- Department of Health Policy and Management, School of Public Health, Peking University, Beijing, China
Background: Many countries and regions worldwide are improving their healthcare systems through the integration and unification of health insurance programs covering different groups of people. In China, the past 10 years has been the time when Chinese government promote the Urban and Rural Residents Basic Medical Insurance (URRBMI) by integrating the Urban Residents' Basic Medical Insurance (URBMI) and New Rural Cooperative Medical Scheme (NRCMS).
Objectives: To evaluate the impact of the URRBMI on equity in relation to health services.
Methods: The quantitative data used in this study were obtained from the CFPS 2014–2020 database, and all respondents with health insurance type UEBMI, URBMI, and NRCMS were included. UEBMI respondents were set as the control group and URBMI or NRCMS as the intervention group, and a DID method model was used to analyze the impact of integrating health insurance on health service utilization, costs and health status. Heterogeneity analysis was also conducted after stratifying the sample according to income level and chronic disease status. This was done to investigate whether there were differences in the effects of the integrated health insurance program across different social groups.
Results: The implementation of URRBMI is found to be associated with a significant increase in inpatient service utilization (OR = 1.51, P < 0.01) among rural Chinese residents. Regression results by income stratum show that the utilization of inpatient services increased in rural areas for high-, middle- and low-income groups, with the fastest increase (OR = 1.78, P < 0.05) emerging for low-income groups. Analysis by chronic disease status shows that rural residents with chronic disease are associated with a higher increase in hospitalization rates (OR = 1.64, P < 0.01).
Conclusion: The implementation of URRBMI is found to have improved health insurance's ability to withstand risks and effectively improve access to health services for rural residents. In this regard, it can be considered as playing a positive role in bridging the gap in health service utilization between rural and urban areas and in improving regional equity.
1. Introduction
One of the critical dimensions of universal health coverage (UHC) most widely advocated worldwide is equitable access to health services. If equitable access to health services holds in respect of a given region, then people of different socioeconomic status have equal opportunities to access health services when they are needed. Among the many factors influencing access to health care, the coverage and level of coverage of health insurance plans are critical (1). Based on the “law of large numbers”, health insurance systems rely on a variety of sources to raise funds and provide compensation for a specific range of health services to assist those in need. This is done through a risk-sharing mechanism, which plays an active role in preventing catastrophic health expenditures and ensuring that health service needs can be met.
Since 2003, China has witnessed the establishing of three government-led health insurance schemes: the “Urban Employees' Basic Medical Insurance” (UEBMI), covering employees in cities; the “Urban Residents' Basic Medical Insurance” (URBMI), covering the urban non-working population; and the “New Rural Cooperative Medical Scheme” (NRCMS), applying to all rural residents (2). This health insurance system, with its multitude of schemes, has emerged as suffering from certain limitations, particularly in terms of fund raising, in respect of which it can be observed that UEBMI has the highest fundraising capacity and NRCMS the lowest (3, 4). In 2013, for example, per capita funding for each of the three types of health insurance scheme were 1561 CNY, 400 CNY and 370 CNY (Ministry of Human Resources and Social Security of the People's Republic of China, 2013; National Health Commission of the People's Republic of China, 2013), and such gaps in fundraising capacity can be observed to have an impact on benefits packages. NRCMS has the highest ability of cost sharing of these three health insurance schemes (5–7). According to the National Health Service Survey (NHSS) in 2013, the co-payment rates for NRCMS, URBMI and UEBMI were 49.9, 46.4, and 31.2%, respectively (8).
Such disparities in co-payment rate leads to a significant gap in health service utilization between the enrollees on URBMI and NRCMS and those on UEBMI. Based on NHSS, in 2013, the inpatient rate for UEBMI enrollees was 11.2%, and the non-hospitalization rate due to financial hardship was 4.6% (8). However, the inpatient rate for URBMI enrollees was 7.1% and for NRCMS it was 9.0%, and the non-hospitalization rates for URBMI and NRCMS were 9.1 and 8.2%, respectively. This highlights that differences in fundraising levels result in differences in fund pool size, which affects the co-payment rate, and further influences the disparity in health services utilization among enrollees of different health insurance schemes, as well as exacerbating the inequity in health services between urban and rural areas.
In 2009, lacking a rapid increase in the resources to finance such healthcare schemes, the Chinese government began to strengthen the capacity of risk resistance of health insurance schemes by expanding the risk pool through integration of URBMI and NRCMS (9). This program of integration was named “Urban and Rural Resident Basic Medical Insurance” (URRBMI). The reasoning underpinning this move was that, even if funding would not increase significantly, having a large risk pool would improve benefit packages to a useful extent (7, 10).
The NRCMS can be observed as being a package with a lower level of benefits than the URBMI. And URRBMI, as the health insurance integration plan, was associated with emphasizing bringing the NRCMS benefit package in line with the URBMI (i.e., upgrading the NRCMS benefit) as a means of assisting previously disadvantaged rural residents and improving their access to healthcare. Internationally, it can be seen that similar such methods of engaging in health insurance integration exists. For example, in 2011, Indonesia passed a law to merge all five existing government health insurance risk pools into one universal program in order to reduce inequalities in benefits by promoting cross-subsidization and decreasing administrative costs (11, 12). In addition, health financial equity has also been improved through health insurance integration in South Korea, Turkey and Thailand, where inequity in health financing has been addressed across different income and job groups, especially in rural areas (11).
