Preoperative surgical rehearsal using cadaveric fresh tissue surgical simulation increases resident operative confidence
Introduction
Practice and repetition are important tenets of learning any complex task, such as flying an airplane, playing a musical instrument, or performing surgery. A regimented surgical training paradigm has remained a core foundation since the renowned Dr. William Halstead first applied his innovative ideas to surgical education. However, in the setting of resident work hour restrictions, there is concern that surgeon training will be compromised. Compared with total case numbers prior to duty hour reduction, general surgery residents now perform 20–25% fewer total cases during the course of residency (1). A recent survey of graduating general surgery residents showed that only 50% felt confident performing at least half of the 18 most common procedures (2). Confidence is known to improve academic and athletic performance and has been shown to be correlated with competence in the surgical arena (3-5). Furthermore, a recent survey of fellowship directors revealed that 66% of surgical fellows could not operate independently for thirty minutes (6). These findings demonstrate the need for additional clinical experience to supplement lost operative time.
During the infancy of medicine, when rapid disease progression and high rates of surgical death limited the amount of practice which could be gleaned from clinical cases, cadaver dissection and simulation was a staple of training. Hands-on simulation has been demonstrated to be superior to verbal or written education for the acquisition, maintenance, and transfer of technical skills to the operating room (7-12). Technological advances have now created alternative methods of surgical simulation, from low fidelity bench models to high fidelity virtual reality simulators. However, the majority of simulators target only basic laparoscopic procedures or simple skills, such as suturing and knot tying. Though laparoscopic techniques have replaced many conventional operations, open procedures remain prevalent in many surgical fields, including plastic surgery. For this reason, we have developed a cadaveric simulation laboratory to supplement classic, patient-based learning in our residency program (13-15).
An effective rehearsal in any field of performance requires the fidelity of the theater to be as realistic as possible to maximize confidence and competence. Fresh tissue dissection has multiple advantages over virtual simulation: authenticity of tactile stimulation and perception, three dimensional anatomical relationships, anatomical variation, the opportunity to react to and solve unexpected complications outside of a predetermined and simulated operative algorithm, and the opportunity to learn non-technical skills, such as autonomy, communication, and teamwork. To examine the fidelity between cadaveric simulation and live surgery, we provided residents with the opportunity to fully rehearse upcoming operations of their choice using fresh tissue simulation. We evaluated resident confidence pre- and post-simulation as well as resident perception of the effect of simulation on surgeon speed, safety, technique, and knowledge during the case. In all areas, residents believed that cadaveric rehearsal of complex, open, surgical procedures substantially improved confidence and skill and was superior to traditional, non-simulation methods of pre-operative preparation.
Methods
Fresh Tissue Dissection Laboratory (FTDL)
All rehearsals took place in the FTDL at Los Angeles County Hospital (LAC). Fresh, unembalmed cadavers were received shortly after death and handled according to the Standard Operating Procedures (SOP) of the LAC Fresh Tissue Dissection Lab. SOP were established and approved by the Institutional Review Board in 2005 and revised in 2012 (IRB approval ID: IIR00002007). Procurement of all cadavers occurred according to the SOP and followed strict guidelines in adherence with California law and USC Keck School of Medicine oversight. Each cadaver was used for multiple surgical rehearsals within a 4-week period and refrigerated between uses to maintain tissue integrity.
Participants
Plastic surgery residents from all years of the residency program at the USC Keck School of Medicine were invited to utilize fresh cadaver surgical simulation prior to any scheduled case during the study period.
Rehearsal format
To more closely simulate the live operative environment, rehearsal parameters were defined. Each participant was assisted by a surgical technician and was provided with surgical instruments appropriate for the rehearsed procedure. The cadaver was brought to the simulation suite and positioned appropriately for the planned procedure. The resident was responsible for selection of the appropriate instruments during the case. Pathology was simulated wherever possible, when to do so would not constitute destruction of the tissues. Rehearsal was performed by each participant without attending assistance to simulate autonomy. Participants then performed the actual surgical case, with appropriate attending supervision, within the following seven-day period.
Assessment
Participants completed an anonymous, online survey at the conclusion of each real-time surgical case for which they utilized preoperative simulation in the FTDL. A retrospective pre-rehearsal/post-rehearsal analysis method was chosen to reduce response shift bias (16,17). If asked to score confidence levels separately before an activity and then again after completion of the activity, self-evaluators tend to use different frames of reference for each score, leading to an over- or under-representation of the pre-activity score and inaccuracy of the change in confidence. If asked to score both pre-activity and post-activity confidence levels together after completion of the activity, self-evaluators use a similar frame of reference when choosing both scores, which provides a more controlled assessment of confidence gains.
