Abstract
Background and objectives
While an increasing number of people who snore are seeking medical consultations, the clinical characteristics of snorers are rarely reported. The aim of this study is to characterize the clinical and polysomnographic features in a population of snorers.
Methods
A total of 490 subjects were examined retrospectively. The clinical history, Epworth Sleepiness Scale (ESS) scores, physical examination, and full-night polysomnography (PSG) data were obtained for all the subjects. The correlations between the neck circumference, waist circumference, ESS scores, body mass index (BMI), and apnea-hypopnea index (AHI) of obstructive sleep apnea (OSA) patients were explored. The gender and age differences in OSA patients were analyzed.
Results
OSA was diagnosed in 84.7% of the sample, with 21.2% of the patients having a mild form, 15.4% having a moderate form, and 63.4% having a severe form of OSA. The ESS scores, neck circumference, waist circumference, and BMI were positively correlated with AHI in OSA patients. The ESS scores and BMI were negatively correlated with nadir oxygen saturation (SaO2). A greater number of men than women exhibited moderate to severe forms of the disease. OSA affects the work of males more commonly compared with females. Nocturia was a more common complaint in elderly OSA patients. Heart diseases coexisted more frequently with OSA in elderly patients.
Conclusions
In a population of snorers, OSA is the most common condition identified. The ESS scores and BMI were well correlated with the severity of the disease. Men had a more severe form of OSA than women. Nocturia frequently occurred in elderly OSA patients, as did the coexistence of heart disease.
摘要
目的
探讨因鼾症就诊者临床特点与多导睡眠监测(PSG)结果及其相关性, 加深对鼾症和阻塞性睡眠呼吸暂停综合征(OSA)的理解。
创新点
较为全面地评估了因鼾症就诊者的临床特点和多导睡眠监测结果, 比较了不同严重程度的OSA患者的临床特征, 同时分析了性别和年龄差异对OSA患者临床特点和PSG结果的影响, 有助于进一步全面深刻地理解鼾症和OSA的流行病学和临床特征。
方法
对因夜间睡眠时打鼾就诊的490名患者进行病史采集、 Epworth嗜睡评分(ESS)、 体格检查(BMI)和整夜多导睡眠监测(PSG)。 分析OSA患者临床症状、 BMI、 主观嗜睡与呼吸暂停低通气指数(AHI)、 夜间低氧等的相关关系, 比较不同性别、 不同年龄组OSA患者临床症状和病情严重程度的差异。
结论
因鼾症就诊者中OSA患者比例最高, 且多数为中重度OSA。 OSA患者ESS评分、 BMI与病情严重程度有较好的相关性。 男性OSA患者病情较女性重。 老年OSA患者易出现夜尿增多, 合并心脏病比例增高。
Similar content being viewed by others
1 Introduction
The number of people seeking medical consultations for snoring is increasing. Obstructive sleep apnea (OSA) is the most common sleep-disordered breathing. In view of the obesity pandemic, the incidence of OSA is likely to rise (Jordan et al., 2014). The prevalence of symptomatic OSA in the general population is 2%–4%, and OSA increases with age (de Backer, 2013). OSA is associated with a number of adverse outcomes, including sleep disruption, cognitive dysfunction, traffic accidents, and increased risk of cardiovascular diseases. OSA has become a global health problem, and it reduces the quality of life and increases mortality.
The objectives of this study are to examine the clinical characteristics and polysomnographic outcomes in a population of snorers. The OSA patients were further studied for factors that might be related to the severity of the disease. The gender and age differences in OSA were assessed as well.
2 Materials and methods
2.1 Subjects
A total of 490 snorers, who were admitted to the hospital and underwent a full-night polysomnography (PSG) during January 2013 to April 2014, were enrolled as subjects in this study. None of the subjects were referred because of a previous diagnosis and treatment for OSA, and the PSG tests of all the subjects were valid.
The access to patient records was approved by the local ethics committee, and patient confidentiality was maintained.
