Abstract
Objective
To compare the peri-operative outcomes for laparoscopic distal pancreatectomy (LDP) and open distal pancreatectomy (ODP) for benign or premalignant pancreatic neoplasms in two institutions.
Methods
This prospective comparative study included 91 consecutive patients who underwent LDP (n=45) or ODP (n=46) from Jan. 2010 to Dec. 2012. Demographics, intra-operative characteristics, and post-operative outcomes were compared.
Results
The median operating time in the LDP group was (158.7±38.3) min compared with (92.2±24.1) min in the ODP group (P<0.001). Patients had lower blood loss in LDP than in the ODP ((122.6±61.1) ml vs. (203.1±84.8) ml, P<0.001). The rates of splenic conservation between the LDP and ODP groups were similar (53.3% vs. 47.8%, P=0.35). All spleen-preserving distal pancreatectomies were conducted with vessel preservation. LDP also demonstrated better post-operative outcomes. The time to oral intake and normal daily activities was faster in the LDP group than in the ODP group ((1.6±0.5) d vs. (3.2±0.7) d, P<0.01; (1.8±0.4) d vs. (2.1±0.6) d, P=0.02, respectively), and the postoperative length of hospital stay in LDP was shorter than that in ODP ((7.9±3.8) d vs. (11.9±5.8) d, P=0.006). No difference in tumor size ((4.7±3.2) cm vs. (4.5±1.8) cm, P=0.77) or overall pancreatic fistula rate (15.6% vs. 19.6%, P=0.62) was found between the groups, while the overall post-operative complication rate was lower in the LDP group (26.7% vs. 47.8%, P=0.04).
Conclusions
LDP is safe and effective for benign or premalignant pancreatic neoplasms, featuring lower blood loss and substantially faster recovery.
總結
目 的
评估腹腔镜胰体尾切除术安全有效性,对比腹腔镜胰体尾切除术与开腹胰体尾切除术治疗胰腺体尾部良性或低度恶性病变临床疗效。
创新点
本研究为回顾性对照研究,相较于过往腹腔镜胰体尾切除术与开腹胰体尾切除术的对照研究,其创新点一为本组91 例病例均为良性或低度恶性病例,剔除了恶性病变病例;二为本研究中腹腔镜胰体尾切除术组及开腹胰体尾切除术组分别由两家大型综合医院胰腺疾病诊治中心的两组医生分别施行手术,这样避免了病人及手术方式选择等造成的影响,结果更为客观。
方法
回顾分析自2010 年1 月至2012 年12 月浙江大学医学院附属邵逸夫医院45 例施行腹腔镜胰体尾切除术治疗胰腺体尾部良性或低度恶性病变病例(LDP 组),以及同期上海复旦大学附属中山医院46 例施行开腹胰体尾切除术胰腺体尾部良性或低度恶性病变病例(ODP 组)的相关临床资料,进行对照研究。
结论
本研究包括胰腺体尾部良性或低度恶性病例91 例,其中LDP 组45 例(无中转开腹)和ODP 组 46 例。手术时间分别为(158.7±38.3) min(LDP 组)和(92.2±24.1) min(ODP 组);术中出血LDP 组明显少于ODP 组( (122.6±61.1) ml vs. (203.1±84.8) ml,P<0.001)。两组保脾率相似(53.3% vs. 47.8%,P=0.35),其中LDP 组中保脾病例均保留脾血管。在术后恢复指标方面,LDP 组优于ODP 组,恢复进食流质时间((1.6±0.5) d vs. (3.2±0.7) d,P<0.01)及恢复活动时间((1.8±0.4) d vs. (2.1±0.6) d,P=0.02)较短,且LDP 组术后住院时间也少于ODP 组((7.9±3.8) d vs. (11.9±5.8) d, P=0.006)。术后胰瘘率两组无明显差异(15.6% vs. 19.6%,P=0.62),但术中总并发症率LDP 组低于ODP 组(26.7% vs. 47.8%,P=0.04)。研究结果显示腹腔镜胰体尾切除术治疗胰腺体尾部良性或低度恶性肿瘤安全可行,与开腹胰体尾切除术术相比术中出血更少、术后恢复更快,具有明显微创优势。
Similar content being viewed by others
1 Introduction
Application of minimally invasive techniques, i.e. laparoscopic pancreatic surgery, in the management of distal pancreatic lesions is increasing. It is particularly adapted to distal pancreatic surgery because of the absence of anastomosis in this surgery. Laparoscopic distal pancreatectomy (LDP) was first reported by Cuschieri (1994). Since then, several case series (Melotti et al., 2007; Taylor et al., 2008; Song et al., 2011), comparative cohort studies (Mabrut et al., 2005; Kooby et al., 2008; Jayaraman et al., 2010), and meta-analysis reports (Jusoh and Ammori, 2012; Pericleous et al., 2012; Xie et al., 2012; Nakamura and Nakashima, 2013) have shown that LDP provides similar advantages that have been demonstrated for other minimally invasive surgeries. In patients who underwent laparoscopic surgeries, there were fewer surgical site infections and complications, and decreased length of stay and expenses compared with open distal pancreatectomy (ODP) (Fox et al., 2012; Kneuertz et al., 2012; Venkat et al., 2012).
