 2000;143:701-8.
-
81Koh HK, Geller AC. The public health future of melanoma control. J Am Acad Dermatol. 2011;65:S3-5.
-
82Day AK, Wilson CJ, Hutchinson AD, Roberts RM. The role of skin cancer knowledge in sun-related behaviours: a systematic review. J Health Psychol. 2014;19:1143-62
-
83Benvenuto-Andrade C, Zen B, Fonseca G, De Villa D, Cestari T. Sun exposure and sun protection habits among high-school adolescents in Porto Alegre, Brazil. Photochem Photobiol. 2005;81:630-5.
-
84Buller DB, Cokkinides V, Hall HI, Hartman AM, Saraiya M, Miller E, et al. Prevalence of sunburn, sun protection, and indoor tanning behaviors among Americans: review from national surveys and case studies of 3 states. J Am Acad Dermatol. 2011;65:S114-23.
-
85Lin JS, Eder M, Weinmann S. Behavioral counseling to prevent skin cancer: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med. 2011;154:190-201.
-
86Glanz K, Steffen AD, Schoenfeld E, Tappe KA. Randomized Trial of Tailored Skin Cancer Prevention for Children: The Project SCAPE Family Study. J Health Commun. 2013;18:1368-83.
-
87Crane LA, Asdigian NL, Barón AE, Aalborg J, Marcus AC, Mokrohisky ST, et al. Mailed intervention to promote sun protection of children: a randomized controlled trial. Am J Prev Med. 2012;43:399-410.
-
88Norman GJ, Adams MA, Calfas KJ, Covin J, Sallis JF, Rossi JS, et al. A randomized trial of a multicomponent intervention for adolescent sun protection behaviors. Arch Pediatr Adolesc Med. 2007;161:146-52.
-
89Crane LA, Deas A, Mokrohisky ST, Ehrsam G, Jones RH, Dellavalle R, et al. A randomized intervention study of sun protection promotion in well-child care. Prev Med. 2006;42:162-70.
-
90Stoebner-Delbarre A, Defez C, Borrel E, Sancho-Garnier H, Guillot B; Groupe EPICES. Prevention of skin cancer programs: Analysis of the impact of randomized trials. Ann Dermatol Venereol. 2005;132:641-7.
-
91Saraiya M, Glanz K, Briss PA, Nichols P, White C, Das D, et al. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiations: A systematic review. Am J Prev Med. 2004;27:422-66.
-
92Kyle JW, Hammitt JK, Lim HW, Geller AC, Hall-Jordan LH, Maibach EW, et al. Economic evaluation of the US Environmental Protection Agency's SunWise program: sun protection education for young children. Pediatrics. 2008;121:e1074-84.
-
93Buendía-Eisman A, Feriche-Fernández E, Muñoz-Negro JE, Cabrera-León A, Serrano-Ortega S. Evaluation of a school intervention program to modify sun exposure behaviour. Actas Dermosifiliogr. 2007;98:332-44.
-
94Townsend JS, Pinkerton B, McKenna SA, Higgins SM, Tai E, Steele CB, et al. Targeting children through school-based education and policy strategies: comprehensive cancer control activities in melanoma prevention. J Am Acad Dermatol. 2011;65:S104-13.
-
95Buller DB, Geller AC, Cantor M, Buller MK, Rosseel K, Hufford D, et al. Sun protection policies and environmental features in US elementary schools. Arch Dermatol. 2002;138:771-4.
-
96Cdc.gov [Internet]. Centers for Disease Control and Prevention. Sun safety for America's youth toolkit. Atlanta (GA). July 2009. [cited 2013 Jun 29]. Available from: http://www.cdc.gov/cancer/skin/pdf/toolkit/SunSafetyToolkit_MainText.pdf.
» http://www.cdc.gov/cancer/skin/pdf/toolkit/SunSafetyToolkit_MainText.pdf -
97who.int [Internet]. World Health Oganization. Sun protection and schools: how to make a difference. Geneva: WHO; 2003. [cited 2014 Oct 30]. http://www.who.int/uv/publications/en/sunprotschools.pdf.
» http://www.who.int/uv/publications/en/sunprotschools.pdf -
98Sbd.org.br [Internet]. Sociedade Brasileira de Dermatologia. SBD Kids. [acesso 29 Jun 2013]. Disponível em: http://www.sbd.org.br/acoes/sbd-kids/.
» http://www.sbd.org.br/acoes/sbd-kids/ -
99Reynolds KD, Buller DB, Yaroch AL, Maloy J, Geno CR, Cutter GR. Effects of program exposure and engagement with tailored prevention communication on sun protection by young adolescents. J Health Commun. 2008;13:619-36.
-
100Balk SJ, Fisher DE, Geller AC. Teens and indoor tanning: a cancer prevention opportunity for pediatricians. Pediatrics. 2013;131:772-85.
-
101Armstrong AW, Idriss NZ, Kim RH. Effects of video-based, online education on behavioral and knowledge outcomes in sunscreen use: a randomized controlled trial. Patient Educ Couns. 2011;83:273-7.
-
102Suppa M, Cazzaniga S, Fargnoli MC, Naldi L, Peris K. Knowledge, perceptions and behaviours about skin cancer and sun protection among secondary school students from Central Italy. J Eur Acad Dermatol Venereol. 2013;27:571-9.
-
103Buendía Eisman A, Arias Santiago S, Moreno-Gimenez JC, Cabrera-León A, Prieto L, Castillejo I, et al. An Internet-based programme to promote adequate UV exposure behaviour in adolescents in Spain. J Eur Acad Dermatol Venereol. 2013;27:442-53.
-
104Glazebrook C, Garrud P, Avery A, Coupland C, Williams H. Impact of a multimedia intervention "Skinsafe" on patients' knowledge and protective behav- iors. Prev Med. 2006;42:449-54.
-
105Glanz K, Schoenfeld ER, Steffen A. A randomized trial of tailored skin cancer prevention messages for adults: Project SCAPE. Am J Public Health. 2010;100:735-41.
-
106Prochaska JO, Velicer WF, Redding C, Rossi JS, Goldstein M, DePue J, et al. Stage-based expert systems to guide a population of primary care patients to quit smoking, eat healthier, prevent skin cancer, and receive regular mammo- grams. Prev Med. 2005;41:406-16.
-
107Prochaska JO, Velicer WF, Rossi JS, Redding CA, Greene GW, Rossi SR, et al. Multiple risk expert systems interventions: impact of simultaneous stage- matched expert system interventions for smoking, high-fat diet, and sun exposure in a population of parents. Health Psychol. 2004;23:503-16.
-
108Geller AC, Emmons KM, Brooks DR, Powers C, Zhang Z, Koh HK, et al. A randomized trial to improve early detection and prevention practices among siblings of melanoma patients. Cancer. 2006;107:806-14.
-
109Hillhouse J, Turrisi R, Stapleton J, Robinson J. A randomized controlled trial of an appearance-focused intervention to prevent skin cancer. Cancer. 2008;113:3257-66.
-
110Mahler HI, Kulik JA, Gerrard M, Gibbons FX. Long-term effects of appearance-based interventions on sun protection behaviors. Health Psychol. 2007;26:350-60.
-
111Stapleton J, Turrisi R, Hillhouse J, Robinson JK, Abar B. A comparison of the efficacy of an appearance-focused skin cancer intervention within indoor tanner subgroups identified by latent profile analysis. J Behav Med. 2010;33:181-90.
-
112Turrisi R, Mastroleo NR, Stapleton J, Mallett K. A comparison of 2 brief intervention approaches to reduce indoor tanning behavior in young women who indoor tan very frequently. Arch Dermatol. 2008;144:1521-4.
-
113Fartasch M, Diepgen TL, Schmitt J, Drexler H. The relationship between occupational sun exposure and non-melanoma skin cancer: clinical basics, epidemiology, occupational disease evaluation, and prevention. Dtsch Arztebl Int. 2012;109:715-20.
-
114Reeder AI, Gray A, McCool JP. Occupational sun protection: workplace culture, equipment provision and outdoor workers' characteristics. J Occup Health. 2013;55:84-97.
-
115Falk M, Anderson CD. Influence of age, gender, educational level and self-estimation of skin type on sun exposure habits and readiness to increase sun protection. Cancer Epidemiol. 2013;37:127-32.
-
116Jennings L, Karia PS, Jambusaria-Pahlajani A, Whalen FM, Schmults CD. The Sun Exposure and Behaviour Inventory (SEBI): validation of an instrument to assess sun exposure and sun protective practices. J Eur Acad Dermatol Venereol. 2013;27:706-15.
-
117Jung GW, Senthilselvan A, Salopek TG. Ineffectiveness of sun awareness posters in dermatology clinics. J Eur Acad Dermatol Venereol. 2010;24:697-703.
-
118Haluza D, Cervinka R. Perceived relevance of educative information on public (skin) health: a cross-sectiona l questionnaire survey. J Prev Med Public Health. 2013;46:82-8.
-
119Murphy GM. Photoprotection: public campaigns in Ireland and the U.K. Br J Dermatol. 2002;146:31-3.
-
120Thomas K, Hevey D, Pertl M, Ní Chuinneagáin S, Craig A, Maher L. Appearance matters: the frame and focus of health messages influences beliefs about skin cancer. Br J Health Psychol. 2011;16:418-29.
-
121Jung GW, Senthilselvan A, Salopek TG. Likelihood of dermatology patients to inquire about sun protection measures during a regular clinic visit. J Cutan Med Surg. 2011;15:266-74.
-
122Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27:237-51.
-
123Schalka S, Reis VM. Sun protection factor: meaning and controversies. An Bras Dermatol. 2011;86:507-15.
-
124Monteiro EO. Filtros solares e fotoproteção. RBM Rev Bras Med. 2010;67:5-18.
-
125Shaat NA. The chemistry of ultraviolet filters In: Shaat NA. Sunscreens: regulation and commercial development. 3. ed. Boca Raton: Taylor and Francis; 2005. p. 217-39.
-
126Schlossman D, Sho Y. Inorganic ultraviolet filters In: Shaat NA. Sunscreens: regulation and commercial development. 3. ed. Boca Raton: Taylor and Francis, 2005. p. 239-81.
