Abstract
Background: The Common Drug Review (CDR) was created to provide a single process to review the comparative clinical efficacy and cost effectiveness of new drugs, and then to make formulary listing recommendations to Canadian publicly funded drug benefit plans.
Objective: The objective was to conduct an in-depth analysis of Canadian Expert Drug Advisory Committee (CEDAC) recommendations to date, to explore predictors and possible explanatory factors associated with negative recommendations.
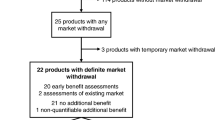
Methods: Final recommendations were identified from inception (September 2003) to 31 December 2009. Using only publicly available information, recommendations were analysed under the following categories: submission specifics, drug characteristics, clinical factors and economic factors. Descriptive analyses were conducted, followed by statistical analyses, to determine which factors independently predicted a ‘do not list’ (DNL) recommendation.
Results: The database consisted of 138 unique final recommendations. The overall DNL rate was 48%. Significant differences in DNL rates were observed between therapeutic areas, ranging from 0% for HIV antivirals up to 88% for analgesic drugs. In the univariate analysis, several factors were significantly associated with a DNL recommendation, including first-in-class drugs and use of clinical scales as an outcome. In the multivariate regression, four factors were significantly predictive of a DNL recommendation: clinical uncertainty (odds ratio [OR] 14), price higher than comparators (OR 9), request for reconsideration (OR 10) and price as the only economic evidence used (OR 18). Incremental cost-effectiveness thresholds were not predictive of recommendations. The hypothesis that economic factors did not impact recommendations when clinical factors were included first was supported by the analysis.
Conclusions: This analysis documented an evidence-driven process that simultaneously weighted multiple factors. Clinical uncertainty and price considerations, but not economic results, had a strong impact on the recommendations. Insufficiency of clinical evidence may have resulted from the gap in evidence available at the time of product launch and the absence of demonstrated benefits to support innovative drugs.






Similar content being viewed by others
Notes
Note that hospitals have a mandated responsibility for funding inpatient medications.
References
Organization for Economic Cooperation and Development. OECD health data 2011: how does Canada compare [online]. Available from URL: http://www.oecd.org/dataoecd/46/33/38979719.pdf [Accessed 2011 Dec 12]
Canadian Institute for Health Information. Drug expenditure in Canada: 1985 to 2009 [online]. Available from URL: http://secure.cihi.ca/cihiweb/products/dex_1985_to_2009_e.pdf [Accessed 2010 Dec 15]
IMS Health Canada. Pharma Focus 2014: leveraging knowledge for future success. Ottawa (ON): IMS, 2010 Jun
Anis AH, Guh D, Wang X. A dog’s breakfast: prescription drug coverage varies widely across Canada. Med Care 2001; 39: 315–26
Gregoire JP, MacNeil P, Skilton K, et al. Inter-provincial variation in government drug formularies. Can J Public Health 2001; 92: 307–12
MacDonald K, Potvin K. Interprovincial variation in access to publicly funded pharmaceuticals: a review based on the WHO anatomical therapeutic chemical classification system. Can Pharm J 2004; 137: 29–34
Menon D, Stafinski T, Stuart G, et al. Access to drugs in Canada. Does where you live matter? Can J Public Health 2005; 96: 454–8
Tierney M, Manns B, Canadian Expert Drug Advisory Committee. Optimizing the use of prescription drugs in Canada through the Common Drug Review. CMAJ 2008; 178 (4): 432–5
Morgan SG, McMahon M, Mitton C, et al. Centralized drug review processes in Australia, Canada, New Zealand, and the United Kingdom. Health Aff (Millwood) 2006; 25: 337–47
Canadian Agency for Drugs and Technologies in Health. Common Drug Review submission guidelines for manufacturers. Ottawa (ON): CADTH, 2011 Nov [online]. Available from URL: http://www.cadth.ca/media/cdr/process/CDR_Submission_Guidelines.pdf [Accessed 2011 Dec 12]
Canadian Agency for Drugs and Technologies in Health. Procedure for Common Drug Review. Ottawa (ON): CADTH, 2011 Nov [online]. Available from URL: http://www.cadth.ca/media/cdr/process/CDR_Procedure_e.pdf [Accessed 2011 Dec 12]