2.2 Clinical assessment
The anthropometric data including gender, age, height, weight, body mass index (BMI), neck circumference, and waist circumference and the detailed clinical data including the symptoms, comorbidities, Epworth Sleepiness Scale (ESS) scores, and physical examination records focusing on the maxillofacial, oropharynx, and neck regions were recorded. Excessive daytime sleepiness was assessed by an ESS score of >10.
2.3 Sleep study
The full-night PSG recordings were reviewed independently by two sleep specialists. A polysomnographic system (Alice 5, Respironics, Philips, Pittsburgh, Pennsylvania, USA) was used to perform the PSG tests. The diagnosis of OSA was confirmed following the criteria proposed by the adult OSA task force of the American Academy of Sleep Medicine(Epstein et al., 2009).
2.4 Statistical analyses
The characteristics of the subjects were summarized as the mean±standard deviation (SD)for the continuous variables and as counts and percentages for the categorical variables. Pearson’s or Spearman’s correlation analysis was used to explore the correlations between the neck circumference, waist circumference, ESS scores, BMI and AHI in the OSA patients. An independent t-test or one-way analysis of variance (ANOVA) was used for the comparison between the groups of continuous variables, and a Chi-squared test or Fisher’s exact test was used for the categorical variables. A binary logistic regression analysis was used to compare the clinical data of the gender and age groups. In all the cases, P<0.05 was considered statistically significant. All the statistical analyses were performed using SPSS, Version 20.0 (SPSS, Inc., Chicago, IL, USA).
3 Results
3.1 General sample
A total of 409 males and 81 females were analyzed with an age of (45.27±11.6) years; 460 patients were young and middle-aged (<65 years), and 30 patients were elderly (<65 years). OSA was identified in 415 (84.7%) patients, simple snoring in 65 (13.3%), mixed sleep apnea (MSA) in 6 (1.2%), and central sleep apnea (CSA) in 4 (0.8%).
In the 409 male patients, OSA was identified in 362 patients (88.5%), simple snoring in 39 (9.5%), MSA in 4 (1.0%), and CSA in 4 (1.0%). In the 81 female patients, OSA was identified in 53 (65.4%) patients, simple snoring in 26 (32.1%), MSA in 2 (2.5%), and CSA in 0 (0%). Gender (84.7%) differences existed for the prevalence of various forms of sleep-disordered breathing (Fisher’s exact test, P<0.001).
In the 460 young and middle-aged patients, OSA was identified in 390 (84.8%) patients, simple snoring in 62 (13.5%), MSA in 4 (0.9%), and CSA in 4 (0.9%). In the 30 elderly patients, OSA was identified in 25 (83.3%) patients, simple snoring in 3 (10.0%), MSA in 2 (6.7%), and CSA in 0 (0%). The prevalence of various forms of sleep-disordered breathing was similar in the age groups.
3.2 Characteristics of OSA patients
Of the 415 OSA patients, 362 patients were male, 53 were female, 390 were young and middle-aged, and 25 were elderly.
In addition to snoring, the majority of the OSA patients had other symptoms; 171 (41.2%) patients complained of gasping/choking at night, 66 (15.9%) of morning headaches, 265 (63.9%) of dry mouth, 242 (58.3%) of daytime sleepiness, 121 (29.2%) of nocturia, 252 (60.7%) of memory loss, and 174 (41.9%) of irritability. OSA influenced the quality of life in 168 patients (40.5%), affected the patient’s work in 121 (29.2%), and had an effect on traffic safety in 62 (14.9%) patients. The mean ESS score was 7.88±4.66, and 130 (31.3%) OSA patients had ESS scores of >10.
Among the OSA patients, 154 (37.1%) had comorbidity with hypertension, 54 (13.0%) with diabetes mellitus, 45 (10.8%) with heart disease, 7 (1.7%)with cerebrovascular disease, 26 (6.3%) with reflux esophagitis, 15 (3.6%) with thyroid diseases, 159 (38.3%) with rhinitis, 180 (43.4%) with pharyngolaryngitis,and 14 (3.4%) patients had a history of upper airway surgery.
