Robotic retroauricular thyroidectomy: initial experience from India
Introduction
Conventionally thyroidectomy is performed through an open neck approach. Technological advancements in this field have allowed the development of remote access surgical approaches to the thyroid. Since the introduction of surgical robotics, transoral robotic surgery (TORS) has been widely applied in head and neck cancer surgery (1-5). Robotic thyroidectomy is getting accepted worldwide, but, majority of the literature is from South Korea. A widely acknowledged approach is the trans-axillary route. Robotic facelift or the retroauricular (RA) approach was initially reported by Terris and colleagues (6-8) and is popularized by Koh and his colleagues (9,10). The purpose of this paper is to review the early experiences with robotic RA thyroidectomy from India.
Why robotic surgery
Conventional thyroidectomy results in a conspicuous anterior neck scar. Thyroidectomy is a procedure which is commonly done in females and mostly in their younger ages. It is evident that a fraction of these patients is unhappy about the scar. It is prudent to develop and improve upon a technique which can avoid the scar. Endoscopic techniques were developed and are still popular. Endoscopic surgery in the neck has many limitations like two-dimensional vision, the need for an assistant to hold the camera, restriction in the number of instruments that can be used together and the relatively difficult learning curve (11-14). Robotic surgery has many advantages (14,15).
Advantages of robotic thyroidectomy (15)
Visualization
Robotic surgery offers three-dimensional stereoscopic vision with high definition and high magnification (10× greater than human eye).
Dexterity
Enhanced dexterity with wristed instruments is a hall mark of robotic surgery.
Precision
Surgeon tremor is absent. Moreover, the visualization, retraction and dexterity help to do precise surgery.
Enhanced retraction
Compared to endoscopic surgery, there is a fourth arm with prograsp forceps to retract.
Surgeon ergonomics
Once the robot is docked, the surgeon sits comfortably in a separate console with forearm on the pad, to control the arms.
Limitations of robotic thyroidectomy (15)
Cost
Cost is an important concern. Cost can be minimized by the multidisciplinary use, especially in an institutional practice.
Learning curve
A learning curve of 35–40 cases is suggested for robotic thyroidectomy. But, this is considerably less compared to endoscopic thyroidectomy (55–60 cases). Proper case selection is the key to overcome the learning curve (12,13).
Instrument size
The Xi system now has 8 mm instruments. Even the 5 mm instruments in the Si system are large. Soon, the miniaturization of the instruments and further technological developments like single arm surgery may solve these issues.
Lack of haptic feedback
Novice surgeons may find the absence of haptic feedback, a difficulty. The visual clues must be relied to assess the surgical field.
Why RA approach
It is like the modified facelift (MFL) approach for parotidectomy. The difference is the absence of a preauricular limb in the MFL incision. The potential advantages of the RA approach are (I) it offers better cosmesis when compared to the standard thyroidectomy and transaxillary incisions; (II) anatomy and the vector of dissection, being a neck procedure, is familiar to the head and neck surgeons; (III) brachial plexus is not at risk; (IV) short area of dissection which is less compared to the transaxillary approach. The advantages of the RA approach come not only from the utilization of the surgical robots, but also from the fact that the access is remotely placed (9).
Patient selection (16-18)
Patient factors
Patients’ physique, including the body mass index (BMI), length and circumference of the neck will have an influence on the surgery. BMI varies between races (19). An average Indian adult has a BMI of the range 21–23 (20). An ideal patient for any remote access approach would be a small or an average sized young patient who is concerned about the neck scarring or a history or hypertrophic scar.
Disease factors
The thyroid pathology will have an influence on selecting the approach. A patient with a thyroid nodule less than 4 cm or a confirmed papillary cancer less than 2 cm in diameter or multinodular goiter with less than 4 cm sized nodules. The size factor matters much in the early phases of the learning curve. As the surgeon gets more experienced, larger sized nodules may also be amenable to robotic surgery. Presence of thyroiditis is a relative contraindication, due to associated fibrosis and adhesions. Malignancy as such is not a contraindication. Neck dissection can be comfortably with RA approach, but it would be prudent to select patients without gross involvement of the nodes in the initial phases of the learning curve.
Relative contraindications
- Well differentiated thyroid cancers > T2;
- Thyroid nodules >4 cm;
- Larger goiters;
- Severe Grave’s disease with enlarged glands;
- Advanced thyroiditis;
- Morbid obesity.
