Abstract
5,10-Methylenetetrahydrofolate reductase (MTHFR) plays a key role in folate metabolism by channeling one-carbon units between nucleotide synthesis and methylation reactions. Severe enzyme deficiency leads to hyperhomocysteinemia and homocystinuria, with altered folate distribution and a phenotype that is characterized by damage to the nervous and vascular systems. Two frequent polymorphisms in the human MTHFR gene confer moderate functional impairment of MTHFR activity for homozygous mutant individuals. The C to T change at nucleotide position 677, whose functional consequences are dependent on folate status, has been extensively studied for its clinical consequences. A second polymorphism, an A to C change at nucleotide position 1298, is not as well characterized.
Still equivocal are associations between MTHFR polymorphisms and vascular arteriosclerotic or thrombotic disease. Neural tube defects and pregnancy complications appear to be linked to impaired MTHFR function. Colonic cancer and acute leukemia, however, appear to be less frequent in individuals homozygous for the 677T polymorphism. MTHFR polymorphisms influence the homocysteine-lowering effect of folates and could modify the pharmacodynamics of antifolates and many other drugs whose metabolism, biochemical effects, or target structures require methylation reactions. However, only preliminary evidence exists for gene-drug interactions.
This review summarizes the biochemical basis and clinical evidence for interactions between MTHFR polymorphisms and several disease entities, as well as potential interactions with drug therapies. Future investigations of MTHFR in disease should consider the influence of other variants of functionally-related genes as well as the medication regimen of the patients. Animal models for genetic deficiencies in folate metabolism will likely play a greater role in our understanding of folate-dependent disorders.


Similar content being viewed by others
Notes
11 International Union of Biochemistry, Enzyme Commission (EC) nomenclature.
References
Rothenberg SP, Iqbal P, da Costa M. Effect of folate compounds on the accumulation of methotrexate and the activity of dihydrofolate reductase in liver, kidney, and intestine of the mouse. J Pharm Exp Ther 1982; 223: 631–4
Heidelberger C. The nucleotides of fluorinated pyrimidines and their biological activities. Ciba Found Symp 1971; 2: 125–40
Chiang PK, Gordon RK, Tal J, et al. S-adenosylmethionine and methylation. FASEB J 1996; 10: 471–80
Daubner SC, Matthews RG. Purification and properties of methylenetetrahydrofolate reductase from pig liver. J Biol Chem 1982; 257: 140–5
Frosst P, Blom HJ, Milos R, et al. Identification of a candidate genetic risk factor for vascular disease: a common mutation in methylentetrahydrofolate reductase. Nat Genet 1995; 10: 111–3
Goyette P, Sumner JS, Milos R, et al. Human methylentetrahydrofolatereductase: isolation of cDNA, mapping and mutation identification. Nat Genet 1994; 7: 195–200
Guenther BD, Sheppard CA, Tran P, et al. The structure and properties of methylenetetrahydrofolate reductase from escherichia coli suggest how folate ameliorates human hyperhomocysteinemia. Nat Struct Biol 1999; 6: 359–65
Shan X, Wang L, Hoffmaster R, et al. Functional characterization of human methylenetetrahydrofolate reductase in Saccharomyces cerevisiae. J Biol Chem 1999; 274: 32613–18
Raymond RK, Kastanos EK, Appling DR. Saccharomyces cerevisiae expresses two genes encoding isozymes of methyleneterahydrofolate reductase. Arch Biochem Biophys 1999; 372: 300–8
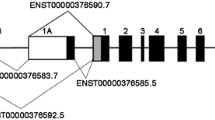
Goyette P, Pai A, Milos R, et al. Gene structure of human and mouse methylenetetrahydrofolate reductase (MTHFR). Mamm Genome 1998; 9: 652–6
Gaughan DJ, Barbaux S, Kluijtmans LAJ, et al. The human and mouse methylenetetrahydrofolate reductase (MTHFR) genes: genomic organization, mRNA structure and linkage to the CLCN6 gene. Gene 2000; 257: 279–89
Goyette P, Frosst P, Rosenblatt DS, et al. Seven novel mutations in the methylenetetrahydrofolate reductase gene and genotype/phenotype correlations in severe MTHFR deficiency. Am J Hum Genet 1995; 56: 1052–9
Goyette P, Christensen B, Rosenblatt DS, et al. Severe and mild mutations in cis for the methylenetetrahydrofolate reductase (MTHFR) gene, and description of 5 novel mutations in MTHFR. Am J Hum Genet 1996; 59: 1268–75
