Commentary: Idiopathic Intracranial Hypertension Without Papilledema (IIHWOP) in Chronic Refractory Headache
- 1Unità Operativa Complessa Clinica Neurologica, IRCCS Institute of Neurological Sciences of Bologna, Bologna, Italy
- 2Department of Biomedical and NeuroMotor Sciences, Alma Mater Studiorum–University of Bologna, Bologna, Italy
- 3Neuroradiology Department, IRCCS Institute of Neurological Sciences of Bologna, Bologna, Italy
Background: To determine the prevalence of Idiopathic intracranial hypertension without papilledema (IIHWOP) testing revised diagnostic criteria by Friedman in refractory chronic headache (CH) patients.
Methods: This is a prospective observational study. Each patient underwent ophthalmologic evaluation and Optical Coherence Tomography; brain magnetic resonance venography (MRV) and a lumbar puncture (LP) with opening pressure (OP) measurement. CSF withdrawal was performed in patients with CSF OP > 200 mmH20. IIHWOP was defined according Friedman's diagnostic criteria. Effect of CSF withdrawal was evaluated clinically in a 6-month follow-up and with a MRV study at 1 month.
Results: Forty-five consecutive patients were enrolled. Five were excluded due to protocol violations. Analyses were conducted in 40 patients (32 F, 8 M; mean age 49.4 ± 10.8). None had papilledema. Nine patients (22.5%) had OP greater than 200 mmH2O, two of them above 250 mmH2O. Two (5%) had neuroimaging findings suggestive of elevated intracranial pressure. One of them (2.5%) met the newly proposed diagnostic criteria by Friedman for IIHWOP. After CSF withdrawal seven (77.8%) of the nine patients improved. No changes in neuroimaging findings were found.
Conclusions: We found a low prevalence (2.5%) of IIHWOP in refractory CH patients according to current diagnostic criteria. In agreement with Friedman's criteria, our results confirm that a diagnosis of IIHWOP should be based on CSF OP and the combination of neuroradiological findings. However, where to set the CSF OP upper limit in IIHWOP needs further field testing. Although IIHWOP is a rare clinical condition, it should be considered and treated in refractory CH patients.
Introduction
Chronic headache (CH) is a challenging clinical entity because management is complex and often unsatisfactory. A diagnosis of idiopathic intracranial hypertension without papilledema (IIHWOP) should be considered in patients with CH refractory to preventive therapy. Headache attributed to IIHWOP often mimics chronic migraine or chronic tension-type headache and the distinction from primary headaches can be clinically difficult. Lumbar puncture (LP) is mandatory to confirm diagnosis, but controversies exist regarding the CSF opening pressure (OP) cut-off value for the diagnosis of intracranial hypertension. The early accepted upper limit of normal CSF pressure was 200 mmH2O (1). Based on a long history of evidence (2, 3), recently, revised diagnostic criteria for pseudotumor cerebri syndrome by Friedman set the upper limit to 250 mmH2O and recognized the importance of MRI (4). According to these criteria, in the absence of papilledema or sixth nerve palsy, the diagnosis of IIHWOP can be suggested by the combination of elevated OP and the presence of at least three of the following neuroimaging findings: empty sella, distention of the perioptic subarachnoid space with or without a tortuous optic nerve, flattening of the posterior sclerae and transverse venous sinus stenosis (Table 1). Undoubtedly, the diagnosis of IIHWOP is mandatory to improve patient management. The aim of this study was to verify the prevalence of IIHWOP in chronic headache patients resistant to prophylactic therapies and to test revised diagnostic criteria by Friedman.
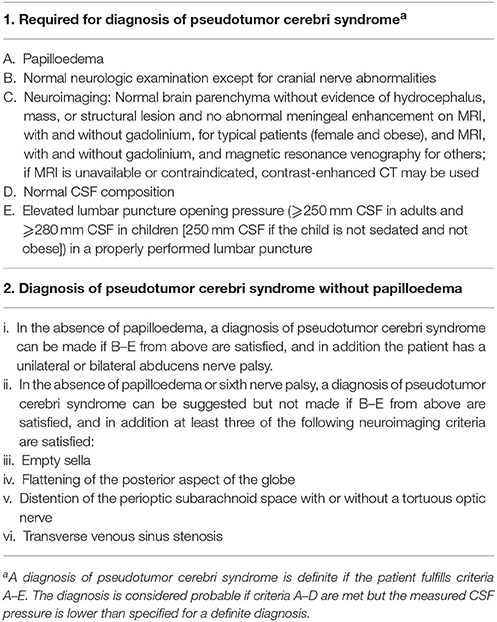
Table 1. Diagnostic criteria for pseudotumor cerebri syndrome (4).
Materials and Methods
Outcome Measures
The primary endpoint of the study was to analyze the prevalence of IIHWOP in a series of consecutive refractory chronic headache patients.
The secondary endpoints were to test the revised diagnostic criteria by Friedman to detect IIHWOP and to verify the effect of CSF withdrawal on headache frequency and intensity.
Standard Protocol Approvals and Patient Consents
The study was conducted in agreement with principles of good clinical practice and the study protocol was approved by the Local Ethics Committee of the local health service of Bologna, Italy (n. 12017/CE). All patients gave their written informed consent to study participation.
Participants
Patients with refractory chronic migraine (CM) and Chronic Tension-type Headache (CTTH) with or without medication overuse referred to the tertiary Headache Centre of IRCCS Institute of Neurological Sciences of Bologna, Italy, were consecutively recruited from September 2013 to February 2016. Diagnosis of CM, CTTH and medication overuse were established according to the International Classification of Headache Disorders-3 beta version criteria (5). Refractoriness was defined as the failure of at least 3 trials of preventive therapies at adequate doses and at least one detoxification attempt in case of medication overuse. Inadequate response was defined as absence of reduction of migraine attack frequency or days by at least 50% after at least 3 months of therapy at a stable dose considered appropriate for migraine or tension type prevention according to accepted guidelines (6, 7). Exclusion criteria included the presence of papilledema on a routine fundoscopic examination, age <18 years, pregnancy and breast-feeding, secondary headaches, as well as serious ongoing physical or psychiatric illness.
Study Protocol
Each participant underwent: (1) a complete neurological and physical examination including height and weight measurements; (2) ophthalmologic evaluation with funduscopic examination and Optical Coherence Tomography (OCT) to rule out the presence of papilledema; (3) brain magnetic resonance imaging (MRI) including magnetic resonance venography (MRV) to detect neuroimaging features highly suggestive of idiopathic intracranial hypertension including transverse sinus stenosis, empty sella, flattening of the posterior aspect of the globe and distension of the perioptic subarachnoid space with or without a tortuous optic nerve; (4) an LP to measure CSF OP, which is the gold standard for the diagnosis of idiopathic intracranial hypertension. Prior to diagnostic procedures, we performed face-to-face structured interviews to gather detailed information about the clinical features of headache and associated symptoms including age at onset, days of headache per month, side and intensity of pain, years of chronic headache; presence, duration, and type of medication overuse; and potential related comordidities such as sleep apnea were ruled out. Headache diary data referring to 30 days before LP were collected as baseline evaluation.
Optical Coherence Tomography (OCT)
Subjects underwent average and single sector (temporal, superior, nasal and inferior) RNFL thickness measurements by OCT (StratusOCT, software version 4.0.1; Carl Zeiss Meditec Inc, Dublin, CA, USA). We used the RNFL thickness 3.4 acquisition protocol, as previously described (8). Patients were compared with age- and sex-matched controls. For both groups we used a randomly selected eye for statistical analysis.
MR Imaging and MR Venography
Each patient underwent an MRI morphological study of the brain, carried out with a 3T MR system (Signa 3T GE) with a standard head coil. All the examinations included T1 and T2 weighted sequences and MRV studies. MRV studies were executed with 2D time-of-flight sequence acquired in the coronal plane and with a 3D contrast-enhanced ultrafast gradient-echo angiographic sequence with elliptic centric ordering of k-space collection (Time Resolved Imaging of Contrast Kinetics-TRICKS). The sequence was acquired in the sagittal plane with covering the whole head. Venous phase correct time delay was calculated administering a small 2 ml test bolus of gadolinium chelates followed by 10 ml bolus of normal saline. The angiographic sequence was then acquired after the injection of a 30 ml bolus of gadolinium chelate contrast agent at a rate of 2 ml/s followed by 30 ml saline flush at 2 ml/s.
Image Processing and Review
Source images from contrast-enhanced MRV (CE-MRV) of each patient were reviewed on a PACS viewing workstation by two neuroradiologists (F.T. and L.C.) who were blinded to the patient's clinical features. In addition to the sagittal source images it was also possible to review reformatted images of the volume using 1–2 mm thick section in the coronal and axial plane and 3D maximum intensity projection (MIP) reconstructions. Transverse sinus stenosis, empty sella, flattening of the posterior aspect of the globe and distension of the perioptic subarachnoid space with or without a tortuous optic nerve were defined as present or absent. The presence of at least three of four neuroimaging findings were needed to satisfied Friedman's criteria (4). Disagreements were resolved by consensus.
Lumbar Puncture
All LPs were performed as previously described, using a 20 gauge spinal needle and with the patient lying in the lateral decubitus position (9). CSF OP was measured by a standard spinal manometer calibrated in mmHg connected to the spinal needle via a three-way stopcock. All pressure values were multiplied by 13.56 (the Hg specific weight) for the conversion in mm H2O. We used the OP value of 250 mmH2O to define IIHWOP according to Friedman's criteria (4). According to previous findings that suggest that CSF withdrawal may result in a sustained remission of chronic migraine, we performed CSF withdrawal in patients with OP values above 200 mmH2O: intracranial pressure measurements were repeated every 2 mL of extracted CSF, up to about 100 mmH2O (9). In patients who showed an OP ≤ 200 mm H2O, the procedure was stopped after a 6 mL CSF withdrawal for routine analysis.
Follow-Up
A follow-up visit at 1 month was planned for all patients. Effect of CSF withdrawal was evaluated in patients with an OP > 200 mmH2O at 1, 3 and 6 months after LP. Moreover, the MRI study including MRV was repeated 1 month after CSF withdrawal to evaluate changes in neuroimaging findings. Patients recorded all headache attacks and drugs taken for headache during the whole study period on a clinical diary.
Statistics
All data were analyzed using the SPSS software package (version 21- IBM Analytics). T-test or Mann-Whitney test, as appropriate, was used to compare continuous variables, while Chi-square test was adopted for categorical variables. Results were expressed by mean ± standard deviation, median with interquartile range (IQR) or percentage. The Spearman bivariate test was used to detect the strength of correlation between selected variables. Values of p < 0.05 were considered statistically significant. A Bonferroni correction was applied for multiple comparisons.
Results
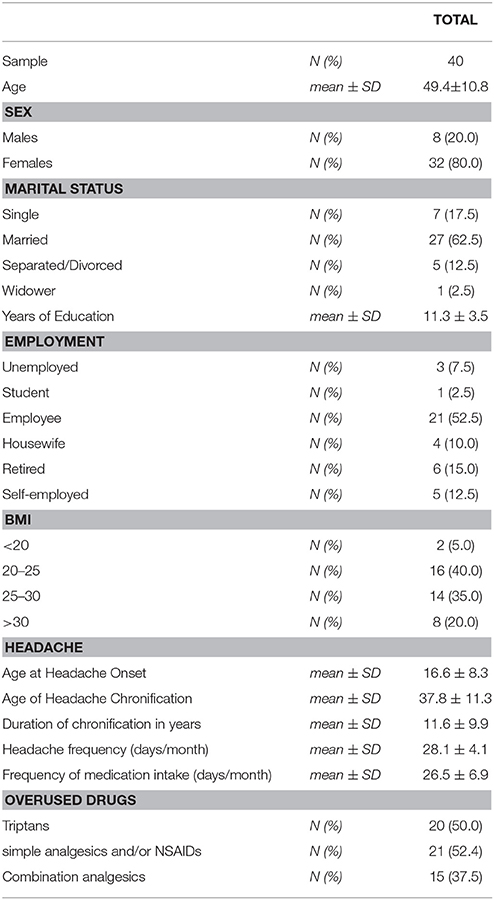
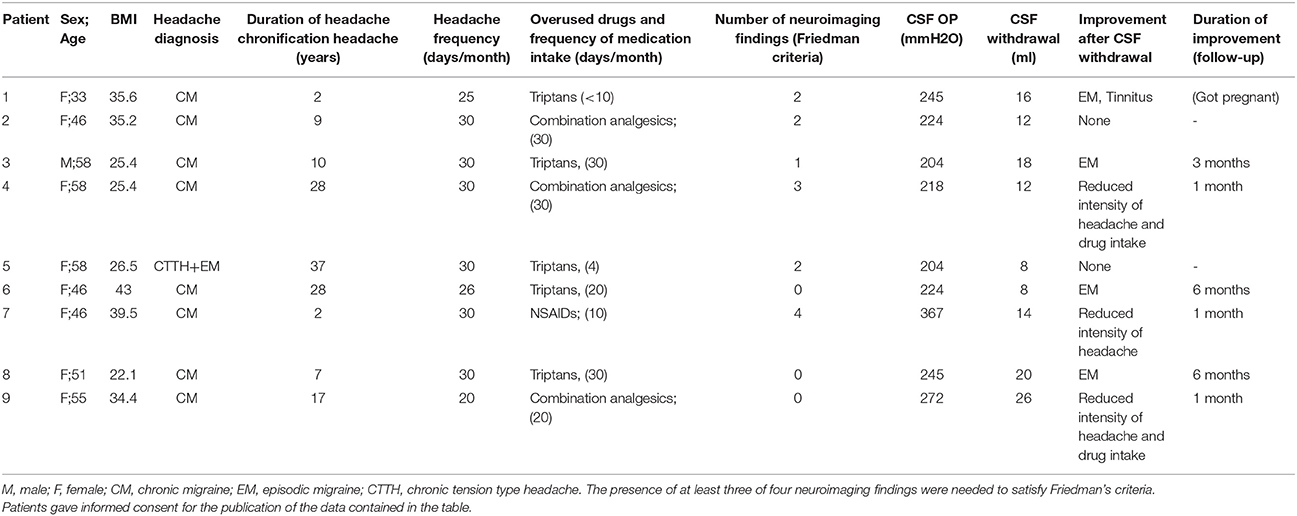
Forty-five patients were enrolled. Five patients were excluded due to protocol violations (one patient withdrew consent, two refused to undergo LP, one refused to undergo brain MRV and one refused to undergo both LP and MRV). Analyses were conducted in 40 patients (32 F, 8 M; mean age 49.4 ± 10.8; mean BMI 26.7 ± 6.4).
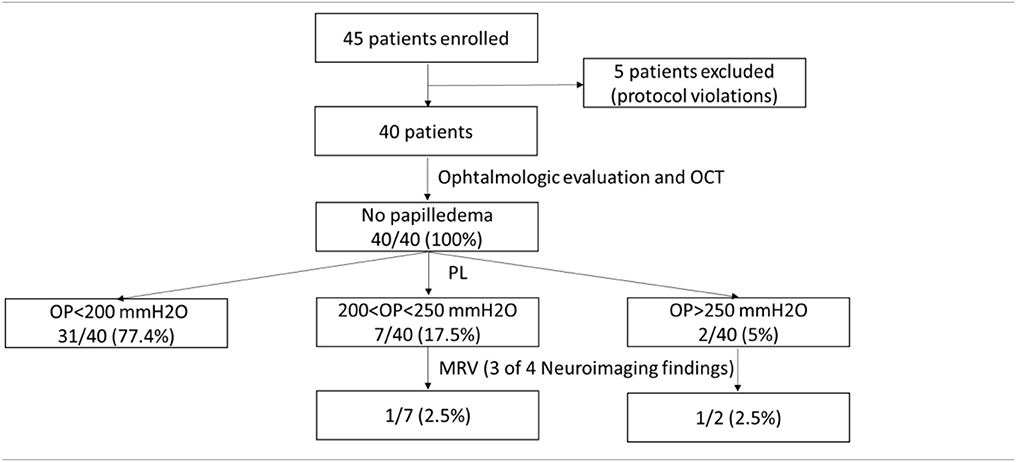
The diagnosis of headache was chronic migraine in 39 patients (97.5%) and chronic tension-type headache with concomitant episodic migraine in 1 patient. Mean chronification duration was 11.6 ± 9.9 years (range 1–32 years). At baseline mean headache frequency was 26.5 ± 6.5 days/month. Overall, 37 patients (92.5%) were medication overusers. The most commonly overused agents were triptans (N = 20; 54%) and non-steroidal anti-inflammatory drugs (n = 14; 37.8%). Fifteen patients (37.5%) overused two or more different compounds at a time (Table 2). Three patients complained of symptoms suggesting IIWHOP, such as tinnitus.
Neurological Examination
Neurological examination was unremarkable in all patients. None of them had unilateral or bilateral abducens nerve palsy.
Ophthalmological Examination and OCT
None of the patients had papilledema. All the patients underwent OCT. Four patients were excluded due to poor quality of OCT scan images. Thirty-six patients (29 F, 7 M; mean age 49.3 ± 10.8 years; range 22–67 years) were compared to 43 sex- and age-matched controls (32 F, 11 M; mean age 49.6 ± 12.1 years; range 23–68 years). The RNFL average thickness was within normal range in both groups and did not significantly differ between patients and controls (99.1 ± 8.9 μm in migraine patients vs 99.5 ± 13.0 μm in controls, p = 0.8). Moreover, there was no significant difference in the RNFL thickness in any of the optic nerve quadrants analyzed.
LP
Two of forty patients (5%) had an OP above 250 mmH2O. Other seven (17.5%) had an OP between 200 and 250 mmH2O. All patients displayed normal CSF composition. We compared patients with OP < 200 mmH2O (Group 1) with those with OP > 200 mmH2O (Group 2). No statistical significant differences were found between group 1 and 2 regarding age, sex, years of education, duration of chronification (Table 3). Regarding BMI a statistical difference (p = 0.015) was found before Bonferroni correction. Two of the three patients with tinnitus have OP between 200 and 250 mmH2O.
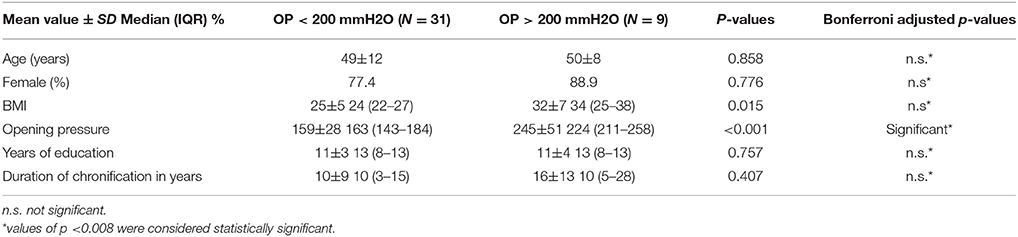
Table 3. Comparisons of features of patients with OP < 200 mmH2O and patients with OP > 200 mmH2O (Group 1 and Group 2).
Neuroimaging Criteria
All patients had normal brain parenchyma. Two of them (5%) had at least three of the four neuroimaging findings suggestive of elevated intracranial pressure as proposed by Friedman's criteria (Table 4). One of them had all the findings (Figure 1). The other had evidence of transverse sinus stenosis, empty sella, and distension of the perioptic subarachnoid space.
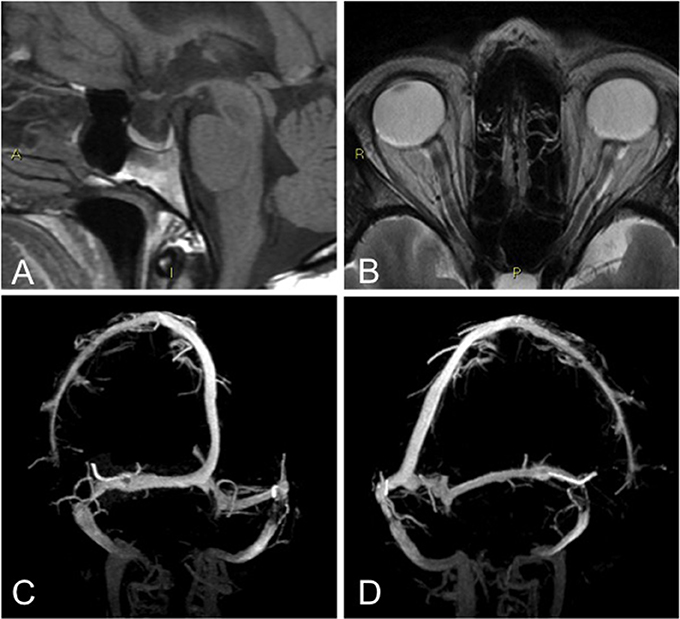
Figure 1. Patient that fulfilled Friedman's criteria: abnormally enlarged sella turcica that appeared partially empty (A), Enlargement of perioptic subarachnoid spaces with faint flattening of the posterior aspect of the globe, on the left side (B), bilateral dural sinus stenosis, at the distal portion of the transverse segment (C,D).
Prevalence of IIHWOP
One patient (2.5%) satisfied the diagnostic criteria for IIHWOP proposed by Friedman (Table 5). She had both OP > 250 mmH2O and all of the four neuroimaging features.
The other patient who had at least three of the four neuroimaging findings had OP > 200 mmH2O, but lower than 250 mmH2O. The other patient with OP > 250 mmH2O had none of neuroimaging criteria.
Follow-Up
At 1 month, considering the whole sample, 15 patients (37.5%) improved after LP, 23 (57.5%) had no benefit and 2 (5%) were lost at follow-up. Out of those that ameliorated, 8 had OP < 200 mmH2O, 5 had OP between 200 and 250 mmH2O, and 2 had OP > 250 mmH2O. Among them, there were no statistically significant differences regarding age (p = 0.694), sex (0.605), BMI (p = 0.072), years of education (p = 0.955) and duration of chronification (p = 0.897), even after Bonferroni correction between the subgroups of patients with OP < 200 mmH20 (n = 8) or those with p> 200 mmH20 (n = 7). Considering the 9 patients with OP >200 mmH2O, seven (77.8%) improved after withdrawal (Table 4). The two patients with OP > 250 mmH2O achieved an improvement of headache intensity and one of them a reduced frequency of medication intake, but no changes in the frequency of attacks. Among the five patients with OP ranging from 200 to 250 mmH2O, four experienced a return to episodic migraine and one decreased headache intensity and acute medications intake; one of them achieved also the recovery of tinnitus. A trial with acetazolamide was taken in account in patients with no contraindications to the use of this drug, and compliant to the treatment. All the 9 patients with OP>200 mmH2O repeated MRV 1 month after CSF withdrawal. No changes of neuroimaging findings were found.
At 3 months one of the two patients with OP > 250 mmH2O relapsed, none of them was treated with acetazolamide due to contraindications, and one was lost at follow-up. Among those with OP between 200 and 250 mmH2O, three patients still presented with an episodic migraine (two of them were treated with acetazolamide) and one patient was lost because she got pregnant. At 6 month of follow-up one relapsed to CM and two patients continued to have an episodic migraine (Table 4).
Discussion
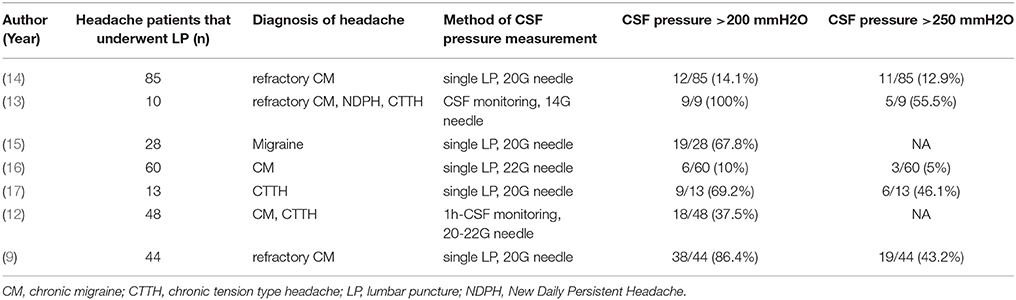
In our series, we found a low prevalence of IIHWOP in refractory CH patients. Only one of forty patients (2.5%) who had OP greater than 250 mmH2O and the neuroimaging finding suggestive of elevated intracranial pressure met the newly proposed diagnostic criteria by Friedman (4). Indeed, according to these criteria, CSF OP alone is not suitable for making a diagnosis and imaging has become an integral part of our diagnostic armamentarium for the diagnosis of IIHWOP. The upper limit of normal intracranial pressure is still debated (4, 10, 11). First of all, increased CSF OP may be due to several factors, including pain, anxiety, sedation, anesthesia, flexing of the neck and Valsalva maneuvers. In order to minimize false positive values a standardized procedure is essential with patients placed in a lateral decubitus position, as relaxed as possible, with legs stretched before pressure measurements. Moreover, CSF pressure monitoring demonstrated that intracranial pressure fluctuates during the day, ranging from normal to pathologic values. This implies that a single-spot opening measurement of CSF OP may fail to identify this condition, if the cut-off value is set at 250 mmH2O (12). However, although CSF pressure monitoring has a high accuracy in recognizing elevated intracranial pressure, it is an invasive procedure that is not practicable in routine use (12, 13). Moreover, the risk to overestimate the syndrome should be taken into account, if the cut-off value is set at 200 mmH2O. Asymptomatic OP greater than 200 mmH2O was found in 11% of neurological patients, probably similar to the general population (10). Previous studies in headache patients reported OP > 250 mmH2O ranging from 5 to 55.5% and OP > 200 mmH2O ranging from 10 to 100% (Table 6) (9, 12–17). These heterogeneous results may be mainly due to different methods and patient selection. Moreover, limited data are available in CH patients, especially those refractory to treatments. In our series, we found OP > 250 mmH2O and OP > 200 mmH2O in 5 and 22.5% respectively. Our results are significantly lower than those recently reported in a series of 44 unresponsive chronic migraine patients, where OP > 250 mmH2O and OP > 200 mmH2O were found in 43.2 and 86.4% respectively (9). In this latter study MRV was used for selecting patients with transverse sinus stenosis, however the difference in outcome cannot be easily explained by different patient selection criteria (18).
To our knowledge, our study is the first one that focused on the combination of neuroradiological findings and OP in refractory CH patients to test IIHWOP criteria. Between the two patients (5%) that satisfied neuroimaging criteria, both have OP higher than 200 mmH2O, but only one higher than 250 mmH2O. On the contrary, considering CSF OP > 250 mmH2O alone, the prevalence of IIHWOP may rise to 5%. However, between the two patients with OP greater than 250 mmH2O, one failed to meet diagnostic criteria due to the absence of neuroimaging findings. Despite the effort to use a standardized procedure, we cannot exclude that the OP found in this patient was a false positive value. Consequently, using CSF OP alone, the risk is to overestimate a diagnosis. These findings confirm the need to combine OP and neuradiological criteria to make the diagnosis.
Moreover, we confirm that neuroimaging features persist after CSF withdrawal (19). This is in contrast with recent evidence showing the reversibility of stenosis after intracranial pressure normalization (20, 21). The difference in outcome can be related to different timing of MRV after withdrawal and to the hypothesis that transverse sinus stenosis is only one of the contributing factors involved in IIHWOP (19).
Our results confirm that CSF withdrawal may have clinical effects on headache in CH patients, with long-term effect (9, 12, 16, 22). A proportion of 77.8% of our refractory patients with OP > 200 mmH2O reported improvement of headache frequency and/or intensity until up to 6 months after withdrawal. Only partial improvement was reported by patients with OP > 250 mmH2O, but the number is too small to make certain assumptions. Moreover, a placebo effect could not be excluded, considering that 25.8% of patients with OP < 200 mmH2O improved after LP. However, we are pretty certain that clinical features did not differ between patients with OP>200 mmH2O and patients with OP < 200 mmH2O. Interestingly, it appears that there was a trend toward statistical significance with the OP and BMI. Patients with higher BMI are trending toward higher OP. Based on a previous meta-analysis of observational studies that suggests an association between migraine and obesity (23), we suppose that refractory headache may be related with BMI and OP. Moreover, we can argue that patients with OP > 200 mmH2O may potentially be a subgroup of those with “pre IIH” as post CSF removal, 7 out of the 9 had improvement of symptoms.
In addition, we suggest that funduscopic evaluation is sufficient and mandatory to exclude papilledema in refractory CH patients, considering that none of our patients with negative funduscopic exam had OCT sign of papilledema. As a corollary, in contrast to a previous report in chronic migraine patients, all our refractory patients had RNFL thickness within normal range, supporting the hypothesis that long duration of headache does not affect the eye (24).
The study was limited by the relatively small sample size to compare patients with OP > 250 mmH2O with those with OP > 200 mmH2O and to evaluate the effect of CSF withdrawal. However, for feasibility reasons we did not recruit further patients. Moreover the effect of CSF withdrawal should be investigated by mean of a randomized control study. We think that a future multicenter study with a larger number of refractory CH patients is necessary in order to reach meaningful results and better define the characteristics of patients with OP > 250 mmH2O.
Conclusion
IIHWOP is a rare clinical condition that should be considered in patients with chronic headache refractory to medical treatment. Our results confirm that the combination of neuroradiological findings (transverse sinus stenosis, empty sella, flattening of the posterior aspect of the globe and distention of the perioptic subarachnoid space) support the presence of increased intracranial pressure. Determination of CSF opening pressure remains mandatory when brain RM finding suggest pseudotumor cerebri and may result in headache improvement. We agree with Friedman's diagnostic criteria that a diagnosis of IIHWOP should be based on the CSF OP and the combination of neuroradiological findings.
However, based on our results, where to set the CSF OP upper limit in IIHWOP, which may be a milder form of pseudotumor cerebri, remains an open question. We suggest that diagnostic criteria should be tested in other studies in different centers in order to validate or revise it.
Author Contributions
VF, FT, LC, CLM, and SC: conceived and designed of the study; VF: supervised the study; VF, GP, FT, LC, CLM, MM, RA, and SC: acquired and interpreted the data; CLM and SA-R: performed the statistical analysis; VF, FT, and SC: drafted the manuscript; GP and PC: substantially contributed to conception and design of the study and critically revised the manuscript. All authors contributed to manuscript revision, read and approved the submitted version.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of Interest Statement
PC has received honoraria for speaking engagements or consulting activities with Allergan Italia, AbbVie srl, Chiesi Farmaceutici, Teva, UCB Pharma S.p.A, Zambon.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Dr. Cecilia Baroncini who provided language assistance.
References
1. Headache Classification Subcommittee of the International Headache Society (IHS). The international classification of headache disorders. Cephalalgia (2004) 24(suppl 1):8–160.
2. Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology(2002) 59:1492–5. doi: 10.1212/01.WNL.0000029570.69134.1B
3. Corbett JJ, Mehta MP. Cerebrospinal fluid pressure in normal obese subjects and patients with pseudotumor cerebri. Neurology (1983) 33:1386–8. doi: 10.1212/WNL.33.10.1386
4. Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology (2013) 81:1159–65. doi: 10.1212/WNL.0b013e3182a55f17
5. Headache Classification Committee of the International Headache Society. The international classification of headache disorders, 3rd edition (beta version). Cephalalgia (2013) 33:629–808. doi: 10.1177/0333102413485658
6. Tfelt-Hansen PC. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards subcommittee of the American Academy of Neurology and the American Headache Society. Neurology (2013) 80:869–70. doi: 10.1212/01.wnl.0000427909.23467.39
7. Martelletti P, Katsarava Z, Lampl C, Magis D, Bendtsen L, Negro A, et al. Refractory chronic migraine: a consensus statement on clinical definition from the European Headache Federation. J Headache Pain (2014) 15:47. doi: 10.1186/1129-2377-15-47
8. Barboni P, Savini G, Valentino ML, Montagna P, Cortelli P, De Negri AM, et al. Retinal nerve fiber layer evaluation by optical coherence tomography in Leber's hereditary optic neuropathy. Ophthalmology (2005) 112:120–6. doi: 10.1016/j.ophtha.2004.06.034
9. De Simone R, Ranieri A, Montella S, Cappabianca P, Quarantelli M, Esposito F, et al. Intracranial pressure in unresponsive chronic migraine. J Neurol. (2014) 261:1365–73. doi: 10.1007/s00415-014-7355-2
10. Bono F, Cristiano D, Mastrandrea C, Latorre V, D'Asero S, Salvino D, et al. The upper limit of normal CSF opening pressure is related to bilateral transverse sinus stenosis in headache sufferers. Cephalalgia (2010) 30:145–51. doi: 10.1111/j.1468-2982.2009.01896.x
11. De Simone R, Ranieri A, Montella S, Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology (2014) 82:1011–12. doi: 10.1212/WNL.0000000000000200
12. Bono F, Salvino D, Tallarico T, Cristiano D, Condino F, Fera F, et al. Abnormal pressure waves in headache sufferers with bilateral transverse sinus stenosis. Cephalalgia (2010) 30:1419–25. doi: 10.1177/0333102410370877
13. Torbey MT, Geocadin RG, Razumovsky AY, Rigamonti D, Williams MA. Utility of CSF pressure monitoring to identify idiopathic intracranial hypertension without papilledema in patients with chronic daily headache. Cephalalgia (2004) 24:495–502. doi: 10.1111/j.1468-2982.2004.00688.x
14. Mathew NT, Ravishankar K, Sanin LC. Coexistence of migraine and idiopathic intracranial hypertension without papilledema. Neurology (1996) 46:1226–30. doi: 10.1212/WNL.46.5.1226
15. Bono F, Messina D, Giliberto C, Cristiano D, Broussard G, Fera F, et al. Bilateral transverse sinus stenosis predicts IIH without papilledema in patients with migraine. Neurology (2006) 67:419–23. doi: 10.1212/01.wnl.0000227892.67354.85
16. Vieira DS, Masruha MR, Gonçalves AL, Zukerman E, Senne Soares CA, Naffah-Mazzacoratti Mda G, et al. Idiopathic intracranial hypertension with and without papilloedema in a consecutive series of patients with chronic migraine. Cephalalgia (2008) 28:609–13. doi: 10.1111/j.1468-2982.2008.01564.x
17. Bono F, Messina D, Giliberto C, Cristiano D, Broussard G, D'Asero S, et al. Bilateral transverse sinus stenosis and idiopathic intracranial hypertension without papilledema in chronic tension-type headache. J Neurol. (2008) 255:807–12. doi: 10.1007/s00415-008-0676-2
18. Fofi L, Giugni E, Vadalà R, Vanacore N, Aurilia C, Egeo G, et al. Cerebral transverse sinus morphology as detected by MR venography in patients with chronic migraine. Headache (2012) 52:1254–61. doi: 10.1111/j.1526-4610.2012.02154.x
19. Bono F, Giliberto C, Mastrandrea C, Cristiano D, Lavano A, Fera F, et al. Transverse sinus stenoses persist after normalization of the CSF pressure in IIH. Neurology (2005) 65:1090–3. doi: 10.1212/01.wnl.0000178889.63571.e5
20. Rohr AC, Riedel C, Fruehauf M-C, van Baalen A, Bartsch T, Hedderich J, et al. MR imaging findings in patients with secondary intracranial hypertension. AJNR Am J Neuroradiol. (2011) 32:1021–9. doi: 10.3174/ajnr.A2463
21. Horev A, Hallevy H, Plakht Y, Shorer Z, Wirguin I, Shelef I. Changes in cerebral venous sinuses diameter after lumbar puncture in idiopathic intracranial hypertension: a prospective MRI study. J Neuroimaging (2013) 23:375–8. doi: 10.1111/j.1552-6569.2012.00732.x
22. Wang SJ, Silberstein SD, Patterson S, Young WB. Idiopathic intracranial hypertension without papilledema: a case-control study in a headache center. Neurology (1998) 51:245–9. doi: 10.1212/WNL.51.1.245
23. Ornello R, Ripa P, Pistoia F, Degan D, Tiseo C, Carolei A, et al. Migraine and body mass index categories: a systematic review and meta-analysis of observational studies. J Headache Pain (2015) 16:27. doi: 10.1186/s10194-015-0510-z
Keywords: chronic headache, refractory headache, idiopathic intracranial hypertension, MRI, lumbar puncture
Citation: Favoni V, Pierangeli G, Toni F, Cirillo L, La Morgia C, Abu-Rumeileh S, Messia M, Agati R, Cortelli P and Cevoli S (2018) Idiopathic Intracranial Hypertension Without Papilledema (IIHWOP) in Chronic Refractory Headache. Front. Neurol. 9:503. doi: 10.3389/fneur.2018.00503
Received: 24 March 2018; Accepted: 08 June 2018;
Published: 26 June 2018.
Edited by:
Vincenzo Guidetti, Sapienza Università di Roma, ItalyReviewed by:
Marcelo M. Valença, Universidade Federal de Pernambuco, BrazilCherubino Di Lorenzo, Fondazione Don Carlo Gnocchi Onlus (IRCCS), Italy
Copyright © 2018 Favoni, Pierangeli, Toni, Cirillo, La Morgia, Abu-Rumeileh, Messia, Agati, Cortelli and Cevoli. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sabina Cevoli, sabina.cevoli@unibo.it
 Valentina Favoni
Valentina Favoni Giulia Pierangeli1,2
Giulia Pierangeli1,2 Samir Abu-Rumeileh
Samir Abu-Rumeileh Pietro Cortelli
Pietro Cortelli Sabina Cevoli
Sabina Cevoli