The management of Helicobacter pylori infection and prevention and control of gastric cancer in China
- 1Department Of Gastroenterology, Digestive Disease Hospital, The First Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, China
- 2JiangXi Clinical Research Center for Gastroenterology, Nanchang, Jiangxi, China
Helicobacter pylori (H. pylori) infection, a type-1 carcinogen, was closely associated with gastric cancer (GC). Successfully eradicating H. pylori infection could reduce the incidence of GC. China was a country with high incidence of GC and high prevalence of H. pylori infection. Nearly half of worldwide GC new cases and deaths attributed to H. pylori infection occurred in China. H. pylori prevalence varied over time with the improvement of socioeconomic status and sanitary conditions. The knowledge of antibiotic resistance rate in time was important to guide the clinical choice of antibiotics use in the regimens. With the publication of five Chinese consensus reports on the management of H. pylori infection and the effort of public preach of H. pylori-related knowledge, the standardization of H. pylori diagnosis and treatment by clinicians was improved. Bismuth-containing quadruple therapy was widely applied in clinical practice of H. pylori eradication because of high efficacy and safety. High-dose Proton Pump Inhibitor-amoxicillin dual therapy or vonoprazan-amoxicillin dual therapy showed comparable efficacy and lower side effects than bismuth-containing quadruple therapy, which were the alternative choice. The diagnosis rate of early GC was low and distinguishing Chinese GC risk population for the further endoscopy screening was important. Efforts have been done to establish prediction models to stratify GC risk in the Chinese GC risk population. We reviewed the current situation of the management of H. pylori infection and prevention and control of GC in China here.
Introduction
In China, lung, colorectum and gastric cancer (GC) was the most common diagnosed cancer (Xia et al., 2022). The new case number and death number attributed to GC in China was 456, 124 and 390, 182 in 2018 (Bray et al., 2018). Meanwhile, the prevalence of Helicobacter pylori (H. pylori) infection was high in China, especially in area with high incidence of GC (Xie and Lu, 2015; Hooi et al., 2017). H. pylori infection was the main risk factor of GC (Malfertheiner et al., 2017), which was defined as type-1 carcinogen by the World Health Organization in 1994 and listed as the carcinogen by the 15th Report on carcinogens released by The U.S. Department of Health and Human Services in 2021. Nearly 90% of non-cardia GC were attributed to H. pylori infection, H. pylori-induced GC were estimated to be 810, 000 cases in 2018, which exceeded human papillomavirus-induced cervical cancer and hepatitis B virus-induced liver cancer, ranking the first among infection-attributable cancer (de Martel et al., 2020). China accounted for a third of worldwide cancer cases attributable to infection, especially H. pylori infection. We reviewed the current management of H. pylori infection and prevention and control of GC in China here.
Helicobacter pylori prevalence
H. pylori was a common infection worldwide, with different prevalence among different regions. H. pylori was mainly acquired in childhood. H. pylori gastritis was defined as an infectious disease by Kyoto global consensus report on Helicobacter pylori gastritis (Sugano et al., 2015), whose transmission route included oral-oral, fecal-oral and gastro-oral (Leja et al., 2016). As such, H. pylori was closely related with socioeconomic status and sanitary conditions (Goh et al., 2011). In 1990, China was a country with low human development index (value: 0.499), which gradually increased to 0.761 (defined as high human development index) in 2018. Hooi et al. (2017) included 26 studies (103, 128 subjects) conducted in China from 1983-2013 for pooled analysis of H. pylori prevalence, the results demonstrated that the overall infection rate of H. pylori was 55.82%, which indicated that estimated more than 700 million subjects in China were infected with H. pylori. However, the interval of included studies were 20 years, which might not reflect the current situation of H. pylori prevalence. Moreover, the studies published in Chinese might be missed in this analysis. A slightly decreased H. pylori infection rate was observed around the world (2000-2008: 46.8% vs. 2009-2016: 44.9%) (Zamani et al., 2018). Consistent with this trend, the prevalence of H. pylori infection was decreased over time in China from 1983 to 2013 (Nagy et al., 2016). The decreased prevalence of H. pylori infection was more obvious in urban areas in comparison with rural areas. The overall H. pylori prevalence was higher in rural areas (66%) than urban areas (47%), which might be attributed to the differences of socioeconomic status and sanitary conditions. The weighted mean prevalence of H. pylori infection increased from 48% among individuals aged 18-30 years to 59% among individuals aged 50-60 years.
A recent systematic review and meta-analysis focusing on H. pylori prevalence in China included 412 eligible studies (published in English or Chinese) with 1, 377, 349 subjects for pooled analysis of H. pylori prevalence (Ren et al., 2022). H. pylori infection rate was reported as 44.2% (range 35.8%-66.4%) in the mainland of China in this study, which indicated that estimated 589 million individuals were H. pylori positive. H. pylori prevalence were high (>60%) in developing regions (Xizang, Guizhou etc.) and low (<40%) in developed regions (Beijing, Chongqing, Tianjin etc.). The significantly decreased H. pylori prevalence was also observed (1983-1994: 58.3% vs. 2015-2019: 40%). The infection rate of H. pylori was 28.0% in children and adolescents and 46.1% in adults. The overall global infection rate of H. pylori in children was 32.3%. H. pylori prevalence was higher in older children (41.6% in 13-18 years old) than in younger children (33.9% in 7-12 years old and 26.0% in 0-6 years old). Lower economic status, more siblings or children, room sharing, no access to a sewage system, having a mother or a sibling or siblings infected with H. pylori, drinking unboiled or non-treated water and older age were significantly associated with paediatric H. pylori infection (Yuan et al., 2022). Considering the improvement of socioeconomic status and sanitary conditions, it was not surprised that H. pylori prevalence had been decreased during the past decades. However, high infection rate of H. pylori was reported in developing areas or regions with high incidence of GC. Eradicating H. pylori effectively is important for decreasing H. pylori prevalence. Moreover, forming good health habits are effective for prevention of H. pylori transmission. Zeng et al. (2015) reported that the oral recombinant H. pylori vaccine was effective, safe, and immunogenic for H. pylori-naive children, which could substantially reduce the incidence of H. pylori infection. Further H. pylori vaccine studies are still needed to explore the protection of the vaccine against H. pylori infection and H. pylori-associated diseases during a long period.
Helicobacter pylori recurrence
H. pylori recurrence remained a significant public health concern, which consisted of recrudescence or reinfection. Recrudescence was defined as reappearance of the original infection during short-term period (6 months), which was associated with the use of low efficient H. pylori regimen (Bell et al., 1993). Reinfection was defined as infection with a new strain of H. pylori occurred after 6 months, which required reexposure and was therefore more likely occurred in countries with high H. pylori prevalence and poor sanitation (Niv and Hazazi, 2008). We included 132 studies (53, 934 patient-years) for analyzing global H. pylori recurrence rate and explored the influence factors (Hu et al., 2017c). The global annual H. pylori recurrence, reinfection and recrudescence rate were 4.3%, 3.1% and 2.2%, respectively. Only three researches (Mitchell et al., 1998; Zhou et al., 2003; Zhou et al., 2017) had been conducted in China to explore the H. pylori recurrence rate until the year 2017. The pooled annual H. pylori recurrence rate was 2.1%, which was relatively low. The included subjects from the three studies were in developed regions (Beijing, Guangzhou, Jinan etc.), which might not reflect the total H. pylori recurrence rate in the mainland of China, especially in regions with low socioeconomic status and sanitary conditions. We further analyzed the associations between H. pylori recurrence rate and human development index (reflecting the socioeconomic status), H. pylori prevalence (reflecting sanitary conditions) and different periods. H. pylori recurrence rate was inversely related to the human development index and directly related to H. pylori prevalence, which might be explained by that subjects living in a country with low socioeconomic status and high H. pylori prevalence had more possibility of exposure of H. pylori. H. pylori recurrence rate remained relatively stable during three periods (1990s, 2000s and 2010s).
