Weight gain as a surrogate marker of longer survival in advanced non-small cell lung cancer patients
Since the earliest report of Hippocrates (460–377 BC), weight loss (WL) has been perceived as a condition that is closely associated with poor prognosis in patients presenting with chronic illnesses, including the cancer. As a pivotal component of the irreversible and fatal cancer-related anorexia cachexia syndrome (CACS), WL, is present to some degree in 80% of non-small cell lung cancer (NSCLC) patients at presentation which has been clearly proved to negatively alter patients’ performance status, quality of life (QOL), response to treatment, and prognosis (1,2). However, WL is not a problem encountered only upon diagnosis but is also commonly reported during the course of aggressive chemotherapy, radiotherapy (RT), and particularly the concurrent chemoradiotherapy (C-CRT), which may further diminish QOL measures and clinical outcomes. WL during NSCLC treatment may be associated with side effects including fatigue, anorexia, nausea, vomiting, esophagitis, early satiety, dysphagia, diarrhea, and infections (3).
In the August 2016 issue of Annals of Oncology Patel et al. (4) reported the outcomes of retrospective analysis of 2,301 stage IIIB or IV non-squamous NSCLC patients enrolled on three previous phase III clinical trials (5-7) with the primary endpoint of the impact of weight gain (WG) experienced during the treatment or at the 30-day post-study discontinuation follow-up visit. In this commendable study the authors divided the 421 (18.3%) patients with WG into two groups: those with >5% vs. ≤5% WG. Majority of these patients had stage IV disease (n=340; 81%). Their results demonstrated a significant association between superior median overall survival (OS) and >5% WG (16.7 vs.10.7 months; HR: 0.57; P<0.001). Likewise, the patients who experienced >5% WG had approximately 2 months superior median progression-free survival (PFS; 6.9 vs. 4.8 months; HR: 0.61; P<0.001) and 25% superior overall response rate (50.8 vs. 25.4%; P<0.001). The authors also reported that these positive relationships were independent of other confounding variables.
Current standard treatment options for metastatic and locally-advanced NSCLC (LA-NSCLC) include systemic chemotherapy, targeted therapies, and palliative RT for metastatic and C-CRT for LA-NSCLC patients, respectively (8,9). However, starkly contrasting with the significant improvements in diagnostic tools and treatment options in the last three decades, the survival rates remained poor and almost constant for both the metastatic (range, 8–12 months) and locally advanced (range, 16–24 months) disease stages (8-10). Given the poor outcomes in this patient populace, it is essential to determine prognostic factors beyond the conventionally utilized performance status, T, N, M stages, pretreatment WL, and objective response to treatment. Therefore, the impressive results of the Patel’s large retrospective review are of vital significance with respect to that it confirms the suggested novel prognostic and predictive roles for WG in NSCLC patients (10-12).