China was able to initiate and fully implement URRBMI before the year of 2019. However, most of the most recent studies on the effect of integrating URBMI and NRCMS in the country are from before 2016. Moreover, such studies tend to be negatively affected by short implementation times and small sample sizes, rendering the results potentially unstable. It is on this basis that this study expands the timeframe to 2020 and uses the nationally representative data to assess the impacts of the integrated health insurance programs on health equity in China, obtaining more stable and reliable policy evaluation results through greater sample size analysis.
2. Study design and methods
2.1. Material
This study considers data from China Family Panel Studies (CFPS), which is a nationally representative, comprehensive, longitudinal social survey of the Chinese population. The database covers a wide range of topics and includes intergraded modules relating to education, regions, health and other areas of information (13, 14). During the sampling phase of the CFPS, a multi-stage random sampling method was used to select ~15,000 households nationwide. This involved interviewing all household members in each sample to obtain data using a face-to-face questionnaire (15). Strict quality control protocols are in force in respect of the project implementation process, including professional database construction. CFPS surveys are conducted every 2 years, with the most recent once having been conducted in 2020. CFPS is given ethical approval by the Biomedical Ethics Review Committee of Peking University, with all participants being required to provide written informed consent. The ethical approval number is IRB00001052-14010.
2.2. Sample
The data collection was conducted between 2014 and 2020, and the inclusion criteria for the sample was phrased in terms of all the individuals who participated in the CFPS survey. Participants were excluded if they were not insured by NCMS, URBMI, UEBMI, or URRBMI or if the relevant data entries were missing control or outcome values.
2.3. Variables
2.3.1. Outcome variables
The following variables were selected as outcome variables: (1) whether the individual had been hospitalized in the past year (1 = yes; 0 = no), relating to the utilization of inpatient services; (2) total hospitalization expenditure in the past year (if the inpatient care utilization in past year = 0, this variable is absent); (3) outpatient care utilization in past 2 weeks (1 = yes; 0 = no); (4) medical expenditure in the past year other than hospitalization, relating to the total expenditure associated with the given outpatient over the past year (if the outpatient care utilization in past year = 0, this variable is absent); (5) total out-of-pocket medical expenditure paid by individuals in the past year, reflecting personal burden; (6) self-assessed health status (if the answer to “what is your health status? “is “Excellent; very good or good”, then the value is 1, if the answer is “Fair or Poor”, then the value is 0). All cost indicators were measured in RMB, and the consumer price index (CPI) level from the same survey period was used for standardization.
2.3.2. Control variables
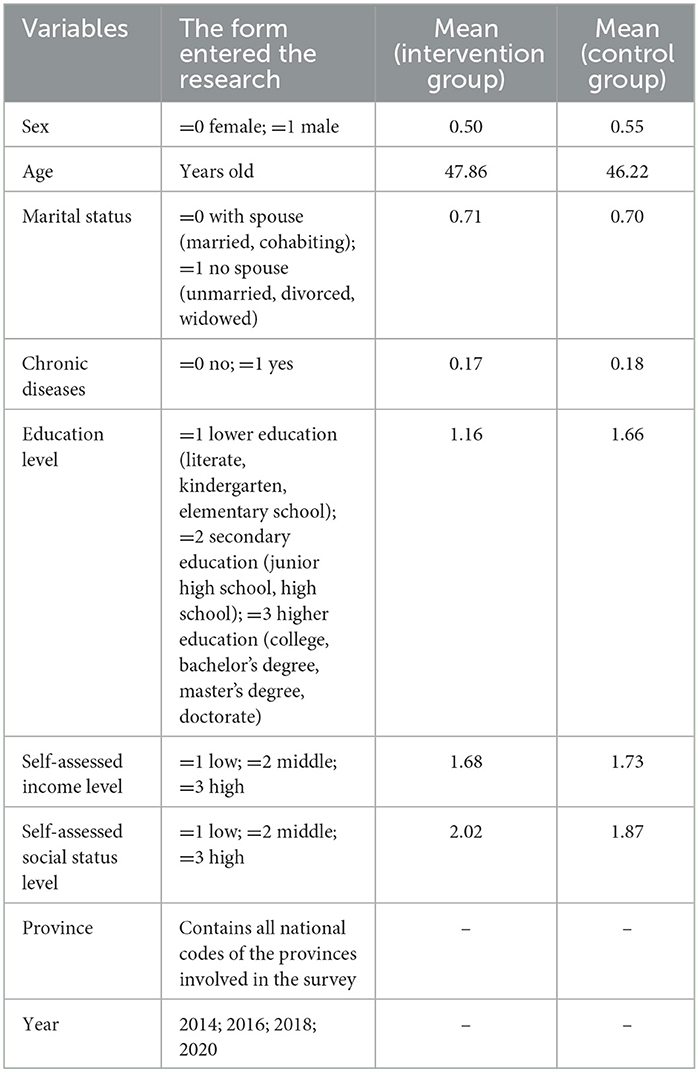
Social economic status variables were used as control variables, including the participants' personal characteristics, health status, location, etc., and the manner evident in the classification of these variables in the existing literature (16, 17). The specific rules governing this classification are provided in Table 1. The average levels of each control variable in the intervention group and the control group are close, indicating that the sample distribution in the two groups is relatively balanced.
