Anaesthetic considerations for non-intubated thoracic surgery
Introduction
General anaesthesia with intubation and single lung ventilation has always been considered essential for thoracic surgery (1) in order to provide safe and optimal operating conditions for surgical manipulation. Over the last decade there has been a huge evolution in thoracic surgery with the development of multiport and uniportal minimally invasive techniques (2,3). Similarly, less conventional thoracic anaesthesia strategies have evolved to encompass less invasive surgical techniques and enhance fast track perioperative pathways. There is a growing interest in non-intubated techniques during which thoracic surgery is performed on patients who are spontaneously ventilating awake, under minimal sedation with the aid of local or regional anaesthesia or under general anaesthesia with a supraglottic airway device (4,5). The concept is to allow the creation of a spontaneous pneumothorax as the surgeon enters the chest. This can provide excellent lung isolation without the need for positive pressure ventilation on the dependant lung.
There are increasing numbers of publications relating to thoracoscopic minor and major lung surgeries taking place under spontaneous ventilation. Initial results are encouraging and illustrate that these techniques appear to be feasible, safe, and may be of greater benefit to the patient (6-15).
The technique does, however, present a greater technical challenge for the anaesthetist and surgical team. Thorough patient selection, strict planning, preparation and vigilance are essential. This review aims to highlight the advantages and practicalities of performing non-intubated thoracic surgery with video demonstration.
Potential advantages
Non-intubated procedures aim to minimize the adverse effects of tracheal intubation and positive pressure ventilation such as intubation related injuries (16,17), ventilation induced lung injury (18) and residual neuromuscular blockade (19).
Published data demonstrates that non-intubated techniques offer quicker recovery times, better pain scores, lower morbidity rates and shorter hospital length of stays compared with intubated surgery (6-15) and there may also be an attenuation of stress hormone and immunologic responses (15,20,21). Awake and minimal sedation techniques also avoid the need for general anaesthesia, thus maintaining a more physiological cardiopulmonary and neurological status and avoiding post-operative nausea and vomiting.
Patient selection
Initial reports of non-intubated video-assisted thoracic surgery (VATS) in the literature include lower-risk patients for relatively minor thoracic procedures. More recently, however, there is a growing body of evidence that a non-intubated technique is safe and feasible in a number of thoracic procedures including the management of pulmonary nodule resection (6,22,23), pleural and pericardial effusions (11,14), decortication for empyema (20), pneumothorax surgery (7,9,11), lung and pleural biopsy (24-26), thymectomy (27), lung volume reduction surgery (LVRS) (10,28) metastasectomy (29), and anatomical lung cancer resections including segmentectomy and lobectomy (12,13,15,30-34).
Traditionally the technique was performed on patients with American Society of Anaesthesiologists (ASA) grade 1 or 2, with a good airway, body mass index of less than 30 and no significant cardiorespiratory issues (6,7). There are now, however, increasing reports of higher risk patients undergoing non-intubated thoracic surgery such as elderly patients (13), patients with cardiorespiratory disease, interstitial lung disease (25,26), severe emphysema (10,28) and patients with muscular diseases (27,35). In theory, these are the populations of patients who will profit the most from a non-intubated technique and avoiding muscle relaxation, intubation and positive pressure ventilation. They may also benefit from an awake or minimal sedation technique and avoiding a general anaesthetic.
It is essential, however, to balance the risk-benefit of this alternative technique. The patient must still be suitable for intubation and general anaesthesia as this will be the default management if there are complications or failure of the technique. There are a few absolute and relative contraindications to the technique and these are listed in Table 1.
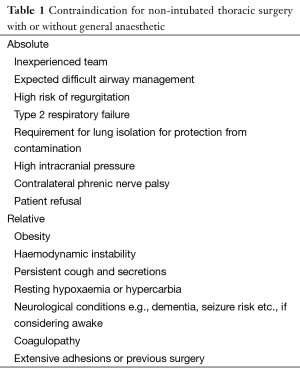
Full table
Preoperative preparation
Patient
There should always be a discussion with the patient about the risks and benefits of the technique with informed consent. Patient understanding and cooperation is vital if an awake technique is to be used. Patients should be briefed on what to expect from the theatre environment, personnel, positioning, monitoring, analgesic techniques, sedation and possible conversion to general anaesthesia.
