Impact of enhanced recovery after surgery protocols on postoperative morbidity and mortality in patients undergoing routine hepatectomy: review of the current evidence
Introduction
Hepatectomy is essential part of multidisciplinary approach in treatment of primary and secondary liver malignancies. Despite significant improvements in perioperative management and surgical technique, 30-day morbidity and mortality are reported to be at 14–55% (1,2) and 0–11.9% (1,2) respectfully and are associated with prolonged hospital stay and resources utilization.
Enhanced recovery after surgery (ERAS) protocols have been pioneered by Kehlet and include multimodality approach to perioperative care to reduce length of stay and complications rate. It was since successfully accepted by many surgical subspecialties but only recently applied in hepato-bilio-pancreatic surgery. With current data suggesting potential benefit in decreasing length of stay and decreasing complications rate, we decided to analyze an impact ERAS protocols have on perioperative morbidity and mortality among published series.
Methods
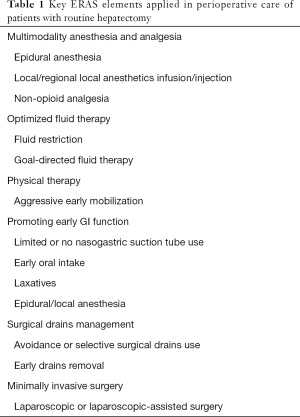
All studies, published in English medical literature for the last 10 years (January 1st, 2006 to January 1st, 2016) with key words “enhanced recovery protocol” or “fast-track protocol” and “hepatectomy” or “liver resection” including more than 20 patients aged older than 18 years old were identified in PubMed database. All studies used similar approach in perioperative management incorporating key ERAS elements presented in Table 1. Both randomized and non-randomized studies were included. All pertinent data, including type of cases, type of study, study endpoints, number of patients, morbidity and mortality, type of complications (medical vs. surgical) and impact of ERAS program were extracted and analyzed. Difference in morbidity and mortality, when available, was presented as statistically significant if p value was below 0.05.
Full table
Results
Fifteen studies were identified (3-17). All studies excluded patients with complex biliary or vascular reconstructions. Overall, nine studies were prospective, three were randomized control trials, two were retrospective studies and one observation study were found. Number of enrolled patients ranged from 26 to 304. Study endpoints varied and included feasibility, length of stay and perioperative morbidity, completion of fast-track/ERAS protocol and functional recovery. One study was examining effect of laxatives on GI recovery (6) and one study compared effects of intrathecal analgesia versus epidural analgesia (5). Two studies included only patients undergoing laparoscopic hepatectomy (4,8), four analyzed both laparoscopic and open procedures (4-17) while one study looked only on patients having major open hepatectomy (13). Remaining eight reports included only patients undergoing open hepatectomy (3,5-7,10-12,14). Overall characteristics of all studies are summarized in Table 2.
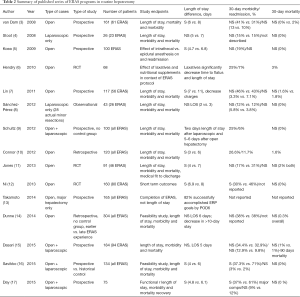
Full table
ERAS protocol impact on length of stay
Out of all studies, ten demonstrated statistically significant reduction of hospital stay (all three randomized studies, six prospective studies and one retrospective study). Study reported by Schultz (9) was excluded from analysis since it had no control group and studies by Hendry (6) and Koea (5) were excluded since both arms were managed according to similar ERAS protocol and primary endpoints were effects of laxatives on GI recovery and intrathecal vs. epidural anesthesia. Study by Connor (10) was reporting gradual introduction of ERAS elements over period of 6 years and was included in final analysis. After excluding abovementioned studies, seven remained studies demonstrated reduced length of stay by median of 2 days (range, 1.1–3 days).
