The role of clinical hypnosis and self-hypnosis to relief pain and anxiety in severe chronic diseases in palliative care: a 2-year long-term follow-up of treatment in a nonrandomized clinical trial
Introduction
Recent neurophysiologic advances in the application of clinical hypnosis for pain and anxiety management in severe chronic diseases
In severe chronic disease, pain is a significant predictor of anxiety and panic-fear symptoms for the patient. Pain and anxiety are universal human experiences in severe chronic illnesses and are always subjective (1). Pain intensity not only depends on the type of stimulus that caused it, but also on the subjective psychological perception of the pain (2,3). Difficulty in maintaining the balance between adequate pain relief and acceptable tolerability, particularly with strong opioids, can lead to the establishment of a “vicious circle” that alternates between lack of efficacy and unpleasant side effects.
Pain management in patients with severe chronic diseases due to aged heterogeneity, multimorbidity, and polypharmacy involves a selection of treatment in an effort to maximize the patients’ functional abilities, in addition to relieving their pain (4). Pain is a complex phenomenon involving both neurophysiologic and psychological components. The neuromatrix theory of pain proposes that pain is a multidimensional physical and psychosocial experience produced by characteristic “neurosignature” patterns of nerve impulses generated by a widely distributed neural network—the “body-self neuromatrix”—in the brain (5). Pathophysiological pain mechanisms in severe chronic diseases involve neural pathways, and a variety of pain-producing substances and modulating mechanisms. These include acetylcholine, serotonin, histamine, bradykinin, prostaglandins, substance P, somatostatin, cholecystokinin, vasoactive intestinal polypeptide, noradrenaline and endogenous opioid peptides. The opioid system controls pain, reward and addictive behaviors. In severe chronic diseases, chronic pain and anxiety, continually stimulating the fight-or-flight response, leads to the constant production and secretion of catecholamines. This has a variety of physiological concerns, including anxiety. Because some catecholamines, such as norepinephrine, act as neurotransmitters in the brain, these substances can modify cognition and other mental processes (6,7).
Anxiety and the motor, cognitive, and affective areas of the cerebral cortex influence the adrenal medulla in severe chronic diseases. Thus, the cortical areas involved in the control of cognition and sensations affect potential sources of central commands to influence pain perception and sympathetic arousal (7). They suggest that there is a link between the descending control top-down influence and the regulation of sympathetic output in chronic pain and anxiety symptoms (8-11). These researches are important to understand the role of clinical hypnosis to relief pain and anxiety. Chronic pain conditioning is conceptualized as a form of cognitive learning in which subjects come to express responses to neutral conditioned stimuli (CS), which are paired with aversive unconditioned stimuli (US) (7). Because of this pairing, the CS acquires the ability to elicit a spectrum of behavioral, autonomic, and endocrine responses that would normally only occur in the context of danger. Chronic pain conditioning can be adaptive and enable efficient behavior in situations like severe chronic diseases. The long loop pathway indicates that sensory information relayed to the amygdale undergoes substantial higher level processing, thereby enabling the assignment of significance, based upon prior experience of anxiety, to complex stimuli (7,11).
This link could provide a neural substrate for the control of “total pain” in severe chronic diseases and related symptoms through mind-body therapies and exercises, such as relaxation, verbal suggestions, visual imagery, clinical hypnosis and self-hypnosis (8,12-25).
In 2002, National Institutes of Health (NIH) institutes, centers, and offices as well as the Agency for Healthcare Research and Quality asked the Institute of Medicine to convene a study committee to explore scientific, policy, and practice questions that arise from the significant and increasing use of complementary and alternative medicine (CAM) therapies in severe chronic illnesses (26).
In palliative care, we cannot treat only the physical diseases, but we can improve the psychosocial and spiritual well-being of the patients in the context of chronic or life-threatening illness.
Mind-body interventions like clinical hypnosis are practices that focus on the interactions between the brain, body, mind, spirit and behavior, with the intent of using the mind to modify physical function and behaviors and promote overall physical (pain) and psychological (anxiety) health (27). Clinical hypnosis should be part of a multidisciplinary approach and aimed at reducing anxiety and pain. Clinical Hypnosis research binds phenomenology and neuroscience (21). Most researchers leverage bottom-up suppression to unlock the underlying mechanisms of unconscious processing. However, a top-down approach—for example via hypnotic suggestion—paves the road to experimental innovation and complementary data that afford new scientific insights concerning attention and the unconscious (21,28,29).
Hypnosis modulates phenomenological aspects of conscious experience, such as pain perception.
Hypnotic analgesia arguably originates from various factors, including the alteration of expectations relative to impending painful events, as well as attentional, cognitive and emotional regulation mechanisms (29,30). For decades, a large number of studies have provided evidence on the efficacy of clinical hypnosis and self-hypnosis as a psychological intervention and adjuvant therapy, in the treatment of chronic pain and anxiety in severe chronic diseases (31-34).
The research aims
The main purpose of this study was to investigate the efficacy of hypnosis and self-hypnosis in relieving pain and anxiety, as an adjuvant therapy (in addition to pharmacological therapy), in severe chronic diseases for a long-term follow up of 1 and 2 years.
The specific aims of this study were: (I) to measure the influence and efficacy of hypnosis, as an adjuvant therapy, on pain in severe chronic diseases and in palliative care; (II) to measure the influence and efficacy of hypnosis, as an adjuvant therapy, on anxiety symptoms in severe chronic diseases and in palliative care; (III) to study the effectiveness of the use of hypnosis and self-hypnosis in relieving pain and anxiety in severe chronic illnesses and in palliative care for a long-term follow-up (1 and 2 years); (VI) to measure the influence of hypnosis on the long-term use of opioids and analgesic medicines (NSAIDS and Corticosteroids).
Methods
This was a long-term follow-up of 2 years in a nonrandomized clinical trial in patients with severe chronic diseases.
Eligibility criteria for participants
Inclusion criteria
- Gender: both male and female participants were studied;
- Age limit: minimum age 18; no maximum age limit;
- Severe chronic disease: the patients in both groups must have suffered from one of the following severe chronic diseases: (i) cancer (C); (ii) chronic neurological diseases (ND); (iii) chronic rheumatic diseases (CRD);
- All the patients in the two groups were only partial responders to conventional pharmacological therapies (before the study started), but had preferred not to increase the use of medicines. They did not want to use anxiolytics for different reasons (such as driving the car or being always perfectly aware);
- Patients could only be enrolled in the groups if they were only using a pharmacological therapy with NSAIDS, Opioids, and/or Corticosteroids;
- Chronic pain: where they were affected with Chronic pain and intensity Visual Analog Scale (VAS) [0–100] ≥40;
- Anxiety: where they were affected by anxiety evaluated by Hamilton Anxiety Rating Scale (HAM-A) (range 0–56). We included in the study all the patients with a HAM-A in a range 1–56;
- Patients enrolled in the group of hypnosis had to attend at least the 50% of the meeting on hypnosis techniques (they had to sign their attendance);
- Patients enrolled in the two groups had the same type of pain: muscular pain, visceral pain and osteoarthritis pain, but not neuropathic pain (see exclusion criteria).
