Noninvasive computed tomography-guided marking technique for peripheral pulmonary nodules
Introduction
Peripheral small pulmonary nodules such as ground glass opacities (GGO) and possible lung metastases require a tissue diagnosis. Minimally invasive thoracoscopic wedge resection (TWR) is a good therapeutic option for these peripheral pulmonary nodules. However, in some cases, it is difficult to identify the exact location of a small peripheral, but not subpleural, nodule during TWR. In such cases, preoperative marking is often employed (1-5). Although preoperative CT-guided marking techniques are the most common, most of them require puncture of the visceral pleura (VP). CT-guided hookwire placement before resection has been performed, but is subject to complications such as pneumothorax, hemothorax, and air embolism from puncture of the VP (6,7). A CT-guided marking technique that does not puncture the VP is less prone to these complications. We developed and performed a marking technique using CT guidance that does not involve VP puncture, based on the report of Nishida et al. (8).
Methods
This study was an exploratory, single-armed study approved by the ethics committee of our institution (No. 1114), and written informed consent was obtained from each patient. The indication for marking was a histologically undiagnosed peripheral pulmonary nodule or nodules ≤20 mm in diameter designated for TWR. Fifty-four patients were enrolled in this study from October 2012 to April 2016.
Technique
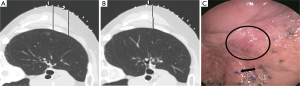
Our hospital is a referral center, so the patients had undergone initial CT scanning at other institutions. Patients with small peripheral pulmonary nodules are generally followed for at least 3 months using thin-section CT (TSCT). TWR is reserved for nodules. Preoperative CT scans were performed 1 day before the operation. Patients were placed in the lateral decubitus position to best approximate their position during TWR, using radiopaque markers on the body surface. Scans were acquired in the maximal expiratory phase. A mark was placed on the patient’s skin at the shortest distance from the nodule (Figure 1A). At operation, patients received general anesthesia and were placed in the lateral decubitus position with the side to be operated uppermost. After the relevant lung was collapsed and the thoracic cavity was entered though either one or two trocar ports, a 16-gauge indwelling catheter (Surflo®, Terumo Corporation, Tokyo, Japan) was inserted perpendicular to the skin surface through the chest wall at the mark and into the thoracic cavity (Figure 1B). The needle was removed and the external catheter hub was fixed to the thoracic wall. After reinflating the lung, a φ 1.0 mm epidural catheter (Hakko Medical, Tokyo, Japan) containing gentian violet dye was inserted through the indwelling catheter. The tip of the catheter touched and tattooed the VP of the inflated lung (Figure 1C), which was identifiable after deflation of the lung (Figure 1D). We usually palpated around the marking point using endoscopic instruments and fingers through the port site, and then TWR was performed using endoscopic staplers.
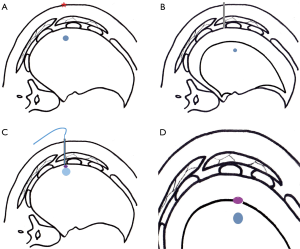
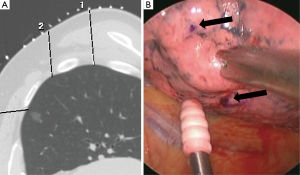
During the preoperative CT, we usually put one mark on the VP for one pulmonary nodule (one-point method, Figure 2). However, if the nodule was located beneath the scapula or ribs, the shortest distance to the nodule may not be a straight vertical line. In such situations, we performed a two-point method. Two marks were placed on the patient’s skin in the same axial plane in the CT examination and the VP tattooing followed. During the operation, the two tattoo points were identified, and we palpated the nodule along the line connecting these two points (Figure 3).
Results
Patient characteristics are shown in Table 1. In this study, ground-glass nodules (GGNs) on preoperative TSCT findings were observed in forty patients (74%). Cases included 39 primary lung cancers, 10 metastatic lung tumors, and 5 benign tumors. The mean tumor size was 10 mm (range, 3–20 mm) and the mean distance of the tumor from the VP was 4 mm (range, 0–17 mm). The one-point method was performed in 41 patients and the two-point method was performed in 13 patients. The mean distance from the nodule to the marking point was 7.0 mm (rage, 0–30 mm). The mean intraoperative marking time was 3.5 min (range, 1–4.5 min). Complications of this procedure were seen in one patient, who developed a hematoma of the chest wall because of injury to an intercostal artery. We could not detect a nodule in one patient because of insufficient collapse of the lung. In the other 53 patients (98%), we detected the nodules and performed successful TWR.

Full table
Discussion
Indications for surgical resection of small pulmonary nodules have been increasing due to recent advancements in CT screening. TWR is a minimally invasive approach to obtain a pathologic diagnosis and may be curative. However, sometimes the target nodule is not readily palpable and time is required to detect it. Preoperative marking allows quick intraoperative identification.