A number of OSA patients had signs of upper airway narrowing as follows: 1 (0.2%) with retrognathia, 54 (13.0%) with tonsillar hypertrophy,and 58 (14.0%) with pharyngeal cavity stenosis. The neck and waist circumferences were (38.46±3.83) and (97.8±9.5) cm, respectively.
According to the AHI, mild was identified in 88 patients (21.2%), moderate in 64 (15.4%), and severe in 263 (63.4%). The mean AHI, respiratory disturbance index (RDI), and respiratory effort related arousal (RERA) of the OSA patients were (42.28±25.00), (42.88±25.19), and (0.59±1.53) h−1. The mean nadir SaO2, average SaO2, oxygen desaturation index (ODI), and percentage of recording time with SaO2 of <90% (T90) of the OSA patients were (70.56±14.79)%, (93.01±3.62)%, (43.62±26.17) h−1, and (23.43±26.72)%, respectively. A total of 58 (14.0%) patients had their nadir SaO2 between 85% and 90%, 74 (17.8%) between 80% and 85%, and 280(67.5%) below 80%.
The correlation analysis showed that neck circumference was positively correlated with the AHI (r=0.341, P<0.001) and RDI (r=0.341, P<0.001); the waist circumference was positively correlated with the AHI (r=0.457, P<0.001) and RDI (r=0.444, P< 0.001); the BMI was positively correlated with the AHI (r=0.389, P<0.001) and RDI (r=0.387, P< 0.001), whereas BMI was negatively correlated with the nadir SaO2(r=−0.392, P<0.001); the ESS scores was positively correlated with the AHI (r=0.288, P< 0.001) and RDI (r=0.292, P<0.001), whereas ESS was negatively correlated with the nadir SaO2(r=−0.258, P<0.001).
3.3 Phenotypes of different severities
The anthropometric data of OSA patients by different severities are shown in Table1. Symptomatic, clinical, and physical examination data by different severities are shown in Tables 2 and 3. The symptoms of dry mouth (52.3%, 54.7%, and 70.0%, respectively;P=0.003) and daytime sleepiness (46.6%, 51.6%, and 63.9%, respectively;P=0.009) were more frequent in the severe OSA patients.



The severe OSA patients had higher ESS scores (6.13±4.27, 6.75±3.46, and 8.75±4.82, respectively; P<0.001) than the mild and moderate OSA patients. The qualities of life (33.0%, 28.1%, and 46.0%, respectively; P=0.009) and work (25.0%, 18.8%, and 33.1%, respectively; P=0.049) were more frequently influenced in the severe OSA patients. Reflux esophagitis (2.3%, 14.1%, and 5.7%, respectively; P=0.01) was more frequent in the moderate and severe OSA patients.
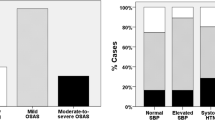
3.4 Gender differences in OSA
The anthropometric and polysomnographic data of the OSA patients by gender are shown in Tables 4 and 5. In the 362 male patients, mild was identified in 67 patients (18.5%), moderate in 53 (14.6%), and severe in 242 (66.9%), according to their AHI. In the 53 female patients, mild was identified in 21 patients (39.6%), moderate in 11 (20.8%), and severe in 21 (39.6%). Moderate and severe OSA were more frequent in males than in females ( χ2=16.249, P<0.001). In the 362 male patients, 49 (13.5%) patients had anadir SaO2 between 85% and 90%, 59 (16.3%) between 80% and 85%, and 252 (69.6%) below 80%. In 53 female patients, 9 (17.0%) patients had a nadir SaO2 between 85% and 90%, 15 (28.3%) between 80% and 85%, and 28 (52.8%) below 80%. A difference existed in the distribution of the nadir SaO2 between the genders (Fisher’s exact test, P=0.041).


The symptomatic, clinical and physical examination data by gender are shown in Tables 6 and 7. Males were affected in their work by OSA more frequently than were females (P=0.045). Thyroid disease was more frequent in female OSA patients (P=0.003).