Team
All team members, especially the anaesthetist and the surgeon should be accomplished and proficient in thoracic surgery and educated and informed regarding the technique and potential complications. The surgeon should be skilled and expert in VATS surgery and the anaesthetist experienced and comfortable with the insertion of double lumen endotracheal tubes and lung isolation in the lateral position.
The anaesthetic assistants must be well briefed in the technique and what equipment and protocols to follow should sudden conversion to general anaesthesia and intubation be required. Anaesthetic induction and emergency drugs should be immediately available, and intubation equipment must be prepared including single and double lumen tubes, a fibreoptic bronchoscope, a bronchial blocker and advanced airway equipment.
Complications should be anticipated and prevented if possible with good judgement to appropriately abandon or convert to conventional intubated general anaesthesia as required.
Monitoring
Minimum standards of monitoring in clinical anaesthesia are set out in guidelines issued by professional bodies (36). During non-intubated VATS, the monitoring employed will be dependant on the patient comorbidities and the surgical procedure.
As a minimum, a 3-lead electrocardiogram, non-invasive blood pressure monitoring and pulse oximetry should be used. End-tidal carbon dioxide monitoring should be employed to monitor airway patency, respiratory rate and pattern but also for early detection of hypercapnia during sedation and one lung spontaneous ventilation. This can be monitored by inserting the detector into the patient’s nostril, attaching to the oxygen mask or via the gas delivery circuit if using a tight fitting mask or supraglottic airway device. Depth of anaesthesia monitoring, such as bispectral index monitoring (BIS), is extremely helpful in guiding sedation and anaesthesia in these patients.
Additional non-invasive and invasive monitoring devices may be utilised depending on the patient’s condition, surgical experience, expected surgical operation time and possible intraoperative risks. In our institution we no longer routinely use invasive monitoring for minor non-intubated VATS procedures.
Figures 1 and 2 demonstrate the typical monitoring during a non-intubated VATS pneumothorax surgery under general anaesthesia with laryngeal mask airwayTM. Figure 1 includes ECG, pulse oximetry trace, end-tidal carbon dioxide and gas monitoring (including oxygen and sevoflurane), BIS monitoring and non-invasive blood pressure monitoring. Figure 2 shows ventilation and spirometry monitoring.
The patient is spontaneously ventilating on one-lung. It is clear from the spirometry and end-tidal carbon dioxide monitoring that the respiratory pattern is stable with tidal volumes of 200–230 mL, a respiratory rate of 18 and minute ventilation of 3.5 L/min. There is no compromise of oxygenation with peripheral oxygen saturations of 98% on 46% oxygen. End tidal carbon dioxide levels are at 7.1 kPa, although this is not causing any compromise to the patient.
Awake/sedation/general anaesthesia
It is important to understand the different options available when implementing a non-intubated technique. Non-intubated VATS purely describes the use of a technique that avoids an endotracheal tube. This may be performed fully awake, under minimal sedation or under deep sedation or general anaesthesia. The data published to date can be somewhat confusing when describing the sedation or anaesthetic technique. Some authors consistently use the comparison “non-intubated versus general anaesthesia” and some describe the technique as sedation when the patients are technically under general anaesthesia (30).
Awake (BIS 90–100)
The majority of early reports of non-intubated techniques were in patients who were awake under thoracic epidural blockade (6-11) for minor VATS procedures. These patients, however, all received pre medication with midazolam, either orally, intramuscularly or intravenously prior to epidural placement. Oxygen is delivered via nasal cannula or facemask.
Sedation (BIS 60–90)
More recently, the use of light sedation has been reported and allows the patient to better tolerate the surgical procedure and decreases anxiety and discomfort. With the use of sedation, less invasive regional techniques can be employed, such as intercostal nerve blocks and paravertebral blocks. Target-controlled sedation is currently the most popular technique in the literature for non-intubated VATS, although depth of sedation can vary markedly between centres. Short acting agents such as propofol and remifentanil either separately or together in a target-controlled infusion are often used as the first choice (12,13,22,32-34,39,40). They can be easily titrated to achieve the desired sedation level to provide anxiolysis without losing responsiveness. These drugs, however, should be titrated by an anaesthetist experienced in their use, as target plasma levels can differ greatly between patients. It is important not to compromise spontaneous ventilation and airway reflexes and care must be taken, especially with remifentanil, to prevent hypercapnia and apnoea. Other drugs used for mild sedation may include dexmedetomidine and midazolam which are less tritable.