The particular prognostic significance of weight preservation or gain has previously been addressed in three retrospective cohort series as aforementioned above (10-12). In the first study reported by Sher et al. from Rush University Medical Center (11), the authors evaluated the prognostic significance of WG during the split course chemoradiotherapy in 92 LA-NSCLC patients with the primary endpoint of OS. In this study the WG was defined as the any weight change greater than the highest quartile of change (4.5 lb) between the initiation and completion of the CRT. The authors reported that the WG was the unique factor to associate with enhanced median OS times (51 vs. 23 months; HR: 0.5; P=0.04). At long-term, the OS probability was more profound in favor of the WG group with respective 5-year OS estimates of 50% vs. 12%. Second study was a smaller preoperative split-course CRT study again from Rush University Medical Center (12) which included 54 patients with locally advanced (n=51) or oligometastatic (n=3) LA-NSCLC patients. Results of multivariate analysis revealed that the initial stage (HR: 2.94; P=0.02) and percent weight change during the CRT course (HR: 0.79; P<0.01) were the factors to associate with OS outcomes. Accordingly patients who experienced WG (n=26) had significantly longer median OS time compared to dose who did not (not reached yet vs. 16.3 months; P=0.001) and 3-year OS probability (71.4% vs. 21.9%). Although these studies suggested a survival enhancing function for WG during CRT course, one may contend that both studies utilized split-course CRT which does not reflect the current standard treatment paradigm for such patients, namely the C-CRT. In this regard, the third study reported by our group represents the largest of ever its kind study which particularly researched the impact of weight change during the course of exclusive radical C-CRT in 425 stage IIIB NSCLC patients (10). In this study, in order to prevent uncontrollable feeding-related measurement biases, any WC was accepted as significant only if the calculated difference came upon a positive or negative body mass index (BMI) change of 0.5 kg/m2 relative to pretreatment levels. Therefore, the study population was divided into 3 groups: group 1: WL (BMI reduction >0.5 kg/m2); group 2: weight preservation (WP: BMI reduction/increment <0.5 kg/m2); and group 3: WG gain (BMI increment >0.5 kg/m2). However, for comparative analysis groups 2 and 3 were consolidated as WP/G. As indicated by this definition, 252 patients (59.3%) experienced WL, while 89 patients (20.9%) and 84 patients (19.8%) demonstrated weight preservation or gain during C-CRT. Survival analysis revealed that WP/G group had significantly superior median OS time (27.3 vs. 17.8 months; P<0.001) and 3-year OS rate (42.3% vs. 0%). Another important finding of our study was the demonstration of significantly longer median locoregional PFS (LRPFS: 17.4 vs. 11.5 months) and distant metastasis free survival (DMFS 14.1 vs. 9.3 months), which translated into longer PFS (8.7 vs. 13.3 months) in WL patients.
Interpreting the three previous reports together with the more recent one by Patel et al. (4), available results suggest the WG experienced during C-CRT as a surrogate marker of superior OS times either in the preoperative split-course induction CRT, definitive split-course induction CRT, or radical C-CRT settings independent of the chemotherapy regimen or RT protocol in use. These results may be influenced by the decreased toxicity rates (particularly the esophagitis, nausea and vomiting) by use of more sophisticated RT techniques such as intensity-modulated or image-guided RT, earlier diagnosis and intervention of treatment related toxicities, and more common use of supportive measures. However, it is obvious that these complications have not been eliminated totally yet by utilization of more sophisticated RT techniques or available pharmaceutical or nutritional additives. Additionally, as some patients with severe toxicity do not experience WL and as currently available nutritional additives have questionable influence on prevention or treatment of WL, such survival gain cannot be explained uniquely by decreased rates of toxicity and indicates presence of other potential factors to be identified. More reasonably these findings rather designate higher response to chemotherapy both as a radiosensitizer at locoregional sites and as a systemic treatment at distant microscopically involved sites (10).
Despite the exact cause(s) of association between WL and poorer locoregional and distant control rates is not fully investigated yet, impaired nutritional status, anti-tumoral immunity, existence of potentially unaltered chronic inflammatory milieu, and more aggressive tumor phenotype with poor or no response to any oncologic treatment may sensibly have assumed a part (13,14). Additionally, unaltered or even increased secretion of cachectic factors by poor or nonresponding tumors may have further contributed to unfavorable outcomes observed in these patients (15). Therefore, WG experienced during the treatment course may have mirrored the reversal of poor immunity, blockade of secretion of cachectic factors, and alteration of chronic inflammatory milieu in a group of NSCLC patients treated with various oncologic interventions. However, in order to conclude more reliably on this subject of critical importance further studies addressing this issue are urgently needed.