Exclusion criteria
- Age <18 years;
- Patients must not have had severe cognitive disorders.;
- Patients must not have had major psychiatric disorders, as schizophrenia;
- Patients could not be enrolled if they suffered from neuropathic pain, and they were using Antidepressants or Antiepileptic, because these could compromise the anxiety study;
- Patients could not be enrolled if they were using Antidepressants, Anxiolytics or Antiepileptic, for any concurrent symptom, because these medicines could compromise the anxiety study;
- Patient could not be enrolled if they were using additional therapies and not only medicines, for example, psychotherapies or anesthesiology blocks (these therapies could compromise the pain and anxiety study);
- Inability to perform informed consent;
- Patients with a life expectation of less than 1 year (one of the aims of the study was a long-term follow-up of 2 years).
The recruitment procedure
This was a non-randomized clinical trial. Participants could choose which group they wanted to be in: this was an ethical choice of the authors, considering that all the patients had severe chronic illnesses and some of them were approaching the end of life. Although randomization is preferable because it helps check for factors other than the intervention that may be responsible for differences in outcomes, non-randomized assignment may be necessary when randomization is not feasible or ethical. The specific purpose of this sequential clinical trial was to compare the two treatments (the group with hypnosis as an adjuvant therapy and the group without hypnosis) as data became available after the follow-up (1 and 2 years).
The effect of the intervention was evaluated by comparing the group of subjects receiving a standard pharmacological intervention (control group) to the group receiving hypnosis as an adjuvant therapy in addition to the standard pharmacological intervention.
This study started on January 2014 at the University of Verona and was approved by the Institutional Review Board. All patients provided written informed consent.
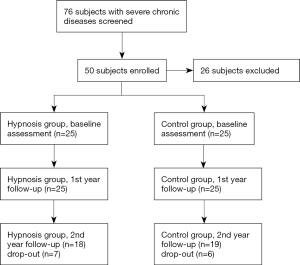
During the first six months, we screened 76 patients with severe chronic illnesses. Only 56 entered in the inclusion criteria and 6 declined to participate in the study.
Figure 1 shows the recruitment procedure and the progress flow chart through the phases of each group’s parallel trial.
Study design
The patients enrolled in our in our study was suffering from the following severe chronic diseases: (I) cancer; (II) neurological severe chronic diseases; (III) rheumatic severe chronic diseases.
We studied 50 patients, divided into two groups (hypnosis and control groups).
Measuring instruments
After the workshop introduction, the demographic data and VAS and HAM-A pre-tests were explained and administered to the two groups to assess the study of baseline.
After the last educational hypnosis session on the final day (after 1 and 2 years), all the participants of both groups were asked to complete the first (1 year) and the second (2 years) follow-up with the post-test VAS and HAM-A questionnaires.
The principal investigator (PI) evaluated (mg/day) the use of the opioids and pharmacological analgesic therapies (NSAIDS and Corticosteroids) for every patient on the medical records at baseline, after 1 year and after 2 years.
The evaluations for pain and anxiety were performed with the validated tests:
- VAS for pain evaluation;
- HAM-A for anxiety evaluation.
The VAS for pain evaluation
The VAS is one of the most commonly used instruments for measuring pain intensity in pain research. For pain intensity, the scale is most commonly anchored by “no pain” (score of 0) and “pain as bad as it could be” or “worst imaginable pain” [score of 100 (100-mm scale)].
Administration method. The VAS pain evaluation is self-completed by the respondent.
Score interpretation: no pain (0–4 mm), mild pain (5–44 mm), moderate pain (45–74 mm), and severe pain (75–100 mm). A higher score indicates greater pain intensity (35).
HAM-A
The purpose of this validated, clinician-rated evaluation is to analyze the severity of anxiety. The scale consists of 14 items. Each of the 14 items contains a number of symptoms (anxiety related symptoms) and each group of symptoms is rated on a scale of 0 to 4, with 4 being the most severe. The total comprehensive score is in the range of 0 to 56. It is pre-established that the results of the evaluation can be interpreted as follows: a score of 17 or less indicates mild anxiety severity; a score from 18 to 24 indicates mild to moderate anxiety severity and, lastly, a score of 25 to 30 indicates a moderate to severe anxiety severity (36,37).
Treatment procedures
We organized two groups, each with 25 patients suffering from severe chronic illnesses, evolving into pain and anxiety. All the patients of both groups, were treated as outpatients referred to the Pain Therapy Clinic with conventional pharmacological therapy (Opioids, NSAIDS and Corticosteroids). All the participants of the two groups, attended a 2-hour workshop with PI, which explained the meaning of clinical hypnosis in palliative care for pain and anxiety relief, and they choose which group to attend (hypnosis or non-hypnosis).
The adjuvant hypnosis therapy was added to the hypnosis group through a group therapy with clinical hypnosis and self-hypnosis, visualizations, metaphors and relaxing music.
At the first workshop with the hypnosis’ group, the PI covered the explanations for the skills and effective instructional practices and techniques.
- The overall goal of the treatment with adjuvant hypnosis was to teach the hypnosis group patients clinical hypnosis and self-hypnosis as an adjuvant therapy to their pharmacological therapy in order to relieve pain and anxiety;
- The techniques of clinical hypnosis and self-hypnosis used in this study are explained in the Supplementary;
- The treatment lasted 2 years;
- For 2 years, a series of weekly, 2-hour workshops were conducted on chronic pain assessment and the management of anxiety and related symptoms, directly teaching the hypnosis group patients how to use hypnosis and self-hypnotic techniques;
- The hypnosis group had to attend 50% of the sessions in 1 year, for 2 years;
- The treatment meetings were held in the meeting room at the Department of Anesthesia, Intensive Care and Pain Therapy at the University of Verona, Italy where the participants could be induced into hypnosis while sitting in their chairs;
- The control group (no hypnosis) was only treated with conventional pharmacological therapy (Opioids, NSAIDS and Corticosteroids) (see exclusion criteria).
