Initial single center experience: radiofrequency ablation assisted vertebroplasty and osteoplasty using a bipolar device in the palliation of bone metastases
Introduction
Percutaneous vertebral augmentation in the form of vertebroplasty (VP) is an accepted form of treatment both in the treatment of insufficiency fractures and in palliation of painful bone metastases (1). The use of radiofrequency ablation (RFA) prior to injection of cement in VP or osteoplasty (OP) has been described as a safe and effective procedure in the treatment of painful metastatic bone disease (2,3).
In prior studies, monopolar devices have been used with some difficulty. The insulative nature of bone requires a large amount of power and inadvertent injury to adjacent structures has been described, often resulting in neuropathic pain. The use of bipolar RFA prior to cementoplasty has the advantage of more precise energy deposition and decreased risk of injury to adjacent structures. This is especially true in the spine, where there is an inherent proximity to adjacent nerves and spinal cord.
It has been anecdotally described that the use of RFA prior to cementoplasty improves the predictability of cement distribution (2,4-6). To our knowledge, no previous studies have demonstrated that this observation is true. In this study, we describe our experience with the use of a new bipolar RFA system (Osteocool, Baylis Medical) in the context of treatment of painful metastatic bone disease. Furthermore, we study the safety profile of this device in the use prior to VP, and compare the rate of cement leaks in patients who have had an RFA assisted VP to those who had conventional VP in our centre. We also evaluated the pain scores pre and post of the RFA group to see if it would improve without any unanticipated effects. The superiority of VP to conservative treatment in insufficiency fractures has been described in the Vertos 2 trial (7).
Methods
Patients referred for symptomatic malignant or insufficiency fractures for VP or OP from January 2011 to May 2015 were retrospectively reviewed. Bipolar RFA was performed (Osteocool RF ablation system, Baylis Medical) reaching a constant temperature of 70 °C over 7 to 15 minutes followed by cement injection. Radiological outcomes were assessed with CT. Pre and post procedural pain scores were also documented for the RFA subset primarily to see if there was any adverse effect when using RFA on pain relief.
Study design
The study was approved by the hospital scientific and ethics committee. This was a single-centre retrospective analysis of all patients who underwent a VP or OP for symptomatic insufficiency fractures or malignant disease in the department of interventional radiology department, between January 2011 to May 2015. All patients who underwent a VP or OP were found through searching of the Picture archiving and communication system (PACS). Patients who had undergone an RFA assisted VP or OP were furthermore found within a prospectively collected database by the interventional radiology department in conjunction with the radiation oncology department. Demographic information was obtained through this database and search of EMRs. Procedures were all done by one of four interventional radiologists with 8 years of experience.
For patients who had an RFA assisted VP or OP, technical success was defined as completion of the procedure under conscious sedation and delivery of cement to the desired location. Morbidity and mortality rates were obtained through review of EMRs. Pain scores prior to and following the procedure were obtained through patient interviews. Patients were asked to rate their pain on a scale of 1 to 10 prior to and following the procedure. Similarly, for patients who had a conventional VP, technical success was defined as completion of the procedure under conscious sedation and delivery of the cement to the desired location. Morbidity and mortality rates were also obtained through review of EMR. Pain scores were not obtained in this group as they were only retrospectively reviewed through our PACS database.
Assessment of cement leaks for both groups was performed using post procedure computerized tomography (CT) scans. Any leak was defined as any leak of cement outside of the vertebral body. Posterior leaks were defined as cement leaks into the posterior epidural space or into the posterior venous plexus. Disc leaks were defined as any cement leak into the above or below intervertebral disc space.
Cement filling was assessed using post procedure CTs. The rate of filling was assessed in three axes (anteroposterior, lateral and craniocaudal). Filling in each axis was given a score of 1 to 4, with a score of 1 given for 0–24% filling, a score of 2 for 25–49% filling, a score of 3 for 50–74% filling and a score of 4 for 75–100% filling. The total cement filling score was taken as the total of the three axis scores.
