Urinothorax: a systematic review
Introduction
Urinothorax (UT), or accumulation of urine in the pleural space, is a very rare cause of pleural effusion (PE). Although some authors consider that the first case was described by France and Back in 1954 (1), for most, UT was first described by Corriere et al. in 1968, in two patients and reproduced in mongrel dogs after the obstruction of both ureters (2). Until January 2006, only 58 cases had been published (3), most being isolated cases and small series involving no more than four patients.
There are no studies with large series describing the characteristics of UT patients. Our goal was to document the clinical and radiological characteristics of these patients, assess the most common causes of UT, analyze the characteristics of pleural fluid (PF), establish whether there is a relationship between the cause of UT and biochemical characteristics of PE, and assess what constitutes the most effective management of UT according to the cause, through a systematic review.
Methods
This systematic review employed a methodology based on the principles of the PRISMA study (Preferred Reporting Items for Systematic reviews and Meta-Analyses) (4). Because there are insufficient large series that respond to the needs of the study, the cases described in the literature were added using this methodology.
Selection criteria
Deemed eligible for inclusion were all cases of any age published in any format, except abstracts of papers presented at conferences and editorials, reviews, or letters to the editor that did not document new cases.
Sources of information
The search strategy included several sources of free databases available by the year of publication, although the full text of the study had to be in English, French, Portuguese or Spanish. The literature search included the following electronic databases (online): Medline (through PubMed interface), Embase and Scopus. Searches were conducted between October 1 and October 31, 2016 for (ME Toubes, A Lama and L Valdés). The following search terms were adopted for each database: urinothorax OR urothorax.
In addition to the electronic data bases consulted, a manual search was performed of reference lists of the included articles. We included any studies fulfilling the above criteria, and then independently screened and assessed each article identifying those we considered potentially relevant. Studies were reviewed in three stages based on the tittle, abstract and then full text with consensus sought at each stage of review.
Data collection process
Data from selected studies were extracted electronically (Microsoft Excel 2010, Microsoft Corp., USA). The information extracted included: authors, data of publication, number of cases in the series, age, gender, presence of dyspnea, cough and fever, time between the cause that originated the PE and the intervention with thoracentesis, side and size of PE, existence of ascites, cause of UT, relationship between the side of the obstructive uropathy and the side of the PE, diagnostic criteria, smell of PF, characteristics of PE [red blood cells, total and percentage nucleated cell count, proteins, PF/serum (PF/S) protein ratio, lactate dehydrogenase (LDH), PF/S LDH ratio, characteristics of transudate or exudate according to Light’s criteria, cholesterol, glucose, PF/S glucose ratio, pH, PF/S creatinine, and carcinoembryonic antigen], culture of PF, treatments received and their response, complications and deaths.
Methodological quality of individual studies
Because the articles reviewed were mostly case descriptions, their quality was not assessed in relation to assessment of study type, internal validity, generalizability, heterogeneity, and precision.
Outcomes of interest
Outcomes of interest were to know the patient demographic data; associated diseases; causes of UT, biochemical, microbiological and cytological characteristics of the PE, and the response to various treatments.
Statistical analysis
Due to the wide heterogeneity and descriptive nature of the studies, simple statistics (proportion, median and range) of each outcome of interest were calculated.
Results
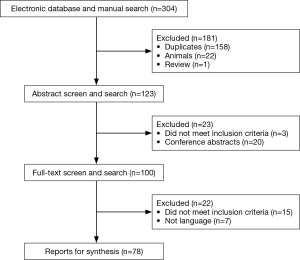
Seventy eight studies involving 88 patients were selected for review, spanning a period of 62 years. Figure 1 presents a flowchart showing a complete breakdown (2,5-24) of how (25-44) appropriate studies (45-64) were identified (65-81), corresponding to isolated case reports (between 1 and 4 cases per article).
