- 1School of Pharmacy, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 2Department of Pharmacy, Affiliated Hospital of North Sichuan Medical College, Nanchong, China
- 3School of Ethnic Medicine, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 4Innovative Institute of Chinese Medicine and Pharmacy, Chengdu University of Traditional Chinese Medicine, Chengdu, China
Traditional Chinese medicine plays a significant role in the treatment of various diseases and has attracted increasing attention for clinical applications. Vascular diseases affecting vasculature in the heart, cerebrovascular disease, atherosclerosis, and diabetic complications have compromised quality of life for affected individuals and increase the burden on health care services. Berberine, a naturally occurring isoquinoline alkaloid form Rhizoma coptidis, is widely used in China as a folk medicine for its antibacterial and anti-inflammatory properties. Promisingly, an increasing number of studies have identified several cellular and molecular targets for berberine, indicating its potential as an alternative therapeutic strategy for vascular diseases, as well as providing novel evidence that supports the therapeutic potential of berberine to combat vascular diseases. The purpose of this review is to comprehensively and systematically describe the evidence for berberine as a therapeutic agent in vascular diseases, including its pharmacological effects, molecular mechanisms, and pharmacokinetics. According to data published so far, berberine shows remarkable anti-inflammatory, antioxidant, antiapoptotic, and antiautophagic activity via the regulation of multiple signaling pathways, including AMP-activated protein kinase (AMPK), nuclear factor κB (NF-κB), mitogen-activated protein kinase silent information regulator 1 (SIRT-1), hypoxia-inducible factor 1α (HIF-1α), vascular endothelial growth factor phosphoinositide 3-kinase (PI3K), protein kinase B (Akt), janus kinase 2 (JAK-2), Ca2+ channels, and endoplasmic reticulum stress. Moreover, we discuss the existing limitations of berberine in the treatment of vascular diseases, and give corresponding measures. In addition, we propose some research perspectives and challenges, and provide a solid evidence base from which further studies can excavate novel effective drugs from Chinese medicine monomers.
Introduction
The global health burden of vascular diseases, such as atherosclerosis, cerebrovascular disease, hypertension, and complications of diabetes, is rapidly increasing (Al Rifai et al., 2021; Ji et al., 2021; Riccardi et al., 2021). Epidemiological surveys have shown that the increasing cost of vascular diseases worldwide compromises quality of life for individuals (Liss et al., 2021). In addition, a broad variety of factors, including inflammation, vascular dysplasia, oxidative stress, and abnormal lipid metabolism, cause vascular diseases (Guzik and Touyz, 2017; Feng et al., 2020). Hence, strategies aiming to reduce inflammation and oxidative stress and normalize the lipid metabolism are generally used to treat and prevent the vascular diseases, and statins, nonsteroidal anti-inflammatory drugs, and novel biological agents are common therapeutic agents (Oesterle et al., 2017; Lu et al., 2018; Doña et al., 2020). However, the high cost and side effect profiles of these drugs make finding cheaper alternatives with fewer side effects and similar or better therapeutic outcomes a matter of urgency. Therapies used in traditional Chinese medicines (TCM) have long been used as complementary and alternative medicines for the treatment of vascular disease in China (Cheng et al., 2017; Li et al., 2018b). Recently, these have garnered research interest owing to fewer adverse reactions and lower toxicities of these compounds compared with those identified and used in western medicine (Xie et al., 2019; Oduro et al., 2020; Atanasov et al., 2021). Undeniably, TCM has made an indelible contribution to human health and is considered a potential source of therapies derived from natural, rather than synthetic, sources. Therefore, there is an increased emphasis on the use of medicinal plants such as those used in TCM in the development of novel drugs.
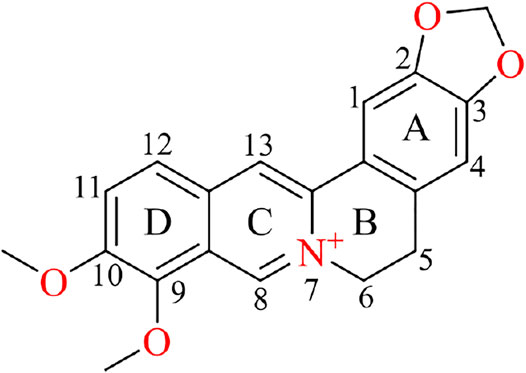
Berberine (C20H18NO4+, CAS no: 2086–83-1, Figure 1), a naturally occurring benzylisoquinoline alkaloid, has a long history of medical applications in TCM (Li et al., 2019). As a natural bioactive ingredient, berberine mainly exists naturally in the roots, rhizomes, and stem bark of various medicinal plants from the Ranunculaceae (Wang et al., 2019), Rutaceae (Ryuk et al., 2012), and Berberidaceae families (Gawel et al., 2020). Berberine was reportedly used in China as a folk medicine by Shennong at approximately 3000 BC, and the first recorded use of berberine is described in the ancient Chinese medical book The Divine Farmer’s Herb-Root Classic (Neag et al., 2018). The hydrochloride salt of berberine, listed as an oral antibacterial agent in Pharmacopoeia of the People’s Republic of China, is a common over-the-counter medication; dosage is usually 0.1 g in pill form taken 1–3 times per day for gastrointestinal infections (Zhang et al., 2021b). Colloquially, it is known as Huangliansu (Chinese: 黄连素; literally translated into English: “the essence of Chinese goldthread”). Modern pharmacological studies have confirmed that berberine exhibits various clinically useful biological properties, including anticardiovascular disease and anticancer properties (Feng et al., 2019; Hu et al., 2019). A growing body of evidence has shown that berberine has poor bioavailability due to first-pass effects in the intestinal lumen, leading to limitations in its clinical application (Xu et al., 2019; Habtemariam, 2020b). However, berberine is currently being evaluated in clinical trials for its important clinical benefits, lower toxicity and side effects compared with currently available therapies in western medicine, with its active metabolites exerting similar bioactive properties as berberine itself (Kumar et al., 2015; Imenshahidi and Hosseinzadeh, 2019). Further studies on berberine’s mechanism of action as well as new applications and novel formulations are therefore warranted.
In recent years, novel unique molecular entities derived from herbal medicines containing berberine have led to increased attention to the potential of this compound in the treatment of vascular diseases (Lee et al., 2018; Ren et al., 2019; Rajabi et al., 2021). Along with advances in pharmacological research, berberine was considered one of the most promising naturally derived drugs for the treatment of numerous human vascular diseases through the modulation of multiple signaling pathways. However, no systematic reviews on the pharmacological and pharmacokinetic properties of berberine in the context of vascular disease have been published. Therefore, in this review, we screened articles on berberine treatment in vascular diseases published in the years 2010–2021 using Web of Science, ScienceDirect, PubMed, Google Scholar and China National Knowledge Infrastructure online databases and summarized the findings to provide insights into the potential application of berberine in vascular diseases.
Physical and Chemical Properties of Berberine
Berberine is a yellow solid, with a melting point of 145.1–146.7°C; it is soluble in hot water, slightly soluble in cold water or ethanol, and insoluble in benzene, ether, chloroform, and other organic solvents (Zhang et al., 2016a). The structure of berberine comprises a dihydroisoquinoline ring and an isoquinoline ring with planar characteristics (Figure 1). The skeleton can be divided into four rings, A, B, C, and D, with the C2 and C3 of the A ring forming a methylenedioxy group responsible for most of the biological activities of berberine, such as anticancer activity (Leyva-Peralta et al., 2019). The “C” ring contains a quaternary ammonium structure (with N+ in the aromatic ring), which is necessary for the antibacterial activity (Gaba et al., 2021). In the “D” ring, C9 and C10 are each attached to a methoxy group. At present, structural modification studies of berberine mainly focus on the “C” and “D” rings (Xiao et al., 2018; Habtemariam 2020a); available evidence suggests that alkylation or acylation in the “D” ring resulted in hypoglycemic activity (Cheng et al., 2010; Shan et al., 2013). The introduction of cinnamic acid at 9-O position exerted strong hypoglycemic effects (Zhang et al., 2016b). C8 and C13 alkylation were shown to enhance cytotoxicity (Singh et al., 2021). Similarly, positions N7 and C13 are prone to modifications that enhance anticellular proliferative activity of berberine (Gaba et al., 2021). Moreover, berberine is fluorescent, with a maximum absorption wavelength of 350 nm and an emission wavelength of 530 nm in 0.01 mol/L sodium dodecyl sulfate solution. Thus, liquid chromatography–mass spectrometry and isotope labeling can be used to measure the content of berberine as part of a TCM or drugs (Chang et al., 2016; Ai et al., 2019).
Pharmacokinetics of Berberine
Absorption
Berberine exerts superior therapeutical effects on the vascular diseases, such as atherosclerosis; however, its effects are limited in clinic due to poor oral absorption and low bioavailability (Han et al., 2021b). Previous research has reported that the absolute bioavailability of berberine is 0.37% when administered in a single oral administration (48.2, 120, or 240 mg/kg body weight) in rats (Feng et al., 2021). Oral treatment with 100 mg/kg berberine has an absolute bioavailability of 0.68% as measured in rat plasma samples, with a mean maximum plasma concentration (Cmax) of 9.48 ng/ml and an area under the curve (AUC)0–36 h of 46.5 ng h/ml (Chen et al., 2011). Sahibzada et al. (2021) found that after a single oral dose of 50 mg/kg berberine in rabbits, the Cmax was 0.411 μg/ml.
Some studies have also reported the absorption of berberine in humans. In one study, the mean Cmax at 8 h post-administration was reported to be approximately 0.4 ng/ml for 400 mg berberine administered orally (n = 20) (Hua et al., 2007). Another study reported that the Cmax of berberine in 10 healthy individuals given 500 mg berberine orally was extremely low, at 0.07 nM (Spinozzi et al., 2014). It is thought that the lower in vivo bioavailability of berberine is closely related to extensive intestinal first-pass elimination, in which the drug is filtered out of the circulation by the liver resulting in a low level of systemic circulation (Guan et al., 2018). After orally administrated with 100 mg/kg berberine to rats, approximately half of berberine ran intact through the gastrointestinal tract and another half was disposed of by the small intestine, resulting in an extremely low extent of absolute oral bioavailability (0.36%) (Liu et al., 2010b). Additionally, a caco-2 cell monolayer model was used to confirm that berberine is the substrate for the drug transporter P glycoprotein, which may contribute to the lower absorption of berberine in small intestinal epithelial cells by passive diffusion (Zhang et al., 2011; Cui et al., 2015).
With its remarkable pharmacological activity, berberine has been used for a variety of diseases in the clinic. However, due to its low in vivo bioavailability, exploring methods that increase the concentration of berberine in blood is key to improving its usefulness in this context. Although intravenous administration provides a direct approach that may improve the bioavailability of berberine, this can lead to serious side effects including respiratory arrest (Han et al., 2021b). Therefore, berberine is often administered orally in clinic. Conversion of biological small molecules into salt compounds may be a method to improve its bioavailability in vivo. The bioavailability of berberine organic acid salts, especially berberine fumarate and berberine succinate, is higher than that of berberine hydrochloride (Cui et al., 2018). Moreover, chemical structure modification can be used to improve bioavailability of this drug. Long-chain alkylation (C5-C9) may enhance hydrophobicity, which has been shown to improve bioavailability; for example, 9-O-benzylation further enhances lipophilicity and imparts neuroprotective effect (Lin et al., 2020; Singh et al., 2021).
Distribution
It has been demonstrated that berberine is rapidly distributed through tissues in the liver, kidneys, muscle, lungs, brain, heart, pancreas, and fat, in descending order of amount, while the concentration of berberine in most of these tissues was higher than that in plasma 4 h after oral administration at a dose of 200 mg/kg in rats. Moreover, berberine concentrations remained relatively stable in liver, heart, brain, muscle, and pancreas tissue in rats (Tan et al., 2013).
However, recent studies on the distribution of berberine in vivo are rare, which may be attributed to the broad tissue distribution in vivo after oral administration. The availability of new technologies such as component analysis by high-performance liquid chromatography electrospray ionization mass spectrometry (HPLC–ESIMS)/mass spectrometry (MS) and MS imaging may permit improved exploration of the berberine tissue distribution (Jove et al., 2019). The fact that berberine is widely distributed in tissues may be useful in the treatment of some diseases, which may broaden the scope of its clinical application. For example, with the character of enrichment in the liver, oral treatment with 100 mg/kg berberine may promote the excretion of cholesterol from the liver to the bile (Li et al., 2015b). Thus, distribution of berberine may be an important pharmacokinetic property requiring further study in future.
Metabolism
One study used a sensitive HPLC-ESIMS/MS method to identify the metabolites of berberine in human plasma, of which berberrubine was most abundant, with high lipid solubility in individuals who received 15 mg/kg oral berberine chloride per day for 3 months (Spinozzi et al., 2014). Evidence showed that berberine had a similar metabolic profile in rats (100 mg/kg administered orally) and humans (300 mg administered orally three times a day for 2 days) via the urine (Qiu et al., 2008). Using liquid chromatography coupled with ion trap time-of-flight mass spectrometry, Ma et al. (2013) revealed that 16 separate metabolites could be identified in rat bile, urine, and feces samples after oral administration of berberine (200 mg/kg). After a single oral administration (48.2, 120, or 240 mg/kg) of berberine in rats, the levels of phase 2 metabolites were much higher than those of phase 1 metabolites for the AUC0–48 h values. Simultaneously, nine major metabolites of berberine (demethyleneberberine, jatrorrhizine-3-O-β-D-glucuronide, jatrorrhizine, berberrubine-9-O-β-D-glucuronide, jatrorrhizine-3-O-sulfate, berberrubine, thalfendine-10-O-β-D-glucuronide, demethyleneberberine-2-O-sulfate, and demethyleneberberine-2-O-β-D-glucuronide) were detected in rat serum using a LC–MS/MS method (Feng et al., 2021). Additionally, it was demonstrated that the metabolism of berberine by oral is closely related to liver function and gut microbiota. After oral administration of 300 mg/kg berberine in mice, cytochrome P3A11 (CYP3A11) and CYP3A25 mRNA and CYP3A11 and CYP2D22 enzyme activity levels were all found to be decreased, while the level of CYP1A2 mRNA was increased (Guo et al., 2011). Similarly, on oral administration of 200 mg/kg berberine in rats, the drug was shown to be metabolized in the liver by the CYP450 isoenzyme via oxidative demethylation at C2, C3, C9, and C10, followed by conjugation of the hydroxyl groups with glucuronic acid (Singh et al., 2021). Furthermore, gut microbiota can also affect the metabolism of berberine after oral administration. It was demonstrated that 200 mg/kg berberine administered orally could be converted into absorbable dihydroberberine by nitroreductases produced by gut microbiota, which showed a nearly 5-fold higher intestinal absorption rate than berberine in rats; the dihydroberberine is then oxidized back to berberine after absorption into the intestinal tissue, and enters the blood (Feng et al., 2015; Han et al., 2021a). Also, gut microbiota was shown to convert berberine into oxyberberine through an oxidation reaction in vitro and in vivo, which exerted a much stronger binding interaction with hemoglobin than plasma (Li et al., 2020a; Chen et al., 2021).
To summarize this section, the liver and intestine are the main metabolizing organs of berberine by oral administration. Inhibiting the first-pass effect may reduce the metabolism of berberine and improve its bioavailability. Interestingly, according to an in-depth study on the metabolism of berberine in vivo, it found that phase II metabolites are the major metabolic products of berberine (Feng et al., 2021), whereas the opposite was true in previous studies (Ma et al., 2013). In addition, particular attention should be paid to nitroreductases produced by gut microbiota, and berberine metabolism in general, in future studies, in order to fully establish the pharmacodynamic basis of this TCM.
Excretion
To better understand the poor absorption of berberine in vivo, some researchers have paid more attention to the excretion of berberine via the digestive tract. Berberine was found in feces with a recovery rate of 22.74% after a single oral dose (200 mg/kg) in 48 h, and thalifendine was the most abundant berberine metabolite excreted in the bile, urine, and feces in rats (Ma et al., 2013). In another study, 18.6% of the berberine was excreted in feces as berberrubine after intragastric administration at a single dose of 48.2 mg/kg. The total recovery of berberine and its metabolites from the urine, bile, and feces was 41.2% in rats (Feng et al., 2021). To summarize, berberine and its metabolites are mainly excreted by the kidneys (urine and feces) and bile in rats and mice (Liu et al., 2016).
Effects of Berberine on Vascular Diseases
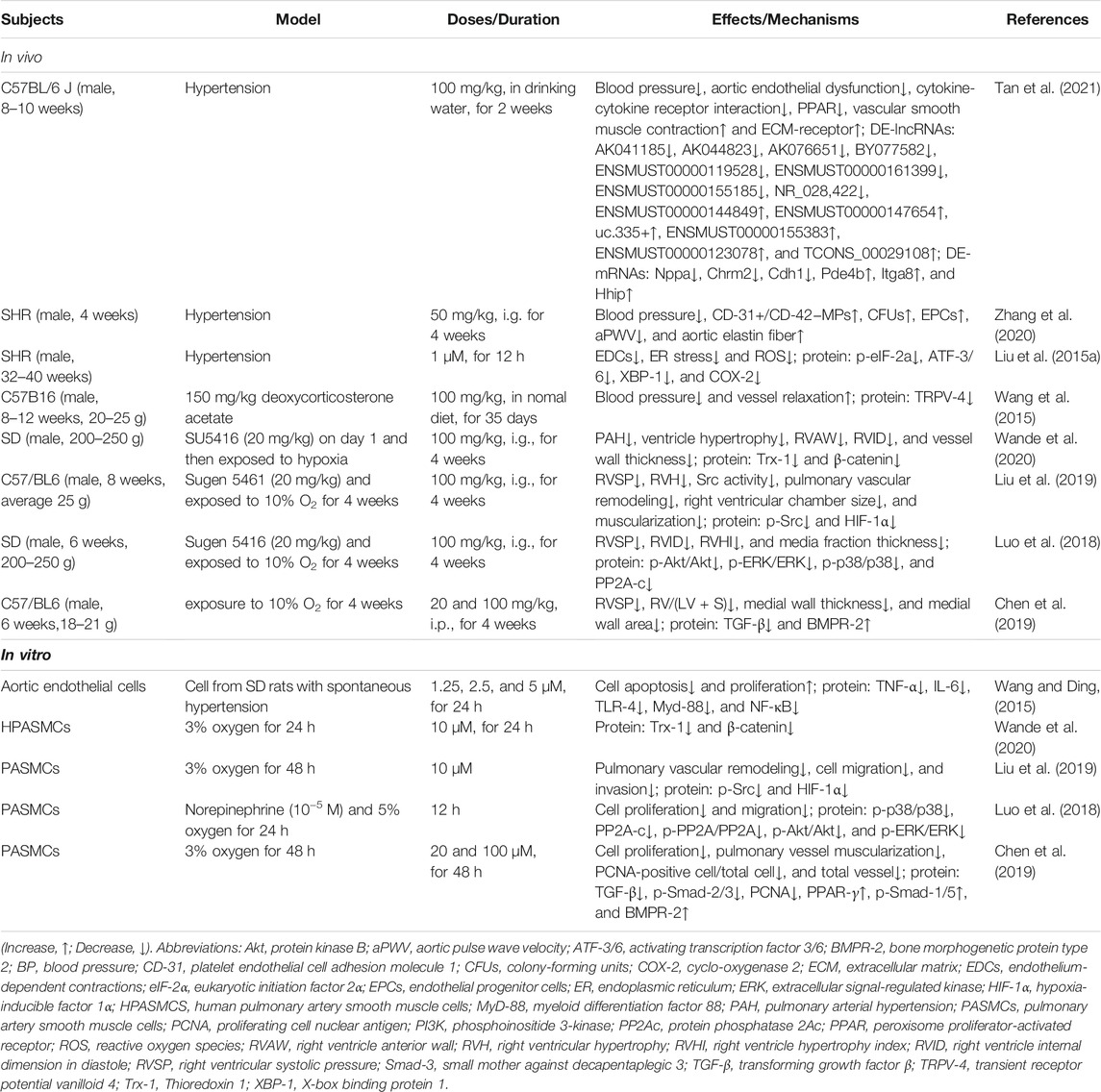
Recently, vascular protective effects of berberine have been reported in experimental studies of diverse vascular diseases. Berberine has shown promising vascular protection against atherosclerosis, cerebrovascular disease, hypertension, diabetes mellitus (DM), and intestinal vascular diseases. The pharmacological properties and molecular pathways of berberine are presented in Figure 2.

FIGURE 2. Biological activities and potential pathways of berberine on vascular diseases. Abbreviations: Akt, protein kinase B; AMPK, AMP-activated protein kinase; AP-1, activator protein 1; Bax, Bcl-2 associated X protein; Bcl-2, B-cell lymphoma 2; BMPR-2, bone morphogenetic protein type 2; ER, endoplasmic reticulum; ERK, extracellular signal-regulated kinase; HIF-1α, hypoxia-inducible factor 1α; JAK-2, janus kinase 2; MAPK, mitogen-activated protein kinase; MMP-2, matrix metalloprotease 2; NF-κB, nuclear factor κB; PI3K, phosphoinositide 3-kinase; SIRT-1, silent information regulator 1; STAT-3, signal transducer and activator of transcription 3; TGF-β, transforming growth factor β; TRPV-4, transient receptor potential vanilloid 4; VEGF, vascular endothelial growth factor; VSMCs, vascular smooth muscle cells.
Vasculature in Heart
Cardiovascular disease (CVD) is a major cause of morbidity and mortality worldwide (Huang et al., 2021). Studies indicate that the abnormal proliferation of vascular smooth muscle cells (VSMCs) is involved in the pathogenesis of CVD (Xiang et al., 2020; Zhang et al., 2021a). It has also been demonstrated that berberine (10, 30 and 100 μmol/L) could inhibit angiotensin IV-induced proliferation in cultured VSMCs by targeting the peroxisome proliferator-activated receptor α (PPAR-α)–nitric oxide (NO) signaling pathway (Qiu et al., 2017).