Statistical analyses
Data were summarized with means ± standard deviation (SD) or number (percentage), as appropriate. Comparisons of variables between groups were performed using the Person’s chi-squared, the Student’s t, or the Wilcoxon’s rank-sum tests, accordingly to the distribution of each variable. Longitudinal scores of VAS and Hamilton were analyzed using repeated measures ANOVA, for testing the effectiveness of the treatment and its potential interaction with the type of chronic disease. Statistical analyses were performed using STATA 14.1.
Results
Demographic data and characteristics of the two groups at baseline
Fifty subjects—14 men and 36 women—participated to the study. The average age of the subjects was 64 years, ranging from a minimum of 33 to a maximum of 93 years. The patients suffered from 3 main types of disease:
- Rheumatic severe chronic diseases (rheumatoid arthritis and autoimmune rheumatic diseases) (n=21);
- Neurologic severe chronic diseases (Multiple sclerosis; Parkinson’s disease; Spinal cord injuries—ASIA B is having some sensory function below the injury, but no motor function; ASIA C is having some sensory function below the injury, some motor function below level of injury, but half the muscles cannot move against gravity—American Spinal Injury Association classification) (n=16);
- Oncologic (breast cancer, colon cancer, leukemia and lymphoma) (n=13).
Half of the patients (n=25) were assigned to the group administered with the hypnotic protocol (hypnosis group), while the remaining 25 followed conventional pharmacological pain therapies (control group). The patients could have chosen if use clinical hypnosis as adjuvant therapy or not. The two groups were homogeneous in the distribution of sex, age, type and subtypes of diseases, and use of opioids at baseline (Table 1).
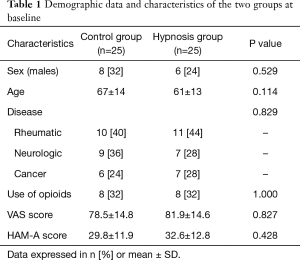
Full table
Data were summarized with SD or number (percentage), as appropriate. Accordingly, to the distribution of each variable, comparisons of variables between the two groups were performed by the chi-squared or the Wilcoxon rank-sum tests.
The two groups were homogeneous in the distribution of sex, type of disease, and use of opioids at baseline (Table1). The patients of the hypnosis group were slightly younger, even if not statistically significantly, than the control group.
One-year follow-up
Examining the 1-year follow-up (n=50), the measurement methods at first follow-up included VAS, HAM-A and the use of opioids. After 1-year follow-up, there were no drop-outs.
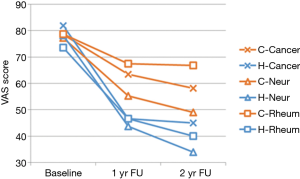
The VAS score at baseline was similar for both the hypnosis and control groups (data expressed in mean ± SD: 81.9±14.6 and 78.5±14.8 respectively); after 1 year, the score decreased in both groups compared to the baseline score and was significantly lower in the hypnosis group compared to the control group (45.9±13.8 and 62.1±15.4, respectively) (Figure 2, Table 2).
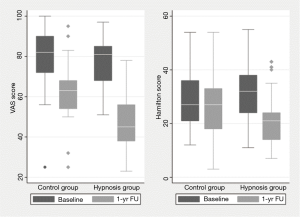
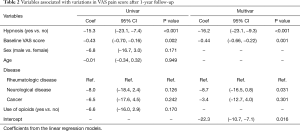
Full table
The mean VAS score reduction was significantly greater after 1 year in those subjects who were treated with the hypnotic therapy compared to those who were not (ΔVAS =−15.3, P<0.001). This association was confirmed in multivariate analysis, after controlling for sex, age, type of disease, use of opioids, and VAS score at baseline (Figure 2, Table 2).
Table 2 represents the associations of the variables with the reduction in VAS score after 1-year follow-up. The administration of hypnotic therapy and the VAS score at baseline were significantly associated with the change in VAS score after 1 year in univariate analysis. Sex and age of the patient and the use of opioids were not associated with a significant decrease in VAS score. In multivariate analysis, treatment with hypnosis was associated with a greater decrease of 16.2 points compared to the control group (P<0.001) independently of the score at baseline and type of disease. Moreover, the decrease in VAS score was greater in patients with neurologic disease compared to patients with rheumatic disease and cancer.
The HAMA Hamilton anxiety score at baseline was similar for both the hypnosis and control groups (32.6±12.8 and 29.8±11.9 respectively) but decreased to 22.9±11.2 and 26.1±12.6 after 1-year follow-up. The score decreased in both groups compared to the baseline score and was significantly lower in the hypnosis group compared to the control group (ΔHAM-A =−9, P<0.001). This association was confirmed in multivariate analysis, after controlling for sex, age, type of disease, use of opioids, and VAS score at baseline (Figure 2, Table 3).
Table 3 represents the associations of the variables with the reduction in HAM-A score after 1 year of follow-up. In univariate analysis, the assigned therapy group was the only variable significantly associated with the change in Hamilton score after 1 year, compared to the control group (P<0.001). Sex and age of the patient, use of opioids, or type of disease were not associated with a significant decrease in the HAM-A Hamilton score. In multivariate analysis, the treatment with hypnosis was associated with a greater decrease of 7 points compared to the control group, independently from the score at baseline.
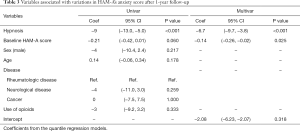
Full table
After 1-year follow-up, we statistically and clinically observed significant reductions in pain (VAS) and anxiety (HAM-A) symptoms in all the individuals in the hypnosis group ( Figure 2). As we can observe in the statistical study in Tables 2 and 3, the reduction was independent of sex, age, diseases or the use of opioids.
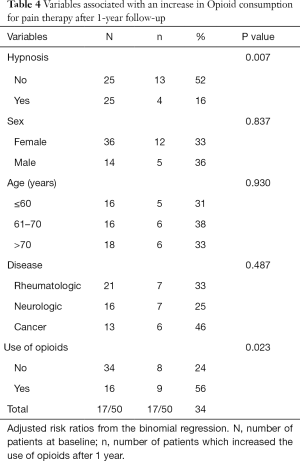
At 1-year follow up, we measured the increase (mg/day) of opioids in the 2 groups.
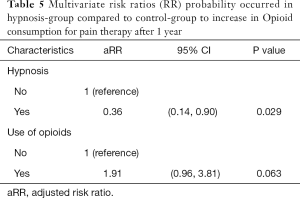
Only 4/25 (16%) of the subjects included in the hypnosis group had to increase the opioids treatment for pain control after 1 year, compared to 13/25 (52%) of the subjects in the control group (P value for difference =0.007) (Table 4). This finding was confirmed in multivariate analysis [adjusted risk (aRR): 0.36; P=0.029] (Table 5).