-
127Agência Nacional de Vigilância Sanitária (Brasil). Resolução nº 211, de 14 de Julho de 2005. Estabelece a Definição e a Classificação de Produtos de Higiene Pessoal, Cosméticos e Perfumes, conforme Anexo I e II desta Resolução e dá outras definições. Diario Oficial da União jul 2005.
-
128Brasil. Agência Nacional de Vigilância Sanitária. Resolução - RDC no 30, de 1o de junho de 2012. Aprova o Regulamento Técnico Mercosul sobre Protetores solares em Cosméticos e dá outras providências. Diario Oficial da União jun 2012. [acesso 6 Nov 2014]. Disponível em: http://portal.anvisa.gov.br/wps/wcm/connect/e15afe804c58f17fb8f0f8dc39d59d3e/Resolu%C3%A7%C3%A3o+RDC+N%C2%BA+30,+de+1%C2%BA+de+Junho+de+2012.pdf?MOD=AJPERES.
» http://portal.anvisa.gov.br/wps/wcm/connect/e15afe804c58f17fb8f0f8dc39d59d3e/Resolu%C3%A7%C3%A3o+RDC+N%C2%BA+30,+de+1%C2%BA+de+Junho+de+2012.pdf?MOD=AJPERES -
129Kenneth K, Palefsky I. Formulation sunscreens products In: Shaat NA. Sunscreens: regulation and commercial development. 3rd ed. Boca Raton: Taylor and Francis; 2005. p. 353-85.
-
130Teixeira SMMCG. Veiculação de filtros solares utilizados na fotoproteção. [dissertação]. Porto (PT): Universidade Fernando Pessoa; 2012.
-
131Prista LN, Alves AC, Morgado R. Técnicas Farmacêuticas e Farmácia Galênica. Vol II, 3. ed. Lisboa: Fundação Calouste Gulbenkian; 1990.
-
132Associação Nacional de Farmacêuticos Magistrais. Manual de Recomendações para Aviamento de Formulações Magistrais: Boas Práticas de Manipulação. São Paulo: ANFARMAG; 1997.
-
133Cross SE, Innes B, Roberts MS, Tsuzuki T, Robertson TA, McCormick P. Human skin penetration of sunscreens nanoparticles: in vitro assessment of a novel micronized zinc oxide formulations. Skin Pharmacol Physiol. 2007;20:148-54.
-
134Kibbe AH. Handbook of Pharmaceutical Excipients. 3. ed. Washington: APhA and PP; 2000.
-
135Draelos ZD. Compliance and sunscreens. Dermatol Clin. 2006;24:101-4.
-
136Draelos ZD. The multifunctional value of sunscreen-containing cosmetics. Skin Therapy Lett. 2011;16:1-3.
-
137Lodén M. The clinical bennefit of moisturizers. J Eur Acad Dermatol Venereol. 2005;19:672-88.
-
138Kraft JN, Lynde CW. Moisturizers: what they are and a practical approach to product selection. Skin Therapy Lett. 2005;10:1-8.
-
139Seite S, Fourtanier A, Rougier A. Photoprotection in moisturizers and daily-care products. G Ital Dermatol Venereol. 2010;145:631-6.
-
140Polefka TG, Meyer TA, Agin PP, Bianchini RJ. Cutaneous oxidative stress. J Cosmet Dermatol. 2012;11:55-64.
-
141Yaar M, Gilchrest BA. Photoageing: mechanism, prevention and therapy. Br J Dermatol. 2007;157:874-87.
-
142Watson RE, Griffiths CE. Pathogenic aspects of cutaneous photoaging. J Cosmet Dermatol. 2005;4:230-6.
-
143Chen L, Hu JY, Wang SQ.The role of antioxidants in photoprotection: a critical review. J Am Acad Dermatol. 2012;67:1013-24.
-
144Wu Y, Matsui MS, Chen JZ, Jin X, Shu CM, Jin GY, et al. Antioxidants add protection to a broad-spectrum sunscreen. Clin Exp Dermatol. 2011;36:178-87.
-
145Matsui MS, Hsia A, Miller JD, Hanneman K, Scull H, Cooper KD, et al. Non-sunscreen photoprotection: antioxidants add value to a sunscreen. J Investig Dermatol Symp Proc. 2009;14:56-96.
-
146Lin JY, Selim MA, Shea CR, Grichnik JM, Omar MM, Monteiro-Riviere NA, et al. UV photoprotection by combination topical antioxidants vitamin C and vitamin E. J Am Acad Dermatol. 2003;48:866-74.
-
147Katiyar SK, Matsui MS, Elmets CA, Mukhtar H. Polyphenolic antioxidant (-)-epigallocatechin-3-gallate from green tea reduces UVB-induced inflammatory responses and infiltration of leukocytes in human skin. Photochem Photobiol. 1999;69:148-53.
-
148Olsen EA, Katz HI, Levine N, Nigra TP, Pochi PE, Savin RC, et al. Tretinoin emollient cream for photodamaged skin: results of 48-week, multicenter, double-blind studies. J Am Acad Dermatol. 1997;37:217-26.
-
149Wang SQ, Stanfield JW, Osterwalder U. In vitro assessments of UVA protection by popular sunscreens available in the United States. J Am Acad Dermatol. 2008;59:934-42.
-
150Agência Nacional de Vigilância Sanitária (Brasil). Resolução nº 19, de 10 de Abril de 2013. Dispõe sobre os requisitos técnicos para a concessão de registro de produtos cosméticos repelentes de insetos e dá outras providências. Diario Oficial da União abr 2013.
-
151Hexsel CL, Bangert SD, Hebert AA, Lim HW. Current sunscreen issues: 2007 food and drug administraion sunscreen labelling recommendations and combination sunscreen/insect repelente products. 2008;59:316-23.
-
152Pollack RJ, Kiszewski AE, Spielman A. Repelling mosquitoes. N Engl J Med. 2002;347:2-3.
-
153Kasichayanula S, House JD, Wang T, Gu X. Percutaneous characterization of the insect repellent DEET and the sunscreen oxybenzone from topical skin application. Toxicol Appl Pharmacol. 2007;223:187-94.
-
154Chen T, Burczynski FJ, Miller DW, Gu X. Percutaneous permeation comparison of repellents picaridin and DEET in concurrent use with sunscreen oxybenzone from commercially available preparations. Pharmazie. 2010;65:835-9.
-
155Murphy ME, Montemarano AD, Debboun M, Gupta R. The effect of sunscreen on the efficacy of insect repellent: A clinical trial. J Am Acad Dermatol. 2000;43:219-22.
-
156Agência Nacional de Vigilância Sanitária. Guia de Avaliação de Segurança de produto cosmético. 2 ed. Brasília: Anvisa; 2003.
-
157Schlumpf M, Cotton B, Conscience M, Haller V, Steinmann B, Lichtensteiger W. In vitro and in vivo estrogenicity of UV screens. Environ Health Perspect. 2001;109:239-44.
-
158Scientific Comission of Consumer safety. European commission. Opinion on the Evaluation of Potentially Estrogenic Effects of UV-filters adopted by the SCCNFP during the 17th Plenary meeting of 12 June 2001.
-
159Schauder S, Ippen H. Contact and photocontact sensitivity to sunscreens. Review of a 15-year experience and of the literature. Contact Dermatitis. 1997;37:221-32.
-
160Avenel-Audran M. Sunscreen products: Finding the allergen. Eur J Dermatol. 2010;20:161-6.
-
161Kaur IP, Agrawal R. Nanotechnology: a new paradigm in cosmeceuticals. Recent Pat Drug Deliv Formul. 2007;1:171-82.
-
162Andersson-Willman B, Gehrmann U, Cansu Z, Buerki-Thurnherr T, Krug HF, Gabrielsson S, et al. Effects of subtoxic concentrations of TiO2 and ZnO nanoparticles on human lymphocytes, dendritic cells and exosome production. Toxicol Appl Pharmacol. 2012;264:94-103.
-
163Roelandts R. History of human photobiology In: Lim HW, Hönigsmann H, Hawk JLM. Photodermatology. New York: Informa Healthcare USA; 2007. p 1-13.
-
164Vainio H, Miller AB, Bianchini F. An international evaluation of the cancer-preventive potential of sunscreens. Int J Cancer. 2000;88:838-42.
-
165Rigel DS. The effect of sunscreen on melanoma risk. Dermatol Clin. 2002;20:601-6.
-
166Diffey BL. Sunscreen and melanoma: The future looks bright. Br J Dermatol. 2005;153:378-81.
-
167Food and Drug Administration. Department of Health, Education and Welfare, FDA. Sunscreen drug products for over-the-counter drugs: proposed safety, effective and labeling conditions. Federal register.43/166.38206-38269.25 August 1978. Available from:http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Over-theCounterOTCDrugs/StatusofOTCRulemakings/ucm090127.pdf
» http://www.fda.gov/downloads/Drugs/DevelopmentApprovalProcess/DevelopmentResources/Over-theCounterOTCDrugs/StatusofOTCRulemakings/ucm090127.pdf -
168Food and Drug Administration. Department of Health and Human Services, FDA. Sunscreen Drug Product for Over-The-Counter Human Use, Final Rule, Federal Register vol. 1978N-0038. Available from: http://www.fda.gov/OHRMS/DOCKETS/98fr/cd031.pdf
» http://www.fda.gov/OHRMS/DOCKETS/98fr/cd031.pdf -
169International Sun Protector Factor Test Method. International SPF Test Method 2006 (COLIPA - CTFA SA - JCIA - CTFA US)
-
170European Cosmetics Association. COLIPA Guidelines. Guidelines for evaluating sun product water resistance. October 2004.
-
171Moyal D, Chardon A, Kollias N. Determination of UVA protection factors using the persistent pigment darkening (PPD) as the end point (part 1):calibration of the method. Photodermatol Photoimmunol Photomed. 2000 Dec;16:245-9.
-
172Moyal D, Chardon A, Kollias N. UVA protecion efficacy of sunscreens can be determinated by the persistent pigment darkening (PPD) method (part 2). Photodermatol Photoimmunol Photomed. 2000;16:250-5.
-
173European Cosmetics Association. COLIPA Method for the in vitro determination of UVA protection provided by sunscreen products. COLIPA Guideline, 2009.
-
174Moyal D, Wichrowski K, Tricaud C. In vivo persistent pigment darkening method: a demonstration of the reproducibility of the UVA protection factors results at several testing laboratories. Photodermatol Photoimmunol Photomed. 2006;22:124-8.
