
Acute effects of air pollutants on daily mortality and hospitalizations due to cardiovascular and respiratory diseases
Introduction
Air pollution is becoming an increasing concern around the world. Several reports have shown associations between acute or chronic exposure to air pollution and morbidity or mortality (1-3). Previous studies have shown association between ambient air pollution exposure and clinical events such as emergency visit, hospital admission for respiratory diseases (4-11), cardiovascular diseases (7,12-19), and cerebrovascular diseases (20). In addition, a number of studies have shown a connection between ambient air pollution exposure and non-accidental mortality (21-26).
The relationship between air pollution and detrimental health effect in Chiang Mai province located in northern Thailand has been recognized for more than a decade. However, only two studies documenting the negative impact of air pollution on health have been published (27,28). The association between ambient air pollutants including nitrogen dioxide (NO2), sulfur dioxide (SO2), particulate matters less than 10 microns (PM10) with decreased lung function measured by peak expiratory flow rate (PEFR) was found in asthma patients (27). Another study revealed the association between PM10 and exacerbations of chronic obstructive pulmonary disease (COPD) and asthma (28). In our study subjects who lived only in the metropolitan area of Chiang Mai province were included and not those from the rural regions of northern Thailand that were more seriously affected by seasonal air pollution caused by agricultural farm burnings and forest fires. Most of the housing style of community dwellers in rural area is open-air houses without built-in air conditioners or air purifiers. This allows the outdoor air to be almost the same as indoor air in terms of particulate content. Chiang Dao district is one of the rural communities located in the north of Chiang Mai approximately 770 kilometers from Bangkok. It covers an area of approximately 1,882 km2 and is surrounded by high mountain range. Besides, the vast majority of rural dwellers are farmers or gardeners. There is around 90,000 Chiang Dao dwellers distributed among 7 administrative sub-districts with only one single 60 bed-community serve the health needs of local dwellers. All wards of this community hospital are open-air style buildings unequipped with air conditioners or air purifier systems exposing the patients to outdoor air pollutants in the same way as their houses. Chiang Dao, like all districts in Chiang Mai, has been facing seasonal air pollution from January to April annually for the past decade. The daily average level of PM10 has been recorded to reach above 50 micrograms per cubic meter (µg)/m3 more than one third of each preceding year (28).
We selected Chiang Dao district for this study based on several reasons; it is one of the districts in Chiang Mai facing high level of seasonal air pollution every year, its geographical features surrounded by mountain ranges, the exposure of community dwellers to outdoor air pollutants 24 hours a day during seasonal smog period because of their open-air housing style, and agricultural occupational hazard. In addition, Chiang Dao hospital is the only available hospital serving the community with open-air wards; therefore we could certainly to identify the association between air pollution and mortality of hospitalized patients. Our first objective is to determine the association between air pollutants and mortality of hospitalized patients and community dwellers. The second objective is to determine the associations between air pollutants and both emergency and hospitalization visits for acute serious respiratory, cardiovascular, and cerebrovascular events in the study population.
Methods
Design and study participants
A time series study was conducted between March 2016 and March 2017 in Chiang Dao district, Chiang Mai, Thailand. The ICD-10 registry records, collected from Chiang Dao hospital for daily emergency- and hospitalization visits due to acute respiratory (acute exacerbation of chronic obstructive pulmonary disease and community-acquired pneumonia, AECOPD and CAP), acute cardiovascular events (acute myocardial infarction and congestive heart failure, MI and HF), and acute cerebrovascular events (hemorrhagic and ischemic strokes, cerebrovascular accident, CVA) were reviewed and adjudicated by at least two physicians in the study team and one physician of Chiang Dao hospital. In addition the daily numbers of emergency and hospitalization visits due to AECOPD, CAP, MI, HF, and CVA were recorded by the physicians on duty in the emergency room with the primary diagnoses based on the International Classification of Diseases (ICD) version 10 (ICD-10 J44.1, J18, I21, I50, and I63 for AECOPD, CAP, MI, HF, and CVA, respectively). These data were reviewed and adjudicated by a dedicated physician team from the emergency room, a pulmonologist, and a cardiologist in the study team based on ICD-10. A special permission was received to extract data on daily deaths of hospitalized patients and community dwellers (excluding accidental and suicidal deaths) of Chiang Dao district from the Registry of hospital deaths and from the Office of certification and registration of local deaths. The study was approved by the Ethics Committee of the Faculty of Medicine, Chiang Mai University (Study code: MED-2558-03032, Date approval: 14th December 2015).