3.5 Age differences in OSA
The anthropometric and polysomnographic data of the OSA patients by age are shown in Tables 8 and 9. The BMI, neck and waist circumferences were similar in the age groups. In 390 young and middle-aged patients, mild OSA was identified in 82 patients (21.0%), moderate in 60 (15.4%), and severe in 248 (63.6%). In 25 elderly patients, mild OSA was identified in 6 patients (24.0%), moderate in 4 patients (16.0%),and severe in 15 patients (60.0%). In 390 young and middle-aged patients, 54 patients (13.8%) had a nadir SaO2 between 85% and 90%, 66 (16.9%) between 80% and 85%, and 267 (68.5%) below 80%. In 25 elderly patients, 4 patients (16.0%) had a nadir SaO2 between 85% and 90%, 8 (32.0%) between 80% and 85%, and 13 (52.0%) below 80%.


The symptomatic, clinical, and physical examination data by age are shown in Tables 10 and 11. More elderly OSA patients complained of nocturia (P=0.004). Heart disease was more frequent in the elderly OSA patients (P=0.014). Pharyngolaryngitis presents itself more frequently in young and middle-aged OSA patients with a P value that just reached the criteria of statistical significance (P=0.05).


4 Discussion
This report is an epidemiological study examining a population of snorers. Our study found that in this population, OSA is the most common condition identified, followed by primary snoring, CSA, and MSA, which are relatively rare.We found that the prevalence of OSA in male subjects is higher, which is in accordance with previous epidemiological studies (Lurie, 2011a). When the subjects were grouped by age, the prevalences of OSA and other types of sleep-disordered breathing conditions were similar in both groups. Previous studies suggested that the prevalence of OSA increased with age (Peppard et al., 2013; Jennum and Riha, 2009), because individuals from the general population were enrolled as subjects in those studies. Our study suggests the prevalence of OSA in male snorers is as high as that in the elderly.
In addition to snoring at night and excessive daytime sleepiness, dry mouth, daytime sleepiness, memory loss, gasping/choking at night, and irritability were common symptoms in OSA patients. Dry mouth, daytime sleepiness, the effect on work, and a reduced quality of life were more frequently reported by severe OSA patients. We found that hypertension was a common comorbidity in OSA patients. OSA contributes to or exacerbates cardiovascular disease (Monahan and Redline, 2011), and hypertension is the most common result (Lurie, 2011b). Through a detailed investigation into the patients’ previous medical history, we found that some OSA patients had refractory hypertension, the pathogenesis of which might be related to the chronic intermittent hypoxia experienced by the patients at night (Parati et al., 2014). Therefore,OSA might be a novel target for cardiovascular risk reduction (Monahan and Redline, 2011). A systematic review and meta-analysis suggested that continuous positive airway pressure lowered blood pressure in OSA patients (Montesi et al., 2012). Patients with OSA commonly have comorbid nocturnal gastroesophageal reflux disease (GERD) (Hesselbacher et al., 2014). In our study, we found that reflux esophagitis was more common in moderate and severe OSA patients, and the prevalence of reflux esophagitis did not differ between the genders and age groups. Basoglu et al. (2014) showed that obesity and sleepiness might be related to the prevalence of GERD in OSA patients, which may help explain the results of our study. Their study showed that the severity of OSA did not influence GERD prevalence, whereas female gender might be related to GERD prevalence. They also evaluated GERD comprehensively, whereas, in our study, we focused on reflux esophagitis, a relatively severe form of GERD. In this study, we found a high incidence of rhinitis in the OSA patients. The increased airway resistance in rhinitis patients might have a role in the pathogenesis of OSA. Parikh et al.(2014) found that in patients with OSA and rhinitis, the ESS score is associated with the symptom severity of rhinitis. Additionally, we found that pharyngolaryngitis was a common comorbidity in OSA patients. A bidirectional relationship might exist between OSA and pharyngolaryngitis. Pharyngolaryngitis might increase upper airway resistance. Conversely,repeated collapse and return of the upper airway in OSA patients might induce pharyngolaryngitis. Local anatomical abnormalities, such as tonsillar hypertrophy, pharyngeal cavity stenosis, and retrognathia, could cause mechanical obstruction of the upper airway (Azagra-Caleroet al., 2012). In OSA patients with anatomical abnormalities of the upper airway, three-dimensional reconstruction of the upper airway by multi-slice spiral computed tomography is proposed. If necessary, a careful surgical assessment is performed. In our study, we found a relatively low incidence of anatomical abnormalities in the OSA patients. Consistent with our findings, Azagra-Calero et al. (2012) suggested that the main cause of OSA is a reduction of the expansion forces of the pharyngeal dilator muscles, as in situations of genioglossal muscle dysfunction, and between the inspiratory activity of the muscle and the respiratory effort, which play an important role in the progression of the disease.