Objective data included post-graduate level of training, type of preoperative surgical simulation performed, and the intervening number of days between preoperative simulation and the actual operative case. Participants were then asked to retrospectively rate their confidence with the intended procedure both before and after simulation, on a scale of 1 to 5, with 1 representing “not confident at all” and 5 representing “very confident”. Subjective perceptions of overall surgical performance, speed, knowledge of anatomy, and technical safety during the actual procedure were also analyzed, using similar 5-point scales. Participants were asked to compare the effectiveness of surgical simulation with their standard methods of preparation, typically review of textbooks or discussion with more experienced surgeons. Resident perception of patient benefit from surgical simulation and the importance of inclusion of surgical simulation within the resident training curriculum completed the survey.
Statistical methods
Ordinal data from Likert questions were analyzed using median values. Statistical significance between paired pre- and post-rehearsal confidence levels was calculated using the Wilcoxon signed rank test. The Kruskal Wallis test was used to demonstrate that there was no significant difference in reported ratings among different postgraduate years. The Wilcoxon rank-sum test was used to demonstrate the significance of changes in confidence levels when rehearsal was performed ≤3 or ≥4 days prior to the scheduled case. Where applicable, interval data was analyzed using means and standard deviation.
Results
Participants
Twenty-six rehearsals were performed by nine residents (PGY 1-7). Senior residents (PGY6, PGY7) most frequently utilized preoperative simulation, representing 75% of the survey respondents.
Procedures performed
A variety of procedures were rehearsed using surgical simulation in the FTDL (Table 1). Participants began by positioning the patient in a manner appropriate to the procedure being rehearsed. The procedure was then performed, in its entirety, independently by the resident. A surgical technician was present to assist, as in the real operative setting.
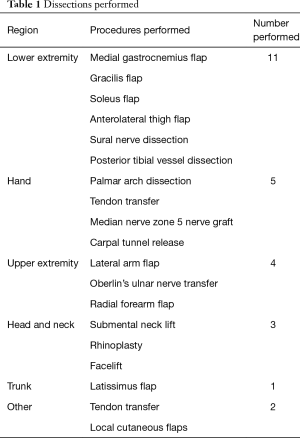
Full table
Approximately 50% of procedures entailed myocutaneous flaps and 50% were performed on the lower extremity. The remainder of the procedures were widely distributed across all body sites, including head and neck, hand or upper extremity, and trunk. Two procedures, identified as “local flap” and “tendon”, were not site-specific. In addition to myocutaneous flaps and dedicated hand or head and neck procedures, participants also simulated nerve and vessel harvest and repair. As examples of the types of procedures rehearsed, two cases are described in more detail.
Case 1
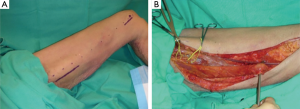
A 27-year-old male with a tibial fracture required free tissue transfer of the gracilis muscle for wound closure. Open reduction and internal fixation of the fracture, followed by harvest and transfer of the gracilis muscle, was planned. The preoperative plan was reviewed with the attending surgeon and the rehearsal was scheduled. The rehearsal included harvest of the gracilis muscle and exposure of recipient blood vessels in the leg (Figure 1). Appropriate anatomic landmarks were identified and the muscle flap was harvested in the standard fashion. The clinical operation was performed 3 days later with success.
Case 2
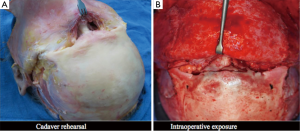
A 26-year-old male sustained a pan-facial fracture, including maxillary, nasoorbitoethmoid (NOE), and frontal sinus fractures. The patient was admitted to the inpatient service, underwent a full trauma work-up, and was deemed to be a candidate for open reduction and internal fixation of the fractures. The case plan was reviewed in detail with the attending surgeon and an operative plan was made, including the use of craniofacial approaches through coronal, transconjunctival, and upper buccal sulcus incisions. As it was the first time the resident would perform the operation, a preoperative rehearsal was employed. The rehearsal included operative positioning, planned anatomical approaches, use of standard instruments, and identification of the landmarks during the surgical approach. The operation was performed without complication within 3 days of the rehearsal (Figure 2).