Full table
Full table
On the other hand, 56% of the subjects who were administered with opioids at baseline had to increase the opioids’ therapy, compared to 24% of the subjects who were not administered with opioids (P value =0.023).
In Table 5 we have studied the relative risk, or RR that is the probability occurred in hypnosis-group compared to control-group to increase in opioid consumption for pain therapy after 1 year.
In multivariate analysis, the hypnosis therapy was associated with a decreased risk of −66% of needing to increase the opioids treatment for pain control (P=0.03) and subjects who were treated with opioids at baseline had a 90% greater risk of increasing the opioids treatment compared to subjects who did not assume opioids (P=0.063).
Two-year follow-up
Drop-out at 2-year follow-up
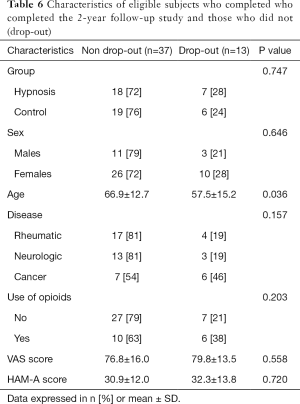
After 2 years, we had a total of 13 drop-outs in the two groups: 7 drop-outs in the hypnosis group; 6 drop-outs in the control group.
Cause of drop-out: cancer—6 cancer patients died of cancer—1 died of breast cancer, 1 died of colon cancer in the control group; 2 died of breast cancer, 2 died of leukemia in the hypnosis group.
Neurological diseases
Two patients with multiple sclerosis dropped out from the control group and 1 from the hypnosis group.
Three patients with neurological diseases (multiple sclerosis) suffered an increase in the severity of the diseases and could no longer come to the hospital. They could not attend the hypnosis group and the control group patients could not come to the hospital for the follow-up.
Rheumatic diseases
Four patients with rheumatic diseases dropped out: 2 suffered an increase in the severity of the diseases and could not come to the hospital for the treatment with hypnosis and follow-up: these patients were part of the hypnosis group.
One patient from the control group decided to use anxiolytics and moved into the exclusion criteria; one patient from the control group suffered an increase in the severity of the disease and could not come to the hospital for the follow-up.
Table 6 shows the Characteristics of eligible subjects who completed the 2-year follow-up study and those who did not (drop-out).
Full table
Almost 20% of subjects with neurologic and rheumatic diseases and about 50% with cancer diseases had dropped out at the 2-year follow-up.
The subjects who dropped out were, on average, younger. Furthermore, there were no significant statistical differences between subjects that completed the study and those who did not complete the 2-year follow-up associated with sex, age and baseline score for VAS and HAMA (Tables 6,7).
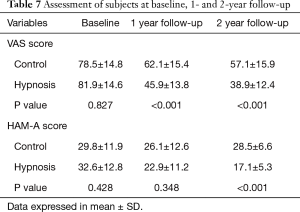
Full table
The P values indicated in Table 7 refer to the comparison between the two groups: they indicate that both the hypnosis and control groups had significantly different scores for VAS after 1 and 2 years. The same can be said of the Hamilton score.
The VAS score at baseline was similar for both the hypnosis and control groups (78±16 and 77±14, respectively).
The VAS average for the hypnosis group decreased from 81.9±14.6 at baseline to 45.9±13.8 at 1-year follow-up, to 38.9±12.4 at 2-year follow-up. The VAS average for the control group decreased from 78.5±14.8 at baseline, to 62.1±15.4 at 1-year follow-up, to 57.1±15.9 at 2-year follow-up.
Variance analysis indicates that the decrease in perceived pain (VAS) was more significant for patients in the hypnosis group than in the control group, after both 1- and 2-year follow-up (P=0.0001). The HAM-A average decreased from 32.6 at baseline to 22.9 and 17.1 respectively at 1- and 2-year follow-up for the hypnosis group but it remained almost the same in the control group (29.8, 26.1 and 28.5 at baseline, 1st and 2nd year respectively).
ANOVA showed that the difference between the two groups was statistically significant (P<0.0001). The change in VAS and the change in Hamilton did not highlight a significant interaction between the treatment group and the type of chronic disease suffered by the patients. This indicates that the effect of hypnosis is not different in people with cancer, chronic rheumatic diseases and chronic neurological diseases.
Figures 3,4 demonstrate a significant decrease for pain and anxiety, for all diseases, in the hypnosis group compared to the control group at 1- and 2-year follow-up.
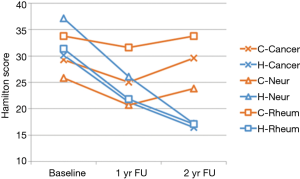
In Figure 4, we can observe that, for all diseases, there was a significant decrease in Hamilton score for the patients in the hypnosis group, while the score remained stable in the control group.
Use of opioids and analgesic medicines (NSAIDs and Corticosteroids) at 2-year follow-up
After the drop-out at the 2-year follow-up, we no longer had a statistically significant number of patients using opioids to study the increment of only opioids in each of the two groups (Table 6). We decided to study (on the medical records of all the patients) the increment (mg/day) from baseline to 2 years, in the use of all the analgesic medicines: Opioids, NSAIDs and Corticosteroids (see exclusion criteria for other types of medicines) (Table 8); from a statistical point of view, we have studied also: time at risk (person-months).
From baseline to 2 years: 16 patients out of 25 (64%) in the control group and 5 out of 25 (20%) in the hypnosis group had increased the use of analgesic medicines (opioids, NSAIDs drugs and Corticosteroids) during the 2 years FU (Chi-squared test: P value=0.002).
The value-at-risk calculated time was 348 and 462 months in patients for the control group and hypnosis group, respectively.
The increase rate in pharmacological therapy was 4.6 subjects/100/months in the control group, while it was 1.1 subjects/100/months in the hypnosis group; the risk of increasing the analgesic therapy (opioids, NSAIDs drugs and Corticosteroids) was 4-times higher (P=0.005) in the control group than in the hypnosis group (IRR: 4.25; 95% CI: 1.55–11.6).
The other variables significantly associated with an increase in analgesic therapy (opioids, NSAIDs drugs and Corticosteroids) were the use of analgesic therapy at baseline (IRR: 3.18; 95% CI: 1.35–7.49; P=0.008) and the VAS score at baseline (IRR: 1.06; 95%CI: 1.02–1.10; P=0.003), while HAM-A score for anxiety was not associated (IRR: 1.01; 95% CI: 0.97–1.04; P=0.759).