Xue et al. (2019) prospectively enrolled patients with successful eradication in developed regions (Beijing and Jinan) from 2013 to 2014 to conduct 13C-urea breath test at one year and 3 years after therapy. 743 patients finished the 1-year follow-up, 13 patients were H. pylori-positive, which indicated that the annual recurrence rate was 1.75%. 607 patients finished the 3-year follow-up, 28 patients recurred, which indicated that the 3-year recurrence rate was 4.61% and the annual recurrence rate was 1.5%. The invasive diagnoses or treatments, the level of income, and the hygiene standard of dining out place were the independent factors influencing H. pylori recurrence. A higher annual recurrence rate of H. pylori (4.75%) was reported in Jiangjin district, Chongqing (Zhou, 2020). Drinking and dining out were independent risk factors of H. pylori recurrence. Consistent with this study, Zhang et al. (2020a) also reported a high annual H. pylori recurrence rate (18.8%) among children. The follow-up of these two studies was short (1 year) and the enrolled patients were limited to one region. We conducted a large-scale multicenter, prospective open cohort, observational study to evaluate H. pylori recurrence rate during long-term follow-up (2012-2018, 7454.3 person-year) (Xie et al., 2020). 5, 193 subjects at 18 hospitals across 15 provinces were enrolled. The overall annual H. pylori recurrence, reinfection and recrudescence rate were 3.1%, 1.5% and 5.1%, respectively. Specific properties of ethnic groups, education level, family history or residence location was found to be at higher risk for H. pylori reinfection. H. pylori recurrence rate was relatively low in China, which could not be considered as the competing consideration to eradicate H. pylori and implement the “screen and treatment” strategy of H. pylori. Additionally, a recent systematic review and meta-analysis provided the sufficient evidences that whole family-based H. pylori treatment could increase eradication rate and reduce recurrence rate compared with single-infected patient treatment approach (Zhao et al., 2021). A family-based H. pylori prevention and eradication strategy would be an effective approach to prevent its intra-familial transmission (Ding et al., 2022).
Helicobacter pylori resistance
Antibiotic resistance of H. pylori was the important factor influencing the efficacy of H. pylori regimen (Hu et al., 2017a). For example, the efficacy of clarithromycin-containing regimens was shown to below 80% when the clarithromycin resistance rates were higher than 20%, which was then classified as unacceptable as the first-line treatment for H. pylori eradication (Graham et al., 2007). Clarithromycin resistance is due to mutations in the 23S rRNA gene. The 23S ribosomal RNA A2143G, A2142G, and A2142C mutations accounted for 80–90% of clarithromycin resistance. Similarly, levofloxacin resistance is mostly due to mutations at positions 87, 88, 91, 97 of gene gyrA. The occurrence of point mutations in the pbp 1A gene was the most common mechanism leading to moderate or low-level amoxicillin resistance. Resistance to tetracycline is mainly caused by point mutations in tet-1 in 16S rRNA genes. Metronidazole resistance is highly complex although rdxA mutations are highly predictive of metronidazole resistance (Peter et al., 2022). Furazolidone resistance is associated with Mutations in the H. pylori porD and oorD genes (Hu et al., 2017a). H. pylori resistance to common antibiotics (clarithromycin, metronidazole and levofloxacin) used in the regimen was quite serious (resistance rate >15%) in majority of World Health Organization Regions (Savoldi et al., 2018). In 2017, clarithromycin-resistant H. pylori was listed as antibiotic-resistant bacteria needing a high priority for antibiotic research and development of new antibiotics by World Health Organization (Tacconelli et al., 2018). In the Asia-Pacific region, the mean prevalence of primary H. pylori resistance was reported as 17% for clarithromycin, 44% for metronidazole, 18% for levofloxacin, 3% for amoxicillin, and 4% for tetracycline (Kuo et al., 2017). The resistance rate of clarithromycin and levofloxacin increased over time mainly after the year 2000. Primary H. pylori resistance to metronidazole remained stable but was above the alarming level from 1990 to 2016. Amoxicillin and tetracycline were considered to be susceptible antibiotics in this region. We also included 23 studies (published in English or Chinese) conducted in China focusing on primary antibiotic resistance of H. pylori to evaluate the overall pooled antibiotic resistance rate (Hu et al., 2017b). The results showed that the prevalence of H. pylori primary resistance to clarithromycin (28.9%), metronidazole (63.8%), and levofloxacin (28.0%) was high and increased over time. However, the resistance rates to amoxicillin (3.1%), tetracycline (3.9%), and furazolidone (1.7%) were low and stable over time.
Considering the differences of antibiotic resistance existed among different regions, we conducted a multi-region prospective 7-year study (2010-2016) to explore the characteristics of H. pylori resistance in China (Liu et al., 2018). H. pylori were successfully cultured from 1, 117 patients in 13 provinces or cities. An E-test was used to determine the minimum inhibitory concentrations of amoxicillin, metronidazole, clarithromycin, levofloxacin and tetracycline. The Kirby-Bauer disc diffusion method was used to determine the inhibition zone for furazolidone. The resistance rate of metronidazole, clarithromycin and levofloxacin was above the alarming level (>15%), as well as the dual antibiotic resistance rate (metronidazole+clarithromycin or metronidazole+ levofloxacin). The resistance rate of amoxicillin, tetracycline and furazolidone resistance was relatively low (<4%). The resistance rate of antibiotics was higher in subjects with age ≥40 years than subjects<40 years old, which might be explained by the exposure time of antibiotics were longer in the elder subjects. Additionally, the resistance rate of metronidazole, clarithromycin and amoxicillin were significantly different among different regions of China. Recently, A retrospective cross-sectional observational study was conducted by the China Center for H. pylori Molecular Medicine to investigate resistance of H. pylori strains to antibiotics from 2018 to 2020 across different regions of China. The results included 4, 242 H. pylori strains. Kirby-Bauer disk diffusion method was used to determine the phenotypic resistance to antibiotics. Overall, the primary antibiotic resistance rates of H. pylori for clarithromycin, levofloxacin and metronidazole were above the alarming level (>15%). The primary antibiotic resistance rates of H. pylori for amoxicillin, furazolidone and tetracycline were relatively low (<4%) except in Northwest China (Zhong et al., 2021). It should be noted that the primary resistance rate of H. pylori for antibiotics in specific region of China (e.g., Northwest China) showed an increasing trend. The selection of antibiotics in the regimens should base on the antibiotic resistance rate in local area. The previously treated adult group exhibited higher resistance rate of antibiotics (99.2% for metronidazole, 58.3% for clarithromycin and 52.3% for levofloxacin) compared with treatment-naive adult (Liu et al., 2019). As such, elevating the efficacy of first-line treatment for H. pylori is important, which could avoid the occurrence of secondary resistance. The situation of H. pylori resistance was serious in China. The combinations of susceptible antibiotics (amoxicillin+furazolidone or amoxicillin+tetracycline or tetracycline+furazolidone) were recommended by the Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection (Liu et al., 2018). Real-time monitoring of antibiotic resistance was also needed to further guide the selection of antibiotics used in the H. pylori regimens.
National survey regarding the management of Helicobacter pylori infection
In 2013, Fourth Chinese National Consensus Report on the management of Helicobacter pylori infection was published, including the indications, diagnosis and treatment of H. pylori. Proton Pump Inhibitor (PPI)-based triple therapy was not recommended as the first-line treatment of H. pylori infection because of its low efficacy (<80%). Bismuth-containing quadruple therapy (BQT) was recommended as the first-line and second-line regimen for eradicating H. pylori, the duration of H. pylori regimens increased from 7 days to 10 or 14 days (Liu et al., 2013). In 2018, Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection was published, which contained 6 aspects including H. pylori indications for eradication, diagnosis, treatment, H. pylori and GC, H. pylori infection in special populations, H. pylori and gastrointestinal microbiota (Liu et al., 2018). H. pylori gastritis is defined as an infectious disease, which was consistent with the recommendation reported in the Kyoto global consensus report on Helicobacter pylori gastritis. H. pylori infection confirmed was included in the H. pylori indications. Considering the serious situation of antibiotic resistance, BQT (recommended 7 regimens) was still recommended as the main empirical therapy for H. pylori eradication because of its high efficacy especially for H. pylori resistant strains. Compared to Fourth Chinese National Consensus Report, two regimens of BQT (PPI+bismuth+amoxicillin+metronidazole, PPI+bismuth+amoxicillin+tetracycline) were extended. In order to investigate the management of H. pylori infection by clinicians in China, the Chinese Study Group on H. pylori conducted an authoritative survey at 14th (2014) and 17th (2017) Congress of Gastroenterology China (Song et al., 2019b). A total of 4, 182 valid samples were obtained in this study. Majority of the clinicians were aware of H. pylori-related diseases (chronic gastritis, peptic ulcer, GC and gastric MALT lymphoma). However, less than 50% of clinicians were familiar with the associations between H. pylori infection and extra‐gastroduodenal diseases. Urea breath test were the preferred choice for detecting H. pylori infection by 80% of the clinicians. The demands for H. pylori detection by patients were increased mainly because of the increased awareness of H. pylori harmfulness by the publics and the preach of H. pylori consensus reports by the gastroenterologists. The proportion rate of quadruple therapy as the first-line treatment for H. pylori infection was higher (76%) in 2017 than that in 2014 (31%). The preferred antibiotic combinations were clarithromycin + amoxicillin, followed by amoxicillin + furazolidone. The combination of clarithromycin and metronidazole was used for the initial eradication by only 1% of the clinician because the dual resistance rate of clarithromycin and metronidazole was high (>15%). From this survey, we found that the management of H. pylori infection has been improved. However, the proportion rate of BQT was only 57% in 2017 and the frequency of resistant antibiotics (clarithromycin, metronidazole and levofloxacin) used in the regimens were still high.
