- 1Department of Community Medicine, International Medical School, Management and Science University, Kuala Lumpur, Malaysia
- 2Global Public Health, Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Bandar Sunway, Malaysia
- 3Department of Public Health, Faculty of Medicine, Asia Metropolitan University, Johor, Malaysia
- 4South East Asia Community Observatory, Monash University Malaysia, Bandar Sunway, Malaysia
- 5Department of Community Medicine, Faculty of Medicine, Manipal University College Malaysia, Melaka, Malaysia
- 6Department of Dentistry, Kabul University of Medical Sciences, Kabul, Afghanistan
- 7Department of Family and Generations, International Institute for Population Sciences, Mumbai, India
- 8School of Criminal Justice Education, J. H. Cerilles State College, Caridad, Philippines
- 9Department of Medical Education and Informatics, Faculty of Medicine, Gazi University, Ankara, Turkey
- 10Faculty of Medicine, Universitas Islam Bandung, Bandung, Indonesia
- 11College of Health Sciences/Nursing Department, Sharjah Institute of Medical and Health Sciences, University of Sharjah, Sharjah, United Arab Emirates
- 12Department of Community Health, Shahrekord University of Medical Sciences, Shahrekord, Iran
- 13Administration and Research, Bangladesh National Nutrition Council, Ministry of Health and Family Welfare, Dhaka, Bangladesh
- 14College of Business Administration, International University of Business Agriculture and Technology, Dhaka, Bangladesh
- 15Public Policies, Education and Communication, Disease Control Coordination, São Paulo State Health Department, São Paulo, Brazil
- 16Faculty of Education, University of City Island, Famagusta, Cyprus
- 17Publication Research Institute and Community Service, Universitas Muhammadiyah Sidenreng Rappang, South Sulawesi, Indonesia
- 18Sekolah Tinggi Ilmu Administrasi Abdul Haris, Makassar, Indonesia
- 19Medical Statistics Division, Department of Medical Research, Ministry of Health, Nay Pyi Taw, Myanmar
- 20Medical Agency for Research and Statistics, Giza, Egypt
- 21Clinical Research Key (CRK-CRO), Nairobi, Kenya
- 22Department for Economy and Health, University for Continuing Education Krems, Danube University Krems, Krems an der Donau, Austria
- 23Department of Health Sciences, St. Pölten University of Applied Sciences, St. Pölten, Austria
- 24Clinical Informatics Research Unit, Faculty of Medicine, University of Southampton, Southampton, United Kingdom
- 25Department of Epidemiology and Health Statistics, School of Public Health, Fujian Medical University, Fuzhou, China
Introduction: It is clear that medical science has advanced much in the past few decades with the development of vaccines and this is even true for the novel coronavirus outbreak. By late 2020, COVID-19 vaccines were starting to be approved by national and global regulators, and across 2021, there was a global rollout of several vaccines. Despite rolling out vaccination programs successfully, there has been a cause of concern regarding uptake of vaccine due to vaccine hesitancy. In tackling the vaccine hesitancy and improving the overall vaccination rates, digital health literacy (DHL) could play a major role. Therefore, the aim of this study is to assess the digital health literacy and its relevance to the COVID-19 vaccination.
Methods: An internet-based cross-sectional survey was conducted from April to August 2021 using convenience sampling among people from different countries. Participants were asked about their level of intention to the COVID-19 vaccine. Participants completed the Digital Health Literacy Instrument (DHLI), which was adapted in the context of the COVID Health Literacy Network. Cross-tabulation and logistic regression were used for analysis purpose.
Results: Overall, the mean DHL score was 35.1 (SD = 6.9, Range = 12–48). The mean DHL score for those who answered “Yes” for “support for national vaccination schedule” was 36.1 (SD 6.7) compared to 32.5 (SD 6.8) for those who either answered “No” or “Don't know”. Factors including country, place of residence, education, employment, and income were associated with the intention for vaccination. Odds of vaccine intention were higher in urban respondents (OR-1.46; C.I.-1.30–1.64) than in rural respondents. Further, higher competency in assessing the relevance of online information resulted in significantly higher intention for vaccine uptake.
Conclusion: Priority should be given to improving DHL and vaccination awareness programs targeting rural areas, lower education level, lower income, and unemployed groups.
Introduction
The COVID-19 pandemic, in which confirmed cases first appeared in China and the outbreak quickly has spread across the globe, was defined as a Public Health Emergency of International Concern on January 30, 2020. The World Health Organization (WHO) officially declared a pandemic on March 11, 2020. The pandemic has since resulted in a significant level of excess deaths and a huge socio-economic impact on countries around the world. During the earlier phases of the pandemic, many countries implemented precautionary measures such as mask wearing, quarantines, and curfews to slow the spread of the virus. These measures were effective in reducing both transmission and the overall burden of COVID-19 disease (1). However, research has conclusively shown that COVID-19 has severe health effects including quality of life (2), mental health (3–7), and psychological distress (8–13).
Since the start of the first outbreak in early 2020, there has been significant commentary about COVID-19 on social media, in which users have been exposed to good and bad quality information about the virus and the emerging outbreaks. In light of the significant amount of false information coming from digital platforms amidst the pandemic, the WHO introduced a new term—an infodemic—defined as “too much information including false or misleading information in digital and physical environments during a disease outbreak”. The WHO urged all nations to combat the COVID-19 infodemic (1).
By late 2020, COVID-19 vaccines were starting to be approved by national and global regulators, and across 2021, there was a global rollout of several vaccine candidates, including those manufactured by Pfizer and AstraZeneca. Since then, countries have urgently attempted to reach their populations and achieve high vaccine uptake. Mortality rates and cases numbers have fallen dramatically as a result of vaccination (14, 15). By reducing the pressures on national and local health services, immunization programs have helped the countries in easing down restrictions, and enabled people to resume their normal lives (16). Nevertheless, the virus is still highly prevalent around the world, with new variants fueling transmission, and too many people still awaiting access to even their first dose of any COVID-19 vaccine. As a result of misinformation and vaccine efficacy, vaccine hesitancy also plagued the global COVID-19 vaccination program (16–18). The acceptance of vaccine was further influenced by the recommendations of medical professionals (19, 20).
