
Geriatric chest wall injury: is it time for a new sense of urgency?
Introduction
Geriatric trauma has become an increasingly recognized management concern for trauma centers and hospitals alike on a national scale. The geriatric trauma patient population poses unique challenges to providers as the aging process, often coupled with pre-existing medical comorbidities, limits the geriatric trauma patient’s physiologic reserve and negatively impacts their response to injury. Outcomes in the geriatric trauma patient population have been amply reported to be worse when compared to younger trauma patients. Increased awareness of these differences in post-traumatic morbidities, lifestyle changes, and survival statistics have spotlighted the need for better understanding of the elderly trauma patient, their response to injury, and for the development of predictive models to allow for improving outcomes.
The population of the United States is aging as life expectancy rates have demonstrated a steady climb to an average of 78.8 years of expected life (1). The rise in life expectancy rates has resulted in an increased density in the United States population of elderly patients (age ≥65). The United States Census Bureau estimates from 2010 revealed that 40 million of the United States population were ≥65 years of age and anticipates an increase to 80 million of the total population being ≥65 years or older by 2040 (2). With pervasive efforts of medical screening, prevention, and chronic medical condition management, more elderly people will lead more active lifestyles and will be more predisposed to injury (3).
As best practice guidelines specific for the geriatric trauma population are being developed, many researchers have identified management strategies that have offset complications and mortality rates inherent to this patient population after injury. For example, avoidance of prolonged occult hypoperfusion, using age as a criterion for trauma team activation, expeditious surgical repair of orthopedic injuries and debridement of burns, as well as the application of geriatric specific trauma services for the inpatient management of elderly trauma patients have demonstrated meaningful impact in survival data in this patient population (4-8).
Additionally, the impact of rib fractures in the 65-year and older patient population has been well documented, as have the mortality and pneumonia rates (9) yet the acceptance of rib plating as a management strategy for injuries to the chest wall continues to be debated as the absolute indications and patient selection criteria for this procedure remains uncertain. Rib fractures in the 65-year and older patient population carry an average mortality risk of 20% and a pneumonia acquisition risk of 19% (9). The mortality rate has been observed to increase approximately 10% thereafter for each additional fractured rib (9), resulting in impressively high negative predictors for survival. With such compelling negative outcome data, the authors wonder why the adoption of rib plating for the geriatric patient is not more widespread.
In this review, we examine the characteristics of the geriatric trauma patient, areas of management where improvement opportunities have been identified, chest wall injury in the elderly patient, rib plating as a treatment option, and offer our data to facilitate a better understanding of rib plating’s impact in the geriatric trauma patient.
Physiological characteristics in the elderly
Age-associated decline in physiologic performance is known to impact human beings on the cellular level, ultimately influencing end organ performance in every organ system. Overall organ performance depreciates from basal expectations and demonstrates a reduction in maximal and functional reserve with age (10). A progressive deterioration in cellular function leads to the loss of cellular capacity to tolerate insult (11,12), taxing adaptive and homeostatic mechanisms, and leading to impaired physiological reserve (11-13). Coupled with organ-specific comorbidities and their associated medical treatments, the age-associated cellular performance decline alters the elderly’s response to physical insult making them more intolerant to a traumatic injury (11,12,14,15).
Advanced aged patients are more likely to harbor cognitive and neuro-sensory/motor difficulties (11,12,14) resulting in generalized weakness, physical performance limitations, and gait instability (12). Age-associated bone loss and osteoporosis (12,14) is exceedingly common in geriatric trauma patients and aging bones are more easily fractured with minor trauma (16). Osteoporosis, particularly in females, is associated with an increased susceptibility to bony injury and fractures (11,12).
Geriatric patients commonly have cardiovascular disease and a subsequent impaired sensitivity to catecholamines (12) which makes mounting a compensatory response to injury or stress less effective. Additionally, polypharmacy associated with the management of hyper- or hypotension, and rhythm or rate irregularities (11,12,14,15) will blunt or impair an elderly patient’s response to injury (12,14).