-
175Diffey BL, Tanner PR, Matts PJ, Nash JF. In vitro assessment of the broad-spectrum ultraviolet protection of sunscreen products. J Am Acad Dermatol. 2000;43:1024-35.
-
176Gaspar LR, Maia Campos PM. Evaluation on the photostability of different UV filter combinations in a sunscreen. Int J Pharm. 2006;307:123-8.
-
177Mahmoud BH, Hexsel CL, Hamzavi IH, Lim HW. Effects of visible light on the skin. Photochem Photobiol. 2008;84:450-62.
-
178Schalka S, Addor FAS, Agelune CM, Pereira VMC. Sunscreen protection against visible light: a new proposal for Evaluation. Surg Cosmet Dermatol 2012;3:45-52.
-
179Schieke SM, Schroeder P, Krutmann J. Cutaneous effects of infrared radiation: from clinical observations to molecular response mechanisms. Photodermatol Photoimmunol Photomed. 2003;19:228-34.
-
180International Organization for Standardization. ISO/TC 217 - Cosmetics WG7 - Sun protection test methods, 1998.
-
181Bouilly-Gauthier D, Jeannes C, Maubert Y, Duteil L, Queille-Roussel C, Piccardi N, et al. Benefits of a dietary supplement on UV-induced skin damage. Br J Dermatol. 2010;163:536-43.
-
182Petit-Frère C, Clingen PH, Grewe M, Krutmann J, Roza L, Arlett CF, et al. Induction of IL6 produc- tion by UV radiation in normal epidermal keratinocytes and in a human keratinocyte line is mediated by DNA damage. J Invest Dermatol. 1998;111:354-9.
-
183Schwarz A, Schwarz T. Molecular determinants of UV-induced immunosuppression. Exp Dermatol. 2002;11:9-12.
-
184Rabe JH, Mamelak AJ, McElgunn PJ, Morison WL, Sauder DN. Photoaging: mechanisms and repair. J Am Acad Dermatol. 2006;55:1-19.
-
185Pillai S, Oresajo C, Hayward J. Ultraviolet radiation and skin aging: role of reactive oxygen species, inflammation and protease activation, and strategies for prevention of inflammation induced: a review. Int J Cosmet Sci. 2005;27:17-34.
-
186Biesalski HK, Berneburg M, Grune T, Kerscher M, Krutmann J, Raab W, et al. Hohenheimer Consensus Talk. Oxidative and premature skin ageing. Exp Dermatol. 2003;12 Suppl 3:3-15.
-
187Bernstein EF, Brown DB, Schwartz MD, Kaidbey K, Ksenzenko SM. The polyhydroxy acid gluconolactone protects against ultraviolet radiation in an in vitro model of cutaneous photoaging. Dermatol Surg. 2004;30:189-95
-
188Seité S, Christiaens F, Bredoux C, Compan D, Zucchi H, Lombard D, et al. A broad-spectrum sunscreen prevents cumulative damage from repeated exposure to suberythe- mal solar ultraviolet radiation representative of temperate latitudes. J Eur Acad Dermatol Venereol. 2010;24:219-22.
-
189Gilaberte Y, González S. Update on Photoprotection Actas Dermosifiliogr. 2010;101:659-72.
-
190Schagen SK, Zampeli VA, Makrantonaki E, Zouboulis CC. Discovering the link between nutrition and skin aging. Dermatoendocrinol. 2012;4:298-307.
-
191Draelos ZD. Nutrition and enhancing youthful- appearing skin. Clin Dermatol. 2010;28:400-8.
-
192Makrantonaki E, Zouboulis C. Skin alterations and diseases in advanced age. Drug Discov Today Dis Mech. 2008;5:e153-62.
-
193Pinnell SR. Cutaneous photodamage, oxidative stress, and topical antioxidant protection. J Am Acad Dermatol. 2003;48:1-19.
-
194Wang SQ, Osterwalder U, Jung K. Ex vivo evaluation of radical sun protection factor in popular sunscreens with antioxidants. J Am Acad Dermatol. 2011;65:525-30.
-
195Fryer MJ. Evidence for the photoprotective effects of vitamin E. Photochem Photobiol. 1993;58:304-12.
-
196Chan AC, Tran K, Raynor T, Ganz PR, Chow CK. Regeneration of vitamin E in human platelets. J Biol Chem. 1991;266:17290-5.
-
197Scarmo S, Cartmel B, Lin H, Leffell DJ, Welch E, Bhosale P, et al. Significant correlations of dermal total carotenoids and dermal lycopene with their respective plasma levels in healthy adults. Arch Biochem Biophys. 2010;504:34-9.
-
198Mireles-Rocha H, Galindo I, Huerta M, Trujillo-Hernández B, Elizalde A, Cortés-Franco R. UVB photoprotection with antioxidants: effects of oral therapy with dalpha-tocopherol and ascorbic acid on the minimal erythema dose. Acta Derm Venereol. 2002;82:21-4.
-
199Placzek M, Gaube S, Kerkmann U, Gilbertz KP, Herzinger T, Haen E, et al. Ultraviolet B-induced DNA damage in human epidermis is modified by the antioxidants ascorbic acid and D-alpha-tocopherol. J Invest Dermatol. 2005;124:304-7.
-
200Eberlein-König B, Ring J. Relevance of vitamins C and E in cutaneous photoprotection. J Cosmet Dermatol. 2005;4:4-9.
-
201Ribaya-Mercado JD, Garmyn M, Gilchrest BA, Russell RM. Skin lycopene is destroyed preferentially over beta-carotene during ul- traviolet irradiation in humans. J Nutr. 1995;125:1854-9.
-
202Sies H, Stahl W. Carotenoids and UV protection. Photochem Photobiol Sci. 2004;3:749-52.
-
203Sies H, Stahl W. Nutritional protection against skin damage from sunlight. Annu Rev Nutr. 2004;24:173-200.
-
204Alaluf S, Heinrich U, Stahl W, Tronnier H, Wiseman S. Dietary carotenoids contribute to normal human skin color and UV photosensitivity. J Nutr. 2002;132:399-403.
-
205Grune T, Lietz G, Palou A, Ross AC, Stahl W, Tang G, et al. Beta-carotene is an important vitamin A source for humans. J Nutr. 2010;140:2268S-2285S.
-
206Köpcke W, Krutmann J. Protection from sunburn with beta-Carotene-a meta-analysis. Photochem Photobiol. 2008;84:284-8.
-
207Stahl W, Heinrich U, Jungmann H, Sies H, Tronnier H. Carotenoids and carotenoids plus vitamin E protect against ultraviolet light-induced erythema in humans. Am J Clin Nutr. 2000;71:795-8.
-
208Mathews-Roth MM, Pathak MA, Parrish J, Fitzpatrick TB, Kass EH, Toda K, et al. A clinical trial of the effects of oral beta-carotene on the responses of human skin to solar radiation. J Invest Dermatol. 1972;59:349-53.
-
209Lee J, Jiang S, Levine N, Watson RR. Carotenoid supplementation reduces erythema in human skin after simulated solar radiation exposure. Proc Soc Exp Biol Med. 2000;223:170-4.
-
210Heinrich U, Gärtner C, Wiebusch M, Eichler O, Sies H, Tronnier H, et al. Supplementation with beta- carotene or a similar amount of mixed carotenoids protects humans from UV-induced erythema. J Nutr. 2003;133:98-101.
-
211Wolf C, Steiner A, Hönigsmann H. Do oral carotenoids protect human skin against ultraviolet ery- thema, psoralen phototoxicity, and ultraviolet-induced DNA damage? J Invest Dermatol. 1988;90:55-7.
-
212Eicker J, Kürten V, Wild S, Riss G, Goralczyk R, Krutmann J, et al. Betacarotene supplementation protects from photoaging-associated mitochondrial DNA mutation. Photochem Photobiol Sci. 2003;2:655-9.
-
213Lorenz RT, Cysewski GR. Commercial potential for Haematococcus microalgae as a natural source of astaxanthin. Trends Biotechnol. 2000;18:160-7.
-
214Higuera-Ciapara I, Félix-Valenzuela L, Goycoolea FM. Astaxanthin: a review of its chemistry and applications. Crit Rev Food Sci Nutr. 2006;46:185-96.
-
215Lyons NM, O'Brien NM. Modulatory effects of an algal extract containing astaxanthin on UVA-irradiated cells in culture. J Dermatol Sci. 2002;30:73-84.
-
216Camera E, Mastrofrancesco A, Fabbri C, Daubrawa F, Picardo M, Sies H, et al. Astaxanthin, canthaxan- thin and beta-carotene differently affect UVA-induced oxidative damage and expression of oxidative stress- responsive enzymes. Exp Dermatol. 2009;18:222-31.
-
217Suganuma K, Nakajima H, Ohtsuki M, Imokawa G. Astaxanthin attenuates the UVA-induced up-regula- tion of matrix-metalloproteinase-1 and skin fibroblast elastase in human dermal fibroblasts. J Dermatol Sci. 2010;58:136-42.
-
218Stahl W, Heinrich U, Aust O, Tronnier H, Sies H. Lycopene-rich products and dietary photoprotection. Photochem Photobiol Sci. 2006;5:238-42.
-
219Lee EH, Faulhaber D, Hanson KM, Ding W, Peters S, Kodali S, et al. Dietary lutein reduces ultraviolet radiation-induced inflammation and immunosuppression. J Invest Dermatol. 2004;122:510-7.
-
220Palombo P, Fabrizi G, Ruocco V, Ruocco E, Fluhr J, Roberts R, et al. Beneficial long-term effects of combined oral/topical antioxidant treatment with the carotenoids lutein and zeaxanthin on human skin: a double-blind, placebo-controlled study. Skin Pharmacol Physiol. 2007;20:199-210.
-
221Manach C, Scalbert A, Morand C, Rémésy C, Jiménez L. Polyphenols: food sources and bioavailability. Am J Clin Nutr. 2004;79:727-47.
-
222Scalbert A, Williamson G. Dietary intake and bioavail- ability of polyphenols. J Nutr. 2000;130:2073S-85S.
-
223Scalbert A, Johnson IT, Saltmarsh M. Polyphenols: antioxidants and beyond. Am J Clin Nutr. 2005;81:215S-217S.