The adjusted incidence rate ratio IRR for the use of analgesic medicines (opioids, NSAIDs drugs and Corticosteroids) and VAS at baseline confirms the univariate analysis that shows a 4-times greater risk of an increase in analgesic medicines in the control group (adj.IRR: 4.36; 95% CI: 1.59–12.0) (Table 8).

Full table
Discussion
During acute and chronic pain in severe chronic diseases, stress and anxiety can aggravate certain features of situations or arguments and place greater psychological weight on the patients’ daily experiences (38). As reported by Mitchell et al. (39), a number of data have been studied regarding anxiety screening and therapy in palliative care. Patients may acquire psychological and behavioral aspects of their pain problems and psychosocial disorders among cancer patients have been reported as a major consequence of the disease and treatment (39). The implications and the impact of pain and anxiety for the patients and their families are of paramount importance in oncology, in severe chronic diseases and in patients receiving palliative care. Studies have demonstrated the association of psychosocial morbidity with maladaptive coping, impairment in social relationships, longer rehabilitation time, poor adherence to treatment, abnormal illness behavior, family dysfunction and, possibly, shorter survival (40). Palliative care aims to provide the maximum possible comfort to people with advanced and severe chronic diseases. The use of non-pharmacological interventions to promote pain and anxiety relief and comfort in palliative care settings has been increasing. However, information on implemented and evaluated interventions, their characteristics, contexts of application and population is scattered in the literature (41). This study confirms researches that have reported the beneficial effects of clinical hypnosis in pain and anxiety relief in palliative care (42-45).
Hypnotizability, which is the capacity to experience a transition into a hypnotic state and to perform hypnotic tasks, has a wide range of degrees from difficulty to be hypnotized at all to being able to respond with intriguing and even surprising intensity to hypnotic instructions.
A recent definition of hypnosis from Division 30 of the American Psychological Association emphasizes that hypnosis does involve an altered state of consciousness including absorption, dissociation and an enhanced capacity to respond to suggestions (46).
Previous studies on hypnotizability using the Minnesota Multiphasic Personality Inventory and other similar personality tests have failed to show any correlation with available hypnotizability scales (47,48). Essential features of clinical hypnosis include the therapist’s expertise and the patient’s focused attention and absorption, which take the subject into a physiological modified state of consciousness on competing stimuli and thoughts (47). Furthermore, if hypnotizability is a stable capability, it should be theoretically possible to test even outside of hypnotic induction profiles (47,48). To summarize, there is a need to reappraise the concepts of hypnosis, hypnotizability and its scales after some half century since their introduction. This might lead to a better understanding of hypnosis, more congruent with a neurophysiological and cognitive perspective (48). In our research, we decided, as other authors have done in clinical studies of hypnosis (48), not to use any hypnotic induction profile in order to respect the patients. In our study 11/25, patients of the control group (no-hypnosis) refused any hypnotic induction profile for hypnotizability.
Interestingly, although patients may not feel psychological symptoms of anxiety as their top concern, these are the most impacted symptoms in severe chronic diseases, as we have observed at baseline, with the HAM-A questionnaire in both the two groups.
There are a number of important clinical implications in the research findings regarding the effects and mechanisms of hypnosis on anxiety and pain (18,19,28,33,34,43,45). Firstly, there is considerable evidence that hypnosis is an effective treatment for chronic pain, coupled with its cost-effectiveness and minimal side effects. In fact, none of our patients in the hypnosis group reported any side effects.
Secondly, we founded a significant statistical decrease in reported pain and anxiety among patients with advanced diseases receiving clinical hypnosis as an adjuvant therapy to analgesic medicines (opioids, NSAIDs drugs and Corticosteroids) compared to patients who were receiving analgesic pharmacological therapy only. Therefore, we can reject our null hypothesis, which stated that there would be no difference between the intervention group and the control group.
To the best of our knowledge, this is the first study to show that, despite difficulties in recruitment and relatively high dropout rates, it is possible to perform a long-term (2 years) intervention with clinical hypnosis and self-hypnosis, which can be considered significant for patients receiving palliative care for relieving pain and anxiety. The statistically and clinically significant reductions in pain (VAS) and anxiety (HAM-A) symptoms experienced by every member of the hypnosis group was independent of their sex, age, diseases or the use of analgesic medicines (opioids, NSAIDs drugs and Corticosteroids). Subjects in the hypnosis group were at lower risk of increasing analgesic pharmacological treatment for pain control. Univariate analysis demonstrated a 4-times greater risk of increasing analgesic medicines (opioids, NSAIDs drugs and Corticosteroids) in the control group after 2 years of treatment.
The current study developed knowledge of hypnosis treatment in palliative care in different aspects: mainly, with hypnosis and self-hypnosis techniques, we were able to replicate the positive impact of the treatment on the participants’ ability to initiate and maintain pain and anxiety relief. Thus, the hypnosis treatment turned out to be effective, even without a therapist, by practicing self-hypnosis at home. This is of course essential for its implementation in clinical practice, especially in palliative care. Our results imply that, in the future, clinical psychologists, psychotherapists and hypnosis practitioners will be able to successfully integrate hypnosis treatment into palliative care. This suggests that hypnosis treatment represents a promising and a well-accepted intervention in populations with severe chronic diseases receiving palliative care.
Finally, the 1- and 2-year follow-up demonstrated long-term stability of the treatment effects.
In conclusion, this is the first completed 2-year, long-term study on the use of clinical hypnosis and self-hypnosis in palliative care with outcome measures that are clinically relevant.
Self-hypnosis was managed directly and easily with the patients and they were able to not only experience pain and anxiety relief, but also some of them, also mentioned reaching a psychological wellbeing and psychosocial and spiritual healing at the end of life.
Another clinical implication is that when using hypnosis or teaching patients self-hypnosis for pain management, clinicians should use a variety of suggestions that target improvement in the multiple components of pain (e.g., sensory, affective, cognitive, motivational). We have explained the detailed techniques in the Supplementary.
Pain and anxiety are the most frequent stress-response problems in palliative care (44).
The patient’s chronic pain and anxiety should always be acknowledged as a real physiologically existent problem with biochemical changes for the patient. We have to consider the “reality” of their suffering. Saunders [1996] observed that the whole experience of a patient’s life was reflected in that patient’s disease, suffering, and dying (49). She advocated the concept of “total pain” as a complex blend of physical, emotional, social and spiritual factors. In her view, total pain can include not only physical pain but also psychological pain (e.g., anxiety, psychosomatic disorders, and fear), social pain (e.g., concern for their family, including bereavement), and/or spiritual pain at the end of life (49).