Absolute contraindications
- Thyroid cancer with evidence of gross invasion;
- Previous neck surgery or irradiation;
- A substernal or retrosternal goiter.
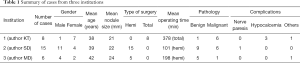
Indian experience
We report the outcome and experiences from the early few cases from three centers from India. da Vinci system (Intuitive Surgical Systems, Sunnyvale, CA, USA) was the commonest robot used. The latest two models are Si and Xi. Si model is approved by the FDA for transoral surgery. It comes with 5 mm instruments and harmonic shears. Xi has 8 mm instruments and is less suitable for transoral surgery. Both the models were used for thyroidectomy. Adequate preclinical, basic instrumental animal and human anatomic specimen training were taken. Clinical training was also done mainly by visiting centers in South Korea. Table 1 shows the summary of the cases of thyroidectomies from three institutions from India.
Full table
First author’s (Krishnakumar Thankappan) institution has done eight cases over a period of 6 months. The patients included seven females and one male. Mean age was 38.3 years (range, 23–65 years). The mean size of the nodule was 21.3 mm (range, 15–30 mm). Total thyroidectomy was done in all patients through a bilateral RA approach. Each lobe was approached from the ipsilateral RA area. The mean operating time was 378 min. The operating time came down with each case was 230 min in the last case. The mean hospital stay was 6 days (range, 5–8 days). On the post-operative pathology, six patients had papillary carcinoma. Three patients had temporary hypocalcemia and one patient developed hypertrophic scar. None of the patients had vocal cord palsy. Overall the outcomes were encouraging. A detailed analysis of the cases is not intended in this paper and hence not reported.
Second author’s (Surender Dabas) institute has done 15 cases of robotic hemithyroidectomy over a period of 16 months. It included 11 males and 4 females. Mean age at presentation was 39.9 years (range, 23–56 years). The average nodule size was 22±3 mm. On pre-operative cytology, six were suggestive of follicular neoplasm, three were differentiated thyroid cancers and two were atypia of unknown significance. All patients underwent hemi-thyroidectomy with one patient also underwent ipsilateral central compartment and lateral neck dissection robotically. Overall mean pocket dissection was 40±12 min for RA approach. Mean Robot docking time was 6.9 min. Mean operative console time for RA approach was 52.6±13 min. Mean total operative time was 101.2 min. Average blood loss during surgery was 45±16 mL. One patient was converted to open thyroidectomy because of dense posterior adhesion which subsequently came out as thyroid lymphoma on final histopathology. Average hospital stay was 1.2±0.5 days. On final histology three patients had papillary carcinoma, two patients had follicular carcinoma, nine had benign pathology, and one patient of thyroid lymphoma. One of the patients with papillary carcinoma underwent ipsilateral neck dissection with central compartment clearance in view of neck nodes on prep imaging but on final histopathology nodes were found to be free of tumor. Post operatively direct laryngoscopy was done in all cases and only one patient had restricted left vocal cord mobility with good compensation which improved in three months. Three of 16 patients initially reported temporary speech dysfunction which gradually improved in 1 month follow-up. All the patients were satisfied with the scar cosmesis. No swallowing difficulty or aspiration was reported on follow-up. No shoulder dysfunction or chyle leak was reported. All the patients are on regular follow-up with no evidence of disease.
Third author’s (Mandar Deshpande) institute has done six robotic thyroidectomies (four males and two females). All cases were hemi-thyroidectomies. Pre-operative cytology was benign in four patients and follicular neoplasm in two patients. Mean age was 42 years (range, 20–57 years). Average nodule size was 2.4 cm. Surgery could be completed robotically in five patients. In one patient, surgery had to be converted to open thyroidectomy because of oozing and not able to control bleeding robotically. Mean time to make working space was 50 min. Mean console time was 148 min. Drain was removed post-operative day 4. Mean hospital stay was 6.5 days. No patient had post-operative recurrent laryngeal nerve palsy. Final histopathology was benign in five patients. In one patient in whom the cytology was follicular neoplasm, the histopathology was follicular variant of papillary carcinoma (low risk).