Vaccine hesitancy has been an important area of concern when considering pandemic response strategies. The main cause of vaccine hesitancy is misinformation that affects decision-making and causes hesitation in vaccination uptake (17). In a systematic review conducted by Cascini et al., a negative association between use of social media and people's intention to vaccinate themselves have been observed (21). Decisions to receive vaccination has been greatly impacted by the exposure to false information on social media. A further study conducted in Ghana, shows the influence of social media on the people's belief about vaccination (22). Additionally, people in Southeast Asia have become hesitant to vaccination due to the existence of misinformation through digital platforms (23). It is therefore important to acknowledge the use of social media as a tool through which misinformation can easily be spread. On the other hand, Morocco, a country located in North Africa has used its digital system to run a smart vaccination campaign. This digital system comprises a vaccination registry, stock, logistics management facilities, and a portal for tracking side effects of the vaccine. In addition, a new platform named “liqah” (“vaccine” in “Arabic”) has been established, which allows doctors to communicate directly with the citizens. The website also shares comprehensive information on the vaccines for the citizens (24). In a study conducted in eight European countries, it is shown that digital technologies and tools have supported the vaccination programs. Digital tools were used to convey information about the safety and efficacy of vaccines and how to access vaccine services (25). Digital health tools can also help with vaccine hesitancy. In order to do this, information from the platform should be conveyed in multiple languages, clearer language, and in a friendly manner. Moreover, the engagement platforms should be trustworthy and provide greater details for people who are in the greatest need of vaccine. Additionally, digital health tools should be inclusive and embrace all races and ethnicities (26).
People are increasingly using electronic resources to make decisions about their health, including social media, demonstrating the importance of digital health literacy (27). The WHO defines Digital Health Literacy as the ability to utilize electronic devices to gain, seek, appraise, and comprehend health information in order to improve health outcomes or address a health concern (28). Digital platforms are ideal places to communicate accurate information about COVID-19. However, social media platforms have become a hub of misinformation negatively impacting people's lives and attitudes concerning the pandemic. Monitoring digital platforms is essential toward ensuring that people have access to the best possible information at the appropriate time. To assess digital health literacy and its relevance to the COVID-19 vaccination, a cross-sectional study was conducted in 11 countries among the general adult population.
Methods
Study design
An internet-based cross-sectional survey was conducted from April to August 2021 using non-random convenience sampling among people from different countries.
Data collection procedures
The sample size is estimated with an infinite population, a confidence level of 95%, a Z score of 1.960, and a margin error of 0.05. We distributed the Google form online without restriction for the specific country using personal contacts by emails, web-based applications (e.g., WhatsApp and Telegram), and social media (e.g., Facebook, LinkedIn, Twitter, and Instagram); over 4,700 subjects completed the surveys. Participants confirmed that they were aged 18 years or older. They were reminded to respond only once and use a unique identifier to create a single account by settings that allow one response per user. Finally, personal data protection was emphasized during the study to secure our data's privacy, availability, and integrity. Confidentiality and privacy of participants' responses were ensured to minimize potential bias caused by self-reported data. Data were collected using the online Google Forms platform. The collected information was exported for review in Microsoft Excel before a fuller analysis using Stata 16 (College Station, TX: StataCorp LLC).
Instrument development and measures
The questionnaire was adapted from the World Health Organization's (WHO) survey tool and guidance on COVID-19 (29). This survey tool monitors knowledge, risk perceptions, preventive behaviors including digital health literacy, and other variables to inform COVID-19 outbreak response measures, including policies, interventions, and communications.
Demographics
Data collected included socio-demographic characteristics of participants, including as age, gender, education (secondary or less/post-secondary/tertiary), country of residence (the focus being Bangladesh, Brazil, Egypt, Indonesia, Iran, Malaysia, Myanmar, Philippines, Thailand, Turkey, United Arab Emirates, others), religion (Islam, Buddhism, Christianity, Hinduism, others), community type (rural/urban), employment status (working/not employed/unemployed/student), and income (self-reported as sufficient/less sufficient).
Vaccine intention
Participants were asked about their level of intention to the COVID-19 vaccine (“I think everyone should be vaccinated according to the National vaccination schedule”; no, I don't know, yes).
Digital health literacy
Participants completed the Digital Health Literacy Instrument (DHLI) (8), which was adapted in the context of the COVID Health Literacy Network. The scale measures one's ability to seek, find, understand, and appraise health information from digital resources. While the original DHLI is comprised of 7 subscales, this study used the following four domains: (1) information searching or using appropriate strategies to look for information (e.g., “When you search the internet for information on coronavirus virus or related topics, how easy or difficult is it for you to find the exact information you are looking for?”) (2) adding self-generated content to online-based platforms (e.g., “When typing a message on a forum or social media such as Facebook or Twitter about the coronavirus a related topic, how easy or difficult is it for you to express your opinion, thought, or feelings in writing?”) (3) evaluating reliability of online information (e.g., “When you search the internet for information on the coronavirus or related topics, how easy or difficult is it for you to decide whether the information is reliable or not?”) and (4) determining relevance of online information [e.g., “When you search the internet for information on the coronavirus or related topics, how easy or difficult is it for you to use the information you found to make decisions about your health (protective measures, hygiene regulations, transmission routes, risks and their prevention)?”]. A total of 12 items (three per each dimension) were asked, and answers were recorded on a four-point Likert scale (1 = very difficult; 4 = very easy). The reliability statistics (Cronbach alpha) for the overall DHL score was 0.92 while the alpha coefficients for the four subscales ranges from 0.73 to 0.88, suggesting acceptable to good internal consistency (30). Only participants who had complete data on all DHL subscales were included in the final analysis.
Ethics statement
The study was designed and conducted in line with the declaration of Helsinki and was approved by the Asia Metropolitan University Ethics Committee in Malaysia (Ref. No: AMU/MREC/NF/18022021). Respondents were informed that their participation was voluntary, and written consent was implied on the completion of the questionnaire. All participants were aged 18 years or older.
