Virtue Quadratic Male Sling for stress incontinence—surgical guide for placement and delayed revision
Introduction
Male stress urinary incontinence (SUI) is a subset of incontinence that occurs with an increase in intraabdominal pressure as seen with lifting, sneezing, coughing, or laughing (1). SUI is a common complaint in men who undergo surgical removal of the prostate, and symptoms can range from mild to severe. A review of the literature shows that the average post prostatectomy incontinence rate after 1 year is 16% (range 4–31%) (2), with approximately 6% of men choosing to undergo a surgical procedure to improve their leakage at a median time of 20 months post-surgery (3).
Urinary outcomes have a major impact on patient satisfaction after prostate surgery and are the strongest predictor for patient health related quality of life after radical prostatectomy (RP) (4). Only 56% of men report to be at their baseline urinary bother by 12 months after RP. Additionally distressing, SUI during sexual activity (termed “climacturia”), was found to affect 28–44% of men who were sexually active after RP (5). Men with persistent stress incontinence after prostatectomy with persistent bother are typically offered surgical treatment with either a male sling or artificial urinary sphincter (AUS).
The male sling is a less complicated procedure than the AUS, but is not typically recommended to patients with moderate to severe symptoms (6). However, slings are an attractive alternative to the AUS since there is no need for activation of the device, operative time is less without the concern for mechanical breakdown, erosion, or need for removal and replacement. When patients are counseled and given the choice between sling surgery and AUS, 92% choose the sling. Even when patients are recommended to have an AUS placed, 25% still choose a sling as first line therapy (7).
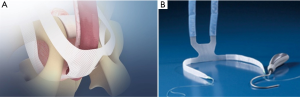
The Virtue Quadratic Male Sling is a four-arm polypropylene mesh sling with two transobturator (TO) arms and two prepubic arms. This sling was designed to provide both urethral elevation and prepubic compression (Figure 1). It has shown good outcomes for mild to severe SUI symptoms (8). An additional benefit of the Virtue sling is the ability to revise and tighten the sling should the mesh fail post-operatively. The cause of failure may be due to surgical technique, early resumption of physical activity causing mesh loosening, or history of radiation treatment (9). The aim of this paper is to describe our optimal technique performing the Virtue quadratic male sling as well as how to perform a sling revision if necessary.
Patient selection and preoperative counseling
A detailed history and focused physical exam is performed. This includes assessing the time of onset, duration, number of pads used, as well as any associated urinary voiding symptoms & neurologic complaints. It is important to assess the patient’s level of quality of life to appropriately counsel surgical options. Cystoscopy or urodynamic testing is performed if the initial evaluation warrants further exploration. Patients are counseled to wait at least 9 months post prostatectomy to ensure stability of their symptoms.
Preoperatively, we counsel patients about the risks regarding mesh placement (explaining this mesh is similar to hernia mesh) including, but not limited to infection, erosion, dissatisfaction, pain, numbness, retention, and limited effectiveness. Conveniently, the patient understands that should the sling fail to improve their symptoms adequately, a revision procedure can be performed before consideration of an AUS.
Contraindications for surgery include bleeding disorder or active urinary tract infection.
Surgical technique
The patient is placed under general anesthesia. LMA or ET tube is appropriate depending on anesthesiologist preference and patient’s comorbidities. Preoperative antibiotics are given using vancomycin and gentamycin.
Table 1 describes what we feel are the key tips and tricks when performing this procedure. We do not routinely perform cystoscopy on the day of the surgery. The patient is positioned in the dorsal lithotomy position with the buttocks slightly hanging off the table and the patient in slight Trendelenburg. Shaving includes the pubic, scrotal, and perineal hair.

Full table
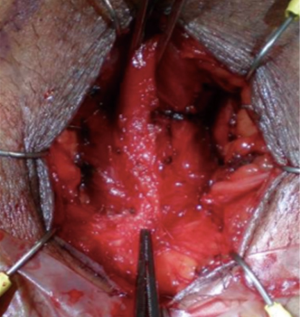
A 14F foley catheter is placed and a 0-0 silk is used to suture the scrotum up and out of the way of the perineum. A 4 cm vertical incision is made and cautery is used to dissect down to the bulbospongiosus muscle which is left intact. Lateral dissection is carried out until the descending pubic rami are identified bilaterally (Figure 2).