2.4. Statistical analysis
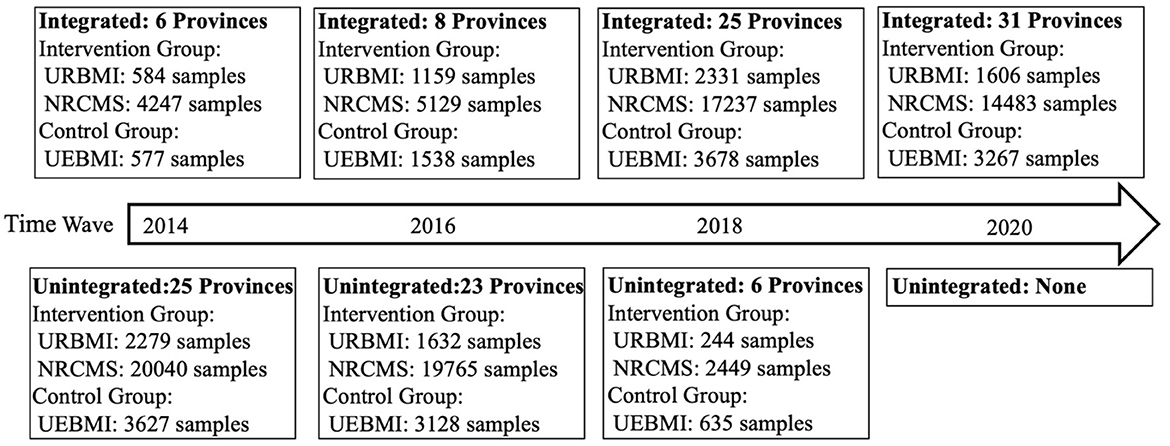
The participants with UEBMI were defined as control group, while the participants with URBMI or NRCMS were defined as the intervention group. The samples of intervention and control groups in each wave before integration and after integration were clearly shown in Figure 1. A difference-in-difference approach (in short, when the dependent variable is a dichotomous variable, the logit model is adopted for regression; when the dependent variable is a continuous numerical variable, the log-linear model is adopted) was used for analyzing the impact of integrated medical insurance for urban and rural residents in terms of health services utilization and health status.
Formula 1 shows the model settings regarding the impact of integration program on health service utilization and health status:
In Formula (1), i, j, t represents survey participants, provinces and years, respectively. Yijt is the outcome variable, and treati is the dummy variable denoting the intervention group and control group (equaling 1 in the case of participants with URBMI or NRCMS, and 0 in the case of participants with UEBMI). integratedjt is the dummy variable, equaling 1 if the province j has implemented integration in time t, and 0 otherwise. β1 represents the differences before and after the implementation of the integration, while β2 represents the differences between control group and intervention group. The coefficient β3 of the interaction term is the real impact of integration implementation. xijt represents independent variables that need to be controlled. Fixed effects are selected in this model, αj controls the fixed effects in different provinces, and θt controls the fixed effects in different years. εijt is a random error term.
In addition, given that the impact of the implementation of integration program on health services utilization may relate to the income level and chronic disease status of the participants, heterogeneity analysis it was judged that also required to be conducted through stratification of income level and chronic disease status. The event study method was used to test the premise of the DID approach, that is, whether the trends of the outcome variables in control group and intervention group were parallel before health insurance integration by controlling all independent variables (with the last period before health insurance integration being taken as the benchmark). The model was set as Formula (2):
In Formula (2), Tj is the integration time of province j, and 1(Tj − t = σ), 1(Tj = t), 1(t − Tj = τ) are dummy variables, representing the time before integration implementation, the time during the integration implementing, and the time after integration implementation, respectively.
The timeline of URRBMI implementation started in 2010, and the provinces data used in our study were from 2014 to 2020, which means we involved the data from URRBMI implementation 6 years ago (the provinces which started URRBMI in the year of 2020) to URRBMI implementation after 10 years (the provinces which started URRBMI in the year of 2010). The values of σ range from 1 to 6 while the values of τ range from 1 to 10, with the coefficient before this indicating the effect value of each period. Since CFPS surveys are conducted every 2 years, the coefficients are shown every 2 years. The meaning of the other variables are the same as in Formula (1).
The statistical analysis in this study was carried out using Stata Version 16.0 (Stata/SE, StataCrop LLC, TX, USA).