Demographic and clinical characteristics
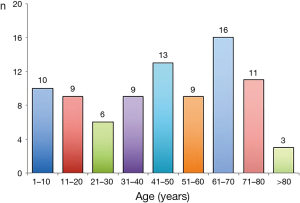
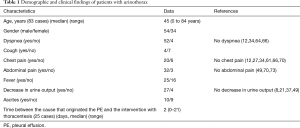
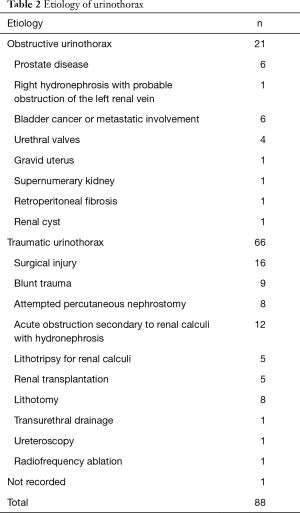
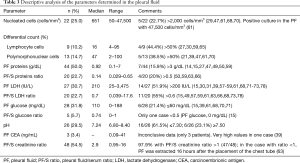
Clinical and demographic characteristics of the 88 patients included in the study are shown in Table 1, and age-group distribution is shown in Figure 2. Median age was 45 years (range, 0–84 years); age was not reported in 2 cases. UT occurred in all age groups, more commonly in men than in women (54/34; 61.4% ratio 1.6). Most patients had dyspnea (52/56; 92.8%), chest pain (20/26; 76.9%), abdominal pain (32/35; 91.4%), decreased urine output (27/31; 87%) and, to a lesser extent, fever (25/41; 61%) and ascites (10/19; 52.6%). Table 2 shows the etiology of UT. Most cases (66/87; 76%) were of traumatic origin and the remainder were due to obstructive uropathy (21; 24%). The cause was not mentioned in one case (15).
Full table
Full table
PE
PE was unilateral in 74 patients (87%), right-sided in 43 (58.1%) and left-sided in 31 (41.9%). In 11 patients, PE was bilateral (12.9%) and corresponded to obstructive (5 cases) (20,22,45,53,62) and traumatic uropathy (6 cases) (17,23,36,62,70,74). In 3 cases the authors did not specify whether it was unilateral or bilateral (15,58,59). The size of the PE was documented in 73 cases. In 47 cases (64.4%), it occupied over two thirds of the hemithorax, in 9 cases (12.3%) less than a third, and in 17 cases (23.3%) the PE occupied between one and two thirds of the hemithorax. UT was mostly ipsilateral to the obstructed urinary tract, but not always (64,80). Thoracentesis was performed in 75 patients (85.2%). Median time between the cause or origin and the intervention with thoracentesis (25 patients) was 2 days (range: 0–21). The color of the PE was documented in 33 cases (37.5%): it was straw-colored in 24 (72.7%) and hematic in 9 cases (27.3%). PF odor was only mentioned in 8 case reports (9.1%), described as urine-like or ammoniacal in all cases (5,15,58,63,66,68,75,78).
Biochemical characteristics and cellular differentiation of PF were described in only a few cases (Table 3). The question of whether the PE was transudate or exudate was mentioned in 32 reports: 18 were transudate and 14 (43.8%) exudate [3 concordant (59,63,66), 1 protein-discordant (50) and 10 LDH-discordant (15,31,39,57,61,68,72,73,78), according to the classification system of Agrawal et al. (82)]. PF/S creatinine ratio was determined in 48 cases (54.5%) and only one (2%) was <1 (0.95) (63). PF culture was performed in 32 cases and proved positive in 3 (9.4%) (5,15,61). PF cytology was performed in 20 cases and was negative in all.
Full table
UT diagnostic criteria were mentioned in 83 cases (94.3%): PF/S creatinine ratio >1 (47; 56.6%); urinary tract contrast extravasation (10; 12%); computed tomography alterations (7; 8.4%); laparotomy findings (5; 6%); association of PE with obstructive uropathy (5; 6%); demonstration of urine in the pleural cavity (4; 4.8%); clinical outcome (2; 2.4%); ultrasound findings (1), renal radionuclide imaging (1) and administration of indigo carmine (1) (1.2% each).