The value of degree of clinically significant WL has been clearly defined in consensus statements in order to create a three-stage classification specific for cancer; namely precachexia, cachexia, and refractory cachexia (16). For this purpose, the criteria for cachexia incorporates body WL >5% over the past 6 months or a BMI of <20 in combination with WL >2% over the past 6 months (16). However, our knowledge about the importance of degree of WG experienced during the cancer treatment is scarce. In general, previous reports did not search for a significant WG cutoff specific to NSCLC patients and grouped patients into two respective groups: those with WL or WG (including the weight preservers). In this respect Patel et al. defined “clinically significant WG” as any gain >5% with the aim of prevention of false measurements which potentially caused by daily fluctuations in hydration and standard error variances (4). However, authors’ additional analysis using “any WG” rather than 5% as the cutoff (n=1,066; 46.3%) demonstrated similar superior median OS outcomes (15.2 and 8.6 months; HR: 0.51) favoring the group of patients with any WG over those without. Comparing the HRs of two different dichotomization methods (0.51 vs. 0.57; for any WG vs. >5% WG, respectively) reveals that preservation or gain of any body weight is even more important than WG >5%. Despite the fact that it is hard to allocate this finding to a single cause, yet it is rationale to hypothesize that even minor and clinically insignificant WG is the representative of the early reversal of the molecular pathways of the irreversible and fatal CACS.
In the two largest studies Patel et al. (4) and Topkan et al. (10) respectively demonstrated that it is possible to preserve pretreatment body weight or induce WG in 46.3% and 40.7% of all metastatic or locally advanced NSCLC patients undergoing chemotherapy or C-CRT. Concentrating on this point, Topkan’s study is intriguing by exhibiting striking long-term survival rate differences at 3-year OS (42.3 vs. 0%), LRPFS (31.2 vs. 0%), PFS (25.3% vs. 0%), and DMFS (26.2 vs. 0%) time points between the WG and WL groups, favoring the former (10). Despite suggesting a surrogate role for WG during C-CRT in accurate anticipation of outcomes in LA-NSCLC, these observations may further hint at tailoring adjuvant or salvage treatments of such patients. Because the response and survival outcomes were poor in the WL cohort, such finding may be suggestive of the need for more intense and efficient but less toxic adjuvant chemotherapeutics. Additionally, it may further suggest closer follow-up of such patients for earlier detection and timely management of resistant or recurrent local disease and/or already existing or de novo metastases. In the presence of stereotactic radiation therapy facilities, some of these patients may further experience tumor control, QOL, and potential survival benefits. On the other hand, favorable results in WG cohort may also raise the question about the need for potentially toxic and currently debated consolidation chemotherapies, which may not yield further clinical gain in such patients.
In conclusion, outcomes of available studies (4,10-12), particularly the largest of ever one by Patel et al. (4), are important by demonstration of a clear survival benefit with prevention of WL in approximately 40–45% of all NSCLC patients (Table 1). However, looking at the other side of the coin, it is dramatic to see that more than 50% of all NSCLC patients are continuing to lose weight despite of aggressive treatment. Therefore, although the potential therapeutic implications have not been fully exploited in humans, it is imperative to continue on clinical research of CACS for improving patients’ tolerance to treatment and QOL. The main goal should incorporate the development of both preventive and therapeutic measures for WL on a multidisciplinary approach basis. For this purpose, considering the multifactorial nature of WL on the way of fatal CACS, targeting the multiple steps of CACS including the hypothalamic pathways, tumor-secreted factors, and chronic inflammation status rather than a single potential target appears to be of vital importance on the way of success.
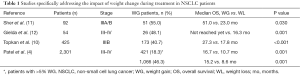
Full table
Acknowledgements
None.
Footnote
Provenance: This is a Guest Perspective commissioned by Section Editor Jianrong Zhang, MD (Department of Thoracic Surgery, First Affiliated Hospital of Guangzhou Medical University, Guangzhou Institute of Respiratory Disease, Guangzhou, China).
