Syndrome of transient headache and neurologic deficits with cerebrospinal fluid lymphocytosis masquerading as meningitis in HIV patient
Introduction
Syndrome of transient headache and neurologic deficits with cerebrospinal fluid lymphocytosis (HaNDL syndrome) is described as “headache attributed to noninfectious inflammatory disease” featuring, as its name suggests, headache that mimics migraine in addition to neurologic symptoms such as hemiparesis, hemiparesthesia and dysphagia (1). While a thorough investigation of past medical history and detailed physical examination can help guide clinical suspicions, cerebrospinal fluid (CSF) analysis is required to make the diagnosis.
Case presentation
A 50-year-old African-American female with a past medical history of HIV, Crohn’s disease and hepatitis C infection presented with complaints of throbbing headache, subjective fever, malaise and photophobia. She denied confusion, weight loss, abdominal pain, nausea, vomiting, heartburn or urinary symptoms. Neurological exam was significant for moderate decrease in cervical spine range of motion with no evident rigidity, and was negative for Kernig or Brundzinski’s signs. She was alert and oriented, cranial II–XII grossly intact with no apparent motor or sensory deficits. Cardiac, pulmonary, abdominal and musculoskeletal exam was unremarkable.
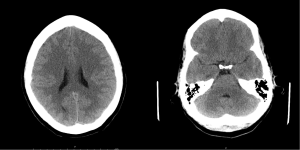
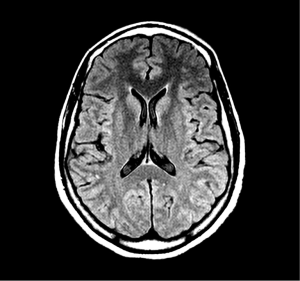
Computed tomography (CT) head without contrast was unremarkable for intracranial abnormalities (Figure 1). Empirical antibiotic therapy was started for suspected bacterial meningitis. Lumbar puncture (LP) was performed and CSF analysis was positive only for isolated elevation in WBC at 20/µL, with total protein 42 mg/dL and glucose 56 mg/dL). CSF was negative for Herpes Simplex virus (HSV), Varicella zoster virus (VZV), and enterovirus PCR, venereal disease research laboratory (VDRL), and Lyme antibodies. Serum studies for blood culture, serum cryptococcal antigen and fluorescent treponemal antibody absorption (FTA-ABS) results all returned negative while C-reactive protein was elevated at 8.5 mg/dL. However, the patient reported abrupt onset of right-sided hemiparesis in both upper and lower extremities while left side remained intact. In addition, she reported worsening of occipital headache as well as photophobia. MRI without contrast showed punctate foci of increased white matter signal likely due to chronic migraine headaches or minimal microvascular ischemic changes (Figure 2). The WBC normalized and septic workup was negative. Bases on the history, physical exam and LP findings the diagnosis of HaNDL syndrome was made. On day 6 after admission, patient reported complete resolution of her symptoms with full recovery of right-sided muscle strength.
Discussion
HaNDL syndrome is considered rare variant of migrainous headache. It is characterized by a migraine-like headache (single episode or multiple up to 12), associated with one of the following: hemiplegia, hemiparesthesia, dysphasia (>4 h), and rarely visual symptoms (2,3). The patients are usually asymptomatic between episodes. However, the neurological deficits can last up to 7 weeks (4). Despite the fact that most patients appear to be substantially ill upon initial evaluation, symptoms usually resolve completely within weeks to months. CSF analysis universally shows isolated pleocytosis, and CSF protein is frequently elevated (4). This is in contrast to familial hemiplegic migraine, which likewise holds the features of hemiparesis and migraine headache but with normal CSF analysis. Furthermore, patients with HaNDL syndrome also differs with its absence in familial history linkage (5).