Treatment of PE
Many different therapeutic measures have been used to treat PE and its symptoms, with widely varying rates of success. Table 4 shows a summary of the most common measures (favorable: total or partial control of PE or its symptoms; unfavorable: no control of PE, recurrence or symptoms). Thoracentesis, either evacuating (3 cases) or repeated (7 cases), did not show favorable results in any case (6,19,23,27,33,38,43,65,73,76). When the only therapeutic measure applied in 5 patients was chest drainage, no improvement was observed (16,25,33,57,67), except in one case (81). Other forms of treatment used anecdotally, such as surgical drainage (10) or pleurodesis (16), were not effective. In three patients, decortication produced favorable results in all (16,25,61).
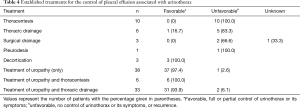
Full table
Better results were obtained when direct therapeutic measures were applied to treat the uropathy, either alone or associated with thoracentesis/thoracic drainage. Of the 38 patients who underwent uropathy treatment alone, only one (2.6%) showed an unfavorable response (48). In 39 patients, thoracentesis (6 cases) or a chest drain (33 patients) was added to uropathy treatment; in the former, the outcome was favorable in all 6 patients and in the latter, only 2 of 33 patients (6%) had unfavorable outcomes (12,61). Treatment of uropathy was varied and included, among others, nephrostomy (19 patients), nephrectomy (17), “double J” catheter (8), lithotripsy (3), urinary catheter (4), ureteroneocystostomy (2), prostatectomy (2), resection of the posterior urethral valve (2), surgical removal of calculus (2) and surgical repair of bladder rupture (2) and ureteral fistula (1). No direct treatment was applied in 4 patients; 2 with renal stone disease resolved spontaneously (28,39) and the other 2 died (38,48). Finally, the treatment applied in 10 patients was not documented (2,8,10,15,45,52,59,61,63,78).
Discussion
Publications on UT involve isolated case reports (between 1 and 4 cases), so key issues such as clinical course, characteristics of PE or the most effective treatments are not well known. These questions were addressed using a systematic review of the literature relating to this disease since a recent previous revision does not include the characteristics of PE or its treatment (79).
UT is a rare form of PE which occurs by the accumulation of urine in the pleural space, as a result of a trauma or blockage of the urinary tract. The mechanism of urine transit has been much debated. One theory is that it ascends directly through anatomical defects of the diaphragm, but it seems more likely that the collection of urine migrates into the pleural space through diaphragmatic lymphatics due to increased retroperitoneal or intraperitoneal pressure caused by urinoma (21). In cases of traumatic origin, the disruption of urinary excretion pathways was associated with unilateral PE. In the absence of trauma, unilateral ureteral or kidney obstruction does not produce UT if the contralateral kidney’s function is preserved. Only obstruction of both ureters, the urethra, or the bladder, can divert the urine, causing ascites and subsequent UT. In patients with renal stones, if the obstruction is not bilateral, the most likely cause of UT is considered to be acute traumatic injury that occurs at the time.
In most cases, the diagnosis is based on demonstrating PE associated with obstructive or traumatic uropathy which resolves after treatment of the obstruction. It is not uncommon for the diagnosis of UT to be established without determining biochemical parameters such as PF/S creatinine ratio, pH or glucose levels. UT is a reversible disease when treatment is directed at correcting its primary cause, so early diagnosis and etiology is especially important.
The disease can occur at any age; the typical patient is male (61.4%; ratio 1.6/1), with dyspnea (92.8%), chest pain (76.9%), abdominal pain (91.4%) and reduced diuresis (87%). UT is usually of traumatic origin (76%), with unilateral PE (87%), and size greater than two thirds of the hemithorax (64.4%). Although respiratory symptoms are classically said to be absent or of minor intensity (3), 92.8% of patients (52/56) had dyspnea; this is consistent with the finding that 64.4% of patients (47/73) presented PE occupying over two thirds of the corresponding hemithorax.