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Inui A. Cancer anorexia-cachexia syndrome: current issues in research and management. CA Cancer J Clin 2002;52:72-91. [Crossref] [PubMed]
- Werner-Wasik M, Scott C, Cox JD, et al. Recursive partitioning analysis of 1999 Radiation Therapy Oncology Group (RTOG) patients with locally-advanced non-small-cell lung cancer (LA-NSCLC): identification of five groups with different survival. Int J Radiat Oncol Biol Phys 2000;48:1475-82. [Crossref] [PubMed]
- Argilés JM, Olivan M, Busquets S, et al. Optimal management of cancer anorexia-cachexia syndrome. Cancer Manag Res 2010;2:27-38. [Crossref] [PubMed]
- Patel JD, Pereira JR, Chen J, et al. Relationship between efficacy outcomes and weight gain during treatment of advanced, non-squamous, non-small-cell lung cancer patients. Ann Oncol 2016;27:1612-9. [Crossref] [PubMed]
- Scagliotti GV, Parikh P, von Pawel J, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol 2008;26:3543-51. [Crossref] [PubMed]
- Rodrigues-Pereira J, Kim JH, Magallanes M, et al. A randomized phase 3 trial comparing pemetrexed/carboplatin and docetaxel/carboplatin as first-line treatment for advanced, nonsquamous non-small cell lung cancer. J Thorac Oncol 2011;6:1907-14. [Crossref] [PubMed]
- Patel JD, Socinski MA, Garon EB, et al. PointBreak: a randomized phase III study of pemetrexed plus carboplatin and bevacizumab followed by maintenance pemetrexed and bevacizumab versus paclitaxel plus carboplatin and bevacizumab followed by maintenance bevacizumab in patients with stage IIIB or IV nonsquamous non-small-cell lung cancer. J Clin Oncol 2013;31:4349-57. [Crossref] [PubMed]
- Furuse K, Fukuoka M, Kawahara M, et al. Phase III study of concurrent versus sequential thoracic radiotherapy in combination with mitomycin, vindesine, and cisplatin in unresectable stage III non-small-cell lung cancer. J Clin Oncol 1999;17:2692-9. [PubMed]
- Curran WJ Jr, Paulus R, Langer CJ, et al. Sequential vs. concurrent chemoradiation for stage III non-small cell lung cancer: randomized phase III trial RTOG 9410. J Natl Cancer Inst 2011;103:1452-60. [Crossref] [PubMed]
- Topkan E, Parlak C, Selek U. Impact of weight change during the course of concurrent chemoradiation therapy on outcomes in stage IIIB non-small cell lung cancer patients: retrospective analysis of 425 patients. Int J Radiat Oncol Biol Phys 2013;87:697-704. [Crossref] [PubMed]
- Sher DJ, Gielda BT, Liptay MJ, et al. Prognostic significance of weight gain during definitive chemoradiotherapy for locally advanced non-small-cell lung cancer. Clin Lung Cancer 2013;14:370-5. [Crossref] [PubMed]
- Gielda BT, Mehta P, Khan A, et al. Weight gain in advanced non-small-cell lung cancer patients during treatment with split-course concurrent chemoradiotherapy is associated with superior survival. Int J Radiat Oncol Biol Phys 2011;81:985-91. [Crossref] [PubMed]
- Laviano A, Meguid MM, Inui A, et al. Therapy insight: Cancer anorexia-cachexia syndrome--when all you can eat is yourself. Nat Clin Pract Oncol 2005;2:158-65. [Crossref] [PubMed]
- Jafri SH, Shi R, Mills G. Advance lung cancer inflammation index (ALI) at diagnosis is a prognostic marker in patients with metastatic non-small cell lung cancer (NSCLC): a retrospective review. BMC Cancer 2013;13:158. [Crossref] [PubMed]
- Suzuki H, Asakawa A, Amitani H, et al. Cancer cachexia--pathophysiology and management. J Gastroenterol 2013;48:574-94. [Crossref] [PubMed]
- Fearon K, Strasser F, Anker SD, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 2011;12:489-95. [Crossref] [PubMed]