For RFA assisted VP and OP, the procedure was performed under fluoroscopic guidance or combined CT and fluoroscopic guidance. An M1M needle (Cook medical, either 11 Gauge or 13 Gauge depending on the location) was inserted into the vertebral body under fluoroscopic control. For OPs, initial needle placement was done under CT guidance. The RFA probe was then inserted and RFA is performed. Live monitoring of the temperature achieved, as well as of the power used and measured impedance was done. Impedance values were recorded at various time points during the procedure. A temperature of 70 °C was achieved and kept constant for 7 to 15 minutes. Once done, the RFA probe was removed and cement (Kyphon—PMMA) injection was done through the same needle, under fluoroscopic guidance. The RFA was stopped earlier than 15 minutes in cases of patient agitation or pain.
Statistical analysis
Pain scores prior to and following the procedure were compared using a paired t-test. Cement leak rates were compared using logistic regression analysis and cement filling rates were compared using linear regression. Results are expressed as odds ratios with 95% confidence intervals and P values.
Results
Study population
Twenty-six patients in the study were treated with the RFA assisted technique. These contributed to 4 OPs and 35 VP levels. Of these, four VP levels were insufficiency fractures. All were technically successful without morbidity or mortality. Fifty-six patients were treated with a non RFA assisted technique. All these were VPs and 142 levels were treated in total. The average age was 72. Two levels in this subset were insufficiency fractures. All were technically successful without morbidity or mortality (Tables 1,2). There was a significantly reduced rate of posterior and venous cement leaks when RFA was used prior to VP. There was no difference in the rate of leakage into the disc spaces when comparing RFA assisted to the conventional technique. Pain scores in the RFA assisted group decreased significantly post procedure with no unanticipated neuropathic events.

Full table
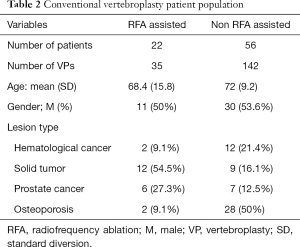
Full table
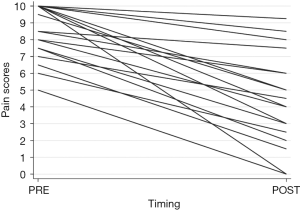
Outcomes and pain scores for RFA assisted group
Technical success was achieved in all RFA assisted VP and OP cases. There was no morbidity related to the procedures. Even in cases where there was a cement leak, these were subclinical and did not result in any morbidity. During the follow up period of this study, the mortality rate, for patients who have had an RFA assisted VP or OP, was 23% (6 of 26 patients). The cause of death was unrelated to the procedure in all cases. There a significant improvement in pain scores following the procedure in a consistent manner. Results are displayed in Table 3 and Figure 1.
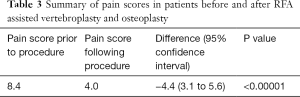
Full table
Cement leaks
There was a significantly reduced rate of cement leaks when RFA was used prior to a VP. Overall, in all cases, the odds ratio was 0.262 (95% CI: 0.113 to 0.607; P=0.002) of having any cement leak if RFA was used prior to the procedure. This relationship persisted when analysis was done only on VPs done for metastatic disease, in which group the odd ratio was 0.194 (95% CI: 0.072 to 0.523; P=0.001). Importantly, the risk of having a posterior leak was also reduced significantly with an odds ratio of 0.166 (95% CI: 0.038 to 0.729; P=0.017) for all cases and 0.069 (95% CI: 0.0088 to 0.539; P=0.011) for VPs done in metastatic disease. However, there was no difference in leaks into the disc space when comparing the RFA to the non RFA group.
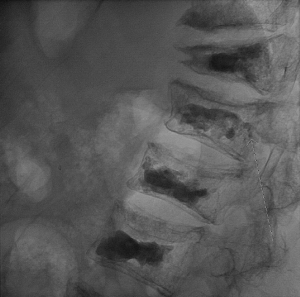
We also noted a trend to having a decrease in venous leaks if RFA was used prior to the VP. In all cases, the odds ratio was 0.435 of having a venous leak if RFA was used compared to if it was not used [95% CI: (0.184 to 1.027); P=0.058]. In metastatic disease cases, the odds ratio was 0.393 [95% CI: (0.150 to 1.030); P=0.057] of having a venous leak if RFA was used prior to the VP versus if it were not. An example of an asymptomatic posterior epidural cement leak can be seen in Figures 2 and 3.

