A 10 years audit of cardiothoracic referrals from a pulmonology service in a developing country: impact of patient human immunodeficiency virus status
Introduction
Clinical audits are often undertaken in medical and surgical units and while the ultimate purpose of a clinical audit may be the improvement of medical care, it is said that they may also provide a method for reflecting on and reviewing clinical practice in a systematic way (1,2). Much has been written about the clinical audit, including a description of what a clinical audit is, how it should be conducted, and what the barriers and facilitators to a clinical audit are (1,2).
Many of the published clinical audits reflect data collected from a single unit or deal with the management of one specific medical condition (3-6). However, some of the medical/surgical specialities, such as cardiothoracic surgery, have established national databases which allow countrywide data to be extracted for clinical audits (7-10). One of these databases in the field of cardiothoracic surgery was established in South Africa, with the expressed aim of being both a resource for answering either specific research questions among a series of patients, or to enable prospective recording of data from a range of patients treated by the speciality, which could be used later in either clinical or healthcare systems research (9). Databases could therefore provide the basis by which one is able to convert the stored information into knowledge that may help guide clinical practice (9). However, there have been few publications documenting the clinical presentations and outcomes of cardiothoracic referrals from pulmonology services from Developing countries, and little information on the impact of patient human immunodeficiency virus (HIV) status on trends in disease manifestations or cardiothoracic outcomes,
In Johannesburg, South Africa, three of the teaching hospitals that fall under the University of the Witwatersrand each have a respiratory (pulmonology) unit and clinicians from these units, as well as staff from the thoracic surgery unit based at Charlotte Maxeke Johannesburg Academic Hospital, meet weekly to discuss cases that might need surgical intervention for diagnosis and/or treatment. The main aims of the current audit were to describe the spectrum of cases presented at these meetings, as well as the impact, if any, of HIV infection on the clinical presentation, complications and outcome of the patients.
Methods
This was a retrospective record review of all cases presented to the Combined Thoracic-Pulmonology meetings held weekly at the Charlotte Maxeke Johannesburg Academic Hospital during the period 1 January 2001 and 31 December 2010. These meetings are attended by junior and senior staff of all three Pulmonology Units based at hospitals attached to the University of the Witwatersrand, together with the staff from the Thoracic Surgery Unit based at Charlotte Maxeke Johannesburg Academic Hospital. Permission to undertake this study was obtained from the Human Research Ethics Committee of the University of the Witwatersrand, Johannesburg, South Africa.
At these weekly meetings, cases are presented from any of the Units, that may require a thoracic surgical procedure for diagnosis and/or treatment, and the relevant clinical and laboratory features and appropriate radiological studies are reviewed. Thereafter a plan of management is decided upon. On a weekly basis new cases are presented and the follow-up of previously presented cases is reviewed until their clinical management has been completed.
For the purposes of the recording of these meetings, specially developed standard clinical record forms are completed and filed. These forms contain information on the patients, which may include details of the demographic features, the major clinical findings (presenting symptoms, findings on clinical examination), appropriate radiological and laboratory findings, lung function studies, the diagnosis (confirmed or suspected), the requested surgical procedure, and the suggested management plan. Discussion is held around the cases and a final management plan is decided upon by consensus.
For the purposes of this audit, the forms were reviewed and all the available information was extracted. Specific data sought included the following:
- Patient details—notably age, gender, HIV status, CD4 cell count, receipt of highly-active retroviral therapy (HAART);
- Clinical details—notably the clinical diagnosis or suspected diagnosis;
- Surgical intervention requested (diagnostic or therapeutic);
- Type of surgical procedure undertaken;
- Outcome following surgical procedure (outcome, complications, cause of death);
- Final tissue diagnosis, where appropriate.
The data were anonymized and entered onto an excel spreadsheet. For the descriptive statistics the values were expressed as numbers (percentages) and means and standard deviations or median and ranges. The trends in the numbers of the various diseases and in the HIV status of the patients over the 10-year period were noted. HIV-positive patients were compared with HIV-negative patients with regard to disease diagnoses on initial presentation, to the rate of postoperative complications and to mortality. Comparison of continuous variables was undertaken using the students unpaired t-test or the Mann-Whitney U test, as appropriate and comparison of categorical variables was undertaken using the Chi squared or Fisher’s exact test, as appropriate. A P value of less than 0.05 was considered to be significant.
Results
A total of 847 patients were entered into the database. The gender was unknown in 20 cases and of the remainder, 450 were male (54.4%) and 377 female (45.6%). The median age of the group was 44.5 (range, 1–84) years. Female patients tended to be younger than male patients [median 42 (range, 1–84) years vs. 46 (range, 4–76) years; P=0.08]. HIV status was known in 488 patients (57.6%) with 229 cases being HIV-seropositive (46.9%) and 259 cases being seronegative (53.1%). There was no gender difference in the known prevalence of HIV-seropositivity [123 males (27.3% of males) and 99 females (26.3% of females)]. Among the HIV-seropositive cases, the median CD4 cell count was 243 (range, 4–1,780) cells/µL. Among the HIV-seropositive patients in whom the data was available (143 cases) 61 patients (42.7%) were documented to be on HAART and 82 were not (57.3%).