Measurements of air pollutants and meteorological parameters
Sampling station was located in Chiang Dao hospital, Chiang Mai, Thailand. Ambient air concentration of pollutants was measured by the DustDETECTTM. The analytical method for PM was specifically designed to monitor the flow of particulate emissions from small stacks and emission points being passed through an air filtration system. The data reported were daily maximum, minimum, and average concentrations for PM10, PM2.5, SO2, NO2, carbon monoxide (CO), and ozone (O3). The unit of the air pollutants was µg/m3. The meteorological data including temperature, relative humidity, rainfall, wind speed, and pressure from the meteorology monitoring stations in Chiang Dao district can be obtained from the meteorological department website at https://meteorology.hrdi.or.th.
Statistical analysis
Results for numerical values were expressed as means ± SD or median, IQR (Interquartile range) and those for categorical data were expressed as absolute frequencies and percentages. The association between daily average concentrations of air pollutants and daily deaths of hospitalized patients and community dwellers, as well as the incidence of AECOPD, CAP, MI, HF, and CVA were analyzed using the application of general linear models with Poisson distribution, a method of analysis which has performed reliably and satisfactorily in previous studies (27,28). Poisson models with log links are often called log-linear models and are used for frequency data. To find out the association between the effect of air pollutants on disease exacerbation, Poisson regression was used for analysis after adjustment for the temperature, wind speed, pressure, rainfall and relative humidity. To assess the lag structure between concentrations of air pollutants and deaths of hospitalized patients and community dwellers as well as emergency and hospitalization visits of serious respiratory, cardiovascular, and cerebrovascular events, we initially examined separate models for each lag from 0 to 7 days prior to the deaths or visits. The lag time zero (lag 0) was defined as the day of air pollutants measurement. Finally, risk regression analysis was applied to the data in order to estimate relative risk (RR) with 95% confidence intervals (CI) of the independent variables in the constructed model. The adjusted RRs were estimated with each 10 µg/m3 increment of PM2.5, PM10, and CO, each 1 µg/m3 increment of NO2, and O3, and each 0.1 µg/m3 increment of SO2. All analyses were carried out with the SPSS statistical package, version 22 for IBM (SPSS Inc., IL, USA).
Results
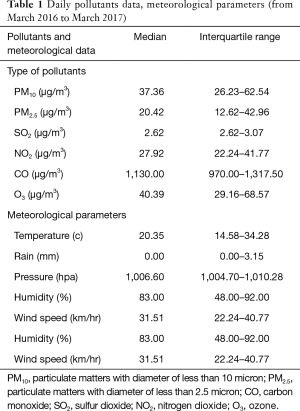
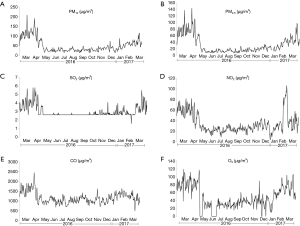
The daily pollutants data including PM10, PM2.5, SO2, NO2, CO, O3, and meteorological parameters are shown in Table 1. Concentrations of all air pollutants were maximal in March of both years (2016 and 2017). The daily variations of each pollutant throughout the study year were shown in Figure 1.