Timing
Though given freedom to choose the timing of the preoperative rehearsal, all residents performed simulations within one week of the actual case. On average, participants performed surgical simulation 4.7±2.1 days before the scheduled case (Figure 3A). However, the large majority of rehearsals were performed either 3 (36%) or 7 (41%) days preoperatively (Figure 3B). Dissections performed by PGY1 residents were not included in this portion of the analysis, as these residents did not go on to personally perform the rehearsed procedures in the operating room.
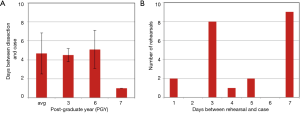
Rehearsal improved resident confidence
The median pre-rehearsal confidence level for all participating residents was 2, with a score of 1 representing “no confidence at all” and 5 representing “very confident” (Figure 4A). Following rehearsal, the median post-rehearsal confidence level for all residents improved to 4 (P<0.01). A sub-analysis by post-graduate training year revealed some minor differences. PGY1 residents cited a lower pre-rehearsal confidence level but an improvement in confidence which mirrored the total resident group. Secondly, while the median pre-rehearsal confidence for PGY3 residents was equivalent to the total group of participating residents, PGY3 residents did not perceive as large of an improvement in their overall confidence level post-rehearsal. However, this study was not sufficiently powered to detect significant differences in subgroup analysis. Additionally, while the timing of the rehearsal was left to the discretion of the resident, the effect of rehearsal on the improvement in confidence was greatest when the rehearsal was performed within 3 days of the scheduled case (P<0.01) (Figure 4B).

Rehearsal improved technical performance, speed, safety, and anatomical knowledge
Post-operatively, residents were asked to score their surgical performance with respect to anatomical knowledge, technical safety, speed, and overall performance, with 1 representing decreased anatomical knowledge, less safe technique, slower speed, and poorer performance, and 5 representing improved anatomical knowledge, much safer technique, much faster speed, and improved performance, respectively, on a Likert scale. All residents felt that their anatomical knowledge (median of 5), technical safety (median of 5), operative speed (median of 4), and overall performance (median of 5) were enhanced during the actual surgical case after participation in procedure-specific, pre-operative, surgical rehearsal (Figure 5A).

Rehearsal was felt to be beneficial and necessary
Residents agreed that pre-operative surgical rehearsal was more effective than standard methods of preparation, such as self-directed reading or preoperative discussion with the attending surgeon (Figure 5B). In addition, all residents strongly believed that pre-operative surgical rehearsal should be included in resident training (Figure 5B). These statements were strongly supported by residents from all levels of training.
Discussion
The use of simulation for surgical training has often been likened to simulation training for pilots. However, a more applicable analogy is rehearsal by a musical ensemble (18). The difference between individual musical study and ensemble rehearsal is well studied and we sought to apply this to surgical education. In surgical training, benchtop models and virtual reality simulators may be sufficient for the practice of specific tasks but do not allow for any ensemble practice, a necessity to acquire the skills to lead a surgical team, independently complete a surgery as the attending surgeon, and address unpredictable minute-to-minute changes in the operating room. While the proficiency of individual skills or tasks is, unarguably, a necessary building block for more complex procedures, oversimplification of a complex process may not teach the deeper understanding needed to truly become a master. Thus, comprehensive rehearsal of surgical performance prior to entering the operating room, as opposed to individual skill practice, was the goal of this study. We hypothesized that the use of cadaver simulation, which can mimic a complex procedure and provide the environment for inter-personal interactions and unexpected complications, would be valuable for improving resident confidence, particularly for open surgical procedures.
Traditional preoperative preparation has included the study of standard textbooks and journal publications followed by benchtop practice of individual technical skills. The degree to which preparation improves actual surgical performance is very difficult to estimate and exactly which preparations are most important is even more difficult to ascertain. However, it is clear from the literature that structured preparation improves performance. Even something as simple as mental guided imagery has been shown to improve the performance of simulated laparoscopic cholecystectomy (19). The use of a defined curriculum for laparoscopic colectomy training, involving a combination of self-directed reading, video-based learning, virtual reality simulation, and cadaver simulation, demonstrated that the preparative curricula improved the performance of the procedures in the operating room compared to conventional independent learning (20). These studies performed rigorous and validated assessments of the impact of the preparation on performance, both clinically and within the simulated environment. However, it remains unclear exactly which part of the curriculum contributed the most to the improved operative skills (20). The main goal of our study was to focus strictly on the effect of rehearsal of a complex technical procedure in a very high fidelity environment on the completion and performance of the procedure and to evaluate the resident’s perception of the experience as it pertained to their confidence in completing the real-time surgical procedure.