Conclusions
Remote access approaches use well-hidden incisions. Robotic approaches score above endoscopic methods. RA approach may have some technical advantages for the head and neck surgeons. Sufficient cadaver and preclinical training should be undertaken. Standardized and formal teaching for robotic surgical skill is necessary. Case selection is important especially in the initial phases of the learning curve. We report the early experience and outcome of 29 cases from three institutions from India. Our early experience with robotic thyroidectomy was encouraging. Further prospective evaluation needs to be done, to see the feasibility and efficacy, especially in India.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Weinstein GS, O’Malley BW Jr, Snyder W, et al. Transoral robotic surgery: radical tonsillectomy. Arch Otolaryngol Head Neck Surg 2007;133:1220-6. [Crossref] [PubMed]
- Hamilton D, Paleri V. Role of transoral robotic surgery in current head & neck practice. Surgeon 2017;15:147-54. [Crossref] [PubMed]
- de Almeida JR, Li R, Magnuson JS, et al. Oncologic Outcomes After Transoral Robotic Surgery: A Multi-institutional Study. JAMA Otolaryngol Head Neck Surg 2015;141:1043-51. [Crossref] [PubMed]
- Burton J, Wong R, Padhya T. Robotic-Assisted Surgery in the Head and Neck. Cancer Control 2015;22:331-4. [PubMed]
- Tateya I, Shiotani A, Satou Y, et al. Transoral surgery for laryngo-pharyngeal cancer - The paradigm shift of the head and cancer treatment. Auris Nasus Larynx 2016;43:21-32. [Crossref] [PubMed]
- Singer MC, Seybt MW, Terris DJ. Robotic facelift thyroidectomy: I. Preclinical simulation and morphometric assessment. Laryngoscope 2011;121:1631-5. [Crossref] [PubMed]
- Terris DJ, Singer MC, Seybt MW. Robotic facelift thyroidectomy: II. Clinical feasibility and safety. Laryngoscope 2011;121:1636-41. [Crossref] [PubMed]
- Terris DJ, Singer MC, Seybt MW. Robotic facelift thyroidectomy: patient selection and technical considerations. Surg Laparosc Endosc Percutan Tech 2011;21:237-42. [Crossref] [PubMed]
- Byeon HK. Comprehensive application of robotic retroauricular thyroidectomy: The evolution of robotic thyroidectomy. Laryngoscope 2016;126:1952-7. [Crossref] [PubMed]
- Byeon HK, Koh YW. The new era of robotic neck surgery: The universal application of the retroauricular approach. J Surg Oncol 2015;112:707-16. [Crossref] [PubMed]
- Lang BH, Wong CK, Tsang JS, et al. A systematic review and meta-analysis comparing outcomes between robotic-assisted thyroidectomy and non-robotic endoscopic thyroidectomy. J Surg Res 2014;191:389-98. [Crossref] [PubMed]
- Lee J, Yun JH, Choi UJ, et al. Robotic versus Endoscopic Thyroidectomy for Thyroid Cancers: A Multi-Institutional Analysis of Early Postoperative Outcomes and Surgical Learning Curves. J Oncol 2012.734541. [PubMed]
- Lee J, Yun JH, Nam KH, et al. The learning curve for robotic thyroidectomy: a multicenter study. Ann Surg Oncol 2011;18:226-32. [Crossref] [PubMed]
- Lee J, Chung WY. Robotic thyroidectomy and neck dissection: past, present, and future. Cancer J 2013;19:151-61. [Crossref] [PubMed]
- Oliveira CM, Nguyen HT, Ferraz AR, et al. Robotic surgery in otolaryngology and head and neck surgery: a review. Minim Invasive Surg 2012;2012:286563.
- Berber E, Bernet V, Fahey TJ 3rd, et al. American Thyroid Association Statement on Remote-Access Thyroid Surgery. Thyroid 2016;26:331-7. [Crossref] [PubMed]
- Bhatia P, Mohamed HE, Kadi A, et al. Remote access thyroid surgery. Gland Surg 2015;4:376-87. [PubMed]
- Alabbas H, Bu Ali D, Kandil E. Robotic retroauricular thyroid surgery. Gland Surg 2016;5:603-6. [Crossref] [PubMed]
- Duncan DT, Castro MC, Gortmaker SL, et al. Racial differences in the built environment--body mass index relationship? A geospatial analysis of adolescents in urban neighborhoods. Int J Health Geogr 2012;11:11. [Crossref] [PubMed]
- Chhabra P, Chhabra SK. Distribution and determinants of body mass index of non-smoking adults in Delhi, India. J Health Popul Nutr 2007;25:294-301. [PubMed]