-
224Nichols JA, Katiyar SK. Skin photoprotection by natural polyphenols: anti-inflammatory, antioxidant and DNA repair mechanisms. Arch Dermatol Res. 2010;302:71-83.
-
225Halliwell B, Rafter J, Jenner A. Health promotion by flavonoids, tocopherols, tocotrienols, and other phenols: direct or indirect effects? Antioxidant or not? Am J Clin Nutr. 2005;81:268S-76S.
-
226Moskaug JØ, Carlsen H, Myhrstad MC, Blomhoff R. Polyphenols and glutathione synthesis regula- tion. Am J Clin Nutr. 2005;81:277S-283S.
-
227Lambert JD, Hong J, Yang GY, Liao J, Yang CS. Inhibition of carcinogenesis by polyphenols: evidence from laboratory investigations. Am J Clin Nutr. 2005;81:284S-291S.
-
228Jeon HY, Kim JK, Kim WG, Lee SJ. Effects of oral epigallocatechin gallate supplementation on the minimal eruthema dose and UV-induced skin damage. Skin Pharmacol Physiol. 2009;22:137-41.
-
229Wei H, Saladi R, Lu Y, Wang Y, Palep SR, Moore J, et al. Isoflavone genistein: photoprotection and clinical implications in dermatology. J Nutr. 2003;133:3811S-3819S.
-
230Erden Inal M, Kahraman A. The protective effect of flavonol quercetin against ultraviolet A induced oxidative stress in rats. Toxicology. 2000;154:21-9.
-
231Erden Inal M, Kahraman A, Köken T. Beneficial effects os quercetin on oxidative stress induced by ultraviolet A. Clin Exp Dermatol. 2001;26:536-9.
-
232Saliou C, Rimbach G, Moini H, McLaughlin L, Hosseini S, Lee J, et al. solar ultraviolet-induced erythema in human skin and nuclear factor-kappa-B-dependent gene expression in keratinocytes are modulated by a French maritime pine bark extract. Free Radic Biol Med. 2001;30:154-60.
-
233Fuller R. Probiotics in man and animals. J Appl Bacteriol. 1989;66:365-78.
-
234Guéniche A, Benyacoub J, Buetler TM, Smola H, Blum S. Supplementation with oral probiotic bac- teria maintains cutaneous immune homeostasis after UV exposure. Eur J Dermatol. 2006;16:511-7.
-
235Peguet-Navarro J, Dezutter-Dambuyant C, Buetler T, Leclaire J, Smola H, Blum S, et al. Supplementation with oral probiotic bacteria protects human cutaneous immune homeostasis after UV exposure-double blind, randomized placebo controlled clinical trial. Eur J Dermatol. 2008;18:504-11.
-
236Guéniche A, Philippe D, Bastien P, Blum S, Buyukpamukcu E, Castiel-Higounenc I. Probiotics for photoprotection. Dermatoendocrinol. 2009;1:275-9.
-
237Morganti P, Bruno C, Guarneri F, Cardillo A, Del Ciotto P, Valenzano F. Role of topical and nutritional supplement to modify the oxidative stress. Int J Cosmet Sci. 2002;24:331-9.
-
238Greul AK, Grundmann JU, Heinrich F, Pfitzner I, Bernhardt J, Ambach A, et al. Photoprotection of UV-irradiated human skin: an antioxidative combination of vitamins E and C, carotenoids, selenium and proanthocyanidins. Skin Pharmacol Appl Skin Physiol. 2002;15:307-15.
-
239Cho HS, Lee MH, Lee JW, No KO, Park SK, Lee HS, et al. Anti-wrinkling effects of the mixture of vitamin C, vitamin E, pycnogenol and evening primrose oil, and molecular mechanisms on hairless mouse skin caused by chronic ultraviolet B irradiation. Photodermatol Photoimmunol Photomed. 2007;23:155-62.
-
240Rona C, Berardesca E. Aging skin and food supplements: the myth and the truth. Clin Dermatol. 2008;26:641-647.
-
241Rhodes LE, Durham BH, Fraser WD, Friedmann PS. Dietary fish oil reduces basal and ultraviolet B-generated PGE2 levels in skin and increases the threshold to provocation of polymorphic light eruption. J Invest Dermatol. 1995;105:532-5.
-
242Gonzalez S, Pathak MA. Inhibition of ultraviolet-induced formation of reactive oxygen species, lipid peroxidation, erythema and skin photosemsitization by Polipodium leucotomos. Photodermatol Photoimmunol Photomed. 1996;12:45-56.
-
243Gonzales S, Pathak MA, Cuevas J, Villarrubia VG, Fitzpatrick TB. Topical or oral administration with an extract of Polypodium leucomotos prevents acute sunburn and psoralen-induced phototoxic reactions as weel as depletion of Langerhans cells in human skin. Photodermatol Photoimmunol Photomed. 1997;13:50-60.
-
244Gonzalez S, Gilaberte Y, Philips N, Juarranz A. Fernblock, a nutriceutical with photoprotective properties and potential preventive agent for skin photoaging and photoinduced skin cancers. Int J Mol Sci. 2011;12:8466-75.
-
245Garcia F, Pivel JP, Guerrero A, Brieva A, Martinez-Alcazar MP, Caamano-Somoza M, et al. Phenolic components and antioxidant activity of Fernblock, an aqueous extract of the aerial parts of the fern Polypodium leucotomos. Methods Find Exp Clin Pharmacol. 2006;28:157-60.
-
246Middelkamp-Hup MA, Pathak MA, Parrado C, Garcia-Caballero T, Rius-Díaz F, Fitzpatrick T, et al. Orally administered Polypodium leucomotos extract decreases psoralen-UVA-induced phototoxicity, pigmentation, and damage of human skin. J Am Acad Dermatol 2004;50:41-9.
-
247Middelkamp-Hup MA, Pathak MA, Parrado C, Goukassian D, Rius-DÍaz F, Mihm MC, et al. Oral polypodium leucomotos extract decreases ultraviolet- induced damage of human skin. J Am Acad Dermatol. 2004;51:910-8.
-
248Capote R, Alonso-Lebrero JL, García F, Brieva A, Pivel JP, González S. Polypodium leucotomos extract inhibits trans-urocanic acid photoisomerization and photodecomposition. J Photochem Photobiol B. 2006;82:173-179.
-
249Alonso-Lebrero JL, Domínguez-Jiménez C, Tejedor R, Brieva A, Pivel JP. Photoprotective properties of a hydrophilic extract of the fern Polypodium leucotomos on human skin cells. J Photochem Photobiol B. 2003;70:31-7.
-
250Caccialanza M, Recalcati S, Piccinno R. Oral polypodium leucotomos extract photoprotective activity in 57 patients with idiopathic photodermatoses. G Ital Dermatol Venereol. 2011;146:85-7.
-
251Ahmed AM, Lopez I, Perese F, Vasquez R, Hynan LS, Chong B, Pandya AG. A Randomized, Double-Blinded, Placebo-Controlled Trial of Oral Polypodium leucotomos Extract as an Adjunct to Sunscreen in the Treatment of Melasma. JAMA Dermatol. 2013;149:981-3.
-
252Andrés-Lacueva C, Monagas M, Khan N, Izquierdo-Pulido M, Urpi-Sarda M, Permanyer J, et al. Flavanol and flavonol contents of cocoa powder products: influence of the manufacturing process. J Agric Food Chem. 2008;56:3111-7.
-
253Williams S, Tamburic S, Lally C. Eating chocolate can significantly protect the skin from UV light. J Cosmet Dermatol. 2009;8:169-73.
-
254Abel E, Hendrix S, McNeelyS, Johnson K, Rosenberg C, Mossavar-Rahmani Y, et al. Daily coffee consumption and prevalence of nonmelanoma skin câncer in Caucasian women. Eur J Cancer Prev. 2007;16:446-52.
-
255Kerzendorfer C, O'Driscoll M. UV-B and caffeine: inhibiting the DNA damage response to protect against the adverse effects of UV-B. J Invest Dermatol. 2009;129:1611-3.
-
256Edwards EK Jr, Horwitz SN, Frost P. Reduction of the erythema response to ultraviolet light by nonsteroidal antiinflammatory agents. Arch Dermatol Res. 1982;272:263-7.
-
257Abdel-Malek Z, Ruwe A, Kavanagh-Starner R, Kadekaro AL, Swope V, Haskell-Luevano C, et al. Alpha-MSH tripeptide analogs activate the melanocortin 1 receptor and reduce UV-induced DNA damage in human melanocytes. Pigment Cell Melanoma Res. 2009;22:635-44.
-
258Harms J, Lautenschlager S, Minder C, Minder E. An Alpha-melanocyte-stimulating hormone analogue in erytropoietic protoporphyria. N Eng J Med. 2009;360:306-7.
-
259Gies P. Photoprotection by clothing. Photodermatol Photoimmunol Photomed. 2007;23:264-74.
-
260Morison WL. Photoprotection by clothing. Dermatol Ther. 2003:16:16-22.
-
261Kullavanijava P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.
-
262Palm M, Donoghue M. Uptade on photoprotection. Dermatologic Therapy. 2007;20;360-376.
-
263Wang SQ, Balagula Y, Osterwalder U. Photoprotection: a review of the current and future technologies. Dermatol Ther. 2010;23:31-47.
-
264Ghazi S, Couteau C, Paparis E, Coiffard LJM. Interest of external photoprotection by means of clothing and sunscreen products in young children. J Eur Acad Dermatol Venereol. 2012;26:1026-30.
-
265Criado P, Melo J, Oliveira Z N. Topical photoprotection in childhood and adolescence. J Pediatr. 2012;88:203-10.
-
266Bauer J, Büttner P, Wiecker TS, Luther H, Garbe C. Effect of Sunscreen and Clothing the Nunber of Melanocitic Nevi in 1812 germa Children Attendin Day. Am J Epidemiol. 2005;161:620-7.
-
267Gambichler T, Laperre J, Hoffmann K. The European standard for sun-protective clothing : EN 13758. J Eur Acad Dermatol Venereol. 2006;20:125-130.
-
268Kütting B, Drexler H. UV-induced skin cancer at workplace and evidence-based prevention. Int Arch Occup Environ Health. 2010;83:843-54.