Canadian Agency for Drugs and Technologies in Health. CDR update: issue 67 [online]. Available from URL: http://www.cadth.ca/index.php/en/cdr/cdr-update/cdr-updateissue-67 [Accessed 2010 Dec 15]
Canadian Agency for Drugs and Technologies in Health. Guide: patient group input to the Common Drug Review. Ottawa (ON): CADTH, 2010 Sep [online]. Available from URL: http://www.cadth.ca/media/cdr/cdr-pdf/Guide-Patient_Group_Input_to_CDR_final_e.pdf [Accessed 2010 Dec 15]
Belanger D. Update from CADTH’s Common Drug Review program: Eyeforpharma 2nd annual market access Canada conference; 2010 Oct 4; Toronto (ON)
Canadian Agency for Drugs and Technologies in Health. CADTH announces expansion of Common Drug Review (CDR) program [media release]. 2007 Apr 12 [online]. Available from URL: http://www.cadth.ca/en/products/cdr/cdr-update/cdr-update-35 [Accessed 2010 Jun 25]
Ekos Research Associates Inc. Evaluation of the first year of operation for the Common Drug Review. Ottawa (ON): EKOS, 2005 Sep 27 [online]. Available from URL: http://www.cadth.ca/media/cdr/cdr_evaluation_firstyear_oct2005.pdf [Accessed 2010 Jun 25]
Standing Committee on Health. Prescription drugs part I–Common Drug Review: an F/P/T process. Ottawa (ON): House of Commons, 2007 Dec [online]. Available from URL: http://www.parl.gc.ca [Accessed 2010 Jun 25]
Canadian Agency for Drugs and Technologies in Health. CDR update–Issue 39: Common Drug Review expansion, clarification [online]. Available from URL: http://www.cadth.ca/en/products/cdr/cdr-update/cdr-update-39 [Accessed 2010 Jun 25]
Wyatt Health Management. The Rx&D International Report on Access to Medicines 2008/2009. Ottawa (ON): Canada’s Research-Based Pharmaceutical Companies, 2009 [online]. Available from URL: http://www.patientscomefirst.ca/inc/pdfs/Rx&D_InternationalReport_en.pdf [Accessed 2010 Dec 15]
Clement FM, Harris A, Li JJ, et al. Using effectiveness and cost-effectiveness to make drug coverage decisions: a comparison of Britain, Australia and Canada. JAMA 2009; 302: 1437–43
Lexchin J, Mintzes B. Medicine reimbursement recommendations in Canada, Australia, and Scotland. Am J Manag Care 2009; 14: 581–8
Gamble JM, Weir DL, Johnson JA, et al. Analysis of drug coverage before and after the implementation of Canada’s Common Drug Review. CMAJ 2011; 183: e1259–66
Canada’s Research-Based Pharmaceutical Companies. Presentation to the House of Commons Standing Committee on Health: notes for remarks by Russell Williams, President of Canada’s Research-Based Pharmaceutical Companies. 2007 Apr 16 [online]. Available from URL: http://www.canadapharma.org/en/media/statements/pdfs/Remarks_April_16_EN_WS_Final.pdf [Accessed 2010 Dec 15]
McMahon M, Morgan S, Mitton C. The Common Drug Review: a NICE start forCanada? Health Policy 2006; 77: 339–51
Laupacis A. Economic evaluations in the Canadian common drug review. Pharmacoeconomics 2006; 24 (11): 1157–62
Canadian Agency for Drugs and Technologies in Health. Common Drug Review documentation [online]. Available from URL: http://www.cadth.ca/en/products/cdr [Accessed 2010 Dec 15]
Clement F. A tri-nation comparison of pharmacoeconomic submissions: CDR, NICE and PBAC. CADTH Invitational Symposium; 2008 Apr 27-29; Edmonton (AB)
Rocchi A, Miller B. CEDAC recommendations: does costeffectiveness matter? CADTH Invitational Symposium; 2008 Apr 27-29; Edmonton (AB)
STATA Statistical Software [computer program]. Release 11. College Station (TX): StataCorp LP, 2009
Bender R, Lange S. Adjusting for multiple testing–when and how? J Clin Epidemiol 2001; 54: 343–9
Rocchi A, Miller E. CDR recommendations: does costeffectiveness matter? CADTH Invitational Symposium; 2008 Apr 27-29; Edmonton (AB)
Laupacis A, Feeny D, Detsky AS, et al. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ 1992; 146 (4): 473–81
Devlin N, Dakin H, Rice N, et al. NICE’s cost-effectiveness threshold revisited: new evidence on the influence of cost effectiveness and other factors on NICE decisions. 13th Annual ISPOR European Congress; 2010 Nov 6-9; Prague
Detsky AS, Laupacis A. Relevance of cost-effectiveness analysis to clinicians and policy makers. JAMA 2007; 298: 221–4
Ontario Ministry of Health and Long-Term Care. Transparent Drug System for Patients Act, 38:2 Bill 102 (2006) [online]. Available from URL: http://www.health.gov.on.ca/english/public/legislation/drugs/hu_drugsact.html [Accessed 2010 Dec 15]
Canadian Agency for Drugs and Technologies in Health. CEDAC final recommendation on reconsideration and reasons for recommendation: aliskiren [online]. Available from URL: http://www.cadth.ca/media/cdr/complete/cdr_complete_Rasilez_June-25-2008_e.pdf [Accessed 2010 Jun 28]