Laparoscopy seems to be under-utilized for distal pancreas resection owing to the complexity of the procedure, the high requirement of technical skills by the surgeon in dissecting the important vascular, and the lower acceptance in the resection of malignant lesions. Further, the limitations of selection bias, small sample size, and pooling of multi-institutional data have hindered a meaningful comparative trial of LDP and ODP. Randomized, controlled trials comparing LDP with the ODP are limited. No consensus exists for or against the use of the laparoscopic approach for distal pancreatectomy in benign and malignant lesions.
To better elucidate the benefits of LDP, here we report a prospective comparative study of the two approaches at two high-volume institutions, aiming to systematically compare the peri-operative outcomes of LDP with ODP for benign or premalignant pancreatic neoplasms.
2 Materials and methods
2.1 Patients
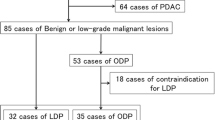
This two-center study was performed from Jan. 2010 to Dec. 2012. Data from 91 consecutive patients who underwent distal pancreatectomy in the Department of General Surgery, Zhongshan Hospital, Shanghai Medical College, Fudan University (Shanghai, China) and the Department of General Surgery, Institute of Micro-Invasive Surgery, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University (Hangzhou, China) entered into our surgical database. This study had been approved by the ethics boards of the two hospitals, and informed consent was obtained from all patients. Patients with benign or premalignant pancreatic neoplasms were screened with thin slice computerized tomography or magnetic resonance imaging before the operation. Patients with malignant tumors, pregnant or lactating women, or those with child-bearing potential, patients who had multiple organ resections during distal pancreatectomy or a history of abdominal surgery, were excluded.
Pre-operative variables included age, gender, body mass index (BMI), significant co-morbidity, operation history, hepatic and renal function, coagulation function, carcinoembryonic antigen, CA19-9, and a-fetoprotein. Intra-operative variables such as operative time, operative blood loss, as well as post-operative time to resume normal daily activities and first time of oral intake, were recorded. Data for post-operative complications within 30 d of the operation were gathered, such as pancreatic fistula, delayed gastric emptying, wound infections, intestinal adhesion and ileus.
The indications for surgical resection of pancreatic cystic neoplasms in our study were as follows: (1) tumor size larger than 4 cm; (2) after surveillance for rapid rate of growth; (3) presence of symptoms such as abdominal pain or distension; (4) inability to definitely exclude a premalignant or malignant tumor.
Distal pancreatectomy was defined as resection of the pancreas to the left of the portal vein, with or without splenic conservation. Pancreatic fistula and delayed gastric emptying was defined according to the guidelines of the International Study Group on Pancreatic Fistulas (ISGPF) (Bassi et al., 2005; Wente et al., 2007). Operative time was defined as the time between patient entry into and exit from the operation room. Post-operative diet began on the first day after first bowel gurgles. Length of stay was calculated from date of operation to date of hospital discharge. Peri-operative mortality was defined as death within 30 d of the operation or within the same hospital admission as the operation.
2.2 Surgical procedure
2.2.1 ODP
All the ODP surgeries were done by one group of surgeons in Zhongshan Hospital (Shanghai, China).
The peritoneal cavity was entered by subcostal incision. The gastrocolic ligament was divided and the omental sac opened. After careful intra-operative exploration, we proceeded to resection the pancreas. The superior and inferior borders of the pancreas were defined, and the splenic vessels were identified and preserved or ligated depending on whether splenic preservation was to be performed. The pancreas was mobilized and transected with the Endo-GIA stapler. At the end of the operation, a drain was placed into the left subdiaphragmatic area.