In lightly sedated patients, oxygen delivered via a facemask or nasal cannula is often adequate and is most commonly used. End tidal carbon dioxide monitoring is, however, recommended, to ensure airway patency, spontaneous ventilation and confirm respiratory rate and pattern.
General anaesthesia (BIS
General anaesthesia (or “deep sedation”) has also been utilized in non-intubated VATS procedures (23,30,31). A general anaesthetic technique prevents problems with patient anxiety and distress and minimizes coughing and movement during the procedure. General anaesthesia can be provided with volatile anaesthetics or a total intravenous target-controlled technique with propofol and remifentanil. Although these techniques have been described in the literature without formal airway support, we would recommend that it is essential. Airway control and oxygen delivery via a closed circuit should be employed with end-tidal gas monitoring. This can be via fitted facemask with airway support or supraglottic airway device.
It can be argued that awake and minimal sedation techniques, which avoid the need for general anaesthesia, maintain a more physiological cardiopulmonary and neurological status and avoid postoperative nausea and vomiting. However, general anaesthesia with a supraglottic airway device is the technique that provides a more stable airway and facilitates oxygenation in cases where an unexpected conversion to open thoracotomy is needed. In our institution we use a combination of oxygen, air and sevoflurane delivered via a supraglottic airway device to provide general anaesthesia during which our patients are unresponsive but without compromise of spontaneous ventilation. Non-intubated general anaesthesia with a supraglottic device may also provide a smoother conversion to intubation with enhanced preoxygenation and no additional requirement for induction of general anaesthesia. An epidural is not essential and regional blockade such as intercostal or paravertebral blocks can be performed once the patient is asleep and in the lateral position.
Regional techniques
Various regional anaesthesia techniques have been described for use in non-intubated VATS procedures. These include local wound infiltration, serratus anterior plane blocks, intercostal nerve blocks, thoracic paravertebral block and thoracic epidural block.
Thoracic epidural analgesia
Thoracic epidural analgesia has been the mainstay of thoracic anaesthetic practice for many years and provides arguably the best pain relief. However, thoracic epidural block is associated with a number of rare but serious complications including nerve injury, epidural abscess and haematoma (41). There are also other significant disadvantages such as difficult placement, failure, inadequate block and sympathetic block and hypotension. The latter often leads to fluid boluses or the need for vasopressors, central line and urinary catheter insertion; which may delay patient mobility, recovery and discharge.
Enhanced recovery programs for thoracic surgery discourage the systematic use of epidural blocks for both video-assisted and open thoracic surgery and encourage the use of alternative regional techniques such as intercostal nerve blocks and paravertebral block (42). In our institution we now very rarely use epidural block and prefer to use intercostal nerve blocks or paravertebral blocks in both our intubated and non-intubated thoracic surgery patients.
Other techniques
Paravertebral blocks can be placed either as single shot block at multiple levels (for example with simple VATS procedures), or via placement of a catheter with an infusion of local anaesthetic for longer or more complex procedures, these may be placed by the anaesthetist or under direct vision by the surgeon. Multilevel intercostal nerve blocks are also commonly utilised and are effective at controlling pain.
Initial published reports on non-intubated surgery utilised thoracic epidural anaesthesia for three-port conventional VATS performed awake or under minimal sedation (6-11,15,32,39,40). However, for simpler procedures or single port VAT surgery, epidural anaesthesia is now not deemed necessary and intercostal nerve blocks and paravertebral block are becoming more popular with the use of targeted sedation (24,25,30,31,33,34,40). These less invasive techniques have also been shown to provide better postoperative outcomes (26).
With the development of the single-port VATS technique, major lung resection surgery is also now being performed under single shot paravertebral or intercostal nerve block and sedation, without the need for epidural (31,34).
Multimodal analgesia
Regardless of the regional technique utilised, a ‘multimodal’ approach to analgesia is recommended. In addition to the regional block, all patients should be prescribed paracetamol, either as an oral dose prior to coming to theatre, or loaded with an intravenous preparation during the case. Paracetamol should be continued regularly postoperatively. Non-steroidal anti-inflammatory agents are highly effective analgesics, but their use is limited by concerns about renal and gastrointestinal side effects. A single dose of a COX-2 inhibitor such as parecoxib intraoperatively, however, has lower rates of gastrointestinal side effects.