Kluijtmans LAJ, Wendel U, Stevens EMB, et al. Identification of four novel mutations in severe methylenetetrahydrofolate reductase deficiency. Eur J Hum Genet 1998; 6: 257–65
Sibani S, Christensen B, O’Ferrell E, et al. Characterization of six novel mutations in the methylenetetrahydrofolate reductase (MTHFR) gene in patients with homocystinuria. Hum Mutat 2000: 15: 280–7
Goyette P, Rozen R. The thermolabile variant 677C→T can further reduce activity when expressed in cis with severe mutations for human methylenetetrahydrofolate reductase. Hum Mutat 2000; 16: 132–8
Weisberg I, Tran P, Christensen B, et al. A second genetic polymorphism in methylenetetrahydrofolate reductase (MTHFR) associated with decreased enzyme activity. Mol Genet Met 1998; 64: 169–72
Kang SS, Wong PWK, Susmano A, et al. Thermolabile methylentetrahydrofolate reductase in patients with coronary artery disease. Am J Hum Genet 1991; 48: 536–45
Jacques PF, Bostom AG, Williams RR, et al. Relation between folate status, a common mutation in methylenetetrahydrofolate reductase, and plasma homocysteine concentrations. Circulation 1996; 93: 7–9
Gudnason V, Stansbie D, Scott J, et al. C677T (thermolabile alanine/valine) polymorphism in methylenetetrahydrofolate reductase (MTHFR): its frequency and impact on plasma homocysteine concentrations in different European populations. Atherosclerosis 1998; 136: 347–54
Botto LD, Yang Q. 5,10-methylenetetrahydrofolate reductase gene variants and congenital anomalies: a HuGe review. Am J Epidemiol 2000; 9: 862–77
Stevenson RE, Schwartz CE, Du YZ, et al. Differences in methylenetetrahydrofolate reductase genotype frequencies between whites and blacks. Am J Hum Genet 1997; 60: 230–3
Schneider JA, Rees DC, Liu YT, et al. Worldwide distribution of a common methylenetetrahydrofolate reductase mutation [letter]. Am J Hum Genet 1998; 62: 1258–60
Pepe G, Camacho Vanegas O, Giusti B, et al. Heterogeneity in world distribution of the thermolabile C677T mutation in 5,10-methylenetetrahydrofolate reductase [letter]. Am J Hum Genet 1998; 63: 917–20
Van der Put NMY, Gabreels F, Stevens EMB, et al. A second common mutation in the methylenetatrahydrofolate reductase gene: an additional risk factor for neural-tube defects? Am J Hum Genet 1998; 62: 1044–51
Meisel C, Cascorbi I, Gerloff T, et al. Identification of six methylenetetrahydrofolate reductase (MTHFR) genotypes resulting from common polymorphisms: impact on plasma homocysteine levels and development of coronary artery disease. Atherosclerosis 2001; 154: 651–8
Weisberg IS, Jacques PF, Selhub J, et al. The 1298A→C polymorphism in methylenetetrahydrofolate reductase(MTHFR): in vitro expression and association with homocysteine. Atherosclerosis 2001; 156: 409–15
Szczeklik A, Sanak M, Jankowski M, et al. Mutation A1298C of Methylenetetrahydrofolate reductase: risk for early coronary disease not associated with hyperhomocysteinemia. Am J Med Genet 2001; 101: 36–9
Hyland K, Smith I, Bottiglieri T, et al. Demyelination and decreased S-adenosylmethionine in 5,10-methylenetatrahydrofolate reductase deficiency. Neurology 1988; 38: 459–62
Surtees R, Leonard J, Austin S. Association of demyelination with deficiency of cerebrospinal fluid S-adenosylmethionine in inborn errors of methyl-transfer pathway. Lancet 1991; 338: 1550–4
Kishi T, Kawamura I, Harada Y, et al. Effect of betaine on S-adenosylmethionine levels in the cerebrospinal fluid in a patient with methylenetetrahydrofolate reductase deficiency and peripheral neuropathy. J Inherit Metab Dis 1994; 17: 560–5
Singer HS, Butler I, Rothenberg S, et al. Interrelationships among serum folate, CSF folate, neurotransmitters, and neuropsychiatric symptoms [abstract]. Neurology 1980; 30: 419
Narisawa K. Brain damage in the infantile type of 5,10-methylenetetrahydrofolate reductase deficiency. In: Botez MI, Reynolds EH, editors. Folic acid in neurology, psychiatry, and internal medicine. New York (NY): Raven Press, 1979: 391–400
Baumgartner ER, Stokstad ELR, Wick H, et al. Comparison of folic acid coenzyme distribution patterns in patients with methylenetetrahydrofolate reductase and methionine synthase deficiencies. Pediatr Res 1985; 19: 1288–92
Erbe RW. Inborn errors of folate metabolism. In: Blakley RL, Whitehead VM, editors. Folates and pterines. Vol 3. Nutritional, pharmacological and physiological aspects. New York (NY): Wiley, 1986: 413–65
Malinow MR. Homocyst(e)ine and arterial occlusive. J Intern Med 1994; 236: 603–17