The patients in the hypnosis group in this study could appreciate that a pharmacological solution, such as the use of analgesic medicines, was not the only one therapy for their symptoms and were therefore willing to undergo physical and psychological care with hypnosis and self-hypnosis.
Many factors may contribute to the symptoms in severe chronic diseases. Chronic anxiety may be a condition in which the patients use the language and behavior of pain to communicate their distress in severe chronic diseases. Hypnosis selectively targeted and modified perception of sensory events and even temporarily abolished co-occurrences of secondary sensory experiences in synesthetes (21,22,29,30). We used these properties of hypnosis on perceptions (21,30) to modulate acute and chronic pain and anxiety. Clinical hypnosis could have modified the perception of physical pain perceptions and addressed pain relief. Indeed, the use of clinical hypnosis may not only relieve anxiety, but could also create an empathetic and compassionate relationship with therapists.
Although response to hypnosis and training in self-hypnosis were variable in all our patients, the available clinical evidence indicated that hypnosis could significantly not only reduce the average daily pain, anxiety and use of medicine, but also all patients reported a personal, increased comfort. Hypnosis resulted in benefits in other suffering-related outcome domains for many individuals: many patients in the hypnosis group described an increase in energy, improved sleep, improved resilience, well-being, self-growth, increased hope and awareness for inner spirituality at the end of life. Therefore, clinicians who treat patients with chronic ‘total pain’, receiving palliative care, would do well to consider learning and incorporating hypnotic techniques into their practice.
At the end of their life, people in the hypnosis group told us that, during self-hypnosis, they had reached a sense of inner peace, acceptance and spiritual healing. This sense of spiritual wellbeing and healing helped the patients and their families near death.
The goal of palliative care is to relieve the suffering of patients and their families through the comprehensive assessment and treatment of the physical, psychosocial, and spiritual symptoms that the patients are experiencing. As death approaches, ‘total pain’ and suffering requires greater effort from clinicians and families alike. Palliative care focuses primarily on anticipating, preventing, diagnosing and treating symptoms experienced by patients with a serious or life-threatening illness and helping patients and their families make important medical, psychological and spiritual decisions. It can be concluded that hypnosis is a reasonable approach for clinicians to use not only for helping patients to cope better with chronic pain, anxiety and reduce the use of analgesic medicines for pain relief, but also for a compassionate palliative care, that will foster growth in dignity and transcendence. With self-hypnosis, we can cultivate inner spiritual positive mental states like kindness and compassion at the end of life, which definitely lead to better suffering relief and psychological and spiritual healing. Pope Francis wrote: “When (a person’s) life becomes very fragile and the conclusion of his earthly existence approaches, we feel the responsibility to assist and support her/him in the best way possible.” (50).
Limitations
Despite considerable difficulties in recruitment, the intended sample size was nearly reached, although over a longer period of time and with delimited inclusion criteria.
- We would have preferred to have organized a randomized trial, however, after an initial short period of randomization, many patients asked to change the therapy group: some patients at the end of life wanted to learn hypnosis to improve their relief from suffering, while others preferred to avoid hypnosis. We ethically decided to respect the motivations of the patients with severe diseases and at the end of life, and the study was not randomized;
- We know that chemotherapy regimens that utilize combination therapy may potentiate or decrease the physical pain perceived by patients via different mechanisms of action. We could not study this variable especially since it is related to many different and multiple chemotherapy variables. In any case, in our study, all the cancer patients that were included in the two groups received chemotherapy during the 2-year study and the number of cancer patients in the two groups was homogeneous;
- Our cohort was small and heterogeneous and the number of the patients receiving palliative care was too small to draw conclusions on “all” palliative care patients.
Conclusions
Our work demonstrated that clinical hypnosis is an emerging field for pain and anxiety relief as adjuvant therapy to medicines in Palliative Care. Future researches and care models should therefore explore the beneficial as well as the potentially harmful aspects of clinical hypnosis within advanced care in severe chronic diseases, thereby focusing on:
- Ways to optimize multidisciplinary care by adopting clinical hypnosis as an adjuvant therapy;
- The use of hypnosis and self-hypnosis as adjuvant therapy for patients with advanced severe diseases.
- Our suggestion for future researches is also to compare clinical hypnosis with a group of patients treated with an adjuvant psychotherapy;
- The development of trials to investigate long-term outcomes of clinical hypnosis in Palliative Care with appropriate comparison groups are required;
- More researches on the effects and effectiveness of hypnosis are needed in Palliative Care;
- Another important reflection considering clinical hypnosis is the goal of the treatment. While our goals were to decrease the intensity of pain, anxiety and the use of analgesic medicines, an arguably important goal may be to increase the quality of life, returning to work or improving function in daily activities or in psycho-social and spiritual healing;
- We suggest collaboration for multi centric researches on clinical hypnosis in Palliative Care.
These issues should be adequately addressed, both in future researches and in implementation trajectories regarding the use of clinical hypnosis as an adjuvant therapy in Palliative Care.
Supplementary
Clinical hypnosis and self-hypnosis techniques for pain and anxiety relief in patients receiving palliative care
Clinical hypnosis can be described as a cognitive process of sustained attention and awareness towards present-moment sensations and experiences with visual imagery and deep emotional regulation. Clinical hypnosis is considered as a means of achieving pain and anxiety relief and well-being, and, if practiced properly, can improve psychological health. Some treatments for anxiety incorporate aspects of the practice of clinical hypnosis and show beneficial effects on treatment outcomes. Nowadays, researches into hypnosis suggest that it influences anxiety symptoms through emotional regulatory mechanisms (rumination, reappraisal, worry and non-acceptance) by considering emotional regulation as a path through which clinical hypnosis stimulates mental health (31,38). The clinical hypnosis techniques used in this research during 2 years of hypnotic training for the hypnosis group are outlined below. We taught different techniques and the patients could decide whether to use just one or several of the preferred self-hypnosis techniques at home. With clinical hypnosis, we can teach the patient to feel different pleasant sensations rather than pain or anxiety.
The different interpretation of symptoms technique
When a state of a lighter or deeper relaxation and hypnosis is achieved with different techniques, the patient is trained to interpret the feeling of chronic pain coming from a specific place in the body. We can transform it slowly from a feeling of pain to a feeling of a different nature: for example, a pleasant tension, a pleasant pressure, a pleasant warmth or a pleasant cold sensation of an anesthetizing nature.
Example of anesthesia in one hand
“… While in a state of relaxation, you can imagine immersing your hand in a container of melting ice cubes and from the wrist up to the tip of your fingers the ice acts on your hand like a very pleasant and powerful anesthesia … making it feel more and more insensitive. You will feel your hand becoming pleasantly cold and pleasantly insensitive … and the anesthesia will increase. You will also know that the anesthesia will last until you say ‘Everything is normal’ to yourself three times.”