PSG monitoring is a labor-intensive and expensive test conducted in a limited number of facilities, which have many patients waiting for appointments. In our study, the correlation analysis revealed that the neck circumference, waist circumference, and BMI were positively correlated with the AHI/RDI and that the BMI was negatively correlated with the nadir SaO2. The analysis of the patients with different disease severity showed that severe patients had a greater BMI as well as larger neck and waist circumferences. Chang et al.(2014) showed that the neck circumference could be a useful clinical predictor of OSA in Chinese patients. Neck circumference, waist circumference, and BMI might be indicators of the severity of OSA and could be used to screen for OSA in the general population. ESS is widely used in the evaluation of patients with sleep-disordered breathing because of its simplicity and convenience (Damiani et al., 2013). We found that ESS scores were positively correlated with AHI/RDI, whereas they were negatively correlated with the nadir SaO2 and were significantly increased in severe OSA patients; therefore, the ESS score might be another indicator of severity. For the patients with a high possibility of severe OSA, full-night PSG should be conducted as early as possible.
The proportion of OSA patients with an AHI of >15 (moderate to severe) or with a nadir SaO2 of <80% was higher in males. The AHI/ADI and ODI were higher in male OSA patients. Consistent with the study of Sforza et al.(2011), our study suggested that male OSA patients had more severe OSA. Consistent with our findings, Banhiran et al. (2014) showed that male gender was a good predictor for moderate to severe OSA. We found that daily work was more frequently affected by OSA in males. No specific quantitative indicators were adopted in this study. Moreover, the types of work might be affected by gender, which could influence the results. A higher incidence of thyroid disease, predominantly Graves’ disease and hypothyroidism, was found in the female OSA patients. It is unclear whether there is an intrinsic relationship between the pathogenesis of OSA and Graves’ disease. A higher incidence of Graves’ disease in females might partly explain the results of our study. There might be an interaction between hypothyroidism and OSA. Hypothyroidism could cause OSA, which might be related to structural change of the upper airway and myopathy associated with hypothyroidism. OSA could cause hypothyroidism through its complicated influence on endocrine and metabolic functions. Ozcan et al. (2014) showed that the incidence of hypothyroidism in OSA patients was 12.77%.
We found that the severity of OSA was similar between the elderly and non-elderly OSA patients. Nocturia was more common in the elderly. The result was consistent with the study of Raheem et al. (2014) showing that age is a predictor of nocturia in OSA patients. Romero et al. (2010) showed that nocturia appeared comparable to snoring as a screening tool for OSA. The mechanism is unknown, and increased secretion of atrial natriuretic peptide (ANP) might be involved (Raheem et al., 2014). ANP acts in the kidneys to increase the excretion of sodium and thus the drainage of water. The workload increases in OSA patients. Physiologically, the compensatory capacity of the kidneys decreases with the increase of age. Therefore, renal function tends to be impaired in elderly OSA patients. We found that the incidence of heart disease was higher in elderly OSA patients. Many cardiovascular diseases, such as hypertension, coronary heart disease, heart failure, and arrhythmia, could be caused or aggravated by OSA, and the coexistence of OSA and cardiovascular diseases increases the mortality rate (Kasai et al., 2012). Oxidative stress, inflammation, and endothelial dysfunction induced by chronic intermittent hypoxia, a main pathophysiological change in OSA, are important mechanisms underlying these lesions (Kasai et al., 2012; Prabhakar and Semenza, 2012; Badran et al., 2014). Therefore, for OSA patients with cardiovascular diseases, continuous positive airway pressure (CPAP) therapy should be initiated as early as possible. The incidence of pharyngolaryngitis was higher in young and middle-aged OSA patients, although the cause is unknown. We suggest that OSA patients should receive a careful diagnosis and treatment for pharyngolaryngitis.