Attempts were made in all patients to conserve the spleen. To avoid the occurrence of splenic infarction or splenic abscess, we used the surgical technique for splenic salvage with conservation of the splenic artery and vein, rather than ligation of the splenic pedicle with preservation of the short gastric vessels (Warshaw, 1988). A splenectomy was performed during distal pancreatectomy for the following reasons: (1) splenic infarction, thrombosis of the splenic vessels, or regional portal hypertension; (2) difficult dissection from the splenic vessels or splenic hilum; (3) intra-operative bleeding from the splenic vessels or the spleen.
2.2.2 LDP
All the LDP surgery was done by one group of surgeons in the Sir Run Run Shaw Hospital (Hangzhou, China).
The technique for LDP has been described elsewhere (Abu Hilal et al., 2009). In short, five ports (three 5-mm ports and two 10/12-mm ports) were used. Typically, the first trocar—preferably optical—was inserted in the umbilicus. The remaining trocars were placed as follows: two 5-mm trocars were placed in the subcostal area in the anterior axillary line on both sides; a 12-mm trocar was placed outside the right rectus abdominis 2 cm above the umbilicus, which permits use of an Endo-GIA stapler, and a 5-mm trocar on the opposite left side. After establishing laparoscopic access, the pancreas was exposed through the division of the lesser sac. The splenic attachments and the short gastric vessels were divided. The splenic vessels were dissected from the pancreas to the splenic hilum. The pancreas was transected with the Endo-GIA stapler. When simultaneous splenectomy was being performed, the splenic artery and vein were ligated and divided.
If imaging examination before operation indicated a splenic preservation, the pancreas was dissected off the splenic vessels; tributary vessels were treated with the harmonic scalpel or clips. Splenic vessels were all conserved during spleen-preserving pancreatectomies.
The specimen was then placed in an endoscopic bag. A minilaparotomy can be carried out at the umbilical port. Peritoneal drains were placed adjacent to the pancreatic remnant and brought out of the abdomen through the 5-mm port sites. In case of intraoperative bleeding from the splenic vessels or the spleen, a conversion from LDP to ODP was necessary.
2.3 Statistical analysis
Demographic, procedural, and post-operative data were documented. Continuous variables were reported as mean±standard error (SE). Categorical variables were reported as number and percentage. Continuous variables were compared using Student’s t-test. Categorical variables were compared using Pearson’s chi-square test or Fisher’s exact test as appropriate. A P-value of less than 0.05 was considered statistically significant. Statistical analyses were conducted using the SPSS 15.0 statistical software program (SPSS Inc., Chicago, IL, USA).
3 Results
3.1 Demographics and pre-operative clinical information
Nighty-one patients (58 females and 33 males) successfully underwent LDP (n=45) or ODP (n=46) for a benign or premalignant tumor of the distal pancreas during the study period. Between the LDP and ODP groups, there were no significant intergroup differences in the following clinical factors: age, sex, or body mass index (BMI) (Table 1). The final histological results were as follows: neuroendocrine tumor (21), serous cystic neoplasm (32), solid pseudopapillary tumors (17), mucinous cystic neoplasm (13), and intraductal papillary mucinous neoplasm (8) (Table 2).
3.2 Intra-operative outcomes
No patient in the LDP group was converted to ODP. The median operative time in the LDP group was (158.7±38.3) min compared with (92.2±24.1) min in the ODP group (P<0.001). Intra-operative blood loss in the LDP group was lower than that in the ODP group ((122.6±61.1) ml vs. (203.1±84.8) ml, P<0.001). The rates of splenic conservation between the LDP and ODP groups were similar (53.3% vs. 47.8%, P=0.35). Splenic vessels were all preserved during spleen-preserving pancreatectomies. No obvious difference in tumor size between the groups was observed ((4.7±3.2) cm vs. (4.5±1.8) cm, P=0.77; Table 3).
3.3 Post-operative outcomes
No patient died in the ODP group or LDP group, or needed a re-operation. The overall post-operative complication rates were lower in the LDP group compared with the ODP group (26.7% vs. 47.8%, P=0.04; Table 4). The overall pancreatic fistula rates between the LDP and ODP groups were similar (15.6% vs. 19.6%, P=0.62). A pancreatic fistula developed in nine patients in the ODP group (7 Grade A and 2 Grade B) versus seven patients in the LDP group (5 Grade A and 2 Grade B). Time to oral intake and time to resume normal daily activities were significantly faster in the LDP group than in the ODP group ((1.6±0.5) d vs. (3.2±0.7) d, P<0.01; (1.8±0.4) d vs. (2.1±0.6) d, P=0.02, respectively). The post-operative length of hospital stay was also shorter in the LDP group compared with the ODP group ((7.9±3.8) d vs. (11.9±5.8) d, P=0.006; Table 4).