Full table
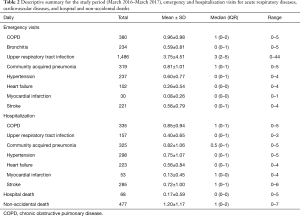
Deaths of hospitalized patients and non-accidental deaths of community dwellers are shown in Table 2. After screening a total of 4,685 visits (3,009 and 1,676 for emergency and hospitalization visit, respectively) at the Chiang Dao hospital between March 2016 and March 2017, total emergency visits of 2,419 and 590 patients with acute respiratory, cardiovascular and cerebrovascular events were included for analysis. The most common of acute respiratory event was upper respiratory tract infection (URI) and the one for acute cardiovascular and cerebrovascular events was acute hypertension (HT). Total hospitalization admissions of 1,676 emergencies (817 for acute respiratory and 859 for cardiovascular and cerebrovascular events) were included for analysis (Table 2). Acute serious respiratory events were defined as AECOPD and CAP and acute serious cardiovascular and cerebrovascular events were defined as MI, HF and CVA in this study.
Full table
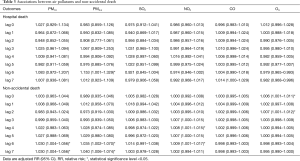
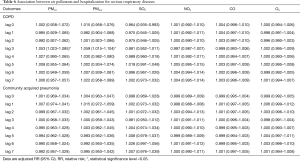
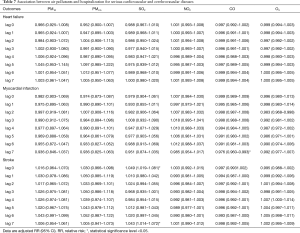
After adjustment for temperature, relative humidity, rainfall, wind speed, and pressure, the association between air pollutants and deaths of hospitalized patients and community dwellers are shown in Table 3. PM2.5, PM10, NO2 and O3 were found to have a positive association with daily mortality of community dwellers on different lag days but only PM2.5 had a positive association with daily mortality of hospitalized patients (adjusted RR =1.153; 95% CI: 1.001–1.329). The associations between each of air pollutants (PM10, PM2.5, SO2, NO2, CO, O3) and emergency and hospitalization visits of AECOPD, CAP, MI, HF, and CVA on different lag days are shown in Tables 4-7. For acute serious respiratory events, PM2.5 and PM10 had a positive association with both emergency and hospitalized visits of AECOPD while SO2, CO, O3 had a positive association with emergency visits of CAP only (Table 4). For acute serious cardiovascular events, NO2 and O3 also had a positive association with emergency visits, but not with hospitalization visits of MI and HF (Tables 5 and 7). Only SO2 had a positive association with CVA (Table 7).
Full table
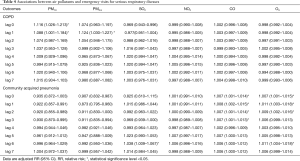
Full table
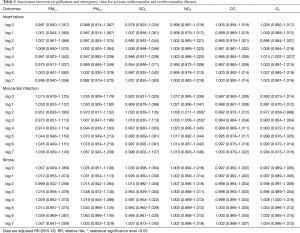
Full table
Full table
Full table
Discussion
This prospective epidemiologic time-series study in a single community with documented exposure to seasonal air pollution revealed the association between air pollutants and daily mortality of hospitalized patients and community dwellers, as well as differential effects of air pollutants on acute serious respiratory (AECOPD and CAP), cardiovascular (MI and HF) and cerebrovascular (CVA) events requiring emergency and/or hospitalization visits soon after exposure.