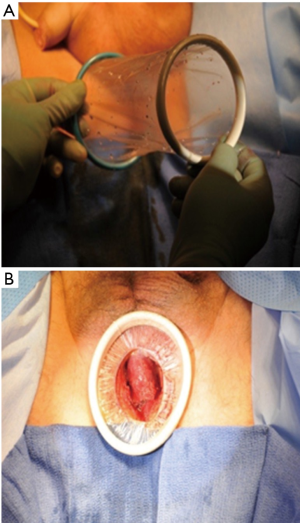
The Alexis retractor included within the kit provides excellent perineal exposure throughout the case. The green ring is folded and placed just under the skin incision. The assistant holds the green ring firmly in place while the surgeon flips the white ring inward until appropriate retraction is achieved (Figure 3).
The bulbospongiosus muscle is retracted superiorly and cautery is used to take down the perineal body attachments in a semi-lunar fashion to create approximately 2 cm mobilization where the central tendon is located (Figure 2).
The pre-pubic arms of the sling each have a blue sheath and are placed superiorly with heavy clamps at the end of each suture (Figure 4). An easy mnemonic to remember is that “blue (like the sky) lies north.”

Surgical pearl: use a headlamp! It helps significantly for adequate perineal visualization.
J hook passer
The J hook passer is used to pass through the TO space in an inside-out fashion. The benefit of the Virtue J hook is that it is designed to be used for both sides using the surgeon’s chosen dominant hand. The tip of the hook has a T- slot and an L- slot. We recommend using the T slot for smaller patients and the L- slot in more obese patients where exposure of the tip after the pass through is a challenge (Figure 5).

TO arm placement
The suture from the clear sheathed TO arm is placed within the T- hook so the knot of the suture sits securely within the hook.
The TO arms are placed using an inside-out technique with the J hook passer (Figure 6). The TO pass is guided by hugging around the lower, descending potion of the pubic rami approximately two finger breaths below the “apex” (the palpable point where the rami meet the symphysis). It is our experience that it is important to favor being lower than higher for successful passage of the hook. The exit point at the skin level of the passer is approximately 2 cm below and 1 cm lateral to the palpable, lower border of the adductor longus tendon. Once the passer is palpated in this spot a small stab incision is made and the knot of the suture is secured with a clamp and pulled through. The same steps are performed on the contralateral side.
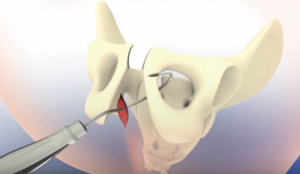
Surgical pearl: the tip of the passer will initially be almost parallel to the floor through the perineal incision. Then, when passing across the rami and through the obturator foramen, the angle of the handle should be at the 2 o’clock position on the patient’s left side, and at the 10 o’clock position on the patient’s right side. Advance the passer tip forward with the non-dominant hand through the perineal incision to negotiate around the rami. Remember, favor a lower entry point versus higher entry point.
Prepubic arm placement
Make two stab incisions 2 cm above the pubic symphysis and 1–3 finger breadths lateral to midline depending on the size of the patient. In smaller patients, we suggest using 3 finger breaths.
Pass the J hook passer, through the pubic stab incision, in front of the pubic bone (prepubic) not retropubic, and guide the needle out the perineal incision taking care to avoid the urethra in the midline. Attach the suture loop of the prepubic arm to the T-slot of the passer and pull up thru the incision. Repeat these steps on the contralateral side.
Surgical pearl: use a small Deaver retractor to allow a finger to be place within the space to help guide the tip of the passer lateral to the urethral complex.
Tensioning
Remove the plastic sheaths from each arm of the sling. Tension the TO arms laterally by simultaneously pulling on the ends of the sling to elevate the bulbous urethra. Tension the prepubic arms superiorly in the same manner to compress the bulbous urethra. We recommend placing heavy clamps at the skin level while watching the drip chamber when measuring the RLPP to adjust to the correct amount of tension on the sling.