Malinow MR, Nieto FJ, Kruger WD, et al. The effects of folic acid supplementation on plasma total homocysteine are modulated by multivitamin use and methylenetetrahydrofolate reductase genotype. Arterioscler Thromb Vasc Biol 1997; 17: 1157–62
Ward M, McNulty H, McPartlin J, et al. Plasma homocysteine, a risk factor for cardiovascular disease, is lowered by physiological doses of folic acid. Q J Med 1997; 90: 519–24
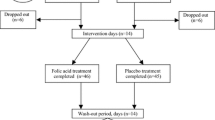
Sunder-Plassmann G, Födinger M, Buchmayer H, et al. Effect of high dose folic acid therapy on hyperhomocysteinemia in hemodialysis patients: results of the Vienna multicenter study. J Am Soc Nephrol 2000; 11: 1106–16
Hauser AC, Hagen W, Rehak PH, et al. Efficacy of folinic versus folic acid for the correction of hyperhomocysteinemia in hemodialysis patients. Am J Kidney Dis 2001; 37: 758–65
Hustad S, Ueland PM, Vollset SE, et al. Riboflavin as a determinant of plasma total homocysteine: effect modification by the methylenetetrahydrofolate reductase C677T polymorphism. Clin Chem 2000; 46: 1065–71
D’Angelo A, Coppola A, Madonna P, et al. The role of vitamin B12 in fasting hyperhomocysteinemia and its interaction with the homozygous C677T mutation of the methylenetetrahydrofolate reductase (MTHFR) gene. A case-control study of patients with early-onset thrombotic events. Thromb Haemost 2000; 83: 563–70
Harmon DL, Woodside JV, Yarnell JWG, et al. The common ‘thermolabile’ variant of methylenetetrahydrofolate reductase is a major determinant of mild hyperhomocysteinemia. Q J Med 1996; 89: 571–7
Bagley PJ, Selhub JA. Common mutation in the methylenetetrahydrofolate reductase gene is associated with an accumulation of formylated tetrahydrofolates in red blood cells. Proc Natl Acad Sci U S A 1998; 95: 13217–20
Lucock M, Daskalakis I, Briggs D, et al. Altered folate metabolism and disposition in mothers affected by a spina bifida pregnancy: Influence of 677C→T methylenetetrahydrofolate reductase and 2756A→G methionine synthase genotypes. Mol Genet Metab 2000; 70: 27–44
Stern LL, Mason LB, Selhub J, et al. Genomic DNA hypomethylation, a characteristic of most cancers, is present in peripheral leukocytes of individuals who are homozygous for the C677T polymorphism in the methylenetetrahydrofolate reductase gene. Cancer Epidemiol Biomarkers Prev 2000; 9: 849–53
Ueland PM, Refsum H, Beresford SAA, et al. The controversy over homocysteine and cardiovascular risk. Am J Clin Nutr 2000; 72: 324–32
Kluijtmans LAJ, van den Heuvel LP, Boers GHJ, et al. Molecular genetic analysis in mild hyperhomocysteinemia: a common mutation in the methylenetetrahydrofolate reductase gene is a genetic risk factor for cardiovascular disease. Am J Hum Genet 1996; 58: 35–41
Gallagher P, Meleady R, Shields D, et al. Homocysteine and risk of coronary heart disease: evidence for a common gene mutation. Circulation 1996; 94: 2154–8
Izumi M, Iwai N, Ohmichi N, et al. Molecular variant of 5,10-methylenetetrahydrofolate rductase is a risk factor for ischemic heart disease in the Japanese population. Atherosclerosis 1996; 121: 293–4
Morita H, Taguchi JI, Kurihara H, et al. Genetic polymorphism of 5,10-methylenetetrahydrofolate reductase (MTHFR) as a risk factor for coronary artery disease. Circulation 1997; 95: 2032–6
Inbal A, Freimark D, Modan B, et al. Synergistic effects of prothrombotic polymorphisms and atherogenic factors on the risk of myocardial infarction in young males. Blood 1999; 93: 2186–90
Gardemann A, Weidemann H, Philipp M, et al. The TT genotype of the methylenetetrahydrofolate reductase C677T polymorphism is associated with the extent of coronary athersclerosis in patients at high risk for coronary artery disease. Eur Heart J 1999; 20: 584–92
Morita H, Kurihara H, Tsubaki S, et al. Methylenetetrahydrofolate reductase gene polymorphism and ischemic stroke in Japanese. Arterioscler Thromb Vasc Biol 1998; 18: 1465–9
Margaglione M, D’Andrea G, D’Addedda M, et al. The methylenetetrahydrofolate reductase TT677 genotype is associated with venous thrombosis independently of the coexistence of the FV Leiden and the prothrombin A20210 mutation. Thromb Haemost 1998; 79: 907–11
Cattaneo M, Tsai MY, Bucciarelli P, et al. A common mutation in the methylenetetrahydrofolate reductase gene (C677T) increases the risk for deep-vein thrombosis in patients with mutant factor V (factor V: Q506). Arterioscler Thromb Vasc Biol 1997; 17: 1662–6