Statistical analysis
Descriptive analysis was conducted for socio-demographic variables. Continuous variables were presented as mean (standard deviation, SD). The outcome variable, vaccine intention, were dichotomized to “Yes” and “No/Don't know” while the DHL sub-scales and overall scores were dichotomized to “sufficient” vs. “limited” by median split in the analysis. Bivariate analyses between the socio-demographic variables and the DHL variables, and the vaccine intention were displayed using cross-tabulations and Chi-squared statistics were reported for statistical significance (p < 0.05). Multivariable logistic regression with robust variance were used to see associations between DHL overall (model 1) and DHL subscales (model 2) with vaccine intention, adjusted for age, sex, education, country, urban/rural, employment status and income. The variable “religion” was not included in the final models due to multicollinearity. Assumptions for logistic regression were met and multicollinearity was checked using variation inflation factor (VIF). Adjusted odds ratios (AOR, 95%CI) were reported in the models with the Hosmer-Lemeshow test reported for model fit. All analyses were conducted using Stata 16 (College Station, TX: StataCorp LLC).
Results
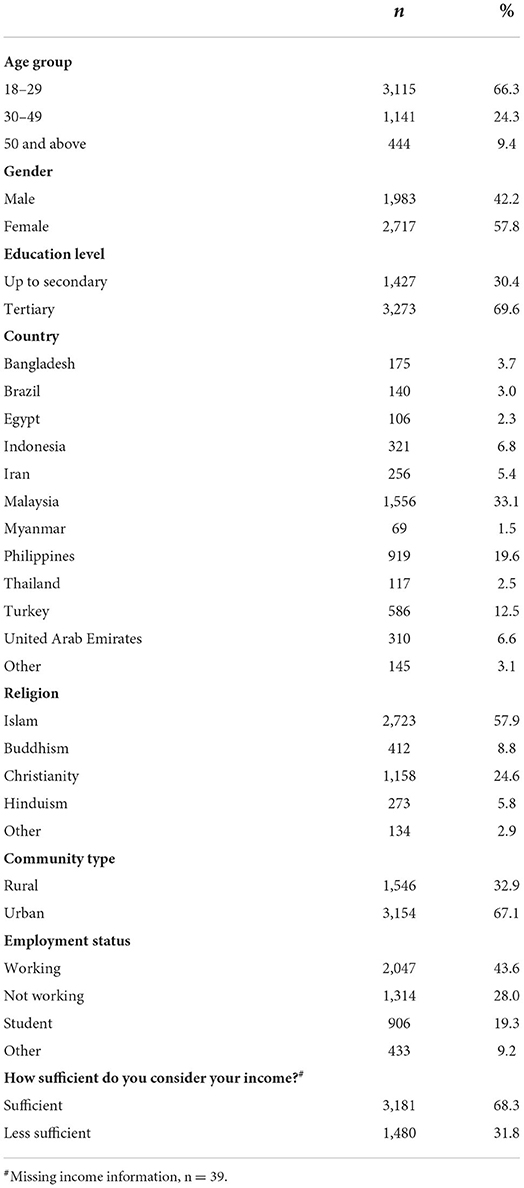
The survey was completed by 4700 participants from 53 countries. The mean age was 29.4 (SD = 11.9 years), with range of 18–77 years. The majority of respondents were 18–29 years old (66%), female (58%), had tertiary level education (70%), and from Malaysia (33%). Other socio-demographic characteristics of the participants are summarized in Table 1.
Overall, the mean DHL score was 35.1 (SD = 6.9, Range = 12–48). The mean DHL score for those who answered “Yes” for “support for national vaccination schedule” was 36.1 (SD 6.7) compared to 32.5 (SD 6.8) for those who either answered “No” or “Don't know”, t(4,587) = 16.0, p < 0.001. The median for all the subscales scores were 9.0, 9.0, 9.0, and 9.0 (range 3–12), respectively, while the median for the total DHL score was 35.0 (range 12–48). The percentages of having “intention to get an immunization” within categories of socio-demographic characteristics and DHL sufficiency cut-off are displayed in Table 2.
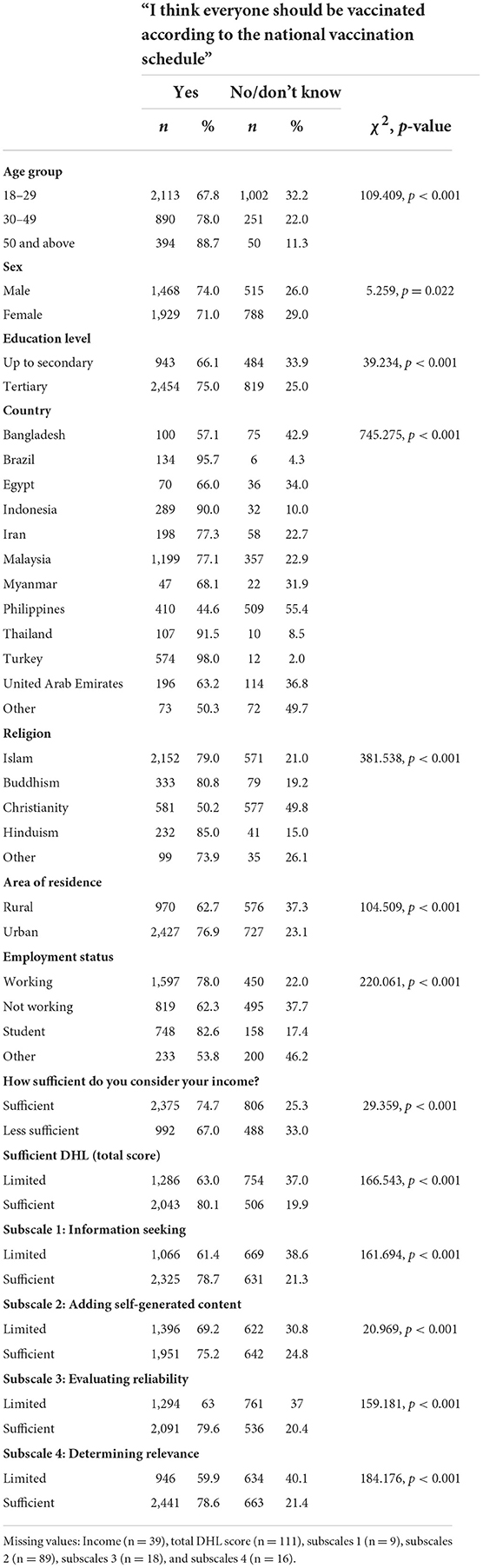
Table 2. Bivariate associations between socio-demographic characteristics and sufficient DHL, with intention for vaccination.