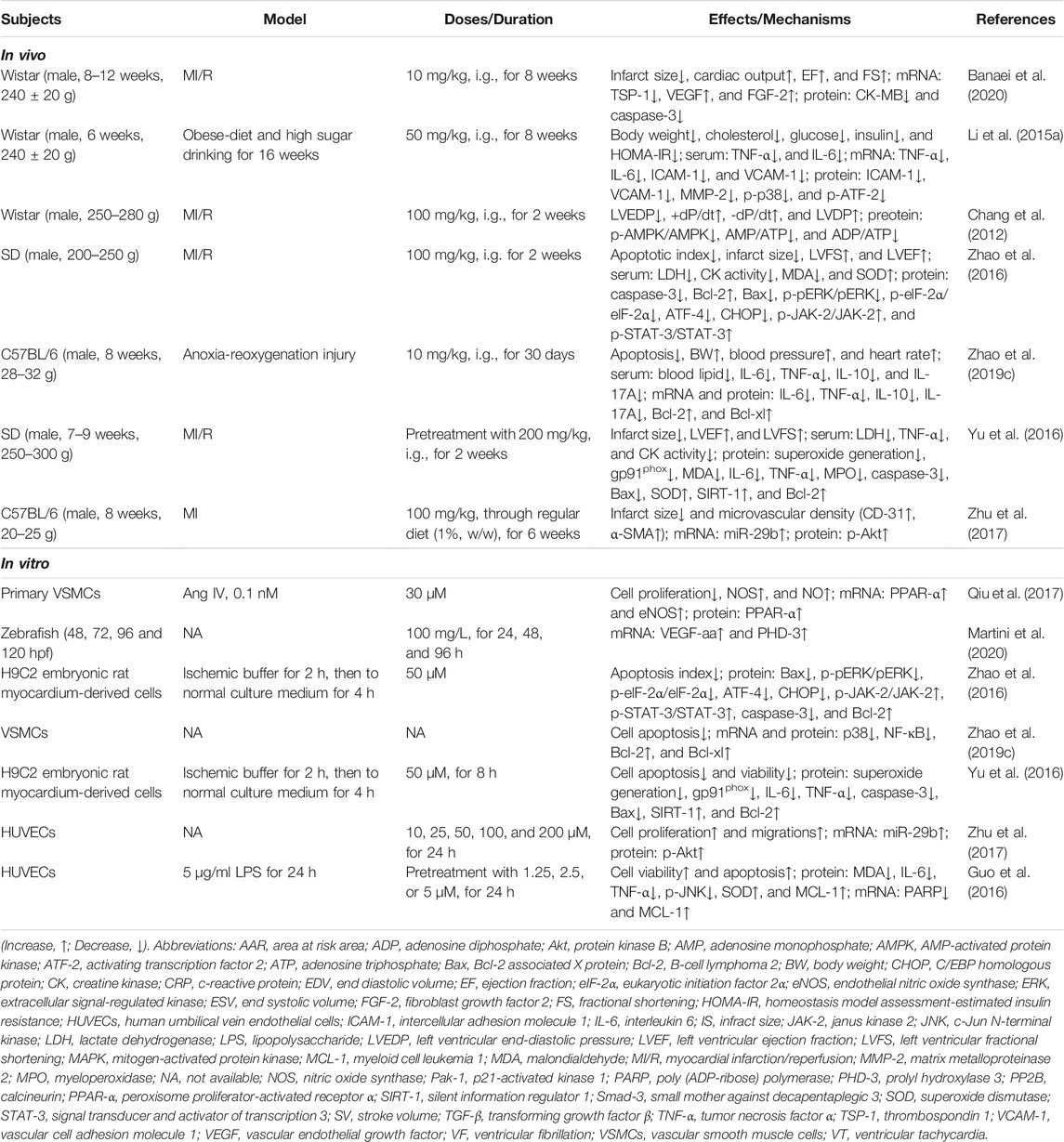
Myocardial Ischemia
Inflammation is one of the most observed cardiovascular conditions, and has a significant role in the progression of CVD (Golia et al., 2014; Lockshin et al., 2018). Aggravating inflammation may induce vascular remodeling after myocardial ischemia (MI), contributing to reduction of the ejection fraction and subsequent heart failure (Lu et al., 2015; Chong et al., 2021). It has been suggested that 50 mg/kg berberine may improve vascular inflammation and remodeling by inhibiting p38 mitogen-activated protein kinase (MAPK) activation, and activating transcription factor 2 phosphorylation (p-ATF-2) and matrix metalloprotease 2 (MMP-2) expression in rats (Li et al., 2015a). Protein hyperacetylation is associated with the development of MI (Treviño-Saldaña and García-Rivas, 2017; Aggarwal et al., 2020). Accumulating studies have demonstrated that silent information regulator 1 (SIRT-1) can regulate oxidative stress and inflammation to inhibit the development and progression of cardiac dysfunction in myocardial ischemia/reperfusion (MI/R) injury (Xue et al., 2020; Chang et al., 2021). Owing to its strong antioxidative and anti-inflammatory activities, oral administration of berberine (200 mg/kg) conferred cardioprotective effects in rats by improving post-MI/R cardiac function recovery and reducing infarct size after MI/R injury; the mechanism of action was found to be associated with the regulation of the SIRT-1 signaling pathway (Yu et al., 2016). As a selective barrier between tissue and blood, endothelial cells play a potential role in the control of inflammatory responses and homeostasis (Krüger-Genge et al., 2019). Endothelial cell dysfunction and/or injury can disrupt the integrity of the endothelial lining and subsequently lead to vascular disease, such as MI (Monteiro et al., 2019). Additionally, large experimental studies suggest that excessive inflammation can directly lead to endothelial cell apoptosis (Bravo-San Pedro et al., 2017; Henning et al., 2018). Lipopolysaccharide (LPS)-induced inflammation and apoptosis in human umbilical vein endothelial cells (HUVECs) were found to be inhibited by pretreatment with 5 μM berberine, mediated by inhibition of c-Jun N-terminal kinase (JNK) phosphorylation, and increased myeloid cell leukemia 1 (MCL-1) expression and superoxide dismutase (SOD) activity (Guo et al., 2016).
Angiogenesis, the formation of new blood vessels from preexisting ones, is indispensable for revascularization and cardiac remodeling following MI (Mathiyalagan et al., 2019; Chong et al., 2021; Tang et al., 2021). Ischemic heart disease is a leading cause of mortality and results from vascular cavity stenosis and occlusion (Garry et al., 2021). Rehabilitation of the myocardial ischemic region involves the activation of several stimulatory and inhibitory modulators of angiogenesis; the most notable of which are vascular endothelial growth factor (VEGF), fibroblast growth factor 2 (FGF-2), and thrombospondin 1 (TSP-1) (Detillieux et al., 2003; Frangogiannis et al., 2005; Martinez et al., 2018; Garikipati et al., 2019). Treatment with 10 mg/kg of berberine-rich extract (5 days a week by gavage) remarkably reduced heart infarct size, and increased the expression of angiogenesis-promoting factors in rats with MI/R injury, including VEGF, FGF-2 and TSP-1 (Banaei et al., 2020). In addition, microRNA plays a key role in many cardiac pathological processes, including MI (Parikh et al., 2020). Treatment with berberine in mice with MI injury was shown to lead to elevated miR-29b can activate the protein kinase B (Akt) signaling pathway, thus promoting angiogenesis and cell proliferation and migration to improve heart function (Zhu et al., 2017). A study in zebrafish embryos revealed that the level of VEGF-aa mRNA was up-regulated by berberine, which interfered with the angiogenic process, promoting bradycardia and reducing the cardiac output, atrial shortening fraction percentage, and atrial stroke volume (Martini et al., 2020). A complex hemodynamic pathological phenomenon exists in ischemia and reperfusion injury that can engage the metabolic and inflammatory machinery in the development of various disorders, including heart failure (Raza et al., 2020). Interestingly, intragastric administration of 100 mg/kg berberine daily for 14 days attenuated ischemia–reperfusion injury via hemodynamic improvements and inhibition of AMPK activity in both non-ischemic and ischemic areas of rat heart tissue (Chang et al., 2012).
Recent evidence has confirmed that endoplasmic reticulum (ER) stress is correlated with the development and progression of various heart diseases including cardiac hypertrophy, ischemic heart diseases, and heart failure (Wang et al., 2018). Prolonged ER stress, however, can become a leading cause of vascular endothelial cell dysfunction and apoptosis in CVD (Chen et al., 2020; Fatima et al., 2021). Oral administration of 200 mg/kg berberine daily for 2 weeks was reported to protect the heart from MI/R injury in rats by activating the janus kinase 2 (JAK-2)/signal transducer and activator of transcription 3 (STAT-3) signaling pathway, as well as by attenuating ER stress-induced apoptosis (Zhao et al., 2016). Alternatively, apoptosis and inflammation are correlated with anoxia-reoxygenation injury in CVD, which typically occurs during MI (Huang et al., 2018; Gan et al., 2020). The decreased inflammatory cytokines and myocardial cell apoptosis resulting from berberine administration may alleviate anoxia-reoxygenation injury by downregulating p38 MAPK-mediated nuclear factor κB (NF-κB) signaling pathway (Zhao et al., 2019c). In conclusion, given its robust anti-inflammatory, antioxidative stress, antiapoptotic, and anti-ER stress effects, berberine may effectively improve CDV and MI by inhibiting the MAPK, AMPK and NF-κB pathways and activating PPARα-NO, VEGF, and JAK-2/STAT-3 pathways (Figure 3 and Table 1).
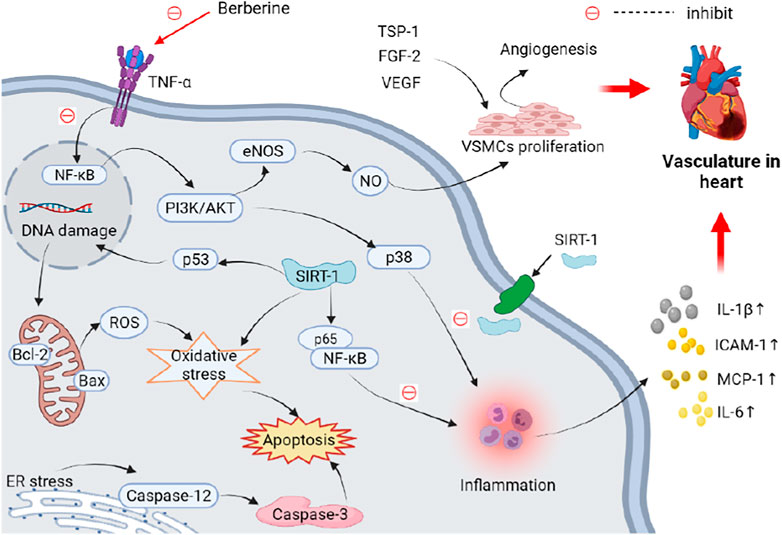
FIGURE 3. Schematic representation of the possible mechanism of anti-vasculature in heart activity of berberine. Elevated miR-29b can activate the Akt signaling pathway, thus promoting angiogenesis and cell proliferation and migration to improve vasculature in heart. Increased inflammation, oxidative stress, and ER stress can induce apoptosis of vascular endothelial cells. These adverse effects on vasculature in heart can be reversed by berberine. Abbreviations: Akt, protein kinase B; Bax, Bcl-2 associated X protein; Bcl-2, B-cell lymphoma 2; eNOS, endothelial nitric oxide synthase; ER, endoplasmic reticulum; FGF-2, fibroblast growth factor 2; ICAM-1, intercellular adhesion molecule 1; IL-1β, interleukin 1β; MAPK, mitogen-activated protein kinase; MCP-1, monocyte chemoattractant protein 1; NF-κB, nuclear factor κB; PI3K, phosphoinositide 3-kinase; ROS, reactive oxygen species; SIRT-1, silent information regulator 1; TNF-α, tumor necrosis factor α; TSP-1, thrombospondin 1; VEGF, vascular endothelial growth factor; VSMCs, vascular smooth muscle cells.
Atherosclerosis
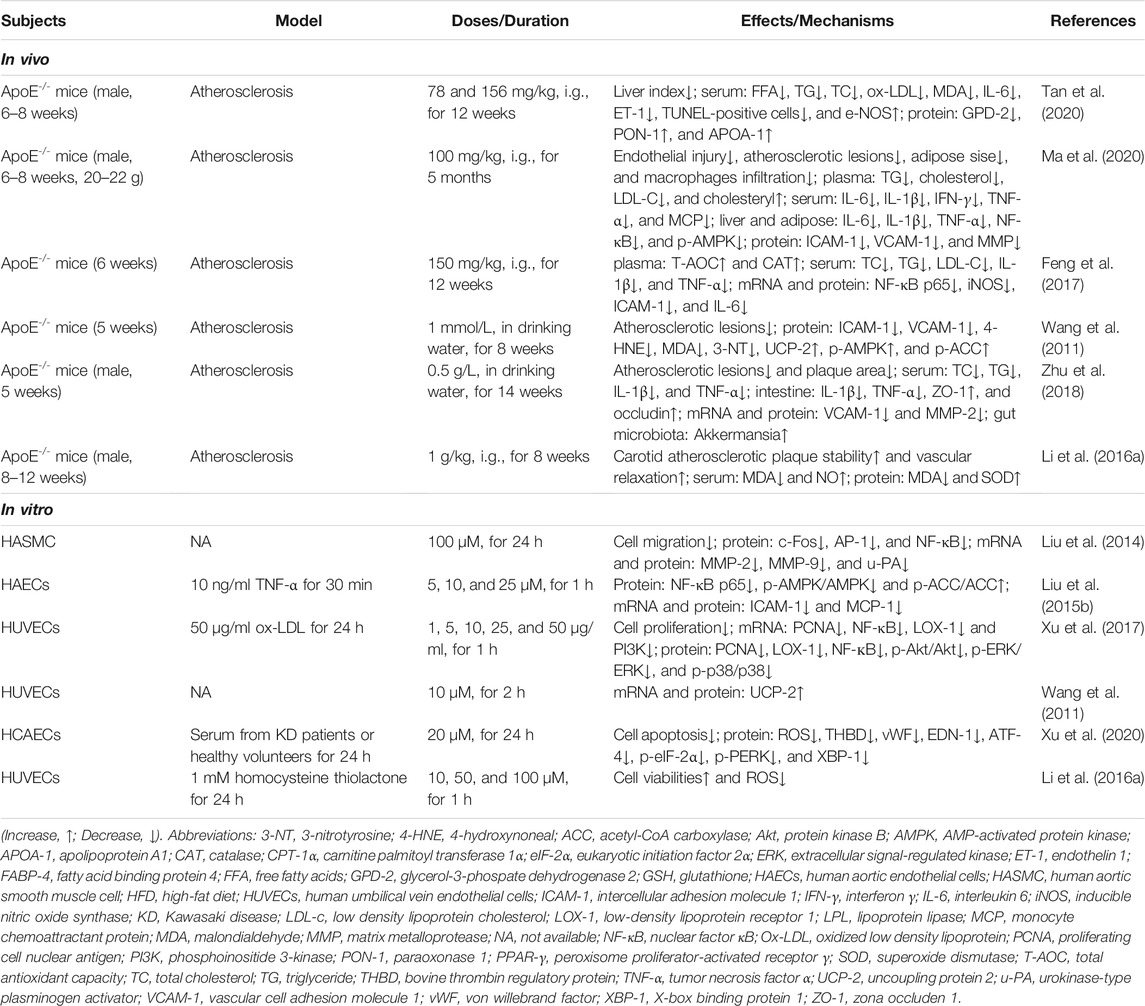
Atherosclerosis is a leading cause of death worldwide, and is characterized by lipid deposition, chronic inflammatory injury, smooth muscle cell proliferation, and plaque formation (Insull, 2009; Wolf and Ley, 2019). The pathological process of atherosclerosis begins with endothelial damage, accompanied by abnormal migration of VSMCs, leading to vascular remodeling (Sitia et al., 2010; Liang et al., 2020). Administration of 25, 50 and 100 μM berberine may suppress the expression of MMP-2, MMP-9 and urokinase-type plasminogen activator (u-PA) to significantly inhibit fetal bovine serum-induced human aortic smooth muscle cell (HASMC) migration, which may act to interrupt the activator protein 1 (AP-1) and NF-κB signaling pathways (Liu et al., 2014). Dysregulation of lipid metabolism is considered another major risk factor for atherosclerosis (Agrawal et al., 2018). An expert committee published the National Cholesterol Education Program in United States, emphasizing that low density lipoprotein (LDL) should be the primary target of cholesterol-lowering therapy in atherosclerosis (Tavares et al., 2021). In particular, clinical trials have demonstrated that lowering LDL levels can reduce the risk of atherosclerosis (Ference et al., 2017; Ji and Lee, 2021). Notably, the increased lipid in the serum and liver was reduced with the administration of berberine, which improved intima-media thickening, restored aortic endothelium-dependent vasodilatation, and alleviated atherosclerotic lesions in APOE(−/−) mice fed a western-type diet for 12 weeks (Tan et al., 2020). Similarly, berberine ameliorated high-fat diet (HFD)-induced hyperlipidemia and lipid accumulation in liver and adipose tissue, alleviated endothelial lesions and reduced the expression of inflammatory cytokines in the plasma of APOE(−/−) mice; it also reduced cholesteryl ester gathering in the aortic arch, resulting in ameliorated arterial plaque build-up via altered AMPK and NF-κB gene expression, and interrupted crosstalk between adipocytes and macrophages (Ma et al., 2020).
Tumor necrosis factor α (TNF-α) is a major proinflammatory factor in the development of vascular inflammation (Jang et al., 2017). Aberrant inflammatory responses may result in the ablation of macrophages, aggravation of vascular endothelial injury, and abnormal tissue proliferation in atherosclerosis (Hui et al., 2010; Brown et al., 2017). In vitro studies have indicated that TNF-α-induced inflammation, which causes excessive expression of intercellular adhesion molecule-1 (ICAM-1) and monocyte chemoattractant protein 1 (MCP-1) could be decreased by berberine in human aortic endothelial cells; this may be associated with inhibition of the NF-κB and AMPK pathways (Liu et al., 2015b). Oxidized LDL (ox-LDL) can act as an antigen to activate the immune inflammatory response, increasing the infiltration of inflammatory cells and the secretion of inflammatory factors in atherosclerosis (Lundberg et al., 2021). Ox-LDL-induced HUVEC proliferation and inflammatory responses were reversed with berberine, which lowered the expression of proliferating cell nuclear antigen (PCNA), NF-кB, and lectin-like oxidized low-density lipoprotein receptor 1 (LOX-1), and inhibited the phosphoinositide 3-kinase (PI3K)/Akt, extracellular signal-regulated kinase 1/2 (ERK-1/2), and p38 MAPK pathways (Xu et al., 2017). Ox-LDL has also been shown to injure endothelial cells directly, and contributes to endothelial dysfunction via overexpression of LOX-1, which induces a further rise in intracellular reactive oxygen species (ROS) (Kattoor et al., 2019; Akhmedov et al., 2021). Orally administrated at 156 mg/kg, berberine improved endothelial dysfunction by reducing aortic ROS generation and the release of inflammatory cytokines in the serum of a mouse model of atherosclerosis (Tan et al., 2020). Additionally, platelet–endothelial cell interactions potentiated by oxidative stress are thought to contribute to early atherosclerosis (Brown et al., 2021). Existing inflammatory and oxidative suppression of berberine prevented the development of the atherosclerotic plaque area by inhibiting translocation of NF-κB to the nucleus (Feng et al., 2017). Uncoupling protein 2 (UCP-2) is an inner mitochondrial membrane protein that belongs to the UCP family and plays an important role in lowering mitochondrial membrane potential and dissipating metabolic energy, preventing the accumulation of oxidative stress (Pierelli et al., 2017). Amazingly, treatment with 1 mmol/L berberine in drinking water led to suppression of oxidative stress and vascular inflammation by stimulating AMPK-dependent UCP-2 expression in mice with atherosclerosis (Wang et al., 2011). Moreover, recent studies found that the gut microbiota played a crucial role in atherosclerosis (Jonsson and Bäckhed, 2017; Verhaar et al., 2020). Another study emphasized that the modulation of gut microbiota, specifically the abundance of the Akkermansia bacterial genus, contributed to the antiatherosclerotic and metabolic protective effects of berberine by suppressing intestinal inflammation and promoting intestinal epithelial barrier integrity (Zhu et al., 2018).
Prolonged activation of the ER stress pathway can lead to aggravated oxidative stress and endothelial cell apoptosis (Tabas, 2010; Linton et al., 2016). Kawasaki disease (KD) is an acute febrile illness characterized by systemic vasculitis, especially in coronary arteries (de Ferranti et al., 2018). Berberine exerted its protective effects on KD-induced apoptosis of human coronary artery endothelial cells by inhibiting oxidative and ER stress (Xu et al., 2020). Endothelial cell apoptosis induced by ER stress is closely linked with plaque progression, which can contribute to unstable atherosclerotic plaques, perhaps in response to thrombosis in atherosclerosis (Yang et al., 2021). Homocysteine increases damage to vascular endothelial cells, thereby reducing vasodilation factors released by endothelial cells and impairing vasodilation in the endothelium, resulting in vascular endothelial apoptosis and inducing oxidation (Salvio et al., 2021). Nevertheless, an in vivo experiment has shown that berberine increased the stability of atherosclerotic plaques and mitigated detrimental effects of vascular endothelial cell activity experimentally induced by 50 mg/kg homocysteine thiolactone, and similar results are found in vitro study induced by 1 mM homocysteine thiolactone (Li et al., 2016a). Collectively, the studies presented here (Table 2) indicate that berberine may improve vascular endothelial damage, abnormal lipid metabolism, chronic inflammation, plaque formation, and cell apoptosis, thereby alleviating atherosclerosis (Figure 4).
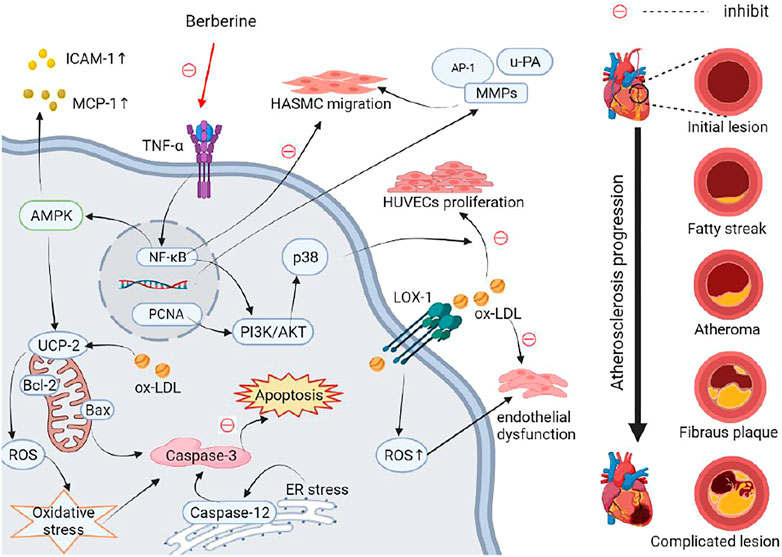
FIGURE 4. Schematic representation of the possible mechanism of anti-atherosclerosis activity of berberine. The dysregulation of lipid metabolism, vascular endothelial damage can induce abnormal migration of VSMCs, leading to vascular remodeling in atherosclerosis. Increased ox-LDL and LOX-1 cause vascular endothelial dysfunction. Inflammation leads to excessive expression of ICAM-1 and MCP-1, and aggravation of vascular endothelial proliferation and migration via up-regulating NF-κB and AMPK pathways. Inflammation, oxidative stress, and ER stress aggravate vascular endothelial cell apoptosis in atherosclerosis. These adverse effects on atherosclerosis can be reversed by berberine. Abbreviations: Akt, protein kinase B; AMPK, AMP-activated protein kinase; AP-1, activator protein 1; Bax, Bcl-2 associated X protein; Bcl-2, B-cell lymphoma 2; ER, endoplasmic reticulum; HASMC, human aortic smooth muscle cell; ICAM-1, intercellular adhesion molecule 1; LOX-1, low-density lipoprotein receptor 1; MAPK, mitogen-activated protein kinase; MCP-1, monocyte chemoattractant protein 1; MMPs, matrix metalloproteases; NF-κB, nuclear factor κB; Ox-LDL, oxidized low density lipoprotein; PCNA, proliferating cell nuclear antigen; PI3K, phosphatidylinositol 3-kinase; ROS, reactive oxygen species; TNF-α, tumor necrosis factor α; UCP-2, uncoupling protein 2; u-PA, urokinase-type plasminogen activator.