Four published series reported no impact of eras program on length of stay (three prospective, one observational and one retrospective study). Studies of Stoot et al. (4) and Sánchez-Pérez et al. (8) were reporting ERAS protocol management of patient undergoing minor laparoscopic hepatectomy, while study of Dunne et al. (14) was comparing length of stay in early versus late ERAS management cohort. Dasari et al. (15) reported no difference in median length of stay in his report of 184 patients undergoing both open and laparoscopic hepatectomies. Takamoto et al. (13) reported completion of ERAS protocol goals and was not geared towards analyzing difference in length of stay.
ERAS protocol impact on postoperative complications and readmission rate.
Out of total 15 studies, 5 were excluded. Studies by Takamoto et al. (13) and Schultz et al. (9) did not have control group and studies by Dunne (14), Hendry (6) and Koea (5) all compared patients treated with similar ERAS protocols. Of reminding ten studies, six were prospective, one retrospective, one observational and two randomized control studies. Majorities of studies have shown similar overall complication rate with decreased rate of either medical complications or grade I–II complications [Jones (11), Ni (12), Day (17)]. Dasari et al. (15) reported decrease in grade III–V (severe complications) with no impact on readmission rates. Readmission rate was similar in all studies with Connor et al. (10) noting trend in increased readmission rate towards later ERAS cohort which paralleled increase in postoperative complications.
ERAS protocol impact on postoperative mortality
Out of all 15 studies, study by Takamoto et al. did not report any mortality data and was excluded. Among remaining 14 studies, there was no statistically significant difference in perioperative mortality (range, 0–2%) (3-17).
Discussion
Based on available reports, implementation of ERAS program for patients undergoing routine hepatectomy reduces length of hospital stay, medical complications without negative impact on postoperative readmission or mortality. Reduction in length of stay was almost uniform finding, excluding studies concentrating on laparoscopic minor hepatectomies (4,8) where ERAS is unlikely to reduce it. Despite Dunne (14) reporting similar length of stay, that study was indeed a comparison of early versus late cohort of patients treated with the same protocol and there was reduction in number of patients staying more than 10 days. Dasari et al. (15) reported similar findings, however pre-ERAS and post-ERAS cohorts are difficult to compare since author unit already practiced some fast-track elements in their perioperative care before introduction of standardized protocol. Overall morbidity seems not to be affected by ERAS management, with some studies demonstrating decrease in medical and low-grade Clavien grade I–II complications. The only study reporting decrease in major complications (grade III–V) is by Dasari et al. (15), which appears to be mostly secondary to higher rate of intra-abdominal collections. There are no details given on a nature of intra-abdominal collections but in reviewing both pre-ERAS and ERAS cohorts, there is increased number of extended resections, open hepatectomy, hepatocellular carcinoma and cirrhosis in pre-ERAS group which can potentially contribute to observed difference. Readmissions and mortality rates are similar in most of the studies. Connor et al. (10) reported increase in readmission rates with parallel decrease of length of stay under ERAS protocol below 4 days while overall complication rate was unaffected. That indicates that some postoperative complications specific to hepatectomy (intraabdominal collections/abscesses/bile leak) may present outside the typical length of stay of the patients managed by ERAS protocol. In the same study, development of complication, total amount of IV fluids given and performance of biliodigestive anastomosis were all associated with increased LOS.
While reporting positive impact on perioperative evolution of patient undergoing hepatectomy, there are significant drawbacks in many of analyzed studies, ranging from lack of control group and comparison to historical control to retrospective or observational character. Many centers had some elements of fast-track management before implementing standardized ERAS protocol and protocol itself varied between different studies. Adherence to ERAS protocol was not reported in majority of studies or was not tracked at all. Finally, some studies excluded certain patients, like those undergoing laparoscopic procedure (11) or bile duct resection (3,7,12), while others included only laparoscopic cases [48] or mixture of open and laparoscopic cases.