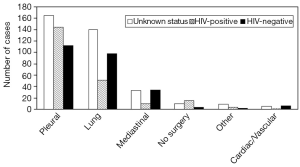
The main reasons for referral of cases to the cardiothoracic surgeons are shown in Figure 1. More than half of the diagnoses were infective conditions, including tuberculosis (TB), pleural disease/pleural effusions/empyema and bacterial infections. The next most common reason for referral was for known or suspected lung malignancy. There were some differences in primary diagnosis when comparing HIV-positive vs. HIV-negative cases (Figure 1B). Presentations for TB were much more common among HIV-seropositive compared with HIV-seronegative patients (46.5% vs. 28.8%; P<0.0001), while presentations for lung cancer were more common among HIV-seronegative compared with HIV-seropositive cases (21.6% vs. 7.5%; P<0.0001).

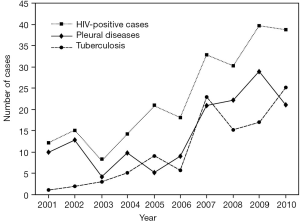
Changes in the disease presentations over the ten year period were evident. In particular there was a considerable increase in presentations for both TB and for pleural disease paralleled by a significant increase in the number of HIV-seropositive patients presented (Figure 2).
The surgical procedures undertaken are shown in Figure 3. Overall, 50.4% of the surgical procedures were therapeutic, 32.8% were diagnostic and 16.9% were both diagnostic and therapeutic.
The rate of complications that occurred in the patients was compared in HIV-seropositive and HIV-seronegative cases. Post-procedure mechanical ventilation was included in the evaluation of the complications, even though this may be undertaken routinely following certain surgical procedures and may therefore not strictly be a complication. In addition to requirement for mechanical ventilation, complications recorded included development of respiratory failure, bleeding or need for blood transfusion, development of sepsis, development of hypotension/shock, requirement for a repeat operation, development of an air leak or bronchopleural fistula, acute kidney injury, metabolic abnormalities, development of a deep venous thrombosis or pulmonary embolism, development of wheezing, confusion, cardiac failure or any other unexpected pulmonary disability. There was no difference in the rate of complications when comparing HIV-seropositive and HIV seronegative patients (13.7% vs. 13.1%; P=0.87). The complication rate was also similar in those patients whose HIV status was unknown (12.3%).
There was also no significant difference in the all-cause mortality post-procedure when comparing those who were HIV-seropositive with those who were HIV-seronegative (6.2% vs. 8.0% respectively; P=0.83). The mortality in those of unknown HIV status was also similar (8.0%).
Discussion
This study is the first in South Africa to audit cases managed jointly by pulmonologists and cardiothoracic surgeons in an academic teaching hospital in a setting of high HIV prevalence. A considerable number of the cases whose HIV status was known were documented to be HIV-seropositive (46.9%). The main findings were that the common disease presentations for consideration for surgical procedures were infective conditions, including TB, pleural disease/pleural effusion/empyema and bacterial infections. Importantly the complication and mortality rates were identical in HIV-seropositive and HIV-seronegative patients.
The major disease conditions presented for possible surgical procedures were also of infective origin including TB, pleural disease/effusion/empyema and bacterial infections. At least part of the explanation for this relates to the large numbers of patients who were HIV-infected. In fact when comparing the patients who were presented at the meeting with TB, significantly more were HIV-seropositive than HIV-seronegative. It has clearly been well characterized that despite antimicrobial prophylaxis and antiretroviral therapy, which have changed the epidemiology and impact of pulmonary infections in HIV-infected patients, pulmonary infections still remain a common cause of morbidity and mortality and TB particularly remains a very important infection (11).
Worldwide it is quite common for the thoracic surgeon to be called upon for the diagnosis and treatment of various conditions associated with HIV infection (12). This is particularly so in sub-Saharan Africa/South Africa given the significant ongoing impact of HIV infection in the population (13). A question that has often been asked is what impact HIV infection has on the complication rate and mortality in association with surgical procedures and should it affect surgical decision making (14). One study undertaken earlier on in the HIV epidemic among patients having surgical management for thoracic manifestations of HIV infection, documented that the mortality rate appeared to be linked to the stage of HIV infection at the time of therapy, rather than the type of surgery undertaken (15). The authors concluded that the Centers for Disease Control and Prevention (CDC) stage and physiological status of HIV-infected patients need to be taken into consideration when considering surgery.
In the current study, HIV status was known in 488 patients and among these patients 46.9% were documented to be HIV-seropositive. Among the HIV-seropositive cases, the median CD4 cell count was 243 (range, 4–1,780) cells/µL and among the patients in whom the data was available (143 cases) 61 patients (42.7%) were documented to be on HAART and 82 were not (57.3%). However, the complication and mortality rates in our patients were very similar in HIV-seropositive and HIV-seronegative cases [13.7% vs. 13.1%; P=0.89) and 6.2% vs. 8.0% (P=0.83), respectively], as well as being very similar to those cases in whom the HIV status was unknown (12.3% and 8.0%, respectively).