In this study, we found that OSA is the most common sleep-disordered breathing condition among snorers. Neck circumference, waist circumference, and BMI are good candidates as indicators to assess the severity of disease. Male OSA patients had more severe conditions, and their work was influenced more frequently. The severity of OSA was similar in young, middle-aged, and elderly OSA patients. The incidences of nocturia and heart disease were higher in elderly OSA patients. The lack of quantitative indicators in the evaluation of some clinical features and a detailed classification of some comorbidities is the limitation of our study, which should be addressed in a future study.
Compliance with ethics guidelines
Chuan SHAO, Jing-bo JIANG, Hong-cheng WU,Shi-bo WU,Bi-yun YU, and Yao-dong TANG declare that they have no conflict of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study. Additional informed consent was obtained from all patients for whom identifying information is included in this article.
References
Azagra-Calero, E., Espinar-Escalona, E., Barrera-Mora, J.M., et al., 2012. Obstructive sleep apnea syndrome (OSAS). Review of the literature. Med. Oral Patol. Oral Cir. Bucal, 17(6):e925–e929. [doi:10.4317/medoral.17706]
Badran, M., Ayas, N., Laher, I., 2014. Insights into obstructive sleep apnea research. Sleep Med., 15(5):485–495. [doi:10.1016/j.sleep.2014.01.009]
Banhiran, W., Junlapan, A., Assanasen, P., et al., 2014. Physical predictors for moderate to severe obstructive sleep apnea in snoring patients. Sleep Breath., 18(1):151–158. [doi:10.1007/s11325-013-0863-y]
Basoglu, O.K., Vardar, R., Tasbakan, M.S., et al., 2014. Obstructive sleep apnea syndrome and gastroesophageal reflux disease: the importance of obesity and gender. Sleep Breath., in press. [doi:10.1007/s11325-014-1051-4]
Chang, E.T., Yang, M.C., Wang, H.M., et al., 2014. Snoring in a sitting position and neck circumference are predictors of sleep apnea in Chinese patients. Sleep Breath., 18(1):133–136. [doi:10.1007/s11325-013-0860-1]
Damiani, M.F., Quaranta, V.N., Falcone, V.A., et al., 2013. The Epworth Sleepiness Scale: conventional self vs physician administration. Chest, 143(6):1569–1575. [doi:10.1378/chest.12-2174]
de Backer, W., 2013. Obstructive sleep apnea/hypopnea syndrome. Panminerva Med., 55(2):191–195.
Epstein, L.J., Kristo, D., Strollo, P.J.Jr., et al., 2009. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J. Clin. Sleep Med., 5(3):263–276.