-
269Bauer A, Diepgen TL, Schmitt J. Is occupational solar ultraviolet irradiation a relevant risk factor for basal cell carcinoma? A systematic review and meta-analysis of the epidemiological literature. Br J Dermatol. 2011;165:612-25.
-
270Adam J. Sun-protective clothing. J Cutan Med Surg. 1998;3:50-3.
-
271Purim K, Leite N. Fotoproteção e exercício físico. Rev Bras Med Esporte. 2010;16-3.
-
272Alves LM, Aegerter MA, Hata K. In vitro determination of sun protection factor (SPF) of solar moderators. An Bras Dermatol. 1991;66:313-9.
-
273Mansur JS, Breder MNR, Mansur MCA, Azulay RD. Determination of sun protecting factor in human beings and by spectrophotometry: comparison between of the two methods. An Bras Dermatol. 1986;61:167-72.
-
274Balogh TS, Velasco MVA, Pedriali CA, Kaneko TM, Baby AR. Proteção à radiação ultravioleta: recursos disponíveis na atualidade em fotoproteção. An Bras Dermatol. 2011;86:732-42.
-
275Australian/New Zealand Standard® [Internet]. AS/NZS 4399:1996. Sun protective clothing-Evaluation and classification. [cited 2014 Oct 30]. Available from: http://www.saiglobal.com/pdftemp/previews/osh/as/as4000/4300/4399.pdf
» http://www.saiglobal.com/pdftemp/previews/osh/as/as4000/4300/4399.pdf -
276Hatua P, Majumdar A, Das A. Predicting the ultraviolet radiation protectio by polyester-cotton blended woven fabrics using nonlinear regression and artificial neural network models. Photodermatol Photoimmunol Photomed. 2013;29:182-9.
-
277Hatch KL, Osterwalder U. Garments as solar ultraviolet radiation screening materials. Dermatol Clin. 2006;24:85-100.
-
278Teixeira SP, Fotoproteção. RBM Rev Bras Med. 2010;10:115-22.
-
279Tuchinda C, Srivannaboon S, Lim H W. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol 2006;54:845-54.
-
280Dain SJ. Sunglasses and sunglass standards. Clin Exp Optom. 2003;86:77-90.
-
281Turnbull DJ, Parisi AV. Increasing the ultraviolet protection provided by shade structures. J Photochem Photobiol B. 2005;78:61-7.
-
282Lambert R, Pereira MM, Mansur HS. Biomateriais; fundamento e aplicações. Rio de Janeiro: Cultura Médica; 2006.
-
283Kein RS, Werth VP, Dowdy JC, Sayre RM. Analysus of compact fluorescent lights for use by patients with phtosensitive conditions. Photochem Photobiol. 2009;85:1004-10.
-
284Kimlin MG, Parisi AV. Ultraviolet radiation penetrating vehicle glass: a field based comparative study. Phys Med Biol 1999;44:917-926.
-
285Duarte I, Rotter A, Malvestiti A, Silva M. The role of glass as a barrier against the transmission of ultraviolet radiation: an experimental study. Photodermatol Photoimmunil Photomed. 2009;25:181-4.
-
286Almutawa F, Buabbas H. Photoprotection: clothing and glass. Dermatol Clin. 2014;32:439-48.
-
287Kniess CT, Kuhnen NC, Riella HG. Estudo do efeito da quantidade de óxido de ferro em cinzas pesadas de carvão mineral na obtenção de vitrocerâmicos. Quim Nova. 2002;25:926-30.
-
288Jou PC, Feldman RJ, Tomecki KJ. UV protection and sunscreens: what to tell patients. Cleve Clin J Med. 2012;79:427-36.
-
289Wolf R, Wolf D, Morganti P, Ruocco V. Sunscreens. Clin Dermatol. 2001;19:452-459.
-
290Orentreich D, Leone AS, Arpino G, Burack H. Sunscreens: practical applications. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.537-59.
-
291Koshy JC, Sharabi SE, Jerkins D, Cox J, Cronin SP, Hollier LH Jr. Sunscreens: evolving aspects of sun protection. Journal of pediatric health care: official publication of National Association of Pediatric Nurse Associates & Practitioners. 2010;24:343-6.
-
292Osterwalder U, Herzog B. Sun protection factors: world wide confusion. Br J Dermatol. 2009;161:13-24.
-
293Kullavanijya P, Lim HW. Photoprotection. J Am Acad Dermatol. 2005;52:937-58.
-
294Groves GA, Agin PP, Sayre PM. In vitro and In vivo methods to define sunscreen protection. Australas J Dermatol. 1979;20:112-9.
-
295Diffey BL. Sunscreens: use and misuse. In: Giacomoni PU, Häder DP, Jori G, editores. Sun protection in man. Amsterdam: Elsevier; 2001. p.523-534.
-
296Lautenschlager S, Wulf HC, Pittelkow MR. Photoprotection. Lancet. 2007;370:528-37.
-
297Lowe NJ. An overview of ultraviolet radiation, sunscreens, and photo-induced dermatoses. Dermatol Clin. 2009;24:9-17.
-
298Isedeh P, Osterwalder U, Lim HW. Teaspoon rule revisited: proper amount of sunscreen application. Photodermatol Photoimmunol Photomed. 2013;29:55-6.
-
299Lakhdar H, Zouhair K, Khadir K, Essari A, Richard A, Seite S, et al. Evaluation of the effectiveness of a broad-spectrum sunscreen in the prevention of chloasma in pregnant women. J Eur Acad Dermatol Venereol. 2007;21:738-42.
-
300Purim KS, Avelar MF. [Photoprotection, melasma and quality of life in pregnant women]. Rev Bras Ginecol Obstet. 2012;34:228-34.
-
301Pichardo R, Vallejos Q, Feldman SR, Schulz MR, Verma A, Quandt SA, et al. The prevalence of melasma and its association with quality of life in adult male Latino migrant workers. Int J Dermatol. 2009;48:22-6.
-
302Urasaki MBM. Alterações fisiológicas da pele percebidas por gestantes assistidas em serviços públicos de saúde. Acta Paul Enferm. 2010;23:519-25.
-
303Abarca J, Odilla Arrollo C, Blanch S, Arellano G. [Melasma in pregnancy: reduction of its appearance with the use of a broad-spectrum photoprotective agent]. Med Cutan Ibero Lat Am. 1987;15:199-203.
-
304Khadir K, Amal S, Hali F, Nejjam F, Lakhdar H. Les signes dermatologiques physiologiques de la grossesse. Ann Dermatol Venerol. 1999;126:15-9.
-
305Sambandan DR, Ratner D. Sunscreens: an overview and update. J Am Acad Dermatol. 2011;64:748-58.
-
306Boisen AM, Shipley T, Jackson P, Hougaard KS, Wallin H, Yauk CL, et al. NanoTIO(2) (UV-Titan) does not induce ESTR mutations in the germline of prenatally exposed female mice. Part FibreToxicol. 2012;9:19.
-
307Hougaard KS, Jackson P, Jensen KA, Sloth JJ, Loschner K, Larsen EH, et al. Effects of prenatal exposure to surface-coated nanosized titanium dioxide (UV-Titan). A study in mice. Part Fibre Toxicol. 2010;7:16.
-
308Umezawa M, Tainaka H, Kawashima N, Shimizu M, Takeda K. Effect of fetal exposure to titanium dioxide nanoparticle on brain development - brain region information. J Toxicol Sci. 2012;37:1247-52.
-
309Stern RS, Weinstein MC, Baker SG. Risk reduction for nonmelanoma skin cancer with childhood sunscreen use. Archives of dermatology. 1986;122(5):537-45.
-
310Wesson KM, Silverberg NB. Sun protection education in the United States: what we know and what needs to be taught. Cutis. 2003;71:71-4,77.
-
311Quatrano NA, Dinulos JG. Current principles of sunscreen use in children. Cur Opin Pediatr. 2013;25:122-9.
-
312Godar DE, Urbach F, Gasparro FP, van der Leun JC. UV doses of young adults. Photochem Photobiol. 2003;77:453-7.
-
313Parisi AV, Meldrum LR, Wong JC, Aitken J, Fleming RA. Effect of childhood and adolescent ultraviolet exposures on cumulative exposure in South East Queensland schools. Photodermatol Photoimmunol Photomed. 2000;16:19-24.
-
314Dusza SW, Halpern AC, Satagopan JM, Oliveria SA, Weinstock MA, Scope A, et al. Prospective study of sunburn and sun behavior patterns during adolescence. Pediatrics. 2012;129:309-17.
-
315Pustisek N, Sikanic-Dugic N, Hirsl-Hecej V, Domljan ML. Acute skin sun damage in children and its consequences in adults. Coll Antropol. 2010;34 Suppl 2:233-7.
-
316Dennis LK, Vanbeek MJ, Beane Freeman LE, Smith BJ, Dawson DV, Coughlin JA. Sunburns and risk of cutaneous melanoma: does age matter? A comprehensive meta-analysis. Ann Epidemiol. 2008;18:614-27.
-
317Balk SJ, Council on Environmental Health; Section on Dermatology. Ultraviolet Radiation: a Hazard to Children and Adolescents. Pediatrics. 2011;127:e791-e817.
-
318HealthyChildren.org/American Academy of Pediatrics [Internet]. Sun Safety: Information for Parents About Sunburn & Sunscreen, 2014. [cited 2014 Oct 30]. Available from: http://www.healthychildren.org/English/safety-prevention/atplay/Pages/Sun-Safety.aspx
» http://www.healthychildren.org/English/safety-prevention/atplay/Pages/Sun-Safety.aspx -
319American Academy of Dermatology [Internet]. Stats and facts - Prevention and care: Sunscreens 2013. [cited 2014 Oct 30]. Available from: http://www.aad.org/media-resources/stats-and-facts/prevention-and-care/sunscreens
» http://www.aad.org/media-resources/stats-and-facts/prevention-and-care/sunscreens -
320Holloway L. Atmospheric sun protection factor on clear days: its observed dependence on solar zenith angle and its relevance to the shadow rule for sun protection. Photochem photobiol. 1992;56:229-34.
-
321Agência Nacional de Vigilância Sanitária. ANVISA/MS. Resolução nº 56, de 9 de novembro de 2009.