4 Discussion
In this prospective two-center comparative study of clinical outcomes for LDP and ODP, we demonstrated that LDP is a feasible, safe, and efficient approach for benign or premalignant pancreatic neoplasms. We observed less blood loss, an earlier return to normal bowel movement, and a significantly shorter post-operative length of stay in the LDP group compared with ODP. The overall morbidity in our study was not different between the LDP and ODP groups, indicating similar safety profiles of the two surgical approaches. These findings are consistent with the best case series published so far (Baker et al., 2009; Casadei et al., 2010; Vijan et al., 2010; Abu Hilal et al., 2012; Soh et al., 2012).
The highlight of this study is that all the pancreatic lesions in the two groups were benign or of low grade. The pathology and the lesion’s size are two main factors that influence the operative difficulty during a distal pancreatectomy. When we compare LDP with ODP, the operative difficulty between two groups should be taken into account because it will influence the feasibility and peri-operative outcomes, such as blood loss, operation time, splenic conservation rate, and morbidity. Further, it is notable that the LDP and the ODP in our study were practiced by specialized surgeon teams in two high-volume centers separately, who specifically focus on laparoscopic pancreatic surgery and the open pancreatic approach. Thus, the selection bias in this two-center comparative study can be avoided to a certain degree.
In contrast to most studies showing that LDP had shorter operation time, we observed a converse result: the median operative time in the LDP group was longer than that in the ODP group. We can rationalize this difference by the skilled practice of the open surgery team. In fact, the operation times of the LDP ((158.7±38.3) min) and ODP ((92.2±24.1) min) groups in our study are shorter than most of the former studies, which reflects benign pathology of all the lesions.
Another interesting finding of our study is the high rate of splenic conservation in the LDP group (55.6%). The patients who underwent laparoscopic spleen-preserving distal pancreatectomy had significantly shorter operative time and less blood loss compared with those who underwent concomitant splenectomy (Shoup et al., 2002; Goh et al., 2008; Lee et al., 2008; Mekeel et al., 2011; Butturini et al., 2012). The rate of splenic conservation in former studies of LDP varied from 2% to 70% (Shoup et al., 2002; Goh et al., 2008; Lee et al., 2008; Casadei et al., 2010; Vijan et al., 2010; Abu Hilal et al., 2012; Butturini et al., 2012). However, most of the former comparative studies included both malignant and benign lesions. Therefore, the high rate of spleen preservation may be attributed to the high rate of malignant lesions in the open group, and the fact that many lesions in the open group were inflammatory strictures secondary to pancreatitis. In our study, considering that all the lesions were benign in both the LDP and the ODP groups, the higher rate of splenic conservation in the LDP group demonstrates a noteworthy advantage of LDP over ODP.
Spleen conservation could be achieved by carefully dissecting the splenic vessels off the pancreas parenchyma or by resecting the main splenic vessels en bloc with the pancreas but maintaining the short gastric vessels and left gastroepiploic arcade to ensure the collateral blood supply to the spleen (Warshaw, 1988). In our study, spleen conservation was accomplished by preserving the main splenic artery and vein. We think that the better vision afforded by the magnification using the laparoscopic instrument and the subtle laparoscopic manipulations available assist in the fine dissection of the pancreas off the splenic artery and vein, resulting in higher splenic conservation rates.
The incidence of post-operative pancreatic fistula, the most common major morbidity after distal pancreatectomy, was not different in this study. Encompassing all grades of fistula, we observed a fistula rate of 15.6% in the LDP group, which is comparable or favorable to that reported by others. Several studies investigated different approaches to prevent pancreatic fistula in distal pancreatectomy. However, none of these methods could reduce the rate of pancreatic fistula significantly. In this study, we routinely used the mechanical linear staplers. The LDP group used small staples (2.5–3.5 mm) depending on the texture of the pancreas (2.5 mm for thin pancreases and 3.5 mm for thick pancreases), whereas the ODP prefers large staples (4.5 mm).
In this study, the pre-operative variables such as demographics, blood profiles, and co-morbid conditions were comparable between the two groups, indicating that patients are relatively alike in terms of their pre-operative status and subsequent comparisons are more meaningful. Although we attempted to circumvent selection bias, a certain degree of bias is inherent between the two institutions in the comparative study. Another limitation of this study is the relatively small number of cases. As distal pancreatectomy is an infrequent procedure, enrolment of large numbers of cases may be a difficult task.