After 4 years, the Chinese Study Group on H. pylori conducted a nationwide, multicenter, cross-sectional questionnaire survey again to investigate the current state of knowledge and practice of H. pylori infection management (Song et al., 2022). The proportion of BQT was high (88%) in the first-line treatment of H. pylori infection. Amoxicillin was the most preferred antibiotic (93.1%) used in the regimen. The preferred antibiotic combinations were still clarithromycin + amoxicillin, followed by amoxicillin+furazolidone. The proportion of regimens used for 14 days or 10 days were 83.3% and 13.5%, respectively. Compared to the survey in 2017, the treatment of H. pylori infection was more standard in 2021. The awareness of H. pylori prevention and treatment in the general Chinese population was also important, an internet-based survey was carried out in 2019 by the National Clinical Research Center for Digestive Diseases, which enrolled 3, 211 people and 546 physicians (Wu et al., 2020). The majority of the surveyed population (87.0%) and physicians (82.2%) supported a national H. pylori screening plan to prevent GC. However, the proportion of subjects who answered correctly to all questions about H. pylori’s infectivity, harmfulness and preventive measures were only 16%, 35% and 43.6%, respectively. More works on health education are needed because the general population in China has insufficient awareness of H. pylori.
Helicobacter pylori treatment
Bismuth-containing quadruple therapy
Standard PPI-based triple therapy was not recommended for H. pylori eradication because of its low efficiency. The monotherapy of bismuth could directly eradicate 20% H. pylori successfully. The addition of bismuth in triple therapy might improve the cure rate, mainly in strains with antibiotic resistance (Dore et al., 2016). Numerous studies have evaluated the efficacy of different antibiotic combinations in BQT in China, including clarithromycin and amoxicillin (Sun et al., 2010), amoxicillin and furazolidone (Xie et al., 2014), amoxicillin and metronidazole (Zhang et al., 2015), amoxicillin and tetracycline (Xie et al., 2018b), tetracycline and metronidazole (Liang et al., 2013), tetracycline and furazolidone (Liang et al., 2013). The efficacy of different antibiotic combinations in BQTs was good or fair in most studies, with the intention-to-treat (ITT) analysis showing an efficacy above 85% and the per protocol (PP) analysis showing an efficacy above 90%. As such, BQT was recommended as the first-line treatment of H. pylori infection by the Fifth Chinese National Consensus Report on the management of Helicobacter pylori infection (Liu et al., 2018). The duration of regimens should be 14 days, except evidences showed that regimens for 10 days achieved high efficacy. Susceptible antibiotics (amoxicillin, tetracycline and furazolidone) were the preferred choices in the regimens. We performed a national, multicenter, open-label, randomized controlled trial to evaluate the efficacy of the combination of susceptible antibiotic (amoxicillin and furazolidone) in BQT for eradicating H. pylori (Xie et al., 2018a). A high efficacy (94.7%) and low side effect (9.7%) were achieved by furazolidone-containing BQT for 10 days. Additionally, an observational study of furazolidone-containing BQT for H. pylori infection in real-world settings was conducted from 2015 to 2018, the eradication rate of furazolidone-containing BQT for 10 days or 14 days was 93.7% and 98.2%, respectively. Meanwhile, low side effect (<20%) was also observed for this regimen (Song et al., 2019a). Another combination of susceptible antibiotic (amoxicillin and tetracycline) in BQT for 10 days was showed to achieve 91.9% eradication rate as the first-line treatment for H. pylori infection, which was confirmed by multicenter, randomized, parallel-controlled clinical trial (Xie et al., 2018b).
Public attentions were paid to the alterations of gastric or intestinal microbiota induced by BQT because antibiotics and PPI used in the regimes might influence the host microbiota to some extent. We included ten asymptomatic young adults with H pylori-related gastritis treated with BQT for 14 days, 7 age-matched adults with H. pylori negative were served as healthy controls. Both fecal and gastric mucosa samples were collected for 16S rRNA gene sequencing at the timepoint of before eradication, after eradication and 6 months after the therapy. The results demonstrated that BQT can restore the diversity of gastric microbiota with enrichment of beneficial bacteria. The composition of gut microbiota after H. pylori eradication trends toward healthy status (He et al., 2019). The main drawback of BQT was the complex of drug administration, which might influence the compliance of the subjects, leading to the decreased efficacy of regimen. Enhanced educational interventions were effective way to improve the adherence among infected patients (Zha et al., 2022). WeChat is a social media platform widely used in China. Luo et al. (2020) found that H. pylori-infected subjects intervened with WeChat as a reminder tool during the treatment exhibited better disease-related knowledge, medication adherence, and eradication rates than that in the control group. The following research with more H. pylori-infected subjects enrolled further confirmed this finding (Ma et al., 2021). Compared to the conventional patient education (verbal education and a specifically designed printout with detailed instructions), the addition of WeChat-based patient-doctor interaction did not yield better results of efficacy or compliance (Lin et al., 2022). Selecting efficient antibiotic combinations in BQT should depend on the local H. pylori resistance. Enhanced patient education (conventional education or social media platform interactions) was also important for the success of H. pylori regimen.
High-dose PPI-amoxicillin dual therapy or vonoprazan-amoxicillin dual therapy
The role of PPI in H. pylori regimen was to maintain the gastric pH high enough for H. pylori to remain in the state of active replication where the organism becomes susceptible to amoxicillin (Graham and Fischbach, 2010) The eradication rate of H. pylori increased when the PPI dosage used in the regimen increased (Labenz, 2001). High-dose dual therapy (HDDT) was defined as the combination of amoxicillin and PPI in high dose for 14 days, which was evaluated for H. pylori eradication in recent years in China. Yang et al. (2019) firstly evaluated HDDT (amoxicillin 750mg q.i.d and esomeprazole 20mg q.i.d) as the first-line treatment of H. pylori. 91.1% eradication rate was achieved by HDDT in adherent infected subjects, which was non-inferior to BQT. The study conducted in Beijing with same regimen also reported the similar high efficacy for HDDT (Song et al., 2020). Changing the frequency of amoxicillin to 1000mg t.i.d in HDDT was also reported to achieve high efficacy (ITT: 89.4%, PP: 90.6%) (Guan et al., 2022). Increasing the dosage of esomeprazole to 40 mg t.i.d in HDDT was shown to achieve 91.7% eradication rate for ITT analysis and 95.7% in PP analysis (Tai et al., 2019). The addition of bismuth in HDDT only improved treatment efficacy among smoker (Yu et al., 2019). The eradication rate of HDDT was low when the duration was 10 days or the esomeprazole was given 20 mg t.i.d (Zhang et al., 2020b). The combination of amoxicillin and rabeprazole (10mg t.i.d) or Ilaprazole (5 mg bid) for 14 days was reported to be with high efficiency for eradicating H. pylori (Niu et al., 2022; Shao et al., 2022). Additionally, the combination of amoxicillin (1000mg t.i.d) and rabeprazole (10mg t.i.d) were also efficient for H. pylori eradication in elder infected subjects or those with multiple comorbidities (Gao et al., 2020). In China, the duration of HDDT should be 14 days. The optimized dosage of amoxicillin was 1000mg t.i.d or 750 mg q.i.d, the dosage of PPIs should be double (i.e. esomeprazole 20mg q.i.d or 40 mg b.i.d) to maintain the high gastric pH level. HDDT showed non-inferior efficacy and lowed side effects rate than BQT in adults or elder patients (Table 1), which was considered as an alternative first-line treatment for H. pylori infection in China. However, the influence of HDDT on the gut microbiota remained unclear and need to be explored in the future research.