It is widely accepted that the PF in UT has the color and smell of urine, but these characteristics have not often been documented (37.5% and 9.1%, respectively). Regarding the color, 27.3% had PF indicating the presence of blood in the urinary tract. Perhaps the most controversial aspect in the literature is whether the UT is transudate or exudate, according to Light’s criteria (83). Classically it is said to be transudate, but in this review PE was exudate in 14/32 cases (43.8%), LDH-discordant in 10/14 cases (71.4%) and showed high LDH in 13/14 cases (92.9%). One explanation could be that urinary LDH is a nonspecific marker of cellular disruption anywhere along the genitourinary tract in otherwise healthy blunt trauma patients (84). In this regard, of the 12 cases with concordant exudate or LDH-discordant exudate of a known cause, 11 (84.6%) were of traumatic origin. The presence of a concordant exudate does not rule out UT (59,63,66). Hematuria urine can do that the UT is hematic and have high levels of protein due to the passage of plasma to the PF. However, only one of these patients showed this characteristic (59). A PF/S creatinine ratio >1 has been considered the biochemical criterion for the diagnosis of UT. It is a highly sensitive parameter (97.9%) but is not specific to UT. In three series of patients with PE (excluding UT), between 12 and 39.6% of cases had a PF/S creatinine ratio >1 (39,85,86). The pH in UT is usually acidic (60% had pH ≤7.30) which is explained by the presence of clearly acidotic urine. However, in 24% (6/25) of the cases reviewed, pH level was ≥7.50 (21,48,56,66,78). It has been speculated that urinoma with hematuric urine, in addition to raising PF protein levels, could have the same effect on the pH (50), but in this review none of the 6 cases with pH ≥7.50 had hematic PF. In 21.4% of patients (6/28), PF glucose values did not exceed 60 mg/dL (15,39,61,68,70,71), possibly due to the low level of glucose in the urine. Despite the information provided by these parameters, their determination is not very common (PF/S creatinine ratio, 54.5%; PF pH, 29.5%; PF glucose, 31.8%) (Table 3). PF usually showed few nucleated cells [only 5 cases had more than 2,000 cells/mm3 (29,47,61,68,70)] and was either lymphocyte-predominant (>50%, 4/9, 44.4%) (27,30,59,65) or polymorphonuclear (5/13; 38.5%) (21,39,47,61,70). In 3 patients, PF culture was positive: two presented Proteus (5,15) while the microorganism was not mentioned in the third, but the treatment was based on PF culture findings (61). This infection undoubtedly explains the number of PF nucleated cells in this case (47,500/mm3). The criteria used to diagnose UT in these patients were intravenous contrast study findings (5) and a PF/S creatinine ratio >1 (15,61).
The management of UT is not well defined to date. The results of this systematic review suggest that it should be based on treatment of the underlying uropathy, either alone or associated with thoracentesis/thoracic drainage. In the 77 patients who received one of these forms of treatment, 74 (96.1%) had a favorable outcome. By contrast, thoracentesis and chest drainage, without uropathy treatment, did not result in a favorable outcome in any of the 16 patients who only received these measures, except in one case (81). Decortication was used in 3 patients and the outcome was favorable in all (16,25,61). However, this approach was adopted mainly for the complications arising from the PE rather than as treatment for the UT itself. Uropathy treatment varies according to the root cause of the UT, and over 20 different measures have been described, ranging from simple urinary catheter (3 patients) to nephrectomy (17) through nephrostomy (19), lithotripsy (3), “double J” catheter (8) or corresponding surgical repair. Favorable outcomes in UT patients have also been described in cases without uropathy treatment after spontaneous resolution of renal stone obstruction (28,39).
Two patients with UT died: in the first it was decided not to perform any invasive measure since the patient had metastatic bladder cancer and the possibility of surviving surgery was limited (38), while the second had declining renal function and other causes (48).
Our review has certain limitations. The most important was the reliance on descriptions of case reports, instead of case series or comparative trials. Therefore, the evaluation of the quality of the reported literature could limit internal validity, generalizability, and accuracy. In addition, some articles highlight the clinical characteristics of the patients, while others stress diagnostic and therapeutic aspects. Due to the heterogeneity of the reported information, it is not possible to provide the details required, making it difficult to correctly classify some effusions or evaluate the response to a particular treatment. As in all rare disease, the publication bias would be another limitation to consider since the successfully treated cases or atypical cases are more likely to get published.
