A meta-analysis of video-assisted thoracoscopic decortication versus open thoracotomy decortication for patients with empyema
Introduction
Thoracic pleural empyema is a collection of pus within a naturally existing thoracic cavity. It is one of the common complications of pneumonia before antibiotic prevailing. It is mainly occurred after the spread of pulmonary infection, penetrating thoracic trauma, thoracic foreign body and postoperative pleural infection (1). Three stages in the pathophysiologic process: stage 1 (exudative) when there is an increase in pleural effusion; stage 2 (fibrinopurulent) which is pleural fluid loculation and fibrinous septa formation; stage 3 (organizational) which includes scar adhesion, thoracic space constriction and inability of lung expansion (2). The symptoms of different stages are various. In the early stage, patients mostly may have fever, chest pain and cough. However, in the final stage, the shortness of breath will be the dominant symptom. Although less empyema cases occurred recently due to the antibiotic utility, it is still associated with great morbidity and mortality (3).
Surgical treatments including chest tube drainage, thoracocentesis and decortications are considerably important for the empyema patients. For the early stage (stage 1) empyema, thoracocentesis and chest tube drainage were suitable choices. But for patients who were stage 2 or 3 and had troubles in breathing because of the lung expansion constriction, decortication is necessary (4). Referring to decortications, Chambers and colleagues published a systematic review in 2010 (5). 14 papers were selected to answer the question whether video-assisted thoracoscopic decortication (VATD) might be superior to open thoracotomy decortication (OTD) for management primary empyema. Chambers’ paper was a qualitative systematic review. The conclude that VATD has superior outcomes for the treatment of persistent pleural collections. Even so, there is still no consensus on whether to choose VATD or OTD. Base on the above review, we make a quantitative systematic review to prove the conclude.
The outcomes of these surgical approaches are various. Open thoracic decortication has been considered to be most favored approach with shorter operative duration, better vision and lung re-expansion in last few decades. However, video-assisted thoracoscopic decortication, a minimally invasive approach, is praised for its less damage and sooner recovery (6-8). To address the difficulty of the surgical approaches selection, the current study analyzes the operative and long-term outcomes of VATD and OTD.
Methods
Search strategy
The electronic search was performed using PubMed, Medline, Cochrane Central Register of Controlled Trial, Cochrane Database of Systematic Reviews, ACP Journal Club and Database of Abstracts of Reviews of Effects from the dates of inception to February 2017. In order to maximize the sensitivity, we combined the words “empyema” with “decortication” or “debridement” and “thoracoscop” or “VATS” and “open” or “thoracotomy” as Mesh terms or in all fields. All the articles were systematically filtered using inclusion and exclusion criteria.
Inclusion and exclusion criteria
The eligible studies for the meta-analysis should investigate patients with empyema or pleural infection and undergone VATD or OTD. Those studies which had chest tube drainage besides VATD and OTD were also included, but only the data of VATD and OTD were extracted. All publications were limited in human species and in English language. Case reports, expert opinions, abstracts, conference presentations, guidelines and reviews were excluded in case of publication bias and data duplication. Those publications with no primary outcomes, no decortication and the studies included less than 20 patients in both treatment groups were also excluded. When encountered duplicated data, only the most novel and complete reports were included for data extraction and assessment.
Data extraction
All the data were extracted from articles, tables, figures and supplement of the publications by two inspectors respectively and independently. Discrepancies between two reviewers were resolved by discussion and consensus with the senior investigator. The extracted data included publication characteristics, sample size, gender, empyema stage, operative duration, postoperative hospital stay, chest tube duration, prolonged air leak, morbidity, relapse and perioperative mortality.