Opiates are also commonly used in combination with the regional technique. Fentanyl and morphine being the most popular choices. These can be titrated to the patient’s physiological responses during surgery and can be used in a patient controlled analgesic model post-operatively.
Facilitating surgery
Lung collapse
During non-intubated thoracic surgery, the lung collapses due to the creation of an iatrogenic pneumothorax. This requires the maintenance of a patent airway, spontaneous ventilation to provide the negative pressure in the pleural space, and the absence of positive pressure on the lung. Lung collapse appears to be comparable to double lumen intubation and one-lung ventilation with adequate surgical field and feasibility. In the case of air trapping and severe adhesions, however, lung collapse may be problematic as is the case during intubated surgery. In a minority of cases, inadequate collapse and troublesome movements of the mediastinum and diaphragm may impede surgical ability.
Figure 3 demonstrates a non-intubated VATS lung biopsy carried out by a trainee surgeon. Note the lung collapse and space provided for surgical manipulation. There is clear movement of the mediastinum and diaphragm as the patient breaths spontaneously but no impedance of surgical feasibility.
Re-expansion
Re-expansion of the collapsed lung can be achieved in a number of ways. With an awake patient, they can be asked to breathe deeply and cough to re-expand the lung. Alternatively, positive pressure can be administered via a facemask or through the supraglottic airway device, while patient breaths spontaneously.
Complications
Hypoxia
Non-intubated VATS surgery relies on the creation of a pneumothorax with collapse of the lung down to the functional residual capacity. This allows adequate space for surgical manouvres. The hypoxia which results from the creation of this open pneumothorax is, however, usually minimal and can be easily treated using supplementary oxygen via nasal cannula, Venturi mask or fitted masks and supraglottic airway devices if under deep sedation and general anaesthesia.
Hypercapnia
Hypercapnia can result from hypoventilation during non-intubated surgery. This can be particularly exacerbated by sedation or general anaesthesia. Our institutional series of non-intubated general anaesthesia cases showed an increase in end tidal carbon dioxide in comparison with an intubated technique (unpublished data). In patients with elevated pulmonary pressures, raised intracranial pressures and arrhythmias this should be avoided, however, “permissive hypercapnia” is a recognized ventilation technique, it is usually well tolerated and resolves immediately post-surgery (33,44).
Cough
Unpredicted lung movement and cough during non-intubated VATS can create problems for the surgeon. Inadequate regional blockade or sedation may result in hyper-reactivity or cough, however, even with adequate blockade and sedation, manipulation of the bronchi, may stimulate a cough reflex. Epidural associated sympathetic block can also lead to increased bronchial tone and hyper-reactivity.
Different techniques have been employed in an attempt to prevent this. Sedation with remifentanil may help to avoid the cough reflex (31), however, this should be managed carefully as an overdosage may cause respiratory depression and apnoea. Specific groups have advocated the use of vagal nerve blockade, which can be performed under direct vision by the surgeon safely and with good effect (12,30,39,40), lignocaine spray to the surface of the lung has been employed and may also prove beneficial (32) or the administration of inhaled or nebulized lignocaine prior to the procedure (5) may help to prevent this complication.
Conversion to intubated thoracic anesthesia
Conversion to an intubated general anaesthetic technique is required occasionally in non-intubated VATS procedures. Reasons for conversion can be divided into surgical issues such as challenging mediastinal, lung or diaphragm movement, inadequate collapse, dense adhesions, bleeding or conversion to thoracotomy; and anaesthetic complications such as the presence of severe hypoxia, persistent hypercapnia and acidosis, airway compromise, haemodynamic instability, inadequate regional blockade or patient anxiety. The incidence of conversion is reported as 0% (24) to 10% (12) and is dependant on the procedure and team experience. In a subgroup of lobectomies the incidence has been reported to rise to 13% (12).
Indications and the procedure for conversion should be discussed with all team members prior to undertaking non-intubated surgery. The ultimate decision to convert, however, lies with the consultant surgeon and anaesthetist.
Elective conversion is always preferable to emergency conversion if at all possible and early, unexpected difficulties should be assessed carefully to prevent having to convert in an emergency due to severe life threatening complications.