Exercise “warm hands” (or for different parts of the body)
Some people prefer to feel a pleasant sensation of warmth.
Duration: 5 or even only 3 minutes.
During this exercise you will repeat to yourselves: “my hands are pleasantly warm”
During the period of “deep relaxation “you will imagine holding your hand in front of the pleasant warmth of flames from an open oven, or under a solar lamp (UVB lamp), or immersed in pleasantly hot water or any other thought of this kind that might come easy to you.
The transferred symptoms technique
After achieving relatively strong analgesia in a certain part of the body with the techniques described above, you aim to mentally transfer the analgesia to another part of the body (for instance, from the hands to the abdomen or to the back) obtaining this way a gradual and progressive reduction of overall suffering ….in a state of well-being…serenity… and peace.
The positive visualization technique (for pain and anxiety relief)
When the patient is in a state of relaxation or in a medium hypnotic state, you introduce particular visualizations that will, after a certain time, cause a greater feeling of visualization, which is capable of modifying the painful and/or anxiety information in the central nervous system, and therefore, reduce the patient’s suffering. We can help the patient by teaching him to visualize himself in a beautiful and serene place: “Peace is present right here and now, in ourselves and in everything we do and see. Every breath we take, every step we take, can be filled with peace, joy, and serenity”.
The desensitization of pain and anxiety technique
During a deep hypnotic state, the patient does not seem to react to the surrounding environment and usually seems to be less sensitive to painful stimulation. This happens even when some or all of the reflexive or vegetative signs of the painful stimulation are present.
The best use for this technique, therefore, is to induce deep relaxation up until the unconscious can register and activate a minor sensitivity to pain, through hypnotic suggestion, for a longer time, even in a state of normal awakening,
The aim of this technique is to diminish anxiety connected with pain, in the case of headaches, for example, where, besides the body pain, a great emotional dysfunction also arises, or in the case of a phantom arm or leg after amputation of an arm or leg, or in the chronic pain of cancer patients.
The methods most used during the state of deep relaxation or hypnosis are:
- Direct instructions for pain reduction;
- The use of metaphors;
- Transportation of the painful symptom;
- Detachment from pain through metaphors, resilience, self-compassion, imagination.
Self-hypnosis technique for pain and anxiety relief
Self-hypnosis is the way to use hypnosis alone, without the therapist.
Steps commonly used for self-hypnosis: self-hypnosis requires some distinct steps.
- Step 1: motivation. Without proper motivation, an individual will find it very difficult to practice self-hypnosis;
- Step 2: relaxation of the body and mind. The individual must be thoroughly relaxed and must set aside time to perform this act. Additionally, distractions should be eliminated as full attention is needed;
- Step 3: concentration. The individual needs to concentrate completely as energy is generated each time the mind focuses on a single image (23-25).
The self-hypnosis CD method
This consists of simply recording (by the therapist) the desired suggestion on a CD, and then giving the CD to the patient to listen to for self-hypnosis. This will be very effective for people that have difficulty in visualizing.
Self-hypnosis is one of the most efficient techniques for pain and anxiety relief and is carried out using different techniques:
- You are experiencing a pleasant feeling in deep relaxation: inner peace, serenity, compassion, happiness…
- You mentally connect this feeling to your symptoms… that are decreasing more and more…
- You are using it mentally to cancel your symptoms…
…The most efficient way to achieve this feeling is to repeat this self-introspective-hypnosis until you achieve your goal and sometimes this will take quite a while.
Acknowledgements
The authors would like to express their immense gratitude to all the patients with severe chronic diseases who participated in this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study started on January 2014 at the University of Verona and was approved by the Institutional Review Board. All patients provided written informed consent.
References
- Bonica JJ. The need of a taxonomy. Pain 1979;6:247-8. [Crossref] [PubMed]
- Almarzouki AF, Brown CA, Brown RJ, et al. Negative expectations interfere with the analgesic effect of safety cues on pain perception by priming the cortical representation of pain in the midcingulate cortex. PLoS One 2017;12:e0180006. [Crossref] [PubMed]
- Vadivelu N, Kai AM, Kodumudi G, et al. Pain and Psychology-A Reciprocal Relationship. Ochsner J 2017;17:173-80. [PubMed]
- Schmader KE, Baron R, Haanpää ML, et al. Treatment considerations for elderly and frail patients with neuropathic pain. Mayo Clin Proc 2010;85:S26-32. [Crossref] [PubMed]
- Melzack R. Evolution of the neuromatrix theory of pain. The Prithvi Raj Lecture: presented at the third World Congress of World Institute of Pain, Barcelona 2004. Pain Pract 2005;5:85-94. [Crossref] [PubMed]
- Steckler T, Holsboer F. Corticotropin-releasing hormone receptor subtypes and emotion. Biol Psychiatry 1999;46:1480-508. [Crossref] [PubMed]
- Dum RP, Levinthal DJ, Strick PL. Motor, cognitive, and affective areas of the cerebral cortex influence the adrenal medulla. Proc Natl Acad Sci U S A 2016;113:9922-7. [Crossref] [PubMed]
- Varga K, Kekecs Z. Oxytocin and cortisol in the hypnotic interaction. Int J Clin Exp Hypn 2014;62:111-28. [Crossref] [PubMed]
- Astin JA, Shapiro SL, Eisenberg DM, et al. Mind-body medicine: state of the science, implications for practice. J Am Board Fam Pract 2003;16:131-47. [Crossref] [PubMed]
- Tononi G, Koch C. Consciousness: here, there and everywhere? Philos Trans R Soc Lond B Biol Sci 2015;370:20140167. [Crossref] [PubMed]
- Blair HT, Schafe GE, Bauer EP, et al. Synaptic plasticity in the lateral amygdala: a cellular hypothesis of fear conditioning. Learn Mem 2001;8:229-42. [Crossref] [PubMed]
- Brugnoli MP. Clinical Hypnosis and Relaxation in Surgery Room, Critical Care and Emergency, for Pain and Anxiety Relief. J Anesth Crit Care Open Access 2014;1:00018.
- Brugnoli MP. Clinical hypnosis for palliative care in severe chronic diseases: a review and the procedures for relieving physical, psychological and spiritual symptoms. Ann Palliat Med 2016;5:280-97. [Crossref] [PubMed]
- Willmarth EK. Clinical hypnosis in pain therapy and palliative care: A handbook of techniques for improving the patient's physical and psychological well-being by Brugnoli, Maria Paola. Am J Clin Hypn 2017;59:318-20. [Crossref] [PubMed]
- Barber TX, Spanos NP, Chaves JF. Hypnotism: Imagination & Human Potentialities. New York: Pergamon Press, 1974.