Multivariable models
The multivariable logistic regression with robust variance models are shown in Table 3. The predictors of interest are sufficient (Sufficient vs. Limited) DHL score (Model 1) and each of the four subscales median cut-off (Model 2). After adjustment for age, sex, education, country, urban/rural, employment status and income, the Adjusted Odds Ratio (AOR) for intention to vaccination was 1.64 (95% CI, 1.41–1.90) for sufficient DHL. In Model 2, only subscale 4 (determining relevance) was a statistically significant factor for predicting intention to vaccination, AOR 1.48 (95% CI, 1.21–1.80).
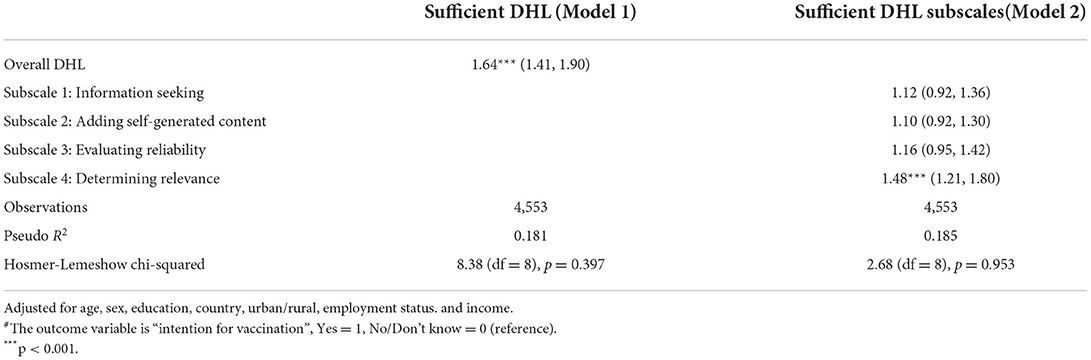
Table 3. Adjusted ORs (95% CI) for sufficient total DHL score and sufficient DHL subscales scores in relation to “intention for vaccination”#.
Discussion
This study provides insights into digital health literacy and its association with the intention of vaccination across 53 countries, but with a predominant focus on 11 countries. To the best of our knowledge, this is the first study to investigate the DHL and intention to vaccinate during the COVID-19 outbreak in a wider geographical area. Our findings indicated that respondents had a high overall score of digital health literacy (M = 2.93, SD = 0.58). Similarly, sufficient DHL levels were reported among the university student population in the US (31), Germany (32), Pakistan (33), Malaysia, China, and the Philippines (34). Although inclusion criteria covered the general population, the respondents were predominantly younger adults, and approximately 70% attained tertiary education, which may explain the similar level of DHL levels with previous studies. For instance, older adults were associated with lower digital health literacy level, limited utilization of technology and electronic devices, and lower confidence in using technology (35). During this digital era with the increasing speed of utilization, digital information sources have tremendous potential benefits to the population's health (36). Thus, attaining a sufficient level of DHL is a positive prospect for positive health behaviors, including combating and preventing COVID-19 infection.
From the perspective of public health, improving health literacy among the population is considered a social vaccine to prevent, protect, and reduce the burden of diseases (37). During the COVID-19 pandemic, DHL is a critical tool to reduce the impact of the infodemic, and to improve the dissemination of high-quality pandemic-related information around topics such as preventive behaviors and vaccination (31, 33). Among our study respondents, those who supported being vaccinated according to the National Vaccination Schedule were found to have significantly higher digital health literacy scores compared to those who opposed this concept. Our findings are correlated with a previous study in the US, where a higher DHL level is associated with the willingness to have COVID-19 vaccination (38).
Among those who have sufficient DHL, some demographic factors were found to be associated with the intention to be vaccinated. In terms of geographic location, respondents from Turkey and Brazil reported having the significant highest intention compared to respondents from Bangladesh. The WHO are cooperating and collaborating with countries to ascertain equal access to the COVID-19 vaccination as it is the key factor to combat the pandemic (38). However, perception of vaccination, intention, and willingness plays a crucial role in the vaccine uptake during the pandemic. In a comparison across various countries, willingness to take the vaccination in low- and middle-income countries in Africa, South Asia, and Latin America was found to be an average of 80.3% in the previous study (39). In the UK, a similar finding of high willingness (88.8%) to take COVID-19 vaccination was reported (40). Meanwhile, in the US, 67% of the study respondents reported their willingness to vaccinate (41). Vaccine acceptance was found to be varied in previous studies across the UK, US, South Asia, Africa, and Latin America (39–41). Among the Canadian population, only 9% of the respondents in the nationwide survey reported that they had no intention to take COVID-19 vaccination (42). Different levels of intention for vaccine uptake across the countries might be contributed by the incidence of COVID-19 infection, public awareness level, and sampling recruitment in studies (43–46). Furthermore, willingness to take vaccination could be varied by contextual influence including politics and policies, individual and group influence, and vaccine-related factors such as the design and the delivery program, recommendations from healthcare personnel, and ability to understand (i.e., language and health literacy) (47). High willingness to vaccinate was reported among the Canadian community (42), where government policy was committed to vaccination by providing the financial, policy, and legislative support, by developing specific strategies for some groups including indigenous, pregnant, and persons with disabilities, minor ethnic groups and immigrants (48, 49). Political ideologies might also be related to vaccine uptake, as some states in the US achieved 70% vaccination, while another state reported only 35% of vaccination (49). Therefore, the local authorities need to understand the community perception, changes in that perception over time around the willingness to vaccinate, and should have a strong political commitment. This is important not only for the COVID-19 vaccine, but also for all other nationally recommended vaccines. The WHO and UNICEF have highlighted a global rise of measles outbreaks in the first quarter of 2022, as population mixing begins to return to pre-pandemic levels but also after 2 years of interrupted healthcare (50). Thus, a proactive approach to health promotion around routine vaccinations is important.