-
322Halder RM, Bridgeman-Shah S. Skin cancer in African Americans. Cancer. 1995;75(2 Suppl):667-73.
-
323Baumann L, Rodriguez D, Taylor SC, Wu J. Natural considerations for skin of color. Cutis; cutaneous medicine for the practitioner. 2006;78(6 Suppl):2-19.
-
324Battie C, Gohara M, Verschoore M, Roberts W. Skin cancer in skin of color: an update on current facts, trends, and misconceptions. J Drugs Dermatol. 2013;12:194-8.
-
325Bradford PT. Skin cancer in skin of color. Dermatol Nurs. 2009;21:170-7, 206; quiz 178.
-
326Dominguez AR, Pandya A. Need for more education for latinos regarding sun-safe behaviors. Arch Dermatol 2011;147:820.
-
327Pichon LC, Corral I, Landrine H, Mayer JA, Adams-Simms D. Perceived skin cancer risk and sunscreen use among African American adults. J Health Psychol. 2010;15:1181-9.
-
328Summers P, Bena J, Arrigain S, Alexis AF, Cooper K, Bordeaux JS. Sunscreen use: Non-Hispanic Blacks compared with other racial and/or ethnic groups. Arch Dermatol. 2011;147:863-4.
-
329Batista T, Fissmer MC, Porton KR, Schuelter-Trevisol F. Assessment of sun protection and skin cancer prevention among preschool children. Rev Paul Pediatr. 2013;31:17-23.
-
330Moehrle M. Outdoor sports and skin cancer. Clin Dermatol. 2008;26:12-5.
-
331Moehrle M, Koehle W, Dietz K, Lischka G. Reduction of minimal erythema dose by sweating. Photodermatol Photoimmunol Photomed. 2000;16:260-2.
-
332Wysong A, Gladstone H, Kim D, Lingala B, Copeland J, Tang JY. Sunscreen use in NCAA collegiate athletes: identifying targets for intervention and barriers to use. Prev Med. 2012;55:493-6.
-
333Loden M, Beitner H, Gonzalez H, Edstrom DW, Akerstrom U, Austad J, et al. Sunscreen use: controversies, challenges and regulatory aspects. Br J Dermatol. 2011;165:255-62.
-
334Bodekaer M, Faurschou A, Philipsen PA, Wulf HC. Sun protection factor persistence during a day with physical activity and bathing. Photodermatol Photoimmunol Photomed. 2008;24:296-300.
-
335Davis A, Deane GH, Diffey BL. Possible dosimeter for ultraviolet radiation. Nature. 1976;261(5556):169-70.
-
336Mills A, McFarlane M, Schneider S. A viologen-based UV indicator and dosimeter. Anal Bioanal Chem. 2006;386:299-305.
-
337Heydenreich J, Wulf HC. Miniature personal electronic UVR dosimeter with erythema response and time-stamped readings in a wristwatch. Photochem Photobiol. 2005;81:1138-44.
-
338Scienterra Limited [Internet]. UV Dosimeter 2013. [cited 2014 Oct 30]. Available from: http://scienterra.com/#/home/4567276438/UV-Dosimeter/3113961.
» http://scienterra.com/#/home/4567276438/UV-Dosimeter/3113961 -
339Vázquez M, Sánchez JL. The efficacy of a broad-spectrum sunscreen in the treatment of melasma. Cutis. 1983;32:92,95-6.
-
340Cestari T, Arellano I, Hexsel D, Ortonne JP; Latin American Pigmentary Disorders Academy. Melasma in Latin America: options for therapy and treatment algorithm. J Eur Acad Dermatol Venereol. 2009;23:760-72.
-
341Ball Arefiev KL, Hantash BM. Advances in the treatment of melasma: a review of the recent literature. Dermatol Surg. 2012;38(7 Pt 1):971-84.
-
342Guinot C, Cheffai S, Latreille J, Dhaoui MA, Youssef S, Jaber K, et al. Aggravating factors for melasma: a prospective study in 197 Tunisian patients. J Eur Acad Dermatol Venereol. 2010;24:1060-9.
-
343Sheth VM, Pandya AG. Melasma: a comprehensive update: part II. J Am Acad Dermatol. 2011;65:699-714; quiz 715.
-
344Ni Z, Mu Y, Gulati O. Treatment of melasma with Pycnogenol. Phytother Res. 2002;16:567-71.
-
345Gupta AK, Gover MD, Nouri K, Taylor S. The treatment of melasma: A review of clinical trials. J Am Acad Dermatol. 2006;55:1048-65.
-
346Guevara IL, Pandya AG. Safety and efficacy of a 4% hydroquinone combined with 10% glycolic acid, antioxidants, and sunscreen in the treatment of melasma. Int J Dermatol. 2003;42:966-72.
-
347Stanfield JW, Feldman SR, Levitt J. Sun protection strength of a hydroquinone 4%/retinol 0.3% preparationn containing sunscreens. J Drugs Dermatol. 2006;5:321-4.
-
348Mahmoud BH, R-UVolo E, Hexsel CL, Liu Y, Owen MR, Kollias N, Lim HW, Hamzavi IV. Impact of long-wavelenght UVA and visible light on melanocompetent skin. J Invest Dermatol. 2010;130:2092-7.
-
349Shaath N. Sunscreens: regulation and comercial development. 3rd ed. Boca Raton: T&F informa; 2005. p. 325.
-
350Rendon M, Berneburg M, Arellano I, Picardo M. Treatment of melasma. J Am Acad Dermatol. 2006;54(5 Suppl 2):S272-81.
-
351Costa FB, Weber MB. Evaluation of solar exposure and sun-protection behaviors among university students in the Metropolitan Region of Porto Alegre, Brazil. An Bras Dermatol. 2004;79:149-55.
-
352Vachiramon V, Suchonwanit P, Thadanipon K. Melasma in men. J Cosmet Dermatol. 2011;11:151-7.
-
353Scheuer E, Warshaw E. Sunscreen allergy: A review of epidemiology, clinical characteristics, and responsible allergens. Dermatitis : contact, atopic, occupational, drug : official journal of the American Contact Dermatitis Society, North American Contact Dermatitis Group. 2006;17:3-11.
-
354Inamadar AC, Palit A. Sensitive skin: an overview. Indian J Dermatol Venereol Leprol. 2013;79:9-16.
-
355Victor FC, Cohen DE, Soter NA. A 20-year analysis of previous and emerging allergens that elicit photoallergic contact dermatitis. J Am Acad Dermatol. 2010;62:605-10.
-
356Avenel-Audran M, Dutartre H, Goossens A, Jeanmougin M, Comte C, Bernier C, et al. Octocrylene, an emerging photoallergen. Arch Dermatol. 2010;146:753-7.
-
357Metry DW, Hebert AA. Topical therapies and medications in the pediatric patient. Pediatr Clin North Am. 2000;47:867-76.
-
358Kennedy Carney C, Cantrell W, Elewski BE. Rosacea: a review of current topical, systemic and light-based therapies. G Ital Dermatol Venereol. 2009;144:673-88.
-
359Tan JK, Girard C, Krol A, Murray HE, Papp KA, Poulin Y, et al. Randomized placebo-controlled trial of metronidazole 1% cream with sunscreen SPF 15 in treatment of rosacea. J Cutan Med Surg. 2002;6:529-34.
-
360Nichols K, Desai N, Lebwohl MG. Effective sunscreen ingredients and cutaneous irritation in patients with rosacea. Cutis. 1998;61:344-6.
-
361Castanedo-Cazares JP, Torres-Alvarez B, Briones-Estevis S, Moncada B. [Inconsistency in sun protection factor (SPF) index in Mexico. The case of sunscreens for oily skin]. Gac Med Mex. 2005;141:111-4.
-
362Stechschulte SA, Kirsner RS, Federman DG. Sunscreens for non-dermatologists: what you should know when counseling patients. Postgrad Med. 2011;123:160-7.
-
363Teulings HE, Overkamp M, Ceylan E, Nieuweboer-Krobotova L, Bos JD, Nijsten T, et al. Decreased risk of melanoma and nonmelanoma skin cancer in patients with vitiligo: a survey among 1307 patients and their partners. Br J Dermatol. 2013;168:162-71.
-
364Yashiro K, Nakagawa T, Takaiwa T, Inai M. Actinic keratoses arising only on sun-exposed vitiligo skin. Clin Exp Dermatol. 1999;24:199-201.
-
365Hercogova J, Buggiani G, Prignano F, Lotti T. A rational approach to the treatment of vitiligo and other hypomelanoses. Dermatol Clin. 2007;25:383-92, ix.
-
366Nordlund JJ, Halder RM, Grimes P. Management of vitiligo. Dermatol Clin. 1993;11:27-33.
-
367Trueb RM. Is androgenetic alopecia a photoaggravated dermatosis? Dermatology. 2003;207:343-8.
-
368Draelos ZD. Sunscreens and hair photoprotection. Dermatol Clin. 2006;24:81-4.
-
369Signori V. Review of the current understanding of the effect of ultraviolet and visible radiation on hair structure and options for photoprotection. Journal of cosmetic science. 2004;55:95-113.
-
370Maillan P. UV protection of artificially coloured hair using a leave-on formulation. Int J Cosmet Sci. 2002;24:117-22.
-
371Ragi JM, Patel D, Masud A, Rao BK. Nonmelanoma skin cancer of the ear: frequency, patients' knowledge, and photoprotection practices. Dermatol Surg. 2010;36:1232-9.
-
372Bucay VW, Day D. Adjunctive skin care of the brow and periorbital region. Clin Plast Surg. 2013;40:225-36.
-
373Tuchinda C, Srivannaboon S, Lim HW. Photoprotection by window glass, automobile glass, and sunglasses. J Am Acad Dermatol. 2006;54:845-54.
-
374Lagerlund M, Dixon HG, Simpson JA, Spittal M, Taylor HR, Dobbinson SJ. Observed use of sunglasses in public outdoor settings around Melbourne, Australia: 1993 to 2002. Prev Med. 2006;42:291-6.
-
375O'Donoghue MN. Eye cosmetics. Dermatol Clin. 2000;18:633-9.
-
376Lucena EE, Costa DC, da Silveira EJ, de Lima KC. [Prevalence and factors associated with orolabial lesions in beach workers]. Rev Saude Publica. 2012;46:1051-7.