The relationship between increased concentrations of air pollutants and non accidental mortality of population which has been well documented worldwide (21-26), was reconfirmed in this study. However the association has never been studied during seasonal air pollution period as in our study in northern Thailand. Moreover, the study revealed that short term exposure to PM2.5 increased the relative risk of daily mortality of hospitalized patients by 15.3% per 10 µg/m3 (lag day 6, relative risk =1.153, 95% CI: 1.001–1.329) which to the best of our knowledge, this is the first time-series study of air pollution which demonstrated the association of air pollutant with daily mortality of hospitalized patients. The relative risk of PM2.5 associated with daily mortality of hospitalized patients in our study was found to be 4.4-fold higher than that of community dwellers (3.5% per 10 µg/m3 at lag day 6, relative risk =1.035, 95% CI: 1.002–1.070) (Table 3). Most probably the hospitalized patients were more vulnerable to the detrimental effect of air pollutants than community dwellers as they were more seriously ill and remained exposed to the ambient air pollutants in the open-air wards.
The daily mortality of community dwellers was sharply increased on lag days 0 and 2 of increased O3 concentration (0.6% and 0.7%), whereas the relative risks of PM10, PM2.5, and NO2 were 3%, 3.5–4%, and 0.8–0.9%, respectively and more delayed (lag day 6–7 for PM10 and PM2.5 and lag day 4, 6 for NO2, respectively) than that of O3. The short-term lag patterns of the associations between air pollutant exposures and mortality were mainly limited to early days of exposure (lag 0–7 days) which is consistent with a previous report of air pollution-mortality relationship in Thailand (23). As in previous studies, non-accidental mortality increased after increase of level of O3 value (23,25,26) and NO2 (21). Interestingly, the associations between non-accidental mortality of PM10 and PM2.5 in our study were increased (range, 3.00–4.00%, lag day 6–7) 3–10 times higher than that of previous studies (range, 0.28–1.10% and 0.22–0.71% for PM2.5 and PM10, respectively) (21-24). A meta-analysis of Asian studies indicated a mean increase in risk of 0.4–0.5% with a one-day per 10 µg/m3 change in PM10 (23). It was reported that the likelihood of an adverse response to an inhaled pollutant depends on the degree of exposure and individual characteristics such as the susceptibility of the exposed person (29). Although, the individual susceptibility could not be identified with our study design, several factors could explain the higher mortality in our study. First, our study population group was elderly people of low socioeconomic status, with exposure to seasonal air pollution for several years due to their occupation, living and housing styles. The intensity [PM10 and PM2.5 mean =88.86 (40.25–208.63) and 61.76 (25.04–14.00) µg/m3, respectively] and duration of exposure (3 months from February – April) of seasonal air pollutants during the study period could also significantly contributed to such a high mortality (Figure 1).
Our results for the two acute serious respiratory events, CAP and AECOPD, were consistent with the previous finding linking the lag structure between pollutant levels and emergency or hospitalization visits. The association between emergency visits for CAP was positive on the same day of increased pollutant levels and lag days from 1–4 days and 1–2 days for CO and O3, respectively. Previous studies have reported that CAP increased shortly (lag day 0–5) after increased levels of SO2, CO and O3 (5,9). Although this study confirmed the association between gaseous air pollutants (SO2, CO and O3) and emergency visits for CAP, it did not confirm the association of any air pollutants with hospital admissions for CAP. The reason could be severe cases presenting to emergency room might be referred to the provincial hospital downtown or mild cases might be managed as outpatient cases. The association between emergency visits of AECOPD were positive at the same day of increased pollutant levels and lag day 1 for PM10, whereas the lag period of PM2.5 was at lag day 1 only which was consistent with some other studies (4,5). However, our previous report on the effect of PM10 on AECOPD in metropolitan area of Chiang Mai during seasonal smog was more delayed (lag day 7) (28). The difference of lag effect between the rural and urban area of the same province besides the difference in study years and degree of exposure to PM10 (e.g., housing style, occupation, protection awareness) might also be explained by the differences in disease severity and management (30). Emergency visits for AECOPD increased shortly (lag 1 day) after increased level of PM2.5 (8,10) while, the association between hospital admissions for AECOPD was positive for both PM10 and PM2.5 on lag day3 as shown in previous studies (4,6,11,31,32).