While the etiology is unclear, it is thought to be related to unilateral vasospasm in the intracranial vessels. Transcranial Doppler sonography performed during and after documented attacks showed asymmetrical fluctuations in middle cerebral arterial blood flow velocity and pulsatility indicating that intracranial vasomotor changes play a role in the pathophysiology of HaNDL (6,7). Studies have also demonstrated reduction in local or widespread ipsilateral cerebral blood flow on the ipsilateral side with neurologic deficits, hence raising the question on whether perfusion disparity participates in the development of HaDNL syndrome (3).
Autoimmune cross-reactivity due to either viral or inflammatory origin, on the other hand, is as well believed to contribute in the process of HaNDL syndrome. Specifically, a recent study has demonstrated autoantibodies to subunit of the T-type voltage-gated calcium channel, CACNA1H, has been linked to HaNDL syndrome (8). In addition, mitogen activated protein kinase-4 (MAPK-4) and DNA-dependent protein kinase catalytic subunit (DPKCU) antibodies were also detected in minority of HaNDL patients (8,9).
HaNDL syndrome has a good prognosis, it is usually self-limited and does not require treatment. However, corticosteroids, calcium channel blockers and acetazolamide has been previously used in treatment (10,11).
In conclusion, the exact etiology behind HaNDL syndrome remains poorly understood. Aside from HaNDL syndrome, other differentials that healthcare providers have to take into consideration upon evaluating patients with similar presentations should include acute meningitis, Mollaret’s meningitis, Lupus, malignancy, Lyme disease, Mycoplasma, ischemic event, atypical migraines and familial hemiplegic migraine (5). Because of the rarity of this syndrome and difficulty in confirming the diagnosis, it poses as a challenge for physicians, especially in acute setting.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013;33:629-808.
- Valença MM, de Oliveira DA, Martins HA. Alice in Wonderland Syndrome, Burning Mouth Syndrome, Cold Stimulus Headache, and HaNDL: Narrative Review. Headache 2015;55:1233-48.
- Filina T, Feja KN, Tolan RW Jr. An adolescent with pseudomigraine, transient headache, neurological deficits, and lymphocytic pleocytosis (HaNDL Syndrome): case report and review of the literature. Clin Pediatr (Phila) 2013;52:496-502.
- Ropper AH, Brown RH. Adams and Victor's Principles of Neurology. 8th Edition. New York: McGraw-Hill Professional, 2005.
- Ducros A, Denier C, Joutel A, Cecillon M, et al. The clinical spectrum of familial hemiplegic migraine associated with mutations in a neuronal calcium channel. N Engl J Med 2001;345:17-24.
- Fumal A, Vandenheede M, Coppola G, et al. The syndrome of transient headache with neurological deficits and CSF lymphocytosis (HaNDL): electrophysiological findings suggesting a migrainous pathophysiology. Cephalalgia 2005;25:754-8.
- Kappler J, Mohr S, Steinmetz H. Cerebral vasomotor changes in the transient syndrome of headache with neurologic deficits and CSF lymphocytosis (HaNDL). Headache 1997;37:516-8.
- Kürtüncü M, Kaya D, Zuliani L, et al. CACNA1H antibodies associated with headache with neurological deficits and cerebrospinal fluid lymphocytosis (HaNDL). Cephalalgia 2013;33:123-9.
- Erdağ E, Çelebisoy N, Yüceyar AN, et al. Antibodies to DNA repair proteins in headache with neurological deficits and cerebrospinal fluid lymphocytosis (HaNDL) patients. Acta Neurol Belg 2015;115:137-40.
- Tsang BK, Kwong JC, Dewey HM. Case of syndrome of headache with neurological deficits and cerebrospinal fluid lymphocytosis (HaNDL) with focal slowing on electroencephalogram. Intern Med J 2012;42:944-7.
- Yilmaz A, Kaleagasi H, Dogu O, et al. Abnormal MRI in a patient with 'headache with neurological deficits and CSF lymphocytosis (HaNDL)'. Cephalalgia 2010;30:615-9.