Different teams have different procedures for conversion and this will depend on the patient’s anatomy, the reason for conversion and anaesthetist preference. In our institution, our default plan for conversion is to perform intubation in the lateral position with the chest remaining open and to attempt to intubate initially with a double lumen tube and secure lung isolation. This is aided by the fact that our patients are usually under general anaesthesia with a supraglottic airway device which can be used to pre oxygenate with positive pressure if required prior to intubation and muscle relaxation is delivered without the need for anaesthetic induction.
Other centres, however, proceed by closing the surgical wounds with sealed dressings and inserting a chest drain to aid lung expansion prior to induction and intubation in either the lateral or supine position (33). If in the lateral position, a number of centres advocate the use of a bronchoscope to guide single lumen tube intubation, followed by insertion of a bronchial blocker (31,33).
Whatever the conversion technique, it is essential that team members are aware and prepared. Preoxygenation where possible should be administered, rapid acting induction and neuromuscular blocking drugs should be used and a selection of intubation aids should be available including a fibreoptic bronchoscope.
Post-operative management
Current evidence indicates that non-intubated VATS confers a reduction in recovery room time, post-operative pain and earlier mobilization and discharge without any differences in complications and mortality (6-15).
In our institution, there is no difference in the protocols and procedures relating to the post-operative management of our non-intubated and intubated VATS patients. Patients are discharged to a dedicated thoracic surgical ward and are not admitted to intensive care or high dependency care unless organ support or advanced monitoring is required. We promote and encourage an enhanced recovery program for all thoracic patients. Post operative management therefore encompasses intravenous fluid maintenance for 12 hours post operatively, reinstatement of oral fluid and foods within 4 hours and aggressive pain control by consultant anaesthetists. All patients get an opioid based patient controlled analgesia for the first 12 hours to supplement regional or local anaesthesia as well as oral multimodal analgesia. In addition, patients are under intense physiotherapy and mobilization within 12 hours. Patients have only a single chest drain inserted and are managed with a portable chest drainage system with nurse led drain removal based on digital measurement.
As in keeping with the published data, our institution sees a decrease in recovery time, better pain relief, a decrease in oxygen requirement and reduced length of stay in our non-intubated patients (unpublished data at time of writing).
Further video examples
Figures 4 and 5 demonstrate the intra-operative combination of monitoring, anaesthetic technique and performance of surgery related to non-intubated procedures.
Figure 4 shows an operating room view of a non-intubated VATS lung biopsy using a spontaneous general anaesthetic technique with LMATM. This demonstrates the monitoring and ventilation, shows the positioning of the patient and LMATMin situ, the thoracoscopic view and lung isolation for surgical manipulation and the uniportal surgical technique employed.
Figure 5 demonstrates a non-intubated VATS procedure which required conversion to mini-thoracotomy. This was performed successfully under spontaneous ventilation without the need for conversion to an intubated technique.
Conclusions
Non-intubated anaesthetic techniques for thoracic surgery are innovative and exciting and drive to reduce the invasiveness of the procedures. We recommend that centres starting out with non-intubated techniques begin by performing minor VATS procedures in selected low risk patients. Early elective conversion should be employed in any unexpected surgical difficulty or cardiopulmonary problem during the learning curve to reduce the risk of emergency conversion and complications. Further research is needed to establish which patients benefit from this technique and the real impact on perioperative mortality and morbidity.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ghosh S, Latimer RD, editors. Thoracic Anaesthesia: Principles and Practice. Oxford: Butterworth-Heinemann, 1999.
- Rocco G, Martucci N, La Manna C, et al. Ten-year experience on 644 patients undergoing single-port (uniportal) video-assisted thoracoscopic surgery. Ann Thorac Surg 2013;96:434-8. [Crossref] [PubMed]
- Ng CS, Gonzalez-Rivas D, D'Amico TA, et al. Uniportal VATS-a new era in lung cancer surgery. J Thorac Dis 2015;7:1489-91. [PubMed]
- Pompeo E, Sorge R, Akopov A, et al. Non-intubated thoracic surgery-A survey from the European Society of Thoracic Surgeons. Ann Transl Med 2015;3:37. [PubMed]
- Gonzalez-Rivas D, Bonome C, Fieira E, et al. Non-intubated video-assisted thoracoscopic lung resections: the future of thoracic surgery? Eur J Cardiothorac Surg 2016;49:721-31. [Crossref] [PubMed]
- Pompeo E, Mineo D, Rogliani P, et al. Feasibility and results of awake thoracoscopic resection of solitary pulmonary nodules. Ann Thorac Surg 2004;78:1761-8. [Crossref] [PubMed]
- Pompeo E, Tacconi F, Mineo D, et al. The role of awake video-assisted thoracoscopic surgery in spontaneous pneumothorax. J Thorac Cardiovasc Surg 2007;133:786-90. [Crossref] [PubMed]
- Pompeo E, Tacconi F, Mineo TC. Comparative results of non-resectional lung volume reduction performed by awake or non-awake anesthesia. Eur J Cardiothorac Surg 2011;39:e51-8. [Crossref] [PubMed]
- Noda M, Okada Y, Maeda S, et al. Is there a benefit of awake thoracoscopic surgery in patients with secondary spontaneous pneumothorax? J Thorac Cardiovasc Surg 2012;143:613-6. [Crossref] [PubMed]
- Pompeo E, Rogliani P, Tacconi F, et al. Randomized comparison of awake nonresectional versus nonawake resectional lung volume reduction surgery. J Thorac Cardiovasc Surg 2012;143:47-54, 54.e1.