Cement filling
Using a linear regression model, we found that the degree of cement filling of the vertebral body was not significantly different whether RFA was or was not used prior to the procedure (P=0.586). This is after adjusting for whether the case was done in metastatic disease or in insufficiency fractures and if the case was done via a uni- or bipedicular approach. Cement filling was also not significantly different in VPs done in metastatic disease versus in insufficiency fractures (P=0.313). There was improved cement filling in cases done by a bipedicular approach compared to a unipedicular approach (P< 0.0001). The overall model fit was R-squared =0.093.
Discussion
We demonstrate the technical feasibility and safety of using a bipolar RFA system prior to OPs and VPs (8,9). One of the advantages of using a bipolar RFA system is a more localized energy deposition, which decreases risk of injury to adjacent structures. This was demonstrated in our study, where we had no instance of injury to adjacent structures during RFA. Furthermore, the issue of high impedance is avoided by the use of a bipolar design and internal cooling of the device, which limits charring, and allows a controlled increase in temperature up to 70 °C. This theoretically increases the size of the ablation zone and should also improve the likelihood of disease control, which we did not evaluate in our study.
Pain score improvement following RFA assisted VP or OP in our study was comparable to other studies in the literature. Pain relief post treatment was probably secondary to multiple factors. Stabilization, mechanical strengthening of the bone, and sealing microfractures likely all contributed to pain reduction. Other mechanisms have been hypothesized. One such mechanism includes the destruction of pain fiber nerve endings. This can be due to the exothermic reaction that occurs during hardening of PMMA (10) or as a result of RFA prior to the procedure. Other factors that may contribute to the therapeutic effect of RFA prior to OP or VP include the reduction of interleukins and TNF responsible for a sensitization of nerve endings and the inhibition of osteoclasts (2). Nevertheless, the synergistic effect of the use of RFA prior to VP or OP in controlling pain remains unproven (11-13).
We confirmed several anecdotal reports (2-6,14) of a more controlled injection of cement when using the RFA technique by showing statistically significant lower rates of cement leaks when RFA was used prior to VPs. More importantly, we noted a lower rate of posterior cement leak, which is often the rate limiting factor in cement delivery. Coupled with the results showing that the degree of cement filling is equivalent between RFA assisted and conventional VPs, we conclude that the use of RFA prior to VPs allowed a lower rate of posterior leaks while maintaining a similar degree of cement filling of the vertebral bodies, which is a notable result.
The cause of improved control of cement injection is still unknown. RFA does not create a mechanical cavity for the cement, as in kyphoplasty procedures. It is postulated that ablation of the lesion changes the consistency of the tumor, which can shrink the tumor and destroy the “cohesion” of the tumor cells (2). Tissue desiccation may play a role by reducing the volume of material within the ablation zone and creating space for the cement. Therefore, RFA prior to cement injection creates a so-called “thermal cavity”, which allows for a more controlled deposition of cement within this cavity. This is supported by a cadaveric study by Woo et al. (9) showing tumor volume reduction with bipolar RF done prior to PV. See Figures 4 and 5 for an RFA assisted VP in renal cell carcinoma, and Figures 6 and 7 for an RFA assisted sacral OP.



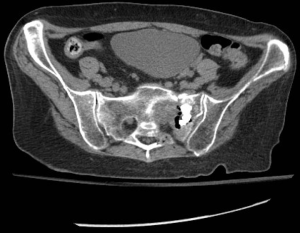
The effect of RFA on the venous plexus may also play a role. It has been suggested that RFA may lead to thrombosis of the venous plexus, which may limit the embolization events during cement injection (3-5). Certainly, the trend towards lower venous leaks in cases that have had RFA prior to VP in our study supports this concept. Furthermore, we have encountered few cases where the morphology of epidural cement leaks suggests initial leak into the posterior lumbar venous plexus, which eventually ruptures the vein and leaks into the epidural space (Figures 6,7). Posterior venous leaks may thereby be a large source of epidural cement and by limiting this route the percentage of posterior leaks would decrease. In addition, we had no venous filling contributing to cement pulmonary emboli in our series. Our hypothesis that this phenomenon is probably related to venous thrombosis is supported by the fact that the use of RFA prior to VP had no effect on the rate of disc space leaks.
