One-and-a-half syndrome with its spectrum disorders
One-and-a-half syndrome, a term originally coined by Fisher in 1976 to describe a syndrome with horizontal movement disorder of eyeballs, presents a combination of ipsilateral conjugate horizontal gaze palsy (one) and ipsilateral internuclear ophthalmoplegia (INO) (a half) (1). Along with one-and-a-half syndrome, there are a series of rare and uncommon syndromes that the lesion is closely related with one-and-a-half syndrome called one-and-a-half syndrome spectrum disorders. The diagnoses of one-and-a-half syndrome and its spectrum disorders rely on distinctive clinical symptoms, neuroanatomy, especially imaging technologies (2). Other associated symptoms including visual impairment, impaired swallowing and fine motor deficits may contribute to locating the lesions. The treatment depends on the causes of the syndrome. The article is mainly to summarize and analyse the clinical features, pathological anatomy and nomenclature of one-and-a-half syndrome spectrum disorders by displaying related clinical cases, in order to improve the understanding of neurologist and oculist about the series of the syndromes. Furthermore, we search related articles on PubMed and diagram these articles (Figure 1).

The brain structures and functions involving horizontal movement disorder in eyeballs
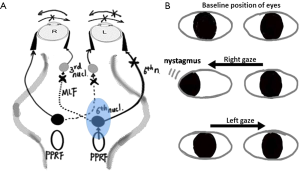
Brain structures involving the horizontal movement in eyeballs mainly include paramedian pontine reticular formation (PPRF), abducens nucleus and medial longitudinal fasciculus (MLF). The disorders of horizontal movement in eyeballs resulting from the damage to the above brain structures are divided into three categories: (I) horizontal gaze palsy; (II) INO; (III) one-and-a-half syndrome (3).
PPRF is the supranuclear center located near the ipsilateral abducens nucleus and the ventral MLF that receives the nerve impulses from visual area of the frontal and parietal lobes and controls horizontal conjugate eye movements (4). It is believed that the PPRF includes excitatory neurons and dominates the ipsilateral abducens nucleus (5). The ipsilateral abducens nucleus emits the abducens nerve, which controls the ipsilateral lateral rectus. It also emits MLF, which dominates the contralateral oculomotor subnucleus and then goes to control the contralateral medial rectus resulting in the ipsilateral eyeball abduction and the contralateral eyeball adduction, forming horizontal conjugate movement of eyes. If the isolated side of PPRF is damaged, the eyes could not gaze at the lesion side, presenting the horizontal gaze palsy to the lesion side (6).
The abducens nucleus is located in colliculus facialis, which is in the lower part of the pons and the bottom of the fourth ventricle (7). It contains two functionally distinct cell groups: the abducens motoneurons that innervate the lateral rectus muscle; the internuclear neurons which axons cross the midline and ascend via the contralateral MLF to oculomotor subnucleus and control the medial rectus (8). Therefore, the unilateral lesion of the abducens nucleus will also produce ipsilateral horizontal gaze paralysis.
MLF are the longitudinal nerve fibers that locate on the back of the pons and are close to the front of the fourth ventricle, a part of which relating to horizontal gaze is from the side of the abducens nucleus to the contralateral oculomotor subnucleus (9). The lesion of unilateral pontine tegmentum can damage the ipsilateral MLF, causing the ipsilateral INO, and its clinical manifestations show the ipsilateral intraocular muscle paralysis and contralateral horizontal nystagmus when staring at the opposite side. If the damage does not involve the midbrain, the convergence reflex is integrated (10).
One-and-a-half syndrome
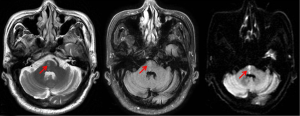
The one-and-a-half syndrome is caused by a lesion of unilateral tegmentum of pons, causing damage to the PPRF (or abducens nucleus) and MLF (Figure 2). The most common cause of one-and-a-half syndrome was cerebrovascular disease, and usually was brain stem lacunar infarction, followed by the demyelinating etiology (multiple sclerosis), and then the infectious cause including neurocysticercosis and brainstem encephalitis. Other uncommon causes were head trauma, brain stem tumor (primary or metastasis), astrocytomas, etc. (6,11). Therefore, the vast majority of one-and-a-half syndrome companied by other positioning signs is due to the different lesions of brainstem (3). Only a very small number of patients showed isolated one-and-a half syndrome, while the lesions are smaller and localized, such as brainstem cysticercosis, brainstem tuberculosis, brainstem cavernous hemangioma and the local hemorrhagic infarction of brainstem (12-15).
We recently diagnosed a patient with one-and-a half syndrome caused by brainstem infarction: an 83-year-old man with 10-year history of hypertension was admitted to the hospital with sudden onset of diplopia and weakness of the left lower limb for 4 days. MR brain imaging demonstrated a new infarction in the right pons (Figure 3). Neurological examination showed weakness of adduction and abduction of the right eye and restricted adduction of the left eye in conjugate horizontal gaze, abduction of the left eye with horizontal nystagmus, left central hemiparesis with grade 4 muscle strength. No other positive sign was found. We finally diagnosed the syndrome according to the representative clinical symptoms and brain magnetic resonance imaging. Antiplatelet, resist atherosclerosis (atorvastatin calcium), improved collateral circulation (butylphthalide) and the adjustment of blood pressure were applied, and the patient was gradually stabilized.
Eight-and-a-half syndrome
Eggenberger (16) reported three cases of one-and-a-half syndrome with ipsilateral peripheral facial paralysis in 1998, which was named eight-and-a-half syndrome (the seventh cranial nerve damage + one-and-a-half syndrome). However, the lesion was not detected at the head by MRI, but the location of the lesion was presumably derived. Therefore, Eggenberger argued that it was important to understand the clinical feature of the syndrome because the lesion may be small so that MRI does not clearly show the lesion.
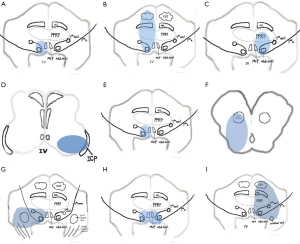
Until 8 years later, Nandhagopal and Krishnamoorthy (17) saw the lesion position in the head MRI T2WI, confirming Eggenberger’s presumption of lesion location. In this case, patients presented sudden onset of horizontal diplopia and right facial paralysis. The primary eye position was normal. The patient had combination of the right gaze paresis, along with impaired adduction in right eye and abduction with nystagmus in the left eye. The vertical movements of two eyes were normal, with right peripheral facial paralysis. The head MRI T2WI showed a high signal at the right paramedian pontine tegmentum. According to the patient’s signs and head MRI, the damaged sites were considered in the right abducens nucleus, right MLF and right facial nerve (Figure 4A). The paracentral artery occlusion of pons was considered in this case.
It is clear that the eight-and-a-half syndrome lesions are located in the ipsilateral PPRF, MLF, facial nerve nucleus or nerve bundle. Or the lesions damaged ipsilateral abducens nucleus, MLF, facial nerve nucleus or nerve bundle. Therefore, the lesion is easily located in the ipsilateral pontine tegmentum.
Similar to one-and-a-half syndrome, the common cause of eight-and-a-half syndrome is pontine infarction caused by the perforating artery occlusion. The rare causes include infection, tumor, demyelination, or brain stem vasculitis. Eight-and-a-half syndrome is the most common variant of one-and-a-half syndrome spectrum disorder.
Nine syndrome
The syndrome is based on the lesion of eight-and-a-half syndrome, due to the expansion of the pontine tegmentum lesion to the surrounding tissue to form a sort of clinical spectrum. So far there have been a total of three cases reported.
Rosini (18) reported the first case in 2013:
Case 1: a 71-year-old patient presented sudden right gaze paralysis and inability to adduction in the right eye, accompanied by right peripheral facial paralysis, left limb sustained mild hemiplegia and hemihypesthesia. The patient has a variety of cerebrovascular risk factors, such as obesity, smoking, hyperlipidemia and obstructive sleep apnea syndrome. Head MRI showed a diffuse-limited lesion in the right brainstem, including the abducens nucleus, adjacent MLF, and facial colliculus, extending to the ipsilateral medial lemniscus and corticospinal tract (Figure 4B). The clinical diagnosis was acute cerebral infarction. According to the head MRI, the lesion was involved in the tegmental and ventromedial pons. The clinical feature was eight-and-a-half syndrome plus the unilateral acroparalysis and hemihypesthesia, i.e., (), so it was named nine syndrome.
Mahale (19) reported two cases of nine syndrome in 2015:
Case 2: a 62-year-old female, acute onset and symptoms persisted, manifested as the left side of one-and-a-half syndrome + ipsilateral peripheral facial paralysis + ipsilateral limb ataxia (the left finger-nose test and heel-knee-tibia test were less stable and the body is dumped to the left when walking in a straight line). Cerebrospinal fluid protein was slightly elevated, mononuclear cells were normal, and anti-NMO antibody and CSF-IgG were negative. The head MRI-Flair showed a high signal of the tegmental and ventrolateral pons (Figure 4C,D), while the DWI/ADC was not diffusion-limited. She was diagnosed with multiple sclerosis.
Case 3: a 54-year-old male patient presented acute headache, the right side of one-and-a-half syndrome, the ipsilateral peripheral facial paralysis, the contralateral torso and limb ataxia (finger-nose test and heel-knee-tibia test were less stable with left dumping). Head CT and head MRI showed the right pons hemorrhage, and the lesions included the right pontine tegmentum and the right locus rubber of midbrain (Figure 4E,F).
Case 1 is the lesions in the ipsilateral tegmental and ventromedial pons. Case 2 is the multiple lesions in the ipsilateral pontine tegmentum with the ipsilateral ventrolateral medipeduncle. Case 3 is the bleeding lesions in the ipsilateral pontine tegmentum and the ipsilateral midbrain, therefore the lesions extended from the pontine tegmentum to the anteromedial, dorsolateral and above the pons. According to the scope of the lesion, this series of signs of eight-and-a-half syndrome + hemiparesis and/or hemihypesthesia, can also be expressed as eight-and-a-half syndrome + ipsilateral or contralateral ataxia, i.e., eight-and-a-half syndrome plus the semi-body symptoms equals nine syndrome (). The etiological factors to date are the cerebrovascular disease (cerebral infarction or hemorrhage) and demyelinating disease.
Thirteen-and-a-half syndrome
Allbon and La Hood (20) reported in 2016 that a patient with a lymphoproliferative disease after renal transplantation had a group of cranial nerve symptoms. A 50-year-old man suddenly presented the right one-and-a-half syndrome with the right facial paralysis, the right lagophthalmos with absent corneal sensation and significant punctate epithelial erosions on the right cornea, accompanied by right facial numbness and right limbs and torso ataxia symptoms. The contrast-enhanced head MRI showed a wide range of high signal in the right pontine tegmentum, right pedunculus cerebellaris medius, and right cerebellum (Figure 4G). After surgical resection of lung lesions, pathological manifestations showed lymphoproliferative diseases, so the diagnosis was central nervous system lymphoma.
Allbon called this case thirteen-and-a-half syndrome, deriving from the central nervous system lymphoma lesions. The lesions spread to the right pontine tegmentum, right lateral pterygopalatine trigeminal nucleus, and facial nucleus, resulting in eight-and-a-half syndrome, combined with right facial hypoesthesia and corneal ulcers. Allbon explained the corneal ulcer as a double result of seventh cranial nerve (neuroparalytic keratitis) and fifth cranial nerve (neurotrophic keratitis). Therefore, eight-and-a-half syndrome plus the ipsilateral fifth cranial nerve (trigeminal nerve) damaged symptoms, it is called thirteen-and-a-half syndrome ().
Fifteen-and-a-half syndrome
Bae and Song (21) reported in 2005 for the first time a patient with one-and-a-half syndrome and bilateral facial paralysis, namely fifteen-and-a-half syndrome (one-and-a-half syndrome + damaged bilateral seventh cranial nerve), i.e., (). The head MRI showed bilateral pontine tegmentum lesion, which might damage the bilateral abducens nucleus, MLF, and bilateral facial nerve (Figure 4H). The affected vessels should be the unilateral central pontine branch, which terminal branches supply the tegmentum of the bilateral pontine tegmentum (22). Although the etiology of one-and-a-half syndrome are numerous, such as cerebrovascular disease, demyelination, infection, etc., the current reported fifteen-and-a-half syndrome is caused by only vascular reason.
Sixteen-and-a-half syndrome
Cummins (23) reported a case in 2011 that a 78-year-old man presented acute onset of eight-and-a-half syndrome on the left side (one-and-a-half syndrome + left sided 7th cranial nerve), right hemiparalysis and left sided hearing loss (8th cranial nerve damaged). The brainstem auditory evoked potential testing showed abnormal after left ear stimulation. Therefore, the series of symptoms is named sixteen-and-a-half syndrome (). Head MRI with DWI revealed ischemic lesions are in the tegmental, the ventromedial, and the ventrolateral pons, which suggested the involved neural structures, such as the left-sided PPRF, abducens nucleus and the left-sided facial colliculus, the corticospinal tract in the ventromedial pons and the cochlear nucleus in ventrolateral pons (Figure 4I). In this case, no vascular examination was reported. It was speculated that it was related to the paracentral branch and the short spiral branch of the basilar artery.
Summary and perspectives
Here we reported a rare series of one-and-a-half syndrome and its spectrum disorders. We also described the clinical and pathological features of different syndromes, and summarized the naming basis, which is helpful to locate the lesion according to the clinical features. As we all know, abducens nucleus, facial nucleus, trigeminal nucleus and vestibular nucleus are located in the pontine. Facial nerve originates from facial nucleus and bypasses abducens nucleus, and eight-and-a-half syndrome comes into being to the seventh cranial nerve damage on the basis of one-and-a-half syndrome. Ascribe to the special neuroanatomy, the incidence of the eight-and-a-half syndrome is higher than the others. Motor nucleus of trigeminal nerve is located in the central pontine tegmental dorsolateral area, and sent out from the junction of the pons ventral and middle cerebellar peduncle. The vestibular nucleus is located at the deep part of the vestibule at the bottom of the fourth ventricle. These syndromes are produced by the different damaged neuron nucleus. Nine syndrome is eight-and-a-half syndrome plus the unilateral acroparalysis and hemihypesthesia. Eight-and-a-half syndrome plus the ipsilateral fifth cranial nerve (trigeminal nerve) forms the thirteen-and-a-half syndrome. One-and-a-half syndrome plus damaged bilateral seventh cranial nerve forms fifteen-and-a-half syndrome. One-and-a-half syndrome plus one sided 7th cranial nerve, hemiparalysis and one-sided hearing loss (8th cranial nerve damaged) forms sixteen-and-a-half syndrome. The incidence of these syndromes is smaller than that of the eight-and-a-half syndrome, especially the fifteen-and-a-half syndrome, perhaps because the nine syndrome, the thirteen-and-a-half syndrome and the sixteen-and-a-half syndrome are caused by unilateral lesion and are all on the basis of eight-and-a-half syndrome.
The common causes of these syndromes are cerebrovascular disease (cerebral infarction or hemorrhage), multiple sclerosis, demyelinating disease or encephalitis. The overwhelming majority of the causes are cerebrovascular disease, which may be caused by the local blood supply of the intracranial vessels and the highest incidence. While the fifteen-and-a-half syndrome is located in bilateral lesion. According to the existing reports, the cause of the syndrome is all cerebrovascular disease. Normally, the blood supply of one side of the pontine is derived from the long peripheral artery of the basilar artery, and the normal bilateral branches are symmetrical. In some patients, there is variation in pontine vessels, unilateral pontine paramedian artery supplies bilateral pontine tegmentum, so that when the vessel is blocked, bilateral dorsal infarction is formative. This may be the reason the fifteen-and-a-half syndrome is rare. It is summarized that when we encounter these syndromes, cerebrovascular disease should come first, then the multiple sclerosis. They are not difficult to diagnose combined with other clinical symptoms and brain magnetic resonance imaging.
Acknowledgements
Funding: Grant support from Key Project of Medical Science Research of Hebei Province, China (No. 20160569) is gratefully acknowledged.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Fisher CM. Some neuro-ophthalmological observations. J Neurol Neurosurg Psychiatry 1967;30:383-92. [Crossref] [PubMed]
- Chilla GS, Tan CH, Xu C, Poh CL. Diffusion weighted magnetic resonance imaging and its recent trend-a survey. Quant Imaging Med Surg 2015;5:407-22. [PubMed]
- Bae YJ, Kim JH, Choi BS, Jung C, Kim E. Brainstem pathways for horizontal eye movement: pathologic correlation with MR imaging. Radiographics 2013;33:47-59. [Crossref] [PubMed]
- Pierrot-Deseilligny C, Goasguen J, Chain F, Lapresle J. Pontine metastasis with dissociated bilateral horizontal gaze paralysis. J Neurol Neurosurg Psychiatry 1984;47:159-64. [Crossref] [PubMed]
- Cohen B, Komatsuzaki A. Eye movements induced by stimulation of the pontine reticular formation: evidence for integration in oculomotor pathways. Exp Neurol 1972;36:101-17. [Crossref] [PubMed]
- Martyn CN, Kean D. The one-and-a-half syndrome. Clinical correlation with a pontine lesion demonstrated by nuclear magnetic resonance imaging in a case of multiple sclerosis. Br J Ophthalmol 1988;72:515-7. [Crossref] [PubMed]
- Ettl A, Salomonowitz E. Visualization of the oculomotor cranial nerves by magnetic resonance imaging. Strabismus 2004;12:85-96. [Crossref] [PubMed]
- Wall M, Wray SH. The one-and-a-half syndrome--a unilateral disorder of the pontine tegmentum: a study of 20 cases and review of the literature. Neurology 1983;33:971-80. [Crossref] [PubMed]
- Frohman TC, Galetta S, Fox R, Solomon D, Straumann D, Filippi M, Zee D, Frohman EM. Pearls & Oy-sters: The medial longitudinal fasciculus in ocular motor physiology. Neurology 2008;70:e57-67. [Crossref] [PubMed]
- Striano S, Luciano R, Meo R, Bilo L, Orefice G, Grasso A. The physiopathology of supranuclear structures in oculomotor disorders. Acta Neurol (Napoli) 1990;12:151-71. [PubMed]
- Bolaños I, Lozano D, Cantú C. Internuclear ophthalmoplegia: causes and long-term follow-up in 65 patients. Acta Neurol Scand 2004;110:161-5. [Crossref] [PubMed]
- Ranjith MP, Divya R, Sahni A. Isolated one and a half syndrome: an atypical presentation of neurocysticercosis. Indian J Med Sci 2009;63:119-20. [Crossref] [PubMed]
- Menon V, Gogoi M, Saxena R, Singh S, Kumar A. Isolated "one and a half syndrome" with brainstem tuberculoma. Indian J Pediatr 2004;71:469-71. [Crossref] [PubMed]
- Raps EC, Galetta SL, King JT, Yachnis AT, Flamm ES. Isolated one-and-a-half syndrome with pontine cavernous angioma: successful surgical removal. J Clin Neuroophthalmol 1990;10:287-90. [PubMed]
- Hitchings L, Crum A, Troost BT. Isolated one-and-one-half syndrome from focal brainstem hypertensive hemorrhage: precise localization with MRI. Neurology 1988;38:1501-2. [Crossref] [PubMed]
- Eggenberger E. Eight-and-a-half syndrome: one-and-a-half syndrome plus cranial nerve VII palsy. J Neuroophthalmol 1998;18:114-6. [Crossref] [PubMed]
- Nandhagopal R, Krishnamoorthy SG. Neurological picture. Eight-and-a-half syndrome. J Neurol Neurosurg Psychiatry 2006;77:463. [Crossref] [PubMed]
- Rosini F, Pretegiani E, Guideri F, Cerase A, Rufa A. Eight and a half syndrome with hemiparesis and hemihypesthesia: the nine syndrome. J Stroke Cerebrovasc Dis 2013;22:e637-8. [Crossref] [PubMed]
- Mahale RR, Mehta A, John AA, Javali M, Abbas MM, Rangasetty S. "Nine" syndrome: A new neuro-ophthalmologic syndrome: Report of two cases. Ann Indian Acad Neurol 2015;18:335-7. [Crossref] [PubMed]
- Allbon DS, La Hood B. Thirteen-And-A-Half Syndrome. J Neuroophthalmol 2016;36:191-2. [Crossref] [PubMed]
- Bae JS, Song HK. One-and-a-half syndrome with facial diplegia: the 15 1/2 syndrome. J Neuroophthalmol 2005;25:52-3. [Crossref] [PubMed]
- Fisher CM. Neuroanatomic evidence to explain why bilateral internuclear ophthalmoplegia may result from occlusion of a unilateral pontine branch artery. J Neuroophthalmol 2004;24:39-41. [Crossref] [PubMed]
- Cummins G, O'Hare A, Dunne R, Connolly S, O'Rourke K, Lynch T. "Sixteen and a half": a novel pontine neuro-ophthalmological syndrome. J Neurol 2011;258:1347-8. [Crossref] [PubMed]