- Pompeo E, Dauri M; Awake Thoracic Surgery Research Group. Is there any benefit in using awake anesthesia with thoracic epidural in thoracoscopic talc pleurodesis? J Thorac Cardiovasc Surg 2013;146:495-7.e1.
- Chen JS, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lobectomy for lung cancer. Ann Surg 2011;254:1038-43. [Crossref] [PubMed]
- Wu CY, Chen JS, Lin YS, et al. Feasibility and safety of nonintubated thoracoscopic lobectomy for geriatric lung cancer patients. Ann Thorac Surg 2013;95:405-11. [Crossref] [PubMed]
- Mineo TC, Sellitri F, Tacconi F, et al. Quality of life and outcomes after nonintubated versus intubated video-thoracoscopic pleurodesis for malignant pleural effusion: comparison by a case-matched study. J Palliat Med 2014;17:761-8. [Crossref] [PubMed]
- Liu J, Cui F, Li S, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. [Crossref] [PubMed]
- Fitzmaurice BG, Brodsky JB. Airway rupture from double-lumen tubes. J Cardiothorac Vasc Anesth 1999;13:322-9. [Crossref] [PubMed]
- Miñambres E, Burón J, Ballesteros MA, et al. Tracheal rupture after endotracheal intubation: a literature systematic review. Eur J Cardiothorac Surg 2009;35:1056-62. [Crossref] [PubMed]
- Lohser J, Slinger P. Lung Injury After One-Lung Ventilation: A Review of the Pathophysiologic Mechanisms Affecting the Ventilated and the Collapsed Lung. Anesth Analg 2015;121:302-18. [Crossref] [PubMed]
- Murphy GS, Szokol JW, Avram MJ, et al. Postoperative residual neuromuscular blockade is associated with impaired clinical recovery. Anesth Analg 2013;117:133-41. [Crossref] [PubMed]
- Tacconi F, Pompeo E, Sellitri F, et al. Surgical stress hormones response is reduced after awake videothoracoscopy. Interact Cardiovasc Thorac Surg 2010;10:666-71. [Crossref] [PubMed]
- Vanni G, Tacconi F, Sellitri F, et al. Impact of awake videothoracoscopic surgery on postoperative lymphocyte responses. Ann Thorac Surg 2010;90:973-8. [Crossref] [PubMed]
- Tseng YD, Cheng YJ, Hung MH, et al. Nonintubated needlescopic video-assisted thoracic surgery for management of peripheral lung nodules. Ann Thorac Surg 2012;93:1049-54. [Crossref] [PubMed]
- Ambrogi MC, Fanucchi O, Korasidis S, et al. Nonintubated thoracoscopic pulmonary nodule resection under spontaneous breathing anesthesia with laryngeal mask. Innovations (Phila) 2014;9:276-80. [Crossref] [PubMed]
- Katlic MR, Facktor MA. Video-assisted thoracic surgery utilizing local anesthesia and sedation: 384 consecutive cases. Ann Thorac Surg 2010;90:240-5. [Crossref] [PubMed]
- Pompeo E, Rogliani P, Cristino B, et al. Awake thoracoscopic biopsy of interstitial lung disease. Ann Thorac Surg 2013;95:445-52. [Crossref] [PubMed]
- Ambrogi V, Mineo TC. VATS biopsy for undetermined interstitial lung disease under non-general anesthesia: comparison between uniportal approach under intercostal block vs. three-ports in epidural anesthesia. J Thorac Dis 2014;6:888-95. [PubMed]
- Matsumoto I, Oda M, Watanabe G. Awake endoscopic thymectomy via an infrasternal approach using sternal lifting. Thorac Cardiovasc Surg 2008;56:311-3. [Crossref] [PubMed]
- Mineo TC, Pompeo E, Mineo D, et al. Awake nonresectional lung volume reduction surgery. Ann Surg 2006;243:131-6. [Crossref] [PubMed]