Hesselbacher, S., Subramanian, S., Rao, S., et al., 2014. Selfreported sleep bruxism and nocturnal gastroesophageal reflux disease in patients with obstructive sleep apnea: relationship to gender and ethnicity. Open Respir. Med. J., 22(8):34–40. [doi:10.2174/1874306401408010034]
Jennum, P., Riha, R.L., 2009. Epidemiology of sleep apnoea/hypopnoea syndrome and sleep-disordered breathing. Eur. Respir. J., 33(4):907–914. [doi:10.1183/09031936.00180108]
Jordan, A.S., McSharry, D.G., Malhotra, A., 2014. Adult obstructive sleep apnoea. Lancet, 383(9918):736–747. [doi:10.1016/S0140-6736(13)60734-5]
Kasai, T., Floras, J.S., Bradley, T.D., 2012. Sleep apnea and cardiovascular disease: a bidirectional relationship. Circulation, 126(12):1495–1510. [doi:10.1161/CIRCULATIONAHA.111.070813]
Lurie, A., 2011a. Obstructive sleep apnea in adults: epidemiology, clinical presentation, and treatment options. In: Borer, J.S. (Ed.), Advances in Cardiology. Karger, Basel, p.1–42. [doi:10.1159/000327660]
Lurie, A., 2011b. Obstructive sleep apnea in adults: cardiovascular disorders associated with obstructive sleep apnea. In: Borer, J.S. (Ed.), Advances in Cardiology. Karger, Basel, p.197–266. [doi:10.1159/000325110]
Monahan, K., Redline, S., 2011. Role of obstructive sleep apnea in cardiovascular disease. Curr. Opin. Cardiol., 26(6):541–547. [doi:10.1097/HCO.0b013e32834b806a]
Montesi, S.B., Edwards, B.A., Malhotra, A., et al., 2012. The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J. Clin. Sleep Med., 8(5): 587–596. [doi:10.5664/jcsm.2170]
Ozcan, K.M., Selcuk, A., Ozcan, I., et al., 2014. Incidence of hypothyroidism and its correlation with polysomnography findings in obstructive sleep apnea. Eur. Arch. Otorhinolaryngol., 271(11):2937–2941. [doi:10.1007/s00405-014-2962-1]
Parati, G., Ochoa, J.E., Bilo, G., et al., 2014. Obstructive sleep apnea syndrome as a cause of resistant hypertension. Hypertens. Res., 37(7):601–613. [doi:10.1038/hr.2014.80]
Parikh, N.G., Junaid, I., Sheinkopf, L., et al., 2014. Clinical control in the dual diagnosis of obstructive sleep apnea syndrome and rhinitis: a prospective analysis. Am. J. Rhinol. Allergy, 28(1):e52–e55. [doi:10.2500/ajra.2014.28.3977]
Peppard, P.E., Young, T., Barnet, J.H., et al., 2013. Increased prevalence of sleep-disordered breathing in adults. Am. J. Epidemiol., 177(9):1006–1014. [doi:10.1093/aje/kws342]
Prabhakar, N.R., Semenza, G.L., 2012. Adaptive and maladaptive cardiorespiratory responses to continuous and intermittent hypoxia mediated by hypoxia-inducible factors 1 and 2. Physiol. Rev., 92(3):967–1003. [doi:10. 1152/physrev.00030.2011]
Raheem, O.A., Orosco, R.K., Davidson, T.M., et al., 2014. Clinical predictors of nocturia in the sleep apnea population. Urol. Ann., 6(1):31–35. [doi:10.4103/0974-7796.127019]
Romero, E., Krakow, B., Haynes, P., et al., 2010. Nocturia and snoring: predictive symptoms for obstructive sleep apnea. Sleep Breath., 14(4):337–343. [doi:10.1007/s11325-009-0310-2]
Sforza, E., Chouchou, F., Collet, P., et al., 2011. Sex differences in obstructive sleep apnoea in an elderly French population. Eur. Respir. J., 37(5):1137–1143. [doi:10.1183/09031936.00043210]
Acknowledgements
We sincerely thank Prof. Li-na ZHANG (Department of Epidemiology, Ningbo University School of Medicine, China) for her excellent assistance in the statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Project supported by the Ningbo Natural Science Foundation of China (No. 2013A610236)
ORCID: Chuan SHAO, http://orcid.org/0000-0001-9073-219X
Rights and permissions
About this article
Cite this article
Shao, C., Jiang, Jb., Wu, Hc. et al. Clinical assessment and polysomnographic study of sleep apnea in a Chinese population of snorers. J. Zhejiang Univ. Sci. B 16, 215–223 (2015). https://doi.org/10.1631/jzus.B1400236
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1631/jzus.B1400236