Arruda VR, von Zuben PM, Chiaparini LC, et al. The mutation Ala677-Val in the methylenetetrahydrofolate reductase gene: a risk factor for arterial disease and venous thrombosis. Thromb Haemost 1997; 77: 818–21
Salomon O, Moisseiev J, Rosenberg N, et al. Analysis of genetic polymorphisms related to thrombosis and other risk factors in patients with retinal vein occlusion. Blood Coag Fibrinolysis 1998; 9: 617–22
Tonstad S, Refsum H, Ose L, et al. The C677T mutation in the methylenetetrahydrofolate reductase gene predisposes to hyperhomocysteinemia in children with familial hypercholesterolemia treated with choiestyramine. J Pediatr 1998; 132: 365–8
Robins AJ, Milewczyk BK, Booth EM, et al. Plasma amino acid abnormalities in chronic renal failure. Clin Chim Acta 1972; 42: 215–17
Bostom AG, Culleton BF. Hyperhomocysteinemia in chronic renal disease. J Am Soc Nephrol 1999; 10: 891–900
Födinger M, Mannhalter C, Wölfl G, et al. Mutation (677 C to T) in the methylenetetrahydrofolate reductase gene aggravates hyperhomocysteinemia in hemodialysis patients. Kidney Int 1997; 52: 517–23
Van Guldener C, Robinson K. Homocysteine and renal disease. Semin Thromb Hemost 2000; 26: 313–24
Kimura H, Gejyo F, Suzuki S, et al. A C677T mutation in the methylenetetrahydrofolate reductase gene modifies serum cysteine in dialysis patients. Am J Kidney Dis 2000; 36: 925–33
Kimura H, Gejyo F, Suzuki S, et al. The 677 methylenetatrahydrofolate reductase gene mutation in hemodialysis patients. J Am Soc Nephrol 2000; 11: 885–93
Liangos O, Kreutz R, Beige J, et al. Methylenetetrahydrofolate reductase gene C677T variant and kidney transplant survival. Nephrol Dial Transplant 1998; 13: 2351–4
Ma J, Stampfer MJ, Hennekens CH, et al. Methylenetetrahydrofolate reductase polymorphism, plasma folate, homocysteine, and risk of myocardial infarction in U. S. physicians. Circulation 1996; 94: 2410–16
Kluijtmans LAJ, Kastelein JJ, Lindemans J, et al. Thermolabile methylenetetrahydrofolate reductase in coronary artery disease. Circulation 1997; 96: 2573–7
Markus HS, Ali N, Swaminathan R, et al. A common polymorphism in the methylenetetrahydrofolate reductase gene, homocysteine, and ischcmic cere-brovascular disease. Stroke 1997; 28: 1739–43
Kluijtmans LA, den Heijer M, Reitsma PH, et al. Thermolabile methylenetetrahydrofolate reductase and factor V Leiden in the risk of deep-vein thrombosis. Thromb Hemost 1998; 79: 254–8
Brattström L, Wilcken DEL, Ohrvik J, et al. Common methylenetetrahydrofolate reductase gene mutation leads to hyperhomocysteinemia but not to vascular disease: the results of a meta-analysis. Circulation 1998; 98: 2520–6
Brattström L, Wilcken DEL. Homocysteine and cardiovascular disease: cause or effect? Am J Clin Nutr 2000; 72: 315–23
Fletcher O, Kessling AM. MTHFR: association with arteriosclerotic vascular disease? Hum Genet 1998; 103: 11–21
Salomon O, Steinberg DM, Zivelin A, et al. Single and combined prothrombotic factors in patients with idiopathic venous thromboembolism: prevalence and risk assessment. Arterioscler Thromb Vasc Biol 1999; 19: 511–18
Tosetto A, Rodeghiero F, Martinelli I, et al. Additional genetic risk factors for venous thromboembolism in carriers of the factor V Leiden mutation. Br J Haematol 1998; 103: 871–6
Cattaneo M, Chantarangkul V, Taioli E, et al. The G20210A mutation of the prothrombin gene in patients with previous first episodes of deep-vein thrombosis: prevalence and association with factor V G1691A, methylenetetrahydrofolate reductase C677T and plasma prothrombin levels. Thromb Res 1999; 93: 1–8
Brown K, Luddington R, Baglin T. Effect of the MTHFR C677T variant on risk of venous thromboembolism: interactions with factor V Leiden and prothrombin (F2G20210A) mutations. Br J Haematol 1998; 103: 42–4
Cumming AM, Olujohungbe A, Keeny S, et al. The methylenetetrahydrofolate reductase gene C677T polymorphism in patients with homozygous sickle cell disease and stroke. Br J Haematol 1999; 107: 569–71
Mager A, Lalezari S, Shohat T, et al. Methylenetetrahydrofolate reductase genotypes and early-onset coronary artery disease. Circulation 1999; 100: 2406–10
Eikelboom JW, Lonn E, Jr Genest J, et al. Homocyst(e)ine and cardiovascular disease: a critical review of the epidemiologic evidence. Ann Int Med 1999; 131: 363–75
Kim YI. Methylenetetrahydrofolate reductase polymorphisms, folate, and cancer risk: a paradigm of gene-nutrient interactions in carcinogenesis. Nutr Rev 2000; 58: 205–17