Cerebrovascular Diseases
Alzheimer’s Disease
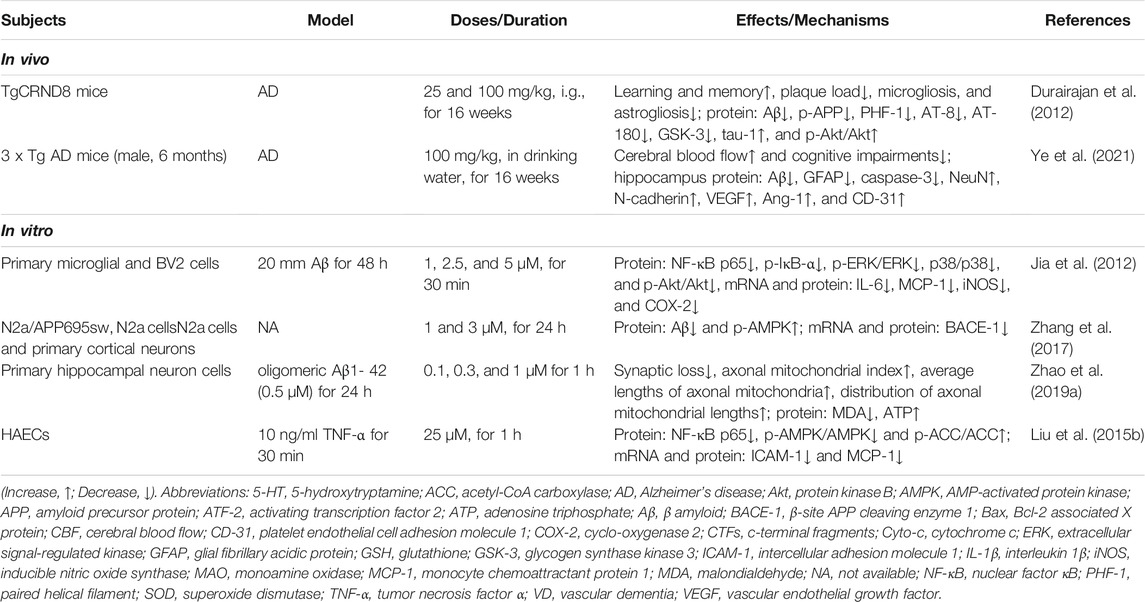
Alzheimer’s disease (AD) is a complex, aging-related, neurodegenerative disease, and the pathology process mainly involves β-amyloid (Aβ) overproduction and accumulation, tau hyperphosphorylation, and neuronal loss (Lian et al., 2016; Spangenberg et al., 2016; Gao et al., 2018). Administration of 0.5 μM berberine significantly suppressed Aβ-induced production of interleukin 6 (IL-6) and MCP-1 by inhibiting the activation of NF-κB and blocking the PI3K/Akt and MAPK pathways (Jia et al., 2012). Accumulated Aβ can result from abnormal processing of amyloid precursor protein (APP) in AD (O'Brien and Wong, 2011). APP C-terminal fragment levels and APP and tau hyperphosphorylation were decreased with 100 mg/kg berberine, administered by oral gavage for 4 months, via the Akt/glycogen synthase kinase 3 (GSK-3) pathway in rats with AD (Durairajan et al., 2012). Similarly, berberine modulates Aβ generation through activation of the AMPK pathway in N2a mouse neuroblastoma cells (Zhang et al., 2017). Moreover, elevated Aβ can mediate synaptic loss and dysfunction, another pathological hallmark of AD, by targeting mitochondria (Hong et al., 2016). Pretreatment with 1 μM berberine alleviated axonal mitochondrial abnormalities by preserving the mitochondrial membrane potential and preventing decreases in ATP, increasing axonal mitochondrial density and length, and improving mitochondrial motility and trafficking in 0.5 μM Aβ cultured hippocampal mouse neurons (Zhao et al., 2019a). Additionally, neuronal loss and cerebral blood flow contributed to dysfunction in memory and reward systems in AD (Dai et al., 2009; Nobili et al., 2017). Studies found that drinking water containing 100 mg/L berberine exerted a strong neuroprotective effect, improving cognitive deficits, inhibiting the apoptosis of neurons, and promoting the formation of micro-vessels by restoring cerebral blood flow and reducing Aβ accumulation in an APP/tau/PS-1 mouse model of AD (Ye et al., 2021). As shown in Table 3, the potential effects of berberine observed in the study suggest that it may effectively prevent AD by reducing accumulated Aβ. Few studies have focused on the improvement of tau hyperphosphorylation and neuronal loss in AD, which should thus be a focus of future research.
Vascular Dementia
Vascular dementia (VD) is the second most common form of dementia and is caused by vascular pathologies causing brain injury (Poh et al., 2021). In a rat model of VD induced by cerebral ischemia–reperfusion injury, increased angiogenesis was observed with berberine chloride (50 mg/kg) treatment, which may be due to the activation of hypoxia-inducible factor 1α (HIF-1α)/VEGF signal pathway (Liu et al., 2018). In general, few studies have focused on the relationship between berberine and vascular in VD. According to the development of new biological in recent years, imaging technology is conducive to strengthen the study of berberine and cerebrovascular diseases. Second near-infrared II (NIR-II) imaging, a kind of biomedical imaging technology with characteristics of high sensitivity, high resolution, and real-time imaging, can visualize the vasculature in the brain (Guo et al., 2019a). Therefore, we can directly utilize the NIR-II to observe the improvement of the vascular in the brain by treatment with berberine.
Hypertension
An epidemiological investigation showed that the incidence of hypertension increases with age across all countries, regions, or ethnicities, and is generally higher in industrialized countries than developing countries (Zhou et al., 2021). Hypertension is more common in the elderly, and mostly manifests as simple systolic hypertension; however, it is increasing in younger age groups (James et al., 2014; Zhang and Moran, 2017). Among the many mechanisms underlying arterial stiffness, endothelial dysfunction is believed to be a critical determinant for its onset and progression (Kostov and Halacheva, 2018; Safar, 2018). Owing to arterial stiffness, elevated arterial blood pressure can contribute to both extracellular matrix (ECM) deposition and remodeling or enhanced contractility or stiffness of VSMCs (Bertorello et al., 2015). In vitro, berberine (at concentrations of 1.25, 2.5, and 5 μM) considerably inhibited aortic endothelial cells in spontaneous hypertensive rats (SHRs) by suppressing cell proliferation, apoptosis, and down-regulating the expression of Toll-like receptor 4 (TLR-4), myeloid differentiation protein 88 (MYD-88), NF-κB, IL-6, and TNF-α (Wang and Ding, 2015). Numerous studies have verified that vascular endothelial cell dysfunction and lncRNA activity may together be associated with hypertension (Lorenzen and Thum, 2016; Konukoglu and Uzun, 2017). The levels of five lncRNAs were found to be modulated by the administration of 100 mg/kg berberine in mice with hypertention, which may preserve vascular endothelial cell function (Tan et al., 2021). Endothelial microparticles (EMPs) are extracellular vesicles that are shed by the endothelium as a result of activation, injury, or apoptosis of endothelial cells, and are considered important biomarkers of the status of endothelial cells and vascular function (Sun et al., 2016). Endothelial progenitor cells (EPCs) mobilized from bone marrow can migrate to the peripheral blood and differentiate into mature endothelial cells, contributing to endothelial recovery (Pyšná et al., 2019). One study found that EPC number and activity was significantly reduced among people with hypertension when compared to healthy individuals, and low circulating levels of EPCs may contribute to endothelial dysfunction (Waclawovsky et al., 2021). Abnormal circulating EMPs and EPCs in SHRs were ameliorated by berberine treatment associated with endothelial dysfunction and arterial stiffness in SHRs (Zhang et al., 2020). Moreover, the production of NO caused by oxidative stress, aging, and spontaneous hypertension increases endothelium-dependent contractions (EDCs), contributing to blunted endothelium-dependent vasodilation (Vanhoutte et al., 2005; Vanhoutte et al., 2017). Continuous ER stress can exert detrimental effects through a maladaptive, unfolded protein response, resulting in cellular defects and disturbed vascular function (Ren et al., 2021). However, incubation with 1 μM berberine has been shown to reduce EDCs by activating the AMPK pathway, thus inhibiting ER stress and ROS generation, leading to cyclo-oxygenase 2 (COX-2) downregulation in SHR carotid arteries (Liu et al., 2015).
Ca2+ signals regulate vascular function in endothelial cells; Ca2+ release from the ER and/or Ca2+ influx through ion channels at the endothelial cell membrane results in endothelium-dependent vasodilation and diminished vascular resistance (Cook et al., 2012; Ottolini et al., 2019; Wang et al., 2021). Notably, endothelial transient receptor potential vanilloid 4 (TRPV-4) channels are associated with hypertension, as they regulate Ca2+ concentrations (Ottolini et al., 2020). Long-term administration of berberine has been shown to directly induce vasorelaxation, decreasing blood pressure and vascular stiffness, by suppressing the activity of TRPV-4 channels (Wang et al., 2015). Additionally, mechanical stretching forces increase the proliferation and apoptosis of VSMCs by activating the protein disulfide isomerase (PDI) redox system. Berberine has been shown to inhibit the PDI ER system and the MAPK pathway, thereby attenuating the simultaneous increases in VSMC proliferation and apoptosis observed in response to mechanical stretching during hypertension (Wang et al., 2020). Collectively, these results demonstrate that berberine may effectively ameliorate endothelial dysfunction, arterial stiffness, and vascular remodeling, resulting in reduced hypertension, and which the mechanism may be related to the inhibition of ER stress and activation of the AMPK pathway. An increasing number of studies on hypertension have focused on the Ca2+ and TRPV-4 pathways in recent years (Table 4).
Pulmonary Arterial Hypertension
Pulmonary arterial hypertension (PAH) is closely associated with extensive vascular remodeling, especially pulmonary arterial medial hypertrophy and muscularization, due to aberrant proliferation of pulmonary artery smooth muscle cells (PASMCs) resulting from hypoxia (Bisserier et al., 2021; Sharifi Kia et al., 2021). Hemodynamic and pulmonary pathological data showed that chronic hypoxia notably elevated the median width of pulmonary arterioles (Choudhary et al., 2011; Khoramzadeh et al., 2019). However, berberine substantially decreased pulmonary vascular remodeling in mice with hypoxia-induced PAH by inhibiting Akt/mammalian target of rapamycin (mTOR)/HIF-1α and transforming growth factor β (TGF-β) pathways, and activating bone morphogenetic protein type 2 (BMPR-2) receptor (Chen et al., 2019; Liu et al., 2019). Wande et al. (2020) demonstrated substantial proliferative activities in hypoxia-induced human PASMCs, were possibly mediated by berberine (at concentrations of 10 μM) via inhibiting the thioredoxin (TRX-1) and β-catenin pathways. Activation of protein phosphatase 2A (PP2A) has been shown to induce apoptosis of PASMCs in people with PAH (Ferron et al., 2011). Berberine may prominently attenuate proliferation and migration of PASMCs induced by norepinephrine, alleviating PAH via PP2A pathway (Luo et al., 2018). These results together show that berberine significantly suppresses pulmonary vascular remodeling and proliferation of vascular endothelial cells in PAH; the antiproliferative and antiapoptotic effects may be mediated by inhibition of the Akt/mTOR/HIF-1α and PP2A pathways (Table 4).
Diabetes Mellitus and its Complications
Diabetes Mellitus
The main cause of DM and associated complications is a low level or lack of pancreatic islet function, including insulin resistance, resulting in disordered glucose metabolism in the body (Pearson, 2019; Han et al., 2021b). Sustained hyperglycemia progresses to various diabetic microangiopathies, including diabetic cardiovascular disease, nephropathy, neuropathy and retinopathy (Reddy et al., 2015; Montero et al., 2019; Tang and Yiu, 2020). Chronic inflammation caused by hyperglycemia is a major feature of DM (Saltiel and Olefsky, 2017). Adipose tissue macrophages (ATMs), including M1 ATMs, can induce inflammatory responses by producing pro-inflammatory cytokines such as TNF-α and IL-6, thus contributing to the induction of insulin resistance in DM (Russo and Lumeng, 2018). Oral berberine (50 mg/kg/day) markedly improved insulin resistance, reduced the inflammation and JNK, IKK-β, and NF-κB p65 phosphorylation by inhibiting M1 macrophage activation in adipose tissue (Ye et al., 2016). Owing to increased aldose reductase (AR) and NADPH oxidase (NOX) activities, platelet hyperreactivity and apoptosis during DM accounts for the accumulation of ROS (Vara et al., 2019; Ajjan et al., 2021). It was demonstrated that 50 mM glucose induced platelet aggregation, apoptosis and superoxide production, which was neutralized by 25 and 50 μM berberine via inhibiting of AR, NOX and GSH reductase activities (Paul et al., 2019). Similarly, 25 μM berberine had protective effects against endothelial injury by attenuating the generation of ROS, cellular apoptosis, NF-κB activation, and expression of adhesion molecules, which were induced by high glucose levels; it also enhanced the endothelium-dependent vasodilatation through the activation of the AMPK pathway (Wang et al., 2009).
Advanced glycation end products (AGEs) are produced via the nonenzymatic glycation reaction and are considered major pathogenic factors that trigger vascular complications in diabetes (Azegami et al., 2021). Incubation with 5 or 10 μg/ml berberine significantly inhibited AGE formation in high-glucose-AGEs-induced micro-endothelial injuries (Hao et al., 2011). Diabetic peripheral neuropathy, characterized by perivascular neuropathy, is reported to be involved in vascular disorders associated with diabetes (Olesen et al., 2021). The mesenteric artery, a part of the splanchnic circulation system, is involved in the regulation of arterial pressure (van Dijk et al., 2020). The iliac artery is mainly responsible for blood supply to the lower extremities and pelvic organs (Maier et al., 2020). Both of these sites are predisposed to large vascular lesions in diabetes. Oral administration of 200 mg/kg berberine markedly enhanced the nitrergic neural activity in the superior mesenteric artery and diminished the adrenergic function in the iliac artery, resulting in vasodilatation in diabetic rats (Geng et al., 2016; Zhao et al., 2019b).
Intracellular Ca2+, which is tightly controlled by Ca2+ channels and transporters, is an important messenger in VSMC dedifferentiation (Nagel et al., 2006). Elevated concentrations of intracellular Ca2+ is a primary stimulus for smooth muscle contraction; it is reported that diabetic vascular dysfunction is tightly coupled to the impairment of intracellular Ca2+ processing in VSMCs (Searls et al., 2010; Yang et al., 2020). Impaired cerebral arterial vasodilation can be alleviated by berberine in a diabetic rat model via down-regulation of the intracellular Ca2+ processing of VSMCs (Ma et al., 2016). Hyperglycemia and hypertension are the two primary risk factors for vascular disease in diabetic patients (Cryer et al., 2016; Petrie et al., 2018). Increases in intracellular Ca2+ along with decreases in K+ can lower the membrane potential and enhance the vasoconstriction response and the proliferation of VSMCs, leading to hypertension (Seki et al., 2017; Sun et al., 2021). Chronic administration of 100 mg/kg berberine reduced blood pressure and improved vasodilation in diabetic rats by activating the Ca2+-activated K+ channel (Ma et al., 2017). Aberrant miR-133a expression in endothelial cells induces endothelial dysfunction and impaired endothelium-dependent vasodilation, aggravating the pathogenesis of cerebrovascular diseases (Li et al., 2016b). Administration of berberine (1.0 g/kg for 8 weeks) reduced miR-133a expression and impairments in learning and memory, increasing the vasodilation in the middle cerebral artery to improve VD associated with diabetes (Yin et al., 2019). Furthermore, existing evidence suggests that hyperglycemia and hypoxia can trigger cerebrovascular dysfunction (Lefferts et al., 2016; Jin et al., 2019). Berberine at a concentration of 30 μM counteracted the attenuating effects of hypoxic/high-glucose conditions on the proliferation and migration of rat brain microvascular endothelial cells, which was in part mediated by the SIRT-1/HIF-1α/VEGF pathway (Mi et al., 2019). According to these studies, berberine had a hypoglycemic effect through improving insulin resistance, and has robust anti-inflammatory, antiapoptotic and antiendothelial injury effects in DM. Berberine appears to improve endothelial dysfunction by regulating Ca2+ and K+ channels in DM (Table 5).
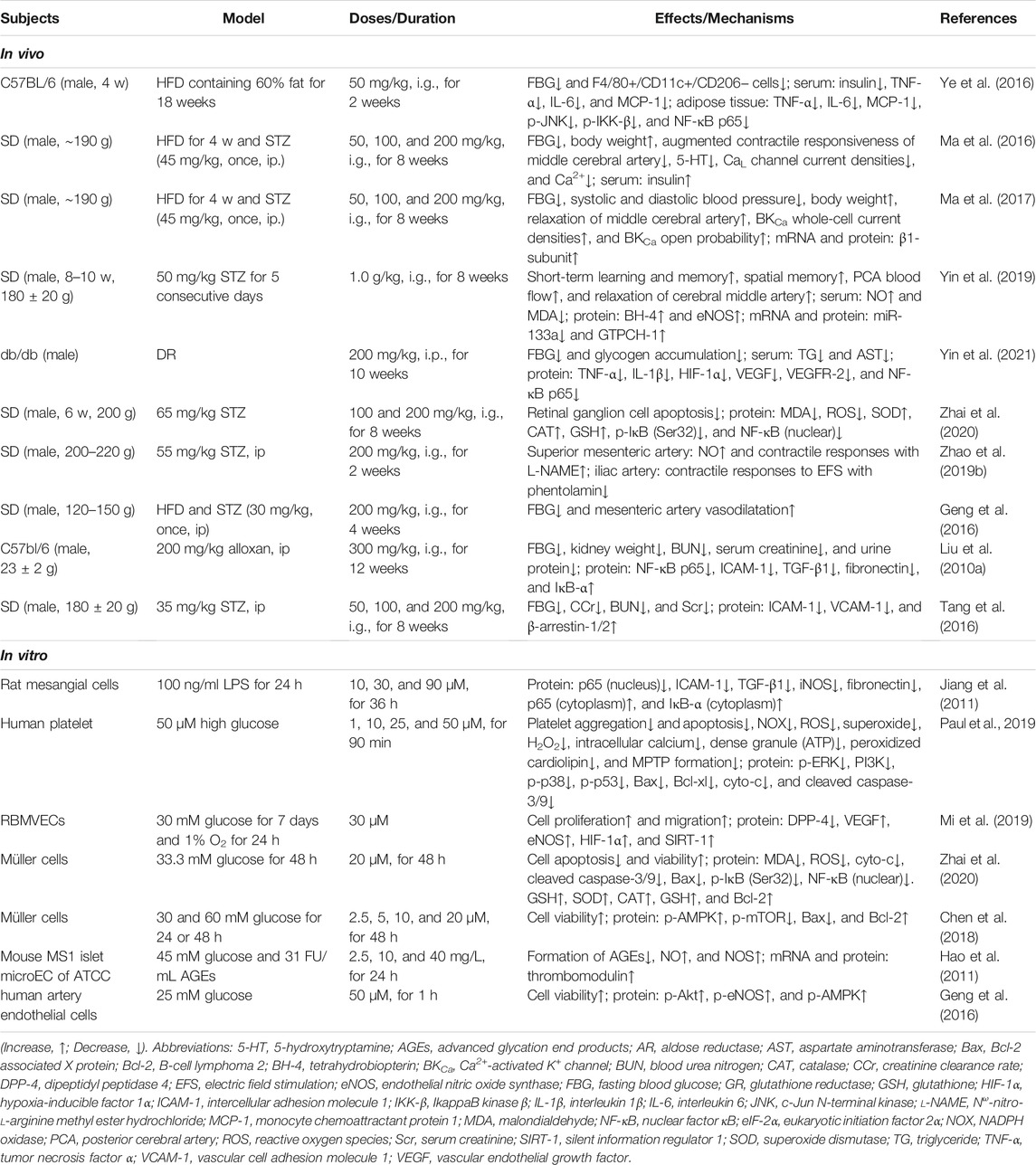
TABLE 5. The in vivo and in vitro mechanism of berberine in the treatment of DM and its complications.
Diabetic Retinopathy
Diabetic retinopathy (DR) is a retinal microvascular disease caused by chronic hyperglycemia leading to angiogenesis in retina (Ai et al., 2019). In recent years, improvement of disordered glucolipid metabolism is considered one of the most effective strategies for the treatment of DM and its complications (Zhao et al., 2021b). Berberine has been shown to block DR development by modulating the glucolipid metabolism and inhibiting the HIF-1α/VEGF/NF-κB pathway (Yin et al., 2021). The pathological processes involved in DR may be related to increased levels of pro-inflammatory factors, leading to oxidative stress and the apoptotic cascade (Ai et al., 2020; Robles-Rivera et al., 2020; Gong et al., 2021). Berberine may deactivate the NF-κB pathway, thus suppressing oxidative stress and cell apoptosis in DR (Zhai et al., 2020). As a major energy receptor and metabolic regulator, AMPK is one of the therapeutic targets for metabolic and vascular diseases (Lu et al., 2019). 10 or 20 μM berberine was shown to have therapeutic effects, protecting Müller cells from 30 mM glucose-induced apoptosis by enhancing autophagy and activating the AMPK/mTOR pathway in DR (Chen et al., 2018). These results together indicate that berberine could attenuate the pathogenesis of DR, mainly through regulating the HIF-1α/VEGF/NF-κB and AMPK/mTOR pathways to inhibit microvascular proliferation, oxidative stress and apoptosis (Table 5).