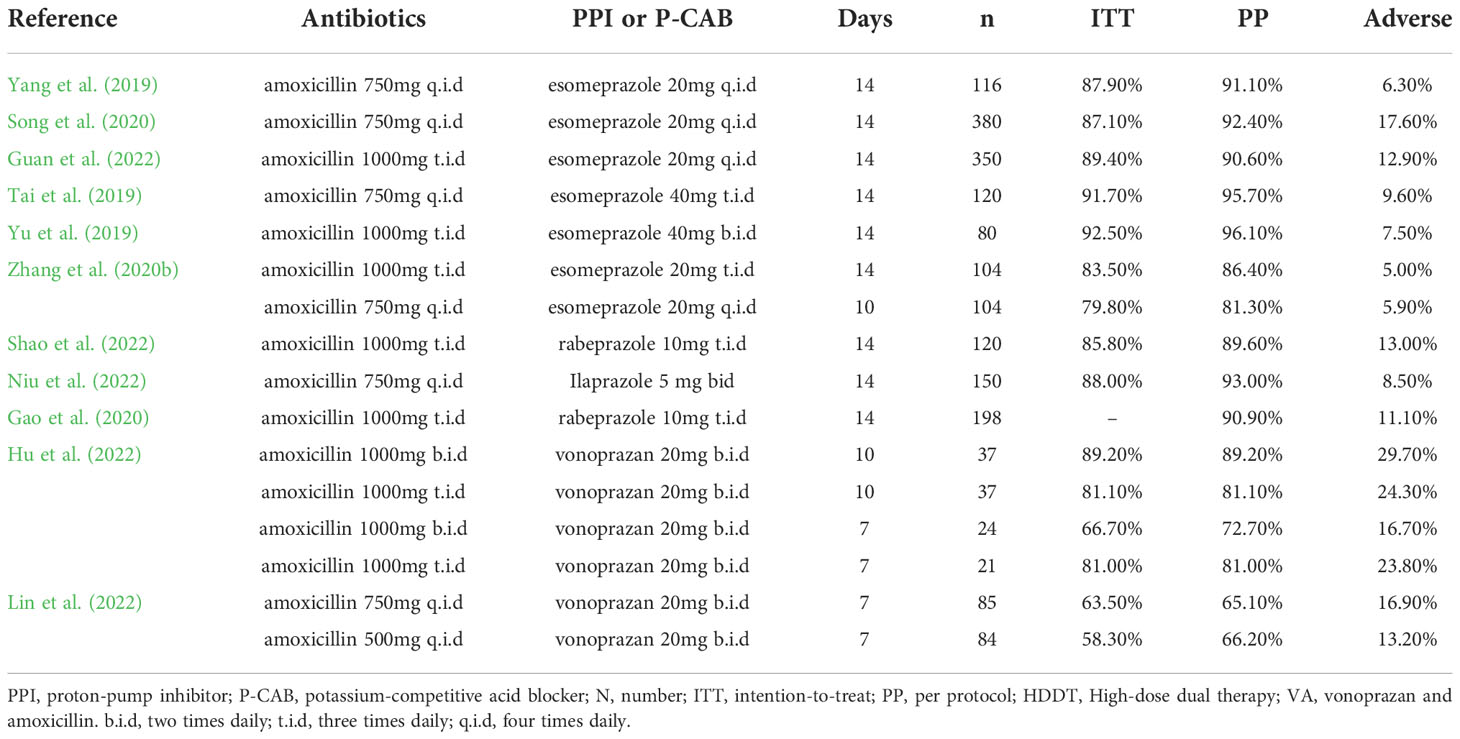
Table 1 Summary of HDDT or VA dual therapy as the first-line treatment of H. pylori infection in China.
Vonoprazan, a potassium-competitive acid blocker, was firstly introduced in Japan, which inhibited the gastric acid faster, longer and stronger in comparison with PPIs (Abadi and Ierardi, 2019). Its combination with amoxicillin (750mg b.i.d or 500mg t.i.d) for 7 days in adults (Furuta et al., 2020); Suzuki et al., 2020) or junior high school students (Gotoda et al., 2020) achieved acceptable eradication rate in Japan. We have conducted a systematic review and meta-analysis to evaluate the efficacy and safety of vonoprazan and amoxicillin (VA) dual therapy (Ouyang et al., 2022), the results showed that the crude eradication rate of VA dual therapy was 87.5% and 89.6% by ITT and PP analysis, respectively. Additionally, the side effect of VA dual therapy was 19.1%. Japan government restrictions limit the duration of regimen to 7 days. Chey et al. (2022) further explored the efficacy of VA dual therapy (amoxicillin 1g t.i.d and vonoprazan 20 mg b.i.d) for 14 days in the United States and Europe. 349 H. pylori-infected subjects received VA dual therapy. The eradication rate of VA dual therapy was 77.2% in all patients. The efficacy of regimen was unsatisfied although it showed superior to lansoprazole triple therapy. The different outcomes were achieved in Japan, United States and Europe, which might be explained by the differences of race and Body Mass Index. We conducted a prospective, randomized clinical pilot study to evaluate the efficacy of VA dual therapy in China (Hu et al., 2022b). 119 H. pylori-infected subjects were randomized to receive either low- or high-dose VA consisting of amoxicillin 1 g either b.i.d. or t.i.d plus VPZ 20 mg b.i.d for 7 or 10 days. Neither 7- or 10-day VA dual therapy with b.i.d. or t.i.d. amoxicillin provides satisfied efficacy (<90%). The following muti-centers study conducted in Lanzhou also showed that the efficacy of VA dual therapy for 7days was relatively low (Lin et al., 2022), which could be explained by the short duration of VA dual therapy and high antibiotic resistance of amoxicillin in this region (Zhong et al., 2021). VA dual therapy (VPZ 20mg bid with amoxicillin 1000mg b.i.d or t.i.d) for 14 days was shown to achieve high efficacy (eradication rate > 90%) as the first-line treatment for H. pylori infection in our center (unpublished data). For H. pylori-infected patients with history of treatment failure, the eradication rate of VA dual therapy (VPZ 20mg q.d or b.i.d with amoxicillin 1000mg t.i.d) for 14 days was 92.5%, which was effective and safe as rescue therapy for H. pylori infection (Gao et al., 2022). More importantly, our results showed that VA dual therapy showed minimal influence on the gut microbiota and short-chain fatty acids (Hu et al., 2022a). VA dual therapy for 14 days showed high efficacy and good safety for eradicating H. pylori. The included samples were limited and the application of VA dual therapy in different regions should be optimized. VA dual therapy is a promising H. pylori regimen in an era of increasing antibiotic resistance although more evidences are needed. Further prospective, multi-center, randomized control trail with more subjects included was needed to evaluate the efficacy and safety of low or high-dose VA dual therapy for 14 days in different regions of China.
The benefit of Helicobacter pylori eradication in the prevention of GC
China was a country with a high risk of GC (>20 per 100 000 person-years), especially in some regions (Changle, Linqu, Wuwei, Yangzhong, Zhuanghe etc.) (Liou et al., 2020). 2, 258 participants with H. pylori positive in Linqu county, Shandong province were randomized into H. pylori eradication, vitamin supplementation, garlic supplementation, or their placebos, who were followed up for 22 years (1995-2017). The results demonstrated that H. pylori treatment significantly reduce reduced risk of death due to GC (odds ratio 0.48, 95% confidence interval 0.32 to 0.71) (Li et al., 2019). In Changle, Fujian province, 1, 630 asymptomatic, H. pylori-infected subjects were randomly assigned to receive H. pylori eradication or placebo, who were then follow-up for 26.5 years (1994-2020). Subjects receiving H. pylori eradication had a lower incidence of GC than their placebo counterparts (hazard ratio, 0.57; 95% CI, 0.33-0.98), the benefit was more obvious in subjects without premalignant gastric lesions or dyspepsia symptoms at baseline (Yan et al., 2022). Mass eradication of H. pylori infection was launched in 2004 and continued until 2018 for a high-risk Taiwanese population aged 30 years or older dwelling on Matsu Islands with H. pylori infection. The effectiveness of H. pylori eradication in reducing GC incidence was 53% (95% CI 30% to 69%). Additionally, the decreased presence and severity of atrophic gastritis and intestinal metaplasia was also observed (Chiang et al., 2021). Acceptable cure rate of H. pylori and low rate of adverse effects were achieved during mass screening and eradication of H. pylori (Lei et al., 2022).