Statistical analysis
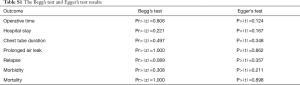
The meta-analysis was performed to compare the VATD and OTD by combining the reported operative duration, postoperative hospital stay and chest tube duration in “Mean ± SD” form. In terms of prolonged air leak, morbidity, relapse and perioperative mortality, risk ratio (RR) was used as a summary statistic. χ2 tests were conducted to assess the heterogeneity between the studies, while I2 (inconsistency index) was used to estimate the variation across the studies (9,10). The I2 was calculated with the formula: in which the Q stood for a heterogeneity statistic and df was defined as the degree of freedom. The heterogeneity was defined as low (25–49%), moderate (50–74%), high (>75%). Random-effect analysis model was used to calculate the mean difference, and RR. If the heterogeneity was severe, a sensitive test or a subgroup analysis would be performed. Z-test was performed to calculate the p value, which was two-sided and defined as statistically different when P<0.05. The statistical analysis was conducted via Review Manager (RevMan) [Computer program]. Version 5.2, 2014. The publication bias was analyzed via Stata 12. It would be considered as insignificant when the p>0.05 both in egger’s and begg’s test (Table S1).
Full table
Results
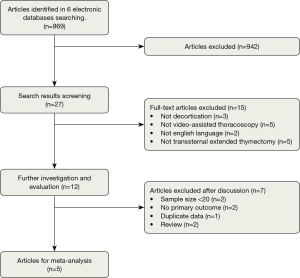
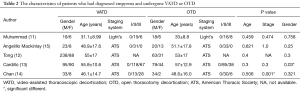
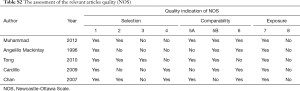
A total of 969 articles were identified in 6 electronic database and other additional sources. After filtered by the exclusion criteria, 27 articles were selected for a further investigation and intensive evaluation. After applied the inclusion criteria, 12 article candidates were selected for group discussion. After the discussion, a final consensus was reached that 5 articles were chosen for extraction and assessment (11-15). There was no any manual search additional relevant article (Figure 1). All of the relevant articles were observational studies (Table 1). As a result, the Newcastle-Ottawa Scale (16) was used to assess the quality of relevant studies including their selection of cases, comparability of populations and exposure. The characteristics of studies were shown (Tables 1,2) and each assessment of study quality by Newcastle-Ottawa Scale were also presented (Table S2).

Full table
Full table
Full table
All the continuous data of clinical characteristics was demonstrated in “Mean ± SD”. The raw data of one article (15) reported in “Medium and interquartile range” was converted into “Mean ± SD” (17). One article (12) only reported the mean and p value of the clinical outcome. As a result, the standard deviation was calculated by the p value. Some clinical outcomes were demonstrated in proportion which were also converted in to dichotomous data.
The analysis of operative outcomes
In these studies, 918 patients who were diagnosed as pleural empyema by thoracic CT scan or thoracocentesis and had undergone decortication surgeries, including 608 patients in VATD groups and 310 patients in OTD groups. The characteristics of patients which had been demonstrated in Table 2. In Tong’s paper (12), there was no information about the Stage. So the patients might cover all stages. The follow-up duration was at least 3–4 weeks. The prolonged air leak was one of the most common complications of decortication which was existing more than 7 days after thoracic surgeries and significantly related to the chest tube duration. The morbidity was defined as the complications within 30 days after surgeries. The morbidities which were related to empyema, postoperative pneumonia or sepsis were taken into account. The relapse was considered when no empyema residual was identified after surgical approaches and re-discovered later. Giuseppe’s study was failed to report chest tube duration. As a result, only four studies were analyzed in chest tube duration outcome.