In summary, despite carrying out a systematic review, the available data are too few to draw firm conclusions. However, it seems that UT may appear at any age, is slightly more common in men, and its origin is usually traumatic. PE is generally unilateral and occupies over two thirds of the hemithorax. PF may be straw-colored or hematic and does not have a specific pattern or cellularity predominance. The PF/S creatinine ratio is almost always >1. Finally, our results indicate that the management of UT should include direct treatment of the underlying uropathy, with or without PE evacuation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- France NE, Back EH. Neonatal ascites associated with urethral obstruction. Arch Dis Child 1954;29:565-8. [Crossref] [PubMed]
- Corriere JN, Miller WT, Murphy JJ. Hydronephrosis as a cause of pleural effusion. Radiology 1968;90:79-84. [Crossref] [PubMed]
- Garcia-Pachon E, Romero S. Urinothorax: a new approach. Curr Opin Pulm Med 2006;12:259-63. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. [Crossref] [PubMed]
- Hume HA, Stevens LW, Erb WH. Urothorax. An unusual complication of multiple traumatic injuries. N Engl J Med 1962;267:289-91. [Crossref] [PubMed]
- Friedland GW, Axman MM, Love T. Neonatal "urinothorax" associated with posterior urethral valves. Br J Radiol 1971;44:471-4. [Crossref] [PubMed]
- Barek LB, Cigtay OS. Urinothorax--an unusual pleural effusion. Br J Radiol 1975;48:685-6. [Crossref] [PubMed]
- Laforet EG, Kornitzer GD. Nephrogenic pleural effusion. J Urol 1977;117:118-9. [PubMed]
- Lahiry SK, Alkhafaji AH, Brown AL. Urinothorax following blunt trauma to the kidney. J Trauma 1978;18:608-10. [Crossref] [PubMed]
- Frantz P, Riquet M, Richard R, et al. Urothorax. J Urol Nephrol (Paris) 1978;84:807-13. [PubMed]
- Belis JA, Milam DF. Pleural effusion due to ureteral obstruction. Urology 1979;14:27-9. [Crossref] [PubMed]
- Baron RL, Stark DD, McClennan BL, et al. Intrathoracic extension of retroperitoneal urine collections. AJR Am J Roentgenol 1981;137:37-41. [Crossref] [PubMed]
- Leung FW, Williams AJ, Oill PA. Pleural effusion associated with urinary tract obstruction: Support for a hypothesis. Thorax 1981;36:632-33. [Crossref] [PubMed]
- Redman JF, Arnold WC, Smith PL, et al. Hypertension and urino-thorax following an attempted percutaneous nephrostomy. J Urol 1982;128:1307-8. [PubMed]
- Stark DD, Shanes JG, Baron RL, et al. Biochemical features of urinothorax. Arch Intern Med 1982;142:1509-11. [Crossref] [PubMed]
- Teyssier G, Chavrier Y, Allard D, et al. Urothorax caused by traumatic ruptura of the subpyelic ureter. Apropos of a case in a 5-year-old. Pediatrie 1983;38:37-41. [PubMed]
- Leroy G, Dupuis F, Guy JP, et al. Urothorax following total cystectomy. Cah Anesthesiol 1984;32:235. [PubMed]
- Carcillo J Jr, Salcedo JR. Urinothorax as a manifestation of nondilated obstructive uropathy following renal transplantation. Am J Kidney Dis 1985;5:211-3. [Crossref] [PubMed]
- Nusser RA, Culhane RH. Recurrent transudative effusion with an abdominal mass. Urinothorax. Chest 1986;90:263-4. [Crossref] [PubMed]
- Ralston MD, Wilkinson RH Jr. Bilateral urinothorax identified by technetium-99m DPTA renal imaging. J Nucl Med 1986;27:56-9. [PubMed]
- Salcedo JR. Urinothorax: report of 4 cases and review of the literature. J Urol 1986;135:805-8. [PubMed]
- Weiss Z, Shalev E, Zuckerman H, et al. Obstructive renal failure and pleural effusion caused by the gravid uterus. Acta Obstet Gynecol Scand 1986;65:187-9. [Crossref] [PubMed]
- Miller KS, Wooten S, Sahn SA. Urinothorax: a cause of low pH transudative pleural effusions. Am J Med 1988;85:448-9. [Crossref] [PubMed]
- O'Donnell A, Schoenberger C, Weiner J, et al. Pulmonary complications of percutaneous nephrostomy and kidney stone extraction. South Med J 1988;81:1002-5. [Crossref] [PubMed]
- Capellier G, Gaussorgues P, Boyer F, et al. Diagnosis of post-traumatic pleural effusion. Ann Fr Anesth Reanim 1989;8:131-2. [Crossref] [PubMed]
- Lee SD. Pleural effusion and hydronephrosis in a newborn. J Am Board Fam Pract 1989;2:55-7. [PubMed]
- Javaloyas M, Picado MJ, Nonell F, et al. Massive pleural effusion secondary to hydronephrosis. Rev Clin Esp 1989;185:19-20. [PubMed]
- Fokaefs E, Melekos MD. Pleural effusion associated with urinary extravasation due to renal colic. Br J Urol 1991;68:435. [Crossref] [PubMed]
- Gandía-Martínez F, Díez-Gutierrez F, Tamayo-Lomas L, et al. Insuficiencia respiratoria secundaria a neumotórax. Med Intensiva 1994;18:28-30.