Surgical pearl: use a small Deaver retractor for good exposure and slowly pull the prepubic arms until the dripping slows to a stop.
Retrograde leak point pressure
The RLPP is a critical element to the success of this procedure (Figure 7). We adopt the method as published by Comiter et al., choosing 60 cm water pressure as the target intraoperative pressure to achieve for tensioning (8).
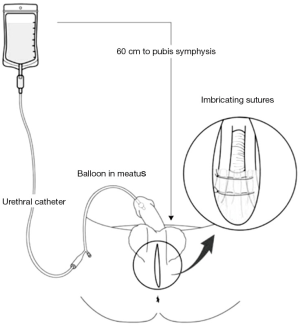
The RLPP procedure is as follows: the foley balloon is deflated and withdrawn until the tip is palpated within the fossa navicularis. Three milliliters of water is instilled into the foley to secure in place.
Sixty cm is measured from the top of a 1 L bag of saline down to the level of the pubic symphysis. Cystoscopy tubing is then attached to the catheter with a stopcock attachment to control the saline flow. Attention is drawn to the fluid drip chamber in order to visualize the dripping of the saline. Normally, with the incontinent patient under general anesthesia, the flow will be substantial when the stopcock is opened. The prepubic arms are pulled until the dripping in the chamber stops. It is at this exact tension of the sling when the dripping stops during this RLPP procedure that the sling itself must be fixed in order to achieve full continence.
Surgical pearl: use a heavy clamp for each prepubic arm of the mesh with tension against the skin to maintain that tension where the dripping stops within the drip chamber once 60 cm water pressure is achieved.
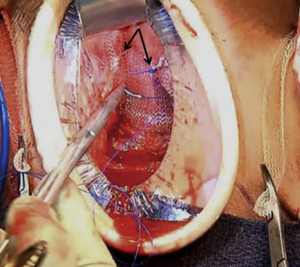
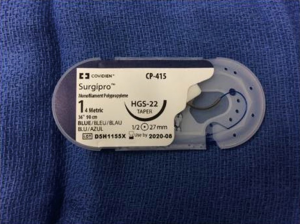
Sling fixation
The mesh is tensioned to the surface of the pubic bone with 2 figures of 8 sutures on each side for a total of 4 fixation sutures. The location of the fixation sutures should be at the junction between the body of the sling and the prepubic arms of the sling (Figure 8). We recommend using a #1 polypropylene suture (Covidien Surgipro #1 HGS-22 tapered needle) (Figure 9). Fixation sutures should be carefully placed making sure the initial figure of 8 throw is securely along the periosteum with the second throw incorporating just the mesh more medially from the first throw. Repeat on the contralateral side. Remove the heavy clamps from the prepubic arms to ensure the RLPP is still showing no dripping in the fluid chamber. We find that it typically takes 2 figure of 8 sutures on each side of the mesh to provide sufficient tension for the sling. For best results place one suture on each side, release the clamps, then place the second set.
Surgical pearl: test the anchoring ability of the fixation suture by pulling on the suture after the first throw; satisfactory anchoring occurs when minimal movement is felt when pulling the suture.
Alternative fixation technique: the same fixation sutures can be pre-placed in the periosteum on each side before the pre-pubic arms are pulled up. This can make periosteal suture placement easier and more secure. Make sure placement is secure by pulling up on the suture and seeing the patient move a little to confirm anchoring. The prepubic arm placement and RLPP procedure are then performed. The suture is then placed through the mesh at the junction of the body and arm and tied down securely at the exact tension when dripping stops during the RLPP procedure. If needed, an additional figure of 8 sutures can be placed through the mesh on each side. It should be mentioned that this alternative fixation technique is a single surgeon experience.
Closure
Replace the 14F foley catheter and ensure it passes past the sling. It may be snug and that is fine. If it cannot pass then cut a suture to release slight tension to confirm passage. Replace that suture once a foley is placed. Cut the prepubic arms at the skin level. For the TO arms, use a tonsil clamp through the perineal incision in the subcutaneous space and tunnel to the mesh at the exit site. Grasp the mesh arm with the end of the tonsil clamp and pull back through the new subcutaneous plane to the perineal incision. Trim the mesh inside the perineal incision. Repeat these steps on contralateral side.