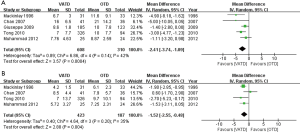
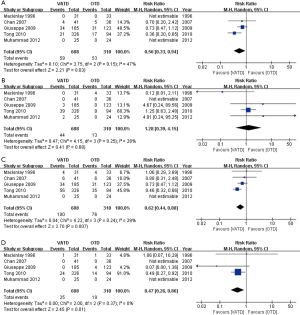
According to the data, both in VATD and OTD groups, male patients accounted for a larger proportion of all patients. But in Giuseppe’s study (13), the gender constitution in two arms was significantly different. While, there were more stage 3 patients in the VATD group in Chan’s study (14) which was inconsistent with others. The postoperative hospital stay [mean difference −2.41; 95% confidence interval (CI), −3.74 to −1.09; P=0.0004], prolonged air leak (9.7% vs. 17.1%; RR 0.56; 95% CI, 0.33 to 0.94; P=0.03), chest tube duration (mean difference −1.52; 95% CI, −2.55 to −0.48; P=0.004), morbidity (16.4% vs. 24.5%; RR 0.62; 95% CI, 0.44 to 0.88; P=0.007) and mortality (4.1% vs. 6.2%; RR 0.47; 95% CI, 0.26 to 0.86; P=0.01) of VATD were statistically less than the OTD. In terms of relapse rate, there was no statistical significance between two surgical approaches (7.2% vs. 4.2%; RR 1.28; 95% CI, 0.39 to 4.15; P=0.68) (Figures 2,3). The operative time (mean difference −36.89; 95% CI, −60.96 to −12.82; P=0.003) of VATD was also less than OTD, but the heterogeneity of it was high. Thus, the subgroup analysis was conducted. However, the heterogeneity of others was not statistically significant with P>0.05.
Discussion
Due to the visceral and parietal pleural adhesion, the expansion of lung and the respiration movement decreased significantly. The empyema patients in stage 2 and stage 3 are mainly suffering from the shortness of breath. As a result, decortication is a suitable and effective approach for them, but the damage is severe at the same time. With the minimally invasive thoracic surgery development, VATD has been introduced to the empyema surgical treatment. Nevertheless, the effectiveness of VATD is still unclear (18,19). The present meta-analysis intends to compare VATD and OTD in different clinical outcomes and provides evidences for surgical approach selection.
The meta-analysis demonstrated that VATD had shorter operative time than OTD patients in two subgroups. Theoretically, shorter operative time may lead to less operative complication and shorter hospital stay. It is consistent with the results that in the aspects of postoperative hospital stay and morbidity, VATD performed better than OTD. However, in the high-quality data and low-quality data subgroups, the mean differences are −56.93 and −9.63, respectively (13,15). The reason that accounts for this big gap is the unsymmetrical data collection. In Giuseppe’s study (13), the OTD patients were treated from January 1996 to October 2001; the VATD patients underwent the operations from September 2000 to December 2006. While in Mackinlay’s report (15), OTD was performed during 1985 to 1991 and VATD was in 1992 to 1994 period. In other studies, both surgical approaches were performed symmetrically without any time gap. According to the candidate studies, the OTD data was recorded earlier than the VATD data. It means the surgeons of these two institutes may not be familiar with the VATD techniques. They may spend more time in performing VATD than their counterparts. Moreover, the unsymmetrical data collection may bring huge bias to the outcomes.
The prolonged air leak, which is defined as air leakage lasting more than 7 days after surgery, is the most common complication of decortication. Due to the chronic infection and fibrinopurulent pleurisy, the adhesion of visceral and parietal pleura is very solid. The priority of decortications is to separate the adhesion and release the lung. It may lead to visceral pleura damage inevitably. In both surgical approaches, chest tubes will be inserted after the operations which are used for air and residual fluid drainage (20,21). The longer chest tube duration may attribute to the longer air leakage. The duration of prolonged air leak and chest tube in VATD group is longer than the OTD group. It suggests that VATD may have less damage than OTD when separating the adhesion between visceral and parietal pleura.
Referring to morbidity and mortality, based on the current study, VATD group apparently outweighed OTD group with less morbidity or mortality. It possibly benefits from the minimally invasive approach. Besides, sepsis is the main cause of postoperative mortality. These results are consistent with other studies which have not been included (22,23). Unfortunately, the candidate articles provided no detail about other complications and causes of death.