The association between air pollutants and emergency or hospitalization visits for cardiovascular events (MI and HF) were also demonstrated in our study. We found emergency visits, but not hospital admissions, of HF increased shortly after increase in O3 concentration (lag day 4) as in the previous study (14). The likely reason could be the same as that for CAP. The previous reports also showed the similar results with our study that emergency visits for MI increased shortly after elevated level of NO2 (ranged from lag day 0 and 2) (15,16). Emergency visits and hospital admissions for CVA increased after increase of level of SO2 (ranged from Lag 0 and 6 day) as reported previously (17-19).
Enhanced oxidative stress and systemic inflammatory pathways triggered by free oxygen radicals from air pollutants capable of penetrating deep into alveoli was reported to play a key role in the pathophysiology of many pulmonary (33) and cardiovascular diseases (34,35) possibly increasing the rate of non-accidental mortality as in our study. The short-term lag pattern of the association between air pollution exposure and non-accidental mortality is very important for healthcare providers and public health authorities (23). Our results showing the impact of air pollution on non-accidental mortality was mainly limited to early days of exposure (lag day 0–7). Developing timely preventive measures are effective in reducing the health effects of air pollution is urgently required for extreme air pollution periods. Guo et al., suggested that the government, public health and medical professionals, and general population should all be well aware of health warning systems and the perception of the dangers of air pollution (23).
The study has many strengths. Firstly, we use time series analysis to assess the trends and relationships using generalize linear models with Poisson regression analysis, which is in the same format as the previous studies (5,27,28). Secondly, the association between all air pollutants and health effects were adjusted with rain, pressure, wind speed, temperature, and humidity. Thirdly, we selected only Chiang Dao district population living in geographic areas exposed to the entire seasonal air pollution period as well as the whole day exposure with their open-air housing style, agricultural occupation, and the open-air wards of community hospital. Moreover, this community hospital is the only health facility that all local dwellers frequented to receive primary health evaluation and management.
Our study also has a number of limitations. Firstly, although the diagnoses of serious respiratory, cardiovascular, and cerebrovascular events were reviewed and adjudicated by dedicated team members and emergency room physicians, some relevant clinical data such as disease severity, clinical and biomedical risk factors, history of frequency of previous attacks, and management were not usually available in routine electronic medical records. However, these records were critically reviewed by the pulmonologist and cardiologist in the study team for relevant diagnoses. Secondly, the health care utilization and mortality data of only one hospital was chosen to estimate the impact of air pollutants, a possible selection bias could affect the validity of the results. However, data from only one hospital in the area could reflect the overall impact of the air pollutants for this specified area. Thirdly, there is no data about the association between long term exposure to air pollutions and health. Effect of long term air pollution should be addressed in the future studies. Lastly, this time series study was only conducted in one district (Chiang Dao district, Chiang Mai, Thailand). Therefore, these results can be generalized only to area s with the same pollution, environmental and socio-economic status.
Conclusions
Our study found that air pollutants are a major environmental health risk and effects on a variety of acute respiratory and cardiovascular diseases and increase non-accidental mortality. Thus, it is necessary to pay attention to the dangers of air pollution and to inform the public on how to minimize their risks from exposure to air pollution. Our findings support the government efforts in reducing high levels of air pollution, in order to improve the public health and reduce the burden of disease due to ambient air pollution in the population e.g., providing clean room, air purifier, and mask.
Acknowledgments
The authors would like to thank the Thai Meteorological Department for providing the data on weather conditions and acknowledge the staff members of Chiang Dao hospital for their data contribution for this study. This study is funded by the grant funding of the Faculty of Medicine, Chiang Mai University (Grant No. 067/2559).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Ethics Committee of the Faculty of Medicine, Chiang Mai University (Study code: MED-2558-03032, Date approval: 14th December 2015).