3. Results
3.1. Sample characteristics
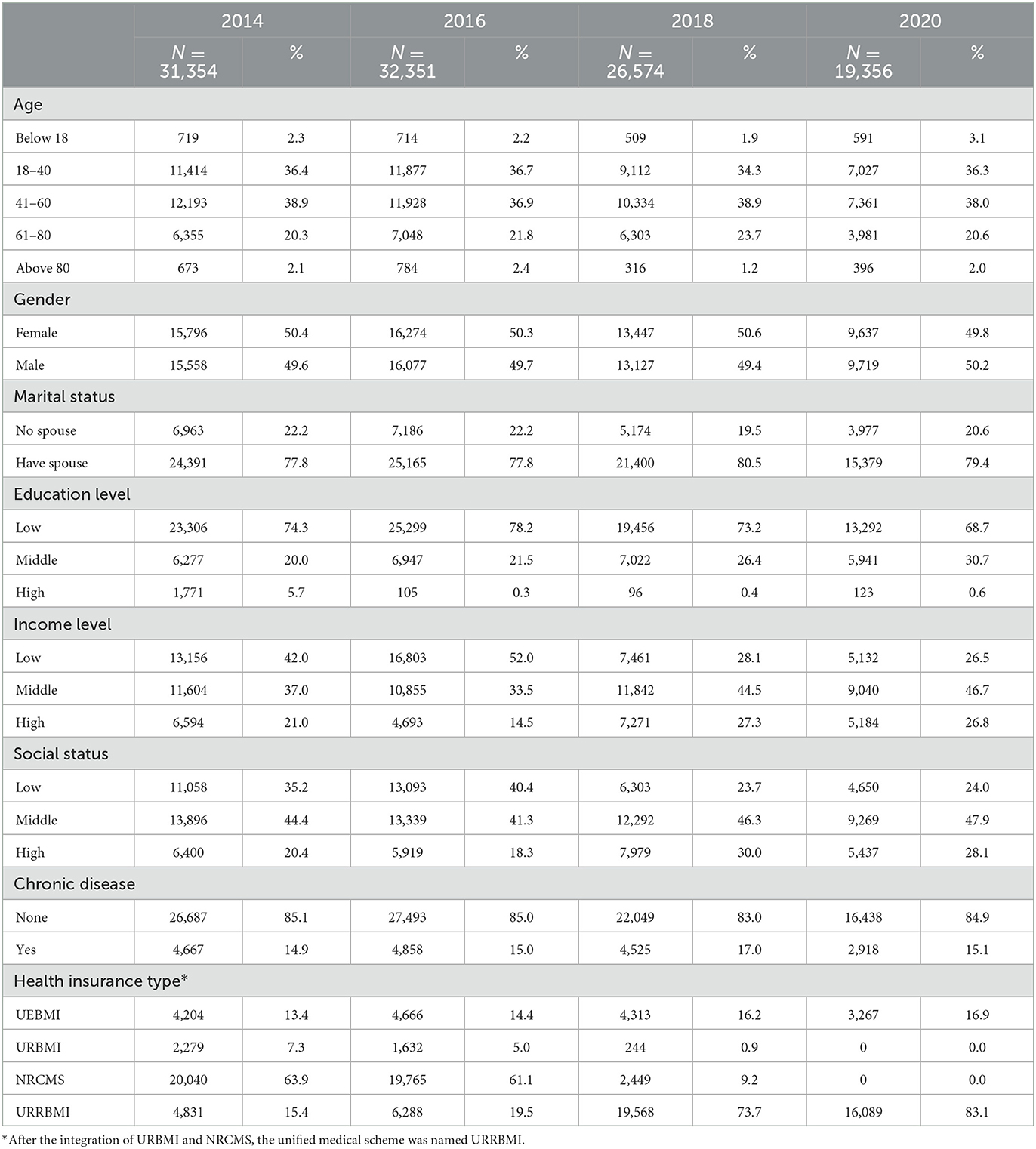
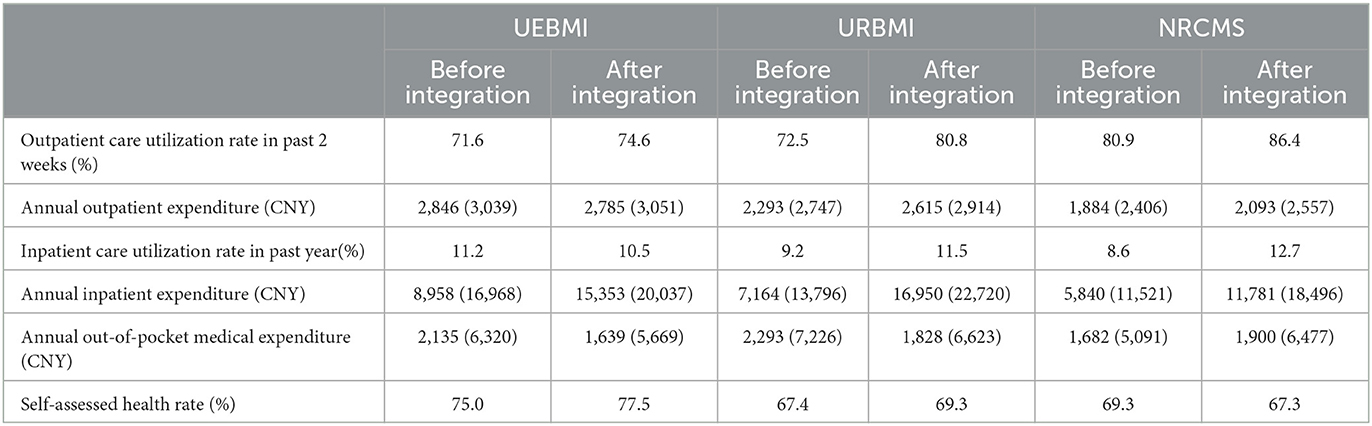
The characteristics of the sample in this study are summarized in Table 2. The total sample size was 109,635, with young adults (aged 18–40) and middle-aged adults (aged 41–60) being predominant in all of the included samples. The proportion of different genders reflected the ratio observed for the wider population. Nearly 80% of the participants in sample were married. Most of the participants have a low level of education, with <1% having a high level of education. Most of the participants have a medium level of income and social status, with relatively few having a low or high level. In addition, the majority of the participants are not listed as having a chronic disease. Aside from 2020, for which there is only a small sample, there were no significant differences in the sample size and composition features among the data for the other years considered (2012, 2014, 2016, and 2018). The proportion of URRBMI in sample increased year by year, increasing from 15.4% in 2014 to 83.1% in 2020 (as of 2020, all the provinces in CFPS database have completed health insurance integration, and the dates of URRBMI implementation in China are presented in Supplementary Table 1). The averages and standard deviations of the independent variables in this study are displayed in Table 3, classified by health insurance type.