-
377Maier H, Schauberger G, Martincigh BS, Brunnhofer K, Honigsmann H. Ultraviolet protective performance of photoprotective lipsticks: change of spectral transmittance because of ultraviolet exposure. Photodermatol Photoimmunol Photomed. 2005;21:84-92.
-
378Schneider S, Deckardt K, Hellwig J, Kuttler K, Mellert W, Schulte S, et al. Octyl methoxycinnamate: two generation reproduction toxicity in Wistar rats by dietary administration. Food Chem Toxicol. 2005;43:1083-92.
-
379Hackenberg S, Zimmermann FZ, Scherzed A, Friehs G, Froelich K, Ginzkey C, et al. Repetitive exposure to zinc oxide nanoparticles induces dna damage in human nasal mucosa mini organ cultures. Environ Mol Mutag. 2011;52:582-9.
-
380Koeneman BA, Zhang Y, Westerhoff P, Chen Y, Crittenden JC, Capco DG. Toxicity and cellular responses of intestinal cells exposed to titanium dioxide. Cell Biol Toxicol. 2010;26:225-38.
-
381Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266-81.
-
382Holick MF. Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79:362-371.
-
383Grant WB. An estimate of premature cancer mortality in the U.S. due to inadequate doses of solar ultraviolet-B radiation. Cancer. 2002;94:1867-75.
-
384Liu PT, Stenger S, Li H, Wenzel L, Tan BH, Krutzik SR, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006;24:1770-1773.
-
385Wilkinson RJ, Llewelyn M, Toossi Z, Patel P, Pasvol G, Lalvani A, et al. Influence of vitamin D deficiency and vitamin D receptor polymorphisms on tuberculosis among Gujarati Asians in west London: a case-control study. Lancet. 2000;355:618-21.
-
386Aloia JF, Li-Ng M. Re. epidemic influenza and vitamin D. Epidemiol Infect. 2007;135:1095-6.
-
387Ginde AA, Liu MC, Camargo CA Jr. Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004. Arch Intern Med. 2009;169:626-32.
-
388Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US population: 1988-1994 compared with 2000-2004. Am J Clin Nutr. 2008;88:1519-27.
-
389Reichrath J. The challenge resulting from positive and negative effects of sunlight: how much solar UV exposure is appropriate to balance between risks of vitamin D deficiency and skin cancer? Prog Biophys Mol Biol. 2006;92:9-16.
-
390Holick MF. Environmental factors that influence the cutaneous production of vitamin D. Am J Clin Nutr. 1995;61:638S-645S.
-
391Webb AR, DeCosta BR, Holick MF. Sunlight regulates the cutaneous production of vitamin D3 by causing its photodegredation. J Clin Endocrinol Metab. 1989;68:882-7.
-
392Webb AR. Who, what, where and when-influences on cutaneous vitamin D synthesis. Prog Biophys Mol Biol. 2006;92:17-25.
-
393Chiu YE, Havens PL, Siegel DH, Ali O, Wang T, Holland KE, et al. Serum 25-hydroxyvitamin D concentration does not correlate with atopic dermatitis severity. J Am Acad Dermatol. 2013;69:40-6.
-
394Hollis BW. Assessment of vitamin D status and definition of normal circulating range of 25-hydroxyvitamin D. Curr Opin Endocrinol Diabetes Obes. 2008;15:489-94.
-
395Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84:18-28.
-
396Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet. 1998;351:805-6.
-
397Vieth R. Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. Am J Clin Nutr. 1999;69:842-56.
-
398Parrish JA, Jaenicke KF, Anderson RR. Erythema and mel- anogenesis action spectra of normal human skin. Photochem Photobiol. 1982;36:187-91.
-
399Fioletov VE, McArthur LJ, Mathews TW, Marrett L. On the relationship between erythemal and vitamin D action spectrum weighted ultraviolet radiation. J Photochem Photobiol B. 2009;95:9-16.
-
400Gilchrest BA. Sun exposure and vitamin D sufficiency. Am J Clin Nutr. 2008;88:570S-577S.
-
401Thieden E, Philipsen PA, Wulf HC. Ultraviolet radiation exposurepattern in winter compared with summer based on time-stamped personal dosimeter readings. Br J Dermatol. 2006;154:133-8.
-
402Godar DE, Wengraitis SP, Shreffler J, Sliney DH. UV doses of Americans. Photochem Photobiol. 2001;73:621-9.
-
403Webb AR, Kline L, Holick MF. Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab. 1988;67:373-8.
-
404Lu Z, Chen TC, Holick MF. Influence of season and time of day on the synthesis of vitamin D3. In: Holick MF, Kligman A, editors. Proceedings of the Biologic Effects of Light Symposium. Berlin: Walter De Gruyter & Co; 1992. p. 48-52.
-
405de Paula Corrêa M, Ceballos JC. solar ultraviolet radiation measurements in one of the most populous cities of the world: aspects related to skin cancer cases and vitamin D availability. Photochem Photobiol. 2010;86:438-44.
-
406World Health Organization. Global solar UV index. A practical guide. Geneva, Switzerland: World Health Organization; 2002.
-
407Norsang G, Ma L, Dahlback A, Zhuoma C, Tsoja W, Porojnicu A, et al. The vitamin D status among Tibetans. Photochem Photobiol. 2009;85:1028-31.
-
408O'Riordan JL. Rickets in the 17th century. J Bone Miner Res. 2006;21:1506-10.
-
409MacLaughlin JA, Anderson RR, Holick MF. Spectral character of sunlight modulates photosynthesis of previtamin D3 and its photoisomers in human skin. Science. 1982;216:1001-3.
-
410Engelsen O, Brustad M, Aksnes L, Lund E. Daily duration of vitamin D synthesis in human skin with relation to latitude, total ozone, altitude, ground cover, aerosols and cloud thickness. Photochem Photobiol. 2005;81:1287-90.
-
411Manicourt DH, Devogelaer JP. Urban tropospheric ozone increases the prevalence of vitamin D deficiency among Belgian postmenopausal women with outdoor activities during summer. J Clin Endocrinol Metab. 2008;93:3893-9.
-
412Dunnigan MG, Paton JP, Haase S, Mcnicol GW, Gardner MD, Smith CM. Late rickets and osteomalacia in the Pakistani community in Glasgow. Scott Med J. 1962;7:159-67.
-
413Bachrach S, Fisher J, Parks JS. An outbreak of vitamin D deficiency rickets in a susceptible population. Pediatrics. 1979;64:871-7.
-
414Rudolf M, Arulanantham K, Greenstein RM. Unsuspected nutritional rickets. Pediatrics 1980: 66: 72-76.
-
415Hodgkin P, Kay GH, Hine PM, Lumb GA, Stanbury SW. Vitamin-D deficiency in Asians at home and in Britain. Lancet. 1973;2:167-71.
-
416Walker SL, Hawk JLM, Young AR. Acute and chronic effects of ultraviolet radiation on the skin. In: Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editors. Fitz-patrick's dermatology in general medicine. 6th ed. New York, NY: McGraw-Hill, 2003:1275-1282. 589.
-
417Clemens TL, Adams JS, Henderson SL, Holick MF. Increased skin pigment reduces the capacity of skin to synthesize vitamin D3. Lancet. 1982;1:74-6.
-
418Holick MF, MacLaughlin JA, Doppelt SH. Regulation of cutaneous previtamin D3 photosynthesis in man: skin pigment is not an essential regulator. Science. 1981;211:590-3.
-
419Lo CW, Paris PW, Holick MF. Indian and Pakistani immigrants have the same capacity as Caucasians to produce vitamin D in response to ultraviolet irradiation. Am J Clin Nutr. 1986;44:683-5.
-
420MacLaughlin J, Holick MF. Aging decreases the capacity of the skin to produce vitamin D3. J Clin Invest. 1985;76:1536-8.
-
421Weisman Y, Schen RJ, Eisenberg Z, Edelstein S, Harell A. Inadequate status and impaired metabolism of vitamin D in the elderly. Isr J Med Sci. 1981;17:19-21.
-
422Lester E, Skinner RK, Wills MR. Season variation in serum- 25-hydroxyvitamin-D in the elderly in Britain. Lancet. 1977;1:979-80.
-
423Dattani JT, Exton-Smith AN, Stephen JM. Vitamin D status of the elderly in relation to age and exposure to sunlight. Hum Nutr Clin Nutr. 1984;38:131-7.
-
424Shuster S, Black MM, McVitie E. The influence of age and sex on skin thickness, skin collagen and density. Br J Dermatol. 1975;93:639-43.
-
425Need AG, Morris HA, Horowitz M, Nordin C. Effects of skin thickness, age, body fat, and sunlight on serum 25-hydroxyvitamin D. Am J Clin Nutr. 1993;58:882-5.
-
426Webb AR, Pilbeam C, Hanafin N, Holick MF. An evaluation of the relative contributions of exposure to sunlight and of diet to the circulating concentrations of 25hydroxyvitamin D in an elderly nursing home population in Boston. Am J Clin Nutr. 1990 Jun;51:1075-81.
-
427Paterson CR, Moody JP, Pennington CR. Skin content of 7-dehydrocholesterol in patients with malabsorption. Nutrition. 1997;13:771-3.
-
428Dobs AS, Levine MA, Margolis S. Effects of pravastatin, a new HMG-CoA reductase inhibitor, on vitamin D synthesis in man. Metabolism. 1991;40:524-8.
-
429Rejnmark L, Vestergaard P, Heickendorff L, Mosekilde L. Simvastatin does not affect vitamin D status, but low vitamin D levels are associated with dyslipidemia: results from a randomized, controlled trial. Int J Endocrinol. 2010;2010:957174.
-
430Montagnani M, Loré F, Di Cairano G, Gonnelli S, Ciuoli C, Montagnani A, et al. Effects of pravastatin treatment on vitamin D metabolites. Clin Ther 1994;16:824-829.
-
431Pérez-Castrillón JL, Vega G, Abad L, Sanz A, Chaves J, Hernandez G, et al. Effects of atorvastatin on vitamin D levels in patients with acute ischemic heart disease. Am J Cardiol. 2007;99:903-5.
-
432Aloia JF, Li-Ng M, Pollack S. Statins and vitamin D. Am J Cardiol. 2007;100:1329.