Respondents who achieved tertiary education were more likely to take the vaccine compared to those who achieved up to secondary education. Education has been reported as one of the influencing factors on intention and willingness to vaccinate in previous studies (51–54), albeit with occasionally conflicting results. For example, a study in Ghana found that higher education was linked to increased hesitancy, rather than increased willingness to vaccinate, with political allegiance likely to be a confounding variable when considering education (55).
The community needs trustworthy information about the disease, including the benefits of physical and mental wellbeing. Since the digital media is the major source of information, competency in online information-searching and evaluating the validity and reliability of information are associated with the utilization of trustworthy information sources (34). People with higher education levels may search for scientifically established information with critical evaluation compared to lower education group regards to COVID-19 related information and vaccination (56, 57). Furthermore, urban residents, employed people, and those who have sufficient income are positively associated with the intention to vaccinate. Previous studies reported that demographic factors such as residency and income influence knowledge, perceptions, and acceptance of COVID-19 vaccination (17, 58).
During the COVID-19 pandemic, people have also searched for health information via the traditional media, including television channels, national newspapers, government webpages (34, 59). Traditional channels play an essential role in providing informed and evidence-based vaccine-related content. In the meantime, there is potential for social media to educate people and reduce vaccine hesitancy (59). In this study, the key finding was that determining relevance of COVID-19 information was a significant factor regarding the intention to vaccinate. Moreover, the mean score for determining the relevance domain was found to be the highest among the DHL domains. Thus, when respondents searched for online information about the COVID-19 vaccines and related topics, most respondents found it to be easy to apply the online information in daily life, and used the online search results to make health-related decisions. This was ultimately associated with positive intentions toward vaccination. While developing vaccine-related information for online health communication strategies, key messages should be credible and relevant. Furthermore, the competency of people to determine the relevance and applicability to improve their health has an impact on the vaccination intention. Improving health literacy in the population and providing credible, timely, relevant information could enhance vaccination uptake in the community.
Strength and limitations
To the best of our knowledge, this is the first to investigate the association between DHL and intention to vaccinate across 53 countries, with a focus on 11 countries in this paper. This study provides the current insight on vaccination intention across international context and highlighted the importance of DHL. Moreover, competency on determining relevance of information subscale in DHL was found to be particularly important for the willingness to take the vaccination.
Despite the strengths, our study has limitations. Since the non-probability method was used for recruitment, selection bias limits the generalizability of the findings. The nature of the cross-sectional study was to observe for a period of time; therefore, changes in vaccination intention and availability of vaccines could not be assessed. Approximately two-thirds of our respondents had tertiary education levels and reported living in an urban community, so the generalizability of the findings to other demographics such as rural populations and those of lower education level is uncertain. Considering that the level of digital health literacy is closely related to the internet penetration rate, level of economic development, reaching vulnerable individuals such as older adults, oversampling, and undersampling in some countries, the research results cannot represent the overall general adult population. Therefore, additional large-scale studies and a more systematic, inclusive sampling method are warranted to improve the representativeness and generalizability of the findings.
Conclusion
This study provides an insight into the importance of DHL on the vaccination intention. The respondents generally have sufficient DHL competency. Among them, demographic factors, such as country, residence area, education, employment, and income were associated with the intention for vaccination. Higher competency in assessing the relevance of online information resulted in significantly higher intention for vaccine uptake. In terms of future perspective, not only for COVID-19 but also for the other vaccines, health promotion should be proactive in sharing relevant, timely and applicable information with the community. Priority should be given to improving DHL and vaccination awareness programs targeting lower education level, lower income, and unemployed groups.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by Asia Metropolitan University Ethics Committee in Malaysia (Ref. No: AMU/MREC/NF/18022021). The patients/participants provided their written informed consent to participate in this study.
Author contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas, took part in drafting, revising or critically reviewing the article, gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Special Projects of the Central Government Guiding Local Science and Technology Development, China (No. 2021L3018). The funder was not involved in study design, in the collection, analysis and interpretation of data, in the writing of the manuscript, nor in the decision to submit the manuscript for publication.
Acknowledgments
We would like to thank all participants involved in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2022.998234/full#supplementary-material
References
1. OECD. The Territorial Impact of COVID-19: Managing the Crisis Across Levels of Government. (2020). Available online at: https://www.oecd.org/coronavirus/policy-responses/the-territorial-impact-of-covid-19-managing-the-crisis-across-levels-of-government-d3e314e1/ (accessed July 10, 2022).