There are two preoperative marking techniques, CT-guided and bronchoscope-guided (3,8). In CT-guided marking technique, percutaneous hookwire placement is the most common procedure (4,5). Hookwire placement is relatively easy for nodule localization. However, puncture of the VP is an associated hazard that may result in complications such as air embolism (6,7). Similar techniques using insertion of pigment or contrast media may carry the same risk because of puncture of the VP. To avoid these complications, several marking techniques without VP puncture have been reported (8,9). We already reported the efficacy and feasibility of CT-guided nodule marking in 2015 (10). Compared with contrast media, gentian violet is easy to see with the naked eye, obviating the need for exposure of radiation during surgery.
Bronchoscope-guided marking techniques can also be performed without puncturing the VP (3,11). However, these marking techniques need both expensive equipment and expert skills. In addition, these techniques are more painful and invasive than CT-guided techniques. Preoperative marking techniques for peripheral pulmonary nodules require a balance among accuracy, technical ease, and minimal invasiveness.
In our experience, NICTM has two limitations. One is that there is no information on the depth of the nodule from the VP. For nodules located >30 mm from the VP, thoracoscopic segmentectomy is necessary to obtain appropriate surgical margins. The other limitation involves the inflation of the lung before tattooing the VP. In this study, we missed one nodule during surgery because of the marking was slipped off from the nodule. We have been waiting >1 minute after inflating the lung to achieve full expansion before tattooing. In addition, sufficient collapse of the lung is important to palpate nodules after marking, requiring close collaboration with the anesthesiologist.
Conclusions
Noninvasive CT-guided marking without puncturing the VP is a feasible and effective procedure to localize peripheral pulmonary nodules prior to TWR.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was an exploratory, single-armed study approved by the ethics committee of our institution (No. 1114), and written informed consent was obtained from each patient.
References
- Sugi K, Kaneda Y, Hirasawa K, et al. Radioisotope marking under CT guidance and localization using a handheld gamma probe for small or indistinct pulmonary lesions. Chest 2003;124:155-8. [Crossref] [PubMed]
- Willekes L, Boutros C, Goldfarb MA. VATS intraoperative tattooing to facilitate solitary pulmonary nodule resection. J Cardiothorac Surg 2008;3:13. [Crossref] [PubMed]
- Okumura T, Kondo H, Suzuki K, et al. Fluoroscopy-assisted thoracoscopic surgery after computed tomography-guided bronchoscopic barium marking. Ann Thorac Surg 2001;71:439-42. [Crossref] [PubMed]
- Sortini D, Feo C, Maravegias K, et al. Intrathoracoscopic localization techniques. Review of literature. Surg Endosc 2006;20:1341-7. [Crossref] [PubMed]
- Ciriaco P, Negri G, Puglisi A, et al. Video-assisted thoracoscopic surgery for pulmonary nodules: rationale for preoperative computed tomography-guided hookwire localization. Eur J Cardiothorac Surg 2004;25:429-33. [Crossref] [PubMed]
- Sakiyama S, Kondo K, Matsuoka H, et al. Fatal air embolism during computed tomography-guided pulmonary marking with a hook-type marker. J Thorac Cardiovasc Surg 2003;126:1207-9. [Crossref] [PubMed]
- Horan TA, Pinheiro PM, Araújo LM, et al. Massive gas embolism during pulmonary nodule hook wire localization. Ann Thorac Surg 2002;73:1647-9. [Crossref] [PubMed]
- Nishida T, Fujii Y, Akizuki K. Preoperative marking for peripheral pulmonary nodules in thoracoscopic surgery: a new method without piercing the pulmonary parenchyma. Eur J Cardiothorac Surg 2013;44:1131-3. [Crossref] [PubMed]
- Kawada M, Okubo T, Poudel S, et al. A new marking technique for peripheral lung nodules avoiding pleural puncture: the intrathoracic stamping method. Interact Cardiovasc Thorac Surg 2013;16:381-3. [Crossref] [PubMed]
- Matsuura Y, Mun M, Nakagawa K, et al. Efficacy and feasibility of a novel and noninvasive computed tomography-guided marking technique for peripheral pulmonary nodules. J Thorac Cardiovasc Surg 2015;149:1208-9. [Crossref] [PubMed]
- Sato M, Omasa M, Chen F, et al. Use of virtual assisted lung mapping (VAL-MAP), a bronchoscopic multispot dye-marking technique using virtual images, for precise navigation of thoracoscopic sublobar lung resection. J Thorac Cardiovasc Surg 2014;147:1813-9. [Crossref] [PubMed]