In summary, the findings in this study confirmed the safety and efficacy of LDP for the treatment of benign and premalignant lesions in the pancreatic body and tail. This laparoscopic approach is associated with less operative blood loss and hospitalization fast recovery compared with ODP. LDP may be progressively adopted as the “gold standard” for the management of benign and premalignant pancreatic lesions. Further studies on the oncologic quality and more prospective randomized comparative trials for LDP should be performed before applying this to the management of pancreatic malignancies.
Compliance with ethics guidelines
Jia-fei YAN, Tian-tao KUANG, Da-yong JI, Xiao-wu XU, Dan-song WANG, Ren-chao ZHANG, Wei-wei JIN, Yi-ping MOU, and Wen-hui LOU declare that they have no conflict of interest.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study.
References
Abu-Hilal M., Jain G., Kasasbeh F., et al., 2009. Laparoscopic distal pancreatectomy: critical analysis of preliminary experience from a tertiary referral centre. Surg. Endosc., 23(12):2743–2747. [doi:10.1007/s00464-009-0499-y]
Abu-Hilal M., Hamdan M., Di-Fabio F., et al., 2012. Laparoscopic versus open distal pancreatectomy: a clinical and cost-effectiveness study. Surg. Endosc., 26(6):1670–1674. [doi:10.1007/s00464-011-2090-6]
Baker M.S., Bentrem D.J., Ujiki M.B., et al., 2009. A prospective single institution comparison of perioperative outcomes for laparoscopic and open distal pancreatectomy. Surgery, 146(4):635–643. [doi:10.1016/j.surg.2009.06.045]
Bassi C., Dervenis C., Butturini G., et al., 2005. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery, 138(1):8–13. [doi:10.1016/j.surg.2005.05.001]
Butturini G., Inama M., Malleo G., et al., 2012. Perioperative and long-term results of laparoscopic spleen-preserving distal pancreatectomy with or without splenic vessels conservation: a retrospective analysis. J. Surg. Oncol., 105(4):387–392. [doi:10.1002/jso.22117]
Casadei R., Ricci C., D’Ambra M., et al., 2010. Laparoscopic versus open distal pancreatectomy in pancreatic tumours: a case-control study. Updates Surg., 62(3–4):171–174. [doi:10.1007/s13304-010-0027-6]
Cuschieri A., 1994. Laparoscopic surgery of the pancreas. J.R. Coll. Surg. Edinb., 39(3):178–184.
Fox A.M., Pitzul K., Bhojani F., et al., 2012. Comparison of outcomes and costs between laparoscopic distal pancreatectomy and open resection at a single center. Surg. Endosc., 26(5):1220–1230. [doi:10.1007/s00464-011-2061-y]
Goh B.K., Tan Y.M., Chung Y.F., et al., 2008. Critical appraisal of 232 consecutive distal pancreatectomies with emphasis on risk factors, outcome, and management of the postoperative pancreatic fistula: a 21-year experience at a single institution. Arch. Surg., 143(10):956–965. [doi:10.1001/archsurg.143.10.956]
Jayaraman S., Gonen M., Brennan M.F., et al., 2010. Laparoscopic distal pancreatectomy: evolution of a technique at a single institution. J. Am. Coll. Surg., 211(4):503–509. [doi:10.1016/j.jamcollsurg.2010.06.010]
Jusoh A.C., Ammori B.J., 2012. Laparoscopic versus open distal pancreatectomy: a systematic review of comparative studies. Surg. Endosc., 26(4):904–913. [doi:10.1007/s00464-011-2016-3]
Kneuertz P.J., Patel S.H., Chu C.K., et al., 2012. Laparoscopic distal pancreatectomy: trends and lessons learned through an 11-year experience. J. Am. Coll. Surg., 215(2):167–176. [doi:10.1016/j.jamcollsurg.2012.03.023]
Kooby D.A., Gillespie T., Bentrem D., et al., 2008. Leftsided pancreatectomy: a multicenter comparison of laparoscopic and open approaches. Ann. Surg., 248(3):438–446. [doi:10.1097/SLA.0b013e318185a990]
Lee S.E., Jang J.Y., Lee K.U., et al., 2008. Clinical comparison of distal pancreatectomy with or without splenectomy. J. Korean Med. Sci., 23(6):1011–1014. [doi:10.3346/jkms.2008.23.6.1011]