According to the relapse rate, there was no statistically significant difference between two groups. Some people claimed that the VATD might not be as good as OTD in terms of effect. Their reasons were that the vision of VATD was narrow, thus there might be residual which had been overlooked. Based on the result, we found no difference. However, there were 53 VATD cases converted to OTD intra-operatively (Table 3). The average conversion rate in the present study was 8.7% ranging from 0% to 11.3%. Although the conversion rate was relatively low, it demonstrated that OTD had advantages that VATD lacked (24). If the intercostal spaces are often too narrow, ultrasonography demonstrates an encased lung or the lung fails to expand during VATD, the patient should undergo decortication by full thoracotomy. Surgeons’ learning from case to case and gained technical expertise, conversion rate declined significantly especially stage 3 cases. The present study demonstrates a lower rate of conversion to open thoracotomy as compared to previous studies, which ranged from 28% to 59% (15,25-29). Some studies claimed delayed referral and gram-negative bacteria increase the conversion thoracotomy rate (22,23). Later disease stage would intent to be treated by open surgery. Although some cases were decided to choose VATD, they might be upgraded after thoracic cavity inspection and converted to open surgery. Therefore, some conversions were not inevitable. However, no specific data of the conversion reasons was provided in the studies.

Full table
Besides, numbers of limitations have to be admitted in the current study. Firstly, some outcomes were reported in various forms in the candidate articles. In order to evaluate, the forms have to be unified. For instance, Tong et.al reported operative time in “medium and interquartile range”, which might generate inaccuracies after conversion. Secondly, although the subgroup analysis has been performed, the overall and subgroup difference heterogeneity of operative time outcome is severe. Thirdly, all of the candidates are retrospective observational studies. After applying the Newcastle-Ottawa Scale, two of them had less than 5 stars which had been defined as low-quality studies. The reliability of meta-analysis might be effected by the cases bias due to the unsymmetrical data collection. The result would be more reliable when high-quality studies or multi-center randomized control trials were included. Fourth, the imbalance in patient characteristics between arms cannot be adjusted for due to the lack of individual patient data. The conclusion of the analysis, therefore, suffers from an imbalance between comparator arms which may not have been observed. Finally, none of those conversion cases had been described or demonstrated in detail in the relevant studies. Otherwise, more specific analysis could have been done.
In conclusion, it can be seen from the current meta-analysis that VATD is superior to OTD in the aspects of operative time, hospital stay, prolonged air leak, chest tube duration, morbidity and mortality. Meanwhile, there is no advantage in the relapse rate. In some particular circumstances, VATD may have to convert to OTD. As our opinion, experience, and learning, conversion to an open surgery procedure should not be considered as a failure of thoracoscopy, but rather an exercise of mature surgical judgment. Moreover, limitations have to be admitted in this study. A new meta-analysis will be performed, if there are more well-designed and convincing studies.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Moore KL, Dalley AF. Clinically oriented anatomy: instructor's resource DVD-ROM. Hagerstown, Maryland: Lippincott Williams & Wilkins. 2006.
- Watkins E Jr, Fielder CR. Management of nontuberculous empyema. Surg Clin North Am 1961;41:681-93. [Crossref] [PubMed]
- Hamm H, Light RW. Parapneumonic effusion and empyema. Eur Respir J 1997;10:1150-6. [Crossref] [PubMed]
- Renner H, Gabor S, Pinter H, et al. Is aggressive surgery in pleural empyema justified? Eur J Cardiothorac Surg 1998;14:117-22. [Crossref] [PubMed]