- Geraldía Lama M, León-Jiménez A, Soler-Regal C, et al. Urinothorax: an infrequent cause of pleural effusion. Med Clin (Barc) 1994;103:439. [PubMed]
- Chanatry BJ, Gettinger A. Progressive respiratory insufficiency after cesarean section. Crit Care Med 1995;23:204-7. [Crossref] [PubMed]
- Kees-Folts D, Cole BR. Ureteral urine leak presenting as a pleural effusion in renal transplant recipient. Pediatr Nephrol 1998;12:666-7. [Crossref] [PubMed]
- Hase T, Dodama M, Domau S, et al. A case of urothorax that manifested as post-traumatic pleural effusion after a motorcycle crash. J Trauma 1999;46:967-9. [Crossref] [PubMed]
- Kamble RT, Bhat SP, Joshi JM. Urinothorax: a case report. Indian J Chest Dis Allied Sci 2000;42:189-90. [PubMed]
- Hendriks J, Michielsen D, Van Schil P, et al. Urinothorax: a rare pleural effusion. Acta Chir Belg 2002;102:274-5. [Crossref] [PubMed]
- Oğuzülgen IK, Oguzülgen AI, Sinik Z, et al. An unusual cause of urinothorax. Respiration 2002;69:273-4. [Crossref] [PubMed]
- Parvathy U, Saldanha R, Balakrishnan KR. Blunt abdominal trauma resulting in urinothorax from a missed uretero-pelvic junction avulsion: case report. J Trauma 2003;54:187-9. [Crossref] [PubMed]
- Ray K, Rattan S, Yohannes T. Urinothorax: unexpected cause of a pleural effusion. Mayo Clin Proc 2003;78:1433-4. [Crossref] [PubMed]
- Garcia-Pachon E, Padilla-Navas I. Urinothorax: case report and review of the literature with emphasis on biochemical diagnosis. Respiration 2004;71:533-6. [Crossref] [PubMed]
- Beigelman A, Marks KA, Landau D. Congenital isolated pleural effusion associated with obstructive uropathy. Isr Med Assoc J 2005;7:271-2. [PubMed]
- Lee CC, Fang CC, Chou HC, et al. Urinothorax associated with VURD syndrome. Pediatr Nephrol 2005;20:543-6. [Crossref] [PubMed]
- Buyukcelik M, Satar N, Celik U, et al. An unusual cause of pleural effusion, urinothorax in a child with urinary stone disease. Pediatr Nephrol 2005;20:1487-9. [Crossref] [PubMed]
- Shleyfer E, Nevzorov R, Jotkowitz AB, et al. Urinothorax: An unexpected cause of pleural effusion. Eur J Intern Med 2006;17:300-2. [Crossref] [PubMed]
- Tortora A, Casciani E, Kharrub Z, et al. Urinothorax: an unexpected cause of severe dyspnea. Emerg Radiol 2006;12:189-91. [Crossref] [PubMed]
- Karkoulias K, Sampsonas F, Kaparianos A, et al. Urinothorax: an unexpected cause of pleural effusion in a patient with non-Hodgkin lymphoma. Eur Rev Med Pharmacol Sci 2007;11:373-4. [PubMed]
- Patel NLS, Allen SA. Acute hypoxemic respiratory failure as a manifestation of urinothorax. J Respir Dis 2007;28:156-61.