Ontario Ministry for Health and Long-Term Care. Committee to Evaluate Drugs recommendations and reasons: aliskiren. 2009 Oct [online]. Available from URL: http://www.health.gov.on.ca/english/providers/program/drugs/ced/pdf/aliskiren.pdf [Accessed 2010 Jun 28]
Gavura S, Rocchi A, Shum D, et al. Value versus values: it’s all about the evidence unless it’s cheaper. CADTH Symposium; 2010 Apr 18-20; Halifax (NS) [online]. Available from URL: http://www.cadth.ca/index.php/en/events/symposium-2010/program/concurrent-session-18 [Accessed 2010 Jun 28]
Canadian Agency for Drugs and Technologies in Health. CEDAC final recommendation: insulin detemir resubmission #2 [online]. Available from URL: http://www.cadth.ca/media/cdr/complete/cdr_complete_Levemir_Resubmission_Adults_August_20-2009.pdf [Accessed 2010 Aug 18]
Canadian Agency for Drugs and Technologies in Health. CEDAC final recommendation: hydromorphone hydrochloride [online]. Available from URL: http://www.cadth.ca/media/cdr/complete/cdr_complete_Jurnista_May-19-2010.pdf [Accessed 2010 Aug 18]
LeLorier J, Bell A, Bougher DJ, et al. Drug reimbursement policies in Canada: need for improved access to critical therapies. Ann Pharmacother 2008; 42 (6): 869–73
Clarke JTR. Is the current approach to reviewing new drugs condemning the victims of rare diseases to death? A call for a national orphan drug review policy. CMAJ 2006; 174: 189–90
Skinner BJ. Waiting for reimbursement of new medicines in Canada: it’s time for a rethink. Pharmacoeconomics 2008; 26 (8): 629–32
Drummond M, Evans B, LeLorier J, et al. Evidence and values: requirements for public reimbursement of drugs for rare diseases–a case study in oncology. Can J Clin Pharmacol 2009; 16: 273–81
Ontario Ministry of Health and Long-term Care. Drug system reforms: drugs for rare diseases [online]. Available from URL: http://www.health.gov.on.ca/en/public/programs/drugreforms/bill_102/patientaccess/rare_diseases.aspx [Accessed 2010 Dec 15]
Alberta Ministry of Health and Wellness. Rare Diseases Drug Program [online]. Available from URL: http://www.health.alberta.ca/AHCIP/drugs-rare-diseases.html [Accessed 2010 Dec 15]
Henry DA, Hill SR, Harris A. Drug prices and value for money: the Australian Pharmaceutical Benefits Scheme. JAMA 2005; 294 (20): 2630–2
Pearson SD, Rawlins MD. Quality, innovation, and value for money. NICE and the British National Health Service. JAMA 2005; 294 (20): 2618–22
Raftery JP. Paying for costly pharmaceuticals: regulation of new drugs in Australia, England and New Zealand. Med J Aust 2008; 188: 26–8
Harris AH, Hill SR, Chin G, et al. The role of value for money in public insurance coverage decisions for drugs in Australia: a retrospective analysis 1994-2004. Med Decis Making 2008; 28: 713–22
National Institute for Clinical Excellence. NICE announces measures on end of life medicines [media release]. 2008 Nov 5 [online]. Available from URL: http://www.nice.org.uk/media/6C4/6C/2008066MeasuresOnLifeMedicines.pdf [Accessed 2010 Jun 28]
Chim L, Kelly PJ, Salkeld G, et al. Are cancer drugs less likely to be recommended for listing by Pharmaceutical Benefits Advisory Committee in Australia? Pharmacoeconomics 2010; 28 (6): 463–75
Acknowledgements
This project was supported through an in-kind contribution from Axia Research and PATH Research Institute. An earlier interim analysis was partially funded by an unrestricted grant from Canada’s Research-Based Pharmaceutical Companies. This earlier funding was not associated with any role in the design and conduct of the current study, in the collection, management, analysis and interpretation of the data, or in the preparation, review or approval of the manuscript.
PATH (RG, RH) reported no conflicts of interest. Axia Research (AR, EM) provides consulting services to a number of Canadian pharmaceutical companies.
There were no other substantial contributors to this research.
AR and EM contributed to the study design, data abstraction, descriptive analysis and manuscript preparation. RH contributed to the statistical design, statistical analysis and manuscript preparation. RG contributed to the statistical design and manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rocchi, A., Miller, E., Hopkins, R.B. et al. Common Drug Review Recommendations. PharmacoEconomics 30, 229–246 (2012). https://doi.org/10.2165/11593030-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11593030-000000000-00000