2. Marzo RR, Khanal P, Ahmad A, Rathore FA, Chauhan S, Singh A, et al. Quality of life of the elderly during the COVID-19 pandemic in Asian countries: a cross-sectional study across six countries. Life. (2022) 12:365. doi: 10.3390/life12030365
3. RilleraMarzo R, Villanueva EQ, Chandra U, Htay MNN, Shrestha R, Shrestha S. Risk perception, mental health impacts and coping strategies during Covid-19 pandemic among Filipino healthcare workers. J Public Health Res. (2021) 10:jphr.2021.2604. doi: 10.4081/jphr.2021.2604
4. Marzo RR, Vinay V, Bahari R, Chauhan S, Ming DAF, Fernandez SFAN, et al. Depression and anxiety in Malaysian population during third wave of the COVID-19 pandemic. Clin Epidemiol Global Health. (2021) 12:100868. doi: 10.1016/j.cegh.2021.100868
5. Htay MNN, Marzo RR, Bahari R, AlRifai A, Kamberi F, El-Abasiri RA, et al. How healthcare workers are coping with mental health challenges during COVID-19 pandemic? A cross-sectional multi-countries study. Clin Epidemiol Global Health. (2021) 11:100759. doi: 10.1016/j.cegh.2021.100759
6. Htay MNN, Marzo RR, AlRifai A, Kamberi F, El-Abasiri RA, Nyamache JM, et al. Immediate impact of COVID-19 on mental health and its associated factors among healthcare workers: a global perspective across 31 countries. J Glob Health. 10:020381. doi: 10.7189/jogh.10.020381
7. Kamberi F, Sinaj E, Jaho J, Subashi B, Sinanaj G, Jaupaj K, et al. Impact of COVID-19 pandemic on mental health, risk perception and coping strategies among health care workers in Albania - evidence that needs attention. Clin Epidemiol Global Health. (2021) 12:100824. doi: 10.1016/j.cegh.2021.100824
8. Marzo RR, Aye SS, Naing TW, Kyaw TM, Win MT, Soe HHK, et al. Factors associated with psychological distress among Myanmar residents during COVID-19 pandemic crises. J Public Health Res. (2021) 10:jphr-2021. doi: 10.4081/jphr.2021.2279
9. Marzo RR, Ismail Z, Htay MNN, Bahari R, Ismail R, Villanueva III EQ, et al. Psychological distress during pandemic Covid-19 among adult general population: Result across 13 countries. Clin Epidemiol Global Health. (2021) 10:100708. doi: 10.1016/j.cegh.2021.100708
10. Marzo RR, Singh A, Mukti RF. A survey of psychological distress among Bangladeshi people during the COVID-19 pandemic. Clin Epidemiol Global Health. (2021) 10:100693. doi: 10.1016/j.cegh.2020.100693
11. Abasiri RAE, RilleraMarzo R, Abdelaziz H, SherifBoraii, Abdelaziz H. Evaluating the psychological distress of the coronavirus disease 2019 Pandemic in Egypt. Eur J Mol Clin Med. (2020) 7:1–12.
12. Marzo RR, Villanueva III EQ, Faller EM, Baldonado AM. Factors associated with psychological distress among Filipinos during coronavirus disease-19 pandemic crisis. Open Access Maced J Med Sci. (2020) 8:309–13. doi: 10.3889/oamjms.2020.5146
13. Respati T, Irasanti SN, Sartika D, Akbar IB, Marzo RR, A. nationwide survey of psychological distress among Indonesian residents during the COVID-19 pandemic. Int J Public Health Science. (2021) 10:119–26. doi: 10.11591/ijphs.v10i1.20609
14. Galvani A, Moghadas S, Schneider E. Deaths & Hospitalizations Averted by Rapid US Vaccination Rollout | Commonwealth Fund. The Commonwealth Fund (2021). Available online at: https://www.commonwealthfund.org/publications/issue-briefs/2021/jul/deaths-and-hospitalizations-averted-rapid-us-vaccination-rollout (accessed July 10, 2022).
15. Johnson AG. COVID-19 incidence and death rates among unvaccinated and fully vaccinated adults with and without booster doses during periods of delta and omicron variant emergence — 25 U.S. Jurisdictions, April 4–December 25, 2021. MMWR Morb Mortal Wkly Rep. (2022) 71:132–8. doi: 10.15585/mmwr.mm7104e2
16. Marzo RR, Ahmad A, Islam MS, Essar MY, Heidler P, King I, et al. Perceived COVID-19 vaccine effectiveness, acceptance, and drivers of vaccination decision-making among the general adult population: a global survey of 20 countries. PLoS Negl Trop Dis. (2022) 16:e0010103. doi: 10.1371/journal.pntd.0010103
17. Marzo RR, Sami W, Alam MdZ, Acharya S, Jermsittiparsert K, Songwathana K, et al. Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: a cross-sectional study in six Southeast Asian countries. Trop Med Health. (2022) 50:4. doi: 10.1186/s41182-021-00393-1
18. Elsayed M, El-Abasiri RA, Dardeer KT, Kamal MA, Htay MNN, Abler B, et al. Factors influencing decision making regarding the acceptance of the COVID-19 vaccination in Egypt: a cross-sectional study in an urban, well-educated sample. Vaccines. (2022) 10:20. doi: 10.3390/vaccines10010020
19. Marzo RR, Ahmad A, Abid K, Khatiwada AP, Ahmed A, Kyaw TM, et al. Factors influencing the acceptability of COVID-19 vaccination: a cross-sectional study from Malaysia. Vacunas. (2022) 23:S33–40. doi: 10.1016/j.vacun.2021.07.007
20. King I, Heidler P, Marzo RR. The long and winding road: uptake, acceptability, and potential influencing factors of COVID-19 vaccination in Austria. Vaccines. (2021) 9:790. doi: 10.3390/vaccines9070790
21. Cascini F, Pantovic A, Al-Ajlouni YA, Failla G, Puleo V, Melnyk A, et al. Social media and attitudes towards a COVID-19 vaccination: a systematic review of the literature. EClinicalMedicine. (2022) 48:101454. doi: 10.1016/j.eclinm.2022.101454
22. Amo-Adjei J, Nurzhynska A, Essuman R, Lohiniva AL. Trust and willingness towards COVID-19 vaccine uptake: a mixed-method study in Ghana, 2021. Arch Public Health. (2022) 80:1–12. doi: 10.1186/s13690-022-00827-0
23. Asia Society Policy Institute. Southeast Asia COVID-19 Misinformation - Asia Society Policy Institute. Australia: Asia Society Policy Institute (2021). Available online at: https://southeastasiacovid.asiasociety.org/southeast-asia-and-covid-19-misinformation/ (accessed July 10, 2022).
24. El Otmani Dehbi Z, Sedrati H, Chaqsare S, Idrissi Azami A, Merzouki M, Raji M, et al. Moroccan digital health response to the COVID-19 crisis. Front Public Health. (2021) 9:690462. doi: 10.3389/fpubh.2021.690462
25. Odone A, Gianfredi V, Sorbello S, Capraro M, Frascella B, Vigezzi GP, et al. The use of digital technologies to support vaccination programmes in Europe: state of the art and best practices from experts' interviews. Vaccines. (2021) 9:1126. doi: 10.3390/vaccines9101126
26. Kat J. Digital health tools can help with COVID-19 vaccine hesitancy. Healthcare IT News. (2021). Available online at: https://www.healthcareitnews.com/news/digital-health-tools-can-help-covid-19-vaccine-hesitancy (accessed August 14, 2022).
27. Levin-Zamir D, Bertschi I. Media health literacy, eHealth literacy, and the role of the social environment in context. Int J Environ Res Public Health. (2018) 15:1643. doi: 10.3390/ijerph15081643
28. The Wellness Network. Digital Health Literacy Key Component to Improved Health Outcomes. The Wellness Network (2020). Available online at: https://www.thewellnessnetwork.net/health-news-and-insights/blog/digital-health-literacy/ (accessed July 10, 2022).
29. World Health Organization. Regional Office for Europe. Survey Tool and Guidance: Rapid, Simple, Flexible Behavioural Insights on COVID-19. (2020). Report No.: WHO/EURO:2020-696-40431-54222. Available online at: https://apps.who.int/iris/handle/10665/333549 (accessed August 14, 2022).
30. Taber KS. The Use of Cronbach's alpha when developing and reporting research instruments in science education. Res Sci Educ. (2018) 48:1273–96. doi: 10.1007/s11165-016-9602-2
31. Patil U, Kostareva U, Hadley M, Manganello JA, Okan O, Dadaczynski K, et al. Health literacy, digital health literacy, and COVID-19 pandemic attitudes and behaviors in US college students: implications for interventions. Int J Environ Res Public Health. (2021) 18:3301. doi: 10.3390/ijerph18063301
32. Dadaczynski K, Okan O, Messer M, Leung AY, Rosário R, Darlington E, et al. Digital health literacy and web-based information-seeking behaviors of university students in Germany during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res. (2021) 23:e24097. doi: 10.2196/24097
33. Zakar R, Iqbal S, Zakar MZ, Fischer F. COVID-19 and health information seeking behavior: digital health literacy survey amongst university students in Pakistan. Int J Environ Res Public Health. (2021) 18:4009. doi: 10.3390/ijerph18084009
34. Htay MNN, Parial LL, Tolabing MC, Dadaczynski K, Okan O, Leung AYM, et al. Digital health literacy, online information-seeking behaviour, and satisfaction of Covid-19 information among the university students of East and South-East Asia. PLoS ONE. (2022) 17:e0266276. doi: 10.1371/journal.pone.0266276
35. Rasekaba TM, Pereira P, Rani GV, Johnson R, McKechnie R, Blackberry I. Exploring telehealth readiness in a resource limited setting: digital and health literacy among older people in Rural India (DAHLIA). Geriatrics. (2022) 7:28. doi: 10.3390/geriatrics7020028
36. Shepherd J. “What is the digital era?” In: Social and economic transformation in the digital era. IGI Global. (2004) 1–18. doi: 10.4018/978-1-59140-158-2.ch001
37. Okan O, Messer M, Levin-Zamir D, Paakkari L, Sørensen K. Health literacy as a social vaccine in the COVID-19 pandemic. Health Promot Int. (2022) daab197. doi: 10.1093/heapro/daab197
38. WHO. 172 Countries and Multiple Candidate Vaccines Engaged in COVID-19 Vaccine Global Access Facility. (2020). Available online at: https://www.who.int/news/item/24-08-2020-172-countries-and-multiple-candidate-vaccines-engaged-in-covid-19-vaccine-global-access-facility (accessed July 10, 2022).
39. Solís Arce JS, Warren SS, Meriggi NF, Scacco A, McMurry N, Voors M, et al. COVID-19 vaccine acceptance and hesitancy in low-and middle-income countries. Nat Med. (2021) 27:1385–94. doi: 10.1101/2021.03.11.21253419
40. Chaudhuri K, Chakrabarti A, Chandan JS, Bandyopadhyay S. COVID-19 vaccine hesitancy in the UK: a longitudinal household cross-sectional study. BMC Public Health. (2022) 22:104. doi: 10.1186/s12889-021-12472-3
41. Malik AA, McFadden SM, Elharake J, Omer SB. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. (2020) 26:100495. doi: 10.1016/j.eclinm.2020.100495
42. Tang X, Gelband H, Nagelkerke N, Bogoch II, Brown P, Morawski E, et al. COVID-19 vaccination intention during early vaccine rollout in Canada: a nationwide online survey. Lancet Regional Health-Americas. (2021) 2:100055. doi: 10.1016/j.lana.2021.100055
43. Bari MS, Hossain MJ, Ahmmed F, Sarker MMR, Khandokar L, Chaithy AP, et al. Knowledge, perception, and willingness towards immunization among Bangladeshi population during COVID-19 vaccine rolling period. Vaccines. (2021) 9:1449. doi: 10.3390/vaccines9121449
44. Banik R, Islam M, Pranta MUR, Rahman QM, Rahman M, Pardhan S, et al. Understanding the determinants of COVID-19 vaccination intention and willingness to pay: findings from a population-based survey in Bangladesh. BMC Infect Dis. (2021) 21:1–15. doi: 10.1186/s12879-021-06406-y
45. Nery N, Jr., Ticona JPA, Cardoso CW, Prates APPB, Vieira HCA, Salvador de Almeida A, et al. COVID-19 vaccine hesitancy and associated factors according to sex: a population-based survey in Salvador, Brazil. PLoS ONE. (2022) 17:e0262649. doi: 10.1371/journal.pone.0262649
46. Gramacho WG, Turgeon M. When politics collides with public health: COVID-19 vaccine country of origin and vaccination acceptance in Brazil. Vaccine. (2021) 39:2608–12. doi: 10.1016/j.vaccine.2021.03.080
47. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
48. Government of Canada SC. COVID-19 Vaccine Willingness Among Canadian Population Groups. (2021). Available online at: https://www150.statcan.gc.ca/n1/pub/45-28-0001/2021001/article/00011-eng.htm (accessed August 14, 2022).
49. MacDonald N, Dube E, Graham J. How Government Policies Political Ideologies Impact Vaccine Acceptance: COVID-19 Beyond. The Canadian Vaccination Evidence Resource and Exchange Centre (2021). p. E381–3. Available online at: http://www.cmaj.ca/lookup/doi/10.1503/cmaj.210112 (accessed August 14, 2022).
50. WHO. UNICEF and WHO Warn of Perfect Storm of Conditions for Measles Outbreaks, Affecting Children. (2022). Available online at: https://www.who.int/news/item/27-04-2022-unicef-and-who-warn-of--perfect-storm--of-conditions-for-measles-outbreaks--affecting-children (accessed July 10, 2022).
51. Humer E, Jesser A, Plener PL, Probst T, Pieh C. Education level and COVID-19 vaccination willingness in adolescents. Eur Child Adoles Psychiatry. (2021) 1–3. doi: 10.1007/s00787-021-01878-4
52. Zychlinsky Scharff A, Paulsen M, Schaefer P, Tanisik F, Sugianto RI, Stanislawski N, et al. Students' age and parental level of education influence COVID-19 vaccination hesitancy. Eur J Pediatr. (2022) 181:1757–62. doi: 10.1007/s00431-021-04343-1
53. Ehde DM, Roberts MK, Herring TE, Alschuler KN. Willingness to obtain COVID-19 vaccination in adults with multiple sclerosis in the United States. Mult Scler Relat Disord. (2021) 49:102788. doi: 10.1016/j.msard.2021.102788
54. Williams L, Flowers P, McLeod J, Young D, Rollins L, Team CP. Social patterning and stability of intention to accept a COVID-19 vaccine in Scotland: will those most at risk accept a vaccine? Vaccines. (2021) 9:17. doi: 10.3390/vaccines9010017
55. Brackstone K, Atengble K, Head M, Boateng L. Examining Drivers of COVID-19 Vaccine Hesitancy in Ghana: The Roles of Political Allegiance, Misinformation Beliefs, Sociodemographic Factors. (2022). Available online at: https://www.medrxiv.org/content/10.1101/2022.03.16.22272463v1 (accessed July 9, 2022).
56. Hossian M, Khan MAS, Nazir A, Nabi MH, Hasan M, Maliha R, et al. Factors affecting intention to take COVID-19 vaccine among Pakistani University Students. PLoS ONE. (2022) 17:e0262305. doi: 10.1371/journal.pone.0262305
57. Head KJ, Kasting ML, Sturm LA, Hartsock JA, Zimet GD. A national survey assessing SARS-CoV-2 vaccination intentions: implications for future public health communication efforts. Sci Commun. (2020) 42:698–723. doi: 10.1177/1075547020960463
58. Mohamed NA, Solehan HM, Mohd Rani MD, Ithnin M, Che Isahak CI. Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: a web-based survey. PLoS ONE. (2021) 16:e0256110. doi: 10.1371/journal.pone.0256110
Keywords: COVID-19, health literacy, vaccine intention, multi-country, digital
Citation: Marzo RR, Su TT, Ismail R, Htay MNN, Essar MY, Chauhan S, Patalinghug ME, Kucuk Bicer B, Respati T, Fitriyana S, Baniissa W, Lotfizadeh M, Rahman F, Salim ZR, Villela EFdM, Jermsittiparsert K, Aung Y, Hamza NAE, Heidler P, Head MG, Brackstone K and Lin Y (2022) Digital health literacy for COVID-19 vaccination and intention to be immunized: A cross sectional multi-country study among the general adult population. Front. Public Health 10:998234. doi: 10.3389/fpubh.2022.998234
Received: 19 July 2022; Accepted: 15 August 2022;
Published: 16 September 2022.
Edited by:
Bijaya Kumar Padhi, Post Graduate Institute of Medical Education and Research (PGIMER), IndiaReviewed by:
Zouina Sarfraz, Fatima Jinnah Medical University, PakistanRamadan Abdelmoez Farahat, Kafrelsheikh University, Egypt
Ozden Gokdemir, Izmir University of Economics, Turkey
Prakash Babu Kodali, Central University of Kerala, India
Copyright © 2022 Marzo, Su, Ismail, Htay, Essar, Chauhan, Patalinghug, Kucuk Bicer, Respati, Fitriyana, Baniissa, Lotfizadeh, Rahman, Salim, Villela, Jermsittiparsert, Aung, Hamza, Heidler, Head, Brackstone and Lin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yulan Lin, yulanlin@fjmu.edu.cn; Roy Rillera Marzo, rrmtexas@yahoo.com
†ORCID: Roy Rillera Marzo orcid.org/0000-0001-9414-4010
Burcu Kucuk Bicer orcid.org/0000-0002-5615-264X
Titik Respati orcid.org/0000-0002-9214-660X
Susan Fitriyana orcid.org/0000-0003-2407-4576
Zahir Rayhan Salim orcid.org/0000-0002-3685-8354
Edlaine Faria de Moura Villela orcid.org/0000-0002-7043-2007
Kittisak Jermsittiparsert orcid.org/0000-0003-3245-8705
Yadanar Aung orcid.org/0000-0001-8670-5340
Petra Heidler orcid.org/0000-0003-4979-1838
Michael G. Head orcid.org/0000-0003-1189-0531
Ken Brackstone orcid.org/0000-0002-6882-3260
 Roy Rillera Marzo
Roy Rillera Marzo Tin Tin Su
Tin Tin Su Roshidi Ismail
Roshidi Ismail Mila Nu Nu Htay
Mila Nu Nu Htay Mohammad Yasir Essar
Mohammad Yasir Essar Shekhar Chauhan
Shekhar Chauhan Mark E. Patalinghug
Mark E. Patalinghug Burcu Kucuk Bicer
Burcu Kucuk Bicer Titik Respati10†
Titik Respati10† Wegdan Baniissa
Wegdan Baniissa Zahir Rayhan Salim
Zahir Rayhan Salim Kittisak Jermsittiparsert
Kittisak Jermsittiparsert Nouran Ameen Elsayed Hamza
Nouran Ameen Elsayed Hamza Michael G. Head
Michael G. Head Ken Brackstone
Ken Brackstone Yulan Lin
Yulan Lin