Potter JD. Colorectal Cancer: Molecules and populations. J Natl Cancer Inst 1999; 91: 916–32
Ma J, Stampfer MJ, Giovannucci E, et al. Methylenetetrahydrofolate reductase polymorphism, dietary interactions, and risk of colorectal cancer. Cancer Res 1997; 57: 1098–1102
Chen J, Giovannucci E, Kelsey K, et al. A methylenetetrahydrofolate reductase polymorphism and the risk of colorectal cancer. Cancer Res 1996; 56: 4862–4
Slattery ML, Potter JD, Samowitz W, et al. Methylenetetrahydrofolate reductase, diet, and risk of colon cancer. Cancer Epidemiol Biomarkers Prev 1999; 8: 513–18
Ulrich CM, Kampman E, Bigler J, et al. Lack of association between the C677T MTHFR polymorphism and colorectal hyperplastic polyps. Cancer Epidemiol Biomarkers Prev 2000; 9: 427–33
Chen J, Giovannucci E, Hankinson SE, et al. A prospective study of methylenetetrahydrofolate reductase and methionine synthase gene polymorphisms, and risk of colorectal adenoma. Carcinogenesis 1998; 19: 2129–32
Marugame T, Tsuji E, Inoue H, et al. Methylenetetrahydrofolate reductase polymorphism and risk of colorectal adenomas. Cancer Lett 2000; 151: 181–6
Ulrich CM, Kampman E, Bigler J, et al. Colorectal adenomas and the C677T MTHFR polymorphism: evidence for gene-environment interaction? Cancer Epidemiol Biomarkers Prev 1999; 8: 659–68
Gershoni-Baruch R, Dagan E, Israeli D, et al. Association of the C677T polymorphism in the MTHFR gene with breast and/or ovarian cancer risk in Jewish women. Eur J Cancer 2000; 36: 2313–16
Piyathilake CI, Macaluso M, Johanning GL, et al. Methylenetetrahydrofolate reductase (MTHFR) polymorphism increases the risk of cervical intraepithelial neoplasia. Anticancer Res 2000; 20: 1751–8
Esteller M, Garcia A, Martinez-Palones JM, et al. Germ line polymorphisms in cytochrome P450 1A1 (C4887 CYP P1A1) and methylenetetrahydrofolate reductase (MTHFR) genes and endometrial cancer susceptibility. Carcinogenesis 1997; 18: 2307–11
Skibola CF, Smith MT, Kane E, et al. Polymorphisms in the methylenetetrahydrofolate reductase gene are associated with susceptibility to acute leukemia in adults. Proc Natl Acad Sci USA 1999; 6: 12810–15
Wiemels JL, Smith RN, Taylor GM, et al. Methylenetetrahydrofolate reductase (MTHFR) polymorphisms and risk of molecularly defined subtypes of childhood acute leukemia. Proc Natl Acad Sci USA 2001; 98: 4004–9
Laird PW, Jackson-Grusby L, Fazeli A, et al. Suppression of intestinal neoplasia by DNA hypomethylation. Cell 1995; 81: 197–205
Chen Z, Karaplis AC, Ackerman SL, et al. Mice deficient in methylenetetrahydrofolate reductase exhibit hyperhomocysteinemia and decreased methylation capacity, with neuropathology and aortic lipid deposition. Hum Mol Genet 2001; 10: 433–43
Kamiya H, Kawakami K, Miyanaga T, et al. A methylenetetrahydrofolate reductase polymorphism is associated with expression of p 16 in human lung cancer. Oncol Rep 1998; 5: 911–14
Czeizel AE, Dudas I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med 1992; 327: 1832–5
MRC Vitamin Study Research Group. Prevention of neural-tube defects: results of the Medical Research Council vitamin study. Lancet 1991; 338: 131–7
Steegers-Theunissen RPM, Boers GHJ, Trijbels FJM, et al. Maternal hyperhomocysteinemia: a risk factor for neural-tube defects? Metabolism 1994; 43: 1475–80
Mills JL, McPartlin JM, Kirke PN, et al. Homocysteine metabolism in pregnancies complicated by neural-tube defects. Lancet 1995; 345: 149–51
Barber R, Shalat S, Hendricks K, et al. Investigation of folate pathway gene polyorphisms and the incidence of neural tube defects in a Texas-Hispanic population. Mol Genet Metab 2000; 70: 45–52
Van der Put NMJ, Steegers-Theunissen RPM, Frosst P, et al. Mutated methylenetetrahydrofolate reductase as a risk factor for spina bifida. Lancet 1995; 346: 1070–1
Van der Put NMJ, Eskes TKAB, Blom HJ. Is a common 677C→T mutation in the methylenetetrahydrofolate reductase gene a risk factor for neural tube defects? A meta-analysis. Q J Med 1997; 90: 111–15
Christensen B, Arbour L, Tran P, et al. Genetic polymorphisms in methylenetetrahydrofolate reductase and methionine synthase, folate levels in red blood cells, and risk of neural tube defects. Amer J Med Genet 1999; 84: 151–7
Molloy AM, Mills JL, Kirke PN, et al. Low blood folates in NTD pregnancies are only partly explained by thermolabile 5,10-methylenetatrahydrofolate reductase: low folate status alone may be the critical factor. Am J Med Genet 1998; 78: 155–9