- Kohen DP, Kaiser P. Clinical hypnosis with children and adolescents-what? why? how?: origins, applications, and efficacy. Children (Basel) 2014;1:74-98. [Crossref] [PubMed]
- Grinder J, Bandler R. Patterns of the Hypnotic Techniques of Milton H. Erickson: Volume 1. Capitola: Meta Publications, 1975.
- Hammond DC. Hypnosis in the treatment of anxiety- and stress-related disorders. Expert Rev Neurother 2010;10:263-73. [Crossref] [PubMed]
- Kleinbub JR, Palmieri A, Broggio A, et al. Hypnosis-based psychodynamic treatment in ALS: a longitudinal study on patients and their caregivers. Front Psychol 2015;6:822. [Crossref] [PubMed]
- Lankton S. Special issue on placebo, hypnosis, and antidepressants. Am J Clin Hypn 2013;55:207-8. [Crossref] [PubMed]
- Raz A. Hypnosis: a twilight zone of the top-down variety. Few have never heard of hypnosis but most know little about the potential of this mind-body regulation technique for advancing science. Trends Cogn Sci 2011;15:555-7. [Crossref] [PubMed]
- Raz A. Attention and hypnosis: neural substrates and genetic associations of two converging processes. Int J Clin Exp Hypn 2005;53:237-58. [Crossref] [PubMed]
- Robertson D. The practice of cognitive-behavioural hypnotherapy: a manual for evidence-based clinical hypnosis. London: Karnac, 2012.
- Sepúlveda C, Marlin A, Yoshida T, et al. Palliative care: the World Health Organization's global perspective. J Pain Symptom Manage 2002;24:91-6. [Crossref] [PubMed]
- Anbar RD, Linden JH. Understanding dissociation and insight in the treatment of shortness of breath with hypnosis: a case study. Am J Clin Hypn 2010;52:263-73. [Crossref] [PubMed]
- NIH (National Institutes of Health) institutes, centers, and offices plus the Agency for Healthcare Research and Quality CAM. Complementary and Alternative Medicine in the United States. The National Academies Collection: Reports funded by National Institutes of Health. Institute of Medicine (US) Committee on the Use of Complementary and Alternative Medicine by the American Public. Washington (DC): National Academies Press (US); 2005.
- Elkins G, Johnson A, Fisher W. Cognitive hypnotherapy for pain management. Am J Clin Hypn 2012;54:294-310. [Crossref] [PubMed]
- Kiernan BD, Dane JR, Phillips LH, et al. Hypnotic analgesia reduces R-III nociceptive reflex: further evidence concerning the multifactorial nature of hypnotic analgesia. Pain 1995;60:39-47. [Crossref] [PubMed]
- Rainville P, Hofbauer RK, Bushnell MC, et al. Hypnosis modulates activity in brain structures involved in the regulation of consciousness. J Cogn Neurosci 2002;14:887-901. [Crossref] [PubMed]
- Landry M, Lifshitz M, Raz A. Brain correlates of hypnosis: A systematic review and meta-analytic exploration. Neurosci Biobehav Rev. 2017;81:75-98. [Crossref] [PubMed]
- Erickson MH, Rossi EL. The nature of hypnosis and suggestion. New York: Irvington Publisher Inc, 1980.
- ERICKSON MH. Hypnosis in painful terminal illness. Am J Clin Hypn 1959;1:1117-21.
- Brugnoli A. Hypnotherapy of pain. Minerva Med 1974;65:3288-95. [PubMed]
- Ewin DM. Relieving suffering--and pain--with hypnosis. Geriatrics 1978;33:87-9. [PubMed]
- Jensen MP, Chen C, Brugger AM. Interpretation of Visual Analog Scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain 2003;4:407-14. [Crossref] [PubMed]
- Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol 1959;32:50-5. [Crossref] [PubMed]
- Maier W, Buller R, Philipp M, et al. The Hamilton Anxiety Scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord 1988;14:61-8. [Crossref] [PubMed]
- De Sousa R. The Rationality of Emotion. Cambridge, MA: MIT Press, 1987.
- Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis. Lancet Oncol 2011;12:160-74. [Crossref] [PubMed]
- Grassi L, Caruso R, Sabato S, et al. The UniFe Psychiatry Working Group Coauthors. Psychosocial screening and assessment in oncology and palliative care settings. Front Psychol 2015;5:1485. [Crossref] [PubMed]
- Coelho A, Parola V, Cardoso D, et al. Use of non-pharmacological interventions for comforting patients in palliative care: a scoping review. JBI Database System Rev Implement Rep 2017;15:1867-904. [Crossref] [PubMed]
- Wortzel J, Spiegel D. Hypnosis in Cancer Care. Am J Clin Hypn 2017;60:4-17. [Crossref] [PubMed]
- Handel DL, Néron S. Cancer Palliation: Layered Hypnotic Approaches Mending Symptoms, Minding Hope, and Meaning. Am J Clin Hypn 2017;60:33-49. [Crossref] [PubMed]
- de Graaf E, van Klinken M, Zweers D, et al. From concept to practice, is multidimensional care the leading principle in hospice care? An exploratory mixed method study. BMJ Support Palliat Care 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Ginandes C. Staying the Course: Using Hypnosis to Help Cancer Patients Navigate Their Illness. Am J Clin Hypn 2017;60:85-102. [Crossref] [PubMed]
- Elkins GR, Barabasz AF, Council JR, et al. Advancing research and practice: The revised APA division 30 definition of hypnosis. Am J Clin Hypn 2015;57:378-85. [Crossref] [PubMed]
- Laurence JR, Beaulieu-Prévost D, du Chéné T. Measuring and understanding individual differences in hypnotizability. In: The Oxford handbook of hypnosis. New York: Oxford University Press, 2008:225-53.
- Facco E, Testoni I, Ronconi L, et al. Psychological Features of Hypnotizability: A First Step Towards Its Empirical Definition. Int J Clin Exp Hypn 2017;65:98-119. [Crossref] [PubMed]
- Saunders C. A personal therapeutic journey. BMJ 1996;313:1599-601. [Crossref] [PubMed]
- Abbiati G. Pope Francis shows support for palliative care ahead of the 21st General Assembly of the Pontifical Academy for Life in the Vatican. Available online: http://www.ehospice.com/ArticleView/tabid/10686/ArticleId/14387/language/en-GB/Default.aspx


