Risk Factors for the Occurrence and Progression of Posttraumatic Elbow Stiffness: A Case-Control Study of 688 Cases
- 1Department of Orthopedics, Shanghai Jiao Tong University Affiliated Sixth People's Hospital, Shanghai, China
- 2Youth Science and Technology Innovation Studio, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 3School of Public Health, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 4Shanghai Sixth People's Hospital East Affiliated to Shanghai University of Medicine & Health Sciences, Shanghai, China
Background: Elbow stiffness is a severe complication after trauma. Surgical or conservative treatments may be ineffective for restoring functional elbow motion. We aim to evaluate intrinsic and extrinsic factors for the occurrence and severity of elbow stiffness.
Methods: This retrospective case–control study included mild/moderate stiffness, severe stiffness, and non-stiffness groups between January 2011 and December 2017 at a single orthopedic center. Multivariable logistic regression analysis and subgroup analysis were used to evaluate age, gender, body mass index, muscle strength, fracture type and site, injury mechanism, immobilization time, elbow dysfunction time, multiple surgeries, nerve symptoms, physical therapy, smoking and alcohol abuse, and dominant hand of stiff elbow as potential risk factors for the occurrence and severity of elbow stiffness.
Results: There were 461 patients in the stiffness group and 227 patients in the non-stiffness group. The odds ratios (ORs) of the age, muscle strength, and injury mechanism were 0.960, 0.333, and 0.216 for the occurrence of elbow stiffness. In subgroup evaluation, increased cast immobilization time might be a risk factor for patients receiving conservative therapies (OR = 2.02; p = 0.014). In the evaluation on factors for progression of elbow stiffness, “multiple surgeries” might be a risk factor in surgical treatment by subgroup analysis (OR = 1.943; p = 0.026). Nevertheless, alcohol abuse might increase severity of elbow stiffness in conservatively treated patients (OR = 3.082; p = 0.025).
Conclusion: Increased cast immobilization time in the conservative therapy might be a risk factor for stiffness occurrence. Multiple surgeries might be risk factors for stiffness progression. Alcohol abuse potentially increased stiffness severity after conservative treatment.
Introduction
Elbow motion loss results in considerable daily function and personal hygiene limitation. Elbow stiffness is characterized by restriction in flexion, extension, supination, or pronation (1–4). Trauma is the most common cause for elbow stiffness. Around 10–15% patients fail to recover from elbow injuries and experience motion limitation (5). The etiology mainly includes heterotopic ossification (HO), joint contracture, delay, or failure in bone repair and arthritic degeneration (6–10). The pathophysiological changes are inflammation and fibroblast proliferation in the elbow (11). Previous research reported different protocols on elbow stiffness treatment and interfering factors of improving the prognosis (12–15). Nevertheless, the treatment of elbow stiffness is difficult and the sequel is still not ideal. Many patients experience limited function improvement or even recurrent stiffness after operative or conservative treatment (16–18). Therefore, it is urgent and vital to investigate possible risk factors behind elbow stiffness. Some studies claimed extended elbow immobilization, severe fracture, and multiple surgeries within a short period of time as primary potential risk factors (19, 20). Comprehensive evaluation based on a large sample size is still lacking. In the present study, we discuss and analyze potential risk factors for the onset and progression of elbow stiffness after upper-extremity trauma for the first time. We hypothesize the involvement of some demographical and injury- and treatment-related factors in elbow stiffness.
Methods
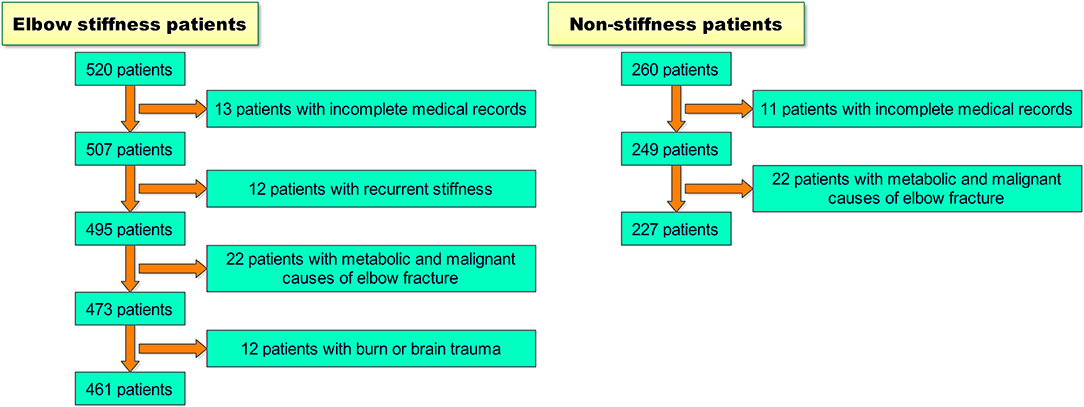
A retrospective case–control study was performed between January 2011 and December 2017 at Shanghai Jiao Tong University affiliated Sixth People's Hospital. Patients were reviewed who were diagnosed with elbow stiffness after upper-extremity trauma and had upper-extremity trauma but did not develop elbow stiffness. In the elbow stiffness group, the inclusion criteria were (1) skeletal mature and complete bone healing, (2) elbow range of motion (ROM) <100°, and (3) history of surgical intervention or conservative treatment for upper-extremity trauma. Exclusion criteria were (1) incomplete medical records, (2) recurrence of elbow stiffness, (3) metabolic and malignant causes of elbow fracture, and (4) burn or brain trauma. In the non-stiffness group, participants did not develop elbow stiffness after upper-extremity trauma. The inclusion criteria were (1) skeletal mature and complete bone healing, (2) elbow ROM ≥100°, and (3) history of surgical intervention or conservative treatment for upper-extremity trauma. Exclusion criteria were (1) incomplete medical records and (2) metabolic and malignant causes of elbow fracture. We reviewed all elbow stiffness patients from our medical history system between January 2011 and December 2017. Among all the 520 patients, we excluded 13 patients with incomplete medical records, 12 patients with recurrent stiffness, 22 patients with metabolic and malignant causes of elbow fracture, and 12 patients with burn or brain trauma. We also reviewed 260 non-stiffness patients by a 2:1 ratio using random sampling from our medical history system during the same period of time. We excluded 11 patients with incomplete medical records and 22 patients with metabolic and malignant causes of elbow fracture. Finally, we included 688 patients in this study, including 461 elbow stiffness patients (233 in the mild/moderate elbow stiffness group, 228 in the severe elbow stiffness group) and 227 non-stiffness patients (Scheme 1).
Mild/moderate elbow stiffness refers to elbow ROM of 50–100°, and severe elbow stiffness refers to elbow ROM of 0–50°. We included some intrinsic demographic factors and extrinsic injury-related factors for consideration from the patients' medical records in this study. Demographic information included age, sex, body mass index (BMI), smoking, alcohol abuse, and dominant hand. BMI was classified into underweight, normal-weight, overweight, and obese levels according to Chinese standard (21). Injury-related information included muscle strength, fracture type, fracture site, injury mechanism, immobilization time, elbow dysfunction time, rehabilitation exercise, nerve symptoms, and multiple surgeries (no fewer than 2 surgeries for the primary trauma and subsequent complications) history. Handgrip muscle strength was measured by a dynamometer around the time of treatment and categorized into normal muscle strength and muscle weakness. Fractures were categorized into open, closed, and combined (multiple fractures with both open and closed wounds) fractures. The injury mechanism involved low-energy trauma (falls from ground levels) and high-energy trauma (e.g., traffic accidents and falls from significant levels). The immobilization involved preoperative, postoperative, and conservative cast immobilization. Fracture sites included distal humerus fracture, radial head fracture, olecranon fracture, terrible triad, elbow dislocation, multiple fractures, and other peri-articular fractures that could fall into either category previously according to the AO classification system. Three independent senior surgeons for elbow surgery reviewed clinical information, including imaging and elbow ROM, and decided their classification of stiffness severity, fracture location, and types. Positive nerve symptoms referred to lasting numbness in upper extremities at least 3 months after an initial injury. We performed subgroup analysis based on treatment type (surgery or conservative therapy) because some variables only existed in either surgery or conservative treatment. Oral and informed consents were acquired from all participants in this study. The IRB approval was obtained from Shanghai Jiao Tong University affiliated Sixth People's Hospital East Campus (No. 2018-013).
Statistical Analysis
The continuous variables with normal and skewed distribution were displayed by median (p25, p75), and the categorical variables were displayed by frequency (percent). Respectively, T-test or non-parametric rank-sum test was adopted to compare the difference between groups of continuous variables, and chi-square test (or Fisher's exact test, where applicable) or non-parametric rank-sum test was adopted to compare the difference between groups of qualitative data. Variables that showed significances between groups in univariate analysis were further evaluated in multivariate analysis using the logistic regression model. A P-value of <0.05 was considered as statistical significance. Statistical analyses were conducted by SPSS 22.0 (IBM, New York, USA).
Results
Factors in the Occurrence of Elbow Stiffness
In the demographic information, significant differences were found in age (p < 0.001), sex (p = 0.001), BMI (p = 0.009), smoking (p = 0.034), and alcohol abuse (p < 0.001) between elbow stiffness and non-stiffness groups (Table 1). In the injury-related information, there were significant differences in muscle strength (p < 0.001), injury mechanism (p < 0.001), and fracture site (p < 0.001) between the above two groups (Table 1). In the multiple logistic regression analysis, sex, BMI, smoking, or alcohol abuse showed insignificant differences between stiffness and non-stiffness groups. The odds ratios (ORs, 95% confidence interval, CI) of the age, muscle strength, and injury mechanism were 0.960 (0.947, 0.973), 0.333 (0.227, 0.488), and 0.216 (0.128, 0.365) (Table 2).
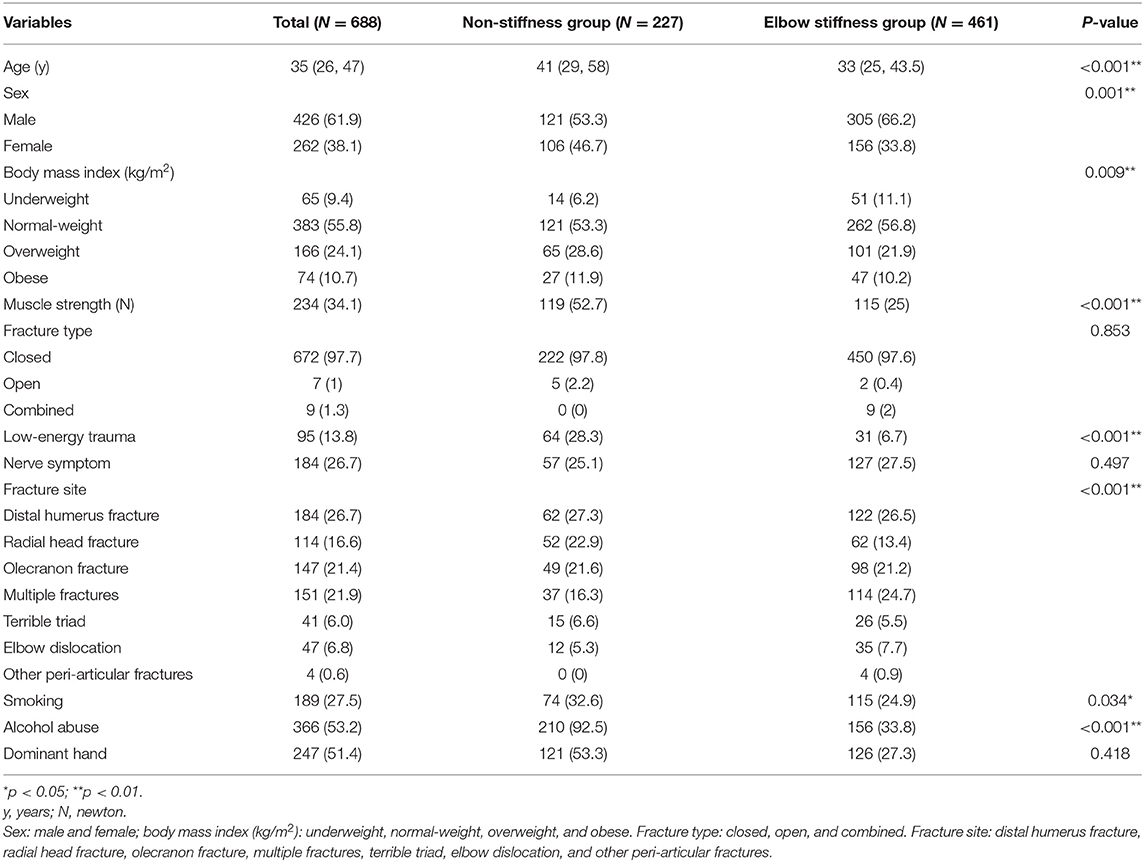
Table 1. Demographic and injury-related information in elbow stiffness group and non-stiffness group.
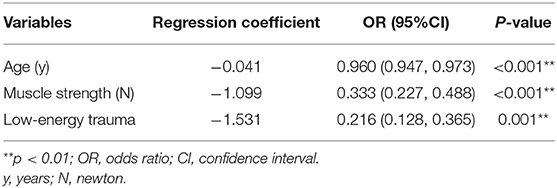
Table 2. Multiple logistic regression analysis of significantly different variables between elbow stiffness and non-stiffness groups.
In the subgroup analysis by surgery, some variables showed a statistically significant difference between elbow stiffness and non-stiffness groups, such as the age (p = 0.001), preoperative immobilization time (p < 0.001), postoperative immobilization time (p < 0.001), sex (p < 0.001), muscle strength (p < 0.001), and injury mechanism (p = 0.001) (Table 3). In the multiple logistic regression analysis, the onset of elbow stiffness might be inversely correlated with the age (OR = 0.95; 95% CI = 0.94, 0.97; p < 0.001), preoperative immobilization time (OR = 0.69; 95% CI = 0.57, 0.84; p < 0.001), postoperative immobilization time (OR = 0.90; 95% CI = 0.87, 0.94; p < 0.001), muscle strength (OR = 0.24; 95% CI = 0.15, 0.41; p < 0.001, and low-energy trauma (OR = 0.14; 95% CI = 0.07, 0.27; p < 0.001).
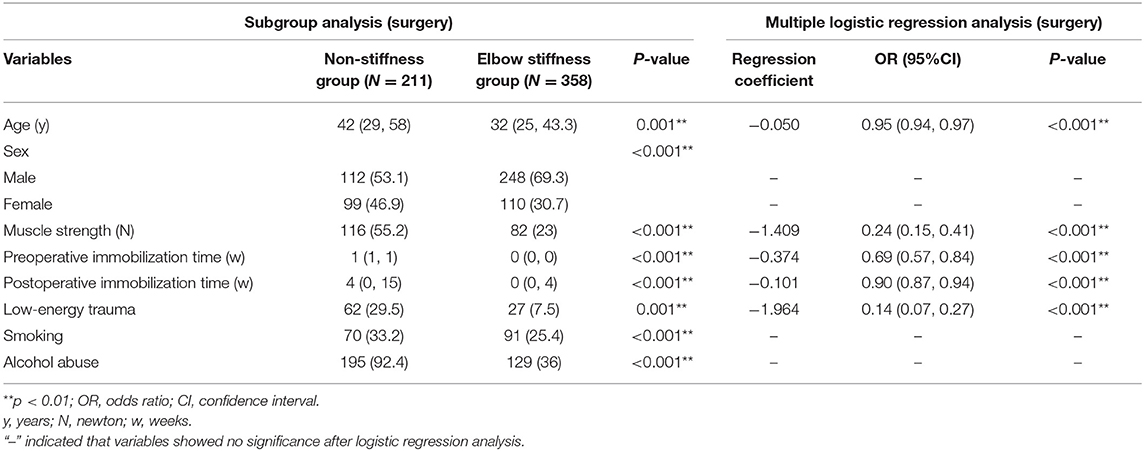
Table 3. Subgroup analysis and multiple logistic regression analysis on occurrence of elbow stiffness by treatment type (surgery).
Conservative therapies were applied in 103 patients from the elbow stiffness group and 16 patients from the non-stiffness group. The subgroup analysis based on conservative treatment indicated that there were significant differences in variables, like the cast immobilization time (p = 0.003), nerve symptoms (p = 0.045), and alcohol abuse (p < 0.001) (Table 4). In the multiple logistic regression analysis, only immobilization time displayed a statistical difference between elbow stiffness and non-stiffness groups for conservative treatment (OR = 2.02; 95% CI = 1.15, 3.54; p = 0.014, Table 4).
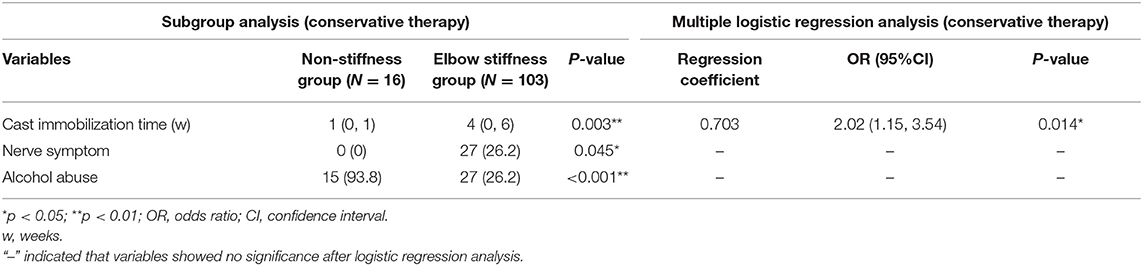
Table 4. Subgroup analysis and multiple logistic regression analysis on occurrence of elbow stiffness by treatment type (conservative therapy).
Factors in the Severity of Elbow Stiffness
In the demographic data, only “age” showed significant differences between mild/moderate and severe elbow stiffness groups (p = 0.001, Table 5). In the injury-related data, there were significant differences in muscle strength only (p = 0.031, Table 5). In the multiple logistic regression analysis, neither age nor muscle strength displayed any difference between mild/moderate and severe elbow stiffness groups.
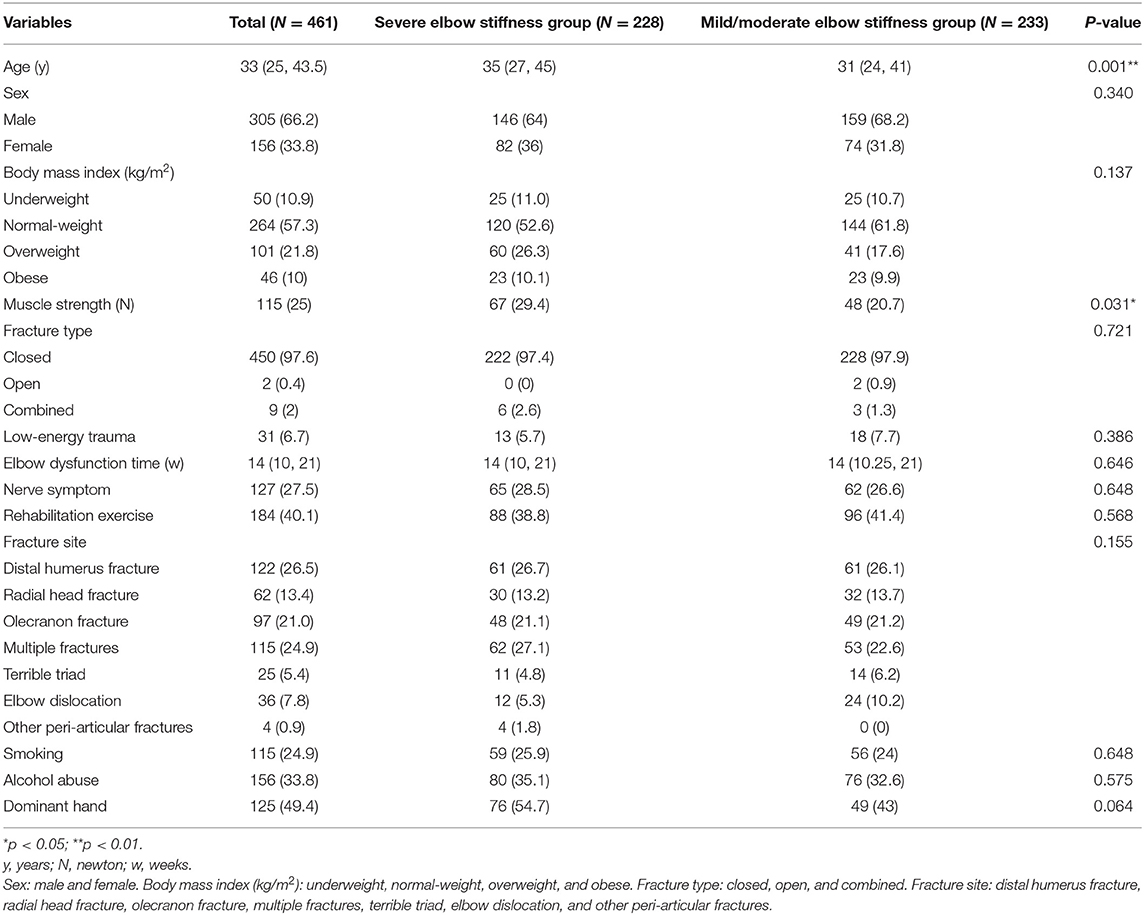
Table 5. Demographic and injury-related information in severe and mild/moderate elbow stiffness groups.
In the subgroup analysis by surgery, the severity of elbow stiffness might be correlated with the age (p = 0.001) and multiple surgeries (p = 0.038) (Table 6). The age and multiple surgeries were evaluated in surgery groups by the multiple logistic regression analysis. “Multiple surgeries” might be associated with increasing severity of elbow stiffness (OR = 1.943; 95% CI = 1.081, 3.490; p = 0.026, Table 6). In the conservative therapies, there were significant differences in the age (p = 0.003), fracture site (p = 0.040), and alcohol abuse (p = 0.016) between mild/moderate and severe elbow stiffness groups (Table 7). Further analysis indicated that the age and alcohol abuse might be risk factors for increased severity of elbow stiffness (age: OR = 1.047; 95% CI = 1.011, 1.085; p = 0.011; alcohol abuse: OR = 3.082; 95% CI = 1.153, 8.237; p = 0.025, Table 7).
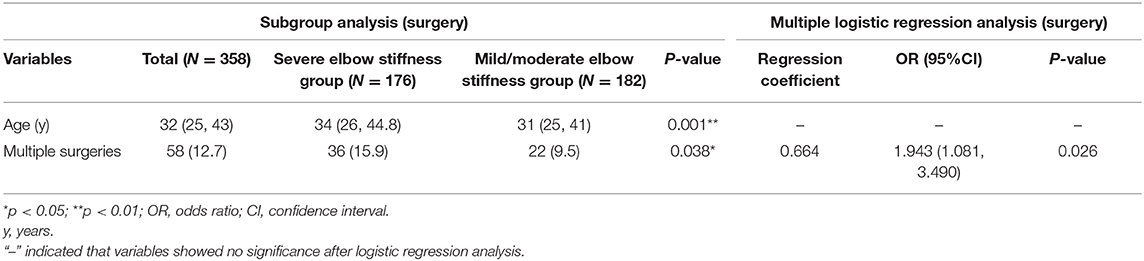
Table 6. Subgroup analysis and multiple logistic regression analysis on severity of elbow stiffness by treatment type (surgery).
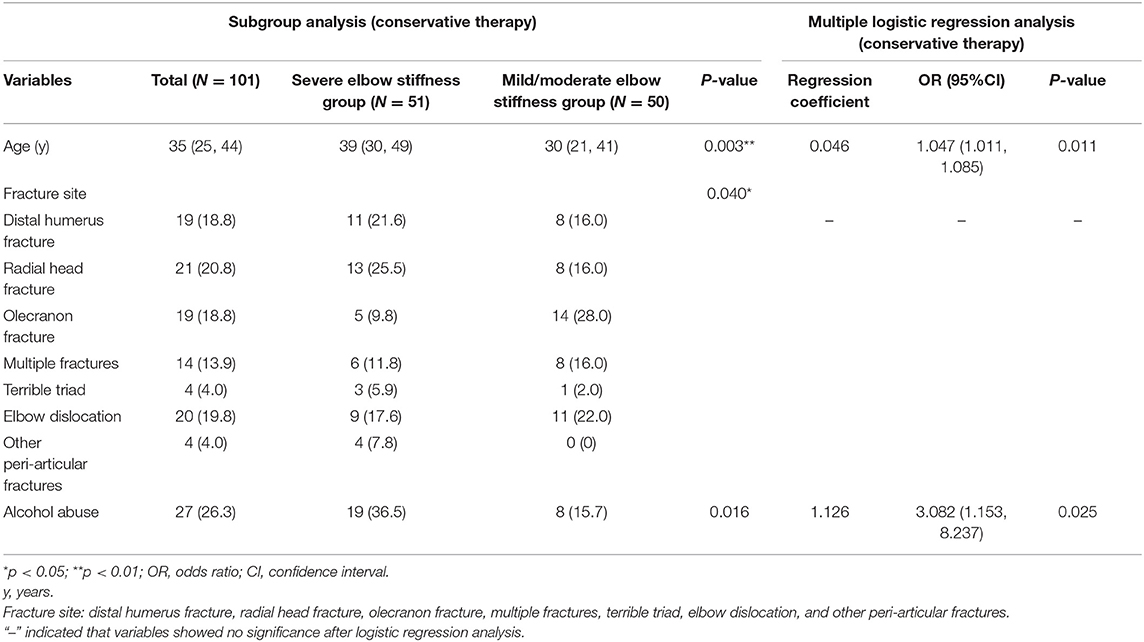
Table 7. Subgroup analysis and multiple logistic regression analysis on severity of elbow stiffness by treatment type (conservative therapy).
Discussion
Elbow injuries are common in trauma. At present, the treatment is ineffective and therefore it is urgent and important to investigate the possible risk factors. In this study, elbow stiffness patients due to traumatic elbow injuries were included instead of other origins. We evaluated risk factors in the occurrence of traumatic elbow stiffness. Younger age, lower muscle strength, and high-energy trauma were associated with the occurrence of elbow stiffness. These variables were validated further in subgroup analysis.
Previously, there were few studies on the potential influence of age in the onset of elbow stiffness. In this study, older age was found to potentially decrease risks for elbow stiffness. According to our observation and literature, young patients tend to develop severe elbow contracture and motion limitation. Their skeletomuscular system is developing rapidly. It may stimulate excretion of different growth factors and contribute to bone regeneration and irregular HO formation (22). The finding was also confirmed in another recent study. Carlock et al. reported that patients with elbow contracture were younger than the non-contracture ones (47.1 vs. 54.9 years, P = 0.004) (23).
Severe stiffness patients suffered from high-energy injuries and were treated by multiple-hardware fixation. They might have a bigger chance of developing stiff elbows due to prolonged postoperative immobilization time (24). There were some debates on the immobilization time. Some literature recommended early postoperative activity because it was good for maintaining elbow motion and preventing stiffness, but protocols varied in different studies. Taylor et al. reported that early mobilization at 3 days after reduction of elbow dislocation increased elbow motion compared by cast immobilization. However, their results were statistically insignificant (25). Increased immobilization time in surgery groups appeared to be a beneficial factor, which was contrasted with its role in conservative therapy. Temporary cast immobilization before surgery was good for anatomical reduction during surgery. It also avoided additional damages to neighboring tissues (26). The connective tissues, such as peripheral nerves, tendons, and ligaments were usually released and repaired intra-operatively. Suitable postoperative immobilization is beneficial for restoring the local structure and regenerating impaired tissues. However, few patients received surgeries within 24 h after injury in this study. This fact might cause bias on the role of immobilization time in the surgical treatment. An appropriate length of immobilization time should be investigated in the future.
For conservative therapies, increased immobilization might be a risk factor for elbow stiffness occurrence. For instance, for each additional week, the risk of elbow stiffness increased by 1.02-fold. Monument et al. believed that prolonged cast immobilization was harmful to elbow motion because it might stimulate capsule contracture and fibrosis and cause structural deformation within the periarticular areas (27). Muscle strength was positively associated with lower occurrence of elbow stiffness. This point was in agreement with some previous literature (28, 29). Lengthy immobilization due to severe trauma, unwillingness, or pain caused muscle atrophy and capsular contracture (30).
We preliminarily found out that the age and muscle strength were correlated with increased severity of elbow stiffness in univariate analysis. However, they were later excluded after multiple logistic regression analysis.
Then, patients were categorized by treatment type so that surgical intervention could be evaluated as a primary factor in deterioration of elbow stiffness. In this study, “multiple surgeries” might be a risk factor in surgical treatment by subgroup analysis (OR = 1.943; p = 0.026). In patients receiving surgeries, it was found to be the only prominent risk factor that might cause severe elbow stiffness. The reasons for multiple surgeries mainly include dislocation, material failure, and change from external fixator to plate. Compared with those who received a single surgery, patients who received multiple surgeries had a 1.943-fold higher risk of developing severe elbow stiffness. Jupiter et al. found that multiple surgeries within 1 to 2 weeks after injury were more likely to lead to HO formation and elbow contracture (31). Modi et al. reported similar findings in the elbow dislocation treatment. They noticed that multiple reduction attempts increased risks of subsequent elbow arthrolysis (32). Wiggers et al. found that multiple surgeries within the first 4 weeks after elbow trauma were a prominent risk factor for HO formation in elbow motion limitation (33). Zheng et al. claimed that they did not find any differences in additional surgeries among mild, moderate and severe elbow stiffness, which might be due to a small sample size (34). Nevertheless, a previous research claimed that patients experienced capsule adhesion and elbow contracture after multiple surgeries, possibly due to local inflammation and elbow joint fibrosis (35).
The age and alcohol abuse were both associated with increased severity of elbow stiffness in patients who received conservative therapies. Alcohol abuse was also identified as a potential risk factor in severe elbow stiffness among conservative therapy groups. Alcohol abuse might increase severity of elbow stiffness in conservatively treated patients (OR = 3.082; p = 0.025). Alcohol-addicted patients bore a 3.082-fold higher risk of developing severe elbow stiffness than non-abuse patients. Alcohol addiction was harmful to bone development because it represented a major reason for bone loss (36). It also resulted in osteoarthritis after trauma and joint structure deformation which potentially worsened elbow stiffness (37).
As to the other risk factors, each additional age put a 1.047-fold higher risk on patients receiving conservative therapies. This was contradictory to the results in multiple logistic regression analysis for the onset of elbow stiffness. For elderly patients, they had a higher likeliness for developing multiple systemic complications that affected immune and hematopoietic systems. Immune diseases and compromised nutritional status might partially increase the severity of elbow stiffness because of the potential effects on elbow structure destruction (38).
The sex, BMI, smoking, and dominant hands did not show any relevance with occurrence or severity of elbow stiffness. Various fracture sites may have different effects on elbow stiffness. In this study, fracture sites showed no relationship with occurrence or progression of this issue. Numbness of upper extremity displayed no differences in any group possibly due to nerve compression beyond elbow contracture in both flexion and extension. Cai et al. reported that the ulnar neuritis was related with elbow flexion instead of extension limitation (39). The nerve symptoms might not be directly correlated with the severity of elbow stiffness. The rehabilitation exercise should improve elbow function recovery. However, many patients developed severe elbow stiffness after violent and incorrect elbow practices (40). The physicians should avoid stressing the healing bones and ligaments over a specific limit and cater to the individualized demand.
There are a few limitations of this study. The main limitation is that this study is based on retrospective evaluation of a database and only a correlation can be identified. In addition, we excluded some patients who had incomplete medical records. The subgroup analysis was exploratory to identify potential confounders in the regression analysis. Thirdly, there is a lack of information on whether the stiffness is induced by structural impingement or capsule fibrosis. The degree of arthrosis as an influencing factor, such as HO occurrence, is also not described. Several other factors that cannot be assessed with this study may be relevant, such as osseous congruency of the elbow, coping strategies, and compliance with physiotherapy treatment. Finally, risk factors such as alcohol, age, immobilization, and multiple surgical procedures are also identified as risk factors without defining the cutoff. We would like to perform prospective randomized controlled trials based on these issues in the future.
Conclusions
The study demonstrates that the increased immobilization time in conservatively treated patients may be risk factors for the occurrence of elbow stiffness. For the severity of elbow stiffness, “multiple surgeries” may increase risks in the surgical treatment between mild/moderate and severe stiffness groups. Alcohol abuse may increase risks for stiffness progression in patients after conservative therapy. The findings are promising for prevention of elbow stiffness.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Shanghai Jiao Tong University affiliated Sixth People's Hospital East Campus. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
CF and YQ conceived the initial idea and study design. YS and HH participated in data extraction and statistical analysis. YQ drafted the manuscript. YQ, SY, and CF revised the manuscript. All authors approved the final manuscript.
Funding
The study was sponsored by the Shanghai Sailing Program (No. 20YF1436000), Projects of National Natural Science Foundation of China (Grant nos. 81830076 and 81672146), Municipal Hospital Newly-developing Cutting-edge Technologies Joint Research Program of Shanghai Shenkang Hospital Development Center (No. SHDC12018130), Special Fund for Research on People's Livelihood (Medical Treatment and Public Health) of Shanghai Pudong Science, Technology and Economic Commission Scientific and Technological Development Fund (No. PKJ2018-Y52), Shanghai Pudong Health Commission Special Program for Clinical Research in the Health Industry (No. PW2018E-01), and the Key Discipline Group of Shanghai Pudong Health Commission (No. Pwzxq2017-03). We appreciate the support from Youth Science and Technology Innovation Studio of Shanghai Jiao Tong University School of Medicine.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Hausman MR, Lang P. Examination of the elbow: current concepts. J Hand Surg Am. (2014) 39:2534–41. doi: 10.1016/j.jhsa.2014.04.028
2. Sardelli M, Tashjian RZ, MacWilliams BA. Functional elbow range of motion for contemporary tasks. J Bone Joint Surg Am. (2011) 93:471–7. doi: 10.2106/JBJS.I.01633
3. Charalambous CP, Morrey BF. Posttraumatic elbow stiffness. J Bone Joint Surg Am. (2012) 94:1428–37. doi: 10.2106/JBJS.K.00711
4. Ciccotti MG, Pollack KM, Ciccotti MC, D'Angelo J, Ahmad CS, Altchek D, et al. Elbow injuries in professional baseball: epidemiological findings from the major league baseball injury surveillance system. Am J Sports Med. (2017) 45:2319–28. doi: 10.1177/0363546517706964
5. Myden C, Hildebrand K. Elbow joint contracture after traumatic injury. J Shoulder Elbow Surg. (2011) 20:39–44. doi: 10.1016/j.jse.2010.07.013
6. Morrey BF. Post-traumatic contracture of the elbow. Operative treatment, including distraction arthroplasty. J Bone Joint Surg Am. (1990) 72:601–18. doi: 10.2106/00004623-199072040-00019
7. Schneeberger AG, Adams R, Morrey BF. Semiconstrained total elbow replacement for the treatment of post-traumatic osteoarthrosis. J Bone Joint Surg Am. (1997) 79:1211–22. doi: 10.2106/00004623-199708000-00014
8. Ring D, Jupiter JB. Operative release of complete ankylosis of the elbow due to heterotopic bone in patients without severe injury of the central nervous system. J Bone Joint Surg Am. (2003) 85-A:849–57. doi: 10.2106/00004623-200305000-00012
9. McKee M, Jupiter J, Toh CL, Wilson L, Colton C, Karras KK. Reconstruction after malunion and nonunion of intra-articular fractures of the distal humerus. Methods and results in 13 adults. J Bone Joint Surg Br. (1994) 76:614–21. doi: 10.1302/0301-620X.76B4.8027152
10. Helfet DL, Kloen P, Anand N, Rosen HS. Open reduction and internal fixation of delayed unions and nonunions of fractures of the distal part of the humerus. J Bone Joint Surg Am. (2003) 85–A:33–40. doi: 10.2106/00004623-200301000-00006
11. Doornberg JN, Bosse T, Cohen MS, Jupiter JB, Ring D, Kloen P. Temporary presence of myofibroblasts in human elbow capsule after trauma. J Bone Joint Surg Am. (2014) 96:e36. doi: 10.2106/JBJS.M.00388
12. Lindenhovius AL, Doornberg JN, Brouwer KM, Jupiter JB, Mudgal CS, Ring D. A prospective randomized controlled trial of dynamic versus static progressive elbow splinting for posttraumatic elbow stiffness. J Bone Joint Surg Am. (2012) 94:694–700. doi: 10.2106/JBJS.J.01761
13. Yu S, Chen M, Fan C. Team approach: elbow contracture due to heterotopic ossification. JBJS Rev. (2017) 5:01874474-201701000-00004. doi: 10.2106/JBJS.RVW.16.00008
14. Edwards SG, Rhodes DA, Jordan TW, Sietsema DL. The olecranon osteotomy-facilitated elbow release (OFER). J Bone Joint Surg Am. (2017) 99:1859–65. doi: 10.2106/JBJS.16.00715
15. Dunham CL, Castile RM, Chamberlain AM, Lake SP. The role of periarticular soft tissues in persistent motion loss in a rat model of posttraumatic elbow contracture. J Bone Joint Surg Am. (2019) 101:e17. doi: 10.2106/JBJS.18.00246
16. Lindenhovius AL, Doornberg JN, Ring D, Jupiter JB. Health status after open elbow contracture release. J Bone Joint Surg Am. (2010) 92:2187–95. doi: 10.2106/JBJS.H.01594
17. Hildebrand KA. Posttraumatic elbow joint contractures: defining pathologic capsular mechanisms and potential future treatment paradigms. J Hand Surg Am. (2013) 38:2227–33. doi: 10.1016/j.jhsa.2013.07.031
18. Everding NG, Maschke SD, Hoyen HA, Evans PJ. Prevention and treatment of elbow stiffness: a 5-year update. J Hand Surg Am. (2013) 38:2496–507. doi: 10.1016/j.jhsa.2013.06.007
19. Foruria AM, Augustin S, Morrey BF, Sánchez-Sotelo J. Heterotopic ossification after surgery for fractures and fracture-dislocations involving the proximal aspect of the radius or ulna. J Bone Joint Surg Am. (2013) 95:e66. doi: 10.2106/JBJS.K.01533
20. Foruria AM, Lawrence TM, Augustin S, Morrey BF, Sanchez-Sotelo J. Heterotopic ossification after surgery for distal humeral fractures. Bone Joint J. (2014) 96-B:1681–7. doi: 10.1302/0301-620X.96B12.34091
21. Zong XN, Li H. Construction of a new growth references for China based on urban Chinese children: comparison with the WHO growth standards. PLoS ONE. (2013) 8:59569. doi: 10.1371/journal.pone.0059569
22. Agarwal S, Loder S, Brownley C, Cholok D, Mangiavini L, Li J, et al. Inhibition of Hif1α prevents both trauma-induced and genetic heterotopic ossification. Proc Natl Acad Sci USA. (2016) 113:E338–47. doi: 10.1073/pnas.1515397113
23. Carlock KD, Bianco IR, Kugelman DN, Konda SR, Egol KA. Risk factors for elbow joint contracture after surgical repair of traumatic elbow fracture. J Am Acad Orthop Surg. (2020). doi: 10.5435/JAAOS-D-18-00801. [Epub ahead of print].
24. Fusaro I, Orsini S, Stignani Kantar S, Sforza T, Benedetti MG, Bettelli G, et al. Elbow rehabilitation in traumatic pathology. Musculoskelet Surg. (2014) 98(Suppl. 1):95–102. doi: 10.1007/s12306-014-0328-x
25. Taylor F, Sims M, Theis JC, Herbison GP. Interventions for treating acute elbow dislocations in adults. Cochrane Database Syst Rev. (2012) 4:CD007908. doi: 10.1002/14651858.CD007908.pub2
26. Edelman D, Ilyas AM. Temporary bridge plate stabilization of unstable elbow fractures and dislocations. Tech Hand Up Extrem Surg. (2018) 22:46–50. doi: 10.1097/BTH.0000000000000191
27. Monument MJ, Hart DA, Salo PT, Befus AD, Hildebrand KA. Posttraumatic elbow contractures: targeting neuroinflammatory fibrogenic mechanisms. J Orthop Sci. (2013) 18:869–77. doi: 10.1007/s00776-013-0447-5
28. Howell JN, Chleboun G, Conatser R. Muscle stiffness, strength loss, swelling and soreness following exercise-induced injury in humans. J Physiol. (1993) 464:183–96. doi: 10.1113/jphysiol.1993.sp019629
29. Lee Y, Ashton-Miller JA. Effects of age, gender and level of co-contraction on elbow and shoulder rotational stiffness and damping in the impulsively end-loaded upper extremity. Ann Biomed Eng. (2015) 43:1112–22. doi: 10.1007/s10439-014-1185-3
30. Kawanishi N, Funakoshi T, Machida S. Time-course study of macrophage infiltration and inflammation in cast immobilization-induced atrophied muscle of mice. Muscle Nerve. (2018) 57:1006–13. doi: 10.1002/mus.26061
31. Jupiter JB, O'Driscoll SW, Cohen MS. The assessment and management of the stiff elbow. Instr Course Lect. (2003) 52:93–111.
32. Modi CS, Wasserstein D, Mayne IP, Henry PD, Mahomed N, Veillette CJ. The frequency and risk factors for subsequent surgery after a simple elbow dislocation. Injury. (2015) 46:1156–60. doi: 10.1016/j.injury.2015.02.009
33. Casavant AM, Hastings H 2nd. Heterotopic ossification about the elbow: a therapist's guide to evaluation and management. J Hand Ther. (2006) 19:255–66. doi: 10.1197/j.jht.2006.02.009
34. Zheng W, Liu J, Song J, Fan C. Risk factors for development of severe post-traumatic elbow stiffness. Int Orthop. (2018) 42:595–600. doi: 10.1007/s00264-017-3657-1
35. Maurel DB, Boisseau N, Benhamou CL, Jaffre C. Alcohol and bone: review of dose effects and mechanisms. Osteoporos Int. (2012) 23:1–16. doi: 10.1007/s00198-011-1787-7
36. Haugen IK, Magnusson K, Turkiewicz A, Englund M. The prevalence, incidence, and progression of hand osteoarthritis in relation to body mass index, smoking, and alcohol consumption. J Rheumatol. (2017) 44:1402–9. doi: 10.3899/jrheum.170026
37. Dyer GS, Blazar PE. Rheumatoid elbow. Hand Clin. (2011) 27:43–48. doi: 10.1016/j.hcl.2010.10.003
38. Cai J, Zhou Y, Chen S, Sun Y, Yuanming O, Ruan H, et al. Ulnar neuritis after open elbow arthrolysis combined with ulnar nerve subcutaneous transposition for post-traumatic elbow stiffness: outcome and risk factors. J Shoulder Elbow Surg. (2016) 25:1027–33. doi: 10.1016/j.jse.2016.01.013
39. Scalzitti DA. Because of the risk of developing heterotopic ossification, are passive range of motion exercises contraindicated following traumatic injuries? Phys Ther. (2003) 83:659–67. doi: 10.1093/ptj/83.7.659
Keywords: elbow stiffness, risk factor, surgery, alcohol, trauma
Citation: Qian Y, Yu S, Shi Y, Huang H and Fan C (2020) Risk Factors for the Occurrence and Progression of Posttraumatic Elbow Stiffness: A Case-Control Study of 688 Cases. Front. Med. 7:604056. doi: 10.3389/fmed.2020.604056
Received: 08 September 2020; Accepted: 06 November 2020;
Published: 16 December 2020.
Edited by:
Tobias Winkler, Charité - University Medicine Berlin, GermanyReviewed by:
Kathi Thiele, Charité – Universitätsmedizin Berlin, GermanyMichel Van Den Bekerom, Vrije Universiteit Amsterdam, Netherlands
Copyright © 2020 Qian, Yu, Shi, Huang and Fan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hengye Huang, huanghy1107@shsmu.edu.cn; Cunyi Fan, cyfan@sjtu.edu.cn
†These authors have contributed equally to this work
 Yun Qian
Yun Qian Shiyang Yu1,2†
Shiyang Yu1,2†  Cunyi Fan
Cunyi Fan