Lanoue L, Rozen R, Sulik KK. Antisense inhibition of methylenetetrahydrofolate reductase results in neural tube defects in cultured mouse embryos [abstract]. FASEB J 1997; 11: 2414
Hansen DK, Barbee SA, Grafton TF, et al. Antitsense modulation of 5,10-methylenetatrahydrofolate reductase expression produces neural-tube defects in mouse embryos. Reprod Toxicol 2001; 15: 21–9
Hall J, Solehdin F. Folic acid for the prevention of congenital anomalies. Eur J Pediatr 1998; 157: 445–50
Botto LD, Mulinare J, Erickson JD. Occurrence of congenital heart defects in relation to maternal multivitamin use. Am J Epidemiol 2000; 151: 878–84
Shaw GM, Rozen R, Finnell RH, et al. Infant C677T mutation inMTHFR, maternal periconceptional vitamin use, and cleft lip. Am J Med Genet 1998; 80: 196–8
Mills JL, Kirke PN, Molloy AM, et al. Methylenetetrahydrofolate reductase thermolabile variant and oral clefts. Am J Med Genet 1999; 86: 71–4
Martinelli M, Scapoli L, Pezzetti F, et al. C677T variant form at the MTHFR gene and CL/P: a risk factor for mothers? Am J Med Genet 2001; 98: 357–60
James SJ, Pogribna M, Pogribny IP, et al. Abnormal folate metabolism and mutation in the methylenetetrahydrofolate reductase gene may be maternal risk factors for Down syndrome. Am J Clin Nutr 1999; 70: 495–501
Hobbs CA, Sherman SL, Yi P, et al. Polymorphisms in genes involved in folate metabolism as maternal risk factors for Down syndrome. Am J Hum Genet 2000; 67: 623–30
Dean JC, Morre SJ, Osborne A, et al. Fetal anticonvulsant syndrome and mutation in the maternal MTHFR gene. Clin Genet 1999; 56: 216–20
Nelen WL, Blom HJ, Steegers EA, et al. Hyperhomocysteinemia and recurrent early pregnancy loss: a meta-analysis. Fertil Steril 2000; 74: 1196–9
Goddijn-Wessel TAW, Wouters MGAJ, van der Molen EF, et al. Hyperhomocysteinemia: a risk factor for placental abruption or infarction. Eur J Obstet Gynec Reprod Biol 1996; 66: 23–9
Ray JG, Laskin CA. Folic acid and homocyst(e)ine metabolism defects and the risk of placental abruption, pre-eclampsia, and spontaneous pregnancy loss: a systematic review. Placenta 1999; 20: 519–29
Zusterzeel PL, Visser W, Blom HJ, et al. Methylenetetrahydrofolate reductase polymorphisms in preeclampsia and the HELLP syndrome. Hypertens Pregnancy 2000; 19: 99–307
Grandone E, Margaglione M, Colaizzo D, et al. Factor V Leiden, C>T MTHFR polymorphism and genetic susceptibility to preeclampsia. Thromb Haemost. 1997; 77: 1052–4
Kupferminc MJ, Eldor A, Steinman N, et al. Increased frequency of genetic thrombophilia in women with complications of pregnancy. N Engl J Med 1999; 340: 9–13
Brenner B, Sarig G, Weiner Z. Thrombophilic polymorphisms are common in women with fetal loss without apparent cause. Thromb Haemost 1999; 82: 6–9
Rigo Jr J, Nagy B, Fintor L, et al. Maternal and neonatal outcome of preeclamptic pregnancies: the potential roles of factor V Leiden mutation and 5,10-methylenetetrahydrofolate reductase. Hypertens Pregnancy 2000; 19: 163–72
Foka ZJ, Lambropoulos AF, Saravelos H, et al. Factor V Leiden and prothrombin G20210A mutations, but not methylenetetrahydrofolate reductase C677T, are associated with recurrent miscarriages. Hum Reprod 2000; 15: 458–62
Muñoz-Moran E, Dieguez-Lucena JL, Fernandez-Areas N, et al. Genetic selection and folate intake during pregnancy. Lancet 1998; 352: 1120–1
Rozen R, Fraser FC, Shaw G. Decreased proportion of female newborn infants homozygous for the 677 C T mutation in methylenetetrahydrofolate reductase [letter]. Am J Med Genet 1999; 83: 142–3
Bentivoglio G, Melica F, Cristoforoni P. Folinic acid in the treatment of human male infertility. Fertil Steril 1993; 60: 698–701
Bezold G, Lange M, Peter RU. Homozygous methylenetetrahydrofolate reductase C677T mutation and male infertility [letter]. N Engl J Med 2001; 344: 1172–3
Bottiglieri T. Folate, vitamin B12, and neuropsychiatric disorders. Nutr Rev 1996; 54: 382–90
Wuerthele SE, Yasuda RP, Freed WJ, et al. The effect of local application of homocysteine on neuronal activity in the central nervous system of the rat. Life Sci 1982; 31: 2683–91
Flott-Rahmel B, Schumann M, Schluff P, et al. Homocysteic and sulphocystyeinic acid exhibit excitotoxicity in organotypic cultures from rat brain. Eur J Pediatr 1997; 157Suppl. 2: SI 12–17
Bottiglieri T, Hyland K, Reynolds EH. The clinical potential of ademetionine (Sadenosylmethionine) in neurological disorders. Drugs 1994; 48: 137–52