Mabrut J.Y., Fernandez-Cruz L., Azagra J.S., et al., 2005. Laparoscopic pancreatic resection: results of a multicenter European study of 127 patients. Surgery, 137(6):597–605. [doi:10.1016/j.surg.2005.02.002]
Mekeel K.L., Moss A.A., Reddy K.S., et al., 2011. Laparoscopic distal pancreatectomy: does splenic preservation affect outcomes? Surg. Laparosc. Endosc. Percutan. Tech., 21(5):362–365. [doi:10.1097/SLE.0b013e31822e0ea8]
Melotti G., Butturini G., Piccoli M., et al., 2007. Laparoscopic distal pancreatectomy: results on a consecutive series of 58 patients. Ann. Surg., 246(1):77–82. [doi:10.1097/01.sla.0000258607.17194.2b]
Nakamura M., Nakashima H., 2013. Laparoscopic distal pancreatectomy and pancreatoduodenectomy: is it worthwhile? A meta-analysis of laparoscopic pancreatectomy. J. Hepatobiliary Pancreat. Sci., 20(4):421–428. [doi:10.1007/s00534-012-0578-7]
Pericleous S., Middleton N., McKay S.C., et al., 2012. Systematic review and meta-analysis of case-matched studies comparing open and laparoscopic distal pancreatectomy: is it a safe procedure? Pancreas, 41(7):993–1000. [doi:10.1097/MPA.0b013e31824f3669]
Shoup M., Brennan M.F., Mc-White K., et al., 2002. The value of splenic preservation with distal pancreatectomy. Arch. Surg., 137(2):164–168. [doi:10.1001/archsurg.137.2.164]
Soh Y.F., Kow A.W., Wong K.Y., et al., 2012. Perioperative outcomes of laparoscopic and open distal pancreatectomy: Our institution’s 5-year experience. Asian J. Surg., 35(1):29–36. [doi:10.1016/j.asjsur.2012.04.005]
Song K.B., Kim S.C., Park J.B., et al., 2011. Single-center experience of laparoscopic left pancreatic resection in 359 consecutive patients: changing the surgical paradigm of left pancreatic resection. Surg. Endosc., 25(10):3364–3372. [doi:10.1007/s00464-011-1727-9]
Taylor C., O’Rourke N., Nathanson L., et al., 2008. Laparoscopic distal pancreatectomy: the Brisbane experience of forty-six cases. HPB (Oxford), 10(1):38–42. [doi:10.1080/13651820701802312]
Venkat R., Edil B.H., Schulick R.D., et al., 2012. Laparoscopic distal pancreatectomy is associated with significantly less overall morbidity compared to the open technique: a systematic review and meta-analysis. Ann. Surg., 255(6):1048–1059. [doi:10.1097/SLA.0b013e318251ee09]
Vijan S.S., Ahmed K.A., Harmsen W.S., et al., 2010. Laparoscopic vs open distal pancreatectomy: a single institution comparative study. Arch. Surg., 145(7):616–621. [doi:10.1001/archsurg.2010.120]
Warshaw A.L., 1988. Conservation of the spleen with distal pancreatectomy. Arch. Surg., 123(5):550–553. [doi:10.1001/archsurg.1988.01400290032004]
Wente M.N., Bassi C., Dervenis C., et al., 2007. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery, 142(5):761–768. [doi:10.1016/j.surg.2007.05.005]
Xie K., Zhu Y.P., Xu X.W., et al., 2012. Laparoscopic distal pancreatectomy is as safe and feasible as open procedure: a meta-analysis. World J. Gastroenterol., 18(16):1959–1967. [doi:10.3748/wjg.v18.i16.1959]
Author information
Authors and Affiliations
Corresponding authors
Additional information
The two authors contributed equally to this work
Project supported by the Department of Health of Zhejiang Province, China (Nos. 2011ZHB003 and 2013RCB010)
ORCID: Jia-fei YAN, http://orcid.org/0000-0003-4382-3835
Rights and permissions
About this article
Cite this article
Yan, Jf., Kuang, Tt., Ji, Dy. et al. Laparoscopic versus open distal pancreatectomy for benign or premalignant pancreatic neoplasms: A two-center comparative study. J. Zhejiang Univ. Sci. B 16, 573–579 (2015). https://doi.org/10.1631/jzus.B1400257
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1631/jzus.B1400257
Key words
- Laparoscopy
- Distal pancreatic resection
- Pancreatic neoplasm
- Splenic preservation
- Pancreatic benign tumors