It is important to place local anesthetic throughout the four male sling arms and along the path of the J-hook passer. Long acting liposomal bupivacaine (Exparel) has been helpful in improving post-operative pain control.
We complete a multi-layer closure of the perineal incision and the skin incisions using running 3-0 chromic and 3-0 vicryl undyed suture in a horizontal mattress fashion. Skin glue may be used for all the incisions, and should be all that is necessary for the pubic and TO stab incisions. A dressing of fluffs and scrotal support is placed prior to waking the patient up from anesthesia.
The Virtue Quadratic Male Sling is considered to be an outpatient surgery. Patients are sent home with ice pack and 1 week of Cephalexin as well as tramadol for pain control.
Surgical pearl: intraoperative liposomal bupivacaine (20 in 50 mL of Saline) gives 72 hours of pain relief. If not available, use 20 mL of ropivacaine with 8 mg dexamethasone for 36 hours relief (a technique popularized by orthopedic surgery).
Postoperative care
We remove the foley catheter in our clinic on post-operative day 1 and check the wound at 2 weeks. The patients are seen at a 6-week follow up to evaluate symptoms, and are instructed to refrain from lifting (“nothing heavier than a gallon of milk”), squatting or straining for 6–8 weeks. Patients who are too active post-operatively risk loosening the mesh or breaking a suture and may experience a dramatic change in their continent status.
Revision technique
For patients with residual bothersome leakage (who report improvement but not to expectations, or no improvement at all) at 9 months after initial placement of the quadratic sling, a second revision surgery can be performed to tighten the sling. This is an attractive option for patients who are hesitant to undergo AUS placement but are significantly bothered by their symptoms. There is no additional mesh placed, but rather, sutures are added to tighten this existing sling. Additionally, revising this sling does not limit the possibility of subsequently placing an AUS in the future should the patient’s incontinence become refractory to sling treatment.
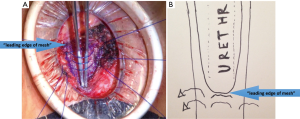
When revising the sling, initial steps to the procedure are the same as during de novo placement. A vertical perineal incision is made over the previous incision approximately 4 cm in length. The Alexis wound retractor size extra small (Applied Medical) is placed in a similar fashion as described above to provide adequate exposure. Dissection is carried down to the previously placed mesh. We have found that a cicatrix forms characterized as an in growth of fibrous tissue throughout the mesh of the sling adding bulk and fixation to this sling, a critical concept to recognize. An inverted triangle of mesh is dissected whereas the base of this triangle is the actual “leading edge” of the sling. This triangle is 3 cm in length on each side.
The RLPP is performed as described above (Figure 7), and is used to evaluate tightness of suture placement.
Imbricating #1 prolene plication sutures are placed superficially into the dense fibrous mesh and tied down (Figure 10). This imbrication is identical to a penile plication imbrication suture. Three sutures are used with the first one placed at the base of the inverted triangle of mesh. The tensioning is completed when the drip chamber has a slow leak or has stopped. At that point, the urethral catheter is replaced into the bladder.
Similarly to the initial surgery, the incision is closed in multiple layers using horizontal mattress sutures at the skin to provide a water tight closure.
Surgical pearl: the most important revision suture is the first suture on the “leading edge” of the base of the triangle and RLPP should be confirmed after throwing a surgeon’s knot down.
Discussion
The Virtue Quadratic Male Sling is a safe and efficacious treatment for post-prostatectomy incontinence. This can be revised in the event of refractory or worsening leakage over time. One study showed a 50% pad reduction in 79% of men, and cured symptoms in 46% of these patients after 12 months (8). Additionally, sling procedures have been shown in small studies to be an effective and viable treatment option for men with climacturia (10).
Common pitfalls to the initial sling placement include not performing RLPP, and incorrect placement of fixation sutures which if performed incorrectly can negatively affect outcomes. We believe RLPP provides an intraoperative assessment of adequate urethral closure pressure and is critical to ensure proper tensioning of the sling and thus efficacy.
Fixation sutures should be carefully placed at the junction between the body of the sling and the prepubic arms making sure the initial figure of 8 throw is securely along the periosteum with the second throw just grabbing the mesh. Failure to place these sutures through the periosteum may lead to loosening of the mesh and poor outcomes. The use of RLPP and fixation sutures have shown to dramatically improve sling outcomes as well as improve incontinence rates in men with moderate and severe leakage (8).
In our experience, when a sling fails to adequately improve symptoms, patients are given the option of having the sling tightened or having an AUS placed. Not surprisingly, the patient often chooses to have their sling tightened as a simpler procedure to avoid an AUS. This is an outpatient surgery that can potentially improve the leakage that day, as opposed to an AUS which is a mechanical device that takes 6 weeks before it can be activated. An important message to give to the patient at the first visit is that revision of the original sling provides another tool in the urologist’s armamentarium to help patients with distressing post prostatectomy incontinence. This confirms for the patient more added value in the choices they make.
In our patients who choose AUS after sling placement, we have found it useful to place the device while leaving the mesh intact. We believe the sling provides some benefit as a continence mechanism, and can act synergistically to improve overall continence. The surgery is performed either transverse scrotal or perineal with the cuff placed distal to the mesh. This provides a healthy portion of exposed urethra, without the need to remove any sling material.
Common post-operative complaints after sling placement include temporary numbness at the base of the scrotum and soreness in the perineum. We have had no instances of retention in the initial sling population, however revision has a retention rate of 5% that requires a later one week trial of void which is successful. We do not routinely prescribe stronger narcotics than tramadol, and find that long acting liposomal bupivacaine (Exparel) is helpful for prolonged post-operative pain control. We have aborted any bulking procedure for the incontinent male. We have not encountered any other significant complications beyond prolonged pain or numbness but none have required removal of the sling. There are no erosions (rare in of itself in the literature) nor, interestingly enough, infections with the sling over the last decade. In our experience, we have had no results of worsening incontinence after the sling surgery.
Conclusions
The Virtue Quadratic Male Sling with fixation and intraoperative RLPP monitoring is a safe and efficacious treatment for post-prostatectomy incontinence in patients with mild to even severe symptoms. The sling can be revised in the event of refractory or worsening leakage, and does not preclude placement of an AUS should one be needed. This surgical techniques paper describes a step by step approach to performing this efficacious procedure as well as surgical pearls to improve outcomes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn 2002;21:167-78. [Crossref] [PubMed]
- Ficarra V, Novara G, Rosen RC, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 2012;62:405-17. [Crossref] [PubMed]
- Kim PH, Pinheiro LC, Atoria CL, et al. Trends in the use of incontinence procedures after radical prostatectomy: a population based analysis. J Urol 2013;189:602-8. [Crossref] [PubMed]
- Loughlin KR, Prasad MM. Post-prostatectomy urinary incontinence: a confluence of 3 factors. J Urol 2010;183:871-7. [Crossref] [PubMed]
- O'Neil BB, Presson A, Gannon J, et al. Climacturia after definitive treatment of prostate cancer. J Urol 2014;191:159-63. [Crossref] [PubMed]
- Soljanik I, Becker AJ, Stief CG, et al. Repeat retrourethral transobturator sling in the management of recurrent postprostatectomy stress urinary incontinence after failed first male sling. Eur Urol 2010;58:767-72. [Crossref] [PubMed]
- Kumar A, Litt ER, Ballert KN, et al. Artificial urinary sphincter versus male sling for post-prostatectomy incontinence--what do patients choose? J Urol 2009;181:1231-5. [Crossref] [PubMed]
- Comiter CV, Rhee EY, Tu LM, et al. The virtue sling--a new quadratic sling for postprostatectomy incontinence--results of a multinational clinical trial. Urology 2014;84:433-8. [Crossref] [PubMed]
- Rhee EY. Quadratic Male Sling Revision. J Sex Med 2014;11:4-7. [Crossref]
- Christine B, Bella A. 121 Climacturia Following Radical Prostatectomy: The Time is Now to Query and Treat. J Sex Med 2017;14:e47. [Crossref]