Diabetic Nephropathy
Diabetic nephropathy (DN), one of the most serious microvascular complications of DM, is the leading cause of end-stage renal failure (Lai et al., 2018). The early stage of DN is mainly characterized by abnormal renal hemodynamics, which mainly manifests as decreased vascular resistance in the glomerulus (Toledo et al., 2015). Research has shown that accumulation of ECM production in the glomerular mesangial membrane may be related to NF-κB pathway (Gong et al., 2020). The ameliorative effects of berberine (300 mg/kg) on ECM accumulation may be due to decreased TGF-β1 and ICAM-1 resulting from inhibition of the NF-κB pathway, as shown in a rat model of DN (Liu et al., 2010a). Recent studies have shown that abnormal levels of β-arrestins, including β-arrestins 1 and 2, have a role in microvascular permeability by regulating the production and function of ICAM-1 and vascular cell adhesion molecule 1 (VCAM-1) in the kidneys of a rat model of DN (Noh et al., 2017; Zhang et al., 2018). Orally administration of 100 or 200 mg/kg berberine had renoprotective effects owing to decreased ICAM-1 and VCAM-1 levels and increased β-arrestin 1 and 2 in kidneys of a rat model of DN (Tang et al., 2016). Additionally, inflammation in the kidney is another aggravating factor renal vascular damage in DN (Moreno et al., 2018). Berberine may attenuate LPS-induced inflammation and extracellular matrix accumulation via the NF-κB signaling pathway (Jiang et al., 2011). Given its robust antihyperglycemic and anti-inflammatory activities, and its inhibitory effect on angiogenesis, berberine should be considered a candidate drug for DN (Table 5).
Intestinal Vascular Diseases
The intestinal mucosal microvasculature is located underneath the intestinal epithelial layer and accurately regulates the passage of molecules across the gut-vascular barrier (GVB) (Zhong et al., 2021). The rat cecal ligation and puncture (CLP) sepsis model was orally treated with berberine (25 and 50 mg/kg for 5 days) showed a protective effect on GVB function in sepsis through the reduction of gut vascular permeability and the suppression of WNT/β-catenin pathways (He et al., 2018). High-density lipoprotein (HDL) particles are related to apoprotein M (ApoM) which is the main carrier of plasma sphingosine-1-phosphate (S1P) (Tavernier et al., 2020). Though only a small proportion of HDL contains ApoM, ApoM-bound S1P is important in maintaining vascular integrity and inhibiting vascular inflammation (Galvani et al., 2015). In a model of polymicrobial sepsis, berberine removed damaged GVB resulting from TLR4-mediated hyperglycemia, insulin resistance and proinflammatory molecule production, thus enriching ApoM gene expression and plasma ApoM via activating the ApoM/S1P pathway (Li et al., 2020b). A previous study showed that the neonatal small intestine is prone to necrotizing enterocolitis (NEC), a severe acquired disease characterized by inflammation (MohanKumar et al., 2019). However, these changes were notably reversed by treatment with berberine; the anti-inflammatory mechanism of berberine in this context may act via suppression of the PI3K/Akt pathway (Fang et al., 2018). Peritoneal adhesions are fibrous tissues that tether organs to one another or to the peritoneal wall and are a major cause of postsurgical morbidity (Tsai et al., 2018). In the normal healing process, ECM can be completely degraded by the proenzyme MMP (Altoé et al., 2021). Berberine prevented adhesion reformation, promoting the activation of MMP-3 and MMP-8 by directly blocking tissue inhibitor of metalloproteinase-1 (TIMP-1) activation in fibroblasts (Liu et al., 2020). To summarize, berberine can inhibit endothelial and gut vascular permeability, inflammation and adhesion reformation in intestine; it may act through several pathways, including the WNT/β-catenin, ApoM/S1P and PI3K/Akt pathway (Table 6).
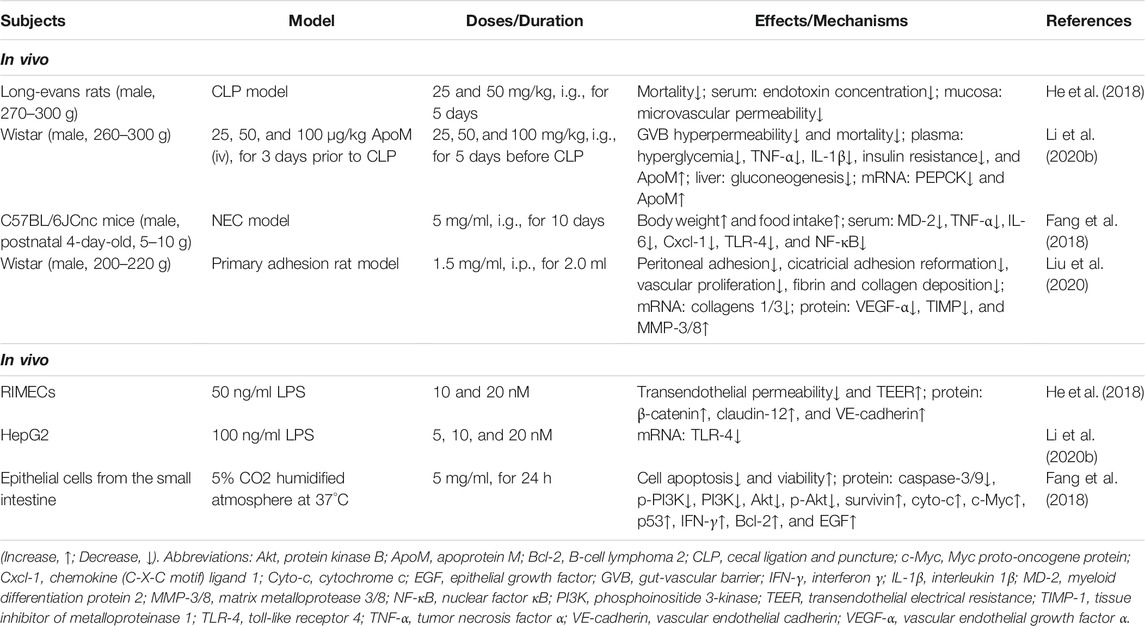
TABLE 6. The in vivo and in vitro mechanism of berberine in the treatment of intestinal vascular diseases.
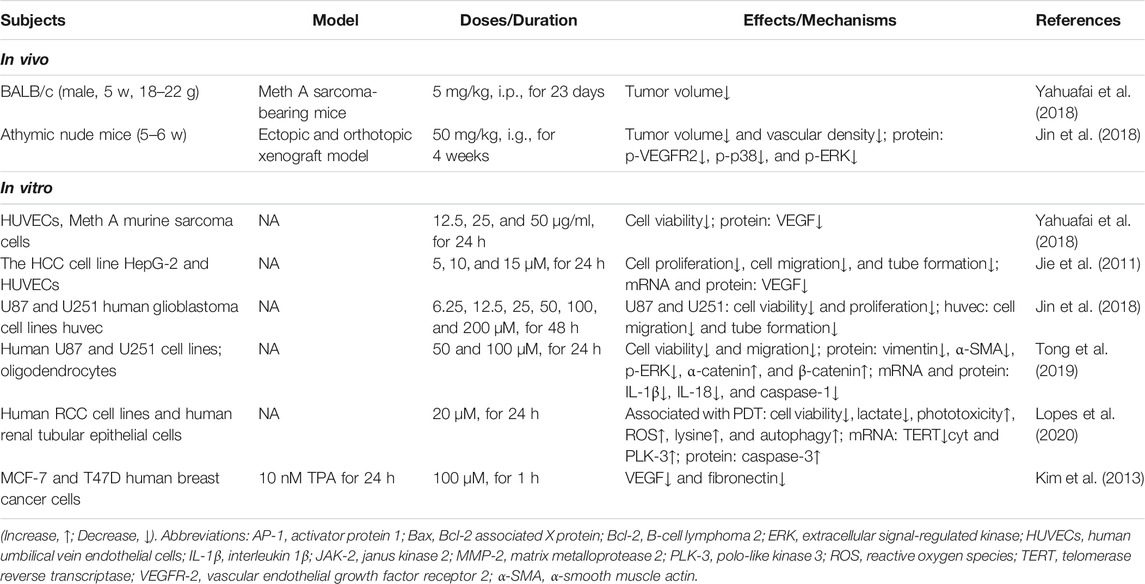
Vasculature in Cancer
Angiogenesis is a process in which new blood vessels form and grow from pre-existing vessels; this process occurs under healthy and pathological conditions, such as cancer (Fang et al., 2021). VEGF promotes angiogenesis in endothelial cells. Berberine has been shown to suppress angiogenic action, HUVEC proliferation and migration, by inhibiting VEGF, against cancerous Meth A cells and hepatocellular carcinoma (Jie et al., 2011; Yahuafai et al., 2018). VEGF-2 is a major mediator of the biological effects of VEGF, and therefore plays an important role in tumor angiogenesis (Sharaky et al., 2020). Berberine was shown to inhibit angiogenesis in glioblastoma xenografts by targeting the VEGFR-2/ERK pathway (Jin et al., 2018). In tumor development, chronic inflammation leads to a sharp increase in VEGF expression (Crusz and Balkwill, 2015). Elevated inflammatory cytokine levels and epithelial–mesenchymal transition in glioma cells were shown to be reversed by 100 μM berberine; the mechanism for this may be via suppressing ERK-1/2 signaling and production of IL-1β and IL-18 (Tong et al., 2019). VEGFR-3 in lymphatic endothelial cells were essential for the development of VSMCs (Antila et al., 2017). Clinically, elevated levels of VEGFR-3 are thought to be correlated with cancers resulting from metastasis via the lymph nodes, such as renal carcinoma (Guida et al., 2014). Following an inflammatory stimulus, the production of ROS by oxidative stress and energy deficit at mitochondrial, lysosomal, or ER loci can directly lead to irreversible damage of tumor cells and initiate cell apoptosis and autophagy (Reuter et al., 2010). Combined with photodynamic therapy, 20 μM berberine triggered metabolite changes in renal carcinoma cells, resulting in inhibited cell proliferation, tumorigenesis, and angiogenesis, and inducing autophagy and apoptosis via increased ROS generation (Lopes et al., 2020). Another study implied that 12-O-tetradecanoyl phorbol-13-acetate (TPA) significantly increased the level of VEGF and fibronectin in both MCF7 and T47D breast cancer cells (Kim et al., 2009). TPA-induced VEGF and fibronectin expression was decreased by berberine treatment, via inhibition of the PI3K/A pathway, in breast cancer cells (Kim et al., 2013). Taken together, these results show that berberine may effectively inhibit the proliferation and angiogenesis of tumor cells by inhibiting VEGF, ERK and PI3K/Akt pathways and promote the apoptosis of tumor cells (Table 7).
Other Vascular Diseases
Rheumatoid arthritis (RA) is a chronic inflammatory autoimmune disease that may involve angiogenesis, particularly during the earliest stages of the disease (Yang et al., 2018; Lyu et al., 2021). Angiogenesis is strictly regulated by several pro- and antiangiogenic factors including VEGF, which have been suggested to be involved in neovascularization in RA joints (Li et al., 2018a). Berberine was shown to have anti-inflammatory and antiangiogenic effects in a rat model of RA by decreasing the level of inflammatory factors, and suppressing p-ERK, p-p38 and p-JNK activation (Wang et al., 2014). Additionally, it is reported that doxorubicin-induced vascular congestion and inflammatory cell infiltration in the liver were largely attenuated by berberine pretreatment (Zhao et al., 2012).
Conclusion and Perspectives
Berberine is a multifunctional, natural product with therapeutic potential in vascular diseases, including cardiovascular disease, atherosclerosis, hypertension, cerebrovascular disease, diabetes and associated complications, intestinal vascular disease and cancer (Zhu et al., 2018; Martini et al., 2020; Yin et al., 2021). The present review has shown the excellent protective effect of berberine in diverse vascular diseases by preserving vascular endothelial cells, improving vascular remodeling and vasoconstriction, and suppressing inflammation, oxidative stress, autophagy, and apoptosis, based on recent in vitro and in vivo experimental reports (Figure 2). Moreover, berberine also modulates the concentration of Na+, Ca2+ and lipid metabolism in the VSMCs (Table 4). What is more, the network diagram of “vascular diseases-target-pathways” was shown in Figure 5, and the underlying mechanism of berberine in the treatment of vascular diseases mentioned in this paper may be related to multiple pathways, including HIF-1α/VEGF, STAT, MAPK, NF-κB, SIRT, PI3K/Akt, AMPK and TRPV-4.
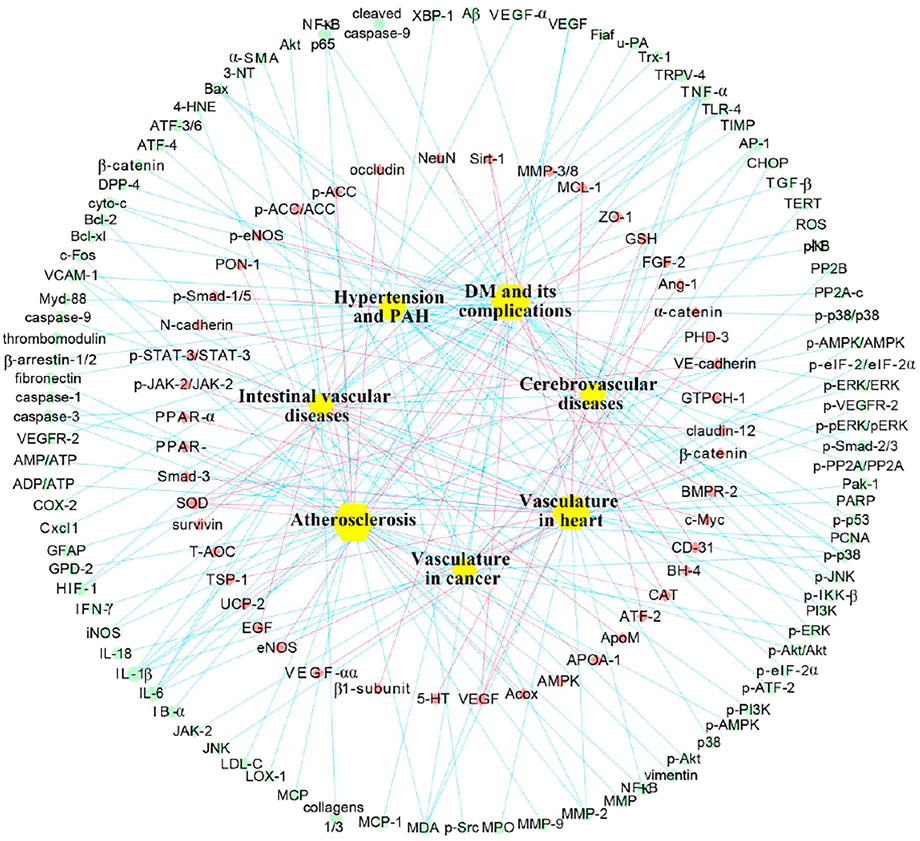
FIGURE 5. Network diagram of berberine involved gene and protein targets in treating vascular diseases. The yellow cubes in the innermost circle are the vascular disease treated with berberine, the red dots in the middle circle represent the up-regulated gene and protein targets, and the blue dots in the outside circle denote the down-regulated gene and proteins. Abbreviations: 3-NT, 3-nitrotyrosine; 4-HNE, 4-hydroxynoneal; 5-HT, 5-hydroxytryptamine; ADP, adenosine diphosphate; Akt, protein kinase B; AMP, adenosine monophosphate; AMPK, AMP-activated protein kinase; AP-1, activator protein 1; APOA-1, apolipoprotein A-1; ApoM, apoprotein M; ATF-4, activating transcription factor 4; ATP, adenosine triphosphate; Bax, Bcl-2 associated X protein; Bcl-2, B-cell lymphoma 2; BH-4, tetrahydrobiopterin; BMPR-2, bone morphogenetic protein type 2; CAT, catalase; CD-31, platelet endothelial cell adhesion molecule 1; CHOP, C/EBP homologous protein; CLP, cecal ligation and puncture; c-Myc, Myc proto-oncogene protein; COX-2, cyclo-oxygenase 2; CPT-1α, carnitine palmitoyl transferase 1α; Cyto-c, cytochrome c; DM, diabetes mellitus; DPP-4, dipeptidyl peptidase 4; EGF, epithelial growth factor; eIF-2α, eukaryotic initiation factor 2α; eNOS, endothelial nitric oxide synthase; ERK, extracellular signal-regulated kinase; FABP-4, fatty acid binding protein 4; FGF-2, fibroblast growth factor 2; GFAP, glial fibrillary acidic protein; GPD-2, glycerol-3-phospate dehydrogenase 2; GSH, glutathione; HIF-1α, hypoxia-inducible factor 1α; IFN-γ, interferon γ; IKK-β, IkappaB kinase β; IL-6, interleukin 6; iNOS, inducible nitric oxide synthase; JNK, c-Jun N-terminal kinase; LDL-c, low density lipoprotein cholesterol; LOX-1, low-density lipoprotein receptor 1; MAO, monoamine oxidase; MCL-1, myeloid cell leukemia 1; MCP, monocyte chemoattractant protein; MDA, malondialdehyde; MMP-2, matrix metalloprotease 2; MPO, myeloperoxidase; Myd-88, myeloid differentiation factor 88; NF-κB, nuclear factor κB; PAH, pulmonary arterial hypertension; Pak-1, p21-activated kinase 1; PARP, poly (ADP-ribose) polymerase; PCNA, proliferating cell nuclear antigen; PHD-3, prolyl hydroxylase 3; PI3K, phosphoinositide 3-kinase; PON-1, paraoxonase 1; PP2Ac, protein phosphatase 2Ac; PP2B, calcineurin; PPAR-α, peroxisome proliferator-activated receptor α; ROS, reactive oxygen species; SIRT-1, silent information regulator 1; Smad-3, small mother against decapentaplegic 3; SOD, superoxide dismutase; STAT-3, signal transducer and activator of transcription 3; T-AOC, total antioxidant capacity; TERT, telomerase reverse transcriptase; TGF-β, transforming growth factor β; TIMP, tissue inhibitor of metalloproteinase; TLR-4, toll-like receptor 4; TNF-α, tumor necrosis factor α; TRPV-4, transient receptor potential vanilloid 4; Trx-1, Thioredoxin 1; TSP-1, thrombospondin 1; UCP-2, uncoupling protein 2; u-PA, urokinase-type plasminogen activator; VCAM-1, vascular cell adhesion molecule 1; VEGF-α, vascular endothelial growth factor α; XBP-1, X-box binding protein 1; ZO-1, zona occluden 1; α-SMA, α-smooth muscle actin.
Pharmacokinetics is principally to quantitatively assess the absorption, distribution, metabolism, and excretion (ADME) properties of drugs within a living organism that determine the safety and effective of drugs. Berberine is widely distributed in multiple tissues and organs after entering circulation, and can still accumulate in plasma despite keeping a low-rise concentration (Han et al., 2021a; Chen et al., 2021). According to our review, there are still many issues to overcome regarding the use of berberine to treat the vascular diseases. First, the bioavailability of orally-administered berberine in vivo is low due to first-pass elimination. It is therefore imperative to investigate alternative modes and methods of drug delivery with the aim of increasing the bioavailability of berberine. Numerous studies have showed that the strategic use of nanotechnology, including nanocarriers, liposomes, and microfluidic technology-assisted preparation methods, may increase the bioavailability of berberine for use in cardiovascular and metabolic diseases (Allijn et al., 2017; Guo et al., 2019b; Dewanjee et al., 2020). Structural modification of berberine may also improve bioavailability and efficacy and reduce adverse drug reactions (Mbese et al., 2019; Luo et al., 2021). Han et al. (2019); synthesized, water-soluble berberine derivatives with modified 9-O-monosaccharide (administered at concentrations of 0.2, 1 and 5 μg/ml) were shown to have antidiabetic effects, with lower cytotoxicity and a half-maximal inhibitory concentration (IC50) nearly 1.5 times than that of unmodified berberine in HepG2 liver cancer cells. Additionally, this review found that the toxicity of berberine and its derivatives have been rarely investigated. Considering the long-term development for berberine prevention and treatment of vascular diseases, comprehensive toxicity investigations, especially potentially cumulative toxicity in vivo studies, need to be carried out. It is also necessary to explain the efficacy and toxicity of berberine for use in human pharmacokinetic studies, and the identification of the ideal dosage are of enormous significance if side effects associated with drug accumulation are to be avoided. Relatively newly developed biological techniques, including microfluidic technology, computational toxicological methods, hepatoid cell models, and high-throughput chip models, could be employed to explore the toxicity of berberine (Banerjee et al., 2016; Kimura et al., 2018). In addition, single-cell in vitro models, as reported in the literature reviewed here, may not adequately reflect the pathogenesis of diseases in vivo. A multi-organ in vitro model based on microfluidic technology may be more helpful models of vascular diseases for the evaluation of the safety and efficacy of berberine (Rothbauer et al., 2018; Malik et al., 2021). For the clinical trial of berberine on vascular disease, many factors limit its clinical application, including the low methodological quality and drug–drug interactions (Imenshahidi and Hosseinzadeh, 2019). Therefore, the development of a standardized dosage, administration route, duration and adverse reaction of berberine could also be pursued in clinical settings for better therapeutic efficacy and safety.
Concurrently, we should strengthen the mechanism of berberine in the treatment of vascular diseases. Novel technologies that could be employed to explore the mechanism of action of berberine in the treatment of vascular diseases include CRISPR–CAS-9 gene editing, metabolomics, proteomics, and genomics. Most importantly, recently published investigations of the pharmacological mechanisms of berberine may provide new insights into the treatment of vascular diseases by berberine. For example, Zhao and others demonstrated that 560 mg/kg berberine administered orally in Coptis chinensis can significantly increase insulin secretion via the potassium voltage-gated channel subfamily H member 6 (KCNH-6) potassium channel in mice with HFD-induced hyperglycemia (Zhao et al., 2021a). Overall, this study comprehensively reviewed and summarized the pharmacokinetics properties and therapeutic potentials of berberine in diverse vascular diseases, thus providing experimental evidence for future research to discover novel drugs from Chinese medicine monomers.
Author Contributions
XM, FL, and XA conceived the study; XA, PY, LL, SL, and XL collected, analyzed, and interpreted the relevant literatures; XA, LP, and JL drew all the figures and tables; XA wrote the manuscript; XM and FL supervised the study and revised the manuscript. The final version of the manuscript was read and approved by all authors.