Evers S, Koch HG, Husstedt IW. Plasma homocysteine levels in primary headache. In: Olsen J, Edvinsson L, editors. Headache pathogenesis: monoamine, neu-ropeptides, purines, and nitric oxide. Philadelphia (PA): Lippincott-Raven Publishers, 1997: 215–18
Kowa H, Yasui K, Takeshima T. The homozygous C677T mutation in the methylenetetrahydrofolate reductase gene is a genetic risk factor for migraine. Am J Med Genet 2000; 96: 762–4
Selhub J, Bagley LC, Miller J, et al. B vitamins, homocysteine, and neurocognitive function in the elderly. Am J Clin Nutr 2000; 71 Suppl.: 614S–20
Bottiglieri T, Godfrey P, Flynn T, et al. Cerebrospinal fluid S-adenosylmethionine in depression and dementia: effects of treatment with parenteral and oral S-adenosylmethionine. J Neurol Neurosurg Psychiatry 1990; 53: 1096–8
Morrison, LD, Smith DD, Kish SJ. Brain S-adenosylmethionine levels are severely decreased in Alzheimer’s disease. J Neurochem 1996; 67: 1328–31
Clarke R, Smith AD, Jobst KA, et al. Folate, vitamin B12, and serum total homocysteine in confirmed Alzheimer’s disease. Arch Neurol 1998; 55: 1449–55
Tabet N, Mantle D, Orrell M. Free radicals as mediators of toxicity in Alzheimer’s disease: a review and hypothesis. Adverse Drug React Toxicol Rev 2000; 19: 127–52
Gusseklo J, Heijmans BT, Slagboom PE, et al. Thermolabile methylenetetrahydrofolate reductase gene and the risk of cognitive impairment in those over 85. J Neurol Neurosurg Psychiatry 1999; 67: 535–8
Yoo J-H, Choi G-D, Kang S-S. Pathogenicity of thermolabile methylenetetrahydrofolate reductase for vascular dementia. Arterioscler Thromb Vasc Biol 2000; 20: 1921–5
Bottiglieri T, Laundy M, Crellin R, et al. Homocysteine, folate, methylation, and monoamine metabolism in depression. J Neurol Neurosurg Psychiatry 2000; 69: 228–32
Arinami T, Yamada N, Yamakawa-Kobayashi K, et al. Methylenetetrahydrofolate reductase variant and schizophrenia/depression. Am J Med Genet 1997; 74: 526–8
Regland B, Johansson BV, Grenfeldt B, et al. Homocysteinemia is a common feature of schizophrenia. J Neural Transm 1995; 100: 165–9
Sargent T, Kusubov N, Taylor SE, et al. Tracer kinetic evidence for abnormal methyl metabolism in schizophrenia. Biol Psychiatr 1992; 32: 1078–90
Regland B, Germgard T, Gottfries CG, et al. Homozygous thermolabile methylenetetrahydrofolate reductase in schizophrenia-like psychosis. J Neural Transm 1997; 104: 931–41
Joober R, Benkelfat C, Lal S, et al. Association between the methylenetetrahydrofolate reductase 677C→T missense mutation and schizophrenia. Mol Psychiatry 2000; 5: 323–6
Weinberger DR. Schizophrenia: from neuropathology to neurodevelopment. Lancet 1995; 346: 552–7
Evans WE, Relling MV. Pharmacogenomics: translating functional genomics into rational therapeutics. Science 1999; 286: 487–91
Jackson RC. Biological effects of folic acid antagonists with antineoplastic activity. Pharmacol Ther 1984; 25: 61–82
Refsum H, Ueland PM, Kvinnsland S. Acute and long-term effects of high-dose methotrexate treatment on homocysteine in plasma and urine. Cancer Res 1986; 46: 5385–91
Refsum H, Heiland S, Ueland PM. Fasting plasma homocysteine as a sensitive parameter of antifolate effect: a study of psoriasis patients receiving low-dose methotrexate treatment. Clin Pharmacol Ther 1989; 46: 510–20
Santi DV, McHenry CS, Raines RT, et al. Kinetics and thermodynamics of the interaction of 5-fluoro-2′-deoxyuridylate with thymidylate synthase. Biochemistry 1987; 26: 8606–13
Geisler J, Geisler SB, Lonning PE, et al. Changes in folate status as determined by reduction in total plasma homocysteine levels during leucovorin modulation of 5-fluorouracil therapy in cancer patients. Clin Cancer Res 1998; 4: 2089–93
Toffoli G, Veronesi A, Boiocchi M, et al. MTHFR gene polymorphism and severe toxicity during adjuvant treatment of early breast cancer with cyclophosphamide, methotrexate, and fluorouracil (CMF) [letter]. Ann Oncol 2000; 11: 373–4
Franklin JL, Rosenberg HH. Impaired folic acid absorption in inflammatory bowel disease: effects of salicylazosulfapyridine (Azulfidine). Gastroenterology 1973; 64: 517–25
Haagsma CJ, Blom HJ, van Riel PLCM, et al. Influence of sulfosalazine, methotrexate, and the combination of both on plasma homocysteine concentrations in patients with rheumatoid arthritis. Ann Rheum Dis 1999; 58: 79–84
Lambie DG, Johnson RH. Drugs and folate metabolism. Drugs 1985; 30: 145–55
Carl GF. Effect of chronic valproic acid treatment on folate-dependent methyl biosynthesis in the rat. Neurochem Res 1986; 11: 671–85