In addition to the retrospective nature of our study, the study is also limited by the lack of a presence of a control group. The control group would have allowed us to assess if RFA enhanced pain relief. Our data simply shows it improves pain relief in a similar fashion to conventional VP as noted in the prior Vertos 2 trial (7). Our data may also be slightly influenced by the larger number of VP cases in our series and the limited number of OP cases. We also only had a small number of insufficiency fractures treated and these were in patients who already had malignant disease elsewhere. The utility of RFA in insufficiency fractures is unclear. The only advantage would be a decrease in cement leaks.
Conclusions
RFA assisted OP and VP using a bipolar RF system is safe and effective. The use of RFA allows for a controlled cement injection into what we postulate could be a thermal cavity with a significant decrease in posterior and venous cement leaks. Rate of cement leakage into the disc spaces was unaffected.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the hospital scientific and ethics committee.
References
- Barr JD, Jensen ME, Hirsch JA, et al. Position statement on percutaneous vertebral augmentation: a consensus statement developed by the Society of Interventional Radiology (SIR), American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS), American College of Radiology (ACR), American Society of Neuroradiology (ASNR), American Society of Spine Radiology (ASSR), Canadian Interventional Radiology Association (CIRA), and the Society of NeuroInterventional Surgery (SNIS). J Vasc Interv Radiol 2014;25:171-81. [Crossref] [PubMed]
- Hoffmann RT, Jakobs TF, Trumm C, et al. Radiofrequency ablation in combination with osteoplasty in the treatment of painful metastatic bone disease. J Vasc Interv Radiol 2008;19:419-25. [Crossref] [PubMed]
- Munk PL, Rashid F, Heran MK, et al. Combined cementoplasty and radiofrequency ablation in the treatment of painful neoplastic lesions of bone. J Vasc Interv Radiol 2009;20:903-11. [Crossref] [PubMed]
- Halpin RJ, Bendok BR, Sato KT, et al. Combination treatment of vertebral metastases using image-guided percutaneous radiofrequency ablation and vertebroplasty: a case report. Surg Neurol 2005;63:469-74; discussion 474-5. [Crossref] [PubMed]
- Schaefer O, Lohrmann C, Herling M, et al. Combined radiofrequency thermal ablation and percutaneous cementoplasty treatment of a pathologic fracture. J Vasc Interv Radiol 2002;13:1047-50. [Crossref] [PubMed]
- Georgy BA, Wong W. Plasma-mediated radiofrequency ablation assisted percutaneous cement injection for treating advanced malignant vertebral compression fractures. AJNR Am J Neuroradiol 2007;28:700-5. [PubMed]
- Klazen CA, Lohle PN, de Vries J, et al. Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet 2010;376:1085-92. [Crossref] [PubMed]
- Gofeld M, Yee AJ, Whyne CM, et al. New Palliative Intervention for Painful Metastatic Bone Disease: The OsteoCool™ System. European Cells and Materials 2012;23:11.
- Woo J, Pezeshki P, Yee AJ, et al. Validation of a novel bone tumor RF ablation system - Physics and animal data. Groupe Rech Interdiscip sur les Biomatériaux Ostéoarticulaires Inject 2011;21.
- Halpin RJ, Bendok BR, Liu JC. Minimally invasive treatments for spinal metastases: vertebroplasty, kyphoplasty, and radiofrequency ablation. J Support Oncol 2004;2:339-51; discussion 352-5. [PubMed]
- Anselmetti GC, Manca A, Ortega C, et al. Treatment of extraspinal painful bone metastases with percutaneous cementoplasty: a prospective study of 50 patients. Cardiovasc Intervent Radiol 2008;31:1165-73. [Crossref] [PubMed]
- Kojima H, Tanigawa N, Kariya S, et al. Clinical assessment of percutaneous radiofrequency ablation for painful metastatic bone tumors. Cardiovasc Intervent Radiol 2006;29:1022-6. [Crossref] [PubMed]
- Proschek D, Kurth A, Proschek P, et al. Prospective pilot-study of combined bipolar radiofrequency ablation and application of bone cement in bone metastases. Anticancer Res 2009;29:2787-92. [PubMed]
- Lane MD, Le HB, Lee S, et al. Combination radiofrequency ablation and cementoplasty for palliative treatment of painful neoplastic bone metastasis: experience with 53 treated lesions in 36 patients. Skeletal Radiol 2011;40:25-32. [Crossref] [PubMed]