Robotic-assisted surgery in the pediatric surgeons’ world: Current situation and future prospectives
- Department of Pediatric Surgery, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, Hubei, China
Robotic-assisted surgery has been fully embraced by surgeons for the adult population; however, its acceptance is too slow in the world of pediatric surgeons. It is largely due to the technical limitations and the inherent high cost associated with it. In the past two decades, indeed, there has been considerable advancement in pediatric robotic surgery. A large number of surgical procedures were performed on children with the assistance of robots, even with comparative success rates to standard laparoscopy. As a newly developing field, it still has many challenges and obstacles. This work is centered on the current status and progression of pediatric robotic surgery as well as the future perspectives in the field of pediatric surgery.
Introduction
Laparoscopic procedures have been proven safe and valuable in adult and pediatric populations over the last few years. As previously shown, laparoscopy resulted in decreased hospital stays, smaller surgical scars, and expedited recovery (1). It even replaced open surgeries as the gold standard in some cases. However, its widespread use was impeded in more complex situations, particularly in intracorporeal anastomosis or extensive reconstruction. Laparoscopic procedures was difficult and largely related to the technological limitations with available laparoscopic instruments, 2D visualization, and a steep learning curve (2, 3). Additionally, infant and toddler patients pose a further challenge, for instance, narrow operative working space and quite delicate tissue mobilization in minimally invasive surgery (MIS) (4). With the introduction and application of robotic surgical platforms, a significant move has been made in the history of surgical evolution. Robots provide a magnified 3D view, more dexterity, high precision, and motion scaling, facilitating precise intracorporeal suturing and exposure (5). As a result of these advantages, this technology is adopted gradually for assisting pediatric surgeons in their surgical procedures. Its use has been applied widely, including pediatric urology, gastrointestinal surgery, and gynecology (6, 7). A growing number of reports have investigated its safety and efficiency in the pediatric population, compared with different approaches (open or laparoscopic surgeries). In this review, we are chiefly concerned with the available literature up to date, briefly surveyed the current status of robotic-assisted surgery in pediatrics, and critically analyzed its future development.
Integration and history of robotics in pediatric surgery
da Vinci (Intuitive Surgical, Sunnyvale, CA, USA), the first robotic surgical system, was approved by FDA in 2000. It has been the only robotic surgery platform for a very long time and remains the predominant robotics system used worldwide. Despite preliminary studies showing that the conventional laparoscopic approach resulted in improved cosmesis and more efficiency compared with the open approach (8), the robot, instead, has revolutionized the concept of MIS. Since then, surgeons worldwide have embraced the rise of this new robotic surgery. The robotic platform provides many advancements, solving many tricky problems encountered during standard laparoscopy (9, 10). First, it has stable 3D visualization with 10 times magnification, and the camera is manipulated by the surgeon instead of the assistant. Second, it allows 7 degrees of freedom with uniquely designed endo-wrist instruments. The movements of robotic arms are not inverted, entirely different from traditional laparoscopy. Third, the ability to reduce tremors during movements and motion scaling is the best-known and more significant advantages. Finally, in stark contrast to laparoscopy, the robot offers surgeons better ergonomics to execute MIS procedures. Therefore, robotic surgery is currently a reality in surgical practice and has been widely accepted by the surgical field.
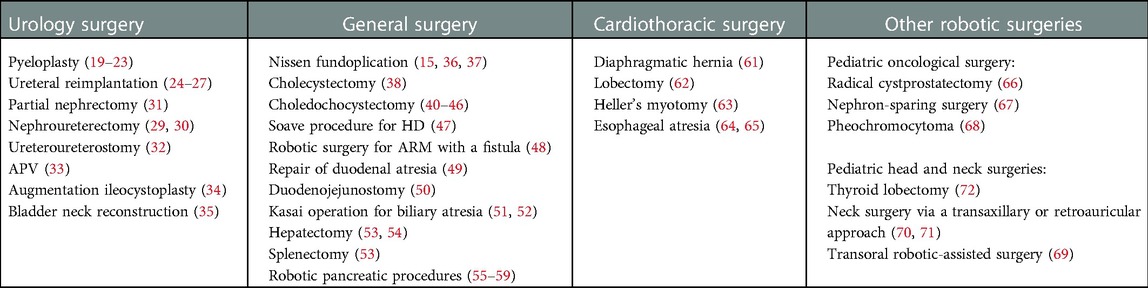
Many literature works reported that robotic surgery resulted in shorter hospital stays and equivalent measurable outcomes in the adult population, compared with conventional open or laparoscopic approaches (11, 12). This approach has become the gold standard in some selected procedures, such as prostatectomy. Just like the other new technology in surgery, pediatric robotic surgery is experiencing slow but steady development but still lagged far behind adult robotic surgery. This limitation is mainly because of the smaller working space of pediatric patients, and currently, no instrument with the appropriate size is available for them (13, 14). Therefore, at the initial attempts, practitioners cautiously selected teenagers to perform common robotic surgeries. In 2001, a case report describing a 10-year-old girl who underwent robotic Nissen fundoplication was the first report on this technology in pediatrics (15). Unlike extirpating in adult surgery, children usually require reconstructive procedures in most cases, which poses a further challenge, specifically in babies and infants. However, pediatric surgeons have always been adventurers and leaders in advancing surgical technology. When performing robotic surgeries, various tricks can be employed to overcome these limitations in pediatric patients (16, 17), such as placing ports to a more linear position with less triangulation, intussuscepting a 5-mm assistant trocar for suture introduction, performing aspiration and traction of the forth arms usually used in adults, and positioning pediatric patients with dedicated cushions and protecting with soft padding to prevent collision against the arms. Therefore, it appears that the robotic platform has enabled MIS in children to become mainstream in many complicated cases, which were previously difficult by laparoscopy, particularly in young children or infants (14). In recent years, pediatric robotic surgery has seen broader implementation and prevalence (see Table 1).
Distinctive robotic surgeries for pediatric patients
Robotic urologic surgery in pediatric patients
The initial reported robotic urologic surgery in adults began with prostatectomy (18) and was subsequently followed by pediatric robot-assisted laparoscopic pyeloplasty (RALP), first accomplished in 2002 (19). Until 2015, about 40% of pyeloplasty surgeries on children were performed by robots in the United States (7). Several meta-analyses and systematic reviews of surgical outcomes after RALP have been reported. These data indicated that RALP achieved a shorter operative time (excluding docking time), decreased hospitalization, and a similar success rate to either open or laparoscopic procedures (20–23). Robotic ureteral reimplantation (RUR) is the second most common pediatric procedure with this technology, treated for vesicoureteral reflux (VUR), with a reported resolution rate of 77%–100% (24). Although it has been shown that there is a feasible selection for the laparoscopic technique through an extravesical or intravesical approach, RUR was largely performed by the extravesical (Lich-Gregoir) approach. There are some technical difficulties, such as trocar placement, pneumovesicum stability, and instrument navigation in small-capacity bladders, making intravesical RUR extremely challenging (25). Boysen and colleagues reviewed 260 patients from 9 centers who underwent extravesical RUR. The radiographic reflux resolution rate was 87.9%, with a total of 363 ureters, and the complication rate was low at 9.6%, in agreement with published data on open surgeries (26). Conversely, a 2016 study by Kurtz and colleagues compared 108 robotic vs. 1,494 open UR in 17 centers and demonstrated a higher complication rate in the robotic group (13.0% vs. 4.5%) (27). This difference might be related to case selection and the early learning curve of the operator (28). This approach is feasible for complete and partial nephrectomy or nephroureterectomy and has been reported by some study groups (29–31). However, it does not have any reconstructive phase, and we have a suspicion that the robot indeed offers a real advantage. Further multi-institutional and large-cohort studies are needed to assess which specific patients can benefit from robotic surgery.
Possibly because of the less steep learning curve of robotic surgery, it has subsequently been reported for more complicated reconstructive procedures in pediatric urology, including ureteroureterostomy, Mitrofanoff appendicovesicostomy (APV), bladder augmentation, bladder neck reconstruction, and augmentation ileocystoplasty (AI), among many others. Lee and colleagues retrospectively compared robotic to open ureteroureterostomy and concluded that there was a slightly shorter hospital stay in the robotic group, with no signification of operative times and complications (32). APV was traditionally carried out via open surgery, creating a continent tunnel in neurogenic bladder cases. Pedraza and colleagues described their successful experience of the first robotic APV in a 7-year-old boy with congenital posterior urethral valves (33). A small retrospective review, composing 17 robotic RAI and 13 open AI procedures, demonstrated that narcotic analgesia use, complication rate, and change in the bladder volume were similar between the two groups, while the median LOS was shorter in the RAI group (34). A more recent report by Adamic et al. included 24 patients who underwent RAI, of which 20 patients were successfully performed using da Vinci. A series of concomitant procedures were performed, including 16 APV, 8 antegrade continence enema (ACE), and 6 bladder neck reconstruction procedures (35). These results showed that the robot offers not only the intrinsic advantages of MIS but also comparable functional outcomes to open or laparoscopic procedures. It is reliable and effective for more complex procedures in children; however, we have to weigh the benefits of this technology against longer operation times and higher costs.
Robotic general surgery in pediatric patients
Robotic general surgery in pediatric patients has been widely reported despite not reaching the magnitude of pediatric urology. Meininger and colleagues reported their robotic-assisted laparoscopic treatment of Nissen fundoplication in a girl, which was carried out in July 2000 and reported in April 2001; it was the first such case to be reported in a child (15). Since then, fundoplication has become one of the most widely performed robotic general surgeries in pediatrics (36). The published literature confirmed that it achieved similar results to conventional laparoscopic Nissen fundoplication in children (37). Although there are no obvious advantages compared with traditional laparoscopy, in this process, the operator can experience robotic surgical skills, and it is the best choice for pediatric surgeons who are performing robotic surgery for the first time. Cholecystectomies were carried out robotically in some institutes, but this robotic application has been questioned. Opponents believe that children cannot benefit more in this routine operation; on the contrary, it is associated with longer operating times and high costs (38). Single-site robotic cholecystectomy may have great appeal for the pediatric population and provide a potential cosmetic benefit through a novel robotic platform (39).
Excision of choledochal cysts in pediatric patients has been reported by several small cohorts undergoing robotic-assisted surgery (40–42) since first described in 2006 by Woo and colleagues (43). Because of its complexity during total cyst excision with Roux-en-Y reconstruction, open procedures are still relatively prevalent in many centers. A systematic review of robotic choledochocystectomy for children was performed by Wang and colleagues, including eight studies with an average age of 6.3 (0.3–15.9) years. Seventy-nine of 86 cases (91.9%) were successful, and seven patients (8.1%) experienced conversion. Ten patients (11.6%) had complications, including biliary leakage (8), wound disruption (1), and anastomotic stenosis (1, 44). They also investigated the proportion of methods used for intestinal anastomosis, with 54.6% of patients undergoing pull-through intestinal anastomosis and the remaining patients undergoing a complete robotic method. Both methods were feasible, mainly depending on the surgeon's preference. A recent study reported by Koga et al. revealed that total hepaticojejunostomy anastomotic time was significantly shorter and sutures were easier and more precise to handle with robotic equipment compared with conventional laparoscopic surgery (45). In addition, a better and magnified vision of the surgical field provides surgeons with clarity of the hepatic duct anatomy and far easier cyst excision and reconstruction of the biliary tree. Tang and his colleagues also retrospectively evaluated the outcomes in young infants (≤1 year) and control group (>1 years) and concluded that age did not hinder the successful implementation of this robotic surgery (46). These data indicate that robotic hepaticojejunostomy is practical and safe in children and can be considered an emerging approach.
There are relatively few reports on the application of robots in treating Hirschsprung's disease (HD) in children. The latest study was published in 2022, in which Quynh and colleagues analyzed 55 pediatric patients who underwent a robotic-assisted Soave procedure. They speculated that the shorter operative time might be related to experience and teamwork skills with procedural modifications (47). As a result of the advantages provided by robots, they might be helpful in a narrow space, especially in the small pelvic cavity of infants. Some case reports and series documented successful robotic surgery for anorectal malformations (ARMs) with a rectovesical or rectourethral fistula (48). A large cohort of 17 infants with ARMs attained favorable continence and defecation functions after robot-assisted anorectal pull-through (RAARP), which was suspected with minimal damage to perirectal nerves and external sphincters provided by the robotic system. There are also a few reports on robotic surgery for other neonatal diseases, such as the repair of duodenal atresia (49), duodenojejunostomy for SMA syndrome (50), and Kasai operation for biliary atresia. The first five robotic Kasai portoenterostomies were successfully completed (two by Dutta et al. (51) and three by Meehan et al. (52)) without perioperative complications, while the average time was quite longer than previous reports on open modality. The feasibility of robotic Kasai is still a subject of debate, and the long-term efficacy needs further verification (51, 52). Hepatectomy and splenectomy have been carried out robotically in children and have also been relatively prevalent in the literature (53). Rela and colleagues presented the first-ever report of robotic monosegment donor hepatectomy for liver transplantation in a 14-month-old girl with extrahepatic biliary atresia, highlighting the fact that it exhibited the maximum precision (54). Additionally, robotic surgery was increasingly being practiced in the treatment of pediatric pancreatic conditions, such as robotic spleen-preserving distal pancreatectomy (55) or robotic pancreatic enucleation (56) for the treatment of insulinoma, robotic lateral pancreaticojejunostomy for pancreatic duct stones (57), and robotic pancreatoduodenectomy (58) or partial pancreatectomy (59) for pancreatic tumors.
Robotic cardiothoracic surgery in pediatric patients
Because of the smaller working space, pediatric cardiothoracic surgery is limited in the current literature. The most frequent robotic cardiothoracic procedures performed in pediatric patients are diaphragmatic hernia repair, lobectomy, bronchogenic cyst or mediastinal cyst excision, Heller's cardiomyotomy for achalasia, oesophagoplasty, and oesophageal atresia repair (60). Robotic repair of diaphragmatic hernia was successfully carried out in infants or even neonates using da Vinci (61). Durand et al. reported a series of lobectomies in children for treating severe bronchiectasis, comprising 7 robotic resections and 11 thoracoscopies (62). Altokhais et al. described robot-assisted Heller's myotomy in six patients for esophageal achalasia, ranging between 2 and 12 years, which might be a suitable alternative to MIS (63). Two cases of congenital esophageal atresia were successfully repaired using the da Vinci robotic system (64). A late study reported by Ferrero et al. revealed that esophageal robotic-assisted thoracoscopic surgery was performed for 18 patients, comprising 7 esophageal duplications, 4 esophageal atresias, 2 esophagoplasties, and 5 cases of Heller's myotomies. Two neonates (11%) needed a conversion due to exposure difficulties (65). It should be pointed out that the treatment of cardiothoracic diseases by the robot objectively exists the contradiction of large instruments and small thorax, the larger scar of skin puncture than that of a thoracoscope, and the significantly high cost (65). Robot cardiothoracic surgery in pediatric patients is still challenging; the indications should be strictly controlled, and only some selected patients are appropriate.
Other robotic surgeries in pediatric patients
The application of robotics in pediatric oncological surgery was reported in some individual cases. Andenberg et al. reported the case of a 22-month baby with embryonal rhabdomyosarcoma of the bladder, who underwent the first robotic radical cystoprostatectomy (66). With excellent exposure for an oncological resection, Cost et al. presented a pediatric case of renal cell carcinoma, who received robotic nephron-sparing surgery combined with extensive lymphadenectomy (67). The robot could also permit concurrent partial resection of adrenal pheochromocytoma and total resection of extra-adrenal pheochromocytoma in a child with von Hippel–Lindau disease (VHL) (68). Indeed, as a minimally invasive approach, the robot in pediatric oncology surgeries has advantages, such as reduced narcotic analgesia usage, quick postoperative recovery, and low wound infection rate. The biology, treatment, and prognosis of tumors in children differ from those in adults. There is considerable disagreement over the suitability of the robotic approach extrapolated to the pediatric population from the adult literature data on robotic tumor surgery. Currently, robot usage for treating tumors in children is still low, but it is feasible and effective in carefully selected cases, and the application must comply with the oncological surgical principles.
More recently, robotic remote access has been adopted for head and neck surgeries via transaxillary, retroauricular, or transoral approaches, while it is slow in the pediatric population (69–72). In 2005, two teenage patients were first treated with a robotic transaxillary approach. One patient was scheduled for a right thyroid lobectomy, and the other was placed on a vagal nerve stimulator for treating intractable seizures (72). Wu and colleagues retrospectively reviewed pediatric patients (except one 20-year-old) who underwent robot-assisted neck surgery via a transaxillary or retroauricular approach and concluded that it was a feasible option for neck operations in the selected pediatric group in the hands of a vast majority of surgeons (70, 71). Erkul and colleagues reviewed the published literature on pediatric transoral robotic-assisted surgery and concluded that 90.2% of 41 patients could be completely treated robotically, and there was only 1 intraoperative complication (69). Robotic surgery is in the initial stage in the pediatric head and neck area, with limited experience. With increasing usage in head and neck surgery, the results will be encouraging in the future for pediatric robotic surgery.
Limitations and future directions of robotic surgery
The main drawbacks remain the inherent high cost and technical limitations associated robotic surgery. The financial implications are associated with fixed costs (its relatively expensive prices and later maintenance cost) and variable costs of disposable usage. Compared to the large number of adult robotic operations, the number of pediatric operations is still very low, determining the high cost for the individual case. The only available da Vinci system has a stranglehold in the market with higher costs (73). Rowe and colleagues found that robotic surgery had an 11.9% reduction in direct expenses, mostly due to shorter hospitalization (74). They speculated that increased surgical volume and potential competitive market might ideally drive down indirect prices and even overall robotic surgery costs. In addition to the cost, there are other problems with applying da Vinci in the pediatric population, such as the size of robotic instruments (5 or 8 mm), technical limitations, learning curve, and inconvenience. In the past two decades, the robot has been continuously improved and upgraded several times (da Vinci Si, Xi, and SP). Several other distinctive robotic platforms are in various development stages, and even a few are already commercially available, such as Senhance Surgical Robotic System (75), Flex Robotic System (76), SurgiBot (77), and many new upcoming robots (73). The Senhance Surgical Robotic System provides 3-mm-sized instruments, which are particularly suitable for the younger children and neonates (75). However, so far, these new technical refinements have not been extended to pediatric cases. Examination of emerging robotic platforms should focus on the possibility of the future of pediatric robotic surgery specifically.
Conclusion
Although this once seemed far away, pediatric robotic-assisted surgery has become part of the reality of surgeons. As the adoption becomes more widespread, its safety and effectiveness in children have been demonstrated, and the indication is growing steadily across other pediatric surgical subspecialties. However, the benefits of this technique over traditional laparoscopic or open approaches need to be truly assessed through further robust prospective investigations. The costs and technical constraints with the available robotic platform and instruments are the greatest hurdle, deterring its use in the pediatric population specifically. The innovation of robot technology will never stop. Robotic surgery in children will undoubtedly increase with the development of new platforms, miniaturization of instruments, and reduction of inherent costs.
Author contributions
MH and TS contributed to the concept design, reviewed the results, and wrote the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (81773094).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rassweiler JJ, Teber D. Advances in laparoscopic surgery in urology. Nat Rev Urol. (2016) 13(7):387–99. doi: 10.1038/nrurol.2016.70
2. Chen RN, Moore RG, Kavoussi LR. Laparoscopic pyeloplasty. Indications, technique, and long-term outcome. Urol Clin North Am. (1998) 25(2):323–30. doi: 10.1016/s0094-0143(05)70021-5
3. Bauer JJ, Bishoff JT, Moore RG, Chen RN, Iverson AJ, Kavoussi LR. Laparoscopic versus open pyeloplasty: assessment of objective and subjective outcome. J Urol. (1999) 162(3 Pt 1):692–5. doi: 10.1097/00005392-199909010-00016
4. Jaffray B. Minimally invasive surgery. Arch Dis Child. (2005) 90(5):537–42. doi: 10.1136/adc.2004.062760
5. Mizuno K, Kojima Y, Nishio H, Hoshi S, Sato Y, Hayashi Y. Robotic surgery in pediatric urology: current status. Asian J Endosc Surg. (2018) 11(4):308–17. doi: 10.1111/ases.12653
6. Denning NL, Kallis MP, Prince JM. Pediatric robotic surgery. Surg Clin North Am. (2020) 100(2):431–43. doi: 10.1016/j.suc.2019.12.004
7. Varda BK, Wang Y, Chung BI, Lee RS, Kurtz MP, Nelson CP, et al. Has the robot caught up? National trends in utilization, perioperative outcomes, and cost for open, laparoscopic, and robotic pediatric pyeloplasty in the United States from 2003 to 2015. J Pediatr Urol. (2018) 14(4):336 e1–e8. doi: 10.1016/j.jpurol.2017.12.010
8. Klingler HC, Remzi M, Janetschek G, Kratzik C, Marberger MJ. Comparison of open versus laparoscopic pyeloplasty techniques in treatment of uretero-pelvic junction obstruction. Eur Urol. (2003) 44(3):340–5. doi: 10.1016/s0302-2838(03)00297-5
9. Casale P, Kojima Y. Robotic-assisted laparoscopic surgery in pediatric urology: an update. Scand J Surg: SJS. (2009) 98(2):110–9. doi: 10.1177/145749690909800206
10. Fuchs ME, DaJusta DG. Robotics in pediatric urology. Int Braz J Urol. (2020) 46(3):322–7. doi: 10.1590/S1677-5538.IBJU.2020.99.03
11. Dakin GF, Gagner M. Comparison of laparoscopic skills performance between standard instruments and two surgical robotic systems. Surg Endosc. (2003) 17(4):574–9. doi: 10.1007/s00464-002-8938-z
12. Hubens G, Coveliers H, Balliu L, Ruppert M, Vaneerdeweg W. A performance study comparing manual and robotically assisted laparoscopic surgery using the Da Vinci system. Surg Endosc. (2003) 17(10):1595–9. doi: 10.1007/s00464-002-9248-1
13. Gutt CN, Markus B, Kim ZG, Meininger D, Brinkmann L, Heller K. Early experiences of robotic surgery in children. Surg Endosc. (2002) 16(7):1083–6. doi: 10.1007/s00464-001-9151-1
14. Murthy PB, Schadler ED, Orvieto M, Zagaja G, Shalhav AL, Gundeti MS. Setting up a pediatric robotic urology program: a USA institution experience. Int J Urol. (2018) 25(2):86–93. doi: 10.1111/iju.13415
15. Meininger DD, Byhahn C, Heller K, Gutt CN, Westphal K. Totally endoscopic Nissen fundoplication with a robotic system in a child. Surg Endosc. (2001) 15(11):1360. doi: 10.1007/s00464-001-4200-3
16. Howe A, Kozel Z, Palmer L. Robotic surgery in pediatric urology. Asian Journal of Urology. (2017) 4(1):55–67. doi: 10.1016/j.ajur.2016.06.002
17. Andolfi C, Kumar R, Boysen WR, Gundeti MS. Current status of robotic surgery in pediatric urology. J Laparoend & Adv Surgl Tech Part A. (2019) 29(2):159–66. doi: 10.1089/lap.2018.0745
18. Rassweiler J, Binder J, Frede T. Robotic and telesurgery: will they change our future? Curr Opin Urol. (2001) 11(3):309–20. doi: 10.1097/00042307-200105000-00012
19. Gettman MT, Peschel R, Neururer R, Bartsch G. A comparison of laparoscopic pyeloplasty performed with the davinci robotic system versus standard laparoscopic techniques: initial clinical results. Eur Urol. (2002) 42(5):453–7; discussion 7–8. doi: 10.1016/s0302-2838(02)00373-1
20. Cundy TP, Harling L, Hughes-Hallett A, Mayer EK, Najmaldin AS, Athanasiou T, et al. Meta-analysis of robot-assisted vs conventional laparoscopic and open pyeloplasty in children. BJU Int. (2014) 114(4):582–94. doi: 10.1111/bju.12683
21. Autorino R, Eden C, El-Ghoneimi A, Guazzoni G, Buffi N, Peters CA, et al. Robot-assisted and laparoscopic repair of ureteropelvic junction obstruction: a systematic review and meta-analysis. Eur Urol. (2014) 65(2):430–52. doi: 10.1016/j.eururo.2013.06.053
22. Light A, Karthikeyan S, Maruthan S, Elhage O, Danuser H, Dasgupta P. Peri-operative outcomes and complications after laparoscopic vs robot-assisted dismembered pyeloplasty: a systematic review and meta-analysis. BJU Int. (2018) 122(2):181–94. doi: 10.1111/bju.14170
23. Chang SJ, Hsu CK, Hsieh CH, Yang SS. Comparing the efficacy and safety between robotic-assisted versus open pyeloplasty in children: a systemic review and meta-analysis. World J Urol. (2015) 33(11):1855–65. doi: 10.1007/s00345-015-1526-3
24. Cundy TP, Harley SJD, Marcus HJ, Hughes-Hallett A, Khurana S. Global trends in paediatric robot-assisted urological surgery: a bibliometric and progressive scholarly acceptance analysis. J Robot Surg. (2018) 12(1):109–15. doi: 10.1007/s11701-017-0703-3
25. Gundeti MS, Kojima Y, Haga N, Kiriluk K. Robotic-assisted laparoscopic reconstructive surgery in the lower urinary tract. Curr Urol Rep. (2013) 14(4):333–41. doi: 10.1007/s11934-013-0328-7
26. Boysen WR, Ellison JS, Kim C, Koh CJ, Noh P, Whittam B, et al. Multi-institutional review of outcomes and complications of robot-assisted laparoscopic extravesical ureteral reimplantation for treatment of primary vesicoureteral reflux in children. J Urol. (2017) 197(6):1555–61. doi: 10.1016/j.juro.2017.01.062
27. Kurtz MP, Leow JJ, Varda BK, Logvinenko T, Yu RN, Nelson CP, et al. Robotic versus open pediatric ureteral reimplantation: costs and complications from a nationwide sample. J Pediatr Urol. (2016) 12(6):408.e1–e6. doi: 10.1016/j.jpurol.2016.06.016
28. Baek M, Koh CJ. Lessons learned over a decade of pediatric robotic ureteral reimplantation. Investig and Clin Urol. (2017) 58(1):3–11. doi: 10.4111/icu.2017.58.1.3
29. Bansal D, Cost NG, Bean CM, Riachy E, Defoor WR Jr., Reddy PP, et al. Comparison of pediatric robotic-assisted laparoscopic nephroureterectomy and laparoendoscopic single-site nephroureterectomy. Urology. (2014) 83(2):438–42. doi: 10.1016/j.urology.2013.08.066
30. Lee RS, Sethi AS, Passerotti CC, Peters CA. Robot-assisted laparoscopic nephrectomy and contralateral ureteral reimplantation in children. J Endourol. (2010) 24(1):123–8. doi: 10.1089/end.2009.0271
31. Spinoit A, Ploumidis A, Novara G, Mottrie A. Robot-assisted single-site upper pole hemi-nephrectomy in an adult patient with a duplicated collecting system: is it feasible? Minerva Urol Nefrol. (2016) 68(5):466–8.26377890
32. Lee NG, Corbett ST, Cobb K, Bailey GC, Burns AS, Peters CA. Bi-institutional comparison of robot-assisted laparoscopic versus open ureteroureterostomy in the pediatric population. J Endourol. (2015) 29(11):1237–41. doi: 10.1089/end.2015.0223
33. Pedraza R, Weiser A, Franco I. Laparoscopic appendicovesicostomy (mitrofanoff procedure) in a child using the Da vinci robotic system. J Urol. (2004) 171(4):1652–3. doi: 10.1097/01.ju.0000116066.72132.9a
34. Murthy P, Cohn JA, Selig RB, Gundeti MS. Robot-assisted laparoscopic augmentation ileocystoplasty and mitrofanoff appendicovesicostomy in children: updated interim results. Eur Urol. (2015) 68(6):1069–75. doi: 10.1016/j.eururo.2015.05.047
35. Adamic B, Kirkire L, Andolfi C, Labbate C, Aizen J, Gundeti M. Robot-assisted laparoscopic augmentation ileocystoplasty and mitrofanoff appendicovesicostomy in children: step-by-step and modifications to UChicago technique. BJUI compass. (2020) 1(1):32–40. doi: 10.1002/bco2.7
36. Fernandez N, Farhat WA. A comprehensive analysis of robot-assisted surgery uptake in the pediatric surgical discipline. Front Surg. (2019) 6:9. doi: 10.3389/fsurg.2019.00009
37. Hambraeus M, Arnbjornsson E, Anderberg M. A literature review of the outcomes after robot-assisted laparoscopic and conventional laparoscopic Nissen fundoplication for gastro-esophageal reflux disease in children. Int J Med Robot+Comp Ass Surg: MRCAS. (2013) 9(4):428–32. doi: 10.1002/rcs.1517
38. Kulaylat AN, Richards H, Yada K, Coyle D, Shelby R, Onwuka AJ, et al. Comparative analysis of robotic-assisted versus laparoscopic cholecystectomy in pediatric patients. J Pediatr Surg. (2021) 56(10):1876–80. doi: 10.1016/j.jpedsurg.2020.11.013
39. Klazura G, Graf A, Sims T, Rojnica M, Koo N, Lobe TE. Assessment of the Da Vinci single port robotic platform on cholecystectomy in adolescents. J Laparoend & Adv Surg Tech Part A. (2022) 32(4):438–41. doi: 10.1089/lap.2021.0674
40. Chang EY, Hong YJ, Chang HK, Oh JT, Han SJ. Lessons and tips from the experience of pediatric robotic choledochal cyst resection. J Laparoend & Adv Surg Tech Part A. (2012) 22(6):609–14. doi: 10.1089/lap.2011.0503
41. Alizai NK, Dawrant MJ, Najmaldin AS. Robot-assisted resection of choledochal cysts and hepaticojejunostomy in children. Pediatr Surg Int. (2014) 30(3):291–4. doi: 10.1007/s00383-013-3459-5
42. Kim NY, Chang EY, Hong YJ, Park S, Kim HY, Bai SJ, et al. Retrospective assessment of the validity of robotic surgery in comparison to open surgery for pediatric choledochal cyst. Yonsei Med J. (2015) 56(3):737–43. doi: 10.3349/ymj.2015.56.3.737
43. Woo R, Le D, Albanese CT, Kim SS. Robot-assisted laparoscopic resection of a type I choledochal cyst in a child. J Laparoend & Adv Surg Tech Part A. (2006) 16(2):179–83. doi: 10.1089/lap.2006.16.179
44. Wang XQ, Xu SJ, Wang Z, Xiao YH, Xu J, Wang ZD, et al. Robotic-assisted surgery for pediatric choledochal cyst: case report and literature review. World J Clin Cases. (2018) 6(7):143–9. doi: 10.12998/wjcc.v6.i7.143
45. Koga H, Murakami H, Ochi T, Miyano G, Lane GJ, Yamataka A. Comparison of robotic versus laparoscopic hepaticojejunostomy for choledochal cyst in children: a first report. Pediatr Surg Int. (2019) 35(12):1421–5. doi: 10.1007/s00383-019-04565-3
46. Rong L, Li Y, Tang J, Cao G, Wan L, Li X, et al. Robotic-assisted choledochal cyst excision with roux-en-Y hepaticojejunostomy in children: does age matter? Surg Endosc. (2023) 37(1):274–81. doi: 10.1007/s00464-022-09496-0
47. Quynh TA, Hien PD, Du LQ, Long LH, Tran NTN, Hung T. The follow-up of the robotic-assisted soave procedure for Hirschsprung's disease in children. J Robot Surg. (2022) 16(2):301–5. doi: 10.1007/s11701-021-01238-z
48. Chang X, Cao G, Pu J, Li S, Zhang X, Tang ST. Robot-assisted anorectal pull-through for anorectal malformations with rectourethral and rectovesical Fistula: feasibility and short-term outcome. Surg Endosc. (2022) 36(3):1910–5. doi: 10.1007/s00464-021-08473-3
49. Meehan JJ. Robotic repair of congenital duodenal atresia: a case report. J Pediatr Surg. (2007) 42(7):E31–3. doi: 10.1016/j.jpedsurg.2007.05.004
50. Butter A, Jayaraman S, Schlachta C. Robotic duodenojejunostomy for superior mesenteric artery syndrome in a teenager. J Robot Surg. (2010) 4(4):265–9. doi: 10.1007/s11701-010-0215-x
51. Dutta S, Woo R, Albanese CT. Minimal access portoenterostomy: advantages and disadvantages of standard laparoscopic and robotic techniques. J Laparoend & Adv Surg Tech Part A. (2007) 17(2):258–64. doi: 10.1089/lap.2006.0112
52. Meehan JJ, Elliott S, Sandler A. The robotic approach to complex hepatobiliary anomalies in children: preliminary report. J Pediatr Surg. (2007) 42(12):2110–4. doi: 10.1016/j.jpedsurg.2007.08.040
53. Cundy TP, Shetty K, Clark J, Chang TP, Sriskandarajah K, Gattas NE, et al. The first decade of robotic surgery in children. J Pediatr Surg. (2013) 48(4):858–65. doi: 10.1016/j.jpedsurg.2013.01.031
54. Rela M, Rajalingam R, Shetty G, Cherukuru R, Rammohan A. Robotic monosegment donor hepatectomy for pediatric liver transplantation: first report. Pediatr Transplant. (2022) 26(1):e14110. doi: 10.1111/petr.14110
55. Hu MG, Xiao YH, Song DD, Zhao GD, Liu YZ, Wang Z, et al. First experience of robotic spleen-preserving distal pancreatectomy in a child with insulinoma. World J Surg Oncol. (2017) 15(1):199. doi: 10.1186/s12957-017-1265-6
56. Schulte Am Esch J, Kruger M, Barthlen W, Forster C, Mohnike K, Empting S, et al. Technical aspects of paediatric robotic pancreatic enucleation based on a case of an insulinoma. Int J Med Robot+Comp Ass Surg: MRCAS. (2021) 17(6):e2317. doi: 10.1002/rcs.2317
57. Li Y, Cao G, Rong L, Hong M, Li X, Chi S, et al. Robotic lateral pancreaticojejunostomy surgery for pancreatic duct stones in children. J Pediatr Surg. (2021) 56(9):1685–6. doi: 10.1016/j.jpedsurg.2021.04.021
58. Hagendoorn J, Nota C, Borel Rinkes IHM, Molenaar IQ. Robotic pancreatoduodenectomy for a solid pseudopapillary tumor in a ten-year-old child. Surg Oncol. (2018) 27(4):635–6. doi: 10.1016/j.suronc.2018.07.013
59. Lalli R, Merritt N, Schlachta CM, Butter A. Robotic-assisted, spleen-preserving distal pancreatectomy for a solid pseudopapillary tumour in a pediatric patient: a case report and review of the literature. J Robot Surg. (2019) 13(2):325–9. doi: 10.1007/s11701-018-0835-0
60. Ballouhey Q, Villemagne T, Cros J, Vacquerie V, Berenguer D, Braik K, et al. Assessment of paediatric thoracic robotic surgery. Interact Cardiovasc Thorac Surg. (2015) 20(3):300–3. doi: 10.1093/icvts/ivu406
61. Meehan JJ, Sandler A. Robotic repair of a Bochdalek congenital diaphragmatic hernia in a small neonate: robotic advantages and limitations. J Pediatr Surg. (2007) 42(10):1757–60. doi: 10.1016/j.jpedsurg.2007.06.013
62. Durand M, Musleh L, Vatta F, Orofino G, Querciagrossa S, Jugie M, et al. Robotic lobectomy in children with severe bronchiectasis: a worthwhile new technology. J Pediatr Surg. (2021) 56(9):1606–10. doi: 10.1016/j.jpedsurg.2020.11.009
63. Altokhais T, Mandora H, Al-Qahtani A, Al-Bassam A. Robot-assisted Heller's myotomy for achalasia in children. Comp Ass Surg. (2016) 21(1):127–31. doi: 10.1080/24699322.2016.1217352
64. Li S, Cao G, Zhou R, Zhang X, Zhou Y, Tang ST. Feasible techniques in robotic thoracoscopic repair of congenital esophageal atresia: case report and literature review. Surg Case Rep. (2021) 7(1):142. doi: 10.1186/s40792-021-01229-0
65. Ferrero PA, Blanc T, Binet A, Arnaud A, Abbo O, Vatta F, et al. The potential and the limitations of esophageal robotic surgery in children. Eur J Pediatr Surg. (2022) 32(2):170–6. doi: 10.1055/s-0040-1721770
66. Anderberg M, Backman T, Annerstedt M. Robot-assisted radical cystoprostatectomy in a small child with rhabdomyosarcoma: a case report. J Robot Surg. (2008) 2(2):101–3. doi: 10.1007/s11701-008-0089-3
67. Cost NG, Geller JI, DeFoor WR Jr., Wagner LM, Noh PH. A robotic-assisted laparoscopic approach for pediatric renal cell carcinoma allows for both nephron-sparing surgery and extended lymph node dissection. J Pediatr Surg. (2012) 47(10):1946–50. doi: 10.1016/j.jpedsurg.2012.08.017
68. Rogers CG, Blatt AM, Miles GE, Linehan WM, Pinto PA. Concurrent robotic partial adrenalectomy and extra-adrenal pheochromocytoma resection in a pediatric patient with Von Hippel-Lindau disease. J Endourol. (2008) 22(7):1501–3. doi: 10.1089/end.2007.0314
69. Erkul E, Duvvuri U, Mehta D, Aydil U. Transoral robotic surgery for the pediatric head and neck surgeries. Eur Arch Oto-Rhino-Laryngol. (2017) 274(3):1747–50. doi: 10.1007/s00405-016-4425-3
70. Wu EL, Garstka ME, Kang SW, Kandil E. Robotic neck surgery in the pediatric population. JSLS: J Soci Laparoend Surg. (2018) 22(3):e2018.00012. doi: 10.4293/JSLS.2018.00012
71. Venkatakarthikeyan C, Nair S, Gowrishankar M, Rao S. Robotic surgery in head and neck in pediatric population: our experience. Indian J Otolaryngol Head Neck Surg. (2020) 72(1):98–103. doi: 10.1007/s12070-019-01768-x
72. Lobe TE, Wright SK, Irish MS. Novel uses of surgical robotics in head and neck surgery. J Laparoend & Adv Surg Tech Part A. (2005) 15(6):647–52. doi: 10.1089/lap.2005.15.647
73. Sheth KR, Koh CJ. The future of robotic surgery in pediatric urology: upcoming technology and evolution within the field. Front Pediatr. (2019) 7:259. doi: 10.3389/fped.2019.00259
74. Rowe CK, Pierce MW, Tecci KC, Houck CS, Mandell J, Retik AB, et al. A comparative direct cost analysis of pediatric urologic robot-assisted laparoscopic surgery versus open surgery: could robot-assisted surgery be less expensive? J Endourol. (2012) 26(7):871–7. doi: 10.1089/end.2011.0584
75. Bergholz R, Botden S, Verweij J, Tytgat S, Van Gemert W, Boettcher M, et al. Evaluation of a new robotic-assisted laparoscopic surgical system for procedures in small cavities. J Robot Surg. (2020) 14(1):191–7. doi: 10.1007/s11701-019-00961-y
76. Tan Wen Sheng B, Wong P, Teo Ee Hoon C. Transoral robotic excision of laryngeal papillomas with flex(R) robotic system – a novel surgical approach. Am J Otolaryngol. (2018) 39(3):355–8. doi: 10.1016/j.amjoto.2018.03.011
Keywords: robotic-assisted, robotic surgery, children, pediatric surgery, minimally invasive surgery
Citation: Mei H and Tang ST (2023) Robotic-assisted surgery in the pediatric surgeons’ world: Current situation and future prospectives. Front. Pediatr. 11:1120831. doi: 10.3389/fped.2023.1120831
Received: 10 December 2022; Accepted: 24 January 2023;
Published: 14 February 2023.
Edited by:
Satoshi Ieiri, Kagoshima University, JapanReviewed by:
Yuichi Okata, Kobe University, JapanKeigo Yada, St. Luke's International Hospital, Japan
© 2023 Mei and Tang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tang Shao-tao tshaotao83@126.com
Specialty Section: This article was submitted to Pediatric Surgery, a section of the journal Frontiers in Pediatrics
 Hong Mei
Hong Mei Shaotao Tang
Shaotao Tang