- Bhattacharya A, Venkataramarao SH, Kumar S, et al. Urinothorax demonstrated on 99mTc ethylene dicysteine renal scintigraphy. Nephrol Dial Transplant 2007;22:1782-3. [Crossref] [PubMed]
- Deel S, Robinette E Jr. Urinothorax: a rapidly accumulating transudative pleural effusion in a 64-year-old man. South Med J 2007;100:519-21. [Crossref] [PubMed]
- Handa A, Agarwal R, Aggarwal AN. Urinothorax: an unusual cause of pleural effusion. Singapore Med J 2007;48:e289-92. [PubMed]
- Sancho Calvache M, Pomares-Amigó X. Urinothorax: always a transdative pleural effusion? Arch Bronconeumol 2008;44:286. [Crossref] [PubMed]
- Izzo L, Caputo M, de Toma G, et al. Urinoma and urinothorax. Am Surg 2008;74:62-63. [PubMed]
- Agranovich S, Cherniavsky E, Tiktinsky E, et al. Unilateral urinothorax due to nephropleural fistula detected on Tc-99m diethylenetriamine pentaacetic acid renal scintigraphy. Clin Nucl Med 2008;33:889-91. [Crossref] [PubMed]
- Muzhrachi A, Prasad KV. Bilateral urinothorax following spontanious extravasation from the kidney-speculation of an anatomical pathway for the transport of extravasated urine to the pleural cavities: A case report and review of the literature. Q Med J 2008;17:71-4.
- Ziyade S, Ugurlucan M, Soysal O. Urinothorax: urine discharge from thorax. Ann Thorac Surg 2008;85:2141. [Crossref] [PubMed]
- Jelic S, Sampogna RV. Detection of unrecognized urinothorax with renal scintigraphy. Kidney Int 2009;76:353. [Crossref] [PubMed]
- Amro O, Webb-Smith F, Sunderji S. Urinothorax: a rare complication of total abdominal hysterectomy. Obstet Gynecol 2009;114:482-4. [Crossref] [PubMed]
- Wei B, Takayama H, Bacchetta MD. Urinothorax: An uncommon cause of pleural effusion. Respir Med CME 2009;2:179-80. [Crossref]
- Commandeur D, Danguy des Deserts M, Giacardi C, et al. Diagnostic fortuit d'urothorax | Annales Francaises d'Anesthesie et de Reanimation 2010;29:312-3. [Accidental urothorax diagnosis]. [Crossref] [PubMed]
- Mora RB, Silvente CM, Nieto JM, et al. Urinothorax: presentation of a new case as pleural exudate. South Med J 2010;103:931-3. [Crossref] [PubMed]
- Gouli JC, Merrot T, Chaumoitre K, et al. Urinothorax: rare complication of neonatal sectioned posterior urethral valve. Prog Urol 2011;21:146-50. [Crossref] [PubMed]
- Brown B, Trotter C, Cox P, et al. Urinothorax: a rare cause of pleural effusion. W V Med J 2011;107:16-7. [PubMed]
- Laskaridis L, Kampantais S, Toutziaris C, et al. Urinothorax-an underdiagnosed cause of acute dyspnea: report of a bilateral and of an ipsilateral urinothorax case. Case Rep Emerg Med 2012;2012:395653. [Crossref] [PubMed]
- Antoon JW, Knudson-Johnsos M, Kiernan MP. An unusual case of pediatric shortness of breath-answers. Pediatr Nephrol 2012;27:923-5. [Crossref] [PubMed]
- Dimitriadis G, Tahmatzopoulos A, Kampantais S, et al. Unilateral urinothorax can occur contralateral to the affected kidney. Scand J Urol 2013;47:242-3. [Crossref] [PubMed]
- Ameer KA, Thomas R, Sureshkumar VK, et al. An unusual complication of a common gynaecological procedure. J Assoc Physicians India 2013;61:490-2. [PubMed]
- Ferreira PG, Furriel F, Ferreira AJ. Urinothorax as an unusual type of pleural effusion - clinical report and review. Rev Port Pneumol 2013;19:80-3. [Crossref] [PubMed]
- Batura D, Haylock-Vize P, Naji Y, et al. Management of iatrogenic urinothorax following ultrasound guided percutaneous nephrostomy. J Radiol Case Rep 2014;8:34-40. [Crossref] [PubMed]
- Chandra A, Pathak A, Kapur A, et al. Urinothorax: A rare cause of severe respiratory distress. Indian J Crit Care Med 2014;18:320-2. [Crossref] [PubMed]
- Nilsen-Nunn A, Beckley I, Wah T, et al. An unusual presentation of a reno-pleural fistula. J Clin Urol 2014;7:66-8. [Crossref]
- Gupta R, Singh P. Urinothorax - A rare cause of pleural effusion. JK Sci 2014;16:86-8.