-
433Klein GL, Chen TC, Holick MF, Langman CB, Price H, Celis MM. Synthesis of vitamin D in skin after burns. Lancet. 2004;363:291-2.
-
434Klein GL, Herndon DN, Goodman WG, Langman CB, Phillips WA, Dickson IR, et al. Histomorphometric and biochemical characterization of bone following acute severe burns in children. Bone. 1995;17:455-60.
-
435Klein GL, Langman CB, Herndon DN. Vitamin D depletion following burn injury in children: a possible factor in post- burn osteopenia. J Trauma. 2002;52:346-50.
-
436Preece MA, Tomlinson S, Ribot CA, Pietrek J, Korn HT, Davies DM, et al. Studies of vitamin D deficiency in man. Q J Med. 1975;44:575-89.
-
437Dlugos DJ, Perrota PL, Horn WG. Effects of the submarine environment on renalstone risk factors and vitamin D metabolism. Undersea Hyperb Med. 1995;22:145-52
-
438Cusack C, Danby C, Fallon JC, Ho WL, Murray B, Brady J, et al. Photoprotective behaviour and sunscreen use: impact on vitamin D levels in cutaneous lupus erythematosus. Photodermatol Photoimmunol Photomed. 2008;24:260-7.
-
439Kamen DL, Cooper GS, Bouali H, Shaftman SR, Hollis BW, Gilkeson GS. Vitamin D deficiency in systemic lupus erythematosus. Autoimmun Rev. 2006;5:114-7.
-
440Walder BK, Robertson MR, Jeremy D. Skin cancer and immunosuppression. Lancet. 1971;2:1282-3.
-
441Querings K, Girndt M, Geisel J, Georg T, Tilgen W, Reichrath J. 25-Hydroxyvitamin D-deficiency in renal transplant recipients. J Clin Endocrinol Metab. 2006;91:526-9.
-
442Segal E, Baruch Y, Kramsky R, Raz B, Ish-Shalom S. Vitamin D deficiency in liver transplant patients in Israel. Transplant Proc. 2001;33:2955-6.
-
443Massenkeil G, Fiene C, Rosen O, Michael R, Reisinger W, Arnold R. Loss of bone mass and vitamin D deficiency after hematopoietic stem cell transplantation: standard prophylactic measures fail to prevent osteoporosis. Leukemia. 2001;15:1701-5.
-
444Querings K, Reichrath J. A plea for the analysis of vitamin-D levels in patients under photoprotection, including patients with xeroderma pigmentosum (XP) and basal cell nevus syndrome (BCNS). Cancer Causes Control. 2004;15:219.
-
445Sollitto RB, Kraemer KH, DiGiovanna JJ. Normal vitamin D levels can be maintained despite rigorous photoprotection: six years' experience with xeroderma pigmentosum. J Am Acad Dermatol. 1997;37:942-7.
-
446Glass D, Lens M, Swaminathan R, Spector TD, Bataille V. Pigmentation and vitamin D metabolism in Caucasians: low vitamin D serum levels in fair skin types in the UK. PLoS One. 2009;4:e6477.
-
447Malvy DJ, Guinot C, Preziosi P, Galan P, Chapuy MC, Maamer M, et al. Relationship between vitamin D status and skin phototype in general adult population. Photochem Photobiol. 2000;71:466-9.
-
448Binkley N, Novotny R, Krueger D, Kawahara T, Daida YG, Lensmeyer G, et al. Low vitamin D status despite abundant sun exposure. J Clin Endocrinol Metab. 2007;92:2130-5.
-
449Aloai JF. African Americans, 25-hydroxyvitamin D and osteoporosis: a paradox. Am J Clin Nutr. 2008;88:545S-550S.
-
450Morison WL. Photoprotection by clothing. Dermatol Ther. 2003;16:16-22.
-
451Sayre RM, Huges SNG. Sun protective apparel: advancements in sun protection. Skin Cancer J. 1993:8:41-7.
-
452Gambichler T, Hatch KL, Avermaete A, Altmeyer P, Hoffmann K. Influence of wetness on the ultraviolet protection factor (UPF) of textiles: in vitro and in vivo measurements. Photodermatol Photoimmunol Photomed. 2002;18:29-35.
-
453Matsuoka LY, Wortsman J, Dannenberg MJ, Hollis BW, Lu Z, Holick MF. Clothing prevents ultraviolet-B radiation- dependent photosynthesis of vitamin D3. J Clin Endocrinol Metab. 1992;75:1099-103.
-
454Salih FM. Effect of clothing varieties on solar photosynthesis of previtamin D3: an in vitro study. Photodermatol Photoimmunol Photomed. 2004;20:53-8.
-
455Parisi AV, Wilson CA.Pre-vitamin D3 effective ultraviolet transmission through clothing during simulated wear. Photodermatol Photoimmunol Photomed. 2005;21:303-10.
-
456Sedrani SH, Elidrissy AW, El Arabi KM. Sunlight and vitamin D status in normal Saudi subjects. Am J Clin Nutr. 1983;38:129-32.
-
457Fonseca V, Tongia R, el-Hazmi M, Abu-Aisha H. Exposure to sunlight and vitamin D deficiency in Saudi Arabian women. Postgrad Med J. 1984;60:589-91.
-
458MacNeal RJ, Dinulos JG. Update on sun protection and tanning in children. Curr Opin Pediatr. 2007;19:425-9.
-
459Thompson SC, Jolley D, Marks R. Reduction of solar keratoses by regular sunscreen use. N Engl J Med. 1993;329:1147-51.
-
460Naylor MF, Boyd A, Smith DW, Cameron GS, Hubbard D, Neldner KH. High sun protection factor sunscreens in the suppression of actinic neoplasia. Arch Dermatol. 1995;131:170-5.
-
461Darlington S, Williams G, Neale R, Frost C, Green A. A randomized controlled trial to assess sunscreen application and betacarotene supplementation in the prevention of solar keratoses. Arch Dermatol. 2003;139:451-5.
-
462Matsuoka LY, Ide L, Wortsman J, MacLaughlin JA, Holick MF. Sunscreens suppress cutaneous vitamin D3 synthesis. J Clin Endocrinol Metab. 1987;64:1165-8.
-
463Matsuoka LY, Wortsman J, Hanifan N, Holick MF. Chronic sunscreen use decreases circulating concentrations of 25-hydroxyvitamin D. A preliminary study. Arch Dermatol. 1988;124:1802-4.
-
464Norval M, Wulf HC. Does chronic sunscreen use reduce vitamin D to insufficient levels? Br J Dermatol. 2009;161:732-6.
-
465Matsuoka LY, Wortsman J, Hollis BW. Use of topical sunscreen for the evaluation of regional synthesis of vitamin D3. J Am Acad Dermatol. 1990;22:772-5.
-
466Holick MF, Matsuoka LY, Wortsman J. Regular use of sun- screen on vitamin D levels. Arch Dermatol. 1995;131:1337-9.
-
467Marks R, Foley PA, Jolley D, Knight KR, Harrison J, Thompson SC. The effect of regular sunscreen use on vitamin D levels in an Australian population. Arch Dermatol. 1995;131:415-21.
-
468Chesney RW, Rosen JF, Hamstra AJ, Smith C, Mahaffey K, DeLuca HF. Absence of seasonal variation in serum concentrations of 1,25-dihydroxyvitamin D despite a rise in 25-hydroxyvitamin D in summer. J Clin Endocrinol Metab. 1981;53:139-42.
-
469Tjellesen L, Nielsen B, Christiansen C. Seasonal fluctuations in serum concentrations of vitamin D metabolites. Br Med J (Clin Res Ed). 1982;284:196-7.
-
470Maia M, Maeda S, Marçon CR. Correlation between photoprotection and concentrations of 25-hydroxyvitamin D and parathyroid hormone. An Bras Dermatol. 2007;82:233-7.
-
471Kligman EW, Watkins A, Johnson K, Kronland R. The impact of lifestyle factors on serum 25-hydroxy vitamin D levels in older adults: a preliminary study. Fam Pract Res J. 1989;9:11-9.
-
472Kimlin M, Harrison S, Nowak M, Moore M, Brodie A, Lang C. Does a high UV environment ensure adequate vitamin D status? J Photochem Photobiol B. 2007 Dec 14;89:139-47.
-
473Harris SS, Dawson-Hughes B. Reduced sun exposure does not explain the inverse association of 25-hydroxyvitamin D with percent body fat in older adults. J Clin Endocrinol Metab. 2007;92:3155-7.
-
474Thieden E, Philipsen PA, Sandby-Møller J, Wulf HC. Sunscreen use related to UV exposure, age, sex, and occupation based on personal dosimeter readings and sunexposure behavior diaries. Arch Dermatol. 2005;141:967-73.
-
475Bech-Thomsen N, Wulf HC. Sunbathers' application of sunscreen is probably inadequate to obtain the sun protection factor assigned to the preparation. Photodermatol Photoimmunol Photomed. 1992-1993;9:242-4.
-
476Stender IM, Lock-Andersen J, Wulf HC. Sun-protection behavior and selfassessed burning tendency among sun- bathers. Photodermatol Photoimmunol Photomed. 1996;12:162-5.
-
477Farrerons J, Barnadas M, Rodríguez J, Renau A, Yoldi B, López-Navidad A,et al. Clinically pre- scribed sunscreen (sun protection factor 15) does not decrease serum vitamin D concentration sufficiently either to induce changes in parathyroid function or in metabolic markers. Br J Dermatol. 1998;139:422-7.
-
478Farrerons J, Barnadas M, López-Navidad A, Renau A, Rodríguez J, Yoldi B, et al. Sun- screen and risk of osteoporosis in the elderly: a two-year follow-up. Dermatology. 2001;202:27-30.
-
479Ross AC, Manson JE, Abrams SA, Aloia JF, Brannon PM, Clinton SK, et al. The 2011 Report on Dietary Reference Intakes for Calcium and Vitamin D from the Institute of Medicine: What Clinicians Need to Know. J Clin Endocrinol Metab. 2011;96:53-8.
-
480Binkley N, Ramamurthy R, Krueger D. Low Vitamin D Status: Definition, Prevalence, Consequences, and Correction. Endocrinol Metab Clin North Am. 2010;39:287-301.
Publication Dates
-
Publication in this collection
Nov-Dec 2014
History
-
Received
21 Aug 2014 -
Accepted
28 Oct 2014