- Chambers A, Routledge T, Dunning J, et al. Is video-assisted thoracoscopic surgical decortication superior to open surgery in the management of adults with primary empyema? Interact Cardiovasc Thorac Surg 2010;11:171-7. [Crossref] [PubMed]
- Cheng YJ, Wu HH, Chou SH, et al. Video-assisted thoracoscopic surgery in the treatment of chronic empyema thoracis. Surg Today 2002;32:19-25. [Crossref] [PubMed]
- Hope WW, Bolton WD, Stephenson JE. The utility and timing of surgical intervention for parapneumonic empyema in the era of video-assisted thoracoscopy. Am Surg 2005;71:512-4. [PubMed]
- Luh SP, Hsu GJ, Cheng-Ren C. Complicated parapneumonic effusion and empyema: pleural decortication and video-assisted thoracic surgery. Curr Infect Dis Rep 2008;10:236-40. [Crossref] [PubMed]
- Higgins J, Thompson S, Deeks J, et al. Statistical heterogeneity in systematic reviews of clinical trials: a critical appraisal of guidelines and practice. J Health Serv Res Policy 2002;7:51-61. [Crossref] [PubMed]
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539-58. [Crossref] [PubMed]
- Muhammad MI. Management of complicated parapneumonic effusion and empyema using different treatment modalities. Asian Cardiovasc Thorac Ann 2012;20:177-81. [Crossref] [PubMed]
- Tong BC, Hanna J, Toloza EM, et al. Outcomes of video-assisted thoracoscopic decortication. Ann Thorac Surg 2010;89:220-5. [Crossref] [PubMed]
- Cardillo G, Carleo F, Carbone L, et al. Chronic postpneumonic pleural empyema: comparative merits of thoracoscopic versus open decortication. Eur J Cardiothorac Surg 2009;36:914-8. [Crossref] [PubMed]
- Chan DT, Sihoe AD, Chan S, et al. Surgical treatment for empyema thoracis: is video-assisted thoracic surgery "better" than thoracotomy? Ann Thorac Surg 2007;84:225-31. [Crossref] [PubMed]
- Angelillo Mackinlay TA, Lyons GA, Chimondeguy DJ, et al. VATS debridement versus thoracotomy in the treatment of loculated postpneumonia empyema. Ann Thorac Surg 1996;61:1626-30. [Crossref] [PubMed]
- Wells GA, Shea BJ, O'Connell D, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analysis. Appl Eng Agric 2000;18:727-34.
- Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 2005;5:13. [Crossref] [PubMed]
- Lawrence DR, Ohri SK, Moxon RE, et al. Thoracoscopic debridement of empyema thoracis. Ann Thorac Surg 1997;64:1448-50. [Crossref] [PubMed]
- Wait MA, Sharma S, Hohn J, et al. A randomized trial of empyema therapy. Chest 1997;111:1548-51. [Crossref] [PubMed]
- Cassina PC, Hauser M, Hillejan L, et al. Video-assisted thoracoscopy in the treatment of pleural empyema: stage-based management and outcome. J Thorac Cardiovasc Surg 1999;117:234-8. [Crossref] [PubMed]
- Wurnig PN, Wittmer V, Pridun NS, et al. Video-assisted thoracic surgery for pleural empyema. Ann Thorac Surg 2006;81:309-13. [Crossref] [PubMed]
- Lardinois D, Gock M, Pezzetta E, et al. Delayed referral and gram-negative organisms increase the conversion thoracotomy rate in patients undergoing video-assisted thoracoscopic surgery for empyema. Ann Thorac Surg 2005;79:1851-6. [Crossref] [PubMed]
- Luh SP, Chou MC, Wang LS, et al. Video-assisted thoracoscopic surgery in the treatment of complicated parapneumonic effusions or empyemas: outcome of 234 patients. Chest 2005;127:1427-32. [PubMed]
- Solaini L, Prusciano F, Bagioni P. Video-assisted thoracic surgery in the treatment of pleural empyema. Surg Endosc 2007;21:280-4. [Crossref] [PubMed]
- Waller DA, Rengarajan A. Thoracoscopic decortication: a role for video-assisted surgery in chronic postpneumonic pleural empyema. Ann Thorac Surg 2001;71:1813-6. [Crossref] [PubMed]
- Cassina PC, Hauser M, Hillejan L, et al. Video-assisted thoracoscopy in the treatment of pleural empyema: stage-based management and outcome. J Thorac Cardiovasc Surg 1999;117:234-8. [Crossref] [PubMed]
- Metin M, Yeginsu A, Sayar A, et al. Treatment of multiloculated empyema thoracis using minimally invasive methods. Singapore Med J 2010;51:242-6. [PubMed]
- Shahin Y, Duffy J, Beggs D, et al. Surgical management of primary empyema of the pleural cavity: outcome of 81 patients. Interact Cardiovasc Thorac Surg 2010;10:565-7. [Crossref] [PubMed]
- Lackner RP, Hughes R, Anderson LA, et al. Video-assisted evacuation of empyema is the preferred procedure for management of pleural space infections. Am J Surg 2000;179:27-30. [Crossref] [PubMed]