Conclusions
Perioperative ERAS management of the patients undergoing hepatectomy is safe. Hospital length of stay is reduced without adverse impact on postoperative complication rate and mortality. There is a potential for reduced medical or low grade (Clavien I–II) complications while surgical complications are unchanged. Further insight into adherence to ERAS protocol and comparison of similar type of cases/operative procedures is needed to implement ERAS protocol as a standard of care for patients after liver resections.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Aloia TA, Fahy BN, Fischer CP, et al. Predicting poor outcome following hepatectomy: analysis of 2313 hepatectomies in the NSQIP database. HPB (Oxford) 2009;11:510-5. [Crossref] [PubMed]
- Egger ME, Ohlendorf JM, Scoggins CR, et al. Assessment of the reporting of quality and outcome measures in hepatic resections: a call for 90-day reporting in all hepatectomy series. HPB (Oxford) 2015;17:839-45. [Crossref] [PubMed]
- van Dam RM, Hendry PO, Coolsen MM, et al. Initial experience with a multimodal enhanced recovery programme in patients undergoing liver resection. Br J Surg 2008;95:969-75. [Crossref] [PubMed]
- Stoot JH, van Dam RM, Busch OR, et al. The effect of a multimodal fast-track programme on outcomes in laparoscopic liver surgery: a multicentre pilot study. HPB (Oxford) 2009;11:140-4. [Crossref] [PubMed]
- Koea JB, Young Y, Gunn K. Fast track liver resection: the effect of a comprehensive care package and analgesia with single dose intrathecal morphine with gabapentin or continuous epidural analgesia. HPB Surg 2009;2009:271986. [Crossref] [PubMed]
- Hendry PO, van Dam RM, Bukkems SF, et al. Randomized clinical trial of laxatives and oral nutritional supplements within an enhanced recovery after surgery protocol following liver resection. Br J Surg 2010;97:1198-206. [Crossref] [PubMed]
- Lin DX, Li X, Ye QW, et al. Implementation of a fast-track clinical pathway decreases postoperative length of stay and hospital charges for liver resection. Cell Biochem Biophys 2011;61:413-9. [Crossref] [PubMed]
- Sánchez-Pérez B, Aranda-Narváez JM, Suárez-Muñoz MA, et al. Fast-track program in laparoscopic liver surgery: Theory or fact? World J Gastrointest Surg 2012;4:246-50. [Crossref] [PubMed]
- Schultz NA, Larsen PN, Klarskov B, et al. Evaluation of a fast-track programme for patients undergoing liver resection. Br J Surg 2013;100:138-43. [Crossref] [PubMed]
- Connor S, Cross A, Sakowska M, et al. Effects of introducing an enhanced recovery after surgery programme for patients undergoing open hepatic resection. HPB (Oxford) 2013;15:294-301. [Crossref] [PubMed]
- Jones C, Kelliher L, Dickinson M, et al. Randomized clinical trial on enhanced recovery versus standard care following open liver resection. Br J Surg 2013;100:1015-24. [Crossref] [PubMed]
- Ni CY, Yang Y, Chang YQ, et al. Fast-track surgery improves postoperative recovery in patients undergoing partial hepatectomy for primary liver cancer: A prospective randomized controlled trial. Eur J Surg Oncol 2013;39:542-7. [Crossref] [PubMed]
- Takamoto T, Hashimoto T, Inoue K, et al. Applicability of enhanced recovery program for advanced liver surgery. World J Surg 2014;38:2676-82. [Crossref] [PubMed]
- Dunne DF, Yip VS, Jones RP, et al. Enhanced recovery in the resection of colorectal liver metastases. J Surg Oncol 2014;110:197-202. [Crossref] [PubMed]
- Dasari BV, Rahman R, Khan S, et al. Safety and feasibility of an enhanced recovery pathway after a liver resection: prospective cohort study. HPB (Oxford) 2015;17:700-6. [Crossref] [PubMed]
- Savikko J, Ilmakunnas M, Mäkisalo H, et al. Enhanced recovery protocol after liver resection. Br J Surg 2015;102:1526-32. [Crossref] [PubMed]
- Day RW, Cleeland CS, Wang XS, et al. Patient-Reported Outcomes Accurately Measure the Value of an Enhanced Recovery Program in Liver Surgery. J Am Coll Surg 2015;221:1023-30.e1-2.