The benefit of H. pylori eradication in the prevention of GC was confirmed by randomized control trails with large subjects included and long-term follow-up in China, which supported the mass screening and eradication of H. pylori. The benefit was more obvious in subjects without the incidence of precancerous lesions. The subjects with precancerous lesions also benefit from H. pylori eradication because the successful treatment could prevent the progression of diseases. For example, H. pylori eradication could reduce the incidence of metachronous GC in subjects with early GC undergoing endoscopic mucosal resection (relative risk= 0.49; 95% CI 0.34 to 0.70) (Ford et al., 2020). Additionally, in an analysis of data from a public hospital database with 73, 237 H. pylori positive subjects included on Hong Kong, H. pylori infection eradication reduced the risk of GC in subjects 60 years or older compared to the matched general population (Leung et al., 2018). As such, the Chinese consensus (Du et al., 2020; Ding et al., 2022) have emphasized the importance of early detection, diagnosis, and treatment of H. pylori to reduce the occurrence of GC and a family-based H. pylori prevention and eradication strategy to prevent its intra-familial transmission and related diseases. Additionally, national, provincial and regional specialist clinic of H. pylori infection was established by the office of H. pylori infection and GC prevention and control, which could promote the standard of H. pylori diagnosis and treatment.
The stratification of risk for GC in the Chinese GC risk population
The 5-year survival rate was below 30% when advanced GC was diagnosed (Ajani et al., 2013). Early GC showed good prognosis (5-year survival rate >90%), which could be cured by the endoscopic submucosal dissection (Isobe et al., 2011). However, the diagnosis rate of early GC was low (<10%) in China. An effective way to improve the current serious situation of diagnosis and treatment of GC was the endoscopy screening and treatment in patients with high-risk of GC. The current national screening guideline for GC in China recommended screening beginning at age 40 years for all in the high-risk population (those residing in high-incidence areas for more than 3 years or who have H. pylori infection, a positive family history of GC, or risk factors for GC etc.). Estimated exceed 300 million individuals were defined as high-risk of GC and needed to receive the screening gastroscopy, which is not likely feasible in the clinical practice. An applicable risk prediction rule to further stratify risk for GC in the Chinese GC risk population was needed.
Tu et al. (2017) conducted a cross-sectional study for identifying high-risk individuals and predicting risk of developing GC in Zhuanghe county, a rural county of northern China with high incidence and mortality of GC. The screening program included individuals with 35–70 years old or upper gastrointestinal symptoms or a positive family history of GC. Totally, 9, 002 participants underwent gastroscopy were recruited by the end of 2012. The five biomarkers (especially PGII, the PGI/II ratio, and H. pylori sero-positivity) (Area Under the Curve=0.803) were identified to be associated with the presence of precancerous gastric lesions or GC at enrollment. From 2015 to 2017, The Gastrointestinal Early Cancer Prevention & Treatment Alliance of China conducted a nationwide multi-center cross-sectional study to identify individuals with a high risk prior to gastroscopy, which recruited 14, 929 individuals aged 40–80 years who went to hospitals for a GC screening gastroscopy (Cai et al., 2019). Seven variables (age, sex, PG I/II ratio, G-17 level, H. pylori infection, pickled food and fried food) were comprised as the novel GC risk prediction rule, with scores ranging from 0 to 25. 70.8% of total GC cases and 70.3% of early GC cases were detected when individuals with medium risk (score: 12-16) and high risk (score: 17-25) received gastroscopy. Endoscopy requirements could be reduced by 66.7% according to the low-risk proportion. This nationwide study successfully developed and validated prediction rule identifying individuals at a higher risk in a Chinese high-risk population, which needed to receive further gastroscopy. Compared to ABC method (Miki, 2011), five markers-based method (Tu et al., 2017), the prediction model of seven variables (Cai et al., 2019) showed higher Area Under the Curve and Youden index values, which was further confirmed by a retrospective analysis of data from the Provincial Gastric Cancer Screening Program with 97, 541 individuals included (Hu et al., 2021). A future large population-based screening project should be launched to test and validate its efficacy of novel GC risk prediction rule.
Conclusions
China was a country with high incidence of GC and high infection rate of H. pylori. With the improvement of socioeconomic status and sanitary conditions and successful H. pylori eradication, the prevalence of H. pylori showed a decreased trend over time. Meanwhile, H. pylori recurrence rate remained low during the long-term follow-up. The situation of H. pylori resistant to antibiotics is serious worldwide, including in China. Suspectable antibiotics are recommended to be used in the regimens. With the publication of Chinese consensus report on the management of H. pylori infection and the effort of public preach of H. pylori-related knowledge, the standardization of diagnosis and treatment of H. pylori by clinicians was improved. Efforts were still needed to be done for education of public populations and the supervisor of H. pylori management in clinical practice. For example, the office for prevention and treatment of H. pylori infection and GC was established in 2021, which aimed to launch the national or provincial or county demonstration center of the standard outpatient clinic of H. pylori diagnosis and treatment. BQT was effective and safe, which was recommended as the first-line treatment for H. pylori infection. HDDT and VA dual therapy were the alternative choice. Successful H. pylori eradication reduce the incidence of GC and prevent the progression of H. pylori-related diseases. Prediction models had been developed and validated to stratify GC risk in the Chinese GC risk population.
“Healthy China 2030” proposed the improvement of public health with expectation of 5-year nationwide survival rate of cancer improved by 15%. The combination of primary (effective H. pylori eradication) and secondary prevention (increasing the diagnosis rate of early GC and treated them) was the effective way to decrease the incidence of GC and increase the survival rate of GC.
Author contributions
YH wrote the manuscript. YZ and N-HL designed and revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the National Natural Science Foundation of China (No. 82000531 and 82170580), the Project for Academic and Technical Leaders of Major Disciplines in Jiangxi Province (No. 20212BCJL23065), the Key Research and Development Program of Jiangxi Province (No. 20212BBG73018), the Youth Project of the Jiangxi Natural Science Foundation (No. 20202BABL216006), National Science and Technology Award Reserve Cultivation Project (20192AEI91008) and The First Affiliated Hospital of Nanchang University Clinical Research and Cultivation Project (YFYLCYJPY202002).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Abadi, A., Ierardi, E. (2019). Vonoprazan and Helicobacter pylori treatment: A lesson from Japan or a limited geographic phenomenon? Front. Pharmacol. 10. doi: 10.3389/fphar.2019.00316
Ajani, J. A., Bentrem, D. J., Besh, S., D'Amico, T. A., Das, P., Denlinger, C., et al. (2013). Gastric cancer, version 2.2013: featured updates to the NCCN guidelines. J. Natl. Compr. Canc Netw. 11 (5), 531–546. doi: 10.6004/jnccn.2013.0070
Bell, G. D., Powell, K. U., Burridge, S. M., Harrison, G., Rameh, B., Weil, J., et al. (1993). Reinfection or recrudescence after apparently successful eradication of Helicobacter pylori infection: implications for treatment of patients with duodenal ulcer disease. Q J. Med. 86 (6), 375–382.
Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68 (6), 394–424. doi: 10.3322/caac.21492
Cai, Q., Zhu, C., Yuan, Y., Feng, Q., Feng, Y., Hao, Y., et al. (2019). Development and validation of a prediction rule for estimating gastric cancer risk in the Chinese high-risk population: A nationwide multicentre study. Gut 68 (9), 1576–1587. doi: 10.1136/gutjnl-2018-317556
Chey, W. D., Megraud, F., Laine, L., Lopez, L. J., Hunt, B. J., Howden, C. W. (2022). Vonoprazan triple and dual therapy for Helicobacter pylori infection in the united states and Europe: Randomized clinical trial. Gastroenterology. 163 (3), 608–619. doi: 10.1053/j.gastro.2022.05.055
Chiang, T. H., Chang, W. J., Chen, S. L., Yen, A. M., Fann, J. C., Chiu, S. Y., et al. (2021). Mass eradication of Helicobacter pylori to reduce gastric cancer incidence and mortality: A long-term cohort study on matsu islands. Gut 70 (2), 243–250. doi: 10.1136/gutjnl-2020-322200
de Martel, C., Georges, D., Bray, F., Ferlay, J., Clifford, G. M. (2020). Global burden of cancer attributable to infections in 2018: A worldwide incidence analysis. Lancet Glob Health 8 (2), e180–e190. doi: 10.1016/S2214-109X(19)30488-7
Ding, S. Z., Du, Y. Q., Lu, H., Wang, W. H., Cheng, H., Chen, S. Y., et al. (2022). Chinese Consensus report on family-based Helicobacter pylori infection control and managemen Edition). Gut 71 (2), 238–253. doi: 10.1136/gutjnl-2021-325630
Dore, M. P., Lu, H., Graham, D. Y. (2016). Role of bismuth in improving Helicobacter pylori eradication with triple therapy. Gut 65 (5), 870–878. doi: 10.1136/gutjnl-2015-311019
Du, Y., Zhu, H., Liu, J., Li, J., Chang, X., Zhou, L., et al. (2020). Consensus on eradication of Helicobacter pylori and prevention and control of gastric cancer in China, (2019, shanghai). J. Gastroenterol. Hepatol. 35 (4), 624–629. doi: 10.1111/jgh.14947
Ford, A. C., Yuan, Y., Moayyedi, P. (2020). Helicobacter pylori eradication therapy to prevent gastric cancer: Systematic review and meta-analysis. Gut 69 (12), 2113–2121. doi: 10.1136/gutjnl-2020-320839
Furuta, T., Yamade, M., Kagami, T., Uotani, T., Suzuki, T., Higuchi, T., et al. (2020). Dual therapy with vonoprazan and amoxicillin is as effective as triple therapy with vonoprazan, amoxicillin and clarithromycin for eradication of Helicobacter pylori. Digestion 101 (6), 743–751. doi: 10.1159/000502287
Gao, W., Teng, G., Wang, C., Xu, Y., Li, Y., Cheng, H. (2022). Eradication rate and safety of a "simplified rescue therapy": 14-day vonoprazan and amoxicillin dual regimen as rescue therapy on treatment of Helicobacter pylori infection previously failed in eradication: A real-world, retrospective clinical study in China. Helicobacter 27 (5), e12918. doi: 10.1111/hel.12918
Gao, W., Ye, H., Deng, X., Wang, C., Xu, Y., Li, Y., et al. (2020). Rabeprazole-amoxicillin dual therapy as first-line treatment for H pylori eradication in special patients: A retrospective, real-life study. Helicobacter 25 (5), e12717. doi: 10.1111/hel.12717
Goh, K. L., Chan, W. K., Shiota, S., Yamaoka, Y. (2011). Epidemiology of Helicobacter pylori infection and public health implications. Helicobacter 16 Suppl, 1, 1–1, 9. doi: 10.1111/j.1523-5378.2011.00874.x
Gotoda, T., Kusano, C., Suzuki, S., Horii, T., Ichijima, R., Ikehara, H. (2020). Clinical impact of vonoprazan-based dual therapy with amoxicillin for H. pylori infection in a treatment-naive cohort of junior high school students in Japan. J. Gastroenterol. 55 (10), 969–976. doi: 10.1007/s00535-020-01709-4
Graham, D. Y., Fischbach, L. (2010). Helicobacter pylori treatment in the era of increasing antibiotic resistance. Gut 59 (8), 1143–1153. doi: 10.1136/gut.2009.192757
Graham, D. Y., Lu, H., Yamaoka, Y. (2007). A report card to grade Helicobacter pylori therapy. Helicobacter 12 (4), 275–278. doi: 10.1111/j.1523-5378.2007.00518.x
Guan, J. L., Hu, Y. L., An, P., He, Q., Long, H., Zhou, L., et al. (2022). Comparison of high-dose dual therapy with bismuth-containing quadruple therapy in Helicobacter pylori-infected treatment-naive patients: An open-label, multicenter, randomized controlled trial. Pharmacotherapy 42 (3), 224–232. doi: 10.1002/phar.2662
He, C., Peng, C., Wang, H., Ouyang, Y., Zhu, Z., Shu, X., et al. (2019). The eradication of Helicobacter pylori restores rather than disturbs the gastrointestinal microbiota in asymptomatic young adults. Helicobacter 24 (4), e12590. doi: 10.1111/hel.12590
Hooi, J., Lai, W. Y., Ng, W. K., Suen, M., Underwood, F. E., Tanyingoh, D., et al. (2017). Global prevalence of Helicobacter pylori infection: Systematic review and meta-analysis. Gastroenterology 153 (2), 420–429. doi: 10.1053/j.gastro.2017.04.022
Hu, Y., Bao, H., Jin, H., Zhao, J., Xu, Y., Huang, X., et al. (2021). Performance evaluation of four prediction models for risk stratification in gastric cancer screening among a high-risk population in China. Gastric Cancer 24 (6), 1194–1202. doi: 10.1007/s10120-021-01204-6
Hu, Y., Xu, X., Ouyang, Y. B., He, C., Li, N. S., Xie, C., et al. (2022a). Altered gut microbiota and short-chain fatty acids after vonoprazan-amoxicillin dual therapy for Helicobacter pylori eradication. Front. Cell Infect. Microbiol. 12. doi: 10.3389/fcimb.2022.881968
Hu, Y., Xu, X., Ouyang, Y. B., He, C., Li, N. S., Xie, C., et al. (2022b). Optimization of vonoprazan-amoxicillin dual therapy for eradicating Helicobacter pylori infection in China: A prospective, randomized clinical pilot study. Helicobacter 27 (4), e12896. doi: 10.1111/hel.12896
Hu, Y., Zhu, Y., Lu, N. H. (2017a). Novel and effective therapeutic regimens for Helicobacter pylori in an era of increasing antibiotic resistance. Front. Cell Infect. Microbiol. 7. doi: 10.3389/fcimb.2017.00168
Hu, Y., Zhu, Y., Lu, N. H. (2017b). Primary antibiotic resistance of Helicobacter pylori in China. Dig Dis. Sci. 62 (5), 1146–1154. doi: 10.1007/s10620-017-4536-8
Hu, Y., Wan, J. H., Li, X. Y., Zhu, Y., Graham, D. Y., Lu, N. H. (2017c). Systematic review with meta-analysis: the global recurrence rate of Helicobacter pylori. Aliment Pharmacol. Ther. 46 (9), 773–779. doi: 10.1111/apt.14319
Isobe, Y., Nashimoto, A., Akazawa, K., Oda, I., Hayashi, K., Miyashiro, I., et al. (2011). Gastric cancer treatment in Japan: 2008 annual report of the JGCA nationwide registry. Gastric Cancer 14 (4), 301–316. doi: 10.1007/s10120-011-0085-6
Kuo, Y. T., Liou, J. M., El-Omar, E. M., Wu, J. Y., Leow, A., Goh, K. L., et al. (2017). Primary antibiotic resistance in Helicobacter pylori in the Asia-pacific region: A systematic review and meta-analysis. Lancet Gastroenterol. Hepatol. 2 (10), 707–715. doi: 10.1016/S2468-1253(17)30219-4
Labenz, J. (2001). Current role of acid suppressants in Helicobacter pylori eradication therapy. Best Pract. Res. Clin. Gastroenterol. 15 (3), 413–431. doi: 10.1053/bega.2001.0188
Lei, W. Y., Lee, J. Y., Chen, C. L., Bair, M. J., Wu, J. Y., Wu, D. C., et al. (2022). Screening and eradication of Helicobacter pylori to prevent gastric cancer in indigenous Taiwanese communities: A population-based study and development of an index-case method. Lancet Oncol. 23 Suppl, 1, S2. doi: 10.1016/S1470-2045(22)00401-6
Leja, M., Axon, A., Brenner, H. (2016). Epidemiology of Helicobacter pylori infection. Helicobacter 21 Suppl, 1, 3–1, 7. doi: 10.1111/hel.12332
Leung, W. K., Wong, I., Cheung, K. S., Yeung, K. F., Chan, E. W., Wong, A., et al. (2018). Effects of Helicobacter pylori treatment on incidence of gastric cancer in older individuals. Gastroenterology 155 (1), 67–75. doi: 10.1053/j.gastro.2018.03.028