Respiratory performance in the elderly is altered and this age-associated change is multifactorial in nature. The geriatric trauma patient will have decreased functional residual capacity, impaired mucociliary clearance of bacteria, reduced cough effectiveness and reduction in lung and chest wall compliance (11,12,14). These factors result in increased work of breathing and higher risks of respiratory failure, need of mechanical ventilation, susceptibility to community acquired, hospital acquired and ventilator associated pneumonias, as well as elevated intensive care unit admission rates (12,14,17). As the respiratory system ages, there is loss of parenchymal elasticity and chest wall compliance making the respiratory cycle less effective (18). Maximal inspiratory and expiratory pressures seem to decrease across both male and female age groups over time (18). Steroids, often administered in patients with chronic obstructive pulmonary disease, can disturb wound healing, induce adrenal impairment and have deleterious effects in patients with traumatic brain injury (12,14,19).
Geriatric management observations
Traumatic injuries are the fifth leading cause of death in elderly patients (20). Trauma patients aged ≥65 years present with an array of comorbidities that imply a higher risk of death and severe disability (21), despite having similar injury severity scores to those of younger patients (22,23). Lehmann et al. reported a statewide analysis in Washington state demonstrating a 4-fold increase in deaths and discharge with disability and clinical complications compared to patients under the age of 65 years (24).
Multiple reviews have found that elderly trauma patients are usually under-triaged to trauma centers (12,14,16,25). Demetriades et al. recognized an accelerated mortality rate in elderly patients of 16%, and an ICU admission rate of 24% of elderly when they did not meet trauma team activation criteria, leading to the consideration of age greater than or equal to 70 years alone as a criterion for trauma team activation (5). Furthermore, elderly patients have been shown to have a decreased mortality risk if they are transferred to trauma centers with a high volume of elderly trauma patients practice experience (26), findings which suggest a more aggressive approach to the management of the geriatric trauma patient is needed to improve survival.
Patients older than 55 years of age with prolonged occult hypoperfusion have been identified exhibiting a near 6-fold increase in mortality compared to patients younger than 55 years of age. These findings indicate that geriatric patients, having less physiologic reserve, may not have been able to adequately compensate for prolonged occult hypoperfusion, emphasizing the importance of rapidly correcting serologic acidosis as an endpoint in resuscitation in this population (4).
Geriatric trauma services, dedicating an inpatient unit and care delivery team, have established patient management trends for patients 60 years and older. The team based approach provides expeditious admission and operative services while tailoring the clinical care delivered to the specific needs of the geriatric trauma patient (8). The multidisciplinary approach has improved survival statistics and complication rates across this population of elderly admissions.
Colais et al. demonstrated an association between time to surgery and one-year mortality for all elderly patients hospitalized for hip fractures. The study revealed that patients who underwent hip surgery within two days had a lower one-year mortality compared to those who waited for surgery more than two days. The investigative work confirmed previous reports on the association between delayed surgery and increased mortality and complication rates in elderly patients admitted for hip fractures (6). Expeditious surgical treatments have been shown to be of benefit for not just orthopedic injuries, but also for the early excision and grafting of burns in the elderly. This shortens hospital stay and improves survival (7).
Geriatric chest wall injury and rib plating
Rib fractures after chest wall trauma are a very common injury. However, they carry a significant morbidity and mortality risk, can lead to long term disabilities, pro-longed narcotic use, pneumonia, respiratory difficulties, and complicate the rehabilitation of other injuries (1-3). Historical treatment options have been limited to conservative management in the form of analgesia, pulmonary toilet, oxygen support, and the allowance of time to heal the wound. With the development of plating systems for rib fracture fixation and chest wall stabilization, the practice paradigm for rib fracture management is shifting, as a viable operative intervention now exists to improve clinical outcomes.
Rib fractures in the 65-year and older patient population have been recognized to strongly influence mortality and pneumonia rates as well as increase intensive care stay days, ventilator days and hospital days (9). With estimated mortality and pneumonia rates of 20% and 19%, respectively, and 10% increase in mortality risk for each additional rib (9), rib fractures may be the most commonly encountered threat to survival in the geriatric trauma patient.