- Pompeo E, Mineo TC. Awake pulmonary metastasectomy. J Thorac Cardiovasc Surg 2007;133:960-6. [Crossref] [PubMed]
- Hung MH, Hsu HH, Chen KC, et al. Nonintubated thoracoscopic anatomical segmentectomy for lung tumors. Ann Thorac Surg 2013;96:1209-15. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Single-port thoracoscopic lobectomy in a nonintubated patient: the least invasive procedure for major lung resection? Interact Cardiovasc Thorac Surg 2014;19:552-5. [Crossref] [PubMed]
- Guo Z, Shao W, Yin W, et al. Analysis of feasibility and safety of complete video-assisted thoracoscopic resection of anatomic pulmonary segments under non-intubated anesthesia. J Thorac Dis 2014;6:37-44. [PubMed]
- Chen KC, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic lung resection: a 3-year experience with 285 cases in a single institution. J Thorac Dis 2012;4:347-51. [PubMed]
- Gonzalez-Rivas D, Fernandez R, de la Torre M, et al. Uniportal video-assisted thoracoscopic left upper lobectomy under spontaneous ventilation. J Thorac Dis 2015;7:494-5. [PubMed]
- Al-Abdullatief M, Wahood A, Al-Shirawi N, et al. Awake anaesthesia for major thoracic surgical procedures: an observational study. Eur J Cardiothorac Surg 2007;32:346-50. [Crossref] [PubMed]
- Recommendations for Standards of Monitoring During Anaesthesia and Recovery. 4th Edition. [Accessed on 16 January 2016]. Available online: https://www.aagbi.org/sites/default/files/standardsofmonitoring07.pdf
- Irons JF, Martinez G. The typical monitoring during a non-intubated VATS pneumothorax surgery under general anaesthesia with laryngeal mask airwayTM. Asvide 2016;3:180. Available online: http://www.asvide.com/articles/936
- Irons JF, Martinez G. Ventilation and spirometry monitoring. Asvide 2016;3:181. Available online: http://www.asvide.com/articles/937
- Chen KC, Cheng YJ, Hung MH, et al. Nonintubated thoracoscopic surgery using regional anesthesia and vagal block and targeted sedation. J Thorac Dis 2014;6:31-6. [PubMed]
- Dong Q, Liang L, Li Y, et al. Anesthesia with nontracheal intubation in thoracic surgery. J Thorac Dis 2012;4:126-30. [PubMed]
- NAP 3. The 3rd National Audit Project of the Royal College of Anaesthetists. Major Complications of Central Neuraxial Block in the United Kingdom. [Accessed on 18 January 2016]. Available online: http://www.rcoa.ac.uk/system/files/CSQ-NAP3-Full_1.pdf
- Jones NL, Edmonds L, Ghosh S, et al. A review of enhanced recovery for thoracic anaesthesia and surgery. Anaesthesia 2013;68:179-89. [Crossref] [PubMed]
- Irons JF, Martinez G. A non-intubated VATS lung biopsy carried out by a trainee surgeon. Asvide 2016;3:182. Available online: http://www.asvide.com/articles/938
- Pompeo E. State of the art and perspectives in non-intubated thoracic surgery. Ann Transl Med 2014;2:106. [PubMed]
- Irons JF, Martinez G. An operating room view of a non-intubated VATS lung biopsy using a spontaneous general anaesthetic technique with LMATM. Asvide 2016;3:183. Available online: http://www.asvide.com/articles/939
- Irons JF, Martinez G. A non-intubated VATS procedure which required conversion to mini-thoracotomy. Asvide 2016;3:184. Available online: http://www.asvide.com/articles/940
Cite this article as: Irons JF, Martinez G. Anaesthetic considerations for non-intubated thoracic surgery. J Vis Surg 2016;2:61.