Liang, X., Xu, X., Zheng, Q., Zhang, W., Sun, Q., Liu, W., et al. (2013). Efficacy of bismuth-containing quadruple therapies for clarithromycin-, metronidazole-, and fluoroquinolone-resistant Helicobacter pylori infections in a prospective study. Clin. Gastroenterol. Hepatol. 11 (7), 802–807. doi: 10.1016/j.cgh.2013.01.008
Lin, B. S., Li, Y. Y., Qiao, C., Liu, J., Wang, J., Wan, M., et al. (2022). Implementation of WeChat-based patient-doctor interaction in the management of Helicobacter pylori infection: A propensity score matching analysis. J. Dig Dis. 23 (5-6), 280–287. doi: 10.1111/1751-2980.13114
Lin, Y., Xu, H., Yun, J., Yu, X., Shi, Y., Zhang, D. (2022). The efficacy of vonoprazan combined with different dose amoxicillin on eradication of Helicobacter pylori: An open, multicenter, randomized clinical study. Ann. Transl. Med. 10 (18), 987. doi: 10.21037/atm-22-4133
Liou, J. M., Malfertheiner, P., Lee, Y. C., Sheu, B. S., Sugano, K., Cheng, H. C., et al. (2020). Screening and eradication of Helicobacter pylori for gastric cancer prevention: The Taipei global consensus. Gut 69 (12), 2093–2112. doi: 10.1136/gutjnl-2020-322368
Liu, D. S., Wang, Y. H., Zeng, Z. R., Zhang, Z. Y., Lu, H., Xu, J. M., et al. (2018). Primary antibiotic resistance of Helicobacter pylori in Chinese patients: A multiregion prospective 7-year study. Clin. Microbiol. Infect. 24 (7), 780–785. doi: 10.1016/j.cmi.2017.11.010
Liu, D. S., Wang, Y. H., Zhu, Z. H., Zhang, S. H., Zhu, X., Wan, J. H., et al. (2019). Characteristics of Helicobacter pylori antibiotic resistance: Data from four different populations. Antimicrob. Resist. Infect. Control 8, 192. doi: 10.1186/s13756-019-0632-1
Liu, W. Z., Xie, Y., Cheng, H., Lu, N. H., Hu, F. L., Zhang, W. D., et al. (2013). Fourth Chinese national consensus report on the management of Helicobacter pylori infection. J. Dig Dis. 14 (5), 211–221. doi: 10.1111/1751-2980.12034
Liu, W. Z., Xie, Y., Lu, H., Cheng, H., Zeng, Z. R., Zhou, L. Y., et al. (2018). Fifth Chinese national consensus report on the management of Helicobacter pylori infection. Helicobacter 23 (2), e12475. doi: 10.1111/hel.12475
Li, W. Q., Zhang, J. Y., Ma, J. L., Li, Z. X., Zhang, L., Zhang, Y., et al. (2019). Effects of Helicobacter pylori treatment and vitamin and garlic supplementation on gastric cancer incidence and mortality: Follow-up of a randomized intervention trial. BMJ 366, l5016. doi: 10.1136/bmj.l5016
Luo, M., Hao, Y., Tang, M., Shi, M., He, F., Xie, Y., et al. (2020). Application of a social media platform as a patient reminder in the treatment of Helicobacter pylori. Helicobacter 25 (2), e12682. doi: 10.1111/hel.12682
Malfertheiner, P., Megraud, F., O'Morain, C. A., Gisbert, J. P., Kuipers, E. J., Axon, A. T., et al. (2017). Management of Helicobacter pylori infection-the maastricht V/Florence consensus report. Gut 66 (1), 6–30. doi: 10.1136/gutjnl-2016-312288
Ma, H., Zhao, X. H., Zhang, L. L., Wu, L. M. (2021). Application of WeChat platform in the management of patients infected with Helicobacter pylori. Helicobacter 26 (5), e12832. doi: 10.1111/hel.12832
Miki, K. (2011). Gastric cancer screening by combined assay for serum anti-Helicobacter pylori IgG antibody and serum pepsinogen levels - "ABC method". Proc. Jpn Acad. Ser. B Phys. Biol. Sci. 87 (7), 405–414. doi: 10.2183/pjab.87.405
Mitchell, H. M., Hu, P., Chi, Y., Chen, M. H., Li, Y. Y., Hazell, S. L. (1998). A low rate of reinfection following effective therapy against Helicobacter pylori in a developing nation (China). Gastroenterology 114 (2), 256–261. doi: 10.1016/s0016-5085(98)70475-5
Nagy, P., Johansson, S., Molloy-Bland, M. (2016). Systematic review of time trends in the prevalence of Helicobacter pylori infection in China and the USA. Gut Pathog. 8, 8. doi: 10.1186/s13099-016-0091-7
Niu, M., Zhou, Y., Xie, Y., Li, X., Tian, Y., Yao, L., et al. (2022). Comparison of the dual therapy of ilaprazole-amoxicillin and the bismuth quadruple therapy of ilaprazole-Amoxicillin-Furazolidone-Bismuth glycyrrhizinate for eradication of Helicobacter pylori. Front. Pharmacol. 13. doi: 10.3389/fphar.2022.771876
Niv, Y., Hazazi, R. (2008). Helicobacter pylori recurrence in developed and developing countries: Meta-analysis of 13C-urea breath test follow-up after eradication. Helicobacter 13 (1), 56–61. doi: 10.1111/j.1523-5378.2008.00571.x
Ouyang, Y. B., Wang, M. H., Xu, Y. L., Zhu, Y., Lu, N. H., Hu, Y. (2022). Amoxicillin-vonoprazan dual therapy for Helicobacter pylori eradication: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 37 (9), 1666–1672. doi: 10.1111/jgh.15917
Ren, S., Cai, P., Liu, Y., Wang, T., Zhang, Y., Li, Q., et al. (2022). Prevalence of Helicobacter pylori infection in China: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 37 (3), 464–470. doi: 10.1111/jgh.15751
Savoldi, A., Carrara, E., Graham, D. Y., Conti, M., Tacconelli, E. (2018). Prevalence of antibiotic resistance in Helicobacter pylori: A systematic review and meta-analysis in world health organization regions. Gastroenterology 155 (5), 1372–1382. doi: 10.1053/j.gastro.2018.07.007
Shao, Q. Q., Yu, X. C., Yu, M., Ma, J., Zhao, J. B., Yuan, L., et al. (2022). Rabeprazole plus amoxicillin dual therapy is equally effective to bismuth-containing quadruple therapy for Helicobacter pylori eradication in central China: A single-center, prospective, open-label, randomized-controlled trial. Helicobacter 27 (2), e12876. doi: 10.1111/hel.12876
Song, Z., Chen, Y., Lu, H., Zeng, Z., Wang, W., Liu, X., et al. (2022). Diagnosis and treatment of Helicobacter pylori infection by physicians in China: A nationwide cross-sectional study. Helicobacter 27 (3), e12889. doi: 10.1111/hel.12889
Song, C., Qian, X., Zhu, Y., Shu, X., Song, Y., Xiong, Z., et al. (2019a). Effectiveness and safety of furazolidone-containing quadruple regimens in patients with Helicobacter pylori infection in real-world practice. Helicobacter 24 (4), e12591. doi: 10.1111/hel.12591
Song, C., Xie, C., Zhu, Y., Liu, W., Zhang, G., He, S., et al. (2019b). Management of Helicobacter pylori infection by clinicians: A nationwide survey in a developing country. Helicobacter 24 (6), e12656. doi: 10.1111/hel.12656
Song, Z., Zhou, L., Xue, Y., Suo, B., Tian, X., Niu, Z. Y. (2020). A comparative study of 14-day dual therapy (esomeprazole and amoxicillin four times daily) and triple plus bismuth therapy for first-line Helicobacter pylori infection eradication: A randomized trial. Helicobacter 25 (6), e12762. doi: 10.1111/hel.12762
Sugano, K., Tack, J., Kuipers, E. J., Graham, D. Y., El-Omar, E. M., Miura, S., et al. (2015). Kyoto Global consensus report on Helicobacter pylori gastritis. Gut 64 (9), 1353–1367. doi: 10.1136/gutjnl-2015-309252
Sun, Q., Liang, X., Zheng, Q., Liu, W., Xiao, S., Gu, W., et al. (2010). High efficacy of 14-day triple therapy-based, bismuth-containing quadruple therapy for initial Helicobacter pylori eradication. Helicobacter 15 (3), 233–238. doi: 10.1111/j.1523-5378.2010.00758.x
Suzuki, S., Gotoda, T., Kusano, C., Ikehara, H., Ichijima, R., Ohyauchi, M.. (2020). Seven-day vonoprazan and low-dose amoxicillin dual therapy as first-line Helicobacter pylori treatment: A multicentre randomised trial in Japan. Gut 69 (6), 1019–1026. doi: 10.1136/gutjnl-2019-319954
Tacconelli, E., Carrara, E., Savoldi, A., Harbarth, S., Mendelson, M., Monnet, D. L., et al. (2018). Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 18 (3), 318–327. doi: 10.1016/S1473-3099(17)30753-3