Clanton et al. recently studied the relationship of confidence and competence in the field of surgery by evaluating two simple skills, knot-tying and suturing, after a brief video and hands-on training (5). Those students who cited high confidence levels post-training were found to be more successful at performing the specified task, suggesting that confidence could be used as a predictor of technical competence and that pre-task, hands-on practice serves to improve both confidence and skill (5). Building on this conclusion, we sought to evaluate the effect of pre-operative surgical rehearsal of more complex skill sets. Our study was designed to allow residents to practice the procedure of their choice in full, from initial patient positioning to final wound closure and with a surgical assistant, rather than pre-assigning a simple, standardized task.
After pre-operative, procedure-specific, cadaveric surgical rehearsal, residents perceived significant improvement in operative confidence and felt that the time spent in preparation was more valuable and comprehensive than traditional methods of book-study or discussion with the attending surgeon. Analysis of confidence levels by individual post-graduate year demonstrated improvements across all years. Interns and mid-level residents did not attain as great an increase in confidence as more senior residents, though the change was not statistically significant. This may be attributed to the moderate amount of knowledge and experience of a mid-level resident, which in turn allows them to also realize how much they have yet to master, resulting in a lesser rating of confidence post-simulation. Senior level residents derived significantly more benefit from cadaveric surgical simulation. One might expect that lower-level residents, with less hands-on operative experience, might gain more from cadaveric simulation, while senior residents might find the exercise less helpful. In contrast, it is likely that the opportunity to practice procedures in a simulated operative setting allows senior residents to practice nontechnical skills (21-23), such as communication and autonomy in decision making, as well as anticipation and correction of complications, thus, better preparing them to function independently and proactively in the operating room, a mastery that has been found to be suboptimal in many recent graduates (1,2,6).
Due to the expense and resources required to maintain a cadaver laboratory, discussed in more detail in our other publication (15), cadaveric simulation is not widely used in residency training programs. In our program, the ability to maintain a fresh tissue simulation laboratory has been increased by multiple uses per cadaver and investment by our Graduate Medical Education department in cross-disciplinary surgical simulation. We hope that the positive effect of cadaveric rehearsal will drive the implementation of this type of simulation in other centers. A recent study compared laparoscopic sigmoid colectomies performed on a cadaver versus a virtual reality simulator (23). Cadaveric simulation was demonstrated to be superior to standard simulations when learned techniques were applied to live surgery. Additionally, cadaveric simulation was perceived as more difficult and more errors (i.e., bowel perforations) were made while using the cadaver model system than alternative laparoscopic simulation models. While at first thought these findings could be viewed as detractors for the use of cadaveric simulation, the increased challenge of cadaveric simulation is an asset. The use of a simulator should not be an easy exercise. Rather, it should approximate the task at hand as accurately as possible to maximize training efficiency and minimize real-time operative errors. Costs associated with the implementation of fresh tissue surgical simulation may ultimately be recouped by the improvement in safety that surgical rehearsal provides.
Ultimate proof that high fidelity rehearsal can substitute for shortened hands-on training time will require the objective analysis of complex procedures and clinical outcomes over time. This process is difficult and has been the bane of most surgical education and simulation projects to date. Our study is clearly limited by the use of subjective analysis to evaluate effectiveness from the perspective of resident confidence. The link between resident confidence and performance has been suggested by others and will be studied in greater detail in our future studies. A second limitation of this study is the small sample size, particularly with respect to numbers of residents per year. Extension of this study to include a larger cohort of residents and attending evaluation of resident skills pre- and post-simulation is planned.
In summary, we found that pre-operative surgical rehearsal using cadaveric simulation for a variety of procedures in the field of plastic surgery was identified as a valuable tool to increase resident confidence and led to the perception of improved speed, technique, anatomical knowledge, and patient safety during actual operative cases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board (No. IIR00002007).
References
- Carlin AM, Gasevic E, Shepard AD. Effect of the 80-hour work week on resident operative experience in general surgery. Am J Surg 2007;193:326-9; discussion 329-30. [Crossref] [PubMed]
- Fonseca AL, Reddy V, Longo WE, et al. Operative confidence of graduating surgery residents: a training challenge in a changing environment. Am J Surg 2014;207:797-805. [Crossref] [PubMed]
- Levy AR, Nicholls AR, Polman RC. Pre-competitive confidence, coping, and subjective performance in sport. Scand J Med Sci Sports 2011;21:721-9. [Crossref] [PubMed]
- Stankov L, Lee J, Luo W, et al. Confidence: a better predictor of academic achievement than self-efficacy, self-concept and anxiety? Learn Individ Differ 2012;22:747-58. [Crossref]
- Clanton J, Gardner A, Cheung M, et al. The relationship between confidence and competence in the development of surgical skills. J Surg Educ 2014;71:405-12. [Crossref] [PubMed]
- Mattar SG, Alseidi AA, Jones DB, et al. General surgery residency inadequately prepares trainees for fellowship: results of a survey of fellowship program directors. Ann Surg 2013;258:440-9. [Crossref] [PubMed]
- Jayaraman V, Feeney JM, Brautigam RT, et al. The use of simulation procedural training to improve self-efficacy, knowledge, and skill to perform cricothyroidotomy. Am Surg 2014;80:377-81. [PubMed]
- Aggarwal R, Ward J, Balasundaram I, et al. Proving the effectiveness of virtual reality simulation for training in laparoscopic surgery. Ann Surg 2007;246:771-9. [Crossref] [PubMed]
- Park J, MacRae H, Musselman LJ, et al. Randomized controlled trial of virtual reality simulator training: transfer to live patients. Am J Surg 2007;194:205-11. [Crossref] [PubMed]
- Seymour NE, Gallagher AG, Roman SA, et al. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 2002;236:458-63; discussion 463-4. [Crossref] [PubMed]
- AlJamal YN, Ali SM, Ruparel RK, et al. The rationale for combining an online audiovisual curriculum with simulation to better educate general surgery trainees. Surgery 2014;156:723-8. [Crossref] [PubMed]
- Andreatta P, Saxton E, Thompson M, et al. Simulation-based mock codes significantly correlate with improved pediatric patient cardiopulmonary arrest survival rates. Pediatr Crit Care Med 2011;12:33-8. [Crossref] [PubMed]
- Carey JN, Rommer E, Sheckter C, et al. Simulation of plastic surgery and microvascular procedures using perfused fresh human cadavers. J Plast Reconstr Aesthet Surg 2014;67:e42-8. [Crossref] [PubMed]
- Sheckter CC, Kane JT, Minneti M, et al. Incorporation of fresh tissue surgical simulation into plastic surgery education: maximizing extraclinical surgical experience. J Surg Educ 2013;70:466-74. [Crossref] [PubMed]
- Carey JN, Minneti M, Leland HA, et al. Perfused fresh cadavers: method for application to surgical simulation. Am J Surg 2015;210:179-87. [Crossref] [PubMed]
- Howard G. Response-shift bias: a problem in evaluating interventions with pre/post self-reports. Eval Rev 1980;4:93-106. [Crossref]
- Barclay-Goddard R, Epstein JD, Mayo NE. Response shift: a brief overview and proposed research priorities. Qual Life Res 2009;18:335-46. [Crossref] [PubMed]
- Kneebone RL. Practice, rehearsal, and performance: an approach for simulation-based surgical and procedure training. JAMA 2009;302:1336-8. [Crossref] [PubMed]
- Arora S, Aggarwal R, Sirimanna P, et al. Mental practice enhances surgical technical skills: a randomized controlled study. Ann Surg 2011;253:265-70. [Crossref] [PubMed]
- Palter VN, Grantcharov T. Development and validation of a comprehensive curriculum to teach an advanced minimally invasive procedure: a randomized controlled trial. Ann Surg 2012;256:25-32. [Crossref] [PubMed]
- Yule S, Flin R, Paterson-Brown S, et al. Non-technical skills for surgeons in the operating room: a review of the literature. Surgery 2006;139:140-9. [Crossref] [PubMed]
- Gettman MT, Pereira CW, Lipsky K, et al. Use of high fidelity operating room simulation to assess and teach communication, teamwork and laparoscopic skills: initial experience. J Urol 2009;181:1289-96. [Crossref] [PubMed]
- LeBlanc F, Champagne BJ, Augestad KM, et al. A comparison of human cadaver and augmented reality simulator models for straight laparoscopic colorectal skills acquisition training. J Am Coll Surg 2010;211:250-5. [Crossref] [PubMed]