Other investigators undertaking a literature review of the topic came to the conclusion, as we would, that in otherwise asymptomatic HIV-infected patients, appropriate surgery for the circumstances should be undertaken without much concern about the likelihood of an unfavourable outcome (14). However, cases do need to be evaluated for their state of immunosuppression and in patients with advanced disease, palliative surgery could still be used for relief of acute problems (14).
Our study does have some potential limitations. It was conducted in a single academic centre and so may not have generalizability. It was retrospective in nature and therefore not all the data that we wished to evaluate was either available or had been recorded. For example, the exact diagnosis was not always known at the time of the initial presentation, and so could not be recorded. Furthermore, the exact type of surgery that was subsequently performed was also not known at the initial presentation and so could not be recorded. Some data was also missing. There may have been selection bias in the cases that were presented at the meeting. For example, it is possible that HIV-infected individuals with advanced immunosuppression and/or associated comorbid conditions and/or poor clinical status may have been pre-excluded from presentation at the meeting. In addition, the audit would also have excluded emergency cases that were referred directly to the Cardiothoracic Unit, bypassing the meeting.
Conclusions
Nevertheless, the study does have some strong points. Firstly, it is a relatively unique study in the literature and, to our knowledge, is the first to present data from combined Pulmonology/Cardiothoracic meetings in South Africa. Secondly, it includes a large number of patients studied over a considerable period of time (10 years) such that it provides interesting information regarding trends in respiratory disease profiles, apparently related to the HIV pandemic. Thirdly, and perhaps most importantly, it provides some evidence that the complication rate and outcome in a largely unselected group of patients with HIV infection is similar to that of HIV-uninfected cases, suggesting the ongoing benefit and relative safety of cardiothoracic surgery in these cases.
Acknowledgements
Charles Feldman is supported by the National Research Foundation of South Africa.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- What is clinical audit? Available online: http://ww.rcpsych.ac.uk/pdf/clinauditchap1.pdf
- Johnston G, Crombie IK, Davies HT, et al. Reviewing audit: barriers and facilitating factors for effective clinical audit. Qual Health Care 2000;9:23-36. [Crossref] [PubMed]
- Alam SN, Rehman S, Raza SM, et al. Audit of a general surgical unit: need for self evaluation. Pakistan Journal of Surgery 2007;23:141-4.
- Ali SA, Soomro AG, Tahir SM, et al. Prospective basic clinical audit using minimal clinical data set. J Ayub Med Coll Abbottabad 2010;22:58-61. [PubMed]
- Baseer A, Bilal A, Muslim M. Audit of one year workload of thoracic surgical team at Peshawar. Pak J Chest Med 2007;13.
- Numan RC, Klomp HM, Li W, et al. A clinical audit in a multidisciplinary care path for thoracic surgery: an instrument for continuous quality improvement. Lung Cancer 2012;78:270-5. [Crossref] [PubMed]
- Ferguson TB Jr, Dziuban SW Jr, Edwards FH, et al. The STS National Database: current changes and challenges for the new millennium. Committee to Establish a National Database in Cardiothoracic Surgery, The Society of Thoracic Surgeons. Ann Thorac Surg 2000;69:680-91. [Crossref] [PubMed]
- Shroyer AL, Coombs LP, Peterson ED, et al. The Society of Thoracic Surgeons: 30-day operative mortality and morbidity risk models. Ann Thorac Surg 2003;75:1856-64; discussion 1864-5.
- Linegar A, Smit F, Stroebel A, et al. A South African national database in cardiothoracic surgery. Cardiovasc J Afr 2010;21:153-4. [PubMed]
- Society for Cardiothoracic Surgery in Great Britain & Ireland. 2011 National Thoracic Surgery Activity and Outcomes report. Available online: http://www.scts.org/modules/resources/info.aspx?id=46, accessed 7 April 2016.
- Wolff AJ, O'Donnell AE. HIV-related pulmonary infections: a review of the recent literature. Curr Opin Pulm Med 2003;9:210-4. [Crossref] [PubMed]
- Abolhoda A, Keller SM. Thoracic surgical spectrum of HIV infection. Semin Respir Infect 1999;14:359-65. [PubMed]
- Maartens G, Celum C, Lewin SR. HIV infection: epidemiology, pathogenesis, treatment, and prevention. Lancet 2014;384:258-71. [Crossref] [PubMed]
- Madiba TE, Muckart DJ, Thomson SR. Human immunodeficiency disease: how should it affect surgical decision making? World J Surg 2009;33:899-909. [Crossref] [PubMed]
- Mouroux J, Riquet M, Padovani B, et al. Surgical management of thoracic manifestations in human immunodeficiency virus-positive patients: indications and results. Br J Surg 1995;82:39-43. [Crossref] [PubMed]