Tai, W. C., Liang, C. M., Kuo, C. M., Huang, P. Y., Wu, C. K., Yang, S. C., et al. (2019). A 14 day esomeprazole- and amoxicillin-containing high-dose dual therapy regimen achieves a high eradication rate as first-line anti-Helicobacter pylori treatment in Taiwan: A prospective randomized trial. J. Antimicrob. Chemother. 74 (6), 1718–1724. doi: 10.1093/jac/dkz046
Tu, H., Sun, L., Dong, X., Gong, Y., Xu, Q., Jing, J., et al. (2017). A serological biopsy using five stomach-specific circulating biomarkers for gastric cancer risk assessment: A multi-phase study. Am. J. Gastroenterol. 112 (5), 704–715. doi: 10.1038/ajg.2017.55
Wu, Y., Su, T., Zhou, X., Lu, N., Li, Z., Du, Y. Q. (2020). Awareness and attitudes regarding Helicobacter pylori infection in Chinese physicians and public population: A national cross-sectional survey. Helicobacter 25 (4), e12705. doi: 10.1111/hel.12705
Xia, C., Dong, X., Li, H., Cao, M., Sun, D., He, S., et al. (2022). Cancer statistics in China and united state: Profiles, trends, and determinants. Chin. Med. J. (Engl) 135 (5), 584–590. doi: 10.1097/CM9.0000000000002108
Xie, C., Lu, N. H. (2015). Review: clinical management of Helicobacter pylori infection in China. Helicobacter 20 (1), 1–10. doi: 10.1111/hel.12178
Xie, Y., Song, C., Cheng, H., Xu, C., Zhang, Z., Wang, J., et al. (2020). Long-term follow-up of Helicobacter pylori reinfection and its risk factors after initial eradication: A large-scale multicentre, prospective open cohort, observational study. Emerg. Microbes Infect. 9 (1), 548–557. doi: 10.1080/22221751.2020.1737579
Xie, Y., Zhang, Z., Hong, J., Liu, W., Lu, H., Du, Y., et al. (2018a). Furazolidone-containing triple and quadruple eradication therapy for initial treatment for Helicobacter pylori infection: A multicenter randomized controlled trial in china. [Journal article; multicenter study; randomized controlled trial. Helicobacter 23 (5), e12496. doi: 10.1111/hel.12496
Xie, Y., Zhu, Z., Wang, J., Zhang, L., Zhang, Z., Lu, H., et al. (2018b). Ten-day quadruple therapy comprising low-dose rabeprazole, bismuth, amoxicillin, and tetracycline is an effective and safe first-line treatment for Helicobacter pylori infection in a population with high antibiotic resistance: A prospective, multicenter, randomized, parallel-controlled clinical trial in China. Antimicrob. Agents Chemother. 62 (9), e00432–18. doi: 10.1128/AAC.00432-18
Xie, Y., Zhu, Y., Zhou, H., Lu, Z. F., Yang, Z., Shu, X., et al. (2014). Furazolidone-based triple and quadruple eradication therapy for Helicobacter pylori infection. World J. Gastroenterol. 20 (32), 11415–11421. doi: 10.3748/wjg.v20.i32.11415
Xue, Y., Zhou, L. Y., Lu, H. P., Liu, J. Z. (2019). Recurrence of Helicobacter pylori infection: incidence and influential factors. Chin. Med. J. (Engl) 132 (7), 765–771. doi: 10.1097/CM9.0000000000000146
Yan, L., Chen, Y., Chen, F., Tao, T., Hu, Z., Wang, J., et al. (2022). Effect of Helicobacter pylori eradication on gastric cancer prevention: Updated report from a randomized controlled trial with 26.5 years of follow-up. Gastroenterology 163 (1), 154–162. doi: 10.1053/j.gastro.2022.03.039
Yang, J., Zhang, Y., Fan, L., Zhu, Y. J., Wang, T. Y., Wang, X. W., et al. (2019). Eradication efficacy of modified dual therapy compared with bismuth-containing quadruple therapy as a first-line treatment of Helicobacter pylori. Am. J. Gastroenterol. 114 (3), 437–445. doi: 10.14309/ajg.0000000000000132
Yuan, C., Adeloye, D., Luk, T. T., Huang, L., He, Y., Xu, Y., et al. (2022). The global prevalence of and factors associated with Helicobacter pylori infection in children: A systematic review and meta-analysis. Lancet Child Adolesc. Health 6 (3), 185–194. doi: 10.1016/S2352-4642(21)00400-4
Yu, L., Luo, L., Long, X., Liang, X., Ji, Y., Graham, D. Y., et al. (2019). High-dose PPI-amoxicillin dual therapy with or without bismuth for first-line Helicobacter pylori therapy: A randomized trial. Helicobacter 24 (4), e12596. doi: 10.1111/hel.12596
Zamani, M., Ebrahimtabar, F., Zamani, V., Miller, W. H., Alizadeh-Navaei, R., Shokri-Shirvani, J., et al. (2018). Systematic review with meta-analysis: The worldwide prevalence of Helicobacter pylori infection. Aliment Pharmacol. Ther. 47 (7), 868–876. doi: 10.1111/apt.14561
Zeng, M., Mao, X. H., Li, J. X., Tong, W. D., Wang, B., Zhang, Y. J., et al. (2015). Efficacy, safety, and immunogenicity of an oral recombinant Helicobacter pylori vaccine in children in China: A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 386 (10002), 1457–1464. doi: 10.1016/S0140-6736(15)60310-5
Zha, J., Li, Y. Y., Qu, J. Y., Yang, X. X., Han, Z. X., Zuo, X. Y. (2022). Effects of enhanced education for patients with the Helicobacter pylori infection: A systematic review and meta-analysis. Helicobacter 27 (2), e12880. doi: 10.1111/hel.12880
Zhang, W., Chen, Q., Liang, X., Liu, W., Xiao, S., Graham, D. Y., et al. (2015). Bismuth, lansoprazole, amoxicillin and metronidazole or clarithromycin as first-line Helicobacter pylori therapy. Gut 64 (11), 1715–1720. doi: 10.1136/gutjnl-2015-309900
Zhang, Y., Dong, Q., Tian, L., Zhang, S., Zuo, N., Zhang, S., et al. (2020a). Risk factors for recurrence of Helicobacter pylori infection after successful eradication in Chinese children: A prospective, nested case-control study. Helicobacter 25 (5), e12749. doi: 10.1111/hel.12749
Zhang, Y., Zhu, Y. J., Zhao, Z., Zhao, J. T., Wang, T. Y., Yang, J., et al. (2020b). Efficacy of modified esomeprazole-amoxicillin dual therapies for Helicobacter pylori infection: An open-label, randomized trial. Eur. J. Gastroenterol. Hepatol. 32 (5), 563–568. doi: 10.1097/MEG.0000000000001646
Zhao, J. B., Yuan, L., Yu, X. C., Shao, Q. Q., Ma, J., Yu, M., et al. (2021). Whole family-based Helicobacter pylori eradication is a superior strategy to single-infected patient treatment approach: A systematic review and meta-analysis. Helicobacter 26 (3), e12793. doi: 10.1111/hel.12793
Zhong, Z., Zhang, Z., Wang, J., Hu, Y., Mi, Y., He, B., et al. (2021). A retrospective study of the antibiotic-resistant phenotypes and genotypes of Helicobacter pylori strains in China. Am. J. Cancer Res. 11 (10), 5027–5037.
Zhou, G. (2020). Helicobacter pylori recurrence after eradication therapy in jiangjin district, chongqing, China. Gastroenterol. Res. Pract. 2020, 7510872. doi: 10.1155/2020/7510872
Zhou, L. Y., Lin, S. R., Shen, Z. Y., Zhong, S. Z., Ding, S. G., Huang, X. B., et al. (2003). Five-year follow-up study after Helicobacter pylori eradication: Reinfection and peptic ulcer status. Chin. J. Dig Dis. 4, 45–48. doi: 10.1046/j.1443-9573.2003.00104.x
Keywords: Helicobacter pylori, prevalence, resistance, eradication, gastric cancer
Citation: Hu Y, Zhu Y and Lu N-H (2022) The management of Helicobacter pylori infection and prevention and control of gastric cancer in China. Front. Cell. Infect. Microbiol. 12:1049279. doi: 10.3389/fcimb.2022.1049279
Received: 20 September 2022; Accepted: 14 November 2022;
Published: 01 December 2022.
Edited by:
Xin Zhou, Stanford University, United StatesReviewed by:
Yang Guo, Shenzhen Hospital, Peking University, ChinaWei Hu, Southern Medical University, China
Copyright © 2022 Hu, Zhu and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nong-Hua Lu, lunonghua@ncu.edu.cn; Yin Zhu, zhuyin27@sina.com.cn
 Yi Hu
Yi Hu Yin Zhu
Yin Zhu Nong-Hua Lu
Nong-Hua Lu