Funding
This work was supported by the National Natural Science Foundation of China (82004058 and 81774007), the National Key R&D Program of China (2017YFC1703904), the Regional Innovation and Cooperation Project of the Science and Technology Department of Sichuan Province (2020YFQ0032), the Major Science and Technology Project of Sichuan Science and Technology Department (2019YFSY0046), and the Key R&D and Transformation Program of the Science and Technology Department of Qinghai Province (2020-SF-C33).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aggarwal, S., Banerjee, S. K., Talukdar, N. C., and Yadav, A. K. (2020). Post-translational Modification Crosstalk and Hotspots in Sirtuin Interactors Implicated in Cardiovascular Diseases. Front. Genet. 11, 356. doi:10.3389/fgene.2020.00356
Agrawal, S., Zaritsky, J. J., Fornoni, A., and Smoyer, W. E. (2018). Dyslipidaemia in Nephrotic Syndrome: Mechanisms and Treatment. Nat. Rev. Nephrol. 14 (1), 57–70. doi:10.1038/nrneph.2017.155
Ai, X., Hou, Y., Wang, X., Wang, X., Liang, Y., Zhu, Z., et al. (2019). Amelioration of Dry Eye Syndrome in Db/db Mice with Diabetes Mellitus by Treatment with Tibetan Medicine Formula Jikan Mingmu Drops. J. Ethnopharmacol. 241, 111992. doi:10.1016/j.jep.2019.111992
Ai, X., Yu, P., Hou, Y., Song, X., Luo, J., Li, N., et al. (2020). A Review of Traditional Chinese Medicine on Treatment of Diabetic Retinopathy and Involved Mechanisms. Biomed. Pharmacother. 132, 110852. doi:10.1016/j.biopha.2020.110852
Ajjan, R. A., Kietsiriroje, N., Badimon, L., Vilahur, G., Gorog, D. A., Angiolillo, D. J., et al. (2021). Antithrombotic Therapy in Diabetes: Which, when, and for How Long? Eur. Heart J. 42 (23), 2235–2259. doi:10.1093/eurheartj/ehab128
Akhmedov, A., Sawamura, T., Chen, C. H., Kraler, S., Vdovenko, D., and Lüscher, T. F. (2021). Lectin-Like Oxidized Low-Density Lipoprotein Receptor-1 (LOX-1): A Crucial Driver of Atherosclerotic Cardiovascular Disease. Eur. Heart J. 42 (18), 1797–1807. doi:10.1093/eurheartj/ehaa770
Al Rifai, M., Mahtta, D., Kherallah, R., Kianoush, S., Liu, J., Rodriguez, F., et al. (2021). Prevalence and Determinants of Difficulty in Accessing Medical Care in U.S. Adults. Am. J. Prev. Med. 61 (4), 492–500. doi:10.1016/j.amepre.2021.03.026
Allijn, I. E., Czarny, B. M. S., Wang, X., Chong, S. Y., Weiler, M., da Silva, A. E., et al. (2017). Liposome Encapsulated Berberine Treatment Attenuates Cardiac Dysfunction after Myocardial Infarction. J. Control Release. 247, 127–133. doi:10.1016/j.jconrel.2016.12.042
Altoé, L. S., Alves, R. S., Miranda, L. L., Sarandy, M. M., Bastos, D. S. S., Gonçalves-Santos, E., et al. (2021). Doxycycline Hyclate Modulates Antioxidant Defenses, Matrix Metalloproteinases, and COX-2 Activity Accelerating Skin Wound Healing by Secondary Intention in Rats. Oxid. Med. Cel. Longev. 2021, 4681041. doi:10.1155/2021/4681041
Antila, S., Karaman, S., Nurmi, H., Airavaara, M., Voutilainen, M. H., Mathivet, T., et al. (2017). Development and Plasticity of Meningeal Lymphatic Vessels. J. Exp. Med. 214 (12), 3645–3667. doi:10.1084/jem.20170391
Atanasov, A. G., Zotchev, S. B., Dirsch, V. M., and Supuran, C. T. (2021). Natural Products in Drug Discovery: Advances and Opportunities. Nat. Rev. Drug Discov. 20 (3), 200–216. doi:10.1038/s41573-020-00114-z
Azegami, T., Nakayama, T., Hayashi, K., Hishikawa, A., Yoshimoto, N., Nakamichi, R., et al. (2021). Vaccination against Receptor for Advanced Glycation End Products Attenuates the Progression of Diabetic Kidney Disease. Diabetes 70 (9), 2147–2158. doi:10.2337/db20-1257
Banaei, P., Nazem, F., Nazari, A., and Arjomand, A. (2020). Preconditioning Effect of High-Intensity Interval Training (HIIT) and Berberine Supplementation on the Gene Expression of Angiogenesis Regulators and Caspase-3 Protein in the Rats with Myocardial Ischemia-Reperfusion (IR) Injury. Biomed. Res. Int. 2020, 4104965. doi:10.1155/2020/4104965
Banerjee, P., Siramshetty, V. B., Drwal, M. N., and Preissner, R. (2016). Computational Methods for Prediction of In Vitro Effects of New Chemical Structures. J. Cheminform. 8, 51. doi:10.1186/s13321-016-0162-2
Bertorello, A. M., Pires, N., Igreja, B., Pinho, M. J., Vorkapic, E., Wågsäter, D., et al. (2015). Increased Arterial Blood Pressure and Vascular Remodeling in Mice Lacking Salt-Inducible Kinase 1 (SIK1). Circ. Res. 116 (4), 642–652. doi:10.1161/CIRCRESAHA.116.304529
Bisserier, M., Mathiyalagan, P., Zhang, S., Elmastour, F., Dorfmüller, P., Humbert, M., et al. (2021). Regulation of the Methylation and Expression Levels of the BMPR2 Gene by SIN3a as a Novel Therapeutic Mechanism in Pulmonary Arterial Hypertension. Circulation 144 (1), 52–73. doi:10.1161/CIRCULATIONAHA.120.047978
Bravo-San Pedro, J. M., Kroemer, G., Galluzzi, L., and Galluzzi, L. (2017). Autophagy and Mitophagy in Cardiovascular Disease. Circ. Res. 120 (11), 1812–1824. doi:10.1161/CIRCRESAHA.117.311082
Brown, E., Ozawa, K., Moccetti, F., Vinson, A., Hodovan, J., Nguyen, T. A., et al. (2021). Arterial Platelet Adhesion in Atherosclerosis-Prone Arteries of Obese, Insulin-Resistant Nonhuman Primates. J. Am. Heart Assoc. 10 (9), e019413. doi:10.1161/JAHA.120.019413
Brown, R. A., Shantsila, E., Varma, C., and Lip, G. Y. (2017). Current Understanding of Atherogenesis. Am. J. Med. 130 (3), 268–282. doi:10.1016/j.amjmed.2016.10.022
Chang, W., Zhang, M., Li, J., Meng, Z., Xiao, D., Wei, S., et al. (2012). Berberine Attenuates Ischemia-Reperfusion Injury via Regulation of Adenosine-5'-Monophosphate Kinase Activity in Both Non-ischemic and Ischemic Areas of the Rat Heart. Cardiovasc. Drugs Ther. 26 (6), 467–478. doi:10.1007/s10557-012-6422-0
Chang, X., Wang, Z., Zhang, J., Yan, H., Bian, H., Xia, M., et al. (2016). Lipid Profiling of the Therapeutic Effects of Berberine in Patients with Nonalcoholic Fatty Liver Disease. J. Transl. Med. 14, 266. doi:10.1186/s12967-016-0982-x
Chang, X., Zhang, T., Meng, Q., ShiyuanWang, S., Yan, P., Wang, X., et al. (2021). Quercetin Improves Cardiomyocyte Vulnerability to Hypoxia by Regulating SIRT1/TMBIM6-Related Mitophagy and Endoplasmic Reticulum Stress. Oxid. Med. Cell Longev. 2021, 5529913. doi:10.1155/2021/5529913
Chen, H., Ji, Y., Yan, X., Su, G., Chen, L., and Xiao, J. (2018). Berberine Attenuates Apoptosis in Rat Retinal Müller Cells Stimulated with High Glucose via Enhancing Autophagy and the AMPK/mTOR Signaling. Biomed. Pharmacother. 108, 1201–1207. doi:10.1016/j.biopha.2018.09.140
Chen, H. B., Luo, C. D., Ai, G. X., Wang, Y. F., Li, C. L., Tan, L. H., et al. (2021). A Comparative Investigation of the Interaction and Pharmacokinetics of Hemoglobin with Berberine and its Oxymetabolite. J. Pharm. Biomed. Anal. 199, 114032. doi:10.1016/j.jpba.2021.114032
Chen, L., Luo, W., Zhang, W., Chu, H., Wang, J., Dai, X., et al. (2020). circDLPAG4/HECTD1 Mediates Ischaemia/reperfusion Injury in Endothelial Cells via ER Stress. RNA Biol. 17 (2), 240–253. doi:10.1080/15476286.2019.1676114
Chen, M., Shen, H., Zhu, L., Yang, H., Ye, P., Liu, P., et al. (2019). Berberine Attenuates Hypoxia-Induced Pulmonary Arterial Hypertension via Bone Morphogenetic Protein and Transforming Growth Factor-β Signaling. J. Cell Physiol. 234 (10), 17482–17493. doi:10.1002/jcp.28370
Chen, W., Miao, Y. Q., Fan, D. J., Yang, S. S., Lin, X., Meng, L. K., et al. (2011). Bioavailability Study of Berberine and the Enhancing Effects of TPGS on Intestinal Absorption in Rats. AAPS PharmSciTech 12 (2), 705–711. doi:10.1208/s12249-011-9632-z
Cheng, Y. C., Sheen, J. M., Hu, W. L., and Hung, Y. C. (2017). Polyphenols and Oxidative Stress in Atherosclerosis-Related Ischemic Heart Disease and Stroke. Oxid Med. Cell Longev 2017, 8526438. doi:10.1155/2017/8526438
Cheng, Z., Chen, A. F., Wu, F., Sheng, L., Zhang, H. K., Gu, M., et al. (2010). 8,8-Dimethyldihydroberberine with Improved Bioavailability and Oral Efficacy on Obese and Diabetic Mouse Models. Bioorg. Med. Chem. 18 (16), 5915–5924. doi:10.1016/j.bmc.2010.06.085
Chong, S. Y., Zharkova, O., Yatim, S. M. J. M., Wang, X., Lim, X. C., Huang, C., et al. (2021). Tissue Factor Cytoplasmic Domain Exacerbates Post-Infarct Left Ventricular Remodeling via Orchestrating Cardiac Inflammation and Angiogenesis. Theranostics 11 (19), 9243–9261. doi:10.7150/thno.63354
Choudhary, G., Troncales, F., Martin, D., Harrington, E. O., and Klinger, J. R. (2011). Bosentan Attenuates Right Ventricular Hypertrophy and Fibrosis in Normobaric Hypoxia Model of Pulmonary Hypertension. J. Heart Lung Transpl. 30 (7), 827–833. doi:10.1016/j.healun.2011.03.010
Cook, N. L., Viola, H. M., Sharov, V. S., Hool, L. C., Schöneich, C., and Davies, M. J. (2012). Myeloperoxidase-derived Oxidants Inhibit Sarco/Endoplasmic Reticulum Ca2+-Atpase Activity and Perturb Ca2+ Homeostasis in Human Coronary Artery Endothelial Cells. Free Radic. Biol. Med. 52 (5), 951–961. doi:10.1016/j.freeradbiomed.2011.12.001
Crusz, S. M., and Balkwill, F. R. (2015). Inflammation and Cancer: Advances and New Agents. Nat. Rev. Clin. Oncol. 12 (10), 584–596. doi:10.1038/nrclinonc.2015.105
Cryer, M. J., Horani, T., and DiPette, D. J. (2016). Diabetes and Hypertension: A Comparative Review of Current Guidelines. J. Clin. Hypertens. (Greenwich) 18 (2), 95–100. doi:10.1111/jch.12638
Cui, H. M., Zhang, Q. Y., Wang, J. L., Chen, J. L., Zhang, Y. L., and Tong, X. L. (2015). Poor Permeability and Absorption Affect the Activity of Four Alkaloids from Coptis. Mol. Med. Rep. 12 (5), 7160–7168. doi:10.3892/mmr.2015.4288
Cui, H. X., Hu, Y. N., Li, J. W., Yuan, K., and Guo, Y. (2018). Preparation and Evaluation of Antidiabetic Agents of Berberine Organic Acid Salts for Enhancing the Bioavailability. Molecules 24 (1), 103. doi:10.3390/molecules24010103
Dai, W., Lopez, O. L., Carmichael, O. T., Becker, J. T., Kuller, L. H., and Gach, H. M. (2009). Mild Cognitive Impairment and Alzheimer Disease: Patterns of Altered Cerebral Blood Flow at MR Imaging. Radiology 250 (3), 856–866. doi:10.1148/radiol.2503080751
de Ferranti, S. D., Gauvreau, K., Friedman, K. G., Tang, A., Baker, A. L., Fulton, D. R., et al. (2018). Association of Initially Normal Coronary Arteries with Normal Findings on Follow-Up Echocardiography in Patients with Kawasaki Disease. JAMA Pediatr. 172 (12), e183310. doi:10.1001/jamapediatrics.2018.3310
Detillieux, K. A., Sheikh, F., Kardami, E., and Cattini, P. A. (2003). Biological Activities of Fibroblast Growth Factor-2 in the Adult Myocardium. Cardiovasc. Res. 57 (1), 8–19. doi:10.1016/s0008-6363(02)00708-3
Dewanjee, S., Chakraborty, P., Mukherjee, B., and De Feo, V. (2020). Plant-Based Antidiabetic Nanoformulations: The Emerging Paradigm for Effective Therapy. Int. J. Mol. Sci. 21 (6), 2217. doi:10.3390/ijms21062217
Doña, I., Pérez‐Sánchez, N., Eguiluz‐Gracia, I., Muñoz-Cano, R., Bartra, J., Torres, M. J., et al. (2020). Progress in Understanding Hypersensitivity Reactions to Nonsteroidal Anti‐inflammatory Drugs. Allergy 75 (3), 561–575. doi:10.1111/all.14032
Durairajan, S. S., Liu, L. F., Lu, J. H., Chen, L. L., Yuan, Q., Chung, S. K., et al. (2012). Berberine Ameliorates β-amyloid Pathology, Gliosis, and Cognitive Impairment in an Alzheimer's Disease Transgenic Mouse Model. Neurobiol. Aging 33 (12), 2903–2919. doi:10.1016/j.neurobiolaging.2012.02.016
Fang, C., Xie, L., Liu, C., Fu, C., Ye, W., Liu, H., et al. (2018). Berberine Ameliorates Neonatal Necrotizing Enterocolitis by Activating the Phosphoinositide 3-kinase/protein Kinase B Signaling Pathway. Exp. Ther. Med. 15 (4), 3530–3536. doi:10.3892/etm.2018.5858
Fang, C., Dai, L., Wang, C., Fan, C., Yu, Y., Yang, L., et al. (2021). Secretogranin II Impairs Tumor Growth and Angiogenesis by Promoting Degradation of Hypoxia‐inducible Factor‐1α in Colorectal Cancer. Mol. Oncol. 23, 1. doi:10.1002/1878-0261.13044
Feng, M., Zou, Z., Zhou, X., Hu, Y., Ma, H., Xiao, Y., et al. (2017). Comparative Effect of Berberine and its Derivative 8-Cetylberberine on Attenuating Atherosclerosis in ApoE-/- Mice. Int. Immunopharmacol. 43, 195–202. doi:10.1016/j.intimp.2016.12.001
Feng, R., Shou, J. W., Zhao, Z. X., He, C. Y., Ma, C., Huang, M., et al. (2015). Transforming Berberine into its Intestine-Absorbable Form by the Gut Microbiota. Sci. Rep. 5, 12155. doi:10.1038/srep12155
Feng, X., Sureda, A., Jafari, S., Memariani, Z., Tewari, D., Annunziata, G., et al. (2019). Berberine in Cardiovascular and Metabolic Diseases: From Mechanisms to Therapeutics. Theranostics 9 (7), 1923–1951. doi:10.7150/thno.30787
Feng, X., Wang, K., Cao, S., Ding, L., and Qiu, F. (2021). Pharmacokinetics and Excretion of Berberine and its Nine Metabolites in Rats. Front. Pharmacol. 11, 594852. doi:10.3389/fphar.2020.594852
Feng, X., Zhang, L., Xu, S., and Shen, A. Z. (2020). ATP-citrate Lyase (ACLY) in Lipid Metabolism and Atherosclerosis: An Updated Review. Prog. Lipid. Res. 77, 101006. doi:10.1016/j.plipres.2019.101006
Ference, B. A., Ginsberg, H. N., Graham, I., Ray, K. K., Packard, C. J., Bruckert, E., et al. (2017). Low-density Lipoproteins Cause Atherosclerotic Cardiovascular Disease. 1. Evidence from Genetic, Epidemiologic, and Clinical Studies. A Consensus Statement from the European Atherosclerosis Society Consensus Panel. Eur. Heart J. 38 (32), 2459–2472. doi:10.1093/eurheartj/ehx144
Ferron, L., Ruchon, Y., Renaud, J. F., and Capuano, V. (2011). T-type Ca²+ Signalling Regulates Aldosterone-Induced CREB Activation and Cell Death through PP2A Activation in Neonatal Cardiomyocytes. Cardiovasc. Res. 90 (1), 105–112. doi:10.1093/cvr/cvq379
Fatima, M. T., Hasan, M., Abdelsalam, S. S., Sivaraman, S. K., El-Gamal, H., and Zahid, M. A. (2021). Sestrin2 Suppression Aggravates Oxidative Stress and Apoptosis in Endothelial Cells Subjected to Pharmacologically Induced Endoplasmic Reticulum Stress. Eur. J. Pharmacol. 907, 17424. doi:10.1016/j.ejphar.2021.174247
Frangogiannis, N. G., Ren, G., Dewald, O., Zymek, P., Haudek, S., Koerting, A., et al. (2005). Critical Role of Endogenous Thrombospondin-1 in Preventing Expansion of Healing Myocardial Infarcts. Circulation 111 (22), 2935–2942. doi:10.1161/CIRCULATIONAHA.104.510354
Gaba, S., Saini, A., Singh, G., and Monga, V. (2021). An Insight into the Medicinal Attributes of Berberine Derivatives: A Review. Bioorg. Med. Chem. 38, 116143. doi:10.1016/j.bmc.2021.116143
Galvani, S., Sanson, M., Blaho, V. A., Swendeman, S. L., Obinata, H., Conger, H., et al. (2015). HDL-bound Sphingosine 1-Phosphate Acts as a Biased Agonist for the Endothelial Cell Receptor S1P1 to Limit Vascular Inflammation. Sci. Signal. 8 (389), ra79. doi:10.1126/scisignal.aaa2581
Gan, J., Yuan, J., Liu, Y., Lu, Z., Xue, Y., Shi, L., et al. (2020). Circular RNA_101237 Mediates Anoxia/reoxygenation Injury by Targeting let-7a-5p/IGF2BP3 in C-ardiomyocytes. Int. J. Mol. Med. 45 (2), 451–460. doi:10.3892/ijmm.2019.4441
Gao, Y., Tan, L., Yu, J. T., and Tan, L. (2018). Tau in Alzheimer's Disease: Mechanisms and Therapeutic Strategies. Curr. Alzheimer. Res. 15 (3), 283–300. doi:10.2174/1567205014666170417111859
Garikipati, V. N. S., Verma, S. K., Cheng, Z., Liang, D., Truongcao, M. M., Cimini, M., et al. (2019). Circular RNA CircFndc3b Modulates Cardiac Repair after Myocardial Infarction via FUS/VEGF-A Axis. Nat. Commun. 10 (1), 4317. doi:10.1038/s41467-019-11777-7
Garry, G. A., Bassel-Duby, R., and Olson, E. N. (2021). Direct Reprogramming as a Route to Cardiac Repair. Semin. Cell Dev. Biol. S1084-9521 (21), 00128–132. doi:10.1016/j.semcdb.2021.05.019
Gawel, K., Kukula-Koch, W., Nieoczym, D., Stepnik, K., Ent, W. V., Banono, N. S., et al. (2020). The Influence of Palmatine Isolated from Berberis Sibirica Radix on Pentylenetetrazole-Induced Seizures in Zebrafish. Cells 9 (5), 1233. doi:10.3390/cells9051233
Geng, F. H., Li, G. H., Zhang, X., Zhang, P., Dong, M. Q., Zhao, Z. J., et al. (2016). Berberine Improves Mesenteric Artery Insulin Sensitivity through Up-Regulating Insulin Receptor-Mediated Signalling in Diabetic Rats. Br. J. Pharmacol. 173 (10), 1569–1579. doi:10.1111/bph.13466
Golia, E., Limongelli, G., Natale, F., Fimiani, F., Maddaloni, V., Pariggiano, I., et al. (2014). Inflammation and Cardiovascular Disease: From Pathogenesis to Therapeutic Target. Curr. Atheroscler. Rep. 16 (9), 435. doi:10.1007/s11883-014-0435-z
Gong, Q., Wang, H., Yu, P., Qian, T., and Xu, X. (2021). Protective or Harmful: The Dual Roles of Autophagy in Diabetic Retinopathy. Front. Med. (Lausanne) 8, 644121. doi:10.3389/fmed.2021.644121
Gong, W., Li, J., Chen, W., Feng, F., and Deng, Y. (2020). Resveratrol Inhibits Lipopolysaccharide-Induced Extracellular Matrix Accumulation and Inflammation in Rat Glomerular Mesangial Cells by SphK1/S1P2/NF-Κb Pathway. Diabetes Metab. Syndr. Obes. 13, 4495–4505. doi:10.2147/DMSO.S278267
Guan, C., Qiao, S., Lv, Q., Cao, N., Wang, K., Dai, Y., et al. (2018). Orally Administered Berberine Ameliorates Bleomycin-Induced Pulmonary Fibrosis in Mice through Promoting Activation of PPAR-γ and Subsequent Expression of HGF in Colons. Toxicol. Appl. Pharmacol. 343, 1–15. doi:10.1016/j.taap.2018.02.001
Guida, F. M., Santoni, M., Conti, A., Burattini, L., Savini, A., Zeppola, T., et al. (2014). Alternative Dosing Schedules for Sunitinib as a Treatment of Patients with Metastatic Renal Cell Carcinoma. Crit. Rev. Oncol. Hematol. 92 (3), 208–217. doi:10.1016/j.critrevonc.2014.07.006
Guo, B., Feng, Z., Hu, D., Xu, S., Middha, E., Pan, Y., et al. (2019a). Precise Deciphering of Brain Vasculatures and Microscopic Tumors with Dual NIR-II Fluorescence and Photoacoustic Imaging. Adv. Mater. 31 (30), e1902504. doi:10.1002/adma.201902504
Guo, H. H., Feng, C. L., Zhang, W. X., Luo, Z. G., Zhang, H. J., Zhang, T. T., et al. (2019b). Liver-Target Nanotechnology Facilitates Berberine to Ameliorate Cardio-Metabolic Diseases. Nat. Commun. 10 (1), 1981. doi:10.1038/s41467-019-09852-0
Guo, J., Wang, L., Wang, L., Qian, S., Zhang, D., Fang, J., et al. (2016). Berberine Protects Human Umbilical Vein Endothelial Cells against LPS-Induced Apoptosis by Blocking JNK-Mediated Signaling. Evid. Based Complement. Alternat. Med. 2016, 6983956. doi:10.1155/2016/6983956
Guo, Y., Pope, C., Cheng, X., Zhou, H., and Klaassen, C. D. (2011). Dose-Response of Berberine on Hepatic Cytochromes P450 mRNA Expression and Activities in Mice. J. Ethnopharmacol. 138 (1), 111–118. doi:10.1016/j.jep.2011.08.058
Guzik, T. J., and Touyz, R. M. (2017). Oxidative Stress, Inflammation, and Vascular Aging in Hypertension. Hypertension 70 (4), 660–667. doi:10.1161/HYPERTENSIONAHA.117.07802
Habtemariam, S. (2020b). Berberine Pharmacology and the Gut Microbiota: A Hidden Therapeutic Link. Pharmacol. Res. 155, 104722. doi:10.1016/j.phrs.2020.104722
Habtemariam, S. (2020a). The Quest to Enhance the Efficacy of Berberine for Type-2 Diabetes and Associated Diseases: Physicochemical Modification Approaches. Biomedicines 8 (4), 90. doi:10.3390/biomedicines8040090
Han, L., Sheng, W., Li, X., Sik, A., Lin, H., Liu, K., et al. (2019). Novel Carbohydrate Modified Berberine Derivatives: Synthesis and In Vitro Anti-diabetic Investigation. Medchemcomm 10 (4), 598–605. doi:10.1039/c9md00036d
Han, T., Ko, E., Kim, M., Choi, M., Lee, C., Kim, I. H., et al. (2021a). Mori Ramulus Inhibits Pancreatic β-Cell Apoptosis and Prevents Insulin Resistance by Restoring Hepatic Mitochondrial Function. Antioxidants (Basel) 10 (6), 901. doi:10.3390/antiox10060901
Han, Y., Xiang, Y., Shi, Y., Tang, X., Pan, L., Gao, J., et al. (2021b). Pharmacokinetics and Pharmacological Activities of Berberine in Diabetes Mellitus Treatment. Evid. Based Complement. Alternat. Med. 2021, 9987097. doi:10.1155/2021/9987097
Hao, M., Li, S. Y., Sun, C. K., Jingyu-Xu, J. Y., Lin, Y., Liu, K. X., et al. (2011). Amelioration Effects of Berberine on Diabetic Microendothelial Injury Model by the Combination of High Glucose and Advanced Glycation End Products In Vitro. Eur. J. Pharmacol. 654 (3), 320–325. doi:10.1016/j.ejphar.2010.12.030
He, Y., Yuan, X., Zuo, H., Sun, Y., and Feng, A. (2018). Berberine Exerts a Protective Effect on Gut-Vascular Barrier via the Modulation of the Wnt/Beta-Catenin Signaling Pathway during Sepsis. Cell. Physiol. Biochem. 49 (4), 1342–1351. doi:10.1159/000493412
Henning, R. J., Bourgeois, M., and Harbison, R. D. (2018). Poly(ADP-ribose) Polymerase (PARP) and PARP Inhibitors: Mechanisms of Action and Role in Cardiovascular Disorders. Cardiovasc. Toxicol. 18 (6), 493–506. doi:10.1007/s12012-018-9462-2
Hu, S., Zhao, R., Liu, Y., Chen, J., Zheng, Z., and Wang, S. (2019). Preventive and Therapeutic Roles of Berberine in Gastrointestinal Cancers. Biomed. Res. Int. 2019, 6831520. doi:10.1155/2019/6831520
Hong, S., Beja-Glasser, V. F., Beja-Glasser, V. F., Nfonoyim, B. M., Frouin, A., Li, S., and Ramakrishnan, S. (2016). Complement and Microglia Mediate Early Synapse Loss in Alzheimer Mouse Models. Science 352 (6286), 712–716. doi:10.1126/science.aad8373
Hua, W., Ding, L., Chen, Y., Gong, B., He, J., and Xu, G. (2007). Determination of Berberine in Human Plasma by Liquid Chromatography-Electrospray Ionization-Mass Spectrometry. J. Pharm. Biomed. Anal. 44 (4), 931–937. doi:10.1016/j.jpba.2007.03.022
Huang, C., Neupane, Y. R., Lim, X. C., Shekhani, R., Czarny, B., Wacker, M. G., et al. (2021). Extracellular Vesicles in Cardiovascular Disease. Adv. Clin. Chem. 103, 47–95. doi:10.1016/bs.acc.2020.08.006
Huang, J., Liu, Z., Xu, P., Zhang, Z., Yin, D., Liu, J., et al. (2018). Capsaicin Prevents Mitochondrial Damage, Protects Cardiomyocytes Subjected to Anoxia/reoxygenation Injury Mediated by 14-3-3η/Bcl-2. Eur. J. Pharmacol. 819, 43–50. doi:10.1016/j.ejphar.2017.11.028
Hui, X., Li, H., Zhou, Z., Lam, K. S., Xiao, Y., Wu, D., et al. (2010). Adipocyte Fatty Acid-Binding Protein Modulates Inflammatory Responses in Macrophages through a Positive Feedback Loop Involving C-Jun NH2-Terminal Kinases and Activator Protein-1. J. Biol. Chem. 285 (14), 10273–10280. doi:10.1074/jbc.M109.097907
Imenshahidi, M., and Hosseinzadeh, H. (2019). Berberine and Barberry (Berberis Vulgaris): A Clinical Review. Phytother. Res. 33 (3), 504–523. doi:10.1002/ptr.6252
Insull, W. (2009). The Pathology of Atherosclerosis: Plaque Development and Plaque Responses to Medical Treatment. Am. J. Med. 122 (1 Suppl. l), S3–S14. doi:10.1016/j.amjmed.2008.10.013
James, P. A., Oparil, S., Carter, B. L., Cushman, W. C., Dennison-Himmelfarb, C., Handler, J., et al. (2014). 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report from the Panel Members Appointed to the Eighth Joint National Committee (JNC 8). JAMA 311 (5), 507–520. doi:10.1001/jama.2013.284427
Jang, S. A., Park, D. W., Kwon, J. E., Song, H. S., Park, B., Jeon, H., et al. (2017). Quinic Acid Inhibits Vascular Inflammation in TNF-α-Stimulated Vascular Smooth Muscle Cells. Biomed. Pharmacotherpharmacother 96, 563–571. doi:10.1016/j.biopha.2017.10.021
Ji, E., and Lee, S. (2021). Antibody-Based Therapeutics for Atherosclerosis and Cardiovascular Diseases. Int. J. Mol. Sci. 22 (11), 5770. doi:10.3390/ijms22115770
Ji, L., Tian, H., Webster, K. A., and Li, W. (2021). Neurovascular Regulation in Diabetic Retinopathy and Emerging Therapies. Cell. Mol. Life Sci. 78 (16), 5977–5985. doi:10.1007/s00018-021-03893-9
Jia, L., Liu, J., Song, Z., Pan, X., Chen, L., Cui, X., et al. (2012). Berberine Suppresses Amyloid-Beta-Induced Inflammatory Response in Microglia by Inhibiting Nuclear Factor-kappaB and Mitogen-Activated Protein Kinase Signalling Pathways. J. Pharm. Pharmacol. 64 (10), 1510–1521. doi:10.1111/j.2042-7158.2012.01529.x
Jiang, Q., Liu, P., Wu, X., Liu, W., Shen, X., Lan, T., et al. (2011). Berberine Attenuates Lipopolysaccharide-Induced Extracelluar Matrix Accumulation and Inflammation in Rat Mesangial Cells: Involvement of NF-Κb Signaling Pathway. Mol. Cel. Endocrinol. 331 (1), 34–40. doi:10.1016/j.mce.2010.07.023
Jie, S., Li, H., Tian, Y., Guo, D., Zhu, J., Gao, S., et al. (2011). Berberine Inhibits Angiogenic Potential of Hep G2 Cell Line through VEGF Down-Regulation In Vitro. J. Gastroenterol. Hepatol. 26 (1), 179–185. doi:10.1111/j.1440-1746.2010.06389.x
Jin, F., Xie, T., Huang, X., and Zhao, X. (2018). Berberine Inhibits Angiogenesis in Glioblastoma Xenografts by Targeting the VEGFR2/ERK Pathway. Pharm. Biol. 56 (1), 665–671. doi:10.1080/13880209.2018.1548627
Jin, H., Zhu, Y., Li, Y., Ding, X., Ma, W., Han, X., et al. (2019). BDNF-mediated Mitophagy Alleviates High-Glucose-Induced Brain Microvascular Endothelial Cell Injury. Apoptosis 24 (5–6), 511–528. doi:10.1007/s10495-019-01535-x
Jonsson, A. L., and Bäckhed, F. (2017). Role of Gut Microbiota in Atherosclerosis. Nat. Rev. Cardiol. 14 (2), 79–87. doi:10.1038/nrcardio.2016.183
Jove, M., Spencer, J., Clench, M., Loadman, P. M., and Twelves, C. (2019). Precision Pharmacology: Mass Spectrometry Imaging and Pharmacokinetic Drug Resistance. Crit. Rev. Oncol. Hematol. 141, 153–162. doi:10.1016/j.critrevonc.2019.06.008
Kattoor, A. J., Goel, A., and Mehta, J. L. (2019). LOX-1: Regulation, Signaling and its Role in Atherosclerosis. Antioxidants (Basel) 8 (7), 218. doi:10.3390/antiox8070218
Khoramzadeh, M., Dehghanian, A., and Ketabchi, F. (2019). Roles of Endothelin B Receptors and Endothelial Nitric Oxide Synthase in the Regulation of Pulmonary Hemodynamic in Cirrhotic Rats. J. Cardiovasc. Pharmacol. 73 (3), 178–185. doi:10.1097/FJC.0000000000000650
Kim, S., Choi, J. H., Lim, H. I., Lee, S. K., Kim, W. W., Kim, J. S., et al. (2009). Silibinin Prevents TPA-Induced MMP-9 Expression and VEGF Secretion by Inactivation of the Raf/MEK/ERK Pathway in MCF-7 Human Breast Cancer Cells. Phytomedicine 16 (6–7), 573–580. doi:10.1016/j.phymed.2008.11.006
Kim, S., Oh, S. J., Lee, J., Han, J., Jeon, M., Jung, T., et al. (2013). Berberine Suppresses TPA-Induced Fibronectin Expression through the Inhibition of VEGF Secretion in Breast Cancer Cells. Cell Physiol. Biochem. 32 (5), 1541–1550. doi:10.1159/000356591
Kimura, H., Sakai, Y., and Fujii, T. (2018). Organ/body-on-a-chip Based on Microfluidic Technology for Drug Discovery. Drug Metab. Pharmacokinet. 33 (1), 43–48. doi:10.1016/j.dmpk.2017.11.003
Konukoglu, D., and Uzun, H. (2017). Endothelial Dysfunction and Hypertension. Adv. Exp. Med. Biol. 956, 511–540. doi:10.1007/5584_2016_90
Kostov, K., and Halacheva, L. (2018). Role of Magnesium Deficiency in Promoting Atherosclerosis, Endothelial Dysfunction, and Arterial Stiffening as Risk Factors for Hypertension. Int. J. Mol. Sci. 19 (6), 1724. doi:10.3390/ijms19061724
Krüger-Genge, A., Blocki, A., Franke, R. P., and Jung, F. (2019). Vascular Endothelial Cell Biology: An Update. Int. J. Mol. Sci. 20 (18), 4411. doi:10.3390/ijms20184411
Kumar, A., EkavaliChopra, K., Chopra, K., Mukherjee, M., Pottabathini, R., and Dhull, D. K. (2015). Current Knowledge and Pharmacological Profile of Berberine: An Update. Eur. J. Pharmacol. 761, 288–297. doi:10.1016/j.ejphar.2015.05.068
Lai, X., Tong, D., Ai, X., Wu, J., Luo, Y., Zuo, F., et al. (2018). Amelioration of Diabetic Nephropathy in Db/db Mice Treated with Tibetan Medicine Formula Siwei Jianghuang Decoction Powder Extract. Sci. Rep. 8 (1), 16707. doi:10.1038/s41598-018-35148-2
Lee, A. Y., Park, W., Kang, T. W., Cha, M. H., and Chun, J. M. (2018). Network Pharmacology-Based Prediction of Active Compounds and Molecular Targets in Yijin-Tang Acting on Hyperlipidaemia and Atherosclerosis. J. Ethnopharmacol. 221, 151–159. doi:10.1016/j.jep.2018.04.027
Lefferts, W. K., Babcock, M. C., Tiss, M. J., Ives, S. J., White, C. N., Brutsaert, T. D., et al. (2016). Effect of Hypoxia on Cerebrovascular and Cognitive Function during Moderate Intensity Exercise. Physiol. Behav. 165, 108–118. doi:10.1016/j.physbeh.2016.07.003
Leyva-Peralta, M. A., Robles-Zepeda, R. E., Razo-Hernández, R. S., Berber, L. P. Á., Lara, K. O., Ruiz-Bustos, E., et al. (2019). Berberine as Source of Antiproliferative Hybrid Compounds: In Vitro Antiproliferative Activity and Quantitative Structure-Activity Relationship. Anticancer Agents Med. Chem. 19 (15), 1820–1834. doi:10.2174/1871520619666190503121820
Li, C., Ai, G., Wang, Y., Lu, Q., Luo, C., Tan, L., et al. (2020a). Oxyberberine, a Novel Gut Microbiota-Mediated Metabolite of Berberine, Possesses superior Anti-colitis Effect: Impact on Intestinal Epithelial Barrier, Gut Microbiota Profile and TLR4-MyD88-NF-Κb Pathway. Pharmacol. Res. 152, 104603. doi:10.1016/j.phrs.2019.104603
Li, H., He, C., Wang, J., Li, X., Yang, Z., Sun, X., et al. (2016a). Berberine Activates Peroxisome Proliferator-Activated Receptor Gamma to Increase Atherosclerotic Plaque Stability in Apoe-/- Mice with Hyperhomocysteinemia. J. Diabetes Investig. 7 (6), 824–832. doi:10.1111/jdi.12516
Li, P., Yin, Y. L., Guo, T., Sun, X. Y., Ma, H., Zhu, M. L., et al. (2016b). Inhibition of Aberrant MicroRNA-133a Expression in Endothelial Cells by Statin Prevents Endothelial Dysfunction by Targeting GTP Cyclohydrolase 1 In Vivo. Circulation 134 (22), 1752–1765. doi:10.1161/CIRCULATIONAHA.116.017949
Li, T., Wang, P., Guo, W., Huang, X., Tian, X., Wu, G., et al. (2019). Natural Berberine-Based Chinese Herb Medicine Assembled Nanostructures with Modified Antibacterial Application. ACS Nano 13 (6), 6770–6781. doi:10.1021/acsnano.9b01346
Li, X. X., Li, C. B., Xiao, J., Gao, H. Q., Wang, H. W., Zhang, X. Y., et al. (2015a). Berberine Attenuates Vascular Remodeling and Inflammation in a Rat Model of Metabolic Syndrome. Biol. Pharm. Bull. 38 (6), 862–868. doi:10.1248/bpb.b14-00828
Li, X. Y., Zhao, Z. X., Huang, M., Feng, R., He, C. Y., Ma, C., et al. (2015b). Effect of Berberine on Promoting the Excretion of Cholesterol in High-Fat Diet-Induced Hyperlipidemic Hamsters. J. Transl. Med. 13, 278. doi:10.1186/s12967-015-0629-3
Li, Y., Liu, Y., Wang, C., Xia, W. R., Zheng, J. Y., Yang, J., et al. (2018a). Succinate Induces Synovial Angiogenesis in Rheumatoid Arthritis through Metabolic Remodeling and HIF-1α/VEGF axis. Free Radic. Biol. Med. 126, 1–14. doi:10.1016/j.freeradbiomed.2018.07.009
Li, Y., Liu, Y., Yan, X., Liu, Q., Zhao, Y. H., and Wang, D. W. (2018b). Pharmacological Effects and Mechanisms of Chinese Medicines Modulating NLRP3 Inflammasomes in Ischemic Cardio/Cerebral Vascular Disease. Am. J. Chin. Med. 46 (8), 1727–1741. doi:10.1142/S0192415X18500878
Li, Y., Zhou, J., Qiu, J., Huang, Z., Wang, W., Wu, P., et al. (2020b). Berberine Reduces Gut-Vascular Barrier Permeability via Modulation of ApoM/S1P Pathway in a Model of Polymicrobial Sepsis. Life Sci. 261, 118460. doi:10.1016/j.lfs.2020.118460
Lian, H., Litvinchuk, A., Chiang, A. C., Aithmitti, N., Jankowsky, J. L., and Zheng, H. (2016). Astrocyte-Microglia Cross Talk through Complement Activation Modulates Amyloid Pathology in Mouse Models of Alzheimer's Disease. J. Neurosci. 36 (2), 577–589. doi:10.1523/JNEUROSCI.2117-15.2016
Liang, S., Zhang, J., Ning, R., Du, Z., Liu, J., Batibawa, J. W., et al. (2020). The Critical Role of Endothelial Function in Fine Particulate Matter-Induced Atherosclerosis. Part. Fibre. Toxicol. 17 (1), 61. doi:10.1186/s12989-020-00391-x
Lin, H. J., Ho, J. H., Tsai, L. C., Yang, F. Y., Yang, L. L., Kuo, C. D., et al. (2020). Synthesis and In Vitro Photocytotoxicity of 9-/13-Lipophilic Substituted Berberine Derivatives as Potential Anticancer Agents. Molecules 25 (3), 677. doi:10.3390/molecules25030677
Linton, M. F., Babaev, V. R., Huang, J., Linton, E. F., Tao, H., and Yancey, P. G. (2016). Macrophage Apoptosis and Efferocytosis in the Pathogenesis of Atherosclerosis. Circ. J. 80 (11), 2259–2268. doi:10.1253/circj.CJ-16-0924
Liss, D. T., Uchida, T., Wilkes, C. L., Radakrishnan, A., and Linder, J. A. (2021). General Health Checks in Adult Primary Care: A Review. JAMA 325 (22), 2294–2306. doi:10.1001/jama.2021.6524
Liu, C. S., Zheng, Y. R., Zhang, Y. F., and Long, X. Y. (2016). Research Progress on Berberine with a Special Focus on its Oral Bioavailability. Fitoterapia 109, 274–282. doi:10.1016/j.fitote.2016.02.001
Liu, H., Ren, X., and Ma, C. (2018). Effect of Berberine on Angiogenesis and HIF-1α/VEGF Signal Transduction Pathway in Rats with Cerebral Ischemia - Reperfusion Injury. J. Coll. Physicians Surg. Pak. 28 (10), 753–757.
Liu, L., Liu, J., Huang, Z., Yu, X., Zhang, X., Dou, D., et al. (2015a). Berberine Improves Endothelial Function by Inhibiting Endoplasmic Reticulum Stress in the Carotid Arteries of Spontaneously Hypertensive Rats. Biochem. Biophys. Res. Commun. 458 (4), 796–801. doi:10.1016/j.bbrc.2015.02.028
Liu, P., Gu, Y., Luo, J., Ye, P., Zheng, Y., Yu, W., et al. (2019). Inhibition of Src Activation Reverses Pulmonary Vascular Remodeling in Experimental Pulmonary Arterial Hypertension via Akt/mTOR/HIF-1 Signaling Pathway. Exp. Cell Res. 380 (1), 36–46. doi:10.1016/j.yexcr.2019.02.022
Liu, S. J., Yin, C. X., Ding, M. C., Wang, Y. Z., and Wang, H. (2015b). Berberine Inhibits Tumor Necrosis Factor-α-Induced Expression of Inflammatory Molecules and Activation of Nuclear Factor-Κb via the Activation of AMPK in Vascular Endothelial Cells. Mol. Med. Rep. 12 (4), 5580–5586. doi:10.3892/mmr.2015.4061
Liu, S. J., Yin, C. X., Ding, M. C., Xia, S. Y., Shen, Q. M., and Wu, J. D. (2014). Berberine Suppresses In Vitro Migration of Human Aortic Smooth Muscle Cells through the Inhibitions of MMP-2/9, u-PA, AP-1, and NF-Κb. BMB Rep. 47 (7), 388–392. doi:10.5483/bmbrep.2014.47.7.186
Liu, W., Zhang, X., Liu, P., Shen, X., Lan, T., Li, W., et al. (2010a). Effects of Berberine on Matrix Accumulation and NF-Kappa B Signal Pathway in Alloxan-Induced Diabetic Mice with Renal Injury. Eur. J. Pharmacol. 638 (1–3), 150–155. doi:10.1016/j.ejphar.2010.04.033
Liu, X., Wei, Y., Bai, X., Li, M., Li, H., Wang, L., et al. (2020). Berberine Prevents Primary Peritoneal Adhesion and Adhesion Reformation by Directly Inhibiting TIMP-1. Acta Pharm. Sin. B. 10 (5), 812–824. doi:10.1016/j.apsb.2020.02.003
Liu, Y. T., Hao, H. P., Xie, H. G., Lai, L., Wang, Q., Liu, C. X., et al. (2010b). Extensive Intestinal First-Pass Elimination and Predominant Hepatic Distribution of Berberine Explain its Low Plasma Levels in Rats. Drug Metab. Dispos. 38 (10), 1779–1784. doi:10.1124/dmd.110.033936
Lockshin, B., Balagula, Y., and Merola, J. F. (2018). Interleukin 17, Inflammation, and Cardiovascular Risk in Patients with Psoriasis. J. Am. Acad. Dermatol. 79 (2), 345–352. doi:10.1016/j.jaad.2018.02.040
Lopes, T. Z., de Moraes, F. R., Tedesco, A. C., Arni, R. K., Rahal, P., and Calmon, M. F. (2020). Berberine Associated Photodynamic Therapy Promotes Autophagy and Apoptosis via ROS Generation in Renal Carcinoma Cells. Biomed. Pharmacother. 123, 109794. doi:10.1016/j.biopha.2019.109794
Lorenzen, J. M., and Thum, T. (2016). Long Noncoding RNAs in Kidney and Cardiovascular Diseases. Nat. Rev. Nephrol. 12 (6), 360–373. doi:10.1038/nrneph.2016.51
Lu, C., Wang, X., Ha, T., Hu, Y., Liu, L., Zhang, X., et al. (2015). Attenuation of Cardiac Dysfunction and Remodeling of Myocardial Infarction by microRNA-130a Are Mediated by Suppression of PTEN and Activation of PI3K Dependent Signaling. J. Mol. Cel. Cardiol. 89 (Pt A), 87–97. doi:10.1016/j.yjmcc.2015.10.011
Lu, L., Qin, Y., Chen, C., and Guo, X. (2018). Beneficial Effects Exerted by Paeonol in the Management of Atherosclerosis. Oxid. Med. Cel. Longev. 2018, 1098617. doi:10.1155/2018/1098617
Lu, Q., Li, X., Liu, J., Sun, X., Rousselle, T., Ren, D., et al. (2019). AMPK Is Associated with the Beneficial Effects of Antidiabetic Agents on Cardiovascular Diseases. Biosci. Rep. 39 (2), BSR20181995. doi:10.1042/BSR20181995
Lundberg, A. K., Chung, R. W. S., Zeijlon, L., Fernström, G., and Jonasson, L. (2021). Oxidative Stress Response in Regulatory and Conventional T Cells: A Comparison between Patients with Chronic Coronary Syndrome and Healthy Subjects. J. Transl. Med. 19 (1), 241. doi:10.1186/s12967-021-02906-2
Luo, G., Lin, X., Li, Z., Xiao, M., Li, X., Zhang, D., et al. (2021). Structure-Guided Modification of Isoxazole-type FXR Agonists: Identification of a Potent and Orally Bioavailable FXR Modulator. Eur. J. Med. Chem. 209, 112910. doi:10.1016/j.ejmech.2020.112910
Luo, J., Gu, Y., Liu, P., Jiang, X., Yu, W., Ye, P., et al. (2018). Berberine Attenuates Pulmonary Arterial Hypertension via Protein Phosphatase 2A Signaling Pathway Both In Vivo and In Vitro. J. Cel. Physiol. 233 (12), 9750–9762. doi:10.1002/jcp.26940
Lyu, J., Wang, L., Bai, X., Du, X., Wei, J., Wang, J., et al. (2021). Treatment of Rheumatoid Arthritis by Serum Albumin Nanoparticles Coated with Mannose to Target Neutrophils. ACS Appl. Mater. Inter. 13 (1), 266–276. doi:10.1021/acsami.0c19468
Ma, J. Y., Feng, R., Tan, X. S., Ma, C., Shou, J. W., Fu, J., et al. (2013). Excretion of Berberine and its Metabolites in Oral Administration in Rats. J. Pharm. Sci. 102 (11), 4181–4192. doi:10.1002/jps.23718
Ma, X., Zhang, T., Luo, Z., Li, X., Lin, M., Li, R., et al. (2020). Functional Nano-Vector Boost Anti-atherosclerosis Efficacy of Berberine in Apoe (-/-) Mice. Acta Pharm. Sin. B. 10 (9), 1769–1783. doi:10.1016/j.apsb.2020.03.005
Ma, Y. G., Liang, L., Zhang, Y. B., Wang, B. F., Bai, Y. G., Dai, Z. J., et al. (2017). Berberine Reduced Blood Pressure and Improved Vasodilation in Diabetic Rats. J. Mol. Endocrinol. 59 (3), 191–204. doi:10.1530/JME-17-0014
Ma, Y. G., Zhang, Y. B., Bai, Y. G., Dai, Z. J., Liang, L., Liu, M., et al. (2016). Berberine Alleviates the Cerebrovascular Contractility in Streptozotocin-Induced Diabetic Rats through Modulation of Intracellular Ca²⁺ Handling in Smooth Muscle Cells. Cardiovasc. Diabetol. 15, 63. doi:10.1186/s12933-016-0382-9
Maier, S., Morlock, J., Benk, C., Kari, F. A., Siepe, M., Beyersdorf, F., et al. (2020). Impact of Intermittent Functional Internal Iliac Artery Occlusion on Spinal Cord Blood Supply during TEVAR. Thorac. Cardiovasc. Surg. 68 (4), 315–321. doi:10.1055/s-0039-1688474
Malik, M., Yang, Y., Fathi, P., Mahler, G. J., and Esch, M. B. (2021). Critical Considerations for the Design of Multi-Organ Microphysiological Systems (MPS). Front. Cell Dev. Biol. 9, 721338. doi:10.3389/fcell.2021.721338
Martinez, M. E., Walton, R. D., Bayer, J. D., Haïssaguerre, M., Vigmond, E. J., Hocini, M., et al. (2018). Role of the Purkinje-Muscle Junction on the Ventricular Repolarization Heterogeneity in the Healthy and Ischemic Ovine Ventricular Myocardium. Front. Physiol. 9, 718. doi:10.3389/fphys.2018.00718
Martini, D., Pucci, C., Gabellini, C., Pellegrino, M., and Andreazzoli, M. (2020). Exposure to the Natural Alkaloid Berberine Affects Cardiovascular System Morphogenesis and Functionality during Zebrafish Development. Sci. Rep. 10 (1), 17358. doi:10.1038/s41598-020-73661-5
Mathiyalagan, P., Adamiak, M., Mayourian, J., Sassi, Y., Liang, Y., Agarwal, N., et al. (2019). FTO-dependent N6-Methyladenosine Regulates Cardiac Function during Remodeling and Repair. Circulation 139 (4), 518–532. doi:10.1161/CIRCULATIONAHA.118.033794
Mbese, Z., Khwaza, V., and Aderibigbe, B. A. (2019). Curcumin and its Derivatives as Potential Therapeutic Agents in Prostate, Colon and Breast Cancers. Molecules 24 (23), 4386. doi:10.3390/molecules24234386
Mi, D. H., Fang, H. J., Zheng, G. H., Liang, X. H., Ding, Y. R., Liu, X., et al. (2019). DPP-4 Inhibitors Promote Proliferation and Migration of Rat Brain Microvascular Endothelial Cells under Hypoxic/High-Glucose Conditions, Potentially through the SIRT1/HIF-1/VEGF Pathway. CNS Neurosci. Ther. 25 (3), 323–332. doi:10.1111/cns.13042
MohanKumar, K., Namachivayam, K., Song, T., Jake Cha, B., Slate, A., Hendrickson, J. E., et al. (2019). A Murine Neonatal Model of Necrotizing Enterocolitis Caused by Anemia and Red Blood Cell Transfusions. Nat. Commun. 10 (1), 3494. doi:10.1038/s41467-019-11199-5
Monteiro, J. P., Bennett, M., Rodor, J., Caudrillier, A., Ulitsky, I., and Baker, A. H. (2019). Endothelial Function and Dysfunction in the Cardiovascular System: The Long Non-coding Road. Cardiovasc. Res. 115 (12), 1692–1704. doi:10.1093/cvr/cvz154
Montero, D., Diaz-Canestro, C., Oberholzer, L., and Lundby, C. (2019). The Role of Blood Volume in Cardiac Dysfunction and Reduced Exercise Tolerance in Patients with Diabetes. Lancet Diabetes Endocrinol. 7 (10), 807–816. doi:10.1016/S2213-8587(19)30119-6
Moreno, J. A., Gomez-Guerrero, C., Mas, S., Sanz, A. B., Lorenzo, O., Ruiz-Ortega, M., et al. (2018). Targeting Inflammation in Diabetic Nephropathy: A Tale of Hope. Expert Opin. Investig. Drugs 27 (11), 917–930. doi:10.1080/13543784.2018.1538352
Nagel, D. J., Aizawa, T., Jeon, K. I., Liu, W., Mohan, A., Wei, H., et al. (2006). Role of Nuclear Ca2+/Calmodulin-Stimulated Phosphodiesterase 1A in Vascular Smooth Muscle Cell Growth and Survival. Circ. Res. 98 (6), 777–784. doi:10.1161/01.RES.0000215576.27615.fd
Neag, M. A., Mocan, A., Echeverría, J., Pop, R. M., Bocsan, C. I., Crişan, G., et al. (2018). Berberine: Botanical Occurrence, Traditional Uses, Extraction Methods, and Relevance in Cardiovascular, Metabolic, Hepatic, and Renal Disorders. Front. Pharmacol. 9, 557. doi:10.3389/fphar.2018.00557
Nobili, A., Latagliata, E. C., Viscomi, M. T., Cavallucci, V., Cutuli, D., Giacovazzo, G., et al. (2017). Dopamine Neuronal Loss Contributes to Memory and Reward Dysfunction in a Model of Alzheimer's Disease. Nat. Commun. 8, 14727. doi:10.1038/ncomms14727
Noh, H., Yu, M. R., Kim, H. J., Lee, J. H., Park, B. W., Wu, I. H., et al. (2017). Beta 2-Adrenergic Receptor Agonists Are Novel Regulators of Macrophage Activation in Diabetic Renal and Cardiovascular Complications. Kidney Int. 92 (1), 101–113. doi:10.1016/j.kint.2017.02.013
O'Brien, R. J., and Wong, P. C. (2011). Amyloid Precursor Protein Processing and Alzheimer's Disease. Annu. Rev. Neurosci. 34, 185–204. doi:10.1146/annurev-neuro-061010-113613
Oduro, P. K., Fang, J., Niu, L., Li, Y., Li, L., Zhao, X., et al. (2020). Pharmacological Management of Vascular Endothelial Dysfunction in Diabetes: TCM and Western Medicine Compared Based on Biomarkers and Biochemical Parameters. Pharmacol. Res. 158, 104893. doi:10.1016/j.phrs.2020.104893
Oesterle, A., Laufs, U., and Liao, J. K. (2017). Pleiotropic Effects of Statins on the Cardiovascular System. Circ. Res. 120 (1), 229–243. doi:10.1161/CIRCRESAHA.116.308537
Olesen, K. K. W., Gyldenkerne, C., Thim, T., Thomsen, R. W., and Maeng, M. (2021). Peripheral Artery Disease, Lower Limb Revascularization, and Amputation in Diabetes Patients with and without Coronary Artery Disease: A Cohort Study from the Western Denmark Heart Registry. BMJ Open Diabetes Res. Care 9 (1), e001803. doi:10.1136/bmjdrc-2020-001803
Ottolini, M., Hong, K., Cope, E. L., Daneva, Z., DeLalio, L. J., Sokolowski, J. D., et al. (2020). Local Peroxynitrite Impairs Endothelial Transient Receptor Potential Vanilloid 4 Channels and Elevates Blood Pressure in Obesity. Circulation 141 (16), 1318–1333. doi:10.1161/CIRCULATIONAHA.119.043385
Ottolini, M., Hong, K., and Sonkusare, S. K. (2019). Calcium Signals that Determine Vascular Resistance. Wiley Interdiscip. Rev. Syst. Biol. Med. 11 (5), e1448. doi:10.1002/wsbm.1448
Parikh, M., Kura, B., O'Hara, K. A., Dibrov, E., Netticadan, T., Slezak, J., et al. (2020). Cardioprotective Effects of Dietary Flaxseed Post-Infarction Are Associated with Changes in MicroRNA Expression. Biomolecules 10 (9), 1297. doi:10.3390/biom10091297
Paul, M., Hemshekhar, M., Kemparaju, K., and Girish, K. S. (2019). Berberine Mitigates High Glucose-Potentiated Platelet Aggregation and Apoptosis by Modulating Aldose Reductase and NADPH Oxidase Activity. Free. Radic. Biol. Med. 130, 196–205. doi:10.1016/j.freeradbiomed.2018.10.453
Pearson, E. R. (2019). Type 2 Diabetes: A Multifaceted Disease. Diabetologia 62 (7), 1107–1112. doi:10.1007/s00125-019-4909-y
Petrie, J. R., Guzik, T. J., and Touyz, R. M. (2018). Diabetes, Hypertension, and Cardiovascular Disease: Clinical Insights and Vascular Mechanisms. Can. J. Cardiol. 34 (5), 575–584. doi:10.1016/j.cjca.2017.12.005
Pierelli, G., Stanzione, R., Forte, M., Migliarino, S., Perelli, M., Volpe, M., et al. (2017). Uncoupling Protein 2: A Key Player and a Potential Therapeutic Target in Vascular Diseases. Oxid. Med. Cel. Longev. 2017, 7348372. doi:10.1155/2017/7348372
Poh, L., Razak, S. M. B. A., Lim, H. M., Lai, M. K. P., Chen, C. L., Lim, L. H. K., et al. (2021). AIM2 Inflammasome Mediates Apoptotic and Pyroptotic Death in the Cerebellum Following Chronic Hypoperfusion. Exp. Neurol. 346, 113856. doi:10.1016/j.expneurol.2021.113856
Pyšná, A., Bém, R., Němcová, A., Fejfarová, V., Jirkovská, A., Hazdrová, J., et al. (2019). Endothelial Progenitor Cells Biology in Diabetes Mellitus and Peripheral Arterial Disease and Their Therapeutic Potential. Stem Cell Rev Rep 15 (2), 157–165. doi:10.1007/s12015-018-9863-4
Qiu, F., Zhu, Z., Kang, N., Piao, S., Qin, G., and Yao, X. (2008). Isolation and Identification of Urinary Metabolites of Berberine in Rats and Humans. Drug Metab. Dispos. 36 (11), 2159–2165. doi:10.1124/dmd.108.021659
Qiu, H., Wu, Y., Wang, Q., Liu, C., Xue, L., Wang, H., et al. (2017). Effect of Berberine on PPARα-NO Signalling Pathway in Vascular Smooth Muscle Cell Proliferation Induced by Angiotensin IV. Pharm. Biol. 55 (1), 227–232. doi:10.1080/13880209.2016.1257642
Rajabi, S., Najafipour, H., Jafarinejad-Farsangi, S., Joukar, S., Beik, A., Askaripour, M., et al. (2021). Quercetin, Perillyl Alcohol, and Berberine Ameliorate Right Ventricular Disorders in Experimental Pulmonary Arterial Hypertension: Effects on miR-204, miR-27a, Fibrotic, Apoptotic, and Inflammatory Factors. J. Cardiovasc. Pharmacol. 77 (6), 777–786. doi:10.1097/FJC.0000000000001015
Raza, Z., Saleem, U., and Naureen, Z. (2020). Sphingosine 1-Phosphate Signaling in Ischemia and Reperfusion Injury. Prostaglandins Other Lipid Mediat 149, 106436. doi:10.1016/j.prostaglandins.2020.106436
Reddy, M. A., Zhang, E., and Natarajan, R. (2015). Epigenetic Mechanisms in Diabetic Complications and Metabolic Memory. Diabetologia 58 (3), 443–455. doi:10.1007/s00125-014-3462-y
Ren, J., Bi, Y., Sowers, J. R., Hetz, C., and Zhang, Y. (2021). Endoplasmic Reticulum Stress and Unfolded Protein Response in Cardiovascular Diseases. Nat. Rev. Cardiol. 18 (7), 499–521. doi:10.1038/s41569-021-00511-w
Ren, J., Fu, L., Nile, S. H., Zhang, J., and Kai, G. (2019). Salvia Miltiorrhiza in Treating Cardiovascular Diseases: A Review on its Pharmacological and Clinical Applications. Front. Pharmacol. 10, 753. doi:10.3389/fphar.2019.00753
Reuter, S., Gupta, S. C., Chaturvedi, M. M., and Aggarwal, B. B. (2010). Oxidative Stress, Inflammation, and Cancer: How Are They Linked? Free Radic. Biol. Med. 49 (11), 1603–1616. doi:10.1016/j.freeradbiomed.2010.09.006
Riccardi, G., Giosuè, A., Calabrese, I., and Vaccaro, O. (2021). Dietary Recommendations for Prevention of Atherosclerosis. Cardiovasc. Res. Cvab 173, 1. doi:10.1093/cvr/cvab173
Robles-Rivera, R. R., Castellanos-González, J. A., Olvera-Montaño, C., Flores-Martin, R. A., López-Contreras, A. K., Arevalo-Simental, D. E., et al. (2020). Adjuvant Therapies in Diabetic Retinopathy as an Early Approach to Delay its Progression: The Importance of Oxidative Stress and Inflammation. Oxid. Med. Cel. Longev. 2020, 3096470. doi:10.1155/2020/3096470
Rothbauer, M., Zirath, H., and Ertl, P. (2018). Recent Advances in Microfluidic Technologies for Cell-To-Cell Interaction Studies. Lab. Chip 18 (2), 249–270. doi:10.1039/c7lc00815e
Russo, L., and Lumeng, C. N. (2018). Properties and Functions of Adipose Tissue Macrophages in Obesity. Immunology 155 (4), 407–417. doi:10.1111/imm.13002
Ryuk, J. A., Zheng, M. S., Lee, M. Y., Seo, C. S., Li, Y., Lee, S. H., et al. (2012). Discrimination of Phellodendron Amurense and P. Chinense Based on DNA Analysis and the Simultaneous Analysis of Alkaloids. Arch. Pharm. Res. 35 (6), 1045–1054. doi:10.1007/s12272-012-0612-y
Safar, M. E. (2018). Arterial Stiffness as a Risk Factor for Clinical Hypertension. Nat. Rev. Cardiol. 15 (2), 97–105. doi:10.1038/nrcardio.2017.155
Sahibzada, M. U. K., Zahoor, M., Sadiq, A., Ur Rehman, F., Al-Mohaimeed, A. M., Shahid, M., et al. (2021). Bioavailability and Hepatoprotection Enhancement of Berberine and its Nanoparticles Prepared by Liquid Antisolvent Method. Saudi J. Biol. Sci. 28 (1), 327–332. doi:10.1016/j.sjbs.2020.10.006
Saltiel, A. R., and Olefsky, J. M. (2017). Inflammatory Mechanisms Linking Obesity and Metabolic Disease. J. Clin. Invest. 127 (1), 1–4. doi:10.1172/JCI92035
Salvio, G., Ciarloni, A., Cutini, M., and Balercia, G. (2021). Hyperhomocysteinemia: Focus on Endothelial Damage as a Cause of Erectile Dysfunction. Ijms 22 (1), 418. doi:10.3390/ijms22010418
Searls, Y. M., Loganathan, R., Smirnova, I. V., and Stehno-Bittel, L. (2010). Intracellular Ca2+ Regulating Proteins in Vascular Smooth Muscle Cells Are Altered with Type 1 Diabetes Due to the Direct Effects of Hyperglycemia. Cardiovasc. Diabetol. 9, 8. doi:10.1186/1475-2840-9-8
Seki, T., Goto, K., Kiyohara, K., Kansui, Y., Murakami, N., Haga, Y., et al. (2017). Downregulation of Endothelial Transient Receptor Potential Vanilloid Type 4 Channel and Small-Conductance of Ca2+-Activated K+ Channels Underpins Impaired Endothelium-dependent Hyperpolarization in Hypertension. Hypertension 69 (1), 143–153. doi:10.1161/HYPERTENSIONAHA.116.07110
Shan, Y. Q., Ren, G., Wang, Y. X., Pang, J., Zhao, Z. Y., Yao, J., et al. (2013). Berberine Analogue IMB-Y53 Improves Glucose-Lowering Efficacy by Averting Cellular Efflux Especially P-Glycoprotein Efflux. Metabolism 62 (3), 446–456. doi:10.1016/j.metabol.2012.09.009
Sharaky, M., Kamel, M., Aziz, M. A., Omran, M., Rageh, M. M., Abouzid, K. A. M., et al. (2020). Design, Synthesis and Biological Evaluation of a New Thieno[2,3-D]pyrimidine-Based Urea Derivative with Potential Antitumor Activity against Tamoxifen Sensitive and Resistant Breast Cancer Cell Lines. J. Enzyme Inhib. Med. Chem. 35 (1), 1641–1656. doi:10.1080/14756366.2020.1804383
Sharifi Kia, D., Kim, K., and Simon, M. A. (2021). Current Understanding of the Right Ventricle Structure and Function in Pulmonary Arterial Hypertension. Front. Physiol. 12, 641310. doi:10.3389/fphys.2021.641310
Singh, S., Pathak, N., Fatima, E., and Negi, A. S. (2021). Plant Isoquinoline Alkaloids: Advances in the Chemistry and Biology of Berberine. Eur. J. Med. Chem. 226, 11389. doi:10.1016/j.ejmech.2021.113839
Sitia, S., Tomasoni, L., Atzeni, F., Ambrosio, G., Cordiano, C., Catapano, A., et al. (2010). From Endothelial Dysfunction to Atherosclerosis. Autoimmun. Rev. 9 (12), 830–834. doi:10.1016/j.autrev.2010.07.016
Spangenberg, E. E., Lee, R. J., Najafi, A. R., Rice, R. A., Elmore, M. R., Blurton-Jones, M., et al. (2016). Eliminating Microglia in Alzheimer's Mice Prevents Neuronal Loss without Modulating Amyloid-β Pathology. Brain 139 (Pt 4), 1265–1281. doi:10.1093/brain/aww016
Spinozzi, S., Colliva, C., Camborata, C., Roberti, M., Ianni, C., Neri, F., et al. (2014). Berberine and its Metabolites: Relationship between Physicochemical Properties and Plasma Levels after Administration to Human Subjects. J. Nat. Prod. 77 (4), 766–772. doi:10.1021/np400607k
Sun, I. O., Santelli, A., Abumoawad, A., Eirin, A., Ferguson, C. M., Woollard, J. R., et al. (2016). Loss of Renal Peritubular Capillaries in Hypertensive Patients Is Detectable by Urinary Endothelial Microparticle Levels. Hypertension 72 (5), 1180–1188. doi:10.1161/HYPERTENSIONAHA.118.11766
Sun, Y., Wang, C., Zhang, N., and Liu, F. (2021). Melatonin Ameliorates Hypertension in Hypertensive Pregnant Mice and Suppresses the Hypertension-Induced Decrease in Ca2+-Activated K+ Channels in Uterine Arteries. Hypertens. Res. 44 (9), 1079–1086. doi:10.1038/s41440-021-00675-5
Tabas, I. (2010). The Role of Endoplasmic Reticulum Stress in the Progression of Atherosclerosis. Circ. Res. 107 (7), 839–850. doi:10.1161/CIRCRESAHA.110.224766
Tan, N., Zhang, Y., Zhang, Y., Li, L., Zong, Y., Han, W., et al. (2021). Berberine Ameliorates Vascular Dysfunction by a Global Modulation of lncRNA and mRNA Expression Profiles in Hypertensive Mouse Aortae. PLoS One 16 (2), e0247621. doi:10.1371/journal.pone.0247621
Tan, W., Wang, Y., Wang, K., Wang, S., Liu, J., Qin, X., et al. (2020). Improvement of Endothelial Dysfunction of Berberine in Atherosclerotic Mice and Mechanism Exploring through TMT-Based Proteomics. Oxid. Med. Cel. Longev. 2020, 8683404. doi:10.1155/2020/8683404
Tan, X. S., Ma, J. Y., Feng, R., Ma, C., Chen, W. J., Sun, Y. P., et al. (2013). Tissue Distribution of Berberine and its Metabolites after Oral Administration in Rats. PLoS One 8 (10), e77969. doi:10.1371/journal.pone.0077969
Tang, L. Q., Ni, W. J., Cai, M., Ding, H. H., Liu, S., and Zhang, S. T. (2016). Renoprotective Effects of Berberine and its Potential Effect on the Expression of β-arrestins and Intercellular Adhesion Molecule-1 and Vascular Cell Adhesion Molecule-1 in Streptozocin-Diabetic Nephropathy Rats. J. Diabetes 8 (5), 693–700. doi:10.1111/1753-0407.12349
Tang, S., Fan, C., Iroegbu, C. D., Zhou, W., Zhang, Z., Wu, M., et al. (2021). TMSB4 Overexpression Enhances the Potency of Marrow Mesenchymal Stromal Cells for Myocardial Repair. Front. Cell Dev. Biol. 9, 670913. doi:10.3389/fcell.2021.670913
Tang, S. C. W., and Yiu, W. H. (2020). Innate Immunity in Diabetic Kidney Disease. Nat. Rev. Nephrol. 16 (4), 206–222. doi:10.1038/s41581-019-0234-4
Tavares, A. K. M. M., Ribas, S. A., Paravidino, V. B., Sgambato, M. R., Rodrigues, R. D. R. M., da Rocha, C. M. M., et al. (2021). Effect of Phytosterol Capsule Supplementation Associated with the National Cholesterol Education Program Step 2 Diet on Low-Density Lipoprotein in Children and Adolescents with Dyslipidemia: A Double-Blind Crossover Trial. Nutrition 82, 111051. doi:10.1016/j.nut.2020.111051
Tavernier, G., Caspar-Bauguil, S., and Viguerie, N. (2020). Apolipoprotein M: New Connections with Diet, Adipose Tissue and Metabolic Syndrome. Curr. Opin. Lipidol. 31 (1), 8–14. doi:10.1097/MOL.0000000000000654
Toledo, C., Thomas, G., Schold, J. D., Arrigain, S., Gornik, H. L., Nally, J. V., et al. (2015). Renal Resistive Index and Mortality in Chronic Kidney Disease. Hypertension 66 (2), 382–388. doi:10.1161/HYPERTENSIONAHA.115.05536
Tong, L., Xie, C., Wei, Y., Qu, Y., Liang, H., Zhang, Y., et al. (2019). Antitumor Effects of Berberine on Gliomas via Inactivation of Caspase-1-Mediated IL-1β and IL-18 Release. Front. Oncol. 9, 364. doi:10.3389/fonc.2019.00364
Treviño-Saldaña, N., and García-Rivas, G. (2017). Regulation of Sirtuin-Mediated Protein Deacetylation by Cardioprotective Phytochemicals. Oxid. Med. Cel. Longev. 2017, 1750306. doi:10.1155/2017/1750306
Tsai, J. M., Sinha, R., Seita, J., Fernhoff, N., Christ, S., Koopmans, T., et al. (2018). Surgical Adhesions in Mice Are Derived from Mesothelial Cells and Can Be Targeted by Antibodies against Mesothelial Markers. Sci. Transl. Med. 10 (469), eaan6735. doi:10.1126/scitranslmed.aan6735
van Dijk, L. J. D., Terlouw, L. G., vanNoord, D., Bijdevaate, D. C., Bruno, M. J., and Moelker, A. (2020). Endovascular Pressure Measurements to Assess the Functional Severity of Mesenteric Arterial Stenoses. J. Vasc. Interv. Radiol. 31 (3), 430–437. doi:10.1016/j.jvir.2019.10.019
Vanhoutte, P. M., Feletou, M., and Taddei, S. (2005). Endothelium-Dependent Contractions in Hypertension. Br. J. Pharmacol. 144 (4), 449–458. doi:10.1038/sj.bjp.0706042
Vanhoutte, P. M., Shimokawa, H., Feletou, M., and Tang, E. H. (2017). Endothelial Dysfunction and Vascular Disease - a 30th Anniversary Update. Acta Physiol. (Oxf) 219 (1), 22–96. doi:10.1111/apha.12646
Vara, D., Cifuentes-Pagano, E., Pagano, P. J., and Pula, G. (2019). A Novel Combinatorial Technique for Simultaneous Quantification of Oxygen Radicals and Aggregation Reveals Unexpected Redox Patterns in the Activation of Platelets by Different Physiopathological Stimuli. Haematologica 104 (9), 1879–1891. doi:10.3324/haematol.2018.208819
Verhaar, B. J. H., Prodan, A., Nieuwdorp, M., and Muller, M. (2020). Gut Microbiota in Hypertension and Atherosclerosis: A Review. Nutrients 12 (10), 2982. doi:10.3390/nu12102982
Waclawovsky, G., Boll, L. F. C., Eibel, B., Alegretti, A. P., Spagnol, F., De Paoli, J., et al. (2021). Individuals with Controlled Hypertension Show Endothelial Integrity Following a Bout of Moderate-Intensity Exercise: Randomized Clinical Trial. Sci. Rep. 11 (1), 8528. doi:10.1038/s41598-021-87990-6
Wande, Y., Jie, L., Aikai, Z., Yaguo, Z., Linlin, Z., Yue, G., et al. (2020). Berberine Alleviates Pulmonary Hypertension through Trx1 and β-catenin Signaling Pathways in Pulmonary Artery Smooth Muscle Cells. Exp. Cel. Res. 390 (1), 111910. doi:10.1016/j.yexcr.2020.111910
Wang, C., Dai, X., Wu, S., Xu, W., Song, P., and Huang, K. (2021). FUNDC1-Dependent Mitochondria-Associated Endoplasmic Reticulum Membranes Are Involved in Angiogenesis and Neoangiogenesis. Nat. Commun. 12 (1), 2616. doi:10.1038/s41467-021-22771-3
Wang, J., Guo, T., Peng, Q. S., Yue, S. W., and Wang, S. X. (2015). Berberine via Suppression of Transient Receptor Potential Vanilloid 4 Channel Improves Vascular Stiffness in Mice. J. Cel. Mol. Med. 19 (11), 2607–2616. doi:10.1111/jcmm.12645
Wang, J., Wang, L., Lou, G. H., Zeng, H. R., Hu, J., Huang, Q. W., et al. (2019). Coptidis Rhizoma: A Comprehensive Review of its Traditional Uses, Botany, Phytochemistry, Pharmacology and Toxicology. Pharm. Biol. 57 (1), 193–225. doi:10.1080/13880209.2019.1577466
Wang, L., Deng, L., Lin, N., Shi, Y., Chen, J., Zhou, Y., et al. (2020). Berberine Inhibits Proliferation and Apoptosis of Vascular Smooth Muscle Cells Induced by Mechanical Stretch via the PDI/ERS and MAPK Pathways. Life Sci. 259, 118253. doi:10.1016/j.lfs.2020.118253
Wang, Q., Zhang, M., Liang, B., Shirwany, N., Zhu, Y., and Zou, M. H. (2011). Activation of AMP-Activated Protein Kinase Is Required for Berberine-Induced Reduction of Atherosclerosis in Mice: The Role of Uncoupling Protein 2. PLoS One 6 (9), e25436. doi:10.1371/journal.pone.0025436
Wang, S., Binder, P., Fang, Q., Wang, Z., Xiao, W., Liu, W., et al. (2018). Endoplasmic Reticulum Stress in the Heart: Insights into Mechanisms and Drug Targets. Br. J. Pharmacol. 175 (8), 1293–1304. doi:10.1111/bph.13888
Wang, Y., and Ding, Y. (2015). Berberine Protects Vascular Endothelial Cells in Hypertensive Rats. Int. J. Clin. Exp. Med. 8 (9), 14896–14905.
Wang, Y., Huang, Y., Lam, K. S., Li, Y., Wong, W. T., Ye, H., et al. (2009). Berberine Prevents Hyperglycemia-Induced Endothelial Injury and Enhances Vasodilatation via Adenosine Monophosphate-Activated Protein Kinase and Endothelial Nitric Oxide Synthase. Cardiovasc. Res. 82 (3), 484–492. doi:10.1093/cvr/cvp078
Wang, Z., Chen, Z., Yang, S., Wang, Y., Huang, Z., Gao, J., et al. (2014). Berberine Ameliorates Collagen-Induced Arthritis in Rats Associated with Anti-inflammatory and Anti-angiogenic Effects. Inflammation 37 (5), 1789–1798. doi:10.1007/s10753-014-9909-y
Wolf, D., and Ley, K. (2019). Immunity and Inflammation in Atherosclerosis. Circ. Res. 124 (2), 315–327. doi:10.1161/CIRCRESAHA.118.313591
Xiang, R., Chen, J., Li, S., Yan, H., Meng, Y., Cai, J., et al. (2020). VSMC-specific Deletion of FAM3A Attenuated Ang II-Promoted Hypertension and Cardiovascular Hypertrophy. Circ. Res. 126 (12), 1746–1759. doi:10.1161/CIRCRESAHA.119.315558
Xiao, D., Liu, Z., Zhang, S., Zhou, M., He, F., Zou, M., et al. (2018). Berberine Derivatives with Different Pharmacological Activities via Structural Modifications. Mini Rev. Med. Chem. 18 (17), 1424–1441. doi:10.2174/1389557517666170321103139
Xie, W., Zhu, T., Dong, X., Nan, F., Meng, X., Zhou, P., et al. (2019). HMGB1-triggered Inflammation Inhibition of Notoginseng Leaf Triterpenes against Cerebral Ischemia and Reperfusion Injury via MAPK and NF-Κb Signaling Pathways. Biomolecules 9 (10), 512. doi:10.3390/biom9100512
Xu, H. Y., Liu, C. S., Huang, C. L., Chen, L., Zheng, Y. R., Huang, S. H., et al. (2019). Nanoemulsion Improves Hypoglycemic Efficacy of Berberine by Overcoming its Gastrointestinal Challenge. Colloids Surf. B Biointerfaces. 181, 927–934. doi:10.1016/j.colsurfb.2019.06.006
Xu, M., Qi, Q., Men, L., Wang, S., Li, M., Xiao, M., et al. (2020). Berberine Protects Kawasaki Disease-Induced Human Coronary Artery Endothelial Cells Dysfunction by Inhibiting of Oxidative and Endoplasmic Reticulum Stress. Vascul. Pharmacol. 127, 106660. doi:10.1016/j.vph.2020.106660
Xu, R. X., Sun, X. C., Ma, C. Y., Yao, Y. H., Li, X. L., Guo, Y. L., et al. (2017). Impacts of Berberine on Oxidized LDL-Induced Proliferation of Human Umbilical Vein Endothelial Cells. Am. J. Transl. Res. 9 (10), 4375–4389.
Xue, Y., Fu, W., Liu, Y., Yu, P., Sun, M., Li, X., et al. (2020). Ginsenoside Rb2 Alleviates Myocardial Ischemia/Reperfusion Injury in Rats through SIRT1 Activation. J. Food Sci. 85 (11), 4039–4049. doi:10.1111/1750-3841.15505
Yahuafai, J., Asai, T., Oku, N., and Siripong, P. (2018). Anticancer Efficacy of the Combination of Berberine and PEGylated Liposomal Doxorubicin in Meth A Sarcoma-Bearing Mice. Biol. Pharm. Bull. 41 (7), 1103–1106. doi:10.1248/bpb.b17-00989
Yang, G., Chang, C. C., Yang, Y., Yuan, L., Xu, L., Ho, C. T., et al. (2018). Resveratrol Alleviates Rheumatoid Arthritis via Reducing ROS and Inflammation, Inhibiting MAPK Signaling Pathways, and Suppressing Angiogenesis. J. Agric. Food Chem. 66 (49), 12953–12960. doi:10.1021/acs.jafc.8b05047
Yang, H., Chen, X. Y., Kuang, S. J., Zhou, M. Y., Zhang, L., Zeng, Z., et al. (2020). Abnormal Ca2+ Handling Contributes to the Impairment of Aortic Smooth Muscle Contractility in Zucker Diabetic Fatty Rats. J. Mol. Cel. Cardiol. 141, 82–92. doi:10.1016/j.yjmcc.2020.03.009
Yang, X., Wang, L., Zhang, Z., Hu, J., Liu, X., Wen, H., et al. (2021). Ginsenoside Rb1 Enhances Plaque Stability and Inhibits Adventitial Vasa Vasorum via the Modulation of miR-33 and PEDF. Front. Cardiovasc. Med. 8, 654670. doi:10.3389/fcvm.2021.654670
Ye, C., Liang, Y., Chen, Y., Xiong, Y., She, Y., Zhong, X., et al. (2021). Berberine Improves Cognitive Impairment by Simultaneously Impacting Cerebral Blood Flow and β-Amyloid Accumulation in an APP/tau/PS1 Mouse Model of Alzheimer's Disease. Cells 10 (5), 1161. doi:10.3390/cells10051161
Ye, L., Liang, S., Guo, C., Yu, X., Zhao, J., Zhang, H., et al. (2016). Inhibition of M1 Macrophage Activation in Adipose Tissue by Berberine Improves Insulin Resistance. Life Sci. 166, 82–91. doi:10.1016/j.lfs.2016.09.025
Yin, S., Bai, W., Li, P., Jian, X., Shan, T., Tang, Z., et al. (2019). Berberine Suppresses the Ectopic Expression of miR-133a in Endothelial Cells to Improve Vascular Dementia in Diabetic Rats. Clin. Exp. Hypertens. 41 (8), 708–716. doi:10.1080/10641963.2018.1545846
Yin, Z., Tan, R., Yuan, T., Chen, S., Quan, Y., Hao, Q., et al. (2021). Berberine Prevents Diabetic Retinopathy through Inhibiting HIF-1α/VEGF/NF-κ B Pathway in Db/db Mice. Pharmazie 76 (4), 165–171. doi:10.1691/ph.2021.01012
Yu, L., Li, Q., Yu, B., Yang, Y., Jin, Z., Duan, W., et al. (2016). Berberine Attenuates Myocardial Ischemia/Reperfusion Injury by Reducing Oxidative Stress and Inflammation Response: Role of Silent Information Regulator 1. Oxid. Med. Cel. Longev 2016, 1689602. doi:10.1155/2016/1689602
Zhai, J., Li, Z., Zhang, H., Ma, L., Ma, Z., Zhang, Y., et al. (2020). Berberine Protects against Diabetic Retinopathy by Inhibiting Cell Apoptosis via Deactivation of the NF-κB S-ignaling P-athway. Mol. Med. Rep. 22 (5), 4227–4235. doi:10.3892/mmr.2020.11505
Zhang, C., Zhao, R., Yan, W., Wang, H., Jia, M., Zhu, N., et al. (2016a). Compositions, Formation Mechanism, and Neuroprotective Effect of Compound Precipitation from the Traditional Chinese Prescription Huang-Lian-Jie-Du-Tang. Molecules 21 (8), 1094. doi:10.3390/molecules21081094
Zhang, C. Y., Hu, Y. C., Zhang, Y., Ma, W. D., Song, Y. F., Quan, X. H., et al. (2021a). Glutamine Switches Vascular Smooth Muscle Cells to Synthetic Phenotype through Inhibiting miR-143 Expression and Upregulating THY1 Expression. Life Sci. 277, 119365. doi:10.1016/j.lfs.2021.119365
Zhang, G., Lin, X., Shao, Y., Su, C., Tao, J., and Liu, X. (2020). Berberine Reduces Endothelial Injury and Arterial Stiffness in Spontaneously Hypertensive Rats. Clin. Exp. Hypertens. 42 (3), 257–265. doi:10.1080/10641963.2019.1632339
Zhang, H., Zhao, C., Cao, G., Guo, L., Zhang, S., Liang, Y., et al. (2017). Berberine Modulates Amyloid-β Peptide Generation by Activating AMP-Activated Protein Kinase. Neuropharmacology 125, 408–417. doi:10.1016/j.neuropharm.2017.08.013
Zhang, J., Yin, J., Wang, Y., Li, B., and Zeng, X. (2018). Apelin Impairs Myogenic Response to Induce Diabetic Nephropathy in Mice. FASEB J. 32 (8), 4315–4327. doi:10.1096/fj.201701257R
Zhang, L., Wu, X., Yang, R., Chen, F., Liao, Y., Zhu, Z., et al. (2021b). Effects of Berberine on the Gastrointestinal Microbiota. Front. Cel. Infect. Microbiol. 10, 588517. doi:10.3389/fcimb.2020.588517
Zhang, S., Wang, X., Yin, W., Liu, Z., Zhou, M., Xiao, D., et al. (2016b). Synthesis and Hypoglycemic Activity of 9-O-(lipophilic Group Substituted) Berberine Derivatives. Bioorg. Med. Chem. Lett. 26 (19), 4799–4803. doi:10.1016/j.bmcl.2016.08.027
Zhang, X., Qiu, F., Jiang, J., Gao, C., and Tan, Y. (2011). Intestinal Absorption Mechanisms of Berberine, Palmatine, Jateorhizine, and Coptisine: Involvement of P-Glycoprotein. Xenobiotica 41 (4), 290–296. doi:10.3109/00498254.2010.529180
Zhang, Y., and Moran, A. E. (2017). Trends in the Prevalence, Awareness, Treatment, and Control of Hypertension Among Young Adults in the United States, 1999 to 2014. Hypertension 70 (4), 736–742. doi:10.1161/HYPERTENSIONAHA.117.09801
Zhao, C., Su, P., Lv, C., Guo, L., Cao, G., Qin, C., et al. (2019a). Berberine Alleviates Amyloid β-Induced Mitochondrial Dysfunction and Synaptic Loss. Oxid. Med. Cel. Longev. 2019, 7593608. doi:10.1155/2019/7593608
Zhao, G. L., Yu, L. M., Gao, W. L., Duan, W. X., Jiang, B., Liu, X. D., et al. (2016). Berberine Protects Rat Heart from Ischemia/Reperfusion Injury via Activating JAK2/STAT3 Signaling and Attenuating Endoplasmic Reticulum Stress. Acta Pharmacol. Sin. 37 (3), 354–367. doi:10.1038/aps.2015.136
Zhao, L., Liu, S., Wang, M., Zhi, M., Geng, X., Hou, C., et al. (2019b). Berberine Restored Nitrergic and Adrenergic Function in Mesenteric and Iliac Arteries from Streptozotocin-Induced Diabetic Rats. J. Ethnopharmacol. 244, 112140. doi:10.1016/j.jep.2019.112140
Zhao, M. M., Lu, J., Li, S., Wang, H., Cao, X., Li, Q., et al. (2021a). Berberine Is an Insulin Secretagogue Targeting the KCNH6 Potassium Channel. Nat. Commun. 12 (1), 5616. doi:10.1038/s41467-021-25952-2
Zhao, X., Zhang, J., Tong, N., Chen, Y., and Luo, Y. (2012). Protective Effects of Berberine on Doxorubicin-Induced Hepatotoxicity in Mice. Biol. Pharm. Bull. 35 (5), 796–800. doi:10.1248/bpb.35.796
Zhao, Y., Tian, X., Liu, G., Wang, K., Xie, Y., and Qiu, Y. (2019c). Berberine Protects Myocardial Cells against Anoxia-Reoxygenation Injury via P38 MAPK-Mediated NF-Κb Signaling Pathways. Exp. Ther. Med. 17 (1), 230–236. doi:10.3892/etm.2018.6949
Zhao, Y., Ye, S., Lin, J., Liang, F., Chen, J., Hu, J., et al. (2021b). NmFGF1-Regulated Glucolipid Metabolism and Angiogenesis Improves Functional Recovery in a Mouse Model of Diabetic Stroke and Acts via the AMPK Signaling Pathway. Front. Pharmacol. 12, 680351. doi:10.3389/fphar.2021.680351
Zhong, J., Yu, R., Zhou, Q., Liu, P., Liu, Z., and Bian, Y. (2021). Naringenin Prevents TNF-α-Induced Gut-Vascular Barrier Disruption Associated with Inhibiting the NF-Κb-Mediated MLCK/p-MLC and NLRP3 Pathways. Food Funct. 12 (6), 2715–2725. doi:10.1039/d1fo00155h
Zhou, B., Perel, P., Mensah, G. A., and Ezzati, M. (2021). Global Epidemiology, Health Burden and Effective Interventions for Elevated Blood Pressure and Hypertension. Nat. Rev. Cardiol. 18, 785–802. doi:10.1038/s41569-021-00559-8
Zhu, L., Zhang, D., Zhu, H., Zhu, J., Weng, S., Dong, L., et al. (2018). Berberine Treatment Increases Akkermansia in the Gut and Improves High-Fat Diet-Induced Atherosclerosis in Apoe-/- Mice. Atherosclerosis 268, 117–126. doi:10.1016/j.atherosclerosis.2017.11.023
Keywords: berberine, cardiovascular disease, cerebrovascular disease, diabetes mellitus, pharmacokinetics
Citation: Ai X, Yu P, Peng L, Luo L, Liu J, Li S, Lai X, Luan F and Meng X (2021) Berberine: A Review of its Pharmacokinetics Properties and Therapeutic Potentials in Diverse Vascular Diseases. Front. Pharmacol. 12:762654. doi: 10.3389/fphar.2021.762654
Received: 24 August 2021; Accepted: 20 October 2021;
Published: 03 November 2021.
Edited by:
Yusof Kamisah, Faculty of Medicine Universiti Kebangaan Malaysia, MalaysiaReviewed by:
Nandakumar Natarajan, University of California San Francisco, United StatesJiong-Wei Wang, National University of Singapore, Singapore
Copyright © 2021 Ai, Yu, Peng, Luo, Liu, Li, Lai, Luan and Meng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xianli Meng, xlm999@cdutcm.edu.cn; Fei Luan, luanfeiren@163.com.
 Xiaopeng Ai
Xiaopeng Ai Peiling Yu2
Peiling Yu2 Liuling Luo
Liuling Luo Xianli Meng
Xianli Meng