Despite these negative outcome statistics, the majority of rib fractures in this patient population continue to be managed with conservative measures. The 65-year and older population often carry limited or fragile physiologic reserves and present with pre-existing, multisystem issues making rib fractures a dangerous injury burden to bare. With diminished pulmonary function and capacity coupled with pain-limited respiratory cycles, the injured geriatric chest wall is a primer for deleterious outcomes if left inappropriately attended to.
Our investigative group, Fitzgerald et al. reported an institutional experience in 23 patients ≥65 years old having undergone rib plating. The operative population had no deaths, pneumonias or respiratory complications, outcomes that historical data would have predicted otherwise. Within the operative group, it was also observed that patients demonstrated an accelerated exit from rehabilitation facilities and return to a satisfying functional state, based on responses from surveyed patients (27).
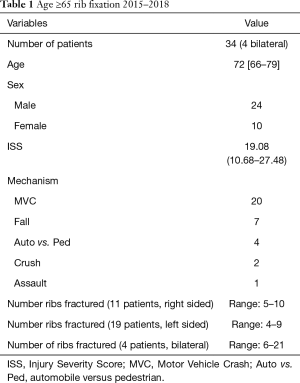
Since 2015, we have recorded 34 additional plating cases in the ≥65 years old patient population. Demographic data, mechanism of injury, injury severity scores, and number of ribs fractured were recorded (Table 1). Follow up imaging was reviewed and findings were reported. We saw no deaths, recurrent pneumothoraces, pleural effusions, soft tissue or hardware infections/malfunctions and had only one readmission over a three-year time span (Table 2). The single readmission was for a pneumonia that was acquired eight months after the patients index admission for trauma. While control groups were not made available for this report, our observations in the rib plated patients outperform historical expectations of patients with rib fractures in this age grouping.
Full table

Full table
Summary/conclusions
The geriatric patient population poses unique challenges to clinical providers and the broad scope of these challenges are more recently recognized. With the known age-associated physiologic diminishment, lack of physiologic reserve and high morbidity and mortality rates encountered in these patients, more aggressive care strategies are needed to improve outcomes as the population is only growing.
Rib fractures are a known threat to geriatric trauma patient survival and can negatively impact recovery and rehabilitation of other injuries. Functional and lifestyle limitations from patient baseline are common endpoints after chest wall trauma in the elderly patient population. With age-associated decline in global pulmonary function, pain from rib fractures and subsequent impairment of the respiratory cycle, rib fractures alter the trajectory of not just survival potential, but quality of recovery as well. Rib plating in this patient population seems to improve these outcome measures and, in the authors’ opinion, should become a strongly considered adjunct, if not first line therapeutic option, for rib fractures in the geriatric patient population.
While no formal management consensus exists, the general trend seems to be towards dedicating more resources to the geriatric trauma patient, more aggressive triage of the geriatric trauma patient to trauma centers, more aggressive and better tailored resuscitation and management strategies for the geriatric trauma patient, and more expeditious surgical care for traditional orthopedic injuries of the geriatric trauma patient. With the world’s literature reporting significant mortality and morbidity associated with rib fractures coupled with the aforementioned concerns in the geriatric trauma patient, why would we not be more aggressive in plating the geriatric trauma patients injured chest wall?
Acknowledgements
None.
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
References
- Arias E. United States Life Tables, 2000. Available online: http://www.cdc.gov/nchs/data/nvsr/nvsr51/nvsr51_03.pdf
- U.S. Census Bureau 2002b and 2008d. Available online: https://www.census.gov/content/dam/Census/library/publications/2014/demo/p23-212.pdf
- Hashmi A, Ibrahim-Zada I, Rhee P, et al. Predictors of mortality in geriatric trauma patients: a systematic review and meta-analysis. J Trauma Acute Care Surg 2014;76:894-901. [Crossref] [PubMed]
- Schulman AM, Claridge JA, Young JS. Young versus old: factors affecting mortality after blunt traumatic injury. Am Surg 2002;68:942-7. [PubMed]
- Demetriades D, Sava J, Alo K, et al. Old age as a criterion for trauma team activation. J Trauma 2001;51:754-6. [Crossref] [PubMed]
- Colais P, Di Martino M, Fusco D, et al. The effect of early surgery after hip fracture on 1-year mortality. BMC Geriatr 2015;15:141. [Crossref] [PubMed]
- Deitch EA. A policy of early excision and grafting in elderly burn patients shortens the hospital stay and improves survival. Burns Incl Therm Inj 1985;12:109-14. [Crossref] [PubMed]
- Mangram A. Innovations in geriatric trauma and resident research education: bridging the gap. Am J Surg 2013;206:834-9. [Crossref] [PubMed]
- Bulger EM, Arneson MA, Mock CN, et al. Rib fractures in the elderly. J Trauma 2000;48:1040-6. [Crossref] [PubMed]
- Yelon JA. Chapter 44. Trauma 7th Edition. New York, NY: McGraw-Hill, 2013:874-85.
- Banks SE, Lewis MC. Trauma in the elderly: considerations for anesthetic management. Anesthesiol Clin 2013;31:127-39. [Crossref] [PubMed]
- Llompart-Pou JA, Pérez-Bárcena J, Chico-Fernández M, et al. Severe trauma in the geriatric population. World J Crit Care Med 2017;6:99-106. [Crossref] [PubMed]
- Frankenfield D, Cooney RN, Smith JS, et al. Age-related differences in the metabolic response to injury. J Trauma 2000;48:49-56; discussion 56-57. [Crossref] [PubMed]
- Bonne S, Schuerer DJ. Trauma in the older adult: epidemiology and evolving geriatric trauma principles. Clin Geriatr Med 2013;29:137-50. [Crossref] [PubMed]
- Adams SD, Holcomb JB. Geriatric trauma. Curr Opin Crit Care 2015;21:520-6. [PubMed]
- Reske-Nielsen C, Medzon R. Geriatric Trauma. Emerg Med Clin North Am 2016;34:483-500. [Crossref] [PubMed]
- Chalfin DB. Outcome assessment in elderly patients with critical illness and respiratory failure. Clin Chest Med 1993;14:583-9. [PubMed]
- Janssens JP. Aging of the respiratory system: impact on pulmonary function tests and adaptation to exertion. Clin Chest Med 2005;26:469-84. [Crossref] [PubMed]
- Edwards P, Arango M, Balica L, et al. Final results of MRC CRASH, a randomised placebo-controlled trial of intravenous corticosteroid in adults with head injury-outcomes at 6 months. Lancet 2005;365:1957-9. [Crossref] [PubMed]
- Aschkenasy MT, Rothenhaus TC. Trauma and falls in the elderly. Emerg Med Clin North Am 2006;24:413-32. vii. [Crossref] [PubMed]
- Keller JM, Sciadini MF, Sinclair E, et al. Geriatric trauma: demographics, injuries, and mortality. J Orthop Trauma 2012;26:e161-5. [Crossref] [PubMed]
- Taylor MD, Tracy JK, Meyer W, et al. Trauma in the elderly: intensive care unit resource use and outcome. J Trauma 2002;53:407-14. [Crossref] [PubMed]
- Llompart-Pou JA, Chico-Fernández M, Sánchez-Casado M, et al. Trauma Neurointensive Care Working Group of the Spanish Society of Intensive Care Medicine (SEMICYUC) Age-related injury patterns in Spanish trauma ICU patients. Results from the RETRAUCI. Injury 2016;47 Suppl 3:S61-5. [Crossref] [PubMed]
- Lehmann R, Beekley A, Casey L, et al. The impact of advanced age on trauma triage decisions and outcomes: a statewide analysis. Am J Surg 2009;197:571-4. [Crossref] [PubMed]
- Kozar RA, Arbabi S, Stein DM, et al. Injury in the aged: Geriatric trauma care at the crossroads. J Trauma Acute Care Surg 2015;78:1197-209. [Crossref] [PubMed]
- Zafar SN, Obirieze A, Schneider EB, et al. Outcomes of trauma care at centers treating a higher proportion of older patients: the case for geriatric trauma centers. J Trauma Acute Care Surg 2015;78:852-9. [Crossref] [PubMed]
- Fitzgerald MT, Ashley DW, Abukhdeir H, et al. Rib fracture fixation in the 65 years and older population: A paradigm shift in management strategy at a Level I trauma center. J Trauma Acute Care Surg 2017;82:524-7. [Crossref] [PubMed]