Goggin T, Gough H, Bissessar A, et al. A comparative study of the relative effects of anticonvulsant drugs and dietary folate on the red cell folate status of patients with epilepsy. Q J Med 1987; 65: 911–19
Kishi T, Fujita N, Eguchi T, et al. Mechanism for reduction of serum folate by antiepileptic drugs during prolonged therapy. J Neurol Sci 1997; 145: 109–12
Hendel J, Dam M, Gram L, et al. The effects of carbamazepine and valproate on folate metabolism in man. Acta Scand 1984; 69: 226–31
Ono H, Sakamoto A, Eguchi T, et al. Plasma total homocysteine concentrations in epileptic patients taking anticonvulsants. Metabolism 1997; 46: 959–62
Schwaninger M, Ringleb P, Winter R, et al. Elevated plasma concentrations of homocysteine in antiepileptic drug treatment. Epilepsia 1999; 40: 345–50
Billings RE. Decreased hepatic methylenetetrahydrofolate reductase activity in mice after chronic phenytoin treatment. Mol Pharmacol 1984; 25: 459–66
Dieterich E, Steveling A, Lukas A, et al. Congenital anomalies in children of epileptic mothers and fathers. Neuropediatrics 1980; 11: 274–83
Yoo J-H, Hong SB. A common mutation in the methylenetetrahydrofolate reductase gene is a determinant of hyperhomocysteinemia in epileptic patients receiving anticonvulsants. Metabolism 1999; 8: 1047–51
Vilaseca MA, Monros E, Artuch R, et al. Anti-epileptic drug treatment in children: hyperhomocysteinemia, B-vitamins and the 677C T mutation of the methylenetetrahydrofolate reductase gene. Europ J Paediatr Neurol 2000; 4: 269–77
Wurtman RJ, Rose S, Matthyse S. L-3,4-dihydroxyphenylalanine effect on S-adenosylmethionine in brain. Science 1970; 169: 395–7
Surtees R, Hyland K. L-3,4-dihydroxyphenylalanine (levodopa) lowers central nervous system S-adenosylmethionine concentrations in humans. J Neurol Neurosur Psychiatry 1990; 53: 569–72
Allain P, Bouil AL, Cordillet E, et al. Sulfate and cysteine levels in the plasma of patients with Parkinson’s disease. Neurotoxicology 1995; 16: 527–30
Kuhn W, Roesbroek R, Blom H, et al. Elevated plasma levels of homocysteine in Parkinson’s disease. Eur J Neurol 1998; 40: 225–7
Müller T, Werne B, Fowler B, et al. Nigral endothelial dysfunction, homocysteine, and Parkinson’s disease. Lancet 1999; 354: 126–7
Pall HS, Surtees R, Sturman SG, et al. S-adenosylmethionine in cerebrospinal fluid in Parkinson’s disease (PD) [abstract]. Neurology 1992; 42: 283
Yasui K, Kowa H, Nakaso K. Plasma homocysteine and MTHFR C677T genotype in levodopa-treated patients with PD. Neurology 2000; 55: 437–40
Brattström LE, Hultberg BL, Hardebo JE. Folic acid responsive postmenopausal homocysteinemia. Metabolism 1985; 35: 1073–7
Wouters MG, Moorrees MT, van der Mooren MJ, et al. Plasma homocysteine and menopausal status. Eur J Clin Invest 1995; 25: 801–5
Van der Mooren MJ, Wouters MGAJ, Blom HJ, et al. Hormone replacement therapy may reduce high serum homocysteine in postmenopausal women. Eur J Clin Invest 1994; 24: 733–6
Mijatovic V, Kenemans P, Jakobs C, et al. A randomized controlled study of the effects of 17beta-estradiol-dydrogesterone on plasma homocysteine in postmenopausal women. Obstet Gynecol 1998; 91: 432–6
Brown CA, McKinney KQ, Young KB, et al. The C677T methylenetetrahydrofolate reductase polymorphism influences the homocysteine-lowering effect of hormone replacement therapy. Mol Genet Metab 1999; 67: 43–8
Dierkes J, Westphal S, Luley C. Serum homocysteine increases after therapy with fenofibrate or bezafibrate. Lancet 1999; 354: 219–20
Bissonnette R, Treacy E, Rozen R, et al. Fenofibrate raises plasma homocysteine levels in the fasted and fed states. Atherosclerosis 2001; 155: 455–62
Christensen B, Frosst P, Lussier-Cacan S, et al. Correlation of a common mutation in methylenetetrahydrofolate reductase (MTHFR) gene with plasma homocysteine in patients with premature coronary artery disease. Arterioscler Thromb Vasc Biol 1997; 17: 569–73
Arbour L, Christensen B, Delormier T, et al. Neural tube defects, folate metabolism, and dietary folate intake in a Northern Canadian Aboriginal Population. Community Genetics. In press
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schwahn, B., Rozen, R. Polymorphisms in the Methylenetetrahydrofolate Reductase Gene. Am J Pharmacogenomics 1, 189–201 (2001). https://doi.org/10.2165/00129785-200101030-00004
Published:
Issue Date:
DOI: https://doi.org/10.2165/00129785-200101030-00004