References
- Fajersztajn L, Saldiva P, Pereira LAA, et al. Short-term effects of fine particulate matter pollution on daily health events in Latin America: a systematic review and meta-analysis. Int J Public Health 2017;62:729-38. [Crossref] [PubMed]
- Rajak R, Chattopadhyay A. Short and long-term exposure to ambient air pollution and impact on health in India: a systematic review. Int J Environ Health Res 2019.1-25. [Epub ahead of print]. [Crossref] [PubMed]
- Newell K, Kartsonaki C, Lam KBH, et al. Cardiorespiratory health effects of gaseous ambient air pollution exposure in low and middle income countries: a systematic review and meta-analysis. Environ Health 2018;17:41. [Crossref] [PubMed]
- Faustini A, Stafoggia M, Colais P, et al. Air pollution and multiple acute respiratory outcomes. Eur Respir J 2013;42:304-13. [Crossref] [PubMed]
- Li R, Jiang N, Liu Q, et al. Impact of Air Pollutants on Outpatient Visits for Acute Respiratory Outcomes. Int J Environ Res Public Health 2017;14:47. [Crossref] [PubMed]
- Cheng MH, Chiu HF, Yang CY. Coarse Particulate Air Pollution Associated with Increased Risk of Hospital Admissions for Respiratory Diseases in a Tropical City, Kaohsiung, Taiwan. Int J Environ Res Public Health 2015;12:13053-68. [Crossref] [PubMed]
- Peng RD, Chang HH, Bell ML, et al. Coarse particulate matter air pollution and hospital admissions for cardiovascular and respiratory diseases among Medicare patients. JAMA 2008;299:2172-9. [Crossref] [PubMed]
- Szyszkowicz M, Kousha T, Castner J, et al. Air pollution and emergency department visits for respiratory diseases: A multi-city case crossover study. Environ Res 2018;163:263-9. [Crossref] [PubMed]
- Nhung NTT, Amini H, Schindler C, et al. Short-term association between ambient air pollution and pneumonia in children: A systematic review and meta-analysis of time-series and case-crossover studies. Environ Pollut 2017;230:1000-8. [Crossref] [PubMed]
- Tian Y, Xiang X, Juan J, et al. Short-term effects of ambient fine particulate matter pollution on hospital visits for chronic obstructive pulmonary disease in Beijing, China. Environ Health 2018;17:21. [Crossref] [PubMed]
- Sun XW, Chen PL, Ren L, et al. The cumulative effect of air pollutants on the acute exacerbation of COPD in Shanghai, China. Sci Total Environ 2018;622-623:875-81. [Crossref] [PubMed]
- Fung KY, Luginaah I, Gorey KM, et al. Air pollution and daily hospital admissions for cardiovascular diseases in Windsor, Ontario. Can J Public Health 2005;96:29-33. [PubMed]
- Lee BJ, Kim B, Lee K. Air pollution exposure and cardiovascular disease. Toxicol Res 2014;30:71-5. [Crossref] [PubMed]
- Liu H, Tian Y, Song J, et al. Effect of Ambient Air Pollution on Hospitalization for Heart Failure in 26 of China's Largest Cities. Am J Cardiol 2018;121:628-33. [Crossref] [PubMed]
- Xie J, He M, Zhu W. Acute effects of outdoor air pollution on emergency department visits due to five clinical subtypes of coronary heart diseases in shanghai, china. J Epidemiol 2014;24:452-9. [Crossref] [PubMed]
- Wang X, Kindzierski W, Kaul P. Air Pollution and Acute Myocardial Infarction Hospital Admission in Alberta, Canada: A Three-Step Procedure Case-Crossover Study. PloS One 2015;10:e0132769. [Crossref] [PubMed]
- Liu H, Tian Y, Xu Y, et al. Association between ambient air pollution and hospitalization for ischemic and hemorrhagic stroke in China: A multicity case-crossover study. Environ Pollut 2017;230:234-41. [Crossref] [PubMed]
- Huang F, Luo Y, Tan P, et al. Gaseous Air Pollution and the Risk for Stroke Admissions: A Case-Crossover Study in Beijing, China. Int J Environ Res Public Health 2017;14:189. [Crossref] [PubMed]
- Zhong H, Shu Z, Zhou Y, et al. Seasonal Effect on Association between Atmospheric Pollutants and Hospital Emergency Room Visit for Stroke. J Stroke Cerebrovasc Dis 2018;27:169-76. [Crossref] [PubMed]
- Wichmann J, Voyi K. Ambient air pollution exposure and respiratory, cardiovascular and cerebrovascular mortality in Cape Town, South Africa: 2001–2006. Int J Environ Res Public Health 2012;9:3978-4016. [Crossref] [PubMed]
- Zhang J, Liu Y, Cui LL, et al. Ambient air pollution, smog episodes and mortality in Jinan, China. Sci Rep 2017;7:11209. [Crossref] [PubMed]
- Chen R, Yin P, Meng X, et al. Fine Particulate Air Pollution and Daily Mortality. A Nationwide Analysis in 272 Chinese Cities. Am J Respir Crit Care Med 2017;196:73-81. [Crossref] [PubMed]
- Guo Y, Li S, Tawatsupa B, et al. The association between air pollution and mortality in Thailand. Sci Rep 2014;4:5509. [Crossref] [PubMed]
- Yi O, Hong Y, Kim H. Seasonal effect of PM(10) concentrations on mortality and morbidity in Seoul, Korea: a temperature-matched case-crossover analysis. Environ Res 2010;110:89-95. [Crossref] [PubMed]
- Yin P, Chen R, Wang L, et al. Ambient Ozone Pollution and Daily Mortality: A Nationwide Study in 272 Chinese Cities. Environ Health Perspect 2017;125:117006. [Crossref] [PubMed]
- Qin L, Gu J, Liang S, et al. Seasonal association between ambient ozone and mortality in Zhengzhou, China. Int J Biometeorol 2017;61:1003-10. [Crossref] [PubMed]
- Wiwatanadate P, Liwsrisakun C. Acute effects of air pollution on peak expiratory flow rates and symptoms among asthmatic patients in Chiang Mai, Thailand. Int J Hyg Environ Health 2011;214:251-7. [Crossref] [PubMed]
- Pothirat C, Tosukhowong A, Chaiwong W, et al. Effects of seasonal smog on asthma and COPD exacerbations requiring emergency visits in Chiang Mai, Thailand. Asian Pac J Allergy Immunol 2016;34:284-9. [PubMed]
- WHO air quality guidelines global update 2005 Report on a Working Group meeting; 2005. Available online: (accessed on 10 April 2016)http://www.euro.who.int
- Pothirat C, Chaiwong W, Phetsuk N, et al. A comparative study of COPD burden between urban vs rural communities in northern Thailand. Int J Chron Obstruct Pulmon Dis 2015;10:1035-42. [Crossref] [PubMed]
- Choi J, Oh JY, Lee YS, et al. Harmful impact of air pollution on severe acute exacerbation of chronic obstructive pulmonary disease: particulate matter is hazardous. Int J Chron Obstruct Pulmon Dis 2018;13:1053-9. [Crossref] [PubMed]
- Canova C, Dunster C, Kelly F, et al. PM10-induced hospital admissions for asthma and chronic obstructive pulmonary disease: the modifying effect of individual characteristics. Epidemiology 2012;23:607-15. [Crossref] [PubMed]
- Guan WJ, Zheng XY, Chung KF, et al. Impact of air pollution on the burden of chronic respiratory diseases in China: Time for urgent action. Lancet 2016;388:1939-51. [Crossref] [PubMed]
- Pope CA, Burnett RT, Thurston GD, et al. Cardiovascular mortality and long-term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation 2004;109:71-7. [Crossref] [PubMed]
- Oparil S, Zaman MA, Calhoun DA. Pathogenesis of hypertension. Ann Intern Med 2003;139:761-76. [Crossref] [PubMed]