- Kumar S, Lata S, Patidar Y. Pleuropericardial effusion: A diagnostic conundrum. Thorax 2014;69:884-5. [Crossref] [PubMed]
- Abdel-Rahman AM. Urinothorax: a rare finding after urinary intervention. Clin Respir J 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Tal Y, Weinberg I, Ben-Yehuda A, et al. Unilateral Obstructive Urinothorax Secondary to Colorectal Carcinoma. Isr Med Assoc J 2015;17:321-2. [PubMed]
- Gandhi RK, Dhandapani BS, Barvadheesh RC. Combination injuries of diaphragm and urinary bladder resulting urinothorax. J Minim Access Surg 2015;11:149-50. [Crossref] [PubMed]
- Ranjan V, Agrawal S, Chipde SS, et al. Urinothorax: A path, less travelled: Case report and review of literature. J Nat Sci Biol Med 2015;6:213-6. [Crossref] [PubMed]
- Rakotoarivelo HN, Rondeau-Lutz M, Groza M, et al. Urinothorax, an unusual cause of pleural effusion. Rev Pneumol Clin 2015;71:372-4. [Crossref] [PubMed]
- Garcia-Simon R, Hergueta-Herrera J, Cañizares-Oliver S, et al. Urinothorax: An unusual complication of an oncologic gynecological surgery. Taiwan J Obstet Gynecol 2015;54:336-8. [Crossref] [PubMed]
- Kalchiem-Dekel O, Davidesko S, Maimon N. Flashcard: A 57-year-old woman with pleural effusion following percutaneous nephrolithotripsy. Eur J Intern Med 2015;26:70-1. [Crossref] [PubMed]
- Casallas A, Castañeda-Cardona C, Roselli D. Urinothorax: case report and systematic review of the literature. Urol Ann 2016;8:91-4. [Crossref] [PubMed]
- Chan DM, Cheung VY. Urinothorax as an early sign of urinary tract injury following total laparoscopic hysterectomy. Int J Gynaecol Obstet 2016;134:102-3. [Crossref] [PubMed]
- Puthenveedu DK, Manickam N, Subramanian AR, et al. Urinothorax: a rare postoperative complication of adrenalectomy. J Clin Diagn Res 2016;10:OD11-2. [PubMed]
- Agrawal V, Doelken P, Sahn SA. Pleural fluid analysis in chylous pleural effusion. Chest 2008;133:1436-41. [Crossref] [PubMed]
- Light RW. Clinical practice. Pleural effusion. N Engl J Med 2002;346:1971-7. [Crossref] [PubMed]
- Henneman PL, Bar’Or D, Marx JA. Urinary lactic dehydrogenase as a marker of renal injury in blunt trauma patients with hematuria. Ann Emerg Med 1988;17:797-800. [Crossref] [PubMed]
- Tudik I, Varmusova E, Kavkova D. Does elevated creatinine pleural fluid/serum ratio really mean urinothorax? Eur Respir J 2004;24:248s.
- Gutierrez Rubio A, Martin Serrano C, Martinez Saez S, et al. Does pleural fluid to serum ratio of creatinine higher than 1 always mean urinothorax? Arch Bronconeumol 2005;41:149.