3.2. Results of main regression
It can be seen from the event study (see Supplementary Figures 1–6) that 95% CI of the coefficients β of each dependent variable before health insurance integration contain 0, indicating that the difference between the intervention group and the control group is not statistically different. As a result, the trends of the outcome variables in control group and intervention group can be observed as being parallel before health insurance integration, and so DID approach can be used to analyze the policy effect.
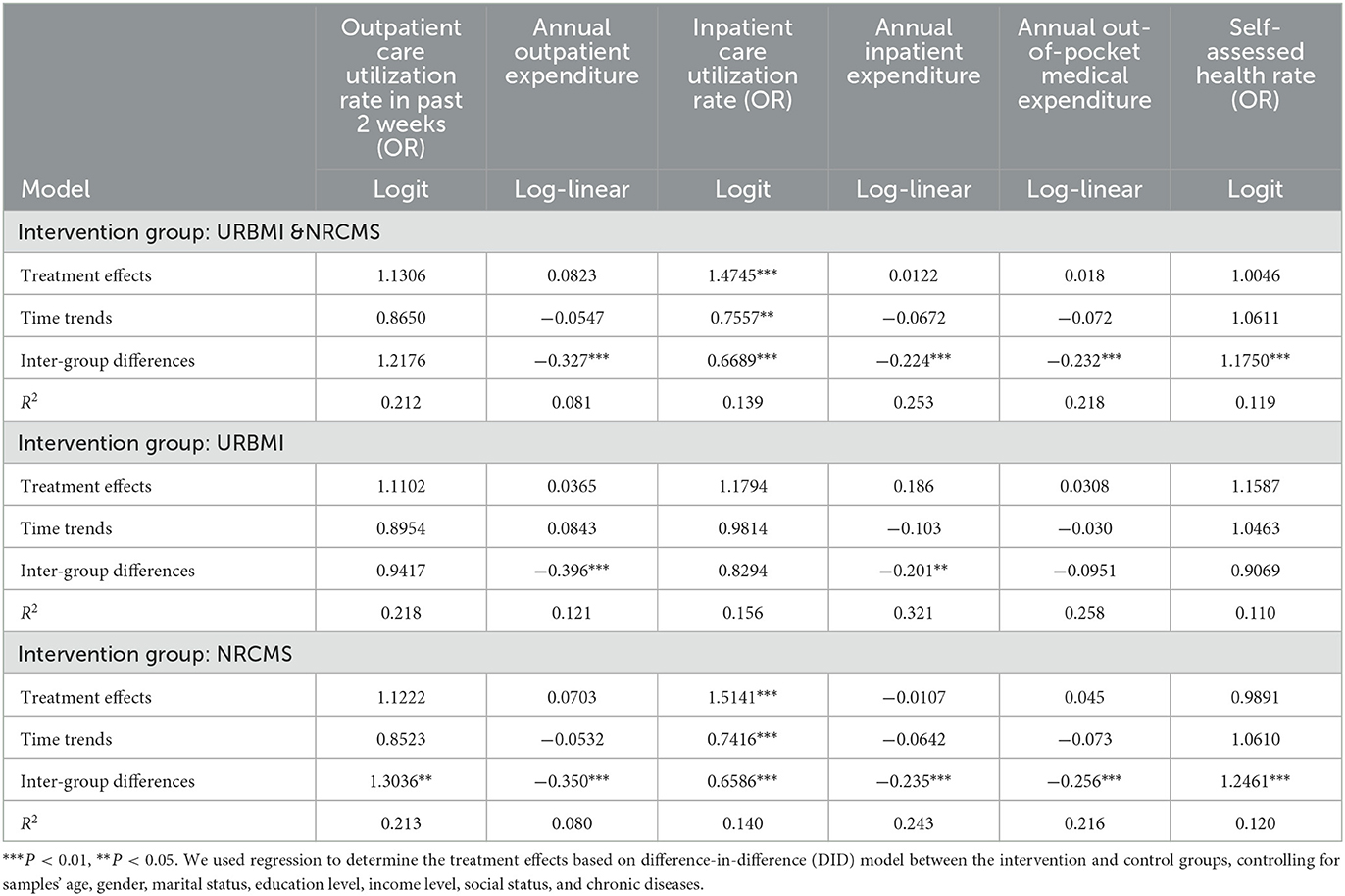
From the main regression results presented in Table 4, it can be seen that, after the implementation of the integration, the odds ratio (OR) of inpatient rate of the participants is 1.47, which is statistically significant, while the changes in 2-week outpatient utilization, total expenditure of inpatient and outpatient, total expenditure of annual co-payment and health status are not statistically significant. Comparing the URBMI and NRCMS as the intervention group, respectively, with the control group (UEBMI), the integration program mainly produced significant effects among the participants whose original medical insurance type was NRCMS, and the odds ratio (OR) of inpatient rate among this group is 1.51. However, health service utilization and the expenditure associated with people who enrolled URBMI before the integration cannot be seen to have produced significant changes after the implementation of the integration program.
3.3. Heterogeneity in results
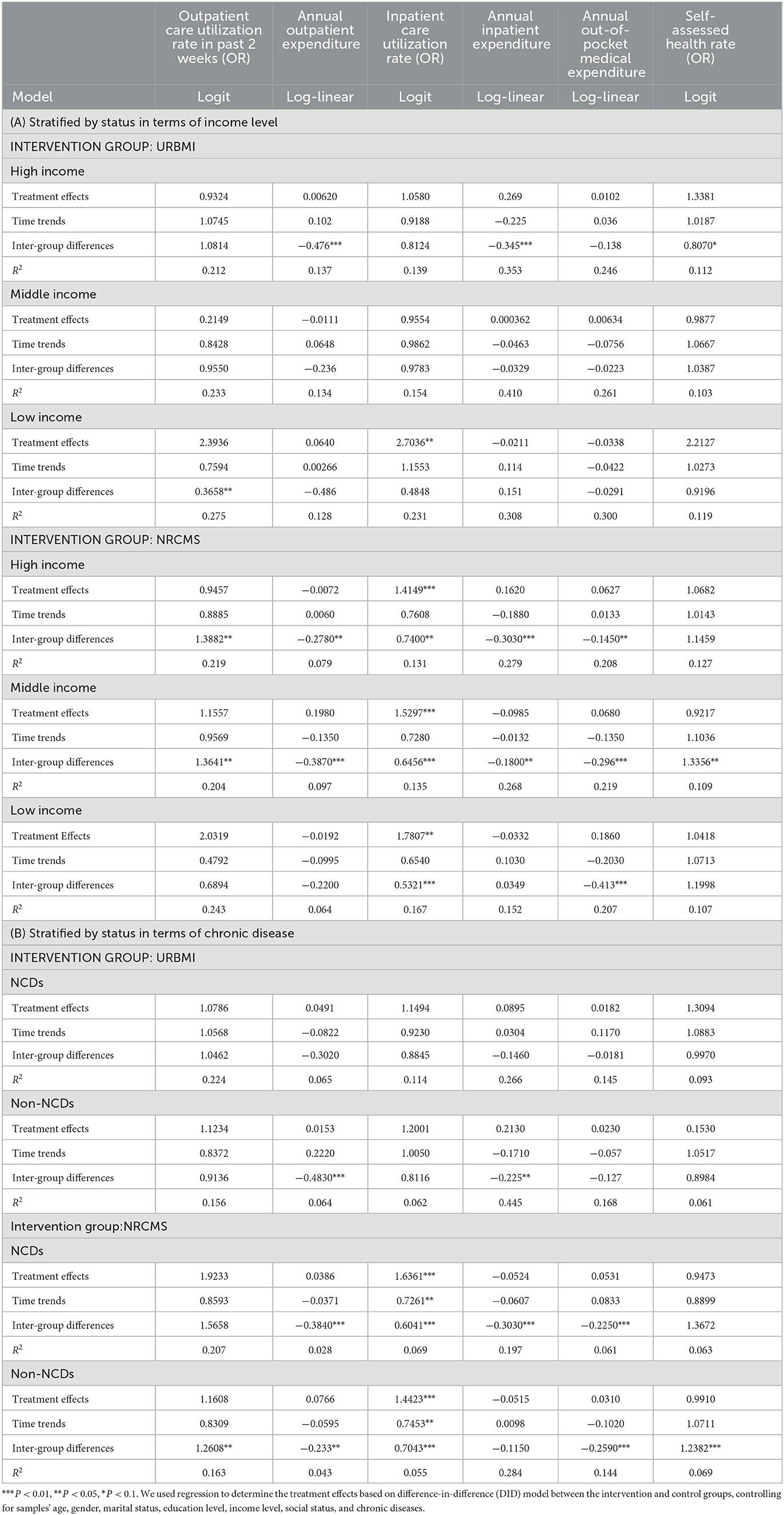
The sample of this study was divided into three groups according to income (low income, middle income, high-income). Through regression analysis, it was found that the low-income group was more significantly affected by the integration, as evidenced by an odds ratio (OR) in inpatient service utilization of 2.70 for participants whose original insurance type was URBMI and one of 1.78 for participants whose original insurance type was NRCMS. Meanwhile, an increase of inpatient rate can also be witnessed for middle-or high-income participants whose original insurance type was NRCMS. In relation to this, the odds ratio (OR) of inpatient rate for middle-income participants is 1.53, and for high-income participant is 1.41 (see Table 5A).
In addition, stratified by status in terms of chronic disease, the results show a statistically significant effect regarding the implementation of the integration on both rural residents with and without chronic disease, mainly in the form of an increase in inpatient services utilization. Meanwhile, the odds ratio (OR) of inpatient rate of rural participants with chronic disease is 1.64, which is higher than that for those without chronic disease (only 1.44; see Table 5B).
4. Discussion
In this study, the influence of URRBMI in China was analyzed by using 8 years of CFPS data, focusing on the changes in the health service utilization gaps between urban and rural residents. The period of 2014 to 2020 was considered on the basis that, during this 8-year period, the URRBMI was introduced or implemented in most of the Chinese provinces. Compared with previous studies that consider only certain provinces or shorter-term impacts, the evidence obtained in this study is more reliable.
The analysis demonstrated that rural residents in China are associated with a significant increase in inpatient service utilization (OR = 1.51, P < 0.01) after the implementation of URRBMI. The regression results by income stratum show that the inpatient service utilization among high-, middle- and low-income groups in rural area all increased. Meanwhile, analysis in terms of chronic disease status showed a significant increase in inpatient rate for rural residents. These findings enable acceptance of the basic hypothesis that the integration of URBMI and NRCMS has increase the insurance cover level of NRCMS, thus increasing the accessibility of inpatient services. Moreover, the participants whose original health insurance type was URBMI with a low level of income can also be seen to have benefited from the integration program, since the inpatient utilization has also increased in this group. This may be due to the point that it is possible to spread risk through expanding the size of the pool, thus providing vulnerable groups with greater access to health services.
Furthermore, while the utilization of inpatient services increased among rural residents, no such increase was found in respect of inpatient expenditure, and the increase in personal burden was also not found to be significant. This suggests that the URRBMI is an initiative program that has had benefits for poorer service users. In addition, no changes were found for outpatient service utilization among rural residents. There are two potential reasons for this. First, the baseline of outpatient services among rural residents was higher; second, health insurance programs in China have been designed to focus on covering expenditure for inpatient services rather than outpatient services, reducing the impact of URRBMI on outpatient services (2).
Overall, it was found that inpatient utilization has significantly increased among rural residents after the implementation of URRBMI, especially among the lower-income population. In this respect, the findings reported here are consistent with those reported by Huang et al., who analyzed data from the China Health and Retirement Longitudinal Study (CHARLS) for the period between 2011 and 2015. Similar comments apply to work by Paek et al., who analyzed data from the Health and Welfare survey database from after 2013 in respect of Thailand and found that the Universal Coverage Scheme highly increased inpatient utilization among the low-income group (16, 18). At the same time, however, a very mixed range of results has been cited in previous studies exploring the effects of URRBMI on outpatient utilization. For example, in research by Ma et al., Shi et al., and Su et al., it is reported that that the integration of URRBMI has significantly improved outpatient care utilization among middle-aged and elderly people in rural China; Huang et al. and Xu et al., by comparison, find no significant impact of the integration on rural residents' outpatient care utilization (16, 19–22). In the present study, a positive increase was found on outpatient utilization among low- and middle-income rural residents, but not to a statistically significant extent. This pattern may be explained in terms of the difference in datasets used. While previous studies have mainly focused on middle-aged and older residents or local situations, the present study used a nationally representative and longitudinal dataset covering the entire population to the inclusion of eight previous years of data (16, 19–22).
There are several limitations affecting the current study that must be acknowledged. First, due to certain constraints, the CFPS database lacks data on the co-payment rates of inpatient and outpatient services for participants at the individual or group level. As a result, it was not possible to evaluate insurance-related benefits after the implementation of URRBMI. Secondly, information is absent on the level of healthcare facilities utilized by participants, and so it was not possible to evaluate whether URRBMI caused changes in patient flow or fluctuations in health expenditure. Finally, it was not possible to determine whether patients have been overutilizing inpatient services in such a way that this has resulted in a “false” increase in inpatient rate after the increase of health care security level. This is due to a lack of specific information on inpatient conditions, including primary diagnoses and so on.
5. Conclusion
China URRBMI implementation has expanded the risk pool and improved the ability of the health insurance program to withstand risks. It has also improved coverage despite constraints in funding. In this respect, URRBMI has effectively improved health service utilization among rural residents, and this has played a positive role in narrowing the gaps in health service utilization between rural and urban areas, as well as in regional equity in health services. There is good reason to consider that such experiences can be extended to countries and regions where there are still multiple health insurance programs covering different populations. If this is done, it may be possible to improve the equity of health services by enhancing management capacity and seeking to integrate health insurance programs. In this way, progress toward UHC's goal of ensuring equitable access to health services can be made.
Data availability statement
The datasets generated and analyzed for this study can be found in the CFPS repository. Please see http://www.isss.pku.edu.cn/cfps/ for more details, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Biomedical Ethics Review Committee of Peking University approved CFPS, and all participants were required to provide written informed consent. The ethical approval number was IRB00001052-14010. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author contributions
QL performed the data compilation and formal data analysis, interpreted the findings, and the manuscript. LZ conceptualized, drafted, wrote the manuscript, and interpreted the findings. WJ conceived of the study and participated in its design and coordination and helped to draft the manuscript. All authors have read and approved the final version of the manuscript and agree with the order of presentation of the authors.
Acknowledgments
We thank Wuping Zhou for his assistance in data collection and data analysis of this paper.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2023.1106166/full#supplementary-material
References
1. Zhou S, Huang T, Li A, Wang Z. Does universal health insurance coverage reduce unmet healthcare needs in China? Evidence from the National Health Service Survey. Int J Equity Health. (2021) 20:43. doi: 10.1186/s12939-021-01385-7
2. Lei X, Lin W. The New Cooperative Medical Scheme in rural China: does more coverage mean more service and better health? Health Econ. (2009) 18 Suppl 2:S25–46. doi: 10.1002/hec.1501
3. Diao L, Liu Y. Inequity under equality: research on the benefits equity of Chinese basic medical insurance. BMC Health Serv Res. (2020) 20:710. doi: 10.1186/s12913-020-05584-w
4. Zhao M, Liu B, Shan L, Li C, Wu Q, Hao Y, et al. Can integration reduce inequity in healthcare utilization? Evidence and hurdles in China. BMC Health Serv Res. (2019) 19:654. doi: 10.1186/s12913-019-4480-8
5. Dib HH, Pan X, Zhang H. Evaluation of the new rural cooperative medical system in China: is it working or not? Int J Equity Health. (2008) 7:17. doi: 10.1186/1475-9276-7-17
6. Yang X, Chen M, Du J, Wang Z. The inequality of inpatient care net benefit under integration of urban-rural medical insurance systems in China. Int J Equity Health. (2018) 17:173. doi: 10.1186/s12939-018-0891-0
7. Ren Y, Zhou Z, Cao D, Ma BH, Shen C, Lai S, et al. Did the integrated urban and rural resident basic medical insurance improve benefit equity in China? Value in Health. (2022) 25:1548–58. doi: 10.1016/j.jval.2022.03.007
8. National Health Service Survey Report in 2013. (2013). Available online at: http://www.nhc.gov.cn/mohwsbwstjxxzx/s8211/201610/9f109ff40e9346fca76dd82cecf419ce.shtml (accessed November 23, 2022).
9. Zhou Q, He Q, Eggleston K, Liu GG. Urban-rural health insurance integration in china: impact on health care utilization, financial risk protection, and health status. Appl Econ. (2022) 54:2491–509. doi: 10.1080/00036846.2021.1998323
10. The State Council. Opinions of the State Council on Integrating the Medical Insurance System for Urban and Rural Residents. (2016). Available online at: http://www.gov.cn/zhengce/content/2016-01/12/content_10582.htm (accessed November 23, 2022).
11. Bazyar M, Yazdi-Feyzabadi V, Rashidian A, Behzadi A. The experiences of merging health insurance funds in South Korea, Turkey, Thailand, and Indonesia: a cross-country comparative study. Int J Equity Health. (2021) 20:66. doi: 10.1186/s12939-021-01382-w
12. Lagomarsino G, Garabrant A, Adyas A, Muga R, Otoo N. Moving towards universal health coverage: health insurance reforms in nine developing countries in Africa and Asia. Lancet. (2012) 380:933–43. doi: 10.1016/S0140-6736(12)61147-7
13. Zhang H, Wang H, Yan H, Wang X. Impact of internet use on mental health among elderly individuals: a difference-in-differences study based on 2016–2018 CFPS Data. Int J Environ Res Public Health. (2021) 19:101. doi: 10.3390/ijerph19010101
14. Tang S, Yao L, Ye C, Li Z, Yuan J, Tang K, et al. Can health service equity alleviate the health expenditure poverty of Chinese patients? Evidence from the CFPS and China health statistics yearbook. BMC Health Serv Res. (2021) 21:718. doi: 10.1186/s12913-021-06675-y
15. Ma X, Wang Z, Liu X. Progress on catastrophic health expenditure in China: evidence from China family panel studies (CFPS) 2010 to 2016. Int J Environ Res Public Health. (2019) 16:4775. doi: 10.3390/ijerph16234775
16. Huang J, Yuan L, Liang H. Which matters for medical utilization equity under universal coverage: insurance system, region or SES. Int J Environ Res Public Health. (2020) 17:4131. doi: 10.3390/ijerph17114131
17. Yang D, Acharya Y, Liu X. Social health insurance consolidation and urban-rural inequality in utilization and financial risk protection in China. Soc Sci Med. (2022) 308:115200. doi: 10.1016/j.socscimed.2022.115200
18. Paek SC, Meemon N, Wan TT. Thailand's universal coverage scheme and its impact on health-seeking behavior. Springerplus. (2016) 5:1952. doi: 10.1186/s40064-016-3665-4
19. Ma C, GZ, Hai Gu. The effects of urban-rural integrated medical insurance system on substantial equity of health care and health — based on equality of opportunity. J Stat Res. (2016) 4:8. doi: 10.16149/j.cnki.23-1523.2017.02.009
20. Shi Z, He P, Zhu D, Lu F, Meng Q. Changes in health care utilization and financial protection after integration of the rural and urban social health insurance schemes in Beijing, China. BMC Health Serv Res. (2022) 22:1226. doi: 10.1186/s12913-022-08602-1
21. Su D, Chen Y-c, Gao H-x, Li H-m, Chang J-j, Jiang D, et al. Effect of integrated urban and rural residents medical insurance on the utilisation of medical services by residents in China: a propensity score matching with difference-in-differences regression approach. BMJ Open. (2019) 9:e026408. doi: 10.1136/bmjopen-2018-026408
Keywords: health insurance integration, URRBMI, health service utilization, health equity, China
Citation: Li Q, Zhang L and Jian W (2023) The impact of integrated urban and rural resident basic medical insurance on health service equity: Evidence from China. Front. Public Health 11:1106166. doi: 10.3389/fpubh.2023.1106166
Received: 23 November 2022; Accepted: 20 February 2023;
Published: 13 March 2023.
Edited by:
Mingsheng Chen, Nanjing Medical University, ChinaReviewed by:
Chenggang Jin, Beijing Normal University, ChinaMingming Xu, School of Public Health, Sun Yat-sen University, China
Copyright © 2023 Li, Zhang and Jian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weiyan Jian, jianweiyan@bjmu.edu.cn
 Qiaosheng Li
Qiaosheng Li Lanyue Zhang
Lanyue Zhang Weiyan